Helicobacter Pylori: A Review of Current Treatment Options in Clinical Practice
Abstract
:1. Introduction
2. Materials and Methods
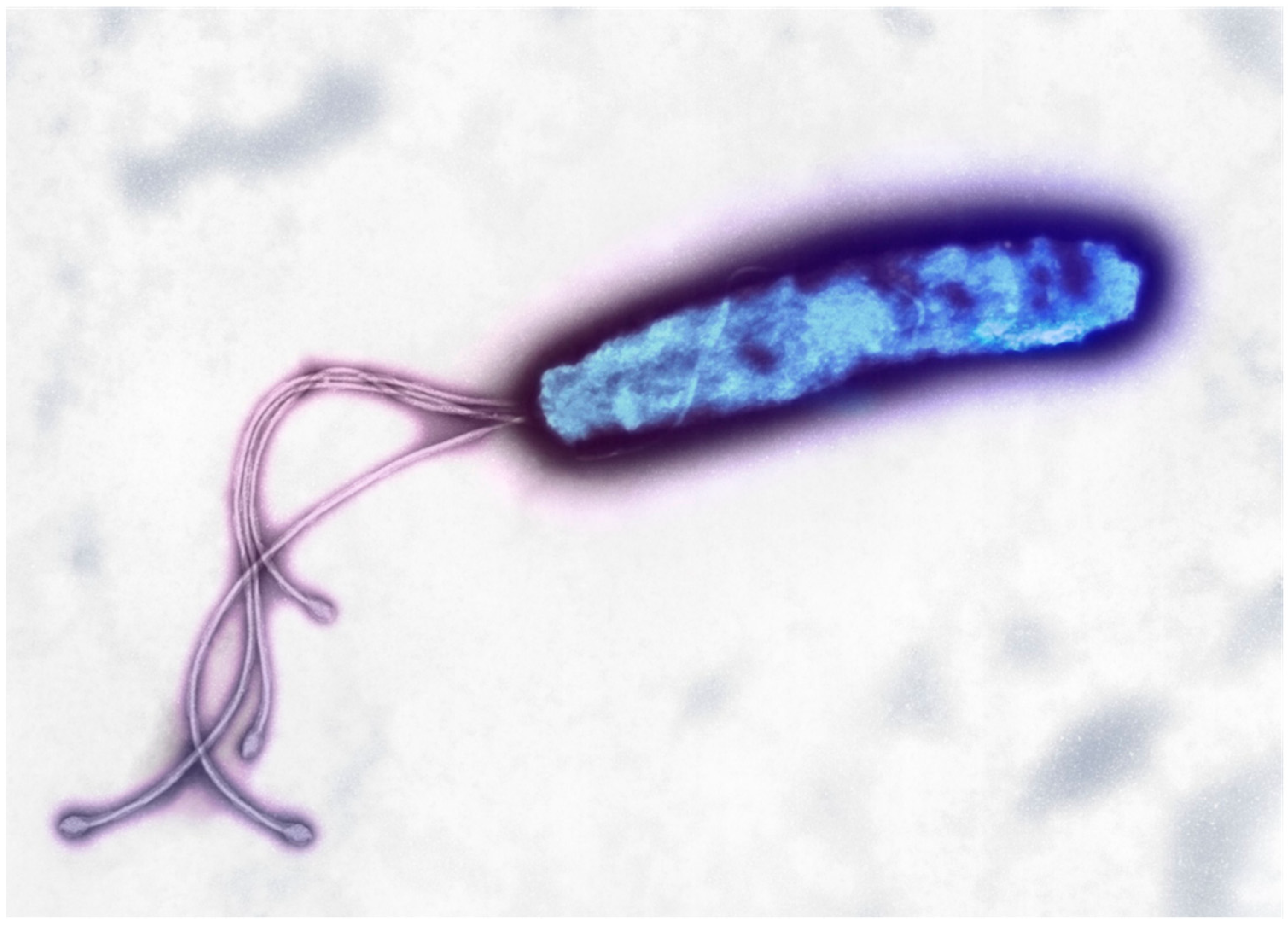
3. H. pylori Overview
4. Etiology, Epidemiology, Pathophysiology
5. Antibiotics Overview
5.1. Clarithromycin
5.2. Amoxicillin
5.3. Bismuth Subsalicylate
5.4. Metronidazole
5.5. Tetracycline/Doxycycline
5.6. Levofloxacin
6. Acid Suppressants Overview
6.1. Proton Pump Inhibitors (PPIs)
6.2. Vonoprazan
7. First-Line Therapies
7.1. Bismuth Quadruple Therapy
7.2. Clarithromycin Triple Therapy
7.3. Concomitant Therapy
7.4. Sequential Therapy
7.5. Hybrid Therapy
8. Common Substitutions and Cautions
8.1. Penicillin Allergy
8.2. Alternatives to Clarithromycin
8.3. Metronidazole and Alcohol Use
8.4. Tetracyclines and Pregnancy
8.5. Follow Up Eradication Confirmation
9. Second-Line Agents for Treatment Failure
9.1. Suggested Approach
9.2. Bismuth Quadruple Therapy
9.3. Levofloxacin-Based Therapy
9.4. High-Dose Dual Therapy
9.5. Rifabutin Triple Therapy
9.6. Clarithromycin-Based therapy
9.7. Factors Associated with Treatment Failure
9.8. Probiotics
10. Cost Considerations
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guevara, B.; Cogdill, A.G. Helicobacter pylori: A Review of Current Diagnostic and Management Strategies. Dig. Dis. Sci. 2020, 65, 1917–1931. [Google Scholar] [CrossRef]
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y.; et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef] [Green Version]
- Kotilea, K.; Bontems, P.; Touati, E. Epidemiology, Diagnosis and Risk Factors of Helicobacter pylori Infection. In Helicobacter pylori in Human Diseases: Advances in Microbiology, Infectious Diseases and Public Health Volume 11; Kamiya, S., Backert, S., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2019; pp. 17–33. ISBN 978-3-030-21916-1. [Google Scholar]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of Antibiotic Resistance in Helicobacter pylori: A Systematic Review and Meta-Analysis in World Health Organization Regions. Gastroenterology 2018, 155, 1372–1382.e17. [Google Scholar] [CrossRef] [Green Version]
- Chey, W.D.; Leontiadis, G.I.; Howden, C.W.; Moss, S.F. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 2017, 112, 212–239. [Google Scholar] [CrossRef]
- Garza-González, E.; Perez-Perez, G.I.; Maldonado-Garza, H.J.; Bosques-Padilla, F.J. A Review of Helicobacter pylori Diagnosis, Treatment, and Methods to Detect Eradication. World J. Gastroenterol. 2014, 20, 1438–1449. [Google Scholar] [CrossRef]
- Moayyedi, P. The Health Economics of Helicobacter pylori Infection. Best Pract. Res. Clin. Gastroenterol. 2007, 21, 347–361. [Google Scholar] [CrossRef]
- Best, L.M.; Takwoingi, Y.; Siddique, S.; Selladurai, A.; Gandhi, A.; Low, B.; Yaghoobi, M.; Gurusamy, K.S. Non-Invasive Diagnostic Tests for Helicobacter pylori Infection. Cochrane Database Syst. Rev. 2018, 3, CD012080. [Google Scholar] [CrossRef] [Green Version]
- Renewed Interest in the Management of Helicobacter pylori Infection. Supplements and Featured Publications. 2021. Available online: https://www.ajmc.com/view/renewed-interest-in-the-management-of-helicobacter-pylori-infection (accessed on 11 August 2022).
