The Interplay between Conventional Cardiovascular Risk Factors and Health-Related Quality of Life in a Cohort of Working Young and Middle-Aged Adults: A Prospective Study
Abstract
1. Introduction
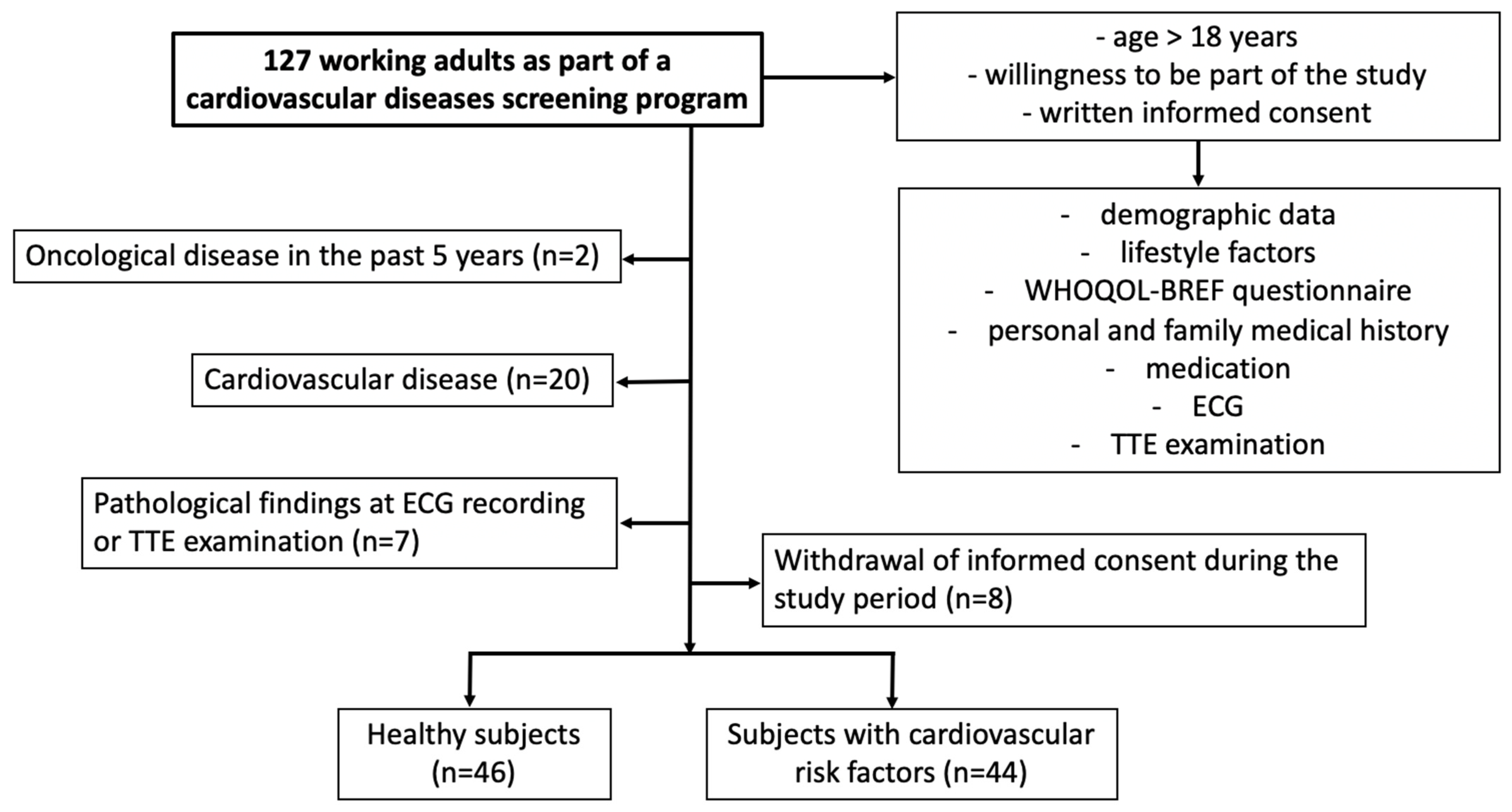
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Transthoracic Echocardiography Acquisition and Analysis
2.4. Health-Related Quality of Life Evaluation
2.5. Medication Adherence Assessment
2.6. Statistical Analysis
3. Results
3.1. Comparison between Subjects with and without Cardiovascular Risk Factors
3.1.1. Clinical and Paraclinical Data
3.1.2. Quality of Life Results
3.2. Associations between Clinical, Paraclinical and QOL Data
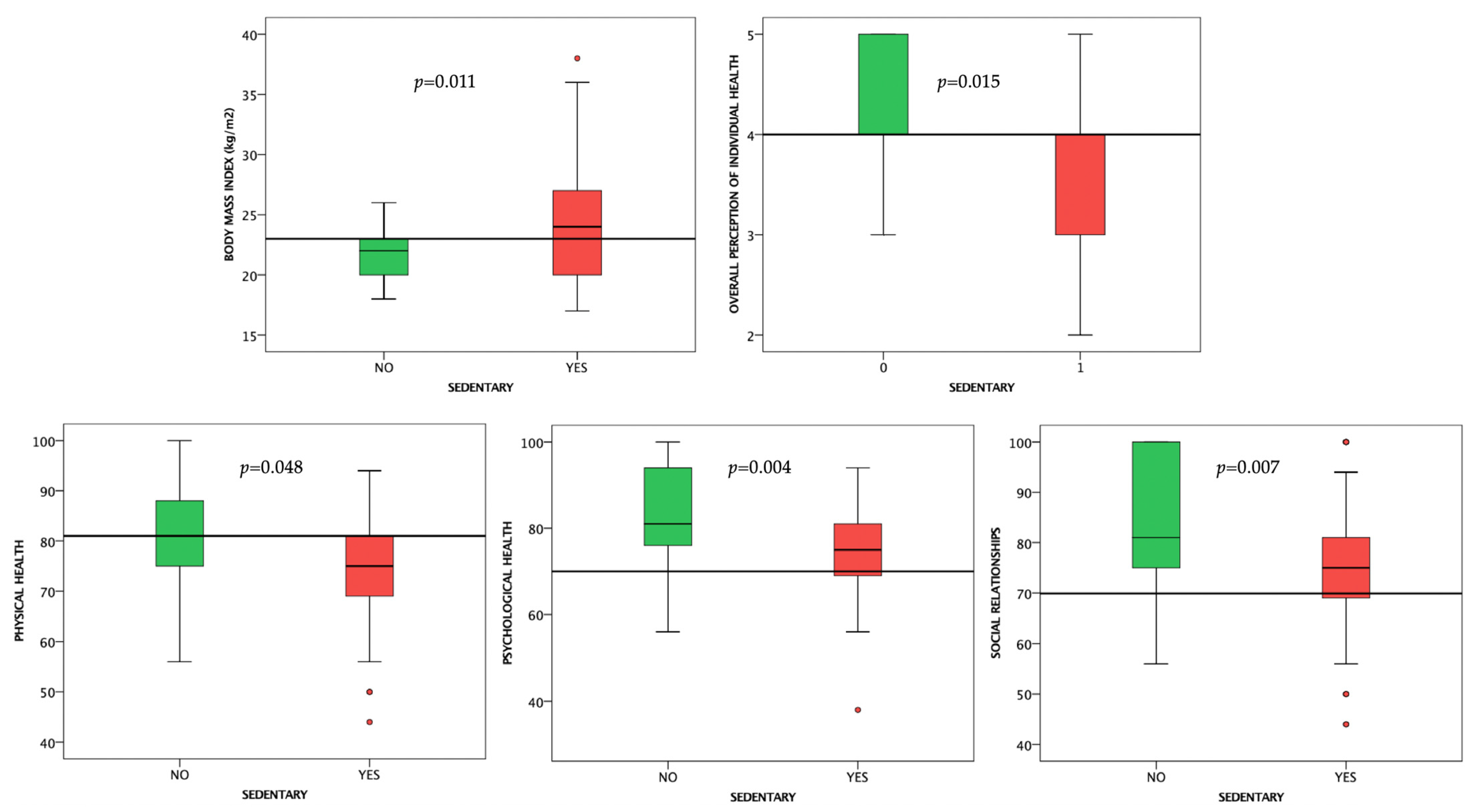
3.2.1. Sedentary Behavior
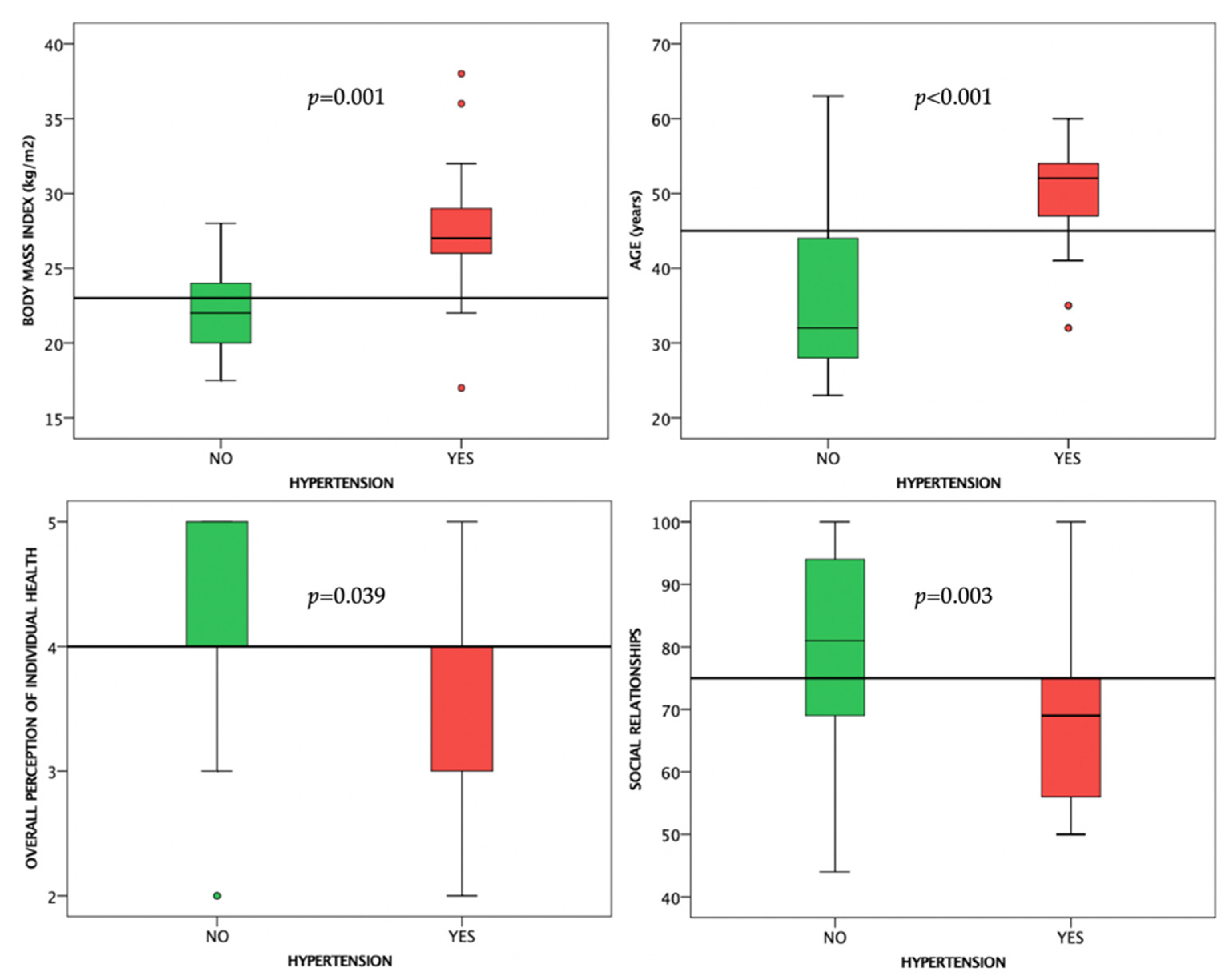
3.2.2. Arterial Hypertension
3.2.3. Type 2 Diabetes Mellitus
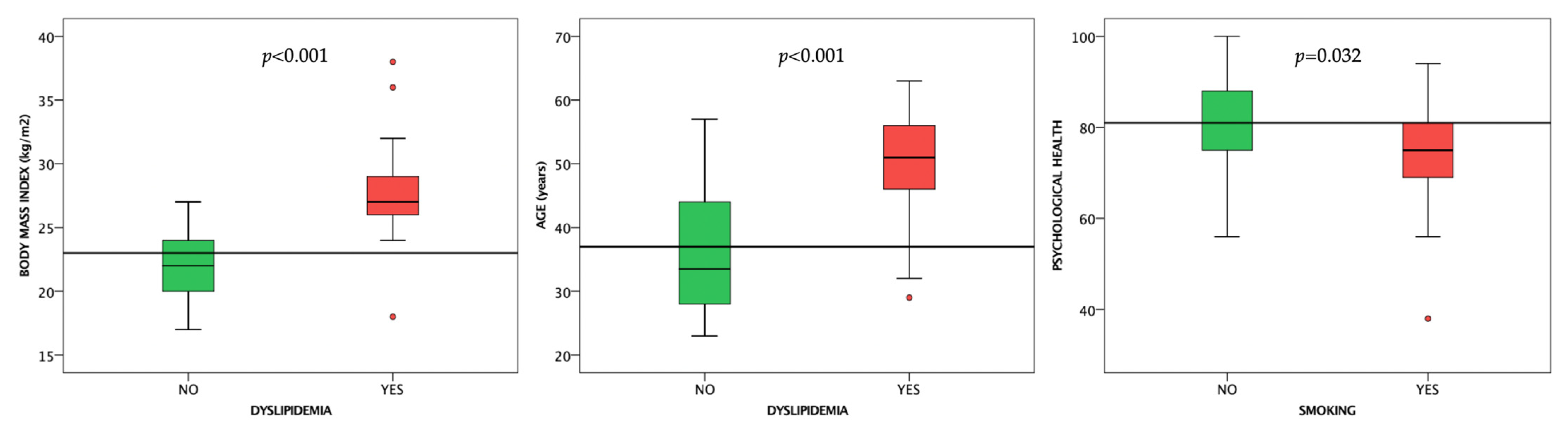
3.2.4. Dyslipidemia
3.2.5. Smoking
3.2.6. Overweight/Obesity
3.2.7. Treatment of Conventional Cardiovascular Risk Factors
3.3. Correlations between WHOQOL-BREF Results and Clinical and Paraclinical Data
3.3.1. WHOQOL-BREF Domains
3.3.2. Age, BMI, and the Presence and Number of Cardiovascular Risk Factors
3.3.3. Sedentary Behavior, Type 2 Diabetes Mellitus, Arterial Hypertension, Dyslipidemia, Smoking
3.3.4. Cardiovascular Medication and Treatment Adherence
3.4. Multiple Regression Analysis of WHOQOL-BREF Domains’ Results
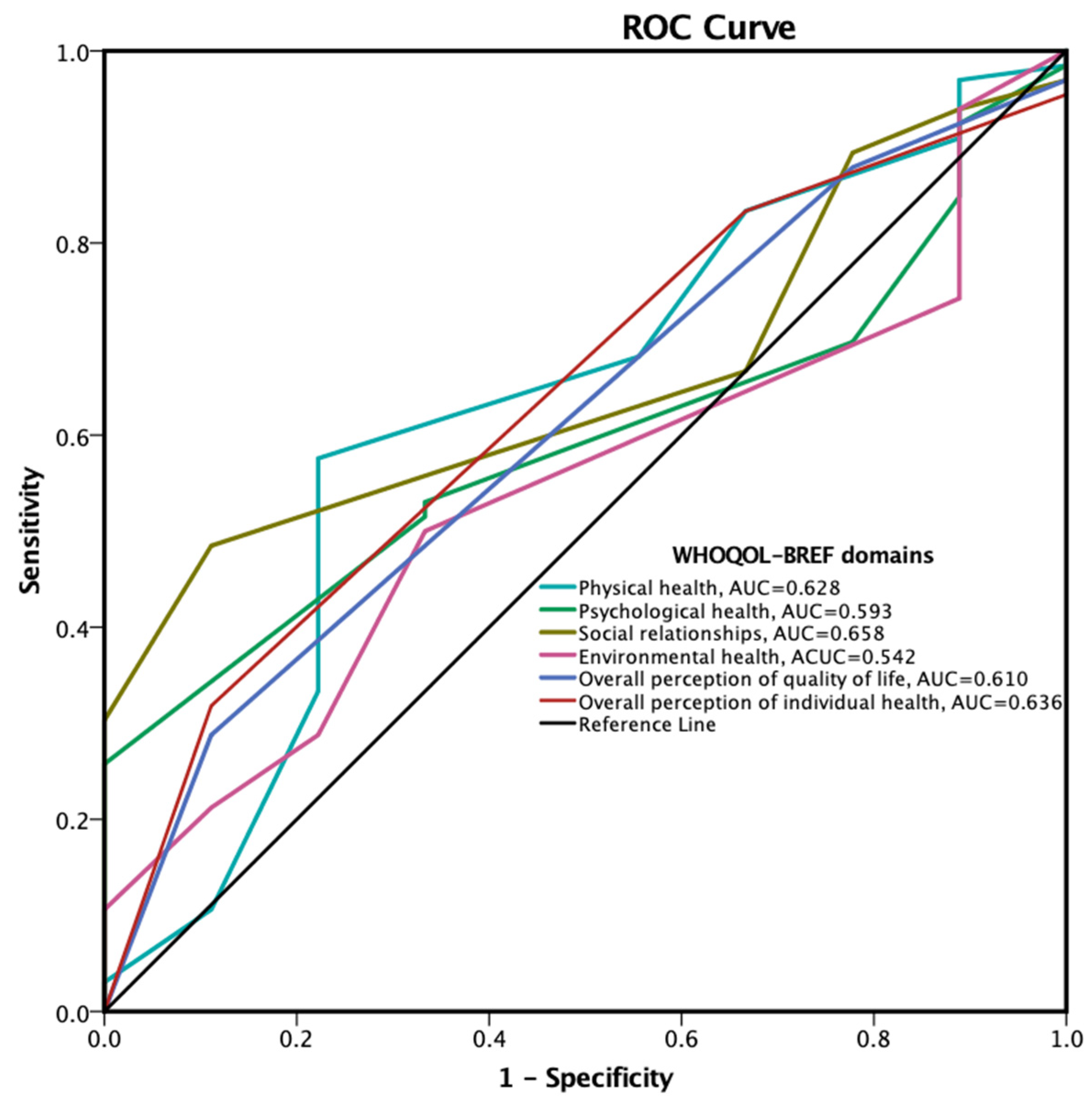
3.5. Treatment Adherence Predictors Based on WHOQOL-BREF Results
4. Discussion
4.1. The Presence and Number of Cardiovascular Risk Factors
4.2. The Need for and the Adherence to Cardiovascular Treatment
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart disease and stroke statistics-2022 update: A report from the American Heart Association. Circulation 2022, 145, E153–E639. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.H.; Eurich, D.T.; Majumdar, S.R.; Padwal, R.S.; Tsuyuki, R.T.; Varney, J.; Johnson, J.A. A Meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006, 333, 15. [Google Scholar] [CrossRef] [PubMed]
- Sabaté, E.; World Health Organization. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003; ISBN 9241545992. [Google Scholar]
- Stringhini, S.; Carmeli, C.; Jokela, M.; Avendaño, M.; Muennig, P.; Guida, F.; Ricceri, F.; D’Errico, A.; Barros, H.; Bochud, M.; et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: A multicohort study and meta-analysis of 1·7 million men and women. Lancet 2017, 389, 1229–1237. [Google Scholar] [CrossRef]
