Photobiomodulation for Lowering Pain after Tonsillectomy: Low Efficacy and a Possible Unexpected Adverse Effect
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethics
2.3. Eligible Criteria
- Age >3 and <18 years;
- Tonsillectomy or adenotonsillectomy due to apneic roncopathy, and/or obstructive sleep apnea, and/or recurrent tonsillitis;
- Exclusion criteria:
- ASA Score > 2;
- Neuropsychiatric comorbidity;
- Pro-hemorrhage coagulation disorders.
2.4. Population Characteristics
2.5. Procedures
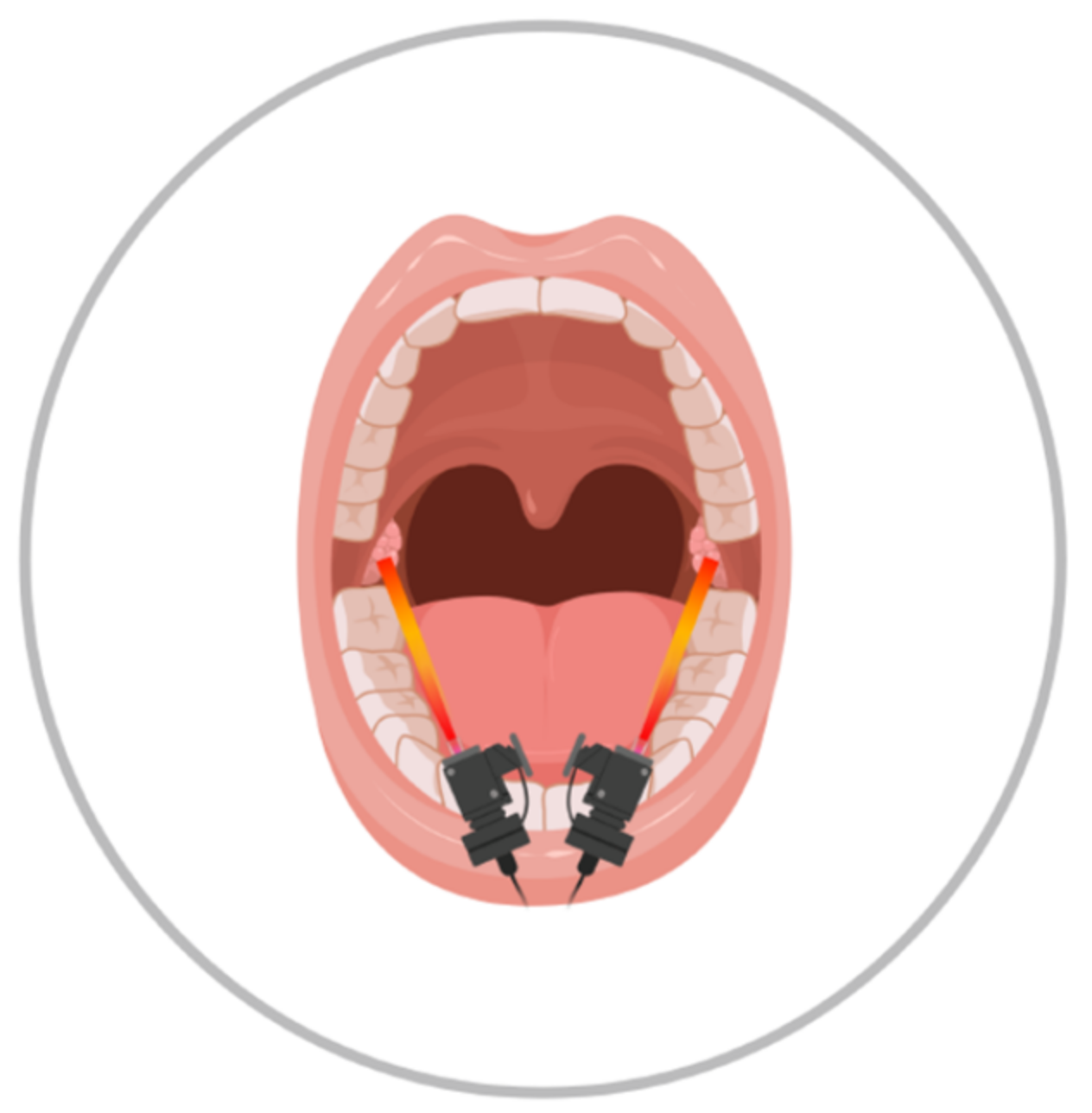
2.6. PBM Protocol
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mitchell, R.B.; Archer, S.M.; Ishman, S.L.; Rosenfeld, R.M.; Coles, S.; Finestone, S.A.; Friedman, N.R.; Giordano, T.; Hildrew, D.; Kim, T.W.; et al. Clinical Practice Guideline: Tonsillectomy in Children (Update)—Executive Summary. Otolaryngol. Neck Surg. 2019, 160, 187–205. [Google Scholar] [CrossRef] [PubMed]
- Hashmi, M.A.; Ahmed, A.; Aslam, S.; Mubeen, M. Post-tonsillectomy pain and vomiting:role of pre-operative steroids. J. Coll. Physicians Surg. Pak. 2012, 22, 505–509. [Google Scholar] [PubMed]
- Matys, J.; Flieger, R.; Świder, K.; Gedrange, T.; Hutchings, G.; Dyszkiewicz-Konwińska, M.; Kempisty, B.; Nammour, S.; Dominiak, M.; Grzech-Leśniak, K. A Clinical Trial of Photobiomodulation Effect on Orthodontic Microscrews Stability Using a 635 nm Red Laser Light. Photobiomodulation. Photomed. Laser Surg. 2020, 38, 607–613. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Zhang, B.; Shen, N.; Wu, N.; Sun, J. A systematic review and meta-analysis of the effect of low-level laser therapy (LLLT) on chemotherapy-induced oral mucositis in pediatric and young patients. Eur. J. Pediatr. 2018, 177, 7–17. [Google Scholar] [CrossRef]
- Ojea, A.R.; Madi, O.; Neto, R.L.; Lima, S.E.; De Carvalho, B.T.; Ojea, M.J.M.; Marcos, R.L.; Da Silva, F.S.; Zamuner, S.R.; Chavantes, M.C. Beneficial Effects of Applying Low-Level Laser Therapy to Surgical Wounds After Bariatric Surgery. Photomed. Laser Surg. 2016, 34, 580–584. [Google Scholar] [CrossRef]
- Karlekar, A.; Bharati, S.; Saxena, R.; Mehta, K. Assessment of feasibility and efficacy of Class IV laser therapy for postoperative pain relief in off-pump coronary artery bypass surgery patients: A pilot study. Ann. Card. Anaesth. 2015, 18, 317–322. [Google Scholar] [CrossRef]