- Öztekin, M.; Yılmaz, B.; Ağagündüz, D.; Capasso, R. Overview of Helicobacter pylori Infection: Clinical Features, Treatment, and Nutritional Aspects. Diseases 2021, 9, 66. [Google Scholar] [CrossRef]
- Geng, W.; Wang, L.; Jiang, N.; Cao, J.; Xiao, Y.-X.; Wei, H.; Yetisen, A.K.; Yang, X.-Y.; Su, B.-L. Single Cells in Nanoshells for the Functionalization of Living Cells. Nanoscale 2018, 10, 3112–3129. [Google Scholar] [CrossRef]
- Fan, G.; Wasuwanich, P.; Rodriguez-Otero, M.R.; Furst, A.L. Protection of Anaerobic Microbes from Processing Stressors Using Metal–Phenolic Networks. J. Am. Chem. Soc. 2022, 144, 2438–2443. [Google Scholar] [CrossRef]
- Geng, W.; Jiang, N.; Qing, G.-Y.; Liu, X.; Wang, L.; Busscher, H.J.; Tian, G.; Sun, T.; Wang, L.-Y.; Montelongo, Y.; et al. Click Reaction for Reversible Encapsulation of Single Yeast Cells. ACS Nano 2019, 13, 14459–14467. [Google Scholar] [CrossRef]
- Parikh, N.S.; Ahlawat, R. Helicobacter pylori; StatPearls Publishing: Tampa, FL, USA, 2022. [Google Scholar]
- Zuckerman, J.M.; Qamar, F.; Bono, B.R. Review of Macrolides (Azithromycin, Clarithromycin), Ketolids (Telithromycin) and Glycylcyclines (Tigecycline). Med. Clin. N. Am. 2011, 95, 761–791, viii. [Google Scholar] [CrossRef]
- Sturgill, M.G.; Rapp, R.P. Clarithromycin: Review of a New Macrolide Antibiotic with Improved Microbiologic Spectrum and Favorable Pharmacokinetic and Adverse Effect Profiles. Ann. Pharmacother. 1992, 26, 1099–1108. [Google Scholar] [CrossRef]
- Khademi, F.; Faghri, J.; Moghim, S.; Esfahani, B.N.; Fazeli, H.; Poursina, F.; Adibi, P.; Madhi, M.; Safaei, H.G. The Study of Mutation in 23S RRNA Resistance Gene of Helicobacter pylori to Clarithromycin in Patients with Gastrointestinal Disorders in Isfahan—Iran. Adv. Biomed. Res 2014, 3, 98. [Google Scholar] [CrossRef]
- Yakoob, J.; Jafri, W.; Abbas, Z.; Abid, S.; Naz, S.; Khan, R.; Khalid, A. Risk Factors Associated with Helicobacter pylori Infection Treatment Failure in a High Prevalence Area. Epidemiol. Infect 2011, 139, 581–590. [Google Scholar] [CrossRef] [Green Version]
- Peterson, W.L.; Graham, D.Y.; Marshall, B.; Blaser, M.J.; Genta, R.M.; Klein, P.D.; Stratton, C.W.; Drnec, J.; Prokocimer, P.; Siepman, N. Clarithromycin as Monotherapy for Eradication of Helicobacter pylori: A Randomized, Double-Blind Trial. Am. J. Gastroenterol 1993, 88, 1860–1864. [Google Scholar] [PubMed]
- Wood, M.J. The Tolerance and Toxicity of Clarithromycin. J. Hosp. Infect 1991, 19 (Suppl. A), 39–46. [Google Scholar] [CrossRef]
- Gribble, M.J.; Chow, A.W. Erythromycin. Med. Clin. N. Am. 1982, 66, 79–89. [Google Scholar] [CrossRef]
- Alfaresi, M.S.; Elkoush, A.A. Characterization of Clarithromycin Resistance in Isolates of Helicobacter pylori from the UAE. Indian J. Gastroenterol. 2010, 29, 116–120. [Google Scholar] [CrossRef]
- Graham, D.Y.; Fischbach, L. Helicobacter pylori Treatment in the Era of Increasing Antibiotic Resistance. Gut 2010, 59, 1143–1153. [Google Scholar] [CrossRef]
- Kaneko, F.; Suzuki, H.; Hasegawa, N.; Kurabayshi, K.; Saito, H.; Otani, S.; Nakamizo, H.; Kawata, K.; Miyairi, M.; Ishii, K.; et al. High Prevalence Rate of Helicobacter pylori Resistance to Clarithromycin during Long-Term Multiple Antibiotic Therapy for Chronic Respiratory Disease Caused by Non-Tuberculous Mycobacteria. Aliment Pharmacol. Ther 2004, 20 (Suppl. S1), 62–67. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, T.; Suzuki, H. Mechanisms of Helicobacter pylori Antibiotic Resistance and Molecular Testing. Front. Mol. Biosci. 2014, 1, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, D.E. Pathophysiology of Antibiotic Resistance: Clarithromycin. Can. J. Gastroenterol. 2000, 14, 891–894. [Google Scholar] [CrossRef] [Green Version]
- Geddes, A.M.; Klugman, K.P.; Rolinson, G.N. Introduction: Historical Perspective and Development of Amoxicillin/Clavulanate. Int. J. Antimicrob. Agents 2007, 30 (Suppl. S2), S109–S112. [Google Scholar] [CrossRef]
- Aronoff, S.C.; Jacobs, M.R.; Johenning, S.; Yamabe, S. Comparative Activities of the Beta-Lactamase Inhibitors YTR 830, Sodium Clavulanate, and Sulbactam Combined with Amoxicillin or Ampicillin. Antimicrob. Agents Chemother. 1984, 26, 580–582. [Google Scholar] [CrossRef] [Green Version]
- Carcione, D.; Siracusa, C.; Sulejmani, A.; Leoni, V.; Intra, J. Old and New Beta-Lactamase Inhibitors: Molecular Structure, Mechanism of Action, and Clinical Use. Antibiotics 2021, 10, 995. [Google Scholar] [CrossRef]
- Salvo, F.; De Sarro, A.; Caputi, A.P.; Polimeni, G. Amoxicillin and Amoxicillin plus Clavulanate: A Safety Review. Expert. Opin. Drug. Saf. 2009, 8, 111–118. [Google Scholar] [CrossRef]
- Amoxicillin: A Broad Spectrum Antibiotic. Available online: https://www.researchgate.net/publication/304704877_Amoxicillin_A_Broad_Spectrum_Antibiotic (accessed on 22 November 2022).
- Bernatová, S.; Samek, O.; Pilát, Z.; Serý, M.; Ježek, J.; Jákl, P.; Siler, M.; Krzyžánek, V.; Zemánek, P.; Holá, V.; et al. Following the Mechanisms of Bacteriostatic versus Bactericidal Action Using Raman Spectroscopy. Molecules 2013, 18, 13188–13199. [Google Scholar] [CrossRef]
- Kowalska-Krochmal, B.; Dudek-Wicher, R. The Minimum Inhibitory Concentration of Antibiotics: Methods, Interpretation, Clinical Relevance. Pathogens 2021, 10, 165. [Google Scholar] [CrossRef]
- Pejcic, A.V.; Milosavljevic, M.N.; Folic, M.; Fernandes, D.; Bentes, J.; Djesevic, M.; Jankovic, S. Amoxicillin-Associated Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis: Systematic Review. J. Chemother. 2022, 1–12. [Google Scholar] [CrossRef]
- Akhavan, B.J.; Khanna, N.R.; Vijhani, P. Amoxicillin. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Madisch, A.; Morgner, A.; Stolte, M.; Miehlke, S. Investigational Treatment Options in Microscopic Colitis. Expert. Opin. Investig. Drugs 2008, 17, 1829–1837. [Google Scholar] [CrossRef]
- Bierer, D.W. Bismuth Subsalicylate: History, Chemistry, and Safety. Rev. Infect. Dis 1990, 12 (Suppl. S1), S3–S8. [Google Scholar] [CrossRef]
- Pitz, A.M.; Park, G.W.; Lee, D.; Boissy, Y.L.; Vinjé, J. Antimicrobial Activity of Bismuth Subsalicylate on Clostridium Difficile, Escherichia Coli O157:H7, Norovirus, and Other Common Enteric Pathogens. Gut Microbes 2015, 6, 93–100. [Google Scholar] [CrossRef] [Green Version]
- Sheele, J.; Cartowski, J.; Dart, A.; Poddar, A.; Gupta, S.; Stashko, E.; Ravi, B.S.; Nelson, C.; Gupta, A. Saccharomyces Boulardii and Bismuth Subsalicylate as Low-Cost Interventions to Reduce the Duration and Severity of Cholera. Pathog. Glob. Health 2015, 109, 275–282. [Google Scholar] [CrossRef] [Green Version]