- Franks, P.; Winters, P.C.; Tancredi, D.J.; Fiscella, K.A. Do changes in traditional coronary heart disease risk factors over time explain the association between socio-economic status and coronary heart disease? BMC Cardiovasc. Disord. 2011, 11, 28. [Google Scholar] [CrossRef] [PubMed]
- Osborne, M.T.; Shin, L.M.; Mehta, N.N.; Pitman, R.K.; Fayad, Z.A.; Tawakol, A. Disentangling the links between psychosocial stress and cardiovascular disease. Circ. Cardiovasc. Imaging 2020, 13, E010931. [Google Scholar] [CrossRef]
- Albus, C.; Waller, C.; Fritzsche, K.; Gunold, H.; Haass, M.; Hamann, B.; Kindermann, I.; Köllner, V.; Leithäuser, B.; Marx, N.; et al. Significance of psychosocial factors in cardiology: Update 2018: Position paper of the German cardiac society. Clin. Res. Cardiol. 2019, 108, 1175–1196. [Google Scholar] [CrossRef]
- Kivimäki, M.; Steptoe, A. Effects of stress on the development and progression of cardiovascular disease. Nat. Rev. Cardiol. 2018, 15, 215–229. [Google Scholar] [CrossRef]
- Santosa, A.; Rosengren, A.; Ramasundarahettige, C.; Rangarajan, S.; Chifamba, J.; Lear, S.A.; Poirier, P.; Yeates, K.E.; Yusuf, R.; Orlandini, A.; et al. Psychosocial risk factors and cardiovascular disease and death in a population-based cohort from 21 Low-, Middle-, and High-Income Countries. JAMA Netw. Open 2021, 4, e2138920. [Google Scholar] [CrossRef]
- Chandola, T.; Brunner, E.; Marmot, M. Chronic stress at work and the metabolic syndrome: Prospective study. Br. Med. J. 2006, 332, 521–524. [Google Scholar] [CrossRef]
- Markovitz, J.H.; Matthews, K.A.; Whooley, M.; Lewis, C.E.; Greenlund, K.J. Increases in job strain are associated with incident hypertension in the CARDIA study. Ann. Behav. Med. 2004, 28, 4–9. [Google Scholar] [CrossRef]
- Kumari, M.; Head, J.; Marmot, M. Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II Study. Arch. Intern. Med. 2004, 164, 1873–1880. [Google Scholar] [CrossRef] [PubMed]
- Kearns, N.T.; Carl, E.; Stein, A.T.; Vujanovic, A.A.; Zvolensky, M.J.; Smits, J.A.J.; Powers, M.B. Posttraumatic stress disorder and cigarette smoking: A systematic review. Depress Anxiety 2018, 35, 1056–1072. [Google Scholar] [CrossRef]
