The Effectiveness of Shoulder Mobility and Strength Programs in Competitive Water-Polo Players
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Girdwood, M.; Webster, M. Quantifying the burden of shoulder and hip pain in water polo players across different playing levels. Int. J. Sports Phys. Ther. 2021, 16, 57–63. [Google Scholar] [CrossRef]
- Croteau, F.; Brown, H.; Pearsall, D.; Robbins, S.M. Prevalence and mechanisms of injuries in water polo: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e001081. [Google Scholar] [CrossRef]
- Stromberg, J.D. Care of water polo players. Curr. Sports Med. Rep. 2017, 16, 363–369. [Google Scholar] [CrossRef]
- Mountjoy, M.; Miller, J.; Junge, A. Analysis of water polo injuries during 8904 player matches at FINA World Championships and Olympic games to make the sport safer. Br. J. Sports Med. 2019, 53, 25–31. [Google Scholar] [CrossRef]
- Cools, A.M.; Johansson, F.R.; Borms, D.; Maenhout, A. Prevention of shoulder injuries in overhead athletes: A science-based approach. Brazilian J. Phys. Ther. 2015, 19, 331–339. [Google Scholar] [CrossRef] [Green Version]
- Burn, M.; McCulloch, P.; Linter, D.; Liberman, S.; Harris, J. Prevalence of scapular dyskinesis in overhead and no overhead athletes: A systematic review. Orthop. J. Sports Med. 2016, 4, 2325967115627608. [Google Scholar] [CrossRef] [Green Version]
- Webster, M.J.; Morris, M.E.; Galna, B. Shoulder pain in water polo: A systematic review of the literature. J. Sci. Med. Sport 2009, 12, 3–11. [Google Scholar] [CrossRef]
- Cejudo, A.; Sánchez-Castillo, S.; Sainz de Baranda, P.; Gámez, J.C.; Santonja-Medina, F. Low range of shoulders horizontal abduction predisposes for shoulder pain in competitive young swimmers. Front. Psychol. 2019, 6, 478. [Google Scholar] [CrossRef]
- Wilk, K.; Bagwell, M.; Davies, G.; Arrigo, C. Return to sport participation criteria following shoulder injury: A clinical commentary. Int. Sports Phys. Ther. 2020, 15, 624–642. [Google Scholar] [CrossRef]
- Witner, A.; Sauers, E. Clinical measures of shoulder mobility in college water-polo players. J. Sport Rehabil. 2006, 15, 45–47. [Google Scholar]
- McMaster, W.C.; Long, S.C.; Caiozzo, V.J. Isokinetic torque imbalances in the rotator cuff of the elite water polo player. Am. J. Sports Med. 1991, 19, 72–75. [Google Scholar] [CrossRef]
- Segawa, E.; Komori, Y.; Hojo, T. The relationship between shoulder injuries and flexibility, shoulder rage of motion characteristics in elite male japanese water-polo players. Jpn. J. Phys. Fit Sport Med. 2017, 66, 263–269. [Google Scholar]
