Gustatory and Saliva Secretory Dysfunctions in COVID-19 Patients with Zinc Deficiency
Abstract
1. Introduction
2. Materials and Methods
3. Results
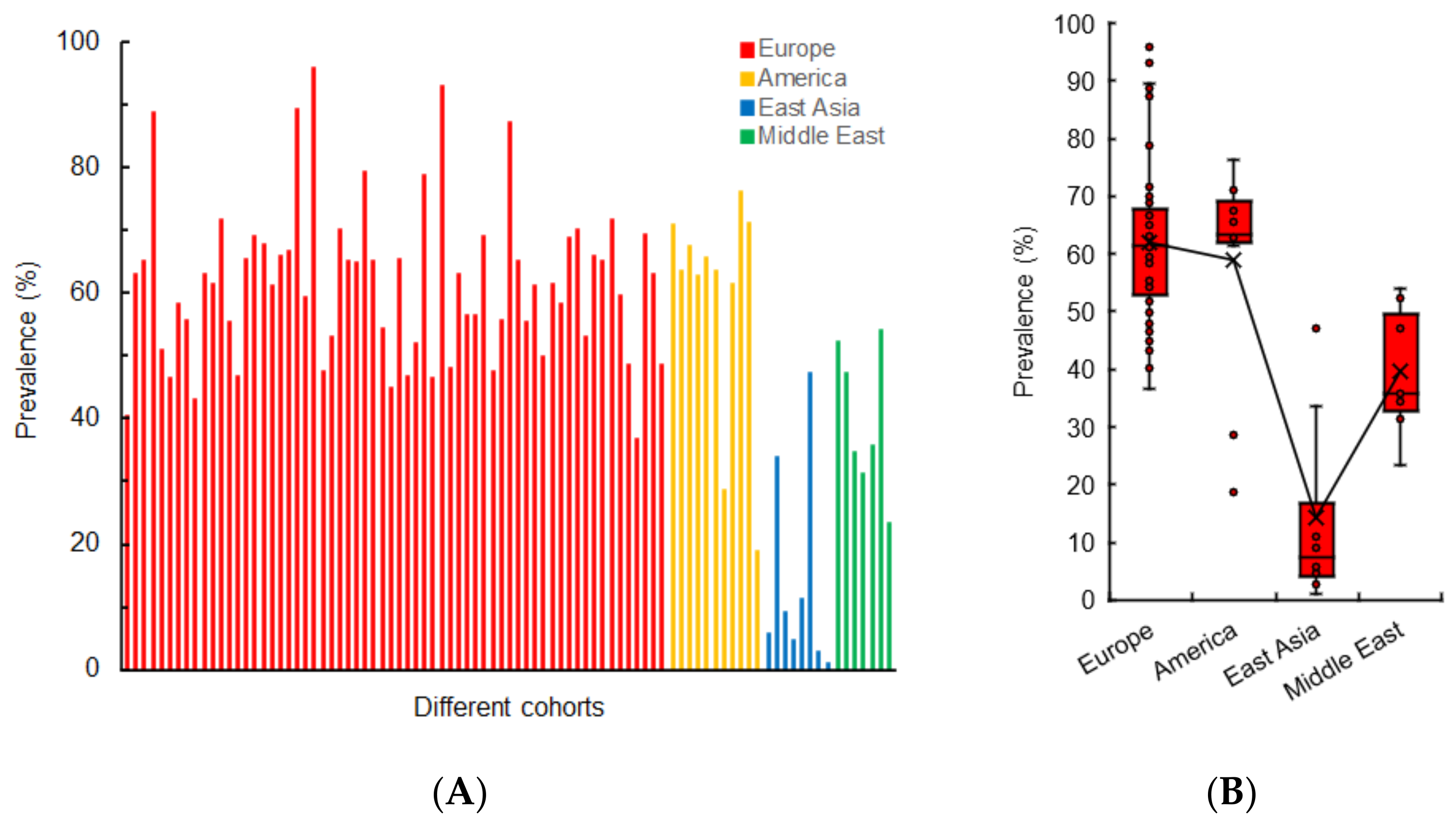
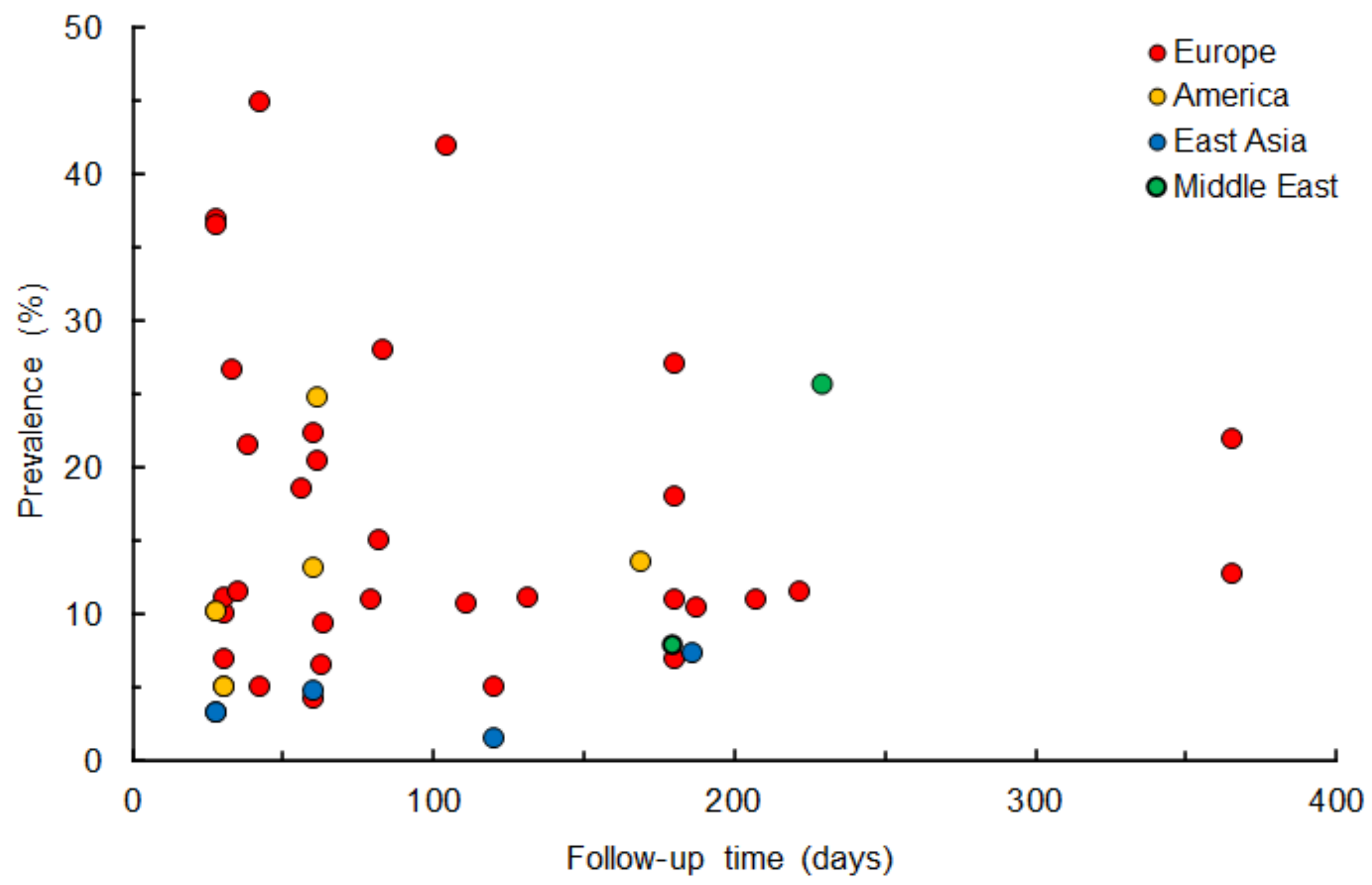
3.1. Gustatory Dysfunction
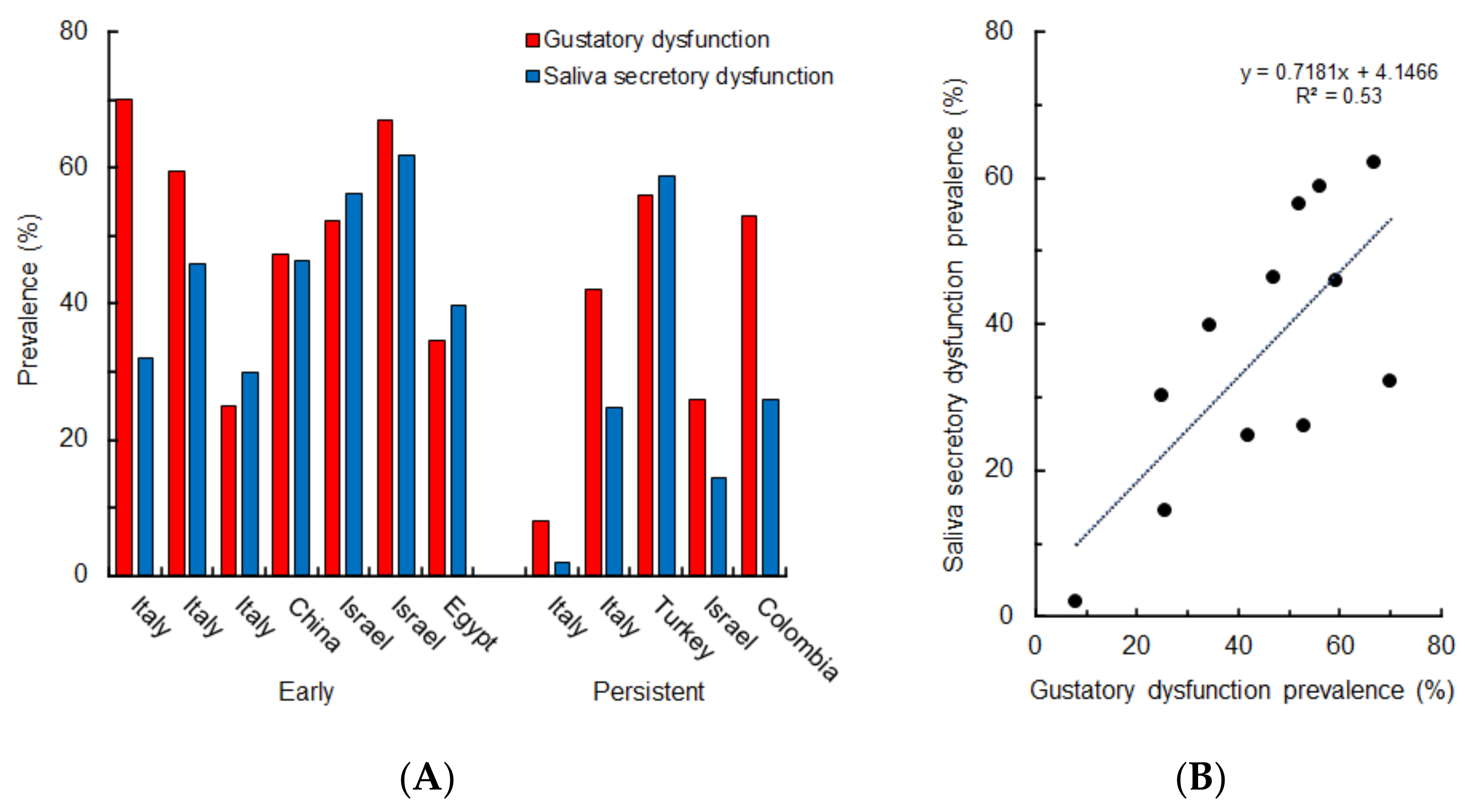
3.2. Saliva Secretory Dysfunction
3.3. Cooccurrence of Oral Symptoms
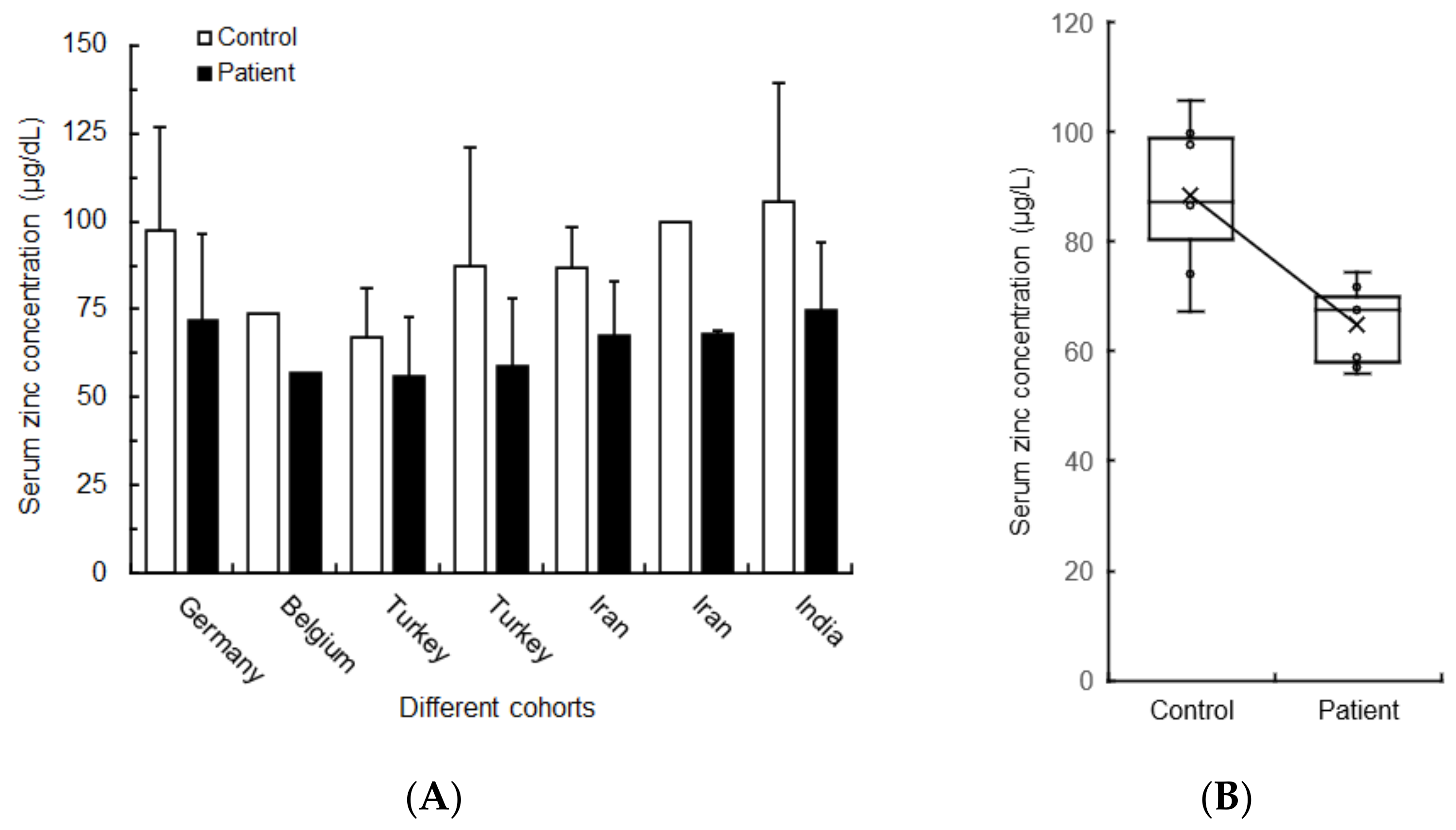
3.4. Hypozincemia Characterizing COVID-19 Patients
4. Discussion
4.1. Pathogenic Speculation from the Perspective of Zinc Deficiency
4.2. Zinc and Zinc-Metalloenzyme Carbonic Anhydrase
4.3. Cellular Zinc Homeostasis
4.4. Metallothionein
4.5. Zinc Transporter
4.6. Zinc Supplementation
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Passarelli, P.C.; Lopez, M.A.; Mastandrea Bonaviri, G.N.; Garcia-Godoy, F.; D’Addona, A. Taste and smell as chemosensory dysfunctions in COVID-19 infection. Am. J. Dent. 2020, 33, 135–137. [Google Scholar]
- Vaira, L.A.; Salzano, G.; Deiana, G.; De Riu, G. Anosmia and ageusia: Common findings in COVID-19 patients. Laryngoscope 2020, 130, 1787. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; De Siati, D.R.; Horoi, M.; Le Bon, S.D.; Dodriguez, A.; Dequanter, D.; Blecic, S.; El Afia, F.; Distinguin, L.; et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur. Arch. Otorhinolaryngol. 2020, 277, 2251–2261. [Google Scholar] [CrossRef] [PubMed]
- Amorim Dos Santos, J.; Normando, A.G.C.; Carvalho da Silva, R.L.; Acevedo, A.C.; De Luca Canto, G.; Sugaya, N.; Santos-Silva, A.R.; Guerra, E.N.S. Oral manifestations in patients with COVID-19: A living systematic review. J. Dent. Res. 2021, 100, 141–154. [Google Scholar] [CrossRef]
- Aragoneses, J.; Suárez, A.; Algar, J.; Rodríguez, C.; López-Valverde, N.; Aragoneses, J.M. Oral manifestations of COVID-19: Updated systematic review with meta-analysis. Front. Med. 2021, 8, 726753. [Google Scholar] [CrossRef]
- Tsuchiya, H. Oral symptoms associated with COVID-19 and their pathogenic mechanisms: A literature review. Dent. J. 2021, 9, 32. [Google Scholar] [CrossRef]
- Nouchi, A.; Chastang, J.; Miyara, M.; Lejeune, J.; Soares, A.; Ibanez, G.; Saadoun, D.; Morélot-Panzini, C.; Similowski, T.; Amoura, Z.; et al. Prevalence of hyposmia and hypogeusia in 390 COVID-19 hospitalized patients and outpatients: A cross-sectional study. Eur. J. Microbiol. Infect. Dis. 2021, 40, 691–697. [Google Scholar] [CrossRef]
- dos Santos, J.A.; Normando, A.G.C.; da Silva, R.L.C.; Acevedo, A.C.; De Luca Canto, G.; Sugaya, N.; Santos-Silva, A.R.; Guerra, E.N.S. Oral manifestations in patients with COVID-19: A 6-month update. J. Dent. Res. 2021, 100, 1321–1329. [Google Scholar] [CrossRef]
- Tsuchiya, H. Characterization and pathogenic speculation of xerostomia associated with COVID-19: A narrative review. Dent. J. 2021, 9, 130. [Google Scholar] [CrossRef] [PubMed]
- Cooper, K.W.; Brann, D.H.; Farruggia, M.C.; Bhutani, S.; Pellegrino, R.; Tsukahara, T.; Weinreb, C.; Joseph, P.V.; Larson, E.D.; Parma, V.; et al. COVID-19 and the chemical senses: Supporting players take center stage. Neuron 2020, 107, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Okada, Y.; Yoshimura, K.; Toya, S.; Tsuchimochi, M. Pathogenesis of taste impairment and salivary dysfunction in COVID-19 patients. Jpn. Dent. Sci. Rev. 2021, 57, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, M.M.; Abuohashish, H.M.; Khairy, D.A.; Bugshan, A.S.; Khan, A.M.; Moothedath, M.M. Pathogenesis of dysgeusia in COVID-19 patients: A scoping review. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 1114–1134. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhao, J.; Peng, J.; Li, X.; Deng, X.; Geng, Z.; Shen, Z.; Guo, F.; Zhang, Q.; Jin, Y.; et al. Detection of 2019-nCoV in saliva and characterization of oral symptoms in COVID-19 patients. Cell Prolif. 2020, 53, e12923. [Google Scholar] [CrossRef]
- Moein, S.T.; Hashemian, S.M.; Mansourafshar, B.; Khorram-Tousi, A.; Tabarsi, P.; Doty, R.L. Smell dysfunction: A biomarker for COVID-19. Int. Forum Allergy Rhinol. 2020, 10, 944–950. [Google Scholar] [CrossRef]
- Yan, C.H.; Faraji, F.; Prajapati, D.P.; Boone, C.E.; DeConde, A.S. Association of chemosensory dysfunction and CODIV-19 in patients presenting with influenza-like symptoms. Int. Forum Allergy Rhinol. 2020, 10, 806–813. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef]
- Vaira, L.A.; Deiana, G.; Fois, A.G.; Pirina, P.; Madeddu, G.; De Vito, A.; Babudieri, S.; Petrocelli, M.; Serra, A.; Bussu, F.; et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases. Head Neck 2020, 42, 1252–1258. [Google Scholar] [CrossRef]
- Spinato, G.; Fabbris, C.; Polesel, J.; Cazzador, D.; Borsetto, D.; Hopkins, C.; Boscolo-Rizzo, P. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 2020, 323, 2089–2090. [Google Scholar] [CrossRef]
- Lapostolle, F.; Schneider, E.; Vianu, I.; Dollet, G.; Roche, B.; Berdah, J.; Michel, J.; Goix, L.; Chanzy, E.; Petrovic, T.; et al. Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: The COVID-call study. Intern. Emerg. Med. 2020, 15, 813–817. [Google Scholar] [CrossRef]
- Beltrán-Corbellini, Á.; Chico-García, J.L.; Martínez-Poles, J.; Rodríguez-Jorge, F.; Natera-Villalba, E.; Gómez-Corral, J.; Gómez-López, A.; Monreal, E.; Parra-Díaz, P.; Cortés-Cuevas, J.L.; et al. Acute-onset smell and taste disorders in the context of COVID-19: A pilot multicentre polymerase chain reaction based case-control study. Eur. J. Neurol. 2020, 27, 1738–1741. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, S.; Garcia-Telles, N.; Aggarwal, G.; Lavie, C.; Lippi, G.; Henry, B.M. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States. Diagnosis 2020, 7, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.; Chan, Y.F.; Teo, N.W.; Cherng, B.P.; Thien, S.Y.; Wong, H.M.; Wijaya, L.; Toh, S.T.; Tan, T.T. The role of self-reported olfactory and gustatory dysfunction as a screening criterion for suspected COVID-19. Eur. Arch. Otorhinolaryngol. 2020, 277, 2389–2390. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.H.; Faraji, F.; Prajapati, D.P.; Ostrander, B.T.; DeConde, A.S. Self-reported olfactory loss associates with outpatient clinical course. Int. Forum Allergy Rhinol. 2020, 10, 821–831. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.U.; Kim, M.-J.; Ra, S.H.; Lee, J.; Bae, S.; Jung, J.; Kim, S.H. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clin. Microbiol. Infect. 2020, 26, 948.e1–948.e3. [Google Scholar] [CrossRef] [PubMed]
- Luers, J.C.; Rokohl, A.C.; Loreck, N.; Wawer Matos, P.A.; Augustin, M.; Dewald, F.; Klein, F.; Lehmann, C.; Heindl, L.M. Olfactory and gustatory dysfunction in coronavirus disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2262–2264. [Google Scholar] [CrossRef]
- Lee, Y.; Min, P.; Lee, S.; Kim, S.W. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J. Korean Med. Sci. 2020, 35, e174. [Google Scholar] [CrossRef]
- Speth, M.M.; Singer-Cornelius, T.; Oberle, M.; Gengler, I.; Brockmeier, S.J.; Sedaghat, A.R. Olfactory dysfunction and sinonasal symptomatology in COVID-19: Prevalence, severity, timing, and associated characteristics. Otolaryngol. Head Neck Surg. 2020, 163, 114–120. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; Place, S.; Van Laethem, Y.; Cabaraux, P.; Mat, Q.; Huet, K.; Plzak, J.; Horoi, M.; Hans, S.; et al. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J. Intern. Med. 2020, 288, 335–344. [Google Scholar] [CrossRef]
- Roland, L.T.; Gurrola, J.G.; Loftus, P.A.; Cheung, S.W.; Chang, J.L. Smell and taste symptom-based predictive model for COVID-19 diagnosis. Int. Forum Allergy Rhinol. 2020, 10, 832–838. [Google Scholar] [CrossRef]
- Vaira, L.A.; Hopkins, C.; Salzano, G.; Petrocelli, M.; Melis, A.; Cucurullo, M.; Ferrari, M.; Gagliardini, L.; Pipolo, C.; Deiana, G.; et al. Olfactory and gustatory function impairment in COVID-19 patients: Italian objective multicenter-study. Head Neck 2020, 42, 1560–1569. [Google Scholar] [CrossRef] [PubMed]
- Menni, C.; Valdes, A.M.; Freidin, M.B.; Sudre, C.H.; Nguyen, L.H.; Drew, D.A.; Ganesh, S.; Varsavsky, T.; Cardoso, M.J.; El-Sayed Moustafa, J.S.; et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat. Med. 2020, 26, 1037–1040. [Google Scholar] [CrossRef] [PubMed]
- Dell’Era, V.; Farri, F.; Garzaro, G.; Gatto, M.; Aluffi Valletti, P.; Garzaro, M. Smell and taste disorders during COVID-19 outbreak: Cross-sectional study on 355 patients. Head Neck 2020, 42, 1591–1596. [Google Scholar] [CrossRef] [PubMed]
- Liguori, C.; Pierantozzi, M.; Spanetta, M.; Sarmati, L.; Cesta, N.; Iannetta, M.; Ora, J.; Mina, G.G.; Puxeddu, E.; Balbi, O.; et al. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav. Immun. 2020, 88, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Paderno, A.; Schreiber, A.; Grammatica, A.; Raffetti, E.; Tomasoni, M.; Gualtieri, T.; Taboni, S.; Zorzi, S.; Lombardi, D.; Deganello, A. Smell and taste alterations in COVID-19: A cross-sectional analysis of different cohorts. Int. Forum Allergy Rhinol. 2020, 10, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Qiu, C.; Cui, C.; Hautefort, C.; Haehner, A.; Zhao, J.; Yao, Q.; Zeng, H.; Nisenbaum, E.J.; Liu, L.; Zhao, Y.; et al. Olfactory and gustatory dysfunctions as an early identifier of COVID-19 in adults and children: An international multicenter study. Otolaryngol. Head Neck Surg. 2020, 163, 714–721. [Google Scholar] [CrossRef]
- Boscolo-Rizzo, P.; Borsetto, D.; Spinato, G.; Fabbris, C.; Menegaldo, A.; Gaudioso, P.; Nicolai, P.; Tirelli, G.; Da Mosto, M.C.; Rigoli, R.; et al. New onset of loss of smell or taste in household contacts of home-isolated SARS-CoV-2-positive subjects. Eur. Arch. Otorhinolaryngol. 2020, 277, 2637–2640. [Google Scholar] [CrossRef]
- Tudrej, B.; Sebo, P.; Lourdaux, J.; Cuzin, C.; Floquet, M.; Haller, D.M.; Maisonneuve, H. Self-reported loss of smell and taste in SARS-CoV-2 patients: Primary care data to guide future early detection strategies. J. Gen. Intern. Med. 2020, 35, 2502–2504. [Google Scholar] [CrossRef]
- Gómez-Iglesias, P.; Porta-Etessam, J.; Montalvo, T.; Valls-Carbó, A.; Gajate, V.; Matías-Guiu, J.A.; Parejo-Carbonell, B.; González-García, N.; Ezpeleta, D.; Láinez, J.M.; et al. An online observational study of patients with olfactory and gustory alterations secondary to SARS-CoV-2 infection. Front. Public Health 2020, 8, 243. [Google Scholar] [CrossRef]
- Parma, V.; Ohla, K.; Veldhuizen, M.G.; Niv, M.Y.; Kelly, C.E.; Bakke, A.J.; Cooper, K.W.; Bouysset, C.; Pirastu, N.; Dibattista, M.; et al. More than smell–COVID-19 is associated with severe impairment of smell, tastes, and chemesthesis. Chem. Senses 2020, 45, 609–622. [Google Scholar] [CrossRef] [PubMed]
- Biadsee, A.; Biadsee, A.; Kassem, F.; Dagan, O.; Masarwa, S.; Ormianer, Z. Olfactory and oral manifestations of COVID-19: Sex-related symptoms—A potential pathway to early diagnosis. Otolaryngol. Head Neck Surg. 2020, 163, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Charani, E.; Ariyanayagam, D.; Abdulaal, A.; Denny, S.J.; Mughal, N.; Moore, L.S.P. New-onset anosmia and ageuisia in adult patients diagnosed with SARS-CoV-2 infection. Clin. Microbiol. Infect. 2020, 26, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Chiesa-Estomba, C.M.; Hans, S.; Barillari, M.R.; Jouffe, L.; Saussez, S. Loss of smell and taste in 2013 European patients with mild to moderate COVID-19. Ann. Intern. Med. 2020, 173, 672–675. [Google Scholar] [CrossRef]
- Carignan, A.; Valiquette, L.; Grenier, C.; Musonera, J.B.; Nkengurutse, D.; Marcil-Héguy, A.; Vettese, K.; Marcoux, D.; Valiquette, C.; Xiong, W.T.; et al. Anosmia and dysgeusia associated with SARS-CoV-2 infection: An age-matched case-control study. CMAJ 2020, 192, E702–E707. [Google Scholar] [CrossRef] [PubMed]
- Abalo-Lojo, J.M.; Pouso-Diz, J.M.; Gonzalez, F. Taste and smell dysfunction in COVID-19 patients. Ann. Otol. Rhinol. Laryngol. 2020, 129, 1041–1042. [Google Scholar] [CrossRef] [PubMed]
- Meini, S.; Suardi, L.R.; Busoni, M.; Roberts, A.T.; Fortini, A. Olfactory and gustatory dysfunctions in 100 patients hospitalized for COVID-19: Sex differences and recovery time in real-life. Eur. Arch. Otorhinolaryngol. 2020, 277, 3519–3523. [Google Scholar] [CrossRef]
- Sierpiński, R.; Pinkas, J.; Jankowski, M.; Zgliczyński, W.S.; Wierzba, W.; Gujski, M.; Szumowski, Ł. Sex differences in the frequency of gastrointestinal symptoms and olfactory or taste disorders in 1942 nonhospitalized patients with coronavirus disease 2019 (COVID-19). Pol. Arch. Intern. Med. 2020, 130, 501–505. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Lechien, J.R.; Portillo-Mazal, P.; Martínez, F.; Cuauro-Sanchez, J.; Calvo-Henriquez, C.; Saussez, S. Olfactory and gustatory dysfunctions in COVID-19. First reports of Latin-American ethnic patients. Am. J. Otolaryngol. 2020, 41, 102605. [Google Scholar] [CrossRef]
- Song, J.; Deng, Y.K.; Wang, H.; Wang, Z.C.; Liao, B.; Ma, J.; He, C.; Pan, L.; Liu, Y.; Alobid, I.; et al. Self-reported taste and smell disorders in patients with COVID-19: Distinct features in China. Curr. Med. Sci. 2021, 41, 14–23. [Google Scholar] [CrossRef]
- Chary, E.; Carsuzaa, F.; Trijolet, J.P.; Capitaine, A.L.; Roncato-Saberan, M.; Fouet, K.; Cazenave-Roblot, F.; Catroux, M.; Allix-Beguec, C.; Dufour, X. Prevalence and recovery from olfactory and gustatory dysfunctions in COVID-19 infection: A prospective multicenter study. Am. J. Rhinol. Allergy 2020, 34, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Fjaeldstad, A.W. Prolonged complaints of chemosensory loss after COVID-19. Dan. Med. J. 2020, 67, A05200340. [Google Scholar] [PubMed]
- Izquierdo-Domínguez, A.; Rojas-Lechuga, M.J.; Chiesa-Estomba, C.; Calvo-Henríquez, C.; Ninchritz-Becerra, E.; Soriano-Reixach, M.; Poletti-Serafini, D.; Villarreal, I.M.; Maza-Solano, J.M.; Moreno-Luna, R.; et al. Smell and taste dysfunction in COVID-19 is associated with younger age in ambulatory settings: A multicenter cross-sectional study. J. Investig. Allergol. Clin. Immunol. 2020, 30, 346–357. [Google Scholar] [CrossRef]
- Sakalli, E.; Temirbekov, D.; Bayri, E.; Alis, E.E.; Erdurak, S.C.; Bayraktaroglu, M. Ear nose throat-related symptoms with a focus on loss of smell and/or taste in COVID-19 patients. Am. J. Otolaryngol. 2020, 41, 102622. [Google Scholar] [CrossRef]
- Mercante, G.; Ferreli, F.; De Virgilio, A.; Gaino, F.; Di Bari, M.; Colombo, G.; Russo, E.; Costantino, A.; Pirola, F.; Cugini, G.; et al. Prevalence of taste and smell dysfunction in coronavirus disease 2019. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Vacchiano, V.; Riguzzi, P.; Volpi, L.; Tappatà, M.; Avoni, P.; Rizzo, G.; Guerra, L.; Zaccaroni, S.; Cortelli, P.; Michelucci, R.; et al. Early neurological manifestations of hospitalized COVID-19 patients. Neurol. Sci. 2020, 41, 2029–2031. [Google Scholar] [CrossRef]
- Rudberg, A.S.; Havervall, S.; Månberg, A.; Falk, A.J.; Aguilera, K.; Ng, H.; Gabrielsson, L.; Salomonsson, A.C.; Hanke, L.; Murrell, B.; et al. SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat. Commun. 2020, 11, 5064. [Google Scholar] [CrossRef]
- Petrocelli, M.; Ruggiero, F.; Baietti, A.M.; Pandolfi, P.; Salzano, G.; Salzano, F.A.; Lechien, J.R.; Saussez, S.; De Riu, G.; Vaira, L.A. Remote psychophysical evaluation of olfactory and gustatory functions in early-stage coronavirus disease 2019 patients: The Bologna experience of 300 cases. J. Laryngol. Otol. 2020, 134, 571–576. [Google Scholar] [CrossRef]
- Poncet-Megemont, L.; Paris, P.; Tronchere, A.; Salazard, J.P.; Pereira, B.; Dallel, R.; Aumeran, C.; Beytout, J.; Jacomet, C.; Laurichesse, H.; et al. High prevalence of headaches during COVID-19 infection: A retrospective cohort study. Headache 2020, 60, 2578–2582. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Lechien, J.R.; Barillari, M.R.; Saussez, S. Patterns of gustatory recovery in patients affected by the COVID-19 outbreak. Virol. Sin. 2020, 35, 833–837. [Google Scholar] [CrossRef]
- Villarreal, I.M.; Morato, M.; Martínez-RuizCoello, M.; Navarro, A.; Garcia-Chillerón, R.; Ruiz, Á.; de Almeida, I.V.; Mazón, L.; Plaza, G. Olfactory and taste disorders in healthcare workers with COVID-19 infection. Eur. Arch. Otorhinolaryngol. 2021, 278, 2123–2127. [Google Scholar] [CrossRef] [PubMed]
- Martin-Sanz, E.; Riestra, J.; Yebra, L.; Larran, A.; Mancino, F.; Yanes-Diaz, J.; Garrote, M.; Colmenero, M.; Montiel, E.; Molina, C.; et al. Prospective study in 355 patients with suspected COVID-19 infection. Value of cough, subjective hyposmia, and hypogeusia. Laryngoscope 2020, 130, 2674–2679. [Google Scholar] [CrossRef] [PubMed]
- Vaira, L.A.; Hopkins, C.; Petrocelli, M.; Lechien, J.R.; Chiesa-Estomba, C.M.; Salzano, G.; Cucurullo, M.; Salzano, F.A.; Saussez, S.; Boscolo-Rizzo, P.; et al. Smell and taste recovery in coronavirus disease 2019 patients: A 60-day objective and prospective study. J. Laryngol. Otol. 2020, 134, 703–709. [Google Scholar] [CrossRef]
- Rojas-Lechuga, M.J.; Izquierdo-Domínguez, A.; Chiesa-Estomba, C.; Calvo-Henríquez, C.; Villarreal, I.M.; Cuesta-Chasco, G.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I. Chemosensory dysfunction in COVID-19 out-patients. Eur. Arch. Otorhinolaryngol. 2021, 278, 695–702. [Google Scholar] [CrossRef]
- Klopfenstein, T.; Zahra, H.; Kadiane-Oussou, N.J.; Lepiller, Q.; Royer, P.Y.; Toko, L.; Gendrin, V.; Zayet, S. New loss of smell and taste: Uncommon symptoms in COVID-19 patients on Nord Franche-Comte cluster, France. Int. J. Infect. Dis. 2020, 100, 117–122. [Google Scholar] [CrossRef]
- Vaira, L.A.; Hopkins, C.; Petrocelli, M.; Lechien, J.R.; Soma, D.; Giovanditto, F.; Rizzo, D.; Salzano, G.; Piombino, P.; Saussez, S.; et al. Do olfactory and gustatory psychophysical scores have prognostic value in COVID-19 patients? A prospective study of 106 patients. J. Otolaryngol. Head Neck Surg. 2020, 49, 56. [Google Scholar] [CrossRef]
- Salepci, E.; Turk, B.; Ozcan, S.N.; Bektas, M.E.; Aybal, A.; Dokmetas, I.; Turgut, S. Symptomatology of COVID-19 from the otorhinolaryngology perspective: A survey of 223 SARS-CoV-2 RNA-positive patients. Eur. Arch. Otorhinolaryngol. 2021, 278, 525–535. [Google Scholar] [CrossRef]
- Brandão Neto, D.; Fornazieri, M.A.; Dib, C.; Di Francesco, R.C.; Doty, R.L.; Voegels, R.L.; Pinna, F.R. Chemosensory dysfunction in COVID-19: Prevalences, recovery rates, and clinical associations on a large Brazilian sample. Otolaryngol. Head Neck Surg. 2021, 164, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Al-Ani, R.M.; Acharya, D. Prevalence of anosmia and ageusia in patients with COVID-19 at a primary health center, Doha, Qatar. Indian J. Otolaryngol. Head Neck Surg. 2020, 1–7. [Google Scholar] [CrossRef]
- Çalıca Utku, A.; Budak, G.; Karabay, O.; Güçlü, E.; Okan, H.D.; Vatan, A. Main symptoms in patients presenting in the COVID-19 period. Scott. Med. J. 2020, 65, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Romero-Sánchez, C.M.; Díaz-Maroto, I.; Fernández-Díaz, E.; Sánchez-Larsen, Á.; Layos-Romero, A.; García-García, J.; González, E.; Redondo-Peñas, I.; Perona-Moratalla, A.B.; Del Valle-Pérez, J.A.; et al. Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology 2020, 95, e1060–e1070. [Google Scholar] [CrossRef] [PubMed]
- Komagamine, J.; Yabuki, T. Initial symptoms of patients with coronavirus disease 2019 in Japan: A descriptive study. J. Gen. Fam. Med. 2020, 22, 61–64. [Google Scholar] [CrossRef]
- Fantozzi, P.J.; Pampena, E.; Di Vanna, D.; Pellegrino, E.; Corbi, D.; Mammucari, S.; Alessi, F.; Pampena, R.; Bertazzoni, G.; Minisola, S.; et al. Xerostomia, gustatory and olfactory dysfunctions in patients with COVID-19. Am. J. Otolaryngol. 2020, 41, 102721. [Google Scholar] [CrossRef] [PubMed]
- Klein, H.; Asseo, K.; Karni, N.; Benjamini, Y.; Nir-Paz, R.; Muszkat, M.; Israel, S.; Niv, M.Y. Onset, duration and unresolved symptoms, including smell and taste changes, in mild COVID-19 infection: A cohort study in Israeli patients. Clin. Microbiol. Infect. 2021, 27, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.E.; Wools-Kaloustian, K.; Fadel, W.F.; Duszynski, T.J.; Yiannoutsos, C.; Halverson, P.K.; Menachemi, N. Symptoms and symptom clusters associated with SARS-CoV-2 infection in community-based populations: Results from a statewide epidemiological study. PLoS ONE. 2021, 16, e0241875. [Google Scholar] [CrossRef]
- Boscolo-Rizzo, P.; Borsetto, D.; Fabbris, C.; Spinato, G.; Frezza, D.; Menegaldo, A.; Mularoni, F.; Gaudioso, P.; Cazzador, D.; Marciani, S.; et al. Evolution of altered sense of smell or taste in patients with mildly symptomatic COVID-19. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 729–732. [Google Scholar] [CrossRef] [PubMed]
- Blair, J.E.; Gotimukul, A.; Wang, F.; Mina, S.A.; Bartels, H.C.; Burns, M.W.; Kole, A.E.; Vikram, H.R.; Gea-Banacloche, J.C.; Seville, M.T.; et al. Mild to moderate COVID-19 illness in adult outpatients: Characteristics, symptoms, and outcomes in the first 4 weeks of illness. Medicine 2021, 100, e26371. [Google Scholar] [CrossRef]
- Panda, S.; Mohamed, A.; Sikka, K.; Kanodia, A.; Sakthivel, P.; Thakar, A.; Bhatnagar, S.; Mohan, A.; Meena, V.P.; Tiwari, P.; et al. Otolaryngologic manifestation and long-term outcome in mild COVID-19: Experience from a tertiary care centre in India. Indian J. Otolaryngol. Head Neck Surg. 2021, 73, 72–77. [Google Scholar] [CrossRef]
- Pellaud, C.; Grandmaison, G.; Pham Huu Thien, H.P.; Baumberger, M.; Carrel, G.; Ksouri, H.; Erard, V.; Chuard, C.; Hayoz, D.; Sridharan, G. Characteristics, comorbidities, 30-day outcome and in-hospital mortality of patients hospitalised with COVID-19 in a Swiss area–a retrospective cohort study. Swiss Med. Wkly. 2020, 150, w20314. [Google Scholar] [CrossRef]
- O’Keefe, J.B.; Tong, E.J.; O’Keefe, G.D.; Tong, D.C. Description of symptom course in a telemedicine monitoring clinic for acute symptomatic COVID-19: A retrospective cohort study. BMJ Open 2021, 11, e044154. [Google Scholar] [CrossRef]
- Paderno, A.; Mattavelli, D.; Rampinelli, V.; Grammatica, A.; Raffetti, E.; Tomasoni, M.; Gualtieri, T.; Taboni, S.; Zorzi, S.; Del Bon, F.; et al. Olfactory and gustatory outcomes in COVID-19: A prospective evaluation in nonhospitalized subjects. Otolaryngol. Head Neck Surg. 2020, 163, 1144–1149. [Google Scholar] [CrossRef]
- Lovato, A.; Galletti, C.; Galletti, B.; de Filippis, C. Clinical characteristics associated with persistent olfactory and taste alterations in COVID-19: A preliminary report on 121 patients. Am. J. Otolaryngol. 2020, 41, 102548. [Google Scholar] [CrossRef] [PubMed]
- Armange, L.; Bénézit, F.; Picard, L.; Pronier, C.; Guillot, S.; Lentz, P.A.; Carré, F.; Tattevin, P.; Revest, M. Prevalence and characteristics of persistent symptoms after non-severe COVID-19: A prospective cohort study. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 2421–2425. [Google Scholar] [CrossRef] [PubMed]
- Caronna, E.; Ballvé, A.; Llauradó, A.; Gallardo, V.J.; Ariton, D.M.; Lallana, S.; López Maza, S.; Olivé Gadea, M.; Quibus, L.; Restrepo, J.L.; et al. Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia 2020, 40, 1410–1421. [Google Scholar] [CrossRef] [PubMed]
- Boscolo-Rizzo, P.; Polesel, J.; Spinato, G.; Menegaldo, A.; Fabbris, C.; Calvanese, L.; Borsetto, D.; Hopkins, C. Predominance of an altered sense of smell or taste among long-lasting symptoms in patients with mildly symptomatic COVID-19. Rhinology 2020, 58, 524–525. [Google Scholar] [CrossRef]
- Carvalho-Schneider, C.; Laurent, E.; Lemaignen, A.; Beaufils, E.; Bourbao-Tournois, C.; Laribi, S.; Flament, T.; Ferreira-Maldent, N.; Bruyère, F.; Stefic, K.; et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin. Microbiol. Infect. 2021, 27, 258–263. [Google Scholar] [CrossRef]
- Niklassen, A.S.; Draf, J.; Huart, C.; Hintschich, C.; Bocksberger, S.; Trecca, E.M.C.; Klimek, L.; Le Bon, S.D.; Altundag, A.; Hummel, T. COVID-19: Recovery from chemosensory dysfunction. A multicentre study on smell and taste. Laryngoscope 2021, 131, 1095–1100. [Google Scholar] [CrossRef]
- Bell, M.L.; Catalfamo, C.J.; Farland, L.V.; Ernst, K.C.; Jacobs, E.T.; Klimentidis, Y.C.; Jehn, M.; Pogreba-Brown, K. Post-acute sequelae of COVID-19 in a non-hospitalized cohort: Results from the Arizona CoVHORT. PLoS ONE 2021, 16, e0254347. [Google Scholar] [CrossRef]
- Chopra, V.; Flanders, S.A.; O’Malley, M.; Malani, A.N.; Prescott, H.C. Sixty-day outcomes among patients hospitalized with COVID-19. Ann. Intern. Med. 2021, 174, 576–578. [Google Scholar] [CrossRef]
- Goërtz, Y.M.J.; Van Herck, M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.C.; Houben-Wilke, S.; Burtin, C.; Posthuma, R.; Franssen, F.M.E.; et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: The post-COVID-19 syndrome? ERJ Open Res. 2020, 6, 00542–02020. [Google Scholar] [CrossRef]
- Spinicci, M.; Vellere, I.; Graziani, L.; Tilli, M.; Borchi, B.; Mencarini, J.; Campolmi, I.; Gori, L.; Rasero, L.; Fattirolli, F.; et al. Clinical and laboratory follow-up after hospitalization for COVID-19 at an Italian tertiary care center. Open Forum Infect. Dis. 2021, 8, ofab049. [Google Scholar] [CrossRef] [PubMed]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef]
- Gherlone, E.F.; Polizzi, E.; Tetè, G.; De Lorenzo, R.; Magnaghi, C.; Rovere Querini, P.; Ciceri, F. Frequent and persistent salivary gland ectasia and oral disease after COVID-19. J. Dent. Res. 2021, 100, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Miyazato, Y.; Morioka, S.; Tsuzuki, S.; Akashi, M.; Osanai, Y.; Tanaka, K.; Terada, M.; Suzuki, M.; Kutsuna, S.; Saito, S.; et al. Prolonged and late-onset symptoms of coronavirus disease 2019. Open Forum Infect. Dis. 2020, 7, ofaa507. [Google Scholar] [CrossRef] [PubMed]
- Bellan, M.; Soddu, D.; Balbo, P.E.; Baricich, A.; Zeppegno, P.; Avanzi, G.C.; Baldon, G.; Bartolomei, G.; Battaglia, M.; Battistini, S.; et al. Respiratory and psychophysical sequelae among patients with COVID-19 four months after hospital discharge. JAMA Netw. Open 2021, 4, e2036142. [Google Scholar] [CrossRef]
- Logue, J.K.; Franko, N.M.; McCulloch, D.J.; McDonald, D.; Magedson, A.; Wolf, C.R.; Chu, H.Y. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw. Open 2021, 4, e210830. [Google Scholar] [CrossRef]
- Blomberg, B.; Mohn, K.G.; Brokstad, K.A.; Zhou, F.; Linchausen, D.W.; Hansen, B.A.; Lartey, S.; Onyango, T.B.; Kuwelker, K.; Sævik, M.; et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. 2021, 27, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- Boscolo-Rizzo, P.; Menegaldo, A.; Fabbris, C.; Spinato, G.; Borsetto, D.; Vaira, L.A.; Calvanese, L.; Pettorelli, A.; Sonego, M.; Frezza, D.; et al. Six-month psychophysical evaluation of olfactory dysfunction in patients with COVID-19. Chem. Senses 2021, 46, bjab006. [Google Scholar] [CrossRef]
- Ghosn, J.; Piroth, L.; Epaulard, O.; Le Turnier, P.; Mentré, F.; Bachelet, D.; Laouénan, C.; French COVID Cohort Study and Investigators Groups. Persistent COVID-19 symptoms are highly prevalent 6 months after hospitalization: Results from a large prospective cohort. Clin. Microbiol. Infect. 2021, 27, 1041.e1–1041.e4. [Google Scholar] [CrossRef]
- Petrocelli, M.; Cutrupi, S.; Salzano, G.; Maglitto, F.; Salzano, F.A.; Lechien, J.R.; Saussez, S.; Boscolo-Rizzo, P.; De Riu, G.; Vaira, L.A. Six-month smell and taste recovery rates in coronavirus disease 2019 patients: A prospective psychophysical study. J. Laryngol. Otol. 2021, 135, 436–441. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Peghin, M.; Palese, A.; Venturini, M.; De Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Augustin, M.; Schommers, P.; Stecher, M.; Dewald, F.; Gieselmann, L.; Gruell, H.; Horn, C.; Vanshylla, K.; Cristanziano, V.D.; Osebold, L.; et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: A longitudinal prospective cohort study. Lancet Reg. Health-Eur. 2021, 6, 100122. [Google Scholar] [CrossRef]
- Gautam, N.; Madathil, S.; Tahani, N.; Bolton, S.; Parekh, D.; Stockley, J.; Goyal, S.; Qureshi, H.; Yasmin, S.; Cooper, B.G.; et al. Medium-term outcome of severe to critically ill patients with SARS-CoV-2 infection. Clin. Infect. Dis. 2022, 74, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.N.; Hoang, V.T.; Lagier, J.C.; Raoult, D.; Gautret, P. Long-term persistence of olfactory and gustatory disorders in COVID-19 patients. Clin. Microbiol. Infect. 2021, 27, 931–932. [Google Scholar] [CrossRef]
- Biadsee, A.; Dagan, O.; Ormianer, Z.; Kassem, F.; Masarwa, S.; Biadsee, A. Eight-month follow-up of olfactory and gustatory dysfunctions in recovered COVID-19 patients. Am. J. Otolaryngol. 2021, 42, 103065. [Google Scholar] [CrossRef]
- Boscolo-Rizzo, P.; Guida, F.; Polesel, J.; Marcuzzo, A.V.; Antonucci, P.; Capriotti, V.; Sacchet, E.; Cragnolini, F.; D’Alessandro, A.; Zanelli, E.; et al. Self-reported smell and taste recovery in coronavirus disease 2019 patients: A one-year prospective study. Eur. Arch. Otorhinolaryngol. 2022, 279, 515–520. [Google Scholar] [CrossRef]
- Boscolo-Rizzo, P.; Guida, F.; Polesel, J.; Marcuzzo, A.V.; Capriotti, V.; D’Alessandro, A.; Zanelli, E.; Marzolino, R.; Lazzarin, C.; Antonucci, P.; et al. Sequelae in adults at 12 months after mild-to-moderate coronavirus disease 2019 (COVID-19). Int. Forum Allergy Rhinol. 2021, 11, 1685–1688. [Google Scholar] [CrossRef]
- Hajikhani, B.; Calcagno, T.; Nasiri, M.J.; Jamshidi, P.; Dadashi, M.; Goudarzi, M.; Eshraghi, A.A.; Mirsaeidi, M.; FACS. Olfactory and gustatory dysfunction in COVID-19 patients: A meta-analysis study. Physiol. Rep. 2020, 8, e14578. [Google Scholar] [CrossRef]
- Kim, J.W.; Han, S.C.; Jo, H.D.; Cho, S.W.; Kim, J.Y. Regional and chronological variation of chemosensory dysfunction in COVID-19: A meta-analysis. J. Korean Med. Sci. 2021, 36, e40. [Google Scholar] [CrossRef]
- Boscutti, A.; Delvecchio, G.; Pigoni, A.; Cereda, G.; Ciappolino, V.; Bellani, M.; Fusar-Poli, P.; Brambilla, P. Olfactory and gustatory dysfunctions in SARS-CoV-2 infection: A systematic review. Brain Behav. Immun. Health 2021, 15, 100268. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Wang, V.Y.; Chen, Y.H.; Ku, C.H.; Wang, P.C. The prevalence of olfactory and gustatory dysfunction in COVID-19—A systematic review. Auris Nasus Larynx 2021. online ahead of print. [Google Scholar] [CrossRef]
- Cirillo, N.; Bizzoca, M.E.; Lo Muzio, E.; Cazzolla, A.P.; Lo Muzio, L. Gustatory dysfunction in COVID-19 patients: A rapid systematic review on 27,687 cases. Acta Odontol. Scand. 2021, 79, 418–425. [Google Scholar] [CrossRef]
- Kumar, A.A.; Lee, S.; Lock, C.; Keong, N.C. Geographical variations in host predisposition to COVID-19 related anosmia, ageusia, and neurological syndromes. Front. Med. 2021, 8, 661359. [Google Scholar] [CrossRef] [PubMed]
- von Bartheld, C.S.; Hagen, M.M.; Butowt, R. Prevalence of chemosensory dysfunction in COVID-19 patients: A systematic review and meta-analysis reveals significant ethnic differences. ACS Chem. Neurosci. 2020, 11, 2944–2961. [Google Scholar] [CrossRef]
- Giacomelli, A.; Pezzati, L.; Conti, F.; Bernacchia, D.; Siano, M.; Oreni, L.; Rusconi, S.; Gervasoni, C.; Ridolfo, A.L.; Rizzardini, G.; et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: A cross-sectional study. Clin. Infect. Dis. 2020, 71, 889–890. [Google Scholar] [CrossRef]
- Al-Rawi, N.H.; Sammouda, A.R.; AlRahin, E.A.; Ali, F.; Arayedh, G.; Daryanavard, H.A.; Saeed, M.H.; Nuaimi, A. Prevalence of anosmia or ageusia in patients with COVID-19 among United Arab Emirates population. Int. Dent. J. 2021. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mutiawati, E.; Fahriani, M.; Mamada, S.S.; Fajar, J.K.; Frediansyah, A.; Maliga, H.A.; Ilmawan, M.; Emran, T.B.; Ophinni, Y.; Ichsan, I.; et al. Anosmia and dysgeusia in SARS-CoV-2 infection: Incidence and effects on COVID-19 severity and mortality, and the possible pathobiology mechanisms—A systematic review and meta-analysis. F1000Research 2021, 10, 40. [Google Scholar] [CrossRef]
- Moraschini, V.; Reis, D.; Sacco, R.; Calasans-Maia, M.D. Prevalence of anosmia and ageusia symptoms among long-term effects of COVID-19. Oral Dis. online ahead of print. 2021. [Google Scholar] [CrossRef]
- Andrews, P.J.; Pendolino, A.L.; Ottaviano, G.; Scarpa, B.; Grant, J.; Gaudioso, P.; Bordin, A.; Marchese-Ragona, R.; Leoni, D.; Cattelan, A.; et al. Olfactory and taste dysfunction among mild-to-moderate symptomatic COVID-19 positive health care workers: An international survey. Laryngoscope Investig. Otolaryngol. 2020, 5, 1019–1028. [Google Scholar] [CrossRef]
- Freni, F.; Meduri, A.; Gazia, F.; Nicastro, V.; Galletti, C.; Aragona, P.; Galletti, C.; Galletti, B.; Galletti, F. Symptomatology in head and neck district in coronavirus disease (COVID-19): A possible neuroinvasive action of SARS-CoV-2. Am. J. Otolaryngol. 2020, 41, 102612. [Google Scholar] [CrossRef] [PubMed]
- Sinjari, B.; D’Ardes, D.; Santilli, M.; Rexhepi, I.; D’Addazio, G.; Di Carlo, P.; Chiacchiaretta, P.; Caputi, S.; Cipollone, F. SARS-CoV-2 and oral manifestation: An observational, human study. J. Clin. Med. 2020, 9, 3218. [Google Scholar] [CrossRef]
- AbuBakr, N.; Salem, Z.A.; Kamel, A.H.M. Oral manifestations in mild-to-moderate cases of COVID-19 viral infection in the adult population. Dent. Med. Probl. 2021, 58, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Omezli, M.M.; Torul, D.E. Evaluation of the xerostomia, taste and smell impairments after COVID-19. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e568–e575. [Google Scholar] [CrossRef]
- Fathi, Y.; Ghasemzadeh Hoseini, E.; Atoof, F.; Mottaghi, R. Xerostomia (dry mouth) in patients with COVID-19: A case series. Future Virol. 2021, 16, 315–319. [Google Scholar] [CrossRef]
- El Kady, D.M.; Gomaa, E.A.; Abdella, W.S.; Ashraf Hussien, R.; Abd ElAziz, R.H.; Khater, A.G.A. Oral manifestations of COVID-19 patients: An online survey of the Egyptian population. Clin. Exp. Dent. Res. 2021, 7, 852–860. [Google Scholar] [CrossRef]
- Anaya, J.M.; Rojas, M.; Salinas, M.L.; Rodríguez, Y.; Roa, G.; Lozano, M.; Rodríguez-Jiménez, M.; Montoya, N.; Zapata, E.; Post-COVID Study Group; et al. Post-COVID syndrome. A case series and comprehensive review. Autoimmun. Rev. 2021, 20, 102947. [Google Scholar] [CrossRef] [PubMed]
- Skalny, A.V.; Rink, L.; Ajsuvakova, O.P.; Aschner, M.; Gritsenko, V.A.; Alekseenko, S.I.; Svistunov, A.A.; Petrakis, D.; Spandidos, D.A.; Aaseth, J.; et al. Zinc and respiratory tract infections: Perspectives for COVID-19 (Review). Int. J. Mol. Med. 2020, 46, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Law, J.S.; Nelson, N.; Henkin, R.I. Zinc localization in taste bud membrane. Biol. Trace Elem. Res. 1983, 5, 219–224. [Google Scholar] [CrossRef]
- Kambe, T.; Tsuji, T.; Hashimoto, A.; Itsumura, N. The physiological, biochemical, and molecular roles of zinc transporters in zinc homeostasis and metabolism. Physiol. Rev. 2015, 95, 749–784. [Google Scholar] [CrossRef]
- Wessels, I.; Rolles, B.; Rink, L. The potential impact of zinc supplementation on COVID-19 pathogenesis. Front. Immunol. 2020, 11, 1712. [Google Scholar] [CrossRef]
- Bagheri-Hosseinabadi, Z.; Pirsadeghi, A.; Rahnama, A.; Bahrehmand, F.; Abbasifard, M. Is there any relationship between serum zinc levels and angiotensin-converting enzyme 2 gene expression in patients with coronavirus disease 2019? Meta Gene 2022, 31, 100991. [Google Scholar] [CrossRef] [PubMed]
- Hennigar, S.R.; Lieberman, H.R.; Fulgoni, V.L., 3rd; McClung, J.P. Serum zinc concentrations in the US population are related to sex, age, and time of blood draw but not dietary or supplemental zinc. J. Nutr. 2018, 148, 1341–1351. [Google Scholar] [CrossRef] [PubMed]
- Yasui, Y.; Yasui, H.; Suzuki, K.; Saitou, T.; Yamamoto, Y.; Ishizaka, T.; Nishida, K.; Yoshihara, S.; Gohma, I.; Ogawa, Y. Analysis of the predictive factors for a critical illness of COVID-19 during treatment—Relationship between serum zinc level and critical illness of COVID-19. Int. J. Infect. Dis. 2020, 100, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Jothimani, D.; Kailasam, E.; Danielraj, S.; Nallathambi, B.; Ramachandran, H.; Sekar, P.; Manoharan, S.; Ramani, V.; Narasimhan, G.; Kaliamoorthy, I.; et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int. J. Infect. Dis. 2020, 100, 343–349. [Google Scholar] [CrossRef]
- Heller, R.A.; Sun, Q.; Hackler, J.; Seelig, J.; Seibert, L.; Cherkezov, A.; Minich, W.B.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker. Redox Biol. 2021, 38, 101764. [Google Scholar] [CrossRef]
- Anuk, A.T.; Polat, N.; Akdas, S.; Erol, S.A.; Tanacan, A.; Biriken, D.; Keskin, H.L.; Moraloglu Tekin, O.; Yazihan, N.; Sahin, D. The relation between trace element status (zinc, copper, magnesium) and clinical outcomes in COVID-19 infection during pregnancy. Biol. Trace Elem. Res. 2021, 199, 3608–3617. [Google Scholar] [CrossRef]
- Gonçalves, T.J.M.; Gonçalves, S.E.A.B.; Guarnieri, A.; Risegato, R.C.; Guimarães, M.P.; de Freitas, D.C.; Razuk-Filho, A.; Junior, P.B.B.; Parrillo, E.F. Association between low zinc levels and severity of acute respiratory distress syndrome by new coronavirus SARS-CoV-2. Nutr. Clin. Pract. 2021, 36, 186–191. [Google Scholar] [CrossRef]
- Abdelmaksoud, A.A.; Ghweil, A.A.; Hassan, M.H.; Rashad, A.; Khodeary, A.; Aref, Z.F.; Sayed, M.; Elsamman, M.K.; Bazeed, S. Olfactory disturbances as presenting manifestation among Egyptian patients with COVID-19: Possible role of zinc. Biol. Trace Elem. Res. 2021, 199, 4101–4108. [Google Scholar] [CrossRef]
- Vogel-González, M.; Talló-Parra, M.; Herrera-Fernández, V.; Pérez-Vilaró, G.; Chillón, M.; Nogués, X.; Gómez-Zorrilla, S.; López-Montesinos, I.; Arnau-Barrés, I.; Sorli-Redó, M.L.; et al. Low Zinc levels at admission associates with poor clinical outcomes in SARS-CoV-2 infection. Nutrients 2021, 13, 562. [Google Scholar] [CrossRef]
- Elham, A.S.; Azam, K.; Azam, J.; Mostafa, L.; Nasrin, B.; Marzieh, N. Serum vitamin D, calcium, and zinc levels in patients with COVID-19. Clin. Nutr. ESPEN 2021, 43, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Beigmohammadi, M.T.; Bitarafan, S.; Abdollahi, A.; Amoozadeh, L.; Salahshour, F.; Mahmoodi Ali Abadi, M.; Soltani, D.; Motallebnejad, Z.A. The association between serum levels of micronutrients and the severity of disease in patients with COVID-19. Nutrition 2021, 91–92, 111400. [Google Scholar] [CrossRef] [PubMed]
- Shakeri, H.; Azimian, A.; Ghasemzadeh-Moghaddam, H.; Safdari, M.; Haresabadi, M.; Daneshmand, T.; Namdar Ahmadabad, H. Evaluation of the relationship between serum levels of zinc, vitamin B12, vitamin D, and clinical outcomes in patients with COVID-19. J. Med. Virol. 2022, 94, 141–146. [Google Scholar] [CrossRef]
- Tomasa-Irriguible, T.M.; Bielsa-Berrocal, L.; Bordejé-Laguna, L.; Tural-Llàcher, C.; Barallat, J.; Manresa-Domínguez, J.M.; Torán-Monserrat, P. Low levels of few micronutrients may impact COVID-19 disease progression: An observational study on the first wave. Metabolites 2021, 11, 565. [Google Scholar] [CrossRef]
- Bagher Pour, O.; Yahyavi, Y.; Karimi, A.; Khamaneh, A.M.; Milani, M.; Khalili, M.; Sharifi, A. Serum trace elements levels and clinical outcomes among Iranian COVID-19 patients. Int. J. Infect. Dis. 2021, 111, 164–168. [Google Scholar] [CrossRef]
- Verschelden, G.; Noeparast, M.; Noparast, M.; Goossens, M.C.; Lauwers, M.; Cotton, F.; Michel, C.; Goyvaerts, C.; Hites, M. Plasma zinc status and hyperinflammatory syndrome in hospitalized COVID-19 patients: An observational study. Int. Immunopharmacol. 2021, 100, 108163. [Google Scholar] [CrossRef]
- Du Laing, G.; Petrovic, M.; Lachat, C.; De Boevre, M.; Klingenberg, G.J.; Sun, Q.; De Saeger, S.; De Clercq, J.; Ide, L.; Vandekerckhove, L.; et al. Course and survival of COVID-19 patients with comorbidities in relation to the trace element status at hospital admission. Nutrients 2021, 13, 3304. [Google Scholar] [CrossRef] [PubMed]
- Kocak, O.F.; Ozgeris, F.B.; Parlak, E.; Kadıoglu, Y.; Yuce, N.; Yaman, M.E.; Bakan, E. Evaluation of serum trace element levels and biochemical parameters of COVID-19 patients according to disease severity. Biol. Trace Elem. Res. 2021. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.S. Discovery of human zinc deficiency: Its impact on human health and disease. Adv. Nutr. 2013, 4, 176–190. [Google Scholar] [CrossRef]
- Fromonot, J.; Gette, M.; Ben Lassoued, A.; Guéant, J.L.; Guéant-Rodriguez, R.M.; Guieu, R. Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19. Clin. Nutr. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Devaux, C.A.; Rolain, J.M.; Raoult, D. ACE2 receptor polymorphism: Susceptibility to SARS-CoV-2, hypertension, multi-organ failure, and COVID-19 disease outcome. J. Microbiol. Immunol. Infect. 2020, 53, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.H. Effect of infections on plasma zinc concentration and implications for zinc status assessment in low-income countries. Am. J. Clin. Nutr. 1998, 68 (Suppl. S2), 425S–429S. [Google Scholar] [CrossRef] [PubMed]
- Shirahashi, R.; Suda, T.; Tamano, M. Hypozincemia in chronic hepatitis C is improved with viral clearance by direct-acting antiviral agents. Intern. Med. 2021, 60, 675–680. [Google Scholar] [CrossRef]
- Singh, S.; Diwaker, A.; Singh, B.P.; Singh, R.K. Nutritional immunity, zinc sufficiency, and COVID-19 mortality in socially similar European populations. Front. Immunol. 2021, 12, 699389. [Google Scholar] [CrossRef]
- Tanaka, M. Secretory function of the salivary gland in patients with taste disorders or xerostomia: Correlation with zinc deficiency. Acta. Otolaryngol. 2002, 122, 134–141. [Google Scholar] [CrossRef]
- Arnaud, J.; Touvier, M.; Galan, P.; Andriollo-Sanchez, M.; Ruffieux, D.; Roussel, A.M.; Hercberg, S.; Favier, A. Determinants of serum zinc concentrations in a population of French middle-age subjects (SU.VI.MAX cohort). Eur. J. Clin. Nutr. 2010, 64, 1057–1064. [Google Scholar] [CrossRef][Green Version]
- Cediel, G.; Olivares, M.; Brito, A.; Cori, H.; López de Romaña, D. Zinc deficiency in Latin America and the Caribbean. Food Nutr. Bull. 2015, 36 (Suppl. S2), S129–S138. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.R.; Song, E.K.; Moser, D.K.; Lennie, T.A. Racial differences in dietary antioxidant intake and cardiac event-free survival in patients with heart failure. Eur. J. Cardiovasc. Nurs. 2018, 17, 305–313. [Google Scholar] [CrossRef]
- Yokokawa, H.; Fukuda, H.; Saita, M.; Miyagami, T.; Takahashi, Y.; Hisaoka, T.; Naito, T. Serum zinc concentrations and characteristics of zinc deficiency/marginal deficiency among Japanese subjects. J. Gen. Fam. Med. 2020, 21, 248–255. [Google Scholar] [CrossRef]
- Chou, H.C.; Chien, C.L.; Huang, H.L.; Lu, K.S. Effects of zinc deficiency on the vallate papillae and taste buds in rats. J. Formos. Med. Assoc. 2001, 100, 326–335. [Google Scholar]
- Ikeda, A.; Sekine, H.; Takao, K.; Ikeda, M. Expression and localization of taste receptor genes in the vallate papillae of rats: Effect of zinc deficiency. Acta. Otolaryngol. 2013, 133, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Sato, M.; Akita, M.; Tomita, H. Localization of zinc in the rat submandibular gland and the effect of its deficiency on salivary secretion. Ann. Otol. Rhinol. Laryngol. 1999, 108, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Fábián, T.K.; Beck, A.; Fejérdy, P.; Hermann, P.; Fábián, G. Molecular mechanisms of taste recognition: Considerations about the role of saliva. Int. J. Mol. Sci. 2015, 16, 5945–5974. [Google Scholar] [CrossRef] [PubMed]
- Abduljabbar, T.; Alhamdan, R.S.; Al Deeb, M.; AlAali, K.A.; Vohra, F. Association of salivary content alteration and early ageusia symptoms in COVID-19 infections: A systematic review. Eur. J. Dent. 2020, 14, S152–S158. [Google Scholar] [CrossRef]
- Angeli, A.; Kartsev, V.; Petrou, A.; Pinteala, M.; Brovarets, V.; Vydzhak, R.; Panchishin, S.; Geronikaki, A.; Supuran, C.T. Carbonic anhydrase inhibition with sulfonamides incorporating pyrazole- and pyridazinecarboxamide moieties provides examples of isoform-selective inhibitors. Molecules 2021, 26, 7023. [Google Scholar] [CrossRef]
- Yagi, T.; Asakawa, A.; Ueda, H.; Ikeda, S.; Miyawaki, S.; Inui, A. The role of zinc in the treatment of taste disorders. Recent Pat. Food Nutr. Agric. 2013, 5, 44–51. [Google Scholar] [CrossRef]
- Henkin, R.I.; Martin, B.M.; Agarwal, R.P. Decreased parotid saliva gustin/carbonic anhydrase VI secretion: An enzyme disorder manifested by gustatory and olfactory dysfunction. Am. J. Med. Sci. 1999, 318, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Henkin, R.I.; Martin, B.M.; Agarwal, R.P. Efficacy of exogenous oral zinc in treatment of patients with carbonic anhydrase VI deficiency. Am. J. Med. Sci. 1999, 318, 392–405. [Google Scholar] [CrossRef] [PubMed]
- Goto, T.; Komai, M.; Bryant, B.P.; Furukawa, Y. Reduction in carbonic anhydrase activity in the tongue epithelium and submandibular gland in zinc-deficient rats. Int. J. Vitam. Nutr. Res. 2000, 70, 110–118. [Google Scholar] [CrossRef]
- Okayama, T.; Watanabe, H. Association between taste perception, nutrient intake, and mental health in young Japanese women. Nutr. Res. Pract. 2019, 13, 41–46. [Google Scholar] [CrossRef]
- Souffriau, J.; Libert, C. Mechanistic insights into the protective impact of zinc on sepsis. Cytokine Growth Factor Rev. 2018, 39, 92–101. [Google Scholar] [CrossRef]
- Santos, H.O. Therapeutic supplementation with zinc in the management of COVID-19-related diarrhea and ageusia/dysgeusia: Mechanisms and clues for a personalized dosage regimen. Nutr. Rev. 2021. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Li, L.; Feng, Z.; Wan, S.; Huang, P.; Sun, X.; Wen, F.; Huang, X.; Ning, G.; Wang, W. Comparative genetic analysis of the novel coronavirus (2019-nCoV/SARS-CoV-2) receptor ACE2 in different populations. Cell Discov. 2020, 6, 11. [Google Scholar] [CrossRef]
- Li, Z.Q.; Hu, X.P.; Zhou, J.Y.; Xie, X.D.; Zhang, J.M. Genetic polymorphisms in the carbonic anhydrase VI gene and dental caries susceptibility. Genet. Mol. Res. 2015, 14, 5986–5993. [Google Scholar] [CrossRef] [PubMed]
- Piekoszewska-Ziętek, P.; Szymański, K.; Olczak-Kowalczyk, D. Polymorphism in the CAVI gene, salivary properties and dental caries. Acta Odontol. Scand. 2020, 78, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Zolfaghari Emameh, R.; Falak, R.; Bahreini, E. Application of system biology to explore the association of neprilysin, angiotensin-converting enzyme 2 (ACE2), and carbonic anhydrase (CA) in pathogenesis of SARS-CoV-2. Biol. Proced. Online 2020, 22, 11. [Google Scholar] [CrossRef]
- Kimura, T.; Kambe, T. The functions of metallothionein and ZIP and ZnT transporters: An overview and perspective. Int. J. Mol. Sci. 2016, 17, 336. [Google Scholar] [CrossRef] [PubMed]
- Hennigar, S.R.; Kelley, A.M.; McClung, J.P. Metallothionein and zinc transporter expression in circulating human blood cells as biomarkers of zinc status: A systematic review. Adv. Nutr. 2016, 7, 735–746. [Google Scholar] [CrossRef]
- Hozumi, I.; Suzuki, J.S.; Kanazawa, H.; Hara, A.; Saio, M.; Inuzuka, T.; Miyairi, S.; Naganuma, A.; Tohyama, C. Metallothionein-3 is expressed in the brain and various peripheral organs of the rat. Neurosci. Lett. 2008, 438, 54–58. [Google Scholar] [CrossRef]
- Irie, Y.; Mori, F.; Keung, W.M.; Mizushima, Y.; Wakabayashi, K. Expression of neuronal growth inhibitory factor (metallothionein-III) in the salivary gland. Physiol. Res. 2004, 53, 719–723. [Google Scholar]
- Yang, J.; Zhang, Y.; Cui, X.; Yao, W.; Yu, X.; Cen, P.; Hodges, S.E.; Fisher, W.E.; Brunicardi, F.C.; Chen, C.; et al. Gene profile identifies zinc transporters differentially expressed in normal human organs and human pancreatic cancer. Curr. Mol. Med. 2013, 13, 401–409. [Google Scholar] [PubMed]
- Ghoshal, K.; Majumder, S.; Zhu, Q.; Hunzeker, J.; Datta, J.; Shah, M.; Sheridan, J.F.; Jacob, S.T. Influenza virus infection induces metallothionein gene expression in the mouse liver and lung by overlapping but distinct molecular mechanisms. Mol. Cell. Biol. 2001, 21, 8301–8317. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Takano, H.; Shimada, A.; Satoh, M. Metallothionein as an anti-inflammatory mediator. Mediat. Inflamm. 2009, 2009, 101659. [Google Scholar] [CrossRef] [PubMed]
- Livanos, A.E.; Jha, D.; Cossarini, F.; Gonzalez-Reiche, A.S.; Tokuyama, M.; Aydillo, T.; Parigi, T.L.; Ladinsky, M.S.; Ramos, I.; Dunleavy, K.; et al. Intestinal host response to SARS-CoV-2 infection and COVID-19 outcomes in patients with gastrointestinal symptoms. Gastroenterology 2021, 160, 2435–2450.e34. [Google Scholar] [CrossRef] [PubMed]
- Irie, Y.; Keung, W.M. Metallothionein-III antagonizes the neurotoxic and neurotrophic effects of amyloid β peptides. Biochem. Biophys. Res. Commun. 2001, 282, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Koh, J.Y. Roles of zinc and metallothionein-3 in oxidative stress-induced lysosomal dysfunction, cell death, and autophagy in neurons and astrocytes. Mol. Brain 2010, 3, 30. [Google Scholar] [CrossRef]
- Chung, R.S.; Vickers, J.C.; Chuah, M.I.; Eckhardt, B.L.; West, A.K. Metallothionein-III inhibits initial neurite formation in developing neurons as well as postinjury, regenerative neurite sprouting. Exp. Neurol. 2002, 178, 1–12. [Google Scholar] [CrossRef]
- Fan, D.; Chettouh, Z.; Consalez, G.G.; Brunet, J.F. Taste bud formation depends on taste nerves. Elife 2019, 8, e49226. [Google Scholar] [CrossRef]
- Scudiero, R.; Cigliano, L.; Verderame, M. Age-related changes of metallothionein 1/2 and metallothionein 3 expression in rat brain. Comptes Rendus Biol. 2017, 340, 13–17. [Google Scholar] [CrossRef]
- Alves, S.M.; Cardoso, S.V.; de Fátima Bernardes, V.; Machado, V.C.; Mesquita, R.A.; Vieira do Carmo, M.A.; Ferreira Aguiar, M.C. Metallothionein immunostaining in adenoid cystic carcinomas of the salivary glands. Oral Oncol. 2007, 43, 252–256. [Google Scholar] [CrossRef]
- Brazão-Silva, M.T.; Cardoso, S.V.; de Faria, P.R.; Dias, F.L.; Lima, R.A.; Eisenberg, A.L.; Nascimento, M.F.; Loyola, A.M. Adenoid cystic carcinoma of the salivary gland: A clinicopathological study of 49 cases and of metallothionein expression with regard to tumour behaviour. Histopathology 2013, 63, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Cherian, M.G.; Jayasurya, A.; Bay, B.H. Metallothioneins in human tumors and potential roles in carcinogenesis. Mutat. Res. 2003, 533, 201–209. [Google Scholar] [CrossRef]
- Penkowa, M.; Hidalgo, J. IL-6 deficiency leads to reduced metallothionein-I+II expression and increased oxidative stress in the brain stem after 6-aminonicotinamide treatment. Exp. Neurol. 2000, 163, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Cohn, Z.J.; Kim, A.; Huang, L.; Brand, J.; Wang, H. Lipopolysaccharide-induced inflammation attenuates taste progenitor cell proliferation and shortens the life span of taste bud cells. BMC Neurosci. 2010, 11, 72. [Google Scholar] [CrossRef] [PubMed]
- Liuzzi, J.P.; Lichten, L.A.; Rivera, S.; Blanchard, R.K.; Aydemir, T.B.; Knutson, M.D.; Ganz, T.; Cousins, R.J. Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response. Proc. Natl. Acad. Sci. USA 2005, 102, 6843–6848. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Woo, W.; Wu, B.; Kummer, A.; Duminy, H.; Xu, Z. Zinc accumulation in N-methyl-N-nitrosourea-induced rat mammary tumors is accompanied by an altered expression of ZnT-1 and metallothionein. Exp. Biol. Med. 2003, 228, 689–696. [Google Scholar]
- Li, M.; Zhang, Y.; Bharadwaj, U.; Zhai, Q.J.; Ahern, C.H.; Fisher, W.E.; Brunicardi, F.C.; Logsdon, C.D.; Chen, C.; Yao, Q. Down-regulation of ZIP4 by RNA interference inhibits pancreatic cancer growth and increases the survival of nude mice with pancreatic cancer xenografts. Clin. Cancer Res. 2009, 15, 5993–6001. [Google Scholar] [CrossRef]
- Aydemir, T.B.; Blanchard, R.K.; Cousins, R.J. Zinc supplementation of young men alters metallothionein, zinc transporter, and cytokine gene expression in leukocyte populations. Proc. Natl. Acad. Sci. USA 2006, 103, 1699–1704. [Google Scholar] [CrossRef]
- Carlucci, P.M.; Ahuja, T.; Petrilli, C.; Rajagopalan, H.; Jones, S.; Rahimian, J. Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients. J. Med. Microbiol. 2020, 69, 1228–1234. [Google Scholar] [CrossRef]
- Heckmann, S.M.; Hujoel, P.; Habiger, S.; Friess, W.; Wichmann, M.; Heckmann, J.G.; Hummel, T. Zinc gluconate in the treatment of dysgeusia—A randomized clinical trial. J. Dent. Res. 2005, 84, 35–38. [Google Scholar] [CrossRef]
- Sakagami, M.; Ikeda, M.; Tomita, H.; Ikui, A.; Aiba, T.; Takeda, N.; Inokuchi, A.; Kurono, Y.; Nakashima, M.; Shibasaki, Y.; et al. A zinc-containing compound, Polaprezinc, is effective for patients with taste disorders: Randomized, double-blind, placebo-controlled, multi-center study. Acta Otolaryngol. 2009, 129, 1115–1120. [Google Scholar] [CrossRef] [PubMed]
- Lane, H.W.; Warren, D.C.; Squyres, N.S.; Cotham, A.C. Zinc concentrations in hair, plasma, and saliva and changes in taste acuity of adults supplemented with zinc. Biol. Trace Elem. Res. 1982, 4, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Joachimiak, M.P. Zinc against COVID-19? Symptom surveillance and deficiency risk groups. PLoS Negl. Trop. Dis. 2021, 15, e0008895. [Google Scholar] [CrossRef]
- Rahman, M.T.; Idid, S.Z. Can Zn Be a Critical Element in COVID-19 Treatment? Biol. Trace Elem. Res. 2021, 199, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Chinni, V.; El-Khoury, J.; Perera, M.; Bellomo, R.; Jones, D.; Bolton, D.; Ischia, J.; Patel, O. Zinc supplementation as an adjunct therapy for COVID-19: Challenges and opportunities. Br. J. Clin. Pharmacol. 2021, 87, 3737–3746. [Google Scholar] [CrossRef] [PubMed]

| Subjects | Disease Severity | Country of Subjects | Number of Subjects | Mean or Median Age (Year, Range) | Female (%) | Test Samples | Mean or Median Concentration (μg/dL, ± SD or Range) | Deficiency Ratio (%) Deficiency Defined at | Comorbidities | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| Hospitalized patients | Severe: 24.1% Mild and moderate: 75.9% | Japan | 29 | ≥65 years Severe: 57.1% Mild and moderate: 31.8% | Severe: 42.9 Mild and moderate: 45.5 | Collected the first day of hospitalization and 2–3 days later | Severe: 62.4 ± 19.2 Mild and moderate: 87.7 ± 19.1 | Severe: 85.7 Mild and moderate: 13.6 <70 μg/dL | Total HT (41.4%) DM (20.7%) KD (10.3%) RD (6.9%) CD (6.9%) | Yasui et al. [134] |
| Hospitalized patients diagnosed by RT-PCR test | Mild: 83.0% Moderate: 6.4% Severe: 10.6% | India | Patients: 47 Control: 45 | 34 (18–77) 32 (18–60) | 38.5 Control: 32.3 | Collected 6 h after hospital admission | Patients: 74.5 (53.4–94.6) Control: 105.8 (95.7–120.9) | 57.4 <80 μg/dL | DM (14.8%) HT (14.8%) CD (3.7%) TD (3.7%) | Jothimani et al. [135] |
| Hospitalized patients diagnosed by RT-PCR test | Survivors: 82.9% Non-survivors: 17.1% | Germany | 35 | Total: 77 (38–94) Survivors: 70 (38–91) Non-survivors: 89 (81–94) | 54.3 51.7 66.7 | Collected consecutively | Patients: 71.7 ± 24.6 Healthy subjects: 97.6 ± 29.4 | Survivors: 40.9 Non-survivors: 73.5 <63.87 μg/dL | NR | Heller et al. [136] |
| Hospitalized pregnant women diagnosed by RT-PCR test | NR (in the first, second, and third trimesters of pregnancy) | Turkey | Patients: 100 Control: 100 | Patients in the first trimester: 28 (17–38) Patients in the second trimester: 29 (18–41) Patients in the third trimester: 30 (22–41) | 100 | Measured on admission to hospital | In the first trimester Patients: 56.0 ± 16.6 Control: 67.2 ± 13.9 In the second trimester Patients: 46.4 ± 12.7 Control: 52.8 ± 12.6 In the third trimester Patients: 46.8 ± 12.5 Control: 54.4 ± 13.6 | NR | NR | Anuk et al. [137] |
| Hospitalized patients diagnosed by RT-PCR test | Admitted to ICU | Brazil | 269 | 74 (66–81) | 48.7 | Measured at admission to ICU | Patients: 59.8 (49.7–67.7) | 79.6 <70 μg/dL | HT (74.0%) DM (42.4%) PD (27.9%) CD (27.5%) KD (13.0%) | Gonçalves et al. [138] |
| Patients diagnosed by RT-PCR test | Mild: 33.6% Moderate: 42.5% Severe: 15.7% Critical 8.2% | Egypt | Total: 134 Mild: 45 Moderate: 57 Severe: 21 Critical: 11 | Mild: 31.8 Moderate: 47.8 Severe: 59.1 Critical: 69.5 | Mild: 46.7 Moderate: 42.1 Severe: 28.6 Critical: 45.5 | Collected prior to zinc therapy | Mild: 67 ± 18 Moderate: 62 ± 14 Severe: 73 ± 18 Critical: 72 ± 22 | NR | Total: DM (~27.3%) HT (~23.8%) CD (~9.1%) | Abdelmaksoud et al. [139] |
| Hospitalized patients diagnosed by RT-PCR test | NR | Spain | 249 | 65 (54–75) | 49.0 | Measured at hospital admission | Patients: 61 | 23.3 <50 μg/dL | HT (56.6%) KD (28.1%) DM (21.3%) CD (14.9%) PD (8.8%) | Vogel-González et al. [140] |
| Hospitalized patients diagnosed by RT-PCR test | Severe: 39.8% | Iran | Patients: 93 Control: 186 | 51 (40–61) | 55.9 | NR | Total patients: 67.6 ± 15.1 Female patients: 68.4 ± 14.3 Male patients: 66.7 ± 16.2 Total control: 86.7 ± 11.8 Female control: 79.4 ± 10.9 Male control: 86.6 ± 14.0 | 52.7 NR | CD (21.5%) DM (16.1%) HT (10.8%) PD (8.6%) | Elham et al. [141] |
| Patients diagnosed by RT-PCR test and admitted to ICU | Minimal: 15.0% Mild: 28.3% Moderate: 45.0% Severe: 11.7% | Iran | Total: 60 APACHE score < 25: 40 APACHE score ≥ 25: 20 | Total: 53.5 APACHE score < 25: 50.0 APACHE score ≥ 25: 56.0 | Total: 35.0 APACHE score < 25: 40.0 APACHE score ≥ 25: 25.0 | NR | Total patients: 70.0 ± 44.5 APACHE score < 25: 80.0 ± 32.8 APACHE score ≥ 25: 50.5 ± 18.0 | NR | APACHE score < 25: DM and HT (27.5%) DM (12.5%) TD (15.0%) | Beigmohammadi et al. [142] |
| Hospitalized patients diagnosed by RT-PCR test | Admitted to non-ICU and survived Admitted to ICU Died | Iran | Total: 293 | 53 (38–65) | 50.2 | Measured within 3 days of admission | Admitted to non-ICU and survived: 118.8 ± 34.4 Admitted to ICU: 98.8 ± 30.5 Died: 94.2 ± 26.0 | NR | CD (27.6%) DM (16.0%) HT (6.1%) KD (6.1%) | Shakeri et al. [143] |
| Hospitalized patients diagnosed by RT-PCR test | Moderate: 32.5% Severe: 67.5% | Spain | 120 | 58.7 | 35.8 | Assessed within the first 24 h of hospital admission | 63.5 ± 13.5 | 74.2 <84 μg/dL | HT (32.5%) DM (16.7%) PD (5.0%) | Tomasa-Irriguible et al. [144] |
| Hospitalized patients diagnosed by RT-PCR test | Severe (admitted to ICU): 49.6% Non-severe (non-ICU ward): 50.6% | Iran | Total: 226 ICU: 112 Non-ICU: 114 | Total: 56.426 ICU: 56 Non-ICU: 56.7 | Total: 49.6 ICU: 50.0 Non-ICU: 49.2 | NR | Normal females: 77.0–114 Normal males: 72.6–127 Total patients: 67.9 ± 1.1 Severe: 67.3 ± 1.8 Non-severe: 68.4 ± 1.4 | NR | Total: KD (24.3%) DM (21.2%) CD (20.4%) PD (7.5%) | Bagher Pour et al. [145] |
| Hospitalized patients diagnosed by RT-PCR test | NR | Belgium | 139 | 65 (54–77) | 34.5 | Assessed within the first 72 h of hospital admission | Plasma zinc concentration Patients: 57 (45–67) Control: 74 (80–120) | 95.7 <80 μg/dL | HT (64.7%) DM (36.0%) KD (22.3%) PD (18.0%) CD (16.5%) | Verschelden et al. [146] |
| Hospitalized patients diagnosed by RT-PCR test | Mild, Moderate, Severe, Critical, Died | Belgium | 79 | (18–100) | 30.4 | Analyzed at hospital admission | Total patients: 73.5 ± 16.6 Female patients: 74.8 ± 17.3 Male patients: 72.9 ± 16.4 with DM: 76.7 ± 17.1 with CD: 73.7 ± 12.7 | 70.6 <66 μg/dL | DM (30.4%) CD (27.8%) | Du Laing et al. [147] |
Hospitalized patients diagnosed by RT-PCR test | Asymptomatic: 6.7% Mild: 25.0% Moderate: 46.7% Severe: 21.7% | Turkey | Patients: 60 Control: 32 | Total patients: 45.5 Asymptomatic: 41.3 Mild: 31.9 Moderate: 54.1 Severe: 58 Control: 48.8 | Total patients: 46.7 Asymptomatic: 50.0 Mild: 13.3 Moderate: 53.6 Severe: 69.2 Control: 46.7 | Collected at hospital admission | Total patients: 58.8 ± 19.5 Asymptomatic: 64.9 ± 12.4 Mild: 60.1 ± 18.1 Moderate: 56.9 ± 22.1 Severe: 56.5 ± 18.1 Control: 87.3 ± 33.5 | NR | NR | Kocak et al. [148] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsuchiya, H. Gustatory and Saliva Secretory Dysfunctions in COVID-19 Patients with Zinc Deficiency. Life 2022, 12, 353. https://doi.org/10.3390/life12030353
Tsuchiya H. Gustatory and Saliva Secretory Dysfunctions in COVID-19 Patients with Zinc Deficiency. Life. 2022; 12(3):353. https://doi.org/10.3390/life12030353
Chicago/Turabian StyleTsuchiya, Hironori. 2022. "Gustatory and Saliva Secretory Dysfunctions in COVID-19 Patients with Zinc Deficiency" Life 12, no. 3: 353. https://doi.org/10.3390/life12030353
APA StyleTsuchiya, H. (2022). Gustatory and Saliva Secretory Dysfunctions in COVID-19 Patients with Zinc Deficiency. Life, 12(3), 353. https://doi.org/10.3390/life12030353