- Schultz, W.M.; Kelli, H.M.; Lisko, J.C.; Varghese, T.; Shen, J.; Sandesara, P.; Quyyumi, A.A.; Taylor, H.A.; Gulati, M.; Harold, J.G.; et al. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation 2018, 137, 2166–2178. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; MacH, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Jha, M.K.; Qamar, A.; Vaduganathan, M.; Charney, D.S.; Murrough, J.W. Screening and management of depression in patients with cardiovascular disease: JACC state-of-the-art review. J. Am. Coll Cardiol. 2019, 73, 1827–1845. [Google Scholar] [CrossRef] [PubMed]
- Vaccarino, V.; Badimon, L.; Bremner, J.D.; Cenko, E.; Cubedo, J.; Dorobantu, M.; Duncker, D.J.; Koller, A.; Manfrini, O.; Milicic, D.; et al. Depression and Coronary Heart Disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur. Heart J. 2020, 41, 1687–1696. [Google Scholar] [CrossRef]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO Cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef]
- Nieuwlaat, R.; Wilczynski, N.; Navarro, T.; Hobson, N.; Jeffery, R.; Keepanasseril, A.; Agoritsas, T.; Mistry, N.; Iorio, A.; Jack, S.; et al. Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2014, 11, CD000011. [Google Scholar] [CrossRef]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef]
- World Health Organization. WHO-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment; WHO: Geneva, Switzerland, 1996. [Google Scholar]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1321–1360. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Humbert, M.; Vachiery, J.L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Heart J. 2016, 37, 67–119. [Google Scholar] [CrossRef] [PubMed]
- Lancellotti, P.; Pibarot, P.; Chambers, J.; la Canna, G.; Pepi, M.; Dulgheru, R.; Dweck, M.; Delgado, V.; Garbi, M.; Vannan, M.A.; et al. Multi-modality imaging assessment of native valvular regurgitation: An EACVI and ESC Council of Valvular Heart Disease Position Paper. Eur. Heart J. Cardiovasc. Imaging 2022, 23, E171–E232. [Google Scholar] [CrossRef] [PubMed]
- Haraldstad, K.; Wahl, A.; Andenæs, R.; Andersen, J.R.; Andersen, M.H.; Beisland, E.; Borge, C.R.; Engebretsen, E.; Eisemann, M.; Halvorsrud, L.; et al. A systematic review of quality of life research in medicine and health sciences. Qual. Life Res. 2019, 28, 2641–2650. [Google Scholar] [CrossRef] [PubMed]
- Uchmanowicz, B.; Jankowska, E.A.; Uchmanowicz, I.; Morisky, D.E. Self-reported medication adherence measured with morisky medication adherence scales and its determinants in hypertensive patients aged ≥60 years: A systematic review and meta-analysis. Front. Pharm. 2019, 10, 168. [Google Scholar] [CrossRef] [PubMed]