- Witvrouw, E.; Danneels, L.; Asselman, P.; D’Have, T.; Cambier, D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players. A prospective study. Am. J. Sports Med. 2003, 31, 41–46. [Google Scholar] [CrossRef]
- Eliot, J. Shoulder pain and flexibility in elite water-polo players. Physiother. Theory Pract. 1993, 79, 693–697. [Google Scholar] [CrossRef]
- Hams, A.; Evans, K.; Adams, R.; Waddington, G.; Witchalls, J. Reduced shoulder strength and change in range of motion are risk factors for shoulder injury in water polo players. Phys. Ther. Sport 2019, 40, 231–237. [Google Scholar] [CrossRef]
- Hams, A.H.; Evans, K.; Adams, R.; Waddington, G.; Witchalls, J. Throwing performance in water polo is related to in-water shoulder proprioception. J. Sports Sci. 2019, 37, 2588–2595. [Google Scholar] [CrossRef]
- Hams, A.H.; Evans, K.; Adams, R.; Waddington, G.; Witchalls, J. Shoulder internal and external rotation strength and prediction of subsequent injury in water-polo players. Scand. J. Med. Sci. Sports 2019, 29, 1414–1420. [Google Scholar] [CrossRef]
- Maestroni, L.; Read, P.; Bishop, C.; Turner, A. Strength and power training in rehabilitation: Underpinning principles and practical strategies to return athletes to high performance. Sports Med. 2020, 50, 239–252. [Google Scholar] [CrossRef]
- Croteau, F.; Paradelo, D.; Pearsall, D.; Robbins, S. Risk factors for shoulder injuries in water polo: A cohort study. Int. J. Sports Phys. Ther. 2021, 16, 135–144. [Google Scholar] [CrossRef]
- Terol-Sanchis, M.; Elvira-Aranda, C.; Gomis-Gomis, M.J.; Pérez-Turpin, J.A. The relationship between speed and strength in the beach volleyball serve. J. Hum. Kinet. 2021, 80, 39–47. [Google Scholar] [CrossRef]
- Iacono, A.; Dello, V.S.; Sanderson, M.; Halperin, I. The isometric horizontal push test: Test-retest reliability and validation study. Int. J. Sports Physiol. Perform. 2020, 15, 581–584. [Google Scholar] [CrossRef]
- Makowski, D.; Mattan, B.; Lüdecke, D. BayestestR: Describing effects and their uncertainty, existence and significance within the bayesian framework. J. Open Source Softw. 2019, 4, 1541. [Google Scholar] [CrossRef]
- Kaćanski, I.; Gava, B.P.; Soldatović, S. Analysis of the shoulder joint mobility in overhead sports before and after experimental treatment. Med. Pregl. 2011, 64, 539–544. [Google Scholar] [CrossRef]
- Yanai, T.; Hay, J.G.; Miller, G.F. Shoulder impingement in front-crawl swimming: I. A method to identify impingement. Med. Sci. Sports Exerc. 2000, 32, 21–29. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Porterfield, R. Simpson. C.D.; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am. J. Sports Med. 2011, 39, 329–335. [Google Scholar] [CrossRef]
- Borsa, P.A.; Laudner, K.G.; Sauers, E.L. Mobility and stability adaptations in the shoulder of the overhead athlete: A theoretical and evidence-based perspective. Sports Med. 2008, 38, 17–36. [Google Scholar] [CrossRef]
- Holt, K.; Boettcher, C.; Halaki, M.; Ginn, K.A. Humeral torsion and shoulder rotation range of motion parameters in elite swimmers. J. Sci. Med. Sport 2017, 20, 469–474. [Google Scholar] [CrossRef]
- Myklebust, G.; Hasslan, L.; Bahr, R.; Steffen, K. High prevalence of shoulder pain among elite Norwegian female handball players. Scand. J. Med. Sci. Sports 2013, 23, 288–294. [Google Scholar] [CrossRef]
- Ellenbecker, T.S.; Roetert, E.P.; Bailie, D.S.; Davies, G.J.; Brown, S.W. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med. Sci. Sports Exerc. 2002, 34, 2052–2056. [Google Scholar] [CrossRef]
- Byram, I.R.; Bushnell, B.D.; Dugger, K.; Charron, K.; Harrell, F.E.; Noonan, T.J. Preseason shoulder strength measurements in professional baseball pitchers: Identifying players at risk for injury. Am. J. Sports Med. 2010, 38, 1375–1382. [Google Scholar] [CrossRef]
- Clarsen, B.; Bahr, R.; Andersson, S.H.; Munk, R.; Myklebust, G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br. J. Sports Med. 2014, 48, 1327–1333. [Google Scholar] [CrossRef]
- Alix-Fages, C.; Del Vecchio, A.; Baz-Valle, E.; Santos-Concejero, J.; Balsalobre-Fernández, C. The role of the neural stimulus in regulating skeletal muscle hypertrophy. Eur. J. Appl. Physiol. 2022, 122, 1111–1128. [Google Scholar] [CrossRef]
- Keiner, M.; Rähse, H.; Wirth, K.; Hartmann, H.; Fries, K.; Haff, G.G. Influence of maximal strength on in-water and dry-land performance in young water polo players. J. Strength Cond. Res. 2020, 34, 1999–2005. [Google Scholar] [CrossRef]
- Martin, M.S.; Pareja-Blanco, F.; De Villarreal, E.S. Effects of different in-season strength training methods on strength gains and water polo performance. Int. J. Sports Physiol. Perform. 2021, 16, 591–600. [Google Scholar] [CrossRef]
- Hibberd, E.E.; Oyama, S.; Spang, J.T.; Prentice, W.; Myers, J.B. Effect of a 6-week strengthening program on shoulder and scapular-stabilizer strength and scapular kinematics in division I collegiate swimmers. J. Sport Rehabil. 2012, 21, 253–265. [Google Scholar] [CrossRef]
- Swanik, K.; Swanik, C.; Lephart, S.M.; Huxel, K. The effect of functional training on the incidence of shoulder pain and strength in intercollegiate swimmers. J. Sport Rehabil. 2002, 11, 142–154. [Google Scholar] [CrossRef]