- Hamblin, M.R. Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation. Photochem. Photobiol. 2018, 94, 199–212. [Google Scholar] [CrossRef] [Green Version]
- Zupin, L.; Barbi, E.; Sagredini, R.; Ottaviani, G.; Crovella, S.; Celsi, F. In vitro effects of photobiomodulation therapy on 50B11 sensory neurons: Evaluation of cell metabolism, oxidative stress, mitochondrial membrane potential (MMP), and capsaicin-induced calcium flow. J. Biophotonics 2021, 14, e202000347. [Google Scholar] [CrossRef]
- Neiva, F.C.; Vieira, F.M.J.; Figueiredo, C.R.; Stamm, A.E.C.; Weckx, L.L.M.; Pignatari, S.S.N. Analgesia com laser terapêutico após tonsilectomia. Rev. Paul. Pediatr. 2010, 28, 322–328. [Google Scholar] [CrossRef] [Green Version]
- Aghamohammadi, D.; Eidi, M.; Lotfi, A.; Hosseinzadeh, H.; Movasaghi, R.; Motighini, N.; Bouraima, S.A. Effect of Low Level Laser Application at the End of Surgery to Reduce Pain after Tonsillectomy in Adults. J. Lasers Med. Sci. 2013, 4, 79–85. [Google Scholar]
- Windfuhr, J.P.; Schloendorff, G.; Baburi, D.; Kremer, B. Life-Threatening Posttonsillectomy Hemorrhage. Laryngoscope 2008, 118, 1389–1394. [Google Scholar] [CrossRef]
- Ignarro, L.J.; Buga, G.M.; Wood, K.S.; Byrns, R.E.; Chaudhuri, G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc. Natl. Acad. Sci. USA 1987, 84, 9265–9269. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.; Pittman, R.N.; Popel, A. Nitric Oxide in the Vasculature: Where Does It Come from and Where Does It Go? A Quantitative Perspective. Antioxid. Redox Signal. 2008, 10, 1185–1198. [Google Scholar] [CrossRef] [Green Version]
- Beltrán, B.; Mathur, A.; Duchen, M.; Erusalimsky, J.; Moncada, S. The effect of nitric oxide on cell respiration: A key to understanding its role in cell survival or death. Proc. Natl. Acad. Sci. USA 2000, 97, 14602–14607. [Google Scholar] [CrossRef] [Green Version]
- Karu, T.I.; Pyatibrat, L.V.; Kolyakov, S.F.; Afanasyeva, N.I. Absorption measurements of a cell monolayer relevant to phototherapy: Reduction of cytochrome c oxidase under near IR radiation. J. Photochem. Photobiol. B Biol. 2005, 81, 98–106. [Google Scholar] [CrossRef]
- Li, F.J.; Zhang, J.Y.; Zeng, X.-T.; Guo, Y. Low-level laser therapy for orthodontic pain: A systematic review. Lasers Med. Sci. 2015, 30, 1789–1803. [Google Scholar] [CrossRef]
- Gavish, L.; Hoffer, O.; Rabin, N.; Halak, M.; Shkilevich, S.; Shayovitz, Y.; Weizman, G.; Haim, O.; Gavish, B.; Gertz, S.D.; et al. Microcirculatory Response to Photobiomodulation—Why Some Respond and Others Do Not: A Randomized Controlled Study. Lasers Surg. Med. 2020, 52, 863–872. [Google Scholar] [CrossRef]
- Zupin, L.; Celsi, F.; Ottaviani, G.; Crovella, S.; Luisa, Z.; Fulvio, C.; Giulia, O.; Sergio, C. Photobiomodulation therapy at different wavelength impacts on retinoid acid–dependent SH-SY5Y differentiation. Lasers Med. Sci. 2020, 35, 221–226. [Google Scholar] [CrossRef]
- Chow, R.T.; David, M.A.; Armati, P.J. 830 nm laser irradiation induces varicosity formation, reduces mitochondrial membrane potential and blocks fast axonal flow in small and medium diameter rat dorsal root ganglion neurons: Implications for the analgesic effects of 830 nm laser. J. Peripher. Nerv. Syst. 2007, 12, 28–39. [Google Scholar] [CrossRef]
- Jimbo, K.; Noda, K.; Suzuki, K.; Yoda, K. Suppressive effects of low-power laser irradiation on bradykinin evoked action potentials in cultured murine dorsal root ganglion cells. Neurosci. Lett. 1998, 240, 93–96. [Google Scholar] [CrossRef]
- Ekim, A.; Armagan, O.; Tascioglu, F.; Oner, C.; Colak, M. Effect of low level laser therapy in rheumatoid arthritis patients with carpal tunnel syndrome. Swiss Med. Wkly. 2007, 137, 347–352. [Google Scholar]
- Fikácková, H.; Dostálová, T.; Navratil, L.; Klaschka, J. Effectiveness of Low-Level Laser Therapy in Temporomandibular Joint Disorders: A Placebo-Controlled Study. Photomed. Laser Surg. 2007, 25, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Ezzati, K.; Fekrazad, R.; Raoufi, Z. The Effects of Photobiomodulation Therapy on Post-Surgical Pain. J. Lasers Med. Sci. 2019, 10, 79–85. [Google Scholar] [CrossRef]
- Ottaviani, G.; Gobbo, M.; Sturnega, M.; Martinelli, V.; Mano, M.; Zanconati, F.; Bussani, R.; Perinetti, G.; Long, C.; Di Lenarda, R.; et al. Effect of Class IV Laser Therapy on Chemotherapy-Induced Oral Mucositis. A Clin. Exp. Study. Am. J. Pathologym. 2013, 183, 1747–1757. [Google Scholar] [CrossRef]

| Median Age | Min Age | Max Age | IQR | nr | |
|---|---|---|---|---|---|
| UT | 5 | 3 | 16 | 2 | 10 |
| T | 5 | 3 | 8 | 2 | 12 |
| Wavelength | Mean Power | Peak Power | Fluence | Frequency | Duration |
|---|---|---|---|---|---|
| 445 nm | 0.1 W | 0.2 W | 6 J/cm2 | 4 Hz | 60 s |
| 660 nm | 0.1 W | 0.2 W | 6 J/cm2 | 4 Hz | 60 s |
| 970 nm | 0.2 W | 0.4 W | 12 J/cm2 | 4 Hz | 60 s |
| Test | Patients | Values | Ref. Value |
|---|---|---|---|
| Platelets count | 1 | 253 × 103 /mL | 150–400 |
| 2 | 422 × 103 /mL | 150–450 | |
| Prothrombin time (INR) | 1 | 1.13 | 0.80–1.20 |
| 2 | 1.15 | ||
| Prothrombin time (Sec) | 1 | NA | |
| 2 | 13.8 s | ||
| Prothrombin time (ratio) | 1 | 1.13 | 0.85–1.15 |
| 2 | 1.15 | 0.78–1.20 | |
| Activated partial tomboplastin time (APTT) (sec) | 1 | NA | |
| 2 | 30.8 s | ||
| Activated partial tomboplastin time (APTT) (ratio) | 1 | 1.13 | 0.85–1.15 |
| 2 | 0.96 | 0.76–1.18 | |
| Fibrionogen (Clauss) | 1 | 404 mg/dL | 180–380 |
| 2 | 346 mg/dL | 160–380 | |
| Antithrombin (chromogenic) | 1 | NA | |
| 2 | 91% | 78–124% | |
| Coagulation Factor XIII | 1 | 106% | 70–130% |
| 2 | NA | NA | |
| Von Willebrand antigen | 1 | 128% | Group 0 = 40–140% Group A, B, AB = 65–165% |
| 2 | NA | NA | |
| Von Willebrand activity | 1 | 97% | Group 0 = 40–130% Group A, B, AB = 50–160% |
| 2 | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Celsi, F.; Staffa, P.; Lamba, M.; Castro, V.; Chermetz, M.; Orzan, E.; Sagredini, R.; Barbi, E. Photobiomodulation for Lowering Pain after Tonsillectomy: Low Efficacy and a Possible Unexpected Adverse Effect. Life 2022, 12, 202. https://doi.org/10.3390/life12020202
Celsi F, Staffa P, Lamba M, Castro V, Chermetz M, Orzan E, Sagredini R, Barbi E. Photobiomodulation for Lowering Pain after Tonsillectomy: Low Efficacy and a Possible Unexpected Adverse Effect. Life. 2022; 12(2):202. https://doi.org/10.3390/life12020202
Chicago/Turabian StyleCelsi, Fulvio, Paola Staffa, Martino Lamba, Veronica Castro, Maddalena Chermetz, Eva Orzan, Raffaella Sagredini, and Egidio Barbi. 2022. "Photobiomodulation for Lowering Pain after Tonsillectomy: Low Efficacy and a Possible Unexpected Adverse Effect" Life 12, no. 2: 202. https://doi.org/10.3390/life12020202
APA StyleCelsi, F., Staffa, P., Lamba, M., Castro, V., Chermetz, M., Orzan, E., Sagredini, R., & Barbi, E. (2022). Photobiomodulation for Lowering Pain after Tonsillectomy: Low Efficacy and a Possible Unexpected Adverse Effect. Life, 12(2), 202. https://doi.org/10.3390/life12020202