- Guerra, C.; Conte, E.; del Rio, A.I.; Motta, J.; Moreno Velásquez, I.; Quintana, H.K. Medication adherence in hypertensive individuals in Panama 2019: A national cross-sectional study. Healthcare 2022, 10, 2244. [Google Scholar] [CrossRef]
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; de Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Huculeci, R.; et al. European Society of Cardiology: Cardiovascular disease statistics 2021: Executive summary. Eur. Heart J. Qual Care Clin. Outcomes 2022, 8, 377–382. [Google Scholar] [CrossRef]
- Tzoulaki, I.; Elliott, P.; Kontis, V.; Ezzati, M. Worldwide exposures to cardiovascular risk factors and associated health effects: Current knowledge and data gaps. Circulation 2016, 133, 2314–2333. [Google Scholar] [CrossRef]
- Trevisol, D.J.; Moreira, L.B.; Kerkhoff, A.; Fuchs, S.C.; Fuchs, F.D. Health-related quality of life and hypertension: A systematic review and meta-analysis of observational studies. J. Hypertens 2011, 29, 179–188. [Google Scholar] [CrossRef]
- Mena-Martin, F.J.; Martin-Escudero, J.C.; Simal-Blanco, F.; Carretero-Ares, J.L.; Arzua-Mouronte, D.; Herreros-Fernandez, V. Health-related quality of life of subjects with known and unknown hypertension: Results from the population-based Hortega Study. J. Hypertens 2003, 21, 1283–1289. [Google Scholar] [CrossRef]
- Hayes, D.K.; Denny, C.H.; Keenan, N.L.; Croft, J.B.; Greenlund, K.J. Health-related quality of life and hypertension status, awareness, treatment, and control: National health andnutrition examination survey, 2001–2004. J. Hypertens 2008, 26, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, K.R.; Barofsky, I. Obesity and health-related quality of life. Obes. Rev. 2001, 2, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Smith, C.M.; Kearns, B.; Haywood, A.; Bissell, P. The association between obesity and quality of life: A retrospective analysis of a large-scale population-based cohort study. BMC Public Health 2021, 21, 1990. [Google Scholar] [CrossRef]
- Busutil, R.; Espallardo, O.; Torres, A.; Martínez-Galdeano, L.; Zozaya, N.; Hidalgo-Vega, Á. The impact of obesity on health-related quality of life in Spain. Health Qual Life Outcomes 2017, 15, 197. [Google Scholar] [CrossRef]
- Marcos-Delgado, A.; Fernández-Villa, T.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Castañer, O.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; Vioque, J.; et al. The effect of physical activity and high body mass index on health-related quality of life in individuals with metabolic syndrome. Int J. Env. Res Public Health 2020, 17, 3728. [Google Scholar] [CrossRef]
- Sayón-Orea, C.; Santiago, S.; Bes-Rastrollo, M.; Martínez-González, M.A.; Pastor, M.R.; Moreno-Aliaga, M.J.; Tur, J.A.; Garcia, A.; Martínez, J.A. Determinants of self-rated health perception in a sample of a physically active population: PLENUFAR VI study. Int J. Env. Res Public Health 2018, 15, 2104. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, L.M.B.; Mizutani, B.M.; Mutti, A.; D’elia, M.P.B.; Coltro, R.S.; Matsubara, B.B. Quality of life and its association with cardiovascular risk factors in a community health care program population. Clinics 2008, 63, 783–788. [Google Scholar] [CrossRef]
- Hayiroǧlu, M.I.; Çinar, T.; Çinier, G.; Karakaya, A.; Yildirim, M.; Güney, B.Ç.; Öz, A.; Gündogmus, P.D.; Ösken, A.; Özkan, A.; et al. The effect of 1-year mean step count on the change in the atherosclerotic cardiovascular disease risk calculation in patients with high cardiovascular risk: A sub-study of the LIGHT randomized clinical Trial. Kardiol. Pol. 2021, 79, 1140–1142. [Google Scholar] [CrossRef]
- Hummer, R.A.; Lariscy, J.T. Educational attainment and adult mortality. In International Handbook of Adult Mortality; Rogers, R.G., Crimmins, E.M., Eds.; Springer: Dordrecht, The Netherlands, 2011; pp. 241–261. ISBN 978-90-481-9996-9. [Google Scholar]
- Zajacova, A.; Lawrence, E.M. The relationship between education and health: Reducing disparities through a contextual approach. Annu. Rev. Public Health 2018, 39, 273–289. [Google Scholar] [CrossRef]
- Van Wilder, L.; Devleesschauwer, B.; Clays, E.; Pype, P.; Vandepitte, S.; de Smedt, D. Polypharmacy and health-related quality of life/psychological distress among patients with chronic disease. Prev. Chronic. Dis. 2022, 19, 220062. [Google Scholar] [CrossRef]
- Vyas, A.; Kang, F.; Barbour, M. Association between polypharmacy and health-related quality of life among US adults with cardiometabolic risk factors. Qual. Life Res. 2020, 29, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Eghbali, M.; Akbari, M.; Seify, K.; Fakhrolmobasheri, M.; Heidarpour, M.; Roohafza, H.; Afzali, M.; Mostafavi-Esfahani, F.S.; Karimian, P.; Sepehr, A.; et al. Evaluation of psychological distress, self-care, and medication adherence in association with hypertension control. Int. J. Hypertens. 2022, 2022, 7802792. [Google Scholar] [CrossRef] [PubMed]
- Pareja-Martínez, E.; Esquivel-Prados, E.; Martínez-Martínez, F.; García-Corpas, J.P. Questionnaires on adherence to antihypertensive treatment: A systematic review of published questionnaires and their psychometric properties. Int. J. Clin. Pharm. 2020, 42, 355–365. [Google Scholar] [CrossRef] [PubMed]


| Parameter | All Subjects (n = 90) | Healthy Subjects (n = 46) | Subjects with Cardiovascular Risk Factors (n = 44) | p Value |
|---|---|---|---|---|
| Age (years) | 42 [29–50] | 37 [28.5–48.5] | 45.5 [28.75–52.25] | 0.245 |
| Men (%) | 33 (44) | 21 (45.7) | 19 (45.2) | 0.713 |
| Body-mass index (kg/m2) | 23 [20–25.5] | 22 [20–23.75] | 25.5 [20–27] | <0.001 |
| Sedentary (%) | 46 (51.1%) | 12 (26.1%) | 34 (77.3%) | 0.001 |
| Heart rate (bpm) | 70 [65–80] | 70 [65–77.5] | 70 [65.75–78.25] | 0.923 |
| Systolic blood pressure (mmHg) | 115 [110–120] | 120 [110–120] | 110 [110–125] | 0.1 |
| Diastolic blood pressure (mmHg) | 60 [55–70] | 67.5 [60–70] | 65 [60–70] | 0.680 |
| Sinus rhythm (%) | 90 (100%) | 46 (100%) | 44 (100%) | 0.989 |
| Biplane LVEF (%) | 58 [55–60] | 58 [55–60] | 57 [55–59] | 0.997 |
| M-mode RV TAPSE (mm) | 21 [18–25] | 21 [19–25] | 21 [19–24] | 0.999 |
| TDI S’ wave velocity (cm/s) | 13 [10–15] | 13 [10–16] | 12 [9–14] | 0.998 |
| E/A ratio | 1.5 [1.1–1.7] | 1.6 [1.1–1.9] | 1.4 [1.1–1.6] | 0.879 |
| Average E/e’ ratio | 6 [4–7] | 5 [4–7] | 6 [4–7] | 0.991 |
| sPAP (mmHg) | 16 [15–22] | 17 [14–21] | 19 [17–22] | 0.993 |
| WHOQOL-BREF Domain | All Subjects (n = 90) | Healthy Subjects (n = 46) | Subjects with Cardiovascular Risk Factors (n = 44) | p Value |
|---|---|---|---|---|
| Physical health | 81 [69–88] | 81 [72–88] | 75 [63–88] | 0.640 |
| Psychological health | 81 [69–88] | 81 [75–94] | 75 [69–84] | 0.021 |
| Social relationships | 75 [69–94] | 81 [69–100] | 75 [69–84] | 0.007 |
| Environmental health | 75 [64–81] | 75 [69–84.5] | 69 [63–83] | 0.497 |
| Overall perception of quality of life | 0.240 | |||
| Very poor | 0 (0%) | 0 (0%) | 0 (0%) | |
| Poor | 3 (3.3%) | 0 (0%) | 3 (6.8%) | |
| Neither poor nor good | 10 (11.1%) | 2 (4.3%) | 8 (16.7%) | |
| Good | 50 (55.5%) | 27 (58.7%) | 23 (54.8%) | |
| Very good | 27 (31.1%) | 17 (37%) | 10 (23.8%) | |
| Overall satisfaction with own health | 0.002 | |||
| Very dissatisfied | 0 (0%) | 0 (0%) | 0 (0%) | |
| Dissatisfied | 3 (3.3%) | 0 (0%) | 3 (6.8%) | |
| Neither satisfied nor dissatisfied | 12 (13.3%) | 1 (2.2%) | 11 (25%) | |
| Satisfied | 43 (47.8%) | 22 (47.8%) | 21 (47.7%) | |
| Very satisfied | 32 (35.6%) | 23 (50%) | 9 (20.5%) | |
| WHOQOL-BREF Domain | Physical Health | Psychological Health | Social Relationships | Environmental Health | Overall QoL | Overall Health |
|---|---|---|---|---|---|---|
| Physical health | r = 0.396 | r = 0.228 | r = 0.178 | r = 0.346 | r = 0.435 | |
| p < 0.001 | p = 0.006 | p < 0.001 | p < 0.001 | p < 0.001 | ||
| Psychological health | r = 0.396 | r = 0.435 | r = 0.380 | r = 0.459 | r = 0.489 | |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | ||
| Social relationships | r = 0.228 | r = 0.435 | r = 0.312 | r = 0.399 | r = 0.357 | |
| p = 0.006 | p < 0.001 | p < 0.001 | p < 0.001 | p = 0.001 | ||
| Environmental health | r = 0.178 | r = 0.380 | r = 0.312 | r = 0.350 | r = 0.273 | |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p = 0.002 | ||
| Overall QoL | r = 0.346 | r = 0.459 | r = 0.399 | r = 0.350 | r = 0.398 | |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | ||
| Overall health | r = 0.435 | r = 0.489 | r = 0.357 | r = 0.273 | r = 0.398 | |
| p < 0.001 | p < 0.001 | p = 0.001 | p = 0.002 | p < 0.001 |
| Dependent Variable | Independent Variable | R2 | Beta | p |
|---|---|---|---|---|
| Physical health | Psychological health | 0.328 | 0.572 | <0.001 |
| Social relationships | 0.100 | 0.317 | 0.003 | |
| Environmental health | 0.063 | 0.252 | 0.019 | |
| Overall perception of quality of life | 0.235 | 0.485 | <0.001 | |
| Overall perception of individual health | 0.293 | 0.541 | <0.001 | |
| Psychological health | Social relationships | 0.281 | 0.530 | <0.001 |
| Environmental health | 0.240 | 0.489 | <0.001 | |
| Overall perception of quality of life | 0.327 | 0.571 | <0.001 | |
| Overall perception of individual health | 0.345 | 0.594 | <0.001 | |
| Social relationships | Environmental health | 0.148 | 0.384 | <0.001 |
| Overall perception of quality of life | 0.156 | 0.395 | <0.001 | |
| Overall perception of individual health | 0.175 | 0.418 | <0.001 | |
| Environmental health | Overall perception of quality of life | 0.156 | 0.395 | <0.001 |
| Overall perception of individual health | 0.106 | 0.326 | 0.002 | |
| Overall perception of quality of life | Overall perception of individual health | 0.244 | 0.493 | <0.001 |
| Dependent Variable | Independent Variables | Beta | p |
|---|---|---|---|
| Physical health | Number of drugs | −0.414 | 0.022 |
| Psychological health | 0.134 | 0.004 | |
| Overall perception of individual health | 0.333 | 0.013 | |
| Psychological health | Age | 0.225 | 0.048 |
| Social relationships | 0.270 | 0.009 | |
| Physical health | 0.339 | 0.004 | |
| Social relationships | Psychological health | 0.430 | 0.009 |
| Environmental health | >0.05 for all | ||
| Overall perception of quality of life | >0.05 for all | ||
| Overall perception of individual health | Presence of cardiovascular risk factors | −0.595 | 0.002 |
| Number of cardiovascular risk factors | 0.802 | 0.041 | |
| Type 2 Diabetes Mellitus | −0.349 | 0.010 | |
| Arterial hypertension | −0.442 | 0.042 | |
| Physical health | 0.316 | 0.013 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Florescu, C.; Ciobanu, P.; Hădăreanu, D.R.; Gheorman, V.; Mustafa, E.R.; Glodeanu, A.D.; Bunescu, M.G.; Mită, A.; Dinescu, V.C. The Interplay between Conventional Cardiovascular Risk Factors and Health-Related Quality of Life in a Cohort of Working Young and Middle-Aged Adults: A Prospective Study. Life 2022, 12, 2132. https://doi.org/10.3390/life12122132
Florescu C, Ciobanu P, Hădăreanu DR, Gheorman V, Mustafa ER, Glodeanu AD, Bunescu MG, Mită A, Dinescu VC. The Interplay between Conventional Cardiovascular Risk Factors and Health-Related Quality of Life in a Cohort of Working Young and Middle-Aged Adults: A Prospective Study. Life. 2022; 12(12):2132. https://doi.org/10.3390/life12122132
Chicago/Turabian StyleFlorescu, Cristina, Petre Ciobanu, Diana Ruxandra Hădăreanu, Veronica Gheorman, Edme Roxana Mustafa, Adina Dorina Glodeanu, Marius Gabriel Bunescu, Adrian Mită, and Venera Cristina Dinescu. 2022. "The Interplay between Conventional Cardiovascular Risk Factors and Health-Related Quality of Life in a Cohort of Working Young and Middle-Aged Adults: A Prospective Study" Life 12, no. 12: 2132. https://doi.org/10.3390/life12122132
APA StyleFlorescu, C., Ciobanu, P., Hădăreanu, D. R., Gheorman, V., Mustafa, E. R., Glodeanu, A. D., Bunescu, M. G., Mită, A., & Dinescu, V. C. (2022). The Interplay between Conventional Cardiovascular Risk Factors and Health-Related Quality of Life in a Cohort of Working Young and Middle-Aged Adults: A Prospective Study. Life, 12(12), 2132. https://doi.org/10.3390/life12122132