- Vilaichone, R.; Prapitpaiboon, H.; Gamnarai, P.; Namtanee, J.; Wongcha-um, A.; Chaithongrat, S.; Mahachai, V. Seven-Day Bismuth-Based Quadruple Therapy as an Initial Treatment for Helicobacter pylori Infection in a High Metronidazole Resistant Area. Asian Pac. J. Cancer Prev. 2015, 16, 6089–6092. [Google Scholar] [CrossRef] [Green Version]
- Sainsbury, S.J. Fatal Salicylate Toxicity from Bismuth Subsalicylate. West. J. Med. 1991, 155, 637–639. [Google Scholar]
- Borbinha, C.; Serrazina, F.; Salavisa, M.; Viana-Baptista, M. Bismuth Encephalopathy—A Rare Complication of Long-Standing Use of Bismuth Subsalicylate. BMC Neurol. 2019, 19, 212. [Google Scholar] [CrossRef] [Green Version]
- Budisak, P.; Abbas, M. Bismuth Subsalicylate. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Rao, G.; Aliwalas, M.G.; Slaymaker, E.; Brown, B. Bismuth Revisited: An Effective Way to Prevent Travelers’ Diarrhea. J. Travel. Med 2004, 11, 239–241. [Google Scholar] [CrossRef] [Green Version]
- Freeman, C.D.; Klutman, N.E.; Lamp, K.C. Metronidazole. A Therapeutic Review and Update. Drugs 1997, 54, 679–708. [Google Scholar] [CrossRef]
- Müller, M. Mode of Action of Metronidazole on Anaerobic Bacteria and Protozoa. Surgery 1983, 93, 165–171. [Google Scholar]
- Hernández Ceruelos, A.; Romero-Quezada, L.C.; Ruvalcaba Ledezma, J.C.; López Contreras, L. Therapeutic Uses of Metronidazole and Its Side Effects: An Update. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 397–401. [Google Scholar] [CrossRef]
- Kurian, M.; Ganapathy, D.; Jain, A.R. Recent Advances of Metronidazole-A Review. Drug Invent. Today 2018, 10, 3536–3541. [Google Scholar]
- Mergenhagen, K.A.; Wattengel, B.A.; Skelly, M.K.; Clark, C.M.; Russo, T.A. Fact versus Fiction: A Review of the Evidence behind Alcohol and Antibiotic Interactions. Antimicrob. Agents Chemother. 2020, 64, e02167-19. [Google Scholar] [CrossRef]
- Gauthier-Lewis, M.; Riley, T.T. Miscellaneous Antimicrobials. Clinical Drug Data; McGraw Hill: New York, NY, USA, 2010; p. 271. [Google Scholar]
- Roberts, M.C. Tetracycline Resistance Determinants: Mechanisms of Action, Regulation of Expression, Genetic Mobility, and Distribution. FEMS Microbiol. Rev. 1996, 19, 1–24. [Google Scholar] [CrossRef]
- Katiyar, S.K.; Edlind, T.D. Enhanced Antiparasitic Activity of Lipophilic Tetracyclines: Role of Uptake. Antimicrob. Agents Chemother. 1991, 35, 2198–2202. [Google Scholar] [CrossRef] [Green Version]
- Speer, B.S.; Shoemaker, N.B.; Salyers, A.A. Bacterial Resistance to Tetracycline: Mechanisms, Transfer, and Clinical Significance. Clin. Microbiol. Rev. 1992, 5, 387–399. [Google Scholar] [CrossRef]
- Chopra, I.; Roberts, M. Tetracycline Antibiotics: Mode of Action, Applications, Molecular Biology, and Epidemiology of Bacterial Resistance. Microbiol. Mol. Biol. Rev. 2001, 65, 232–260. [Google Scholar] [CrossRef] [Green Version]
- R Factors: Infectious Multiple Drug Resistance. S. Falkow. Pion, London, 1975 (Distributor, Academic Press, New York). Xiv, 300 pp. + Plates. $19.95. Pion Advanced Biochemistry Series, 4. | Science. Available online: https://www.science.org/doi/10.1126/science.192.4241.778.a (accessed on 22 November 2022).
- Eliopoulos, G.M.; Eliopoulos, G.M.; Roberts, M.C. Tetracycline Therapy: Update. Clin. Infect. Dis. 2003, 36, 462–467. [Google Scholar] [CrossRef] [Green Version]
- Anderson, V.R.; Perry, C.M. Levofloxacin. Drugs 2008, 68, 535–565. [Google Scholar] [CrossRef]
- Hooper, D.C. Mode of Action of Fluoroquinolones. Drugs 1999, 58 (Suppl. S2), 6–10. [Google Scholar] [CrossRef] [PubMed]
- Tanne, J.H. FDA Adds “Black Box” Warning Label to Fluoroquinolone Antibiotics. BMJ 2008, 337, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erden, B.F.; Ulak, G.; Yildiz, F.; Utkan, T.; Ozdemirci, S.; Gacar, N. Antidepressant, Anxiogenic, and Antinociceptive Properties of Levofloxacin in Rats and Mice. Pharmacol. Biochem. Behav. 2001, 68, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Croom, K.F.; Goa, K.L. Levofloxacin: A Review of Its Use in the Treatment of Bacterial Infections in the United States. Drugs 2003, 63, 2769–2802. [Google Scholar] [CrossRef] [PubMed]
- Podder, V.; Sadiq, N.M. Levofloxacin. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Nishizawa, T.; Munkjargal, M.; Ebinuma, H.; Toyoshima, O.; Suzuki, H. Sitafloxacin for Third-Line Helicobacter pylori Eradication: A Systematic Review. J. Clin. Med. 2021, 10, 2722. [Google Scholar] [CrossRef]
- Sachs, G.; Shin, J.M.; Howden, C.W. Review Article: The Clinical Pharmacology of Proton Pump Inhibitors. Aliment Pharmacol. Ther. 2006, 23 (Suppl. S2), 2–8. [Google Scholar] [CrossRef]
- Richter, J.E. Gastrooesophageal Reflux Disease. Best Pract. Res. Clin. Gastroenterol. 2007, 21, 609–631. [Google Scholar] [CrossRef]
- Sachs, G.; Shin, J.M.; Briving, C.; Wallmark, B.; Hersey, S. The Pharmacology of the Gastric Acid Pump: The H+,K+ ATPase. Annu. Rev. Pharmacol. Toxicol. 1995, 35, 277–305. [Google Scholar] [CrossRef]
- Chiba, T.; Malfertheiner, P.; Satoh, H. Proton Pump Inhibitors: A Balanced View; Karger Book: Basel, Switzerland, 2013. [Google Scholar]
- Yibirin, M.; De Oliveira, D.; Valera, R.; Plitt, A.E.; Lutgen, S. Adverse Effects Associated with Proton Pump Inhibitor Use. Cureus 2021, 13, e12759. [Google Scholar] [CrossRef]
- Abraham, N.S. Proton Pump Inhibitors: Potential Adverse Effects. Curr. Opin. Gastroenterol. 2012, 28, 615–620. [Google Scholar] [CrossRef]
- Ahmed, A.; Clarke, J.O. Proton Pump Inhibitors (PPI). In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Graham, D.Y.; Dore, M.P. Update on the Use of Vonoprazan: A Competitive Acid Blocker. Gastroenterology 2018, 154, 462–466. [Google Scholar] [CrossRef] [Green Version]
- Shin, J.M.; Sachs, G. Long Lasting Inhibitors of the Gastric H,K-ATPase. Expert Rev. Clin. Pharmacol. 2009, 2, 461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Echizen, H. The First-in-Class Potassium-Competitive Acid Blocker, Vonoprazan Fumarate: Pharmacokinetic and Pharmacodynamic Considerations. Clin. Pharmacokinet. 2016, 55, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Fock, K.M.; Ang, T.L.; Bee, L.C.; Lee, E.J.D. Proton Pump Inhibitors. Clin. Pharmacokinet. 2008, 47, 1–6. [Google Scholar] [CrossRef]
- Vonoprazan, a Novel Potassium-Competitive Acid Blocker, as a Component of First-Line and Second-Line Triple Therapy for Helicobacter pylori Eradication: A Phase III, Randomised, Double-Blind Study | Gut. Available online: https://gut.bmj.com/content/65/9/1439 (accessed on 22 November 2022).
- Garnock-Jones, K.P. Vonoprazan: First Global Approval. Drugs 2015, 75, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Kambara, H.; Hosohata, K.; Nakatsuji, T.; Ueno, S.; Oyama, S.; Inada, A.; Niinomi, I.; Wakabayashi, T.; Iwanaga, K. Safety Profile of Vonoprazan Compared with Proton Pump Inhibitors: Insight from a Pharmacovigilance Study. Pharmazie 2020, 75, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Chung, J.-W.; Woo, H.S.; Kim, S.Y.; Kim, J.H.; Kim, Y.J.; Kim, K.O.; Kwon, K.A.; Park, D.K. Two-Week Bismuth-Containing Quadruple Therapy and Concomitant Therapy Are Effective First-Line Treatments for Helicobacter pylori Eradication: A Prospective Open-Label Randomized Trial. World J. Gastroenterol. 2019, 25, 6790–6798. [Google Scholar] [CrossRef] [PubMed]
- Mégraud, F. The Challenge of Helicobacter pylori Resistance to Antibiotics: The Comeback of Bismuth-Based Quadruple Therapy. Therap. Adv. Gastroenterol. 2012, 5, 103–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comparative Effectiveness and Tolerance of Treatments for Helicobacter pylori: Systematic Review and Network Meta-Analysis | The BMJ. Available online: https://www.bmj.com/content/351/bmj.h4052 (accessed on 22 November 2022).
- Quadruple Therapy Using a 3-in-1 Capsule of Bismuth Subcitrate Potassium, Metronidazole, and Tetracycline with Omeprazole Compared to Triple Therapy for the Eradication of Helicobacter pylori: 2010 Presidential Poster: 117. Available online: https://www.researchgate.net/publication/331707058_Quadruple_Therapy_Using_a_3-in-1_Capsule_of_Bismuth_Subcitrate_Potassium_Metronidazole_and_Tetracycline_with_Omeprazole_Compared_to_Triple_Therapy_for_the_Eradication_of_Helicobacter_pylori_2010_Presi (accessed on 22 November 2022).
- Venerito, M.; Krieger, T.; Ecker, T.; Leandro, G.; Malfertheiner, P. Meta-Analysis of Bismuth Quadruple Therapy versus Clarithromycin Triple Therapy for Empiric Primary Treatment of Helicobacter pylori Infection. Digestion 2013, 88, 33–45. [Google Scholar] [CrossRef]
- Shiota, S.; Reddy, R.; Alsarraj, A.; El-Serag, H.B.; Graham, D.Y. Antibiotic Resistance of Helicobacter pylori Among Male United States Veterans. Clin. Gastroenterol. Hepatol. 2015, 13, 1616–1624. [Google Scholar] [CrossRef]
- Greenