Abstract
The pentose phosphate pathway (PPP) is a branch from glycolysis that begins from glucose-6-phosphate (G6P) and ends up with fructose-6-phosphate (F6P) and glyceraldehyde-3-phosphate (GADP). Its primary physiological significance is to provide nicotinamide adenine dinucleotide phosphate (NADPH) and nucleotides for vital activities such as reactive oxygen species (ROS) defense and DNA synthesis. Glucose-6-phosphate dehydrogenase (G6PD) is a housekeeping protein with 514 amino acids that is also the rate-limiting enzyme of PPP, catalyzing G6P into 6-phosphogluconolactone (6PGL) and producing the first NADPH of this pathway. Increasing evidence indicates that G6PD is upregulated in diverse cancers, and this dysfunction influences DNA synthesis, DNA repair, cell cycle regulation and redox homeostasis, which provides advantageous conditions for cancer cell growth, epithelial-mesenchymal transition (EMT), invasion, metastasis and chemoresistance. Thus, targeting G6PD by inhibitors has been shown as a promising strategy in treating cancer and reversing chemotherapeutic resistance. In this review, we will summarize the existing knowledge concerning G6PD and discuss its role, regulation and inhibitors in cancer development and chemotherapy resistance.
1. Introduction
Basic metabolism, including lipid metabolism, glucose metabolism, protein metabolism and so on, is a basic characteristic of life activity that is essential in achieving material interchange, self-renewal and homeostasis maintenance. Glucose metabolism is one of the major energy sources whose complete oxidation, including glycolysis and the tricarboxylic acid cycle (TCA cycle), can release 2840 kJ of energy. Glucose absorbed extracellularly or transformed from other macromolecules is one of the primary carbon sources, and its catabolism mainly includes glycolysis, the TCA cycle and the pentose phosphate pathway (PPP). The catabolism of glucose not only provides nicotinamide adenine dinucleotide phosphate (NADPH), nucleotides and ATP but also supports lipid and amino acids synthesis for a variety of biological activities. PPP, also known as pentose phosphate shunt, is unlike glycolysis and the TCA cycle, because ATP is not produced in this pathway. Instead, it is the main source of NADPH, which is the primary reducing equivalent source for reactive oxygen species (ROS) defense and DNA synthesis. Glucose-6-phosphate dehydrogenase (G6PD) is the first and the rate-limiting enzyme of PPP, which has many essential biochemical functions. G6PD catalyzes glucose-6-phosphate (G6P) into 6-phosphogluconolactone (6PGL) with NADPH production. The dysfunction of G6PD is involved in many diseases, among which cancer is the most common ones. In this review, we will discuss the characteristics of G6PD, roles of G6PD in the development of cancer, inhibitors of G6PD and the mechanisms behind chemotherapy resistance caused by G6PD.
2. Historical Perspective of G6PD
Differential glucose metabolism between normal and tumor cells was observed by Otto Warburg in the early 19th century, which uncovered the research on cancer metabolism [1] In the 1930s, Warburg noticed that, in addition to the glycolytic cascade, G6P could also be metabolized by another oxidative pathway in which NADP+ was used for the oxidation of G6P. It was not until the 1950s, however, that the entire PPP was elucidated by Frank Dickens, Bernard Horecker, Fritz Lipmann and Efraim Racker, in which G6PD was demonstrated as the first enzyme of this pathway [2]. In 1956, human G6PD was first discovered by Carson et al., and its function was to produce NADPH for reduction [3]. In the same year, a G6PD deficiency was discovered in hemolytic anemia erythrocytes because of its low activity [4]. Further, a cloning study demonstrated that mutations existed on G6PD. The research on G6PD deficiency and its role in cancer began in 1965 when Beaconsfield was studying the relationship between areas and G6PD deficiency and G6PD-related cancer [5]. The cDNA of human G6PD was first cloned by Persico et al. in 1986, and the entire amino acid sequence was also uncovered, making the first step for the structural analysis of G6PD variants and beginning to know the enzyme features [6]. The structure of the G6PD protein was first observed in 1994, showing that this protein is a dimer [7], and there was no coenzyme binding sites except for catalytic sites. However, this protein was separated from Leuconostoc mesenteroides, whose glycolysis pathway was not complete [8,9]. G6PD separated from Leuconostoc mesenteroides can use both NAD+ and NADP+ [10,11] as coenzyme, which is different from advanced living organisms [12,13]. It took a long time and much effort to obtain the human G6PD tetramer due to its microheterogeneity. Margaret J. Adams and her colleagues obtained the crystallization [14], and in the following year, the human G6PD tetramer was revealed from a recombinant protein of the Canton variant [14]. This discovery solved the important question of whether the second NADP+ existed.
3. Characteristics of G6PD
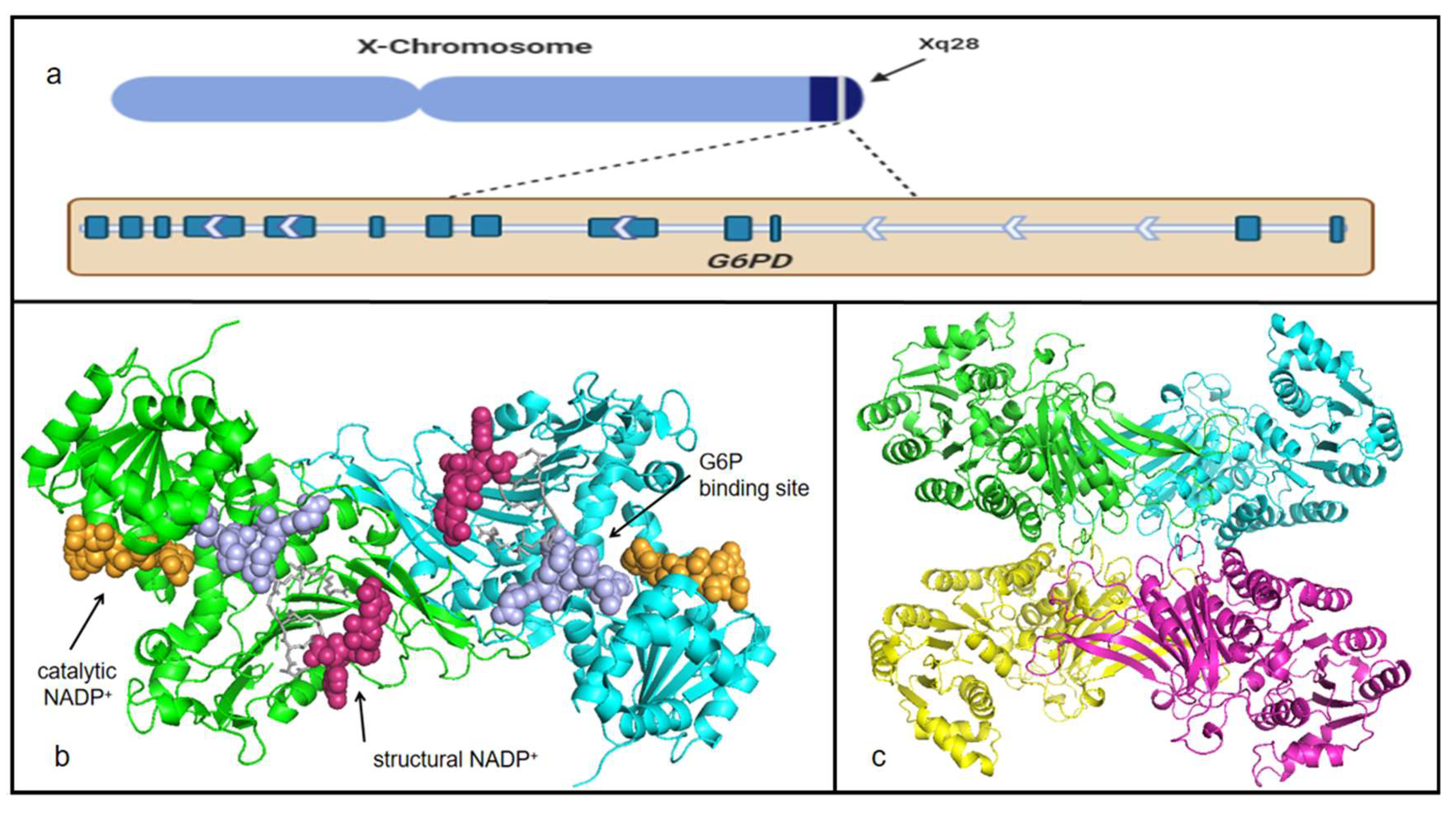
Given the fact that G6PD a typical housekeeping protein, it is expressed in all kinds of tissues and cells [15]. The gene encoding G6PD belongs to the X chromosome, and the location is near the telomeric region of the distal arm [16] (Figure 1a). The functions and structure of G6PD have been confirmed. The total length of this gene is about 18.5 kb, which includes 13 exons and 12 introns, and the last exon contains a terminator [16] (Figure 1a). The promoter of G6PD has been confirmed to be located at CpG land, and it has a sequence of TTAAAT, as well as a great number of stimulatory protein 1 (Sp1) elements, which is especially important for the activity of the promoter [16]. Exon and intron numbers and the exon sizes and sequences are conserved in higher eukaryotes [16]. The 5′-UTR of G6PD includes ATG codons that are out of the translation frame; additionally, the first ATG triplet upstream to a long open reading frame was judged to be the translation initiation site, and it was assigned position No. 1 [6]. mRNA produced by G6PD is 1545 bp [6]. The G6PD gene product is a 59-KD protein with 514 amino acids [6].
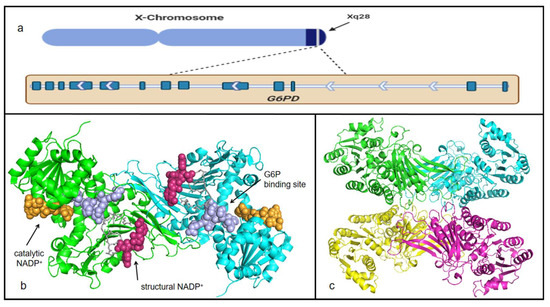
Figure 1.
G6PD location on the chromosome and G6PD protein structure. (a) G6PD location is near the telomeric region of the distal arm. The wide, deep blue represents exons, and the arrows means the order of exons and introns. The first exon and intron are located on the right. For the protein structure, different colors present different peptides. Tertiary structures are downloaded from the website SWISS-MODEL and presented in the software PyMOL. (b) Dimer (a PDB:2bh9.1) of G6PD. Orange dots construct catalytic NADP+—binding sites; purple dots construct G6P-binding sites; pink dots construct structural NADP+—binding sites; gray sticks present sites Asn 363-Lys 366 and Arg 393-Gln 395. (c) Tetramer (b PDB:2bhl.1) of G6PD.
Human G6PD is a kind of NADP+-dependent catalytic enzyme. Secondary and tertiary structures have been revealed in the past few decades. Persico et al. determined the primary structure of G6PD for the first time using the sequence of full-length cDNA clones [6]. Ten years later, the structure and crystal of the mutant ΔG6PD enzyme, which has similar kinetic properties to those of the wild-type enzyme but is more thermostable, was demonstrated by Au et al. [14] The general tertiary structure of G6PD is a tetramer complex, which is constructed predominantly by a hydrophilic dimer–dimer complex [17] (Figure 1c). Each dimer contains two substrate sites and four NADP+—binding sites, two of which act as structural NADP+—binding sites, and the others act as catalytic NADP+—binding sites [6] (Figure 1b). According to the statistics provided by Wang et al., structural NADP+ tightly bound to the corresponding sites, not being removed by the usual dialysis and chromatographic procedures, and the true role of this NADP+ is believed to maintain long-term stability [18]. Catalytic NADP+—binding sites are those that loosely bound NADP+ or NADPH and were easily removed by dialysis [19]. Though tightly bound exists, structural NADP+ still can be removed in the form of NADPH when G6P binds to the substrate site. Once NADPH formed, it is easy to drop out of the structural NADP+—binding sites. Mechanistically, the presence of G6P will change the location of one or two amino acid residues (Asn 363-Lys 366 and Arg 393-Gln 395), each of which spans from the substrate site to the structural NADP+—binding site to the other [17,18,20]. Numerous diseases caused by a deficiency of G6PD affect people worldwide, and a high proportion of the clinical mutations are related to this structural NADP+ site [18,21,22,23]. Monomer is inactive form; however, dimer and tetramer are catalytically functional forms of G6PD [14]. The human enzyme is in a dimer↔tetramer equilibrium, and its stability is dependent on the NADP+ concentration [14]. Conversion towards the dimer happens under high pH conditions [24]. In addition, EDTA, NADPH and G6P favor disruption of the dimer, whereas NADP+ or certain metal ions favor the tetramer [14]. Additionally, the substrate-binding site and the dinucleotide-binding fingerprint are conserved in human G6PD with the sequences RIDHYLGKE (residues 198–206) and GxxGGDLA (residues 38–44), respectively [17].
4. G6PD and Cancer
Cancer is one of the most common diseases in the world, and it remains a leading cause of death worldwide every year. The causes of cancer are complicated, but common features still exist between different kinds of cancer. One of the hallmarks of cancer is reprogrammed energy metabolism [25], and decades ago, Warburg noticed that cancer cells were prone to metabolizing glucose through glycolysis with increased lactate production rather than the oxidative phosphorylation pathway, even in the presence of oxygen, known as the Warburg effect [26]. PPP flux is a main metabolic pathway of glucose, and the dysregulation of proteins in this pathway may be involved in the development of cancer. G6PD as the first and rate-limiting enzyme of PPP also plays an important role in the development of cancer. Indeed, G6PD is upregulated in many cancers. Besides, G6PD overexpression is associated with the degree and stage of cancer, including the size of the tumor, depth of invasion, lymph node metastasis, distant metastasis, TNM stage, and survival rate [27]. Rapid growth and proliferation demand massive biosynthesis and protection from the severe environment. Cancer cells hijack the intracellular metabolic pathway to maintain rapid replication and promote the synthesis of enormous essential cellular components. PPP plays a vital role in metabolism, which can provide both R-5-P for the synthesis nucleotide and NADPH for the redox equilibrium. The overexpression of G6PD influences DNA synthesis, DNA repair, cell cycle regulation, redox equilibrium, proliferation, EMT, invasion and metastasis to provide an advantageous condition for cancer cells [28,29,30,31,32]. What is more, G6PD also acts as a biomarker in diverse cancer in reflecting the clinical prognosis and chemoresistance.
5. The Regulation of G6PD in Cancer
The expression and activity of G6PD are tightly regulated, through transcription, post-transcription, translation, post-translation modification and interactions with other proteins [33] (Table 1).

Table 1.
G6PD expression in different cancers and their effects on cancer.
5.1. Impacts on Cancer at Transcriptional Level
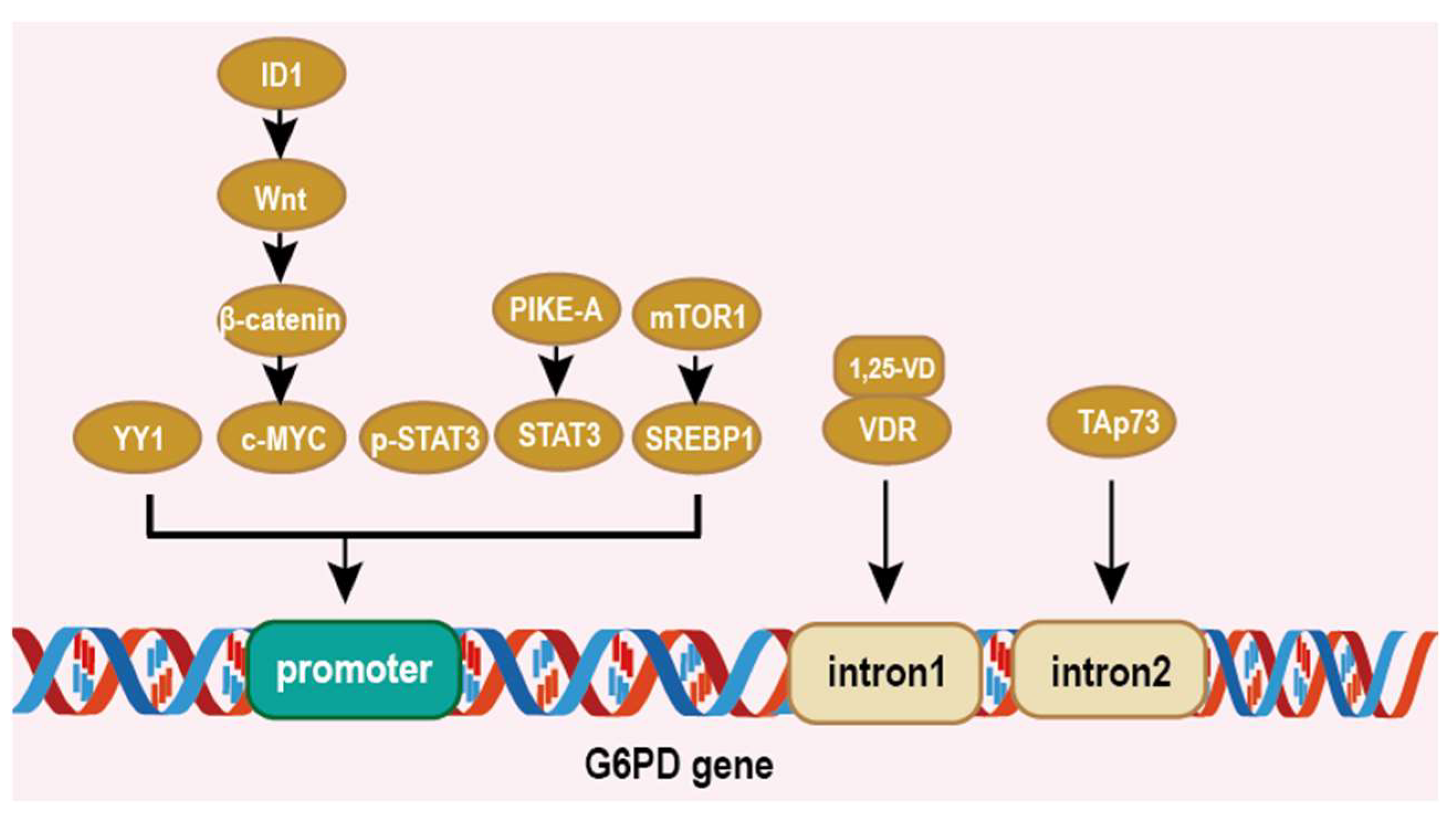
Networks regulating G6PD are complicated in cancer cells and there are multiple cis/trans-regulatory elements controlling G6PD expression [43,44,45]. Simmons et al. reported that the 1, 25-VD/vitamin D receptor (VDR) binds to the vitamin D response elements (VDREs) located at the first intron of the G6PD genome to enhance the G6PD mRNA level [43]. Wu et al. suggested that the transcription factor yin yang 1 (YY1) also positively regulates G6PD at the transcriptional level by directly binding to the G6PD promoter, thus activating PPP and causing metabolic reprogramming [44]. Yin et al. found that c-MYC regulated by the ID1/Wnt/β-catenin axis binds to the promoter of G6PD and promotes G6PD transcription and encourages tumor proliferation and oxaliplatin chemoresistance in hepatocellular carcinoma (HCC) [45]. The Signal Transducer and Activator of Transcription 3 (STAT3) is a transcription factor that is upregulated in many cancers. Zhang et al. found that p-STAT3 activated G6PD gene expression via binding to the G6PD promoter [46]. What is more, Sun et al.’s study showed that PIKE-A induces the expression of G6PD through the binding of STAT3 at the G6PD promoter, thereby promoted glioblastoma cell growth [47]. There have been studies that revealed that the SREBP1 element exists on the G6PD promoter and increases its expression, which is regulated by mTOR1 [48,49]. TAp73, a structural homolog of the tumor suppressor p53, is frequently upregulated in human tumors [31,50]. TAp73 enhances the expression of G6PD by directly binding to the p53 family protein response element (RE) on the second intron of G6PD [31] (Figure 2). These studies indicate that a regulation expression of G6PD at the transcription level and targeting transcription factors maybe a promising therapeutic method.
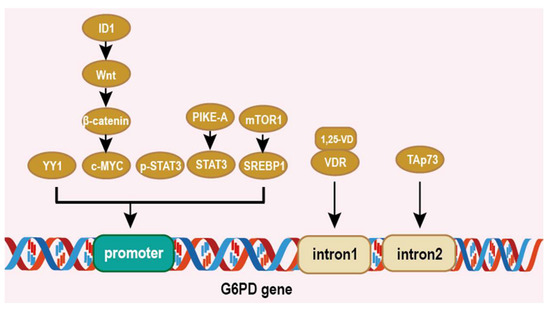
Figure 2.
Regulation of G6PD at the transcriptional level. Elliptical shape represents the protein. Square shape represents the gene elements on G6PD. YY1, c-MYC, p-STAT3, STAT3, SREBP, 1,25VD/VDR and TAp73 bind to different parts of the G6PD gene to regulate G6PD expression.
5.2. Impacts on Cancer at Post-Transcriptional and Translational Level
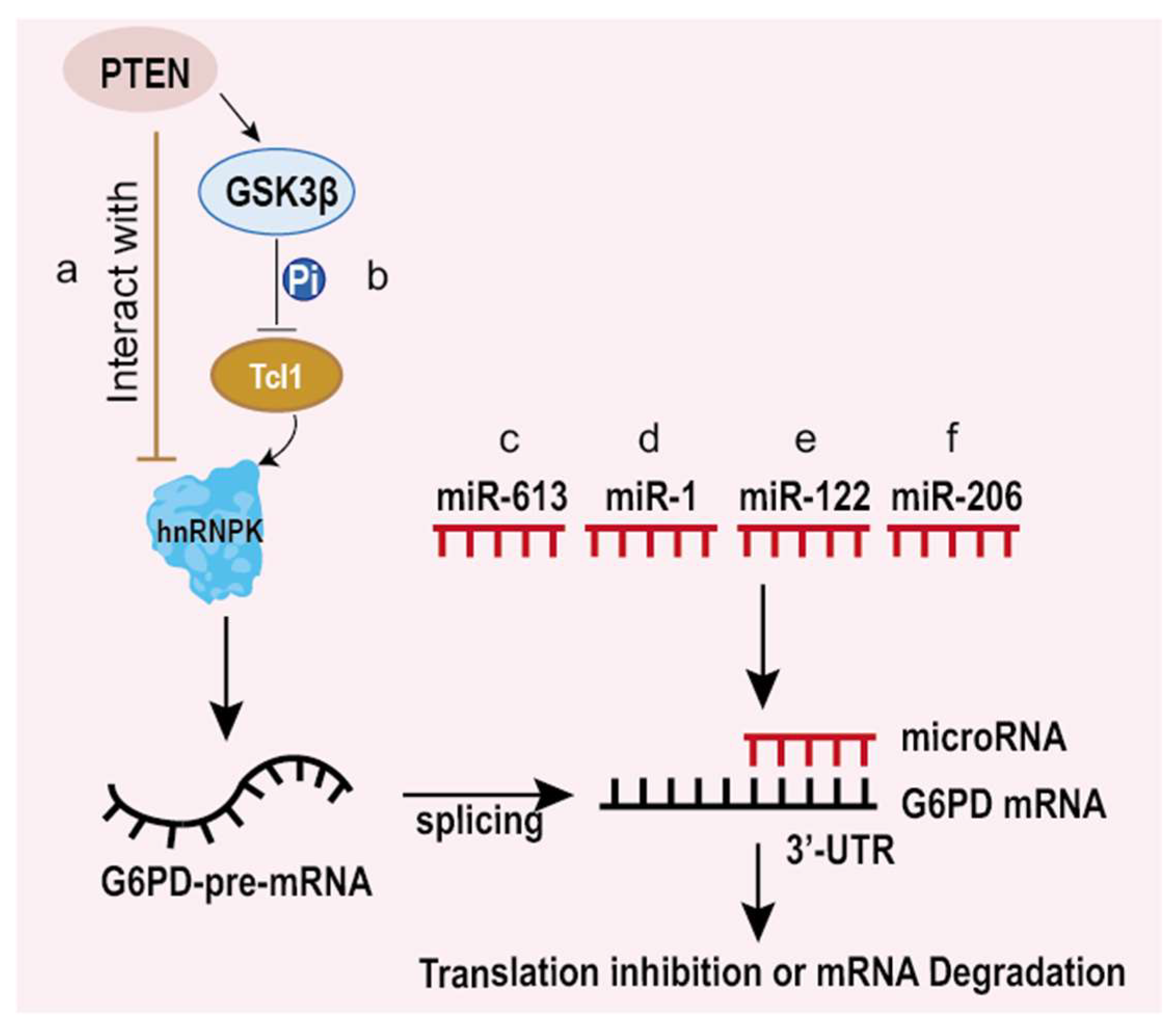
Generally, eukaryotic genes are split genes containing introns and exons. Therefore, mRNA from the DNA template usually needs specific splicing for functional protein translation [51]. According to the work of Hong et al., T-cell leukemia 1 (Tcl1) can promote G6PD pre-mRNA splicing and protein expression by interacting with heterogeneous nuclear ribonucleoprotein (hnRNPK), finally leading to the development of liver cancer (Figure 3a). In addition, the phosphatase and tensin homolog (PTEN) decreased G6PD expression by inhibiting its pre-mRNA splicing through not only interacting with hnRNPK but inactivating Tcl1 through glycogen synthase kinase-3β (GSK3β)-mediated phosphorylation [52] (Figure 3b). This illustrates that PTEN controls G6PD expression through two steps by inhibiting G6PD pre-mRNA splicing, which suggests that G6PD is a key regulatory factor of PTEN in controlling tumor progression and implies that G6PD is a valuable target for anticancer treatments.
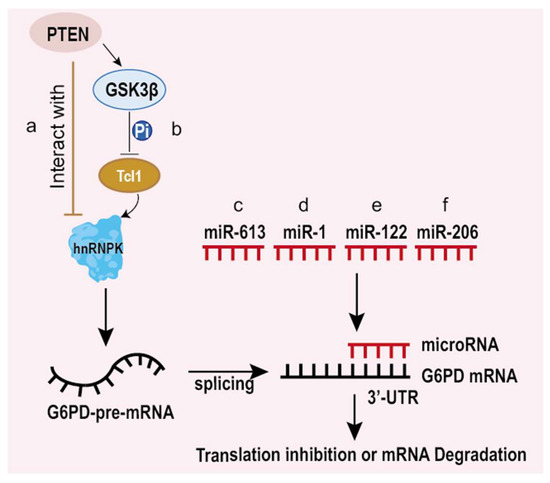
Figure 3.
Regulation of G6PD at the post-transcriptional and translational levels. PTEN decreased G6PD expression by inhibiting its pre-mRNA splicing through not only interacting with hnRNPK (a)but inactivating Tcl1 through glycogen synthase kinase-3β (GSK3β)-mediated phosphorylation (b). MicroRNAs binds to G6PD mRNA to inhibit its translation or degradation. (c) miR-613 binds to the 3′-UTR of G6PD mRNA and promotes the degradation of G6PD mRNA. (d) miR-1 binds to the 3′-UTR of G6PD mRNA and promotes the degradation of G6PD mRNA or inhibition of G6PD translation. (e) miR-122 binds to the 3′-UTR of G6PD mRNA and promotes the degradation of G6PD mRNA. (f) miR-206 binds to the 3′-UTR of G6PD mRNA and promotes the degradation of G6PD mRNA.
MicroRNAs (miRNAs) are small endogenous non-coding RNAs that regulate gene expressions by directly binding to mRNA to suppress the translation or degrade mRNA. Recently, there has been a growing body of evidence revealing that micro RNAs change metabolism, especially aerobic glycolysis to regulate tumorigenesis. A few microRNAs can bind to mRNA of G6PD to degrade G6PD mRNA, influencing the proliferation, migration and invasion of cancer cells. Some kinds of microRNAs play a vital role in regulating the translation of G6PD [28,42,53,54,55,56], which is also involved in controlling cancer progression.
In esophageal squamous cell carcinoma (ESCC), Su et al. found that miR-613 suppresses migration and invasion by decreasing the G6PD expression. Furthermore, they revealed that miR-613 directly binds to the 3′-UTR region of G6PD mRNA, leading to decreased G6PD mRNA [28] (Figure 3c). Hu et al. [53] and He et al. [42] found that miR-1 downregulates endogenous G6PD by directly binding to the 3′-UTR region and inhibiting proliferation and promoting apoptosis in high-risk papillomavirus-associated human cervical cancer and pituitary tumor cells (Figure 3d). Statistics from Barajas et al. [54] displayed for the first time that there are two conservative binding sites for combinations with miR-122 on the 3′-UTR region of G6PD mRNA in liver cancer cells, and interactions between miR-122 and G6PD mRNA reduce the G6PD mRNA and protein levels (Figure 3e). In HR-HPV-positive cervical cancer cells, miR-206 targets the 3′-UTR of G6PD mRNA and blocks its expression as well [55]. Besides, miR-206 is directly responsible for downregulating G6PD, which influences the growth of rhabdomyosarcoma cells [56] (Figure 3f). Thus, these results indicate that G6PD may serve as a therapeutic target for cancer treatment. In addition, micro RNAs not only downregulate G6PD expression individually but can also show a synergistic effect on inhibiting G6PD [54].
5.3. Impacts on Cancer at Post-Translational Modification Level
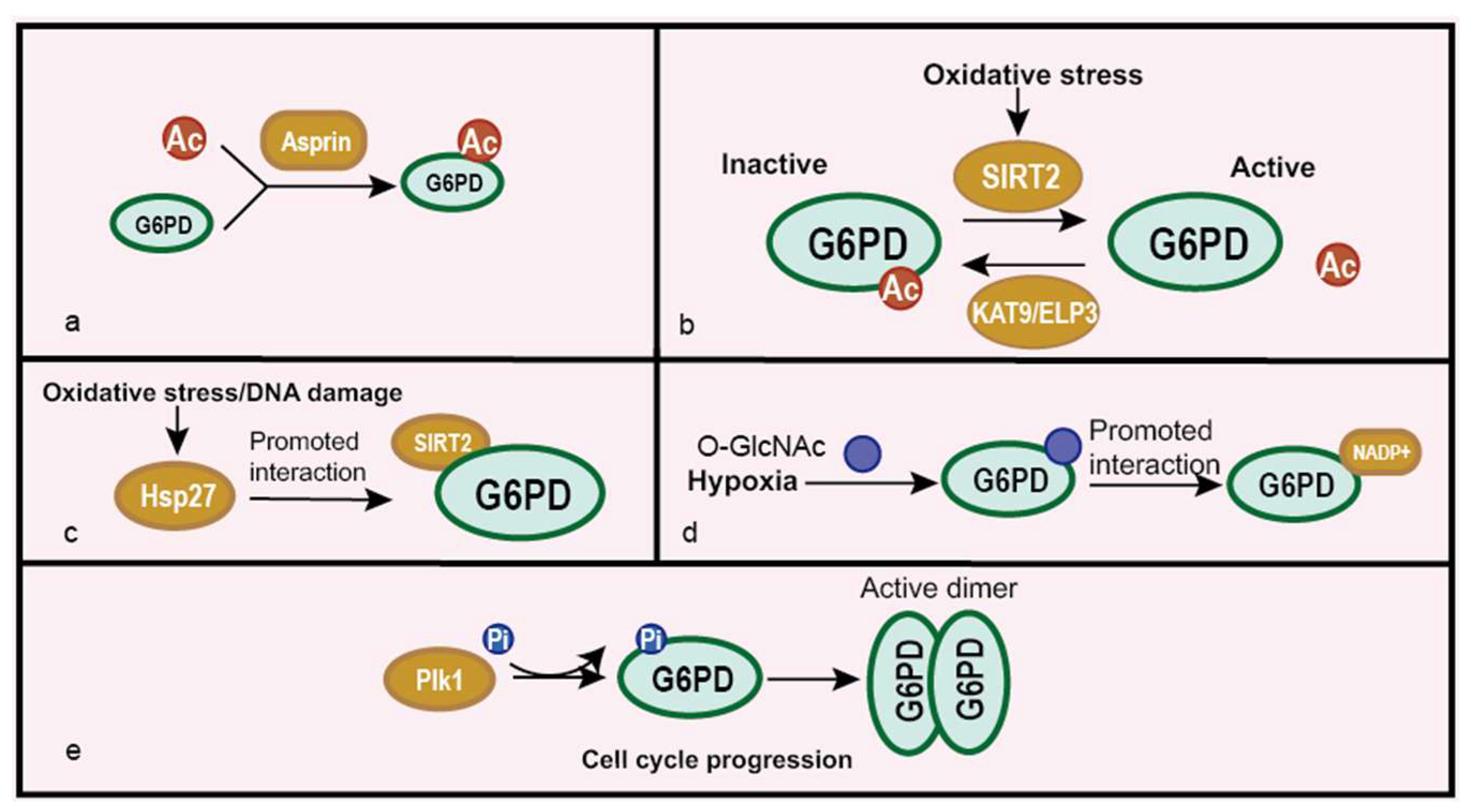
In eukaryotes, post-translational modifications decide the activities and functions of proteins, which also exist in G6PD [57,58,59,60,61]. G6PD acetylation inhibits its function, while deacetylation reverses it [32,57,58,59]. Aspirin can acetylate G6PD at many functional sites and inactivates G6PD in HCT116 cells. The mass spectrometry analysis revealed that 14 lysine residues were acetylated which include essential catalysis sites K235 (in isoform a) and K205 (in isoform b). Acetylation of these two pivotal sites prevents the combination between G6PD and its substrate G-6-P, and acetylation at other lysine residues may decrease the activity of G6PD, leading to the decreased synthesis of ribose sugars and NADPH [57] (Figure 4a). According to the work of Xu et al., silent information regulator 2 (SIRT2) deacetylates G6PD at lysine 403 (K403) and consequently activates it to support the proliferation and clonogenic activity of leukemia cells. Chemical inhibitors against SIRT2 suppress G6PD activity, leading to the reduced cell proliferation of leukemia cells [58]. Elongator acetyltransferase complex subunit 3 (KAT9/ELP3) is identified as a potential acetyltransferase of G6PD, which participates in G6PD K403 acetylation [59] (Figure 4b). Besides, the work of Ye et al. suggests that the binding between G6PD and SIRT2 is enhanced by heat shock protein 27 (Hsp27), leading to the deacetylation and activation of G6PD [32] (Figure 4c). These studies indicate that the acetylation state of G6PD is important in metabolic reprogramming and tumor inhibition or proliferation. O-GlcNAcylation modification also actives G6PD, which can enhance the binding affinity of NADP+ to G6PD and form a higher oligomeric state [60] (Figure 4d). The enhanced activity of G6PD supports cell survival under oxidative stress, and this indicates that O-GlcNAcylation is a key metabolic regulator of the glucose flux. The phosphorylation of G6PD also plays a vital role in regulating G6PD activity. Polo-like kinase1 (Plk1) can bind to and phosphorylate G6PD to positively affect the formation of an active dimer promoting cell cycle progression [61] (Figure 4e). Other modification enzymes need to clarify its role on G6PD and their effects in cancer development. What is more, the additional modifications of G6PD and their function warrant further investigation. Whether modification crosstalk exists on G6PD is still an open question.
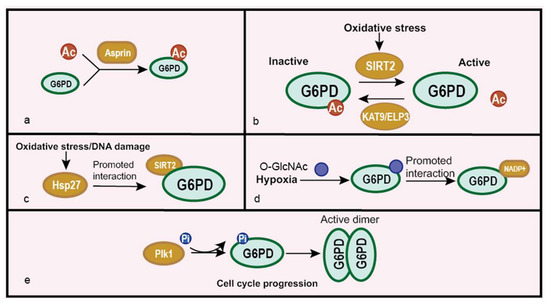
Figure 4.
Regulation of G6PD at the post-translational modification level. (a) Aspirin acetylates G6PD and inhibits its activity. (b) Oxidative stress regulates G6PD acetylation by SIRT2 and KAT9/ELP3. (c) Hsp27 promotes the interaction between SIRT2 and G6PD, enhancing G6PD deacetylation caused by SIRT2 under oxidative stress or the DNA damage condition. (d) O-GlcNAcylation activates G6PD activity by promoting the interaction between G6PD and its co-factor NADPH under hypoxia. (e) Plk1 promotes the phosphorylation of G6PD to stimulate dimer formation during cell cycle progression.
5.4. Impacts on Cancer under Interaction with Other Proteins
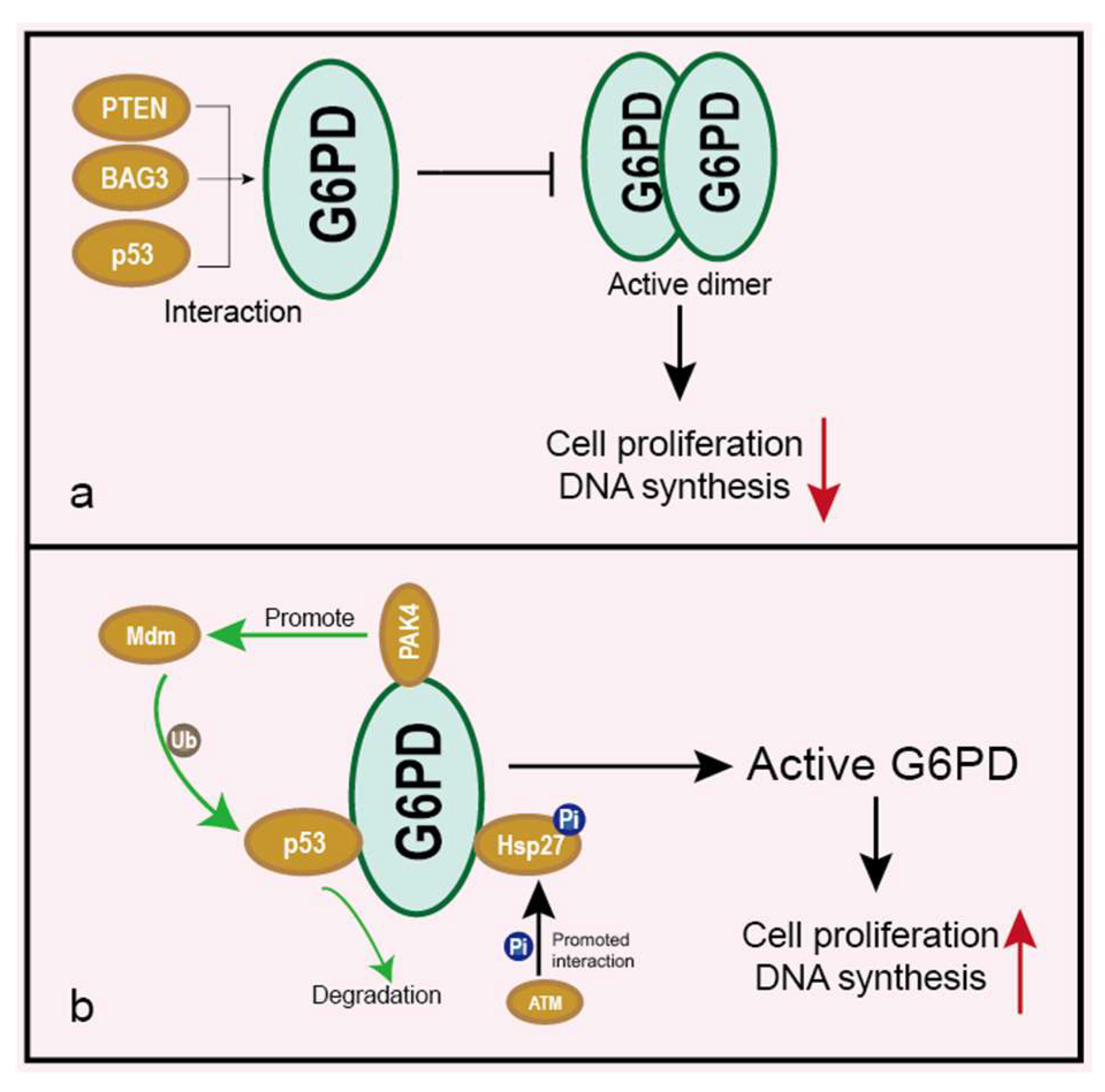
It has been reported that many proteins bind to G6PD, and regulatory interactions with G6PD mainly inhibit the formation of the active oligomeric state [40,62]. Bcl-2 associated athanogene 3 (BAG3) directly interacts with G6PD and consequently inhibits its dimerization and activity, leading to suppression of the PPP flux and the proliferation of hepatocellular carcinomas (HCCs) [40] (Figure 5a). p53 binds to G6PD and prevents the formation of the active dimer, thus inhibiting the PPP flux [62] (Figure 5a). p21-activated kinase 4 (PAK4) can also interact with G6PD and increase G6PD activity via enhancing Mdm2-mediated p53 ubiquitination degradation, resulting in increased colon cancer cell growth [63] (Figure 5b). As mentioned above, PTEN is closely associated with G6PD expression. The authors also discovered that the PTEN protein could directly interact with G6PD and inhibit its activity through preventing the formation of a dimeric G6PD holoenzyme [52] (Figure 5a). ATM phosphorylates Hsp27 and promotes the combination of Hsp27 with G6PD, thus activating G6PD [64] (Figure 5b). These results suggest that interfering interactions between G6PD and other proteins may be an effective therapeutic approach in inhibiting cancer.
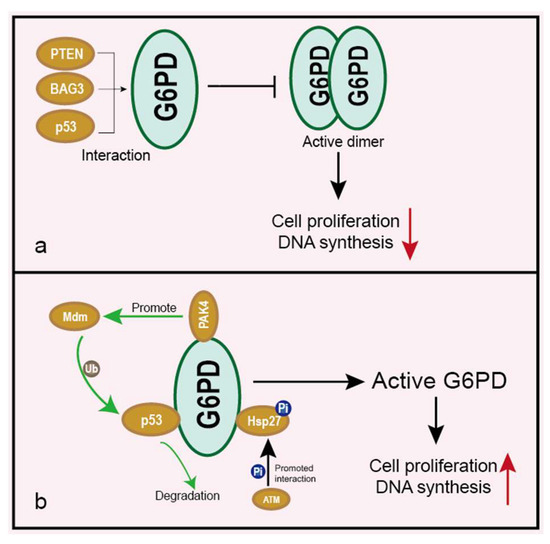
Figure 5.
Interactions between G6PD and other proteins. Elliptical shape represents a protein. Circle shape represents post-translational modification. (a) Proteins such as PTEN, BAG3 or p53 bind to G6PD and inhibit G6PD active dimer formation, leading to the inhibition of cell proliferation and downregulation of DNA synthesis. (b) G6PD is activated through binding with Hsp27 and separating with p53, resulting in an enhanced cell proliferation rate and DNA synthesis. Hsp27 can be phosphorylated by ATM. p53 is ubiquitinated and degraded by the PAK4 pathway.
5.5. Other Pathways Related to G6PD in Cancer
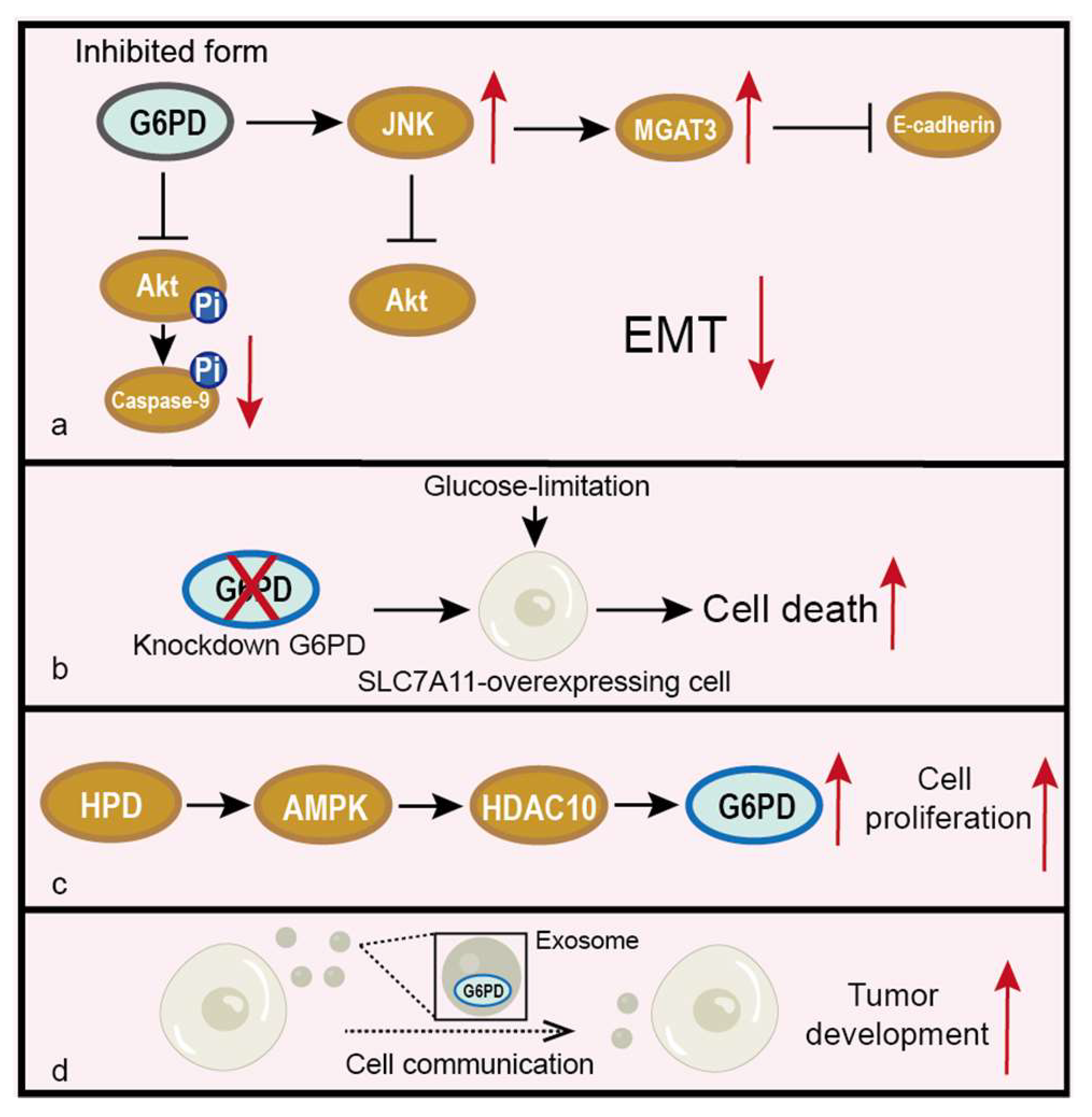
It has been demonstrated that G6PD regulates many signaling pathways [65,66,67]. The study of Wang et al. suggests that the inhibition of G6PD is associated with invasion, metastasis and EMT of oral squamous cell carcinoma (OSCC) through activating JNK, which enhances the E-Cadherin expression level and regulates MGAT3 expression transcriptionally to promote the bisecting GlcNAc-branched N-glycosylation of E-Cadherin [65] (Figure 6a). Chen et al. [66] revealed that the knockdown of G6PD induces intracellular apoptosis through upregulating the cleaved caspase-3, -7 and -9 levels and suppresses the phosphorylated-AKT/AKT pathway, whose activation will phosphorylate Bcl2 and inhibit apoptosis (Figure 6a). Liu et al. demonstrated that the knockdown of G6PD promotes glucose-limitation-induced cell death in solute carrier family 7 member 11 (SLC7A11)-overexpressing cells. What is more, in kidney papillary cell carcinoma (KIRP), high SLC7A11 with high G6PD expression predicted a far worse clinical outcome than either parameter alone [67] (Figure 6b). Therefore, aiming to target G6PD may be a potential way to treat cancer, particularly in cases with high G6PD expression.
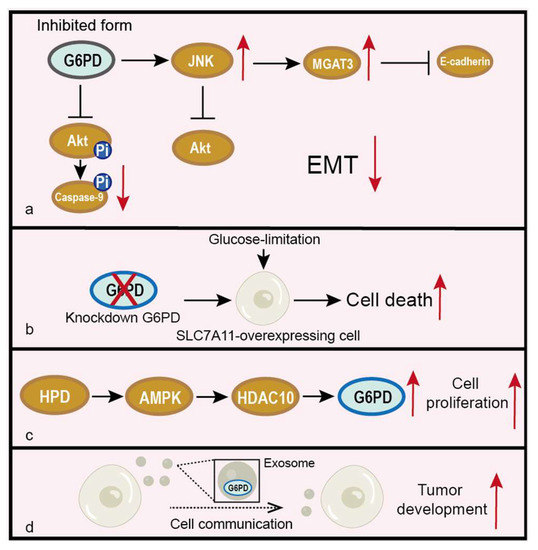
Figure 6.
Regulation of G6PD by other pathways and their effects on tumors. Elliptical shape represents a protein. Circle shape represents post-translational modification. (a) Inactive G6PD will inhibit EMT through regulation of the JNK and Akt pathways. (b) Knockdown of G6PD promotes glucose-limitation-induced cell death in SLC7A11-overexpressing cells. (c) HPD promotes the expression of G6PD through the AMPK/HDAC10 pathway, thus enhancing cell proliferation. (d) G6PD exists in the exosome and mediates tumor development.
G6PD is also regulated by metabolic process, such as the catabolism of amino acids. Shan et al. revealed that 4-hydroxyphenylpyruvate dioxygenase (HPD) promotes a PPP flux through increasing the expression of G6PD mediated by controlling the histone acetylation levels on the G6PD promoter, which were mediated by the HPD-LKB1-AMPK-HDAC10 axis and increasing the acetyl-CoA levels [30] (Figure 6c).
Besides its intracellular function, G6PD may also be involved in cell-cell communications. G6PD is detected in the exosome and mediates metabolic transformation that accounts for tumor development in two late-stage ovarian cell lines, and it could act as a diagnostic, poor prognostic and therapeutic target of late-stage ovarian cancer [68] (Figure 6d).
6. G6PD and Chemotherapy Resistance
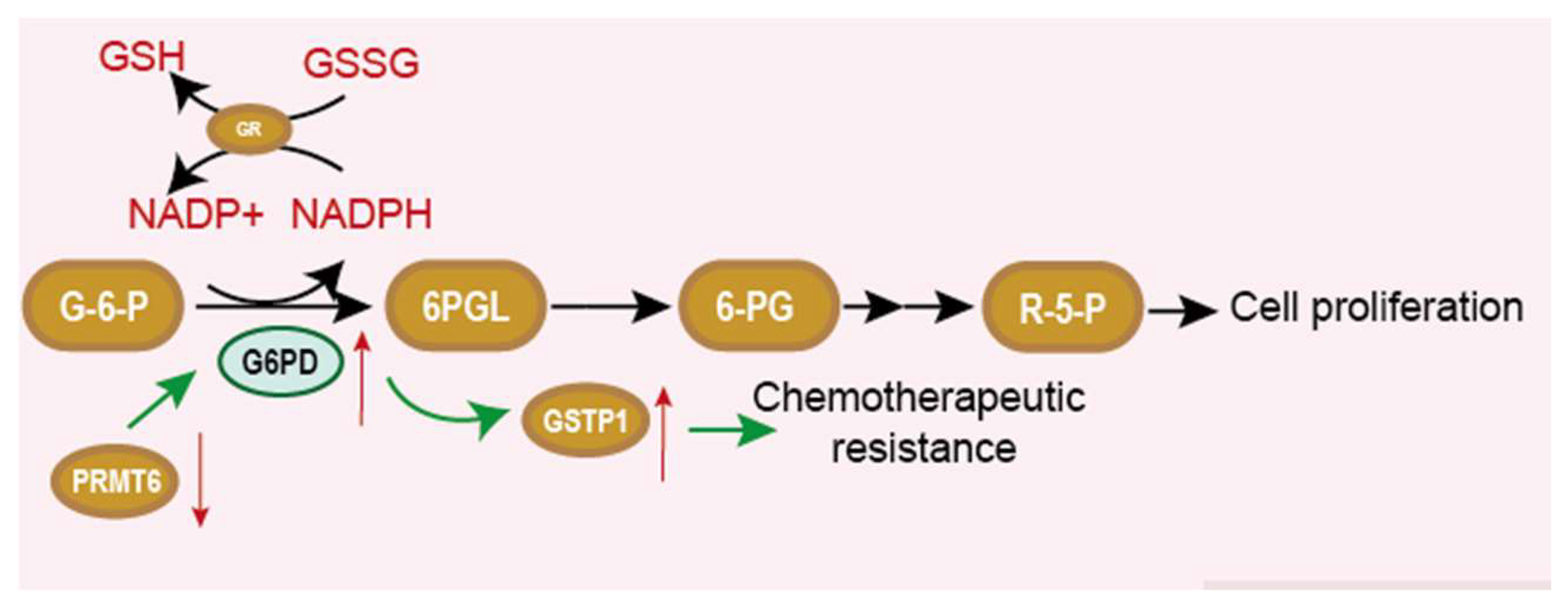
Among clinical treatments of cancer, chemotherapy is the still the standard of care for many types of cancer. At the beginning of a cure, this therapy can inhibit the growth and proliferation of cancer cells. However, the development of chemotherapy resistance frequently leads to therapy failure. Molecular mechanisms contributing to drug resistance are largely unknown, and it is urgently needed to find ways to overcome these obstacles. The inhibition of G6PD is demonstrated to be useful in reversing chemotherapy resistance. Drug resistance is related to the intracellular redox equilibrium. GSH and G6PD producing NADPH play an important role in maintaining this balance. Manuela et al. observed that the G6PD expression level and GSH level were upregulated in doxorubicin-sensitive HT29 cells. Treating cells with G6PD inhibitor dehydroepiandrosterone (DHEA) or 6-aminonicotinamide (6-AN) could decrease G6PD and GSH and reserve a multiple drug resistance [69]. This implicates that active PPP and enhanced G6PD activation are essential for MDR cells to maintain a high GSH level. What is more, another article also improved this perspective [27]. Compared to cisplatin- sensitive cells, more glutamine-derived glutamate can be used for GSH biosynthesis, and G6PD expression and activity are upregulated in cisplatin-resistant cells. Therefore, enhanced G6PD activity maybe induce the resistance of cancer cells to chemotherapeutic drugs [70]. Feng et al. provide perspective on how G6PD links to GSH and contributes to chemotherapy-resistance. Paclitaxel-resistant ovarian cancer cells showed an enhanced PPP flux in which G6PD was overexpressed. The knockdown of G6PD or using G6PD inhibitor 6-AN could improve the therapeutic efficacy of paclitaxel. Further experiments have demonstrated that the downregulation of protein arginine methyltransferase 6 (PRMT6), which methylates H3R2me2a on the promoter of G6PD cause an upregulation of G6PD. Overexpressed G6PD successively enhances the expression of glutathione S-transferase P1 (GSTP1), leading to the conjugation of GSH and paclitaxel (Figure 7). Thus, paclitaxel is exported, and its therapy efficacy is poor. The inhibition of G6PD by shRNA or 6-AN could reverse the resistance to paclitaxel [71].
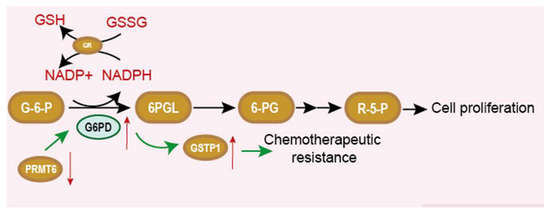
Figure 7.
PPP pathway and the relationship between G6PD, NADPH and GSH. Elliptical shape represents a protein. Square shape represents a chemical. GR is glutathione reductase, which can transform NADPH and GSSG into NADP + and GSH. Downregulation of PRMT6 enhances G6PD expression and promotes drug resistance.
7. Inhibitor of G6PD
There is ample evidence that GP6D is overexpressed and promotes cancer progression in many tumors [66,72]. Thus, the inhibition of G6PD has emerged as a potential therapeutic strategy for treating cancer. The competitive G6PD inhibitor 6-AN and uncompetitive G6PD inhibitor DHEA have been widely used in various cancer studies. In addition, some natural or synthetic compounds can also inhibit G6PD (Table 2 and Figure 8).

Table 2.
G6PD inhibitors in different cancer(cell) types.
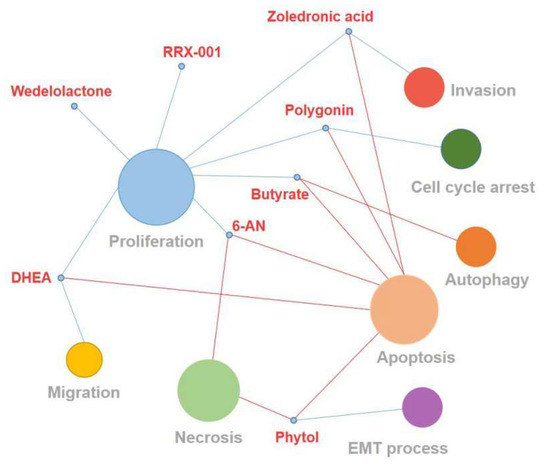
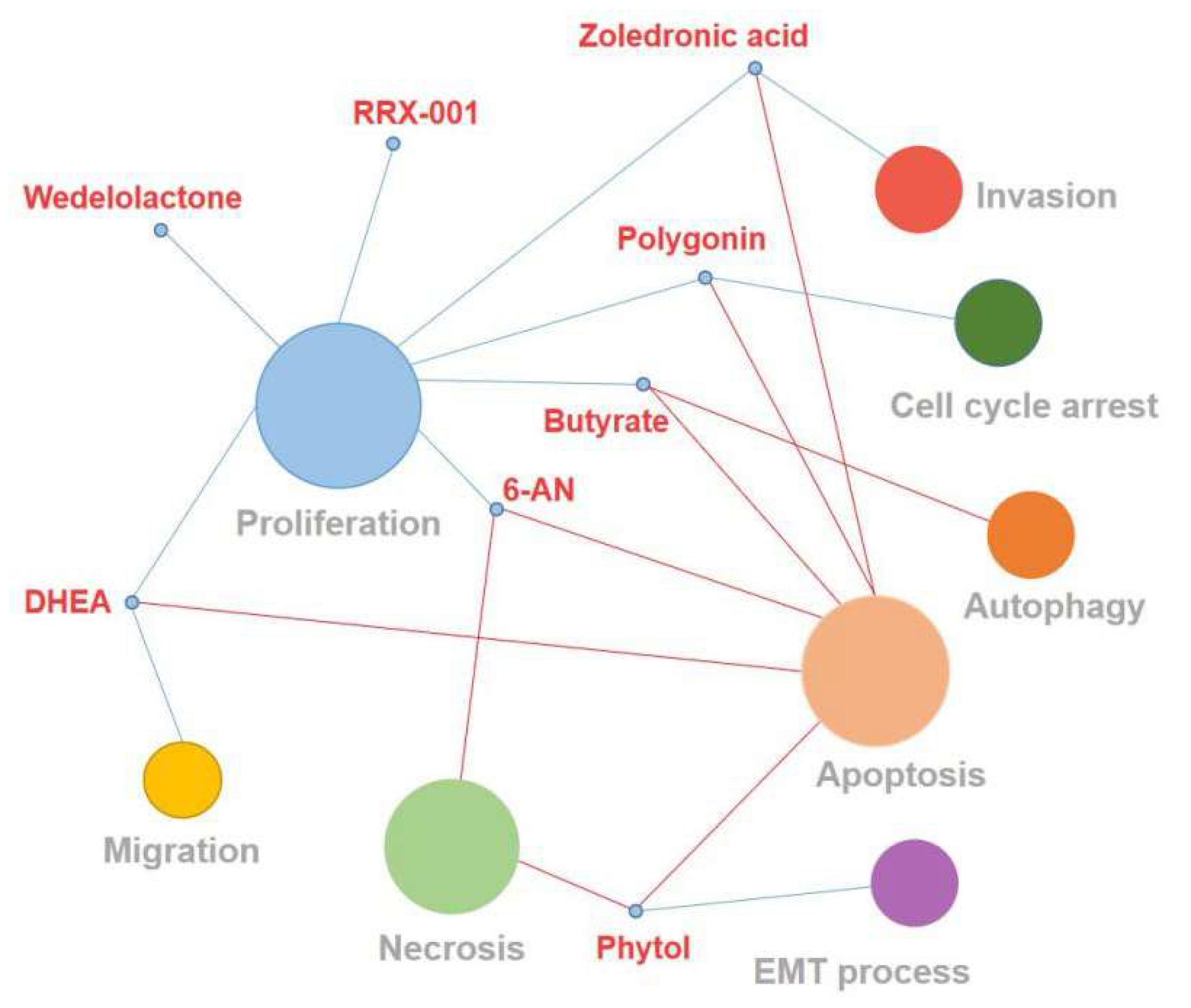
Figure 8.
This figure shows the effect of G6PD inhibitors on cancer cellular function. The blue line represents negative regulation, and the red line represents positive regulation. The size of the circle represents the number of G6PD inhibitors with the same cellular function.
7.1. 6-AN
6-AN, an analog of nicotinamide, competitively inhibits G6PD [73]. Previous studies have demonstrated that the suppression of G6PD by 6-AN can restore the sensitivity of cancer cells to chemotherapy, so it is widely used in the treatment of cancers [72]. For example, G6PD inhibition with 6-AN not only sensitizes leukemic cells to cytarabine treatment by inducing cytotoxicity against acute myeloid leukemia cells but also makes melanoma cells sensitive to metformin treatment through enhancing the cytotoxicity of metformin and resulting in increased apoptosis and necrosis [37,72]. In addition, G6PD inhibitor 6-AN can also significantly reduce the proliferation of bladder cancer cells and exert a synergistic anti-tumor effect with cisplatin [66]. However, some serious side effects such as nerve injury and vitamin B deficiency appear after 6-AN treatment [93].
7.2. DHEA
DHEA is an endogenous steroid produced by the adrenal glands, which acts as a metabolic precursor for the synthesis of androgen and estrogen [76]. As early as 1960, it was reported to have an uncompetitive inhibition of G6PD activity [94]. As an effective inhibitor of the G6PD targeting PPP of cancer cells, DHEA reduces the NADPH levels, NADPH-dependent oxygen-free radical production and nucleic acid synthesis to inhibit tumor development [74,95]. Fang et al. found that DHEA can inhibit the G6PD activity of cervical cancer cells, induce the apoptosis of cancer cells and lead to the decrease of cell migration and proliferation ability [75]. Yang et al. revealed that targeting G6PD by DHEA destroys the redox balance to inhibit growth in breast cancer cells [96]. Although several studies showed that DHEA has anti-cancer, anti-obesity and anti-inflammatory effects on mouse and other rodent models [97,98] DHEA is readily converted into active androgens in vivo, and clinical treatment requires a high oral dose, so its therapeutic effect is limited [94].
7.3. Polydatin
Polydatin (PD) is a resveratrol glycoside extracted from the root or rhizome of polygonum cuspidatum [99]. PD has many biomedical properties, such as antimicrobial, antioxidant and anti-inflammatory [99,100]. In recent years, the antitumor activity of PD has been widely investigated. Previous studies have shown that PD can suppress the growth of various cancer cells by inhibiting cell proliferation, cell cycle arrest, or inducing apoptosis [77,78]. Mele et al. reported that PD can significantly reduce tumor growth and lymph node metastases through directly inhibiting G6PD in orthotopic and metastatic models of oral cancer [94].
7.4. Zoledronic Acid
Zoledronic acid is a kind of bisphosphonate that is commonly used for the treatment of osteoporosis and bone metastasis in solid tumors [79,101]. Zoledronic acid has shown anticancer activity in pancreatic cancer, colon cancer and other cancers by promoting apoptosis and inhibiting cancer cell growth and invasion [79,80]. Zoledronic acid was proven to block Ras signaling and reduce the stability of TAp73, thereby inhibiting the expression of G6PD in bladder cancer cells [81].
7.5. Aspirin
Aspirin is a salicylic acid drug widely used for anti-inflammatory, analgesia and the prevention and treatment of cardiovascular disease [102]. In recent years, mounting studies have revealed that aspirin can inhibit many malignant tumors such as hepatobiliary and colorectal carcinoma [82]. Aspirin can acetylate a variety of proteins in cancer cells, of which G6PD is its acetylation target [36,83]. Ai et al.’s findings suggested that aspirin suppresses G6PD activity in colorectal cancer cells by acetylation, resulting in the decreased synthesis of nucleotide and NADPH [83]. Aspirin may exert anticancer effects via targeting G6PD. However, long-term use of aspirin is associated with significant risks of serious side effects, such as gastrointestinal and cerebral hemorrhage [103,104].
7.6. RRX-001
The dinitroazetidine derivative RRX-001 is a novel chemo-radiotherapy sensitizer in clinical [36,105]. RRX-001 can increase the sensitivity of the tumor to radiation and reverse the drug resistance properties to improve the therapeutic efficiency of chemo-radiotherapy [84]. RRX-001 has a significantly G6PD activity inhibition effect on cancer cell lines, including HepG2, CACO-2 and HT-29 [106]. Cell proliferation is further inhibited by increasing the reactive oxygen/nitrogen species and decreasing ribose 5-phosphate synthesis and glutathione [106,107]. Therefore, RRX-001 as an inhibitor of G6PD for cancer treatment is particularly promising.
7.7. Phytol
A number of compounds have been used to inhibit the G6PD activity in vitro and in vivo. Parth et al. found that phytol has a good binding affinity with G6PD and could also inhibit the activity of G6PD during in silico molecular docking studies [108]. Natural product phytol is an acyclic monounsaturated diterpene alcohol that widely exists in algae, plants and bacteria [85,109]. Previous research has confirmed that phytol represents a wide range of biological activities, such as an antioxidant effect, cytotoxicity and anti-inflammatory and antimicrobial activities. It is worthwhile mentioning that phytol can induce the apoptosis and necrosis of various cancer cells and inhibit the EMT process in HepG2 cells but have little toxicity to normal cells, suggesting that phytol exhibits considerable anticancer potential [85,86]
7.8. Wedelolactone
Wedelolactone, a small molecular compound isolated from Ecliptaalba and Wedelia calendulacea has attracted much attention because of its extensive pharmacological activities, including hepatoprotective, anti-oxidation, anti-inflammatory, immunomodulatory and anti-fibrotic effects, etc. [87,110,111,112] Recent researches has shown that Wedelolactone exhibited a potent anticancer activity against different solid tumors, such as breast, colon and prostate cancers, through inhibiting multiple kinases, the androgen receptor, 5-lipoxygenase and the c-Myc protein [87]. Lately, Luo et al. identified Wedelolactone as a G6PD inhibitor by the high-throughput screening assay. The study demonstrated that it could not only inhibit G6PD significantly in a non-competitive and reversible way but also suppress the proliferation of ovarian cancer cells, which suggests that Wedelolactone affects the proliferation of ovarian cancer cells partly through blocking the enzyme activity of G6PD [88].
7.9. Butyrate
Butyrate is one of the short-chain fatty acids produced by the gut microbiota along with acetic acid and propionic acid. Studies have shown that butyrate exerts several effects in normal colon cells, including supplying energy, maintaining the gut barrier and reducing inflammation [113,114,115], while it exhibits anti-tumorigenic activities through the induction of apoptosis, inhibition of proliferation and promotion of autophagy in various cancer types [89,90,91]. A recent study showed that butyrate can down-regulate the G6PD mRNA and protein levels, reduce the DNA synthesis activity and further enhance the apoptosis efficacy of 5-FU on colon cancer cells. It is reported that butyrate could also inhibit histone deacetylases (HDACs) to depress a number of oncogenic signaling pathways [92]. As a dual inhibitor of G6PD and HDAC, butyrate has great potential to become an anticancer drug in the future.
8. Discussion
Metabolism is necessary for all organisms and cells depend on which provide nutrients, protecting cells from stressed environments and meeting the demands of life. However, increasing evidence has indicated that the metabolic pathways of cancer cells are changed compared to normal cells. These alterations enable cancer cells to acquire more energy, maintain excessive life demands or even transform into malignant cells and improve their ability to translocate and escape from immunological surveillance. Therefore, identifying additional metabolic changes of cancer cells and uncovering efficient methods to modulate these changes may lead to novel cancer treatment. PPP as a glucose metabolism pathway is essential in synthesizing nucleotides and providing NADPH. Targeting the PPP in tumors is an effective approach in treating cancer and improving therapeutic efficacy. Dysfunctions of enzymes in this pathway such as 6PGD contribute to the development of cancer [116,117,118]. Expression changes of G6PD also promote cancer development. The formation of malignant cancer needs many procedures. The beginning of cancer cells stems from uncontrolled growth and continuous replication. Some of cancer cells then evolve the abilities of metastasis and invasion. All of these steps are complicated and involve many pathways. To be noticed, G6PD promotes many of these steps not only as a regulator but also as an actor. In most cancers, G6PD expression is upregulated. The overexpression of G6PD helps cancer cells in their growth, proliferation, EMT, metastasis and invasion. From the normal role of G6PD, we can easily find that the overexpression of G6PD will produce more NADPH and nucleotides. As we all know, NADPH protects cells from life stress, which cancer cells confront a lot. Besides, producing nucleotides can meet the demand of repaid growth and fast proliferation. All of these provide cancer cells with favorable condition to live. Therefore, it is not a surprise that G6PD is involved in the pathways that regulate the cell cycle, expression of cadherin, DNA synthesis and DNA repair. According to several previous studies, the regulations on G6PD depend on multiple aspects from the transcriptional level to the post-translational modification level. Interactions with other proteins could also impact on the functions of G6PD. What is more, the mechanisms regulating G6PD and the pathways regulated by G6PD impact each other and form a circulation. This implied that networks regulating cancer cells are complicated, and G6PD is a promising target. The reverse abnormal expression of G6PD has shown positive effects in inhibiting cancer. However, the roles of G6PD in cancer development mainly depend on its metabolic function in producing NADPH to reduce ROS. Whether G6PD contributes to the development of cancer independent of its metabolic and enzyme function needs to be further discussed. The development of drug resistance is the main cause contributing to the failure of chemotherapy, which is tightly related to the prognosis and survival of patients. Inhibiting G6PD could reverse the chemo-resistance. PPP produces NADPH so that cancer cells with hyper PPP activity have a different intracellular redox system, and this makes drug-resistant cells less susceptible to oxidative stress induced by chemotherapeutic drugs. Reversed chemo-resistance was achieved in the experiment performed by Hong et al., Feng et al. and Yang et al. Based on the essential functions in developing cancer, finding a G6PD inhibitor may be an effective way of treating cancer. Several inhibitors have been found and been proven to suppress the proliferation of cancer cells. However, problems still exist. According to scientific reports, DHEA is an endogenous steroid hormone, and it is a strong noncompetitive inhibitor that can suppress G6PD. Besides, it is the only G6PD inhibitor that was used in vivo. Though DHEA could induce the apoptosis of cancer cells through G6PD, clinical trials of DHEA have been hampered by the high oral dose required and the hindering in the conversion of DHEA to active androgen. Therefore, its effectiveness as a G6PD inhibitor remains controversial. Other chemicals such as polygonin, zoledronic acid, RRX-001, Phytol, 6-AN, ect. inhibit G6PD activity or reduce the expression level of G6PD as well. However, their effectiveness in vivo and whether they can be further used in clinical are still unknown. What is more, whether these inhibitors are also efficient in tumors with low G6PD expression, and whether these inhibitors can reverse the chemoresistance of the current clinical drugs in treating cancer are questions that need to be further explored. Developing more potential drugs aimed at G6PD is a promising but still long and rough way in cancer treatment.
In conclusion, this review described the history and structure of G6PD, the effects of high G6PD expression (or high activity) on cancer, the regulation of G6PD expression from different aspects, and the role of G6PD in chemoresistance. However, the regulated mechanisms linked to G6PD are complicated and not fully understood; thus, which mechanism is most important in cancer development is still unknown. Further studies are necessary to reveal more possibilities of G6PD in cancer because of its important role in both providing biosynthesis material and NADPH for redox equilibrium.
Author Contributions
J.S.: Investigation, Writing—original draft, Visualization, and Software. H.S.: Investigation, Writing—original draft, and Visualization. S.Z.: Conceptualization, Supervision, Writing—original draft, Writing—review and editing, and Funding acquisition. C.S.: Conceptualization, Supervision, Writing—original draft, Writing—review and editing, and Funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the National Nature Science Foundation of China (81973356 and 81902826); the Fundamental Research Funds for the Central Universities, Nankai University (3206054, 91923101, 63213082, and 92122017), supported by the State Key Laboratory of Drug Research (SIMM2105KF-08), and the National Key R&D Program of China (No. 2018YFC2002000).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Warburg, O.; Christian, W.; Griese, A. Wasserstoffübertragendes Co-Ferment, seine Zusammensetzung und Wirkungsweise. Biochem. Z. 1935, 282, 157–205. [Google Scholar]
- Horecker, B.L. The pentose phosphate pathway. J. Biol. Chem. 2002, 277, 47965–47971. [Google Scholar] [CrossRef]
- Alving, A.S.; Carson, P.E.; Flanagan, C.L.; Ickes, C.E. Enzymatic deficiency in primaquine-sensitive erythrocytes. Science 1956, 124, 484–485. [Google Scholar] [PubMed]
- Cappellini, M.D.; Fiorelli, G. Glucose-6-phosphate dehydrogenase deficiency. Lancet 2008, 371, 64–74. [Google Scholar] [CrossRef]
- Beaconsfield, P.; Rainsbury, R.; Kalton, G. Glucose-6-Phosphate Dehydrogenase Deficiency and the Incidence of Cancer. Oncology 1965, 19, 11–19. [Google Scholar] [CrossRef]
- Persico, M.G.; Viglietto, G.; Martini, G.; Toniolo, D.; Paonessa, G.; Moscatelli, C.; Dono, R.; Vulliamy, T.; Luzzatto, L.; D’urso, M. Isolation of human glucose-6-phosphate dehydrogenase (G6PD) cDNA clones: Primary structure of the protein and unusual 5’ non-coding region. Nucleic Acids Res. 1986, 14, 2511–2522. [Google Scholar] [CrossRef]
- Rowland, P.; Basak, A.K.; Gover, S.; Levy, H.R.; Adams, M.J. The three-dimensional structure of glucose 6-phosphate dehydrogenase from Leuconostoc mesenteroides refined at 2.0 A resolution. Structure 1994, 2, 1073–1087. [Google Scholar] [CrossRef]
- Bandell, M.; Lhotte, M.E.; Marty-Teysset, C.; Veyrat, A.; Prévost, H.; Dartois, V.; Divies, C.; Konings, W.N.; Lolkema, J.S. Mechanism of the citrate transporters in carbohydrate and citrate cometabolism in Lactococcus and Leuconostoc species. Appl. Environ. Microbiol. 1998, 64, 1594–1600. [Google Scholar] [CrossRef]
- Marty-Teysset, C.; Lolkema, J.S.; Schmitt, P.; Diviès, C.; Konings, W.N. The citrate metabolic pathway in Leuconostoc mesenteroides: Expression, amino acid synthesis, and alpha-ketocarboxylate transport. J. Bacteriol. 1996, 178, 6209–6215. [Google Scholar] [CrossRef]
- Haghighi, B.; Levy, H.R. Glucose-6-phosphate dehydrogenase from Leuconostoc mesenteroides. Conformational transitions induced by nicotinamide adenine dinucleotide, nicotinamide adenine dinucleotide phosphate, and glucose 6-phosphate monitored by fluorescent probes. Biochemistry 1982, 21, 6421–6428. [Google Scholar] [CrossRef]
- Olive, C.; Geroch, M.E.; Levy, H.R. Glucose 6-phosphate dehydrogenase from Leuconostoc mesenteroides. Kinetic studies. J. Biol. Chem. 1971, 246, 2047–2057. [Google Scholar] [CrossRef]
- Bondar, R.J.; Mead, D.C. Evaluation of glucose-6-phosphate dehydrogenase from Leuconostoc mesenteroides in the hexokinase method for determining glucose in serum. Clin. Chem. 1974, 20, 586–590. [Google Scholar] [CrossRef]
- Ravera, S.; Calzia, D.; Morelli, A.; Panfoli, I. Oligomerization studies of Leuconostoc mesenteroides G6PD activity after SDS-PAGE and blotting. Mol. Biol. 2010, 44, 472–476. [Google Scholar] [CrossRef]
- Au, S.W.; Gover, S.; Lam, V.M.; Adams, M.J. Human glucose-6-phosphate dehydrogenase: The crystal structure reveals a structural NADP(+) molecule and provides insights into enzyme deficiency. Structure 2000, 8, 293–303. [Google Scholar] [CrossRef]
- Spencer, N.Y.; Stanton, R.C. Glucose 6-phosphate dehydrogenase and the kidney. Curr. Opin. Nephrol. Hypertens. 2017, 26, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Allahverdiyev, A.M.; Bagirova, M.; Elcicek, S.; Koc, R.C.; Ates, S.C.; Baydar, S.Y.; Yaman, S.; Abamor, E.S.; Oztel, O.N. Glucose-6-Phosphate Dehydrogenase Deficiency and Malaria: A Method to Detect Primaquine-Induced Hemolysis in vitro. In Dehydrogenases; IntechOpen: London, UK, 2012. [Google Scholar]
- Kotaka, M.; Gover, S.; Vandeputte-Rutten, L.; Au, S.W.; Lam, V.M.; Adams, M.J. Structural studies of glucose-6-phosphate and NADP+ binding to human glucose-6-phosphate dehydrogenase. Acta Crystallogr. D Biol. Crystallogr. 2005, 61 Pt 5, 495–504. [Google Scholar] [CrossRef]
- Wang, X.T.; Chan, T.F.; Lam, V.M.; Engel, P.C. What is the role of the second “structural” NADP+-binding site in human glucose 6-phosphate dehydrogenase? Protein Sci. 2008, 17, 1403–1411. [Google Scholar] [CrossRef] [PubMed]
- Beutler, E.; Hartman, K.; Gelbart, T.; Forman, L. G-6-PD Walter Reed: Possible insight into “structural” NADP in G-6-PD. Am. J. Hematol. 1986, 23, 25–30. [Google Scholar] [CrossRef] [PubMed]
- American Association of Neurological Surgeons (AANS); American Society of Neuroradiology (ASNR); Cardiovascular and Interventional Radiology Society of Europe (CIRSE); Canadian Interventional Radiology Association (CIRA); Congress of Neurological Surgeons (CNS); European Society of Minimally Invasive Neurological Therapy (ESMINT); European Society of Neuroradiology (ESNR); European Stroke Organization (ESO); Society for Cardiovascular Angiography and Interventions (SCAI); Society of Interventional Radiology (SIR); et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar]
- National Organization for Rare Disorders. Available online: https://rarediseases.org/rare-diseases/glucose-6-phosphate-dehydrogenase-deficiency (accessed on 24 July 2019).
- Available online: https://emedicine.medscape.com/article/200390-treatment#d10 (accessed on 25 July 2020).
- Italian G6PD Deficiency Association. Drugs That Should Be Avoided: Offi Cial List. Available online: www.g6pd.org/en/G6PDDeficiency/SafeUnsafe/DaEvitare_ISS-it (accessed on 24 July 2020).
- Cohen, P.; Rosemeyer, M.A. Subunit interactions of glucose-6-phosphate dehydrogenase from human erythrocytes. Eur. J. Biochem. 1969, 8, 8–15. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Warburg, O.; Wind, F.; Negelein, E. The Metabolism of Tumors in the Body. J. Gen. Physiol. 1927, 8, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yuan, W.; Chen, Z.; Wu, S.; Chen, J.; Ge, J.; Hou, F.; Chen, Z. Overexpression of G6PD is associated with poor clinical outcome in gastric cancer. Tumour Biol. 2012, 33, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Gao, C.; Feng, X.; Jiang, M. miR-613 suppresses migration and invasion in esophageal squamous cell carcinoma via the targeting of G6PD. Exp. Ther. Med. 2020, 19, 3081–3089. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Han, Q.; Yang, Z.; Ni, Y.; Agbana, Y.L.; Bai, H.; Yi, Z.; Yi, X.; Kuang, Y.; Zhu, Y. G6PD facilitates clear cell renal cell carcinoma invasion by enhancing MMP2 expression through ROS-MAPK axis pathway. Int. J. Oncol. 2020, 57, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Shan, C.; Lu, Z.; Li, Z.; Sheng, H.; Fan, J.; Qi, Q.; Liu, S.; Zhang, S. 4-hydroxyphenylpyruvate dioxygenase promotes lung cancer growth via pentose phosphate pathway (PPP) flux mediated by LKB1-AMPK/HDAC10/G6PD axis. Cell Death Dis. 2019, 10, 525. [Google Scholar] [CrossRef]
- Du, W.; Jiang, P.; Mancuso, A.; Stonestrom, A.; Brewer, M.D.; Minn, A.J.; Mak, T.W.; Wu, M.; Yang, X. TAp73 enhances the pentose phosphate pathway and supports cell proliferation. Nat. Cell Biol. 2013, 15, 991–1000. [Google Scholar] [CrossRef]
- Ye, H.; Huang, H.; Cao, F.; Chen, M.; Zheng, X.; Zhan, R. HSPB1 Enhances SIRT2-Mediated G6PD Activation and Promotes Glioma Cell Proliferation. PLoS ONE 2016, 11, e0164285. [Google Scholar] [CrossRef]
- Lu, M.; Lu, L.; Dong, Q.; Yu, G.; Chen, J.; Qin, L.; Wang, L.; Zhu, W.; Jia, H. Elevated G6PD expression contributes to migration and invasion of hepatocellular carcinoma cells by inducing epithelial-mesenchymal transition. Acta Biochim. Biophys. Sin. 2018, 50, 70–380. [Google Scholar] [CrossRef]
- Nagashio, R.; Oikawa, S.; Yanagita, K.; Hagiuda, D.; Kuchitsu, Y.; Igawa, S.; Naoki, K.; Satoh, Y.; Ichinoe, M.; Murakumo, Y.; et al. Prognostic significance of G6PD expression and localization in lung adenocarcinoma. Biochim. Biophys. Acta Proteins Proteom. 2019, 1867, 38–46. [Google Scholar] [CrossRef]
- Yang, C.A.; Huang, H.Y.; Lin, C.L.; Chang, J.G. G6PD as a predictive marker for glioma risk, prognosis and chemosensitivity. J. Neurooncol. 2018, 139, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Ju, H.Q.; Lu, Y.X.; Wu, Q.N.; Liu, J.; Zeng, Z.L.; Mo, H.Y.; Chen, Y.; Tian, T.; Wang, Y.; Kang, T.B.; et al. Disrupting G6PD-mediated Redox homeostasis enhances chemosensitivity in colorectal cancer. Oncogene 2017, 36, 6282–6292. [Google Scholar] [CrossRef]
- Poulain, L.; Sujobert, P.; Zylbersztejn, F.; Barreau, S.; Stuani, L.; Lambert, M.; Palama, T.L.; Chesnais, V.; Birsen, R.; Vergez, F.; et al. High mTORC1 activity drives glycolysis addiction and sensitivity to G6PD inhibition in acute myeloid leukemia cells. Leukemia 2017, 31, 2326–2335. [Google Scholar] [CrossRef] [PubMed]
- Mele, L.; la Noce, M.; Paino, F.; Regad, T.; Wagner, S.; Liccardo, D.; Papaccio, G.; Lombardi, A.; Caraglia, M.; Tirino, V.; et al. Glucose-6-phosphate dehydrogenase blockade potentiates tyrosine kinase inhibitor effect on breast cancer cells through autophagy perturbation. J. Exp. Clin. Cancer Res. 2019, 38, 160. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, X.; Zhang, X.; Fan, R.; Gu, H.; Shi, Y.; Liu, H. Glucose-6-phosphate dehydrogenase expression is correlated with poor clinical prognosis in esophageal squamous cell carcinoma. Eur. J. Surg. Oncol. 2015, 41, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.H.; Li, S.; Du, Z.X.; Liu, C.; Liu, B.Q.; Li, C.; Zong, Z.H.; Wang, H.Q. BAG3 elevation inhibits cell proliferation via direct interaction with G6PD in hepatocellular carcinomas. Oncotarget 2016, 7, 700–711. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, D.; Zhu, Y.; Tang, Q.; Lu, H.; Li, H.; Yang, Y.; Li, Z.; Tong, S. A new G6PD knockdown tumor-cell line with reduced proliferation and increased susceptibility to oxidative stress. Cancer Biother. Radiopharm. 2009, 24, 81–90. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Yang, J.; Ding, J.; Li, S.; Wu, H.; Xiong, Y.; Zhou, F.; Jiang, Y.; Teng, L.; Yang, J. Downregulation of glucose-6-phosphate dehydrogenase by microRNA-1 inhibits the growth of pituitary tumor cells. Oncol. Rep. 2018, 40, 3533–3542. [Google Scholar] [CrossRef]
- Bao, B.Y.; Ting, H.J.; Hsu, J.W.; Lee, Y.F. Protective role of 1 alpha, 25-dihydroxyvitamin D3 against oxidative stress in nonmalignant human prostate epithelial cells. Int. J. Cancer 2008, 122, 2699–2706. [Google Scholar] [CrossRef]
- Wu, S.; Wang, H.; Li, Y.; Xie, Y.; Huang, C.; Zhao, H.; Miyagishi, M.; Kasim, V. Transcription Factor YY1 Promotes Cell Proliferation by Directly Activating the Pentose Phosphate Pathway. Cancer Res. 2018, 78, 4549–4562. [Google Scholar] [CrossRef]
- Yin, X.; Tang, B.; Li, J.H.; Wang, Y.; Zhang, L.; Xie, X.Y.; Zhang, B.H.; Qiu, S.J.; Wu, W.Z.; Ren, Z.G. ID1 promotes hepatocellular carcinoma proliferation and confers chemoresistance to oxaliplatin by activating pentose phosphate pathway. J. Exp. Clin. Cancer Res. 2017, 36, 166. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Yang, Z.; Han, Q.; Bai, H.; Wang, Y.; Yi, X.; Yi, Z.; Yang, L.; Jiang, L.; Song, X.; et al. G6PD promotes renal cell carcinoma proliferation through positive feedback regulation of p-STAT3. Oncotarget 2017, 8, 109043–109060. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Sheng, H.; Wu, T.; Song, J.; Sun, H.; Wang, Y.; Wang, J.; Li, Z.; Zhao, H.; Tan, J.; et al. PIKE-A promotes glioblastoma growth by driving PPP flux through increasing G6PD expression mediated by phosphorylation of STAT3. Biochem. Pharmacol. 2021, 192, 114736. [Google Scholar] [CrossRef] [PubMed]
- Düvel, K.; Yecies, J.L.; Menon, S.; Raman, P.; Lipovsky, A.I.; Souza, A.L.; Triantafellow, E.; Ma, Q.; Gorski, R.; Cleaver, S.; et al. Activation of a metabolic gene regulatory network downstream of mTOR complex 1. Mol. Cell 2010, 39, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Amemiya-Kudo, M.; Shimano, H.; Hasty, A.H.; Yahagi, N.; Yoshikawa, T.; Matsuzaka, T.; Okazaki, H.; Tamura, Y.; Iizuka, Y.; Ohashi, K.; et al. Transcriptional activities of nuclear SREBP-1a, -1c, and -2 to different target promoters of lipogenic and cholesterogenic genes. J. Lipid Res. 2002, 43, 1220–1235. [Google Scholar] [CrossRef]
- Jiang, P.; Du, W.; Yang, X. A critical role of glucose-6-phosphate dehydrogenase in TAp73-mediated cell proliferation. Cell Cycle 2013, 12, 3720–3726. [Google Scholar] [CrossRef]
- Wang, E.; Aifantis, I. RNA Splicing and Cancer. Trends Cancer 2020, 6, 631–644. [Google Scholar] [CrossRef]
- Hong, X.; Song, R.; Song, H.; Zheng, T.; Wang, J.; Liang, Y.; Qi, S.; Lu, Z.; Song, X.; Jiang, H.; et al. PTEN antagonises Tcl1/hnRNPK-mediated G6PD pre-mRNA splicing which contributes to hepatocarcinogenesis. Gut 2014, 63, 1635–1647. [Google Scholar] [CrossRef]
- Hu, T.; Chang, Y.F.; Xiao, Z.; Mao, R.; Tong, J.; Chen, B.; Liu, G.C.; Hong, Y.; Chen, H.L.; Kong, S.Y.; et al. miR-1 inhibits progression of high-risk papillomavirus-associated human cervical cancer by targeting G6PD. Oncotarget 2016, 7, 86103–86116. [Google Scholar] [CrossRef]
- Barajas, J.M.; Reyes, R.; Guerrero, M.J.; Jacob, S.T.; Motiwala, T.; Ghoshal, K. The role of miR-122 in the dysregulation of glucose-6-phosphate dehydrogenase (G6PD) expression in hepatocellular cancer. Sci. Rep. 2018, 8, 9105. [Google Scholar] [CrossRef]
- Cui, J.; Pan, Y.; Wang, J.; Liu, Y.; Wang, H.; Li, H. MicroRNA-206 suppresses proliferation and predicts poor prognosis of HR-HPV-positive cervical cancer cells by targeting G6PD. Oncol. Lett. 2018, 16, 5946–5952. [Google Scholar] [CrossRef] [PubMed]
- Coda, D.M.; Lingua, M.F.; Morena, D.; Foglizzo, V.; Bersani, F.; Ala, U.; Ponzetto, C.; Taulli, R. SMYD1 and G6PD modulation are critical events for miR-206-mediated differentiation of rhabdomyosarcoma. Cell Cycle 2015, 14, 1389–1402. [Google Scholar] [CrossRef] [PubMed]
- Ai, G.; Dachineni, R.; Kumar, D.R.; Alfonso, L.F.; Marimuthu, S.; Bhat, G.J. Aspirin inhibits glucose-6-phosphate dehydrogenase activity in HCT 116 cells through acetylation: Identification of aspirin-acetylated sites. Mol. Med. Rep. 2016, 14, 1726–1732. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.N.; Wang, T.S.; Li, X.; Wang, Y.P. SIRT2 activates G6PD to enhance NADPH production and promote leukaemia cell proliferation. Sci. Rep. 2016, 6, 32734. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.P.; Zhou, L.S.; Zhao, Y.Z.; Wang, S.W.; Chen, L.L.; Liu, L.X.; Ling, Z.Q.; Hu, F.J.; Sun, Y.P.; Zhang, J.Y.; et al. Regulation of G6PD acetylation by SIRT2 and KAT9 modulates NADPH homeostasis and cell survival during oxidative stress. EMBO J. 2014, 33, 1304–1320. [Google Scholar] [CrossRef]
- Rao, X.; Duan, X.; Mao, W.; Li, X.; Li, Z.; Li, Q.; Zheng, Z.; Xu, H.; Chen, M.; Wang, P.G.; et al. O-GlcNAcylation of G6PD promotes the pentose phosphate pathway and tumor growth. Nat. Commun. 2015, 6, 8468. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Wang, L.; Huang, D.; Li, Y.; Yang, D.; Li, T.; Li, F.; Sun, L.; Wei, H.; He, K.; et al. Polo-like kinase 1 coordinates biosynthesis during cell cycle progression by directly activating pentose phosphate pathway. Nat. Commun. 2017, 8, 1506. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Du, W.; Wang, X.; Mancuso, A.; Gao, X.; Wu, M.; Yang, X. p53 regulates biosynthesis through direct inactivation of glucose-6-phosphate dehydrogenase. Nat. Cell Biol. 2011, 13, 310–316. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, X.; Li, Y.; Shao, Y.; Xiao, J.; Zhu, G.; Li, F. PAK4 regulates G6PD activity by p53 degradation involving colon cancer cell growth. Cell Death Dis. 2017, 8, e2820. [Google Scholar] [CrossRef]
- Cosentino, C.; Grieco, D.; Costanzo, V. ATM activates the pentose phosphate pathway promoting anti-oxidant defence and DNA repair. EMBO J. 2011, 30, 546–555. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Q.; Niu, L.; Xu, L.; Guo, Y.; Wang, L.; Guo, C. Suppression of G6PD induces the expression and bisecting GlcNAc-branched N-glycosylation of E-Cadherin to block epithelial-mesenchymal transition and lymphatic metastasis. Br. J. Cancer 2020, 123, 1315–1325. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Xu, Z.; Zhu, Z.; Chen, A.; Fu, G.; Wang, Y.; Pan, H.; Jin, B. Modulation of G6PD affects bladder cancer via ROS accumulation and the AKT pathway in vitro. Int. J. Oncol. 2018, 53, 1703–1712. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Olszewski, K.; Zhang, Y.; Lim, E.W.; Shi, J.; Zhang, X.; Zhang, J.; Lee, H.; Koppula, P.; Lei, G.; et al. Cystine transporter regulation of pentose phosphate pathway dependency and disulfide stress exposes a targetable metabolic vulnerability in cancer. Nat. Cell Biol. 2020, 22, 476–486. [Google Scholar] [CrossRef] [PubMed]
- Yi, H.; Zheng, X.; Song, J.; Shen, R.; Su, Y.; Lin, D. Exosomes mediated pentose phosphate pathway in ovarian cancer metastasis: A proteomics analysis. Int. J. Clin. Exp. Pathol. 2015, 8, 15719–15728. [Google Scholar] [PubMed]
- Polimeni, M.; Voena, C.; Kopecka, J.; Riganti, C.; Pescarmona, G.; Bosia, A.; Ghigo, D. Modulation of doxorubicin resistance by the glucose-6-phosphate dehydrogenase activity. Biochem. J. 2011, 439, 141–149. [Google Scholar] [CrossRef]
- Yamawaki, K.; Mori, Y.; Sakai, H.; Kanda, Y.; Shiokawa, D.; Ueda, H.; Ishiguro, T.; Yoshihara, K.; Nagasaka, K.; Onda, T.; et al. Integrative analyses of gene expression and chemosensitivity of patient-derived ovarian cancer spheroids link G6PD-driven redox metabolism to cisplatin chemoresistance. Cancer Lett. 2021, 521, 29–38. [Google Scholar] [CrossRef]
- Feng, Q.; Li, X.; Sun, W.; Sun, M.; Li, Z.; Sheng, H.; Xie, F.; Zhang, S.; Shan, C. Targeting G6PD reverses paclitaxel resistance in ovarian cancer by suppressing GSTP1. Biochem. Pharmacol. 2020, 178, 114092. [Google Scholar] [CrossRef]
- Arbe, M.F.; Agnetti, L.; Breininger, E.; Glikin, G.C.; Finocchiaro, L.M.E.; Villaverde, M.S. Glucose 6-phosphate dehydrogenase inhibition sensitizes melanoma cells to metformin treatment. Transl. Oncol. 2020, 13, 100842. [Google Scholar] [CrossRef]
- Varshney, R.; Dwarakanath, B.; Jain, V. Radiosensitization by 6-aminonicotinamide and 2-deoxy-D-glucose in human cancer cells. Int. J. Radiat. Biol. 2005, 81, 397–408. [Google Scholar] [CrossRef]
- Schwartz, A.G.; Pashko, L.L. Dehydroepiandrosterone, glucose-6-phosphate dehydrogenase, and longevity. Ageing Res. Rev. 2004, 3, 171–187. [Google Scholar] [CrossRef]
- Fang, Z.; Jiang, C.; Feng, Y.; Chen, R.; Lin, X.; Zhang, Z.; Han, L.; Chen, X.; Li, H.; Guo, Y.; et al. Effects of G6PD activity inhibition on the viability, ROS generation and mechanical properties of cervical cancer cells. Biochim. Biophys. Acta 2016, 1863, 2245–2254. [Google Scholar] [CrossRef]
- Mele, L.; Paino, F.; Papaccio, F.; Regad, T.; Boocock, D.; Stiuso, P.; Lombardi, A.; Liccardo, D.; Aquino, G.; Barbieri, A.; et al. A new inhibitor of glucose-6-phosphate dehydrogenase blocks pentose phosphate pathway and suppresses malignant proliferation and metastasis in vivo. Cell Death Dis. 2018, 9, 572. [Google Scholar] [CrossRef]
- Chen, P.; Wang, L.; Sun, S.; Zhou, Q.; Zeng, Z.; Hu, M.; Hussain, M.; Lu, C.; Du, H. High-throughput screening suggests glutathione synthetase as an anti-tumor target of polydatin using human proteome chip. Int. J. Biol. Macromol. 2020, 161, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Shi, B.; Li, Y.; Yin, F. Polydatin inhibits cell proliferation and induces apoptosis in laryngeal cancer and HeLa cells via suppression of the PDGF/AKT signaling pathway. J. Biochem. Mol. Toxicol. 2017, 31, e21900. [Google Scholar] [CrossRef] [PubMed]
- Finianos, A.; Aragon-Ching, J.B. Zoledronic acid for the treatment of prostate cancer. Expert Opin. Pharmacother. 2019, 20, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Chen, F.K.; Liu, C.; Liu, P.J.; Feng, Z.P.; Jia, L.; Yang, Z.X.; Hou, F.; Deng, Z.Y. Zoledronic acid inhibits thyroid cancer stemness and metastasis by repressing M2-like tumor-associated macrophages induced Wnt/β-catenin pathway. Life Sci. 2020, 256, 117925. [Google Scholar] [CrossRef]
- Wang, X.; Wu, G.; Cao, G.; Yang, L.; Xu, H.; Huang, J.; Hou, J. Zoledronic acid inhibits the pentose phosphate pathway through attenuating the Ras-TAp73-G6PD axis in bladder cancer cells. Mol. Med. Rep. 2015, 12, 4620–4625. [Google Scholar] [CrossRef]
- Hua, H.; Zhang, H.; Kong, Q.; Wang, J.; Jiang, Y. Complex roles of the old drug aspirin in cancer chemoprevention and therapy. Med. Res. Rev. 2019, 39, 114–145. [Google Scholar] [CrossRef]
- Ai, G.; Hagen, F.K.; Gunaje, J.B. Aspirin acetylates glucose 6 phosphate dehydrogenase and inhibits its activity in colon cancer cells. Cancer Res. 2013, 73 (Suppl. 8), 3681. [Google Scholar]
- Oronsky, B.; Reid, T.R.; Oronsky, A.; Caroen, S.; Carter, C.A.; Cabrales, P. Brief report: RRx-001 is a c-Myc inhibitor that targets cancer stem cells. Oncotarget 2018, 9, 23439–23442. [Google Scholar] [CrossRef]
- Alencar, M.; Islam, M.T.; Ali, E.S.; Santos, J.; Paz, M.; Sousa, J.; Dantas, S.; Mishra, S.K.; Cavalcante, A. Association of Phytol with Toxic and Cytotoxic Activities in an Antitumoral Perspective: A Meta-Analysis and Systemic Review. Anticancer Agents Med. Chem. 2018, 18, 1828–1837. [Google Scholar] [CrossRef] [PubMed]
- de Alencar, M.; Islam, M.T.; de Lima, R.; Paz, M.; Dos Reis, A.C.; da Mata, A.; Filho, J.; Cerqueira, G.S.; Ferreira, P.; E Sousa, J.; et al. Phytol as an anticarcinogenic and antitumoral agent: An in vivo study in swiss mice with DMBA-Induced breast cancer. IUBMB Life 2019, 71, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Nehybová, T.; Šmarda, J.; Daniel, L.; Stiborek, M.; Kanický, V.; Spasojevič, I.; Preisler, J.; Damborský, J.; Beneš, P. Wedelolactone Acts as Proteasome Inhibitor in Breast Cancer Cells. Int. J. Mol. Sci. 2017, 18, 729. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.; Du, D.; Liu, Y.; Lu, T.; Liu, L.; Jiang, H.; Chen, K.; Shan, C.; Luo, C. Discovery and characterization of a novel glucose-6-phosphate dehydrogenase (G6PD) inhibitor via high-throughput screening. Bioorg. Med. Chem. Lett. 2021, 40, 127905. [Google Scholar] [CrossRef]
- Torun, A.; Enayat, S.; Sheraj, I.; Tunçer, S.; Ülgen, D.H.; Banerjee, S. Butyrate mediated regulation of RNA binding proteins in the post-transcriptional regulation of inflammatory gene expression. Cell Signal. 2019, 64, 109410. [Google Scholar] [CrossRef]
- Yoo, H.Y.; Park, S.Y.; Chang, S.Y.; Kim, S.H. Regulation of Butyrate-Induced Resistance through AMPK Signaling Pathway in Human Colon Cancer Cells. Biomedicines 2021, 9, 1604. [Google Scholar] [CrossRef]
- Magrin, G.L.; Di Summa, F.; Strauss, F.J.; Panahipour, L.; Mildner, M.; Magalhães Benfatti, C.A.; Gruber, R. Butyrate Decreases ICAM-1 Expression in Human Oral Squamous Cell Carcinoma Cells. Int. J. Mol. Sci. 2020, 21, 1679. [Google Scholar] [CrossRef]
- Geng, H.W.; Yin, F.Y.; Zhang, Z.F.; Gong, X.; Yang, Y. Butyrate Suppresses Glucose Metabolism of Colorectal Cancer Cells via GPR109a-AKT Signaling Pathway and Enhances Chemotherapy. Front. Mol. Biosci. 2021, 8, 634874. [Google Scholar] [CrossRef]
- Preuss, J.; Richardson, A.D.; Pinkerton, A.; Hedrick, M.; Sergienko, E.; Rahlfs, S.; Becker, K.; Bode, L. Identification and characterization of novel human glucose-6-phosphate dehydrogenase inhibitors. J. Biomol. Screen. 2013, 18, 286–297. [Google Scholar] [CrossRef]
- Zhao, Z.B.; Liu, Y.; Yao, Y. Computational determination of binding structures and free energies of glucose 6-phosphate dehydrogenase with novel steroid inhibitors. J. Mol. Graph. Model. 2014, 51, 168–172. [Google Scholar] [CrossRef]
- Yang, H.C.; Stern, A.; Chiu, D.T. G6PD: A hub for metabolic reprogramming and redox signaling in cancer. Biomed. J. 2020, 44, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; He, Z.; Yao, J.; Tan, R.; Zhu, Y.; Li, Z.; Guo, Q.; Wei, L. Regulation of AMPK-related glycolipid metabolism imbalances redox homeostasis and inhibits anchorage independent growth in human breast cancer cells. Redox Biol. 2018, 17, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Joshi, K.; Hassan, S.S.; Ramaraj, P. Differential biological effects of dehydroepiandrosterone (DHEA) between mouse (B16F10) and human melanoma (BLM) cell lines. Dermatoendocrinology 2017, 9, e1389360. [Google Scholar] [CrossRef]
- Hakkak, R.; Bell, A.; Korourian, S. Dehydroepiandrosterone (DHEA) Feeding Protects Liver Steatosis in Obese Breast Cancer Rat Model. Sci. Pharm. 2017, 85, 13. [Google Scholar] [CrossRef]
- Chen, Y.; Niu, J.; Li, L.; Li, Z.; Jiang, J.; Zhu, M.; Dong, T.; Zhang, J.; Shi, C.; Xu, P.; et al. Polydatin executes anticancer effects against glioblastoma multiforme by inhibiting the EGFR-AKT/ERK1/2/STAT3-SOX2/Snail signaling pathway. Life Sci. 2020, 258, 118158. [Google Scholar] [CrossRef]
- Liu, Y.L.; Chen, B.Y.; Nie, J.; Zhao, G.H.; Zhuo, J.Y.; Yuan, J.; Li, Y.C.; Wang, L.L.; Chen, Z.W. Polydatin prevents bleomycin-induced pulmonary fibrosis by inhibiting the TGF-β/Smad/ERK signaling pathway. Exp. Ther. Med. 2020, 20, 62. [Google Scholar] [CrossRef] [PubMed]
- Boran, G.; Tavakoli, S.; Dierking, I.; Kamali, A.R.; Ege, D. Synergistic effect of graphene oxide and zoledronic acid for osteoporosis and cancer treatment. Sci. Rep. 2020, 10, 7827. [Google Scholar] [CrossRef]
- Hao, W.; Shen, Y.; Feng, M.; Wang, H.; Lin, M.; Fang, Y.; Tan, L. Aspirin acts in esophageal cancer: A brief review. J. Thorac. Dis. 2018, 10, 2490–2497. [Google Scholar] [CrossRef]
- Song, Y.; Zhong, X.; Gao, P.; Zhou, C.; Shi, J.; Wu, Z.; Guo, Z.; Wang, Z. Aspirin and Its Potential Preventive Role in Cancer: An Umbrella Review. Front. Endocrinol. 2020, 11, 3. [Google Scholar] [CrossRef]
- Singh, A.K.; Trotman, B.W. Use and safety of aspirin in the chemoprevention of colorectal cancer. J. Assoc. Acad. Minor. Phys. 1998, 9, 40–44. [Google Scholar]
- Morgensztern, D.; Rose, M.; Waqar, S.N.; Morris, J.; Ma, P.C.; Reid, T.; Brzezniak, C.E.; Zeman, K.G.; Padmanabhan, A.; Hirth, J.; et al. RRx-001 followed by platinum plus etoposide in patients with previously treated small-cell lung cancer. Br. J. Cancer 2019, 121, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Oronsky, B.; Scicinski, J.; Reid, T.; Oronsky, A.; Carter, C.; Oronsky, N.; Cabrales, P. RRx-001, a novel clinical-stage chemosensitizer, radiosensitizer, and immunosensitizer, inhibits glucose 6-phosphate dehydrogenase in human tumor cells. Discov. Med. 2016, 21, 251–265. [Google Scholar] [PubMed]
- Cirrik, S.; Ugurel, E.; Aksu, A.C.; Oronsky, B.; Cabrales, P.; Yalcin, O. Nitrite may serve as a combination partner and a biomarker for the anti-cancer activity of RRx-001. Biorheology 2019, 56, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Thakor, P.; Subramanian, R.B.; Thakkar, S.S.; Ray, A.; Thakkar, V.R. Phytol induces ROS mediated apoptosis by induction of caspase 9 and 3 through activation of TRAIL, FAS and TNF receptors and inhibits tumor progression factor Glucose 6 phosphate dehydrogenase in lung carcinoma cell line (A549). Biomed. Pharmacother. 2017, 92, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Soltanian, S.; Sheikhbahaei, M.; Ziasistani, M. Phytol Down-Regulates Expression of Some Cancer Stem Cell Markers and Decreases Side Population Proportion in Human Embryonic Carcinoma NCCIT Cells. Nutr. Cancer 2020, 73, 1520–1533. [Google Scholar] [CrossRef]
- Pan, H.; Lin, Y.; Dou, J.; Fu, Z.; Yao, Y.; Ye, S.; Zhang, S.; Wang, N.; Liu, A.; Li, X.; et al. Wedelolactone facilitates Ser/Thr phosphorylation of NLRP3 dependent on PKA signalling to block inflammasome activation and pyroptosis. Cell Prolif. 2020, 53, e12868. [Google Scholar] [CrossRef]
- Zhu, M.M.; Wang, L.; Yang, D.; Li, C.; Pang, S.T.; Li, X.H.; Li, R.; Yang, B.; Lian, Y.P.; Ma, L.; et al. Wedelolactone alleviates doxorubicin-induced inflammation and oxidative stress damage of podocytes by IκK/IκB/NF-κB pathway. Biomed. Pharmacother. 2019, 117, 109088. [Google Scholar] [CrossRef]
- Liu, Y.Q.; Han, X.F.; Bo, J.X.; Ma, H.P. Wedelolactone Enhances Osteoblastogenesis but Inhibits Osteoclastogenesis through Sema3A/NRP1/PlexinA1 Pathway. Front. Pharmacol. 2016, 7, 375. [Google Scholar] [CrossRef]
- Donohoe, D.R.; Garge, N.; Zhang, X.; Sun, W.; O’Connell, T.M.; Bunger, M.K.; Bultman, S.J. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 2011, 13, 517–526. [Google Scholar] [CrossRef]
- Beisner, J.; Filipe Rosa, L.; Kaden-Volynets, V.; Stolzer, I.; Günther, C.; Bischoff, S.C. Prebiotic Inulin and Sodium Butyrate Attenuate Obesity-Induced Intestinal Barrier Dysfunction by Induction of Antimicrobial Peptides. Front. Immunol. 2021, 12, 678360. [Google Scholar] [CrossRef]
- Torun, A.; Enayat, S.; Sheraj, I.; Tunçer, S.; Ülgen, D.H.; Banerjee, S. Butyrate impairs atherogenesis by reducing plaque inflammation and vulnerability and decreasing NFκB activation. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 606–613. [Google Scholar]
- Sukhatme, V.P.; Chan, B. Glycolytic cancer cells lacking 6-phosphogluconate dehydrogenase metabolize glucose to induce senescence. FEBS Lett. 2012, 586, 2389–2395. [Google Scholar] [CrossRef] [PubMed]
- Chan, B.; VanderLaan, P.A.; Sukhatme, V.P. 6-Phosphogluconate dehydrogenase regulates tumor cell migration in vitro by regulating receptor tyrosine kinase c-Met. Biochem. Biophys. Res. Commun. 2013, 439, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Shaw, R.J.; Kosmatka, M.; Bardeesy, N.; Hurley, R.L.; Witters, L.A.; DePinho, R.A.; Cantley, L.C. The tumor suppressor LKB1 kinase directly activates AMP-activated kinase and regulates apoptosis in response to energy stress. Proc. Natl. Acad. Sci. USA 2004, 101, 3329–3335. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).