- Leppänen, M.; Aaltonen, S.; Parkkari, J.; Heinonen, A.; Kujala, U.M. Interventions to prevent sports related injuries: A systematic review and meta-analysis of randomised controlled trials. Sports Med. 2014, 44, 473–486. [Google Scholar] [CrossRef]
- Batalha, N.; Marmeleira, J.; Garrido, N.; Silva, A.J. Does a water-training macrocycle really create imbalances in swimmers’ shoulder rotator muscles? Eur. J. Sport Sci. 2015, 15, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Yildiz, Y.; Aydin, T.; Sekir, U.; Kiralp, M.Z.; Hazneci, B.; Kalyon, T.A. Shoulder terminal range eccentric antagonist/concentric agonist strength ratios in overhead athletes. Scand. J. Med. Sci. Sports 2006, 16, 174–180. [Google Scholar] [CrossRef]
- Tooth, C.; Gofflot, A.; Schwartz, C.; Croisier, J.L.; Beaudart, C.; Bruyère, O.; Forthomme, B. Risk factors of overuse shoulder injuries in overhead athletes: A sistematic review. Sports Health 2020, 12, 478–487. [Google Scholar] [CrossRef]
- McElreath, R. Statistical Rethinking: A Bayesian Course with Examples in R and Stan, 2nd ed.; CRC Press/Taylor & Francis Group: Boca Raton, FL, USA, 2020. [Google Scholar]
| Weeks and Days | Sets × Reps | Exercises |
|---|---|---|
| 6 weeks 3 days per week | 3 × 15 | Shoulder flexion; shoulder extension; IR at 90°; ER at 90°; throwing acceleration; throwing deceleration; low rows; scapular punches; Y’s; T´s; W´s |
| Exercise | Muscular activity | Characteristic addressed |
| Shoulder flexion | DA, Rhomb, SA, Sub, RM | Strengthen scapular stabilizers |
| Shoulder extension | Dors, Rhomb, Sub, Tri, RM | |
| IR at 90° | TI, Rhomb, SA, Sub, RM | |
| ER at 90° | TI, Rhomb, SA, Sub, Supra, RM | Strengthen scapular stabilizers, weak ER |
| Throwing acceleration | TI, Rhomb, SA, Sub, RM | Strengthen scapular stabilizers, improve propioception |
| Throwing decceleration | TI, Rhomb, Sub, Supra, RM, TS | Weak ER, improve propioception |
| Low rows | Rhomb, Sub. RM | Strengthen scapular stabilizers |
| Scapular punches | Rhomb, SA, Sub, RM | Strengthen SA |
| Y arms movement | TI, TM, SA | Strengthen scapular stabilizers, increases scapular up rotation, post tilt, retraction, and ER |
| T arms movement | Infra, TM, SA, RM, TS | |
| W arms movement | Infra, TI, Rhomb, Supra, RM |
| Cgroup (n = 10) | Wgroup (n = 9) | WIgroup (n = 9) | Overall (n = 28) | |
|---|---|---|---|---|
| Age (y) | 22.2 ± 1.2 | 18.6 ± 2.4 | 19.8 ± 2.5 | 20.1 ± 2.5 |
| Height (cm) | 176.7 ± 5.3 | 177.2 ± 3.7 | 178. 7 ± 6.8 | 176.9 ± 6.2 |
| Body mass (kg) | 72.2 ± 5.1 | 75.1 ± 7.7 | 74.4 ± 7.8 | 74.6 ± 8.1 |
| Cgroup (n = 10) | Wgroup (n = 9) | WIgroup (n = 9) | ||
|---|---|---|---|---|
| Shoulder Range of Motion (°). | ||||
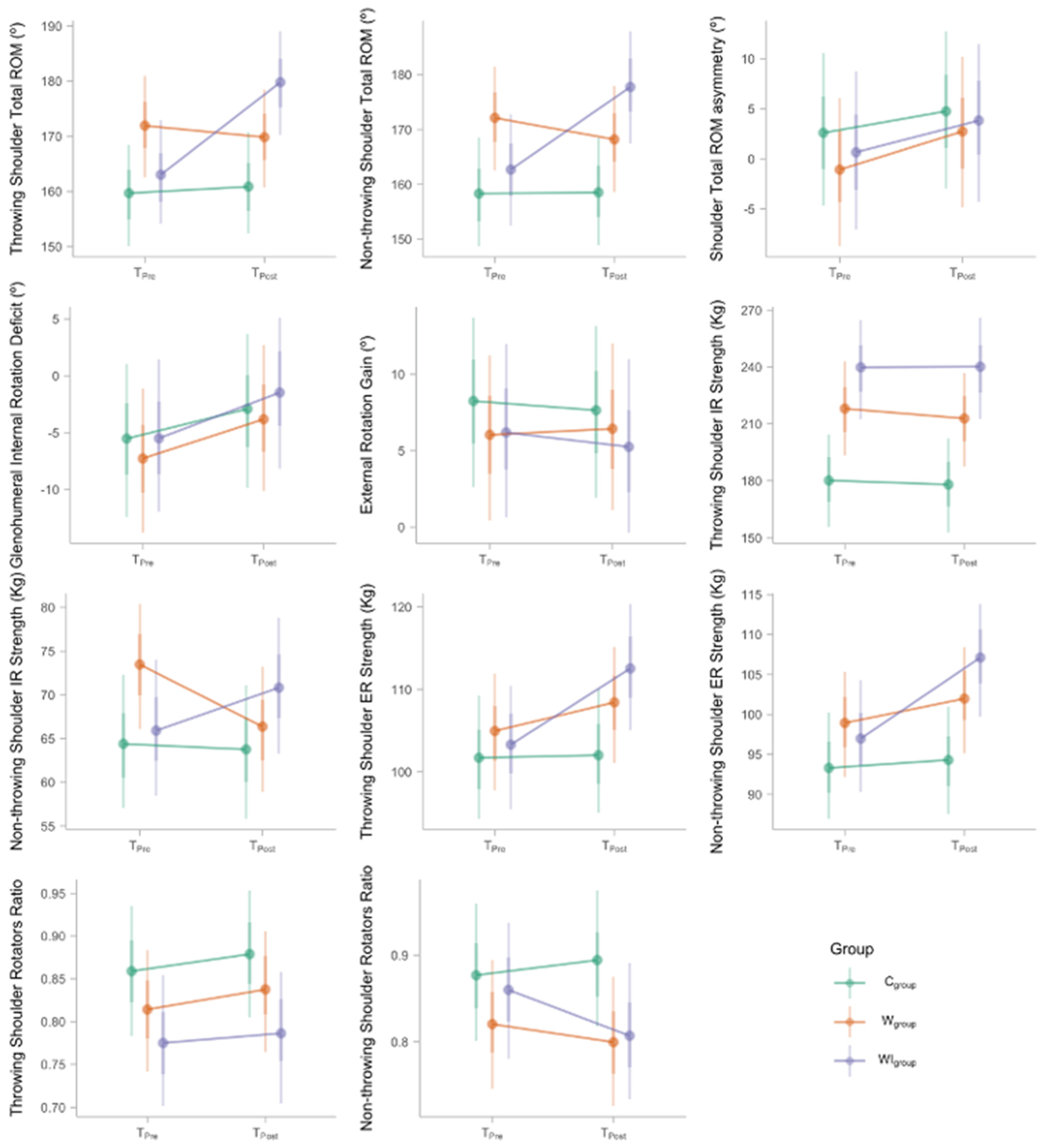
| Throwing shoulder Total ROM | TPre | 160 (150–169) | 172 (163–181) | 163 (154–173) |
| TPost | 161 (152–171) | 170 (161–179) | 180 (170–189) | |
| Non-throwing shoulder Total ROM | TPre | 158 (149–168) | 172 (163–181) | 163 (152–173) |
| TPost | 157 (149–169) | 167 (159–178) | 178 (167–188) | |
| Total ROM asymmetry | TPre | 3 (−5–11) | −1 (−9–6) | 0 (−7–9) |
| TPost | 5 (−3–13) | 3 (−5–10) | 4 (−4–11) | |
| GIRD | TPre | −5 (−12–1) | −7 (−14–−1) | −6 (−12–1) |
| TPost | −3 (−10–4) | −4 (−10–3) | −2 (−8–5) | |
| ERG | TPre | 9 (3–14) | 6 (0–11) | 6 (1–12) |
| TPost | 8 (2–13) | 6 (1–12) | 5 (0–11) | |
| Shoulder Strength (kg) | ||||
| Throwing shoulder IR strength | TPre | 181 (156–204) | 218 (193–243) | 241 (212–265) |
| TPost | 180 (153–202) | 212 (187–237) | 239 (212–266) | |
| Non-throwing shoulder IR strength | TPre | 64 (57–72) | 73 (66–80) | 66 (58–74) |
| TPost | 63 (56–71) | 66 (59–73) | 71 (63–79) | |
| Throwing shoulder ER strength | TPre | 102 (94–109) | 105 (98–112) | 103 (95–110) |
| TPost | 102 (95–110) | 108 (101–115) | 113 (105–120) | |
| Non-throwing shoulder ER strength | TPre | 93 (87–100) | 99 (92–105) | 96 (90–104) |
| TPost | 95 (88–101) | 102 (95–108) | 107 (100–114) | |
| Throwing shoulder Rotators Ratio | TPre | 0.86 (0.78–0.94) | 0.81 (0.74–0.88) | 0.78 (0.70–0.85) |
| TPost | 0.88 (0.80–0.95) | 0.83 (0.76–0.91) | 0.79 (0.70–0.86) | |
| Non-throwing shoulder Rotators Ratio | TPre | 0.87 (0.80–0.96) | 0.82 (0.75–0.89) | 0.86 (0.78–0.94) |
| TPost | 0.90 (0.82–0.98) | 0.80 (0.73–0.88) | 0.81 (0.73–0.89) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Laval, I.; Sitko, S.; Cantonero, J.; Corbi, F.; Cirer-Sastre, R. The Effectiveness of Shoulder Mobility and Strength Programs in Competitive Water-Polo Players. Life 2022, 12, 758. https://doi.org/10.3390/life12050758
López-Laval I, Sitko S, Cantonero J, Corbi F, Cirer-Sastre R. The Effectiveness of Shoulder Mobility and Strength Programs in Competitive Water-Polo Players. Life. 2022; 12(5):758. https://doi.org/10.3390/life12050758
Chicago/Turabian StyleLópez-Laval, Isaac, Sebastian Sitko, Jaime Cantonero, Francisco Corbi, and Rafel Cirer-Sastre. 2022. "The Effectiveness of Shoulder Mobility and Strength Programs in Competitive Water-Polo Players" Life 12, no. 5: 758. https://doi.org/10.3390/life12050758
APA StyleLópez-Laval, I., Sitko, S., Cantonero, J., Corbi, F., & Cirer-Sastre, R. (2022). The Effectiveness of Shoulder Mobility and Strength Programs in Competitive Water-Polo Players. Life, 12(5), 758. https://doi.org/10.3390/life12050758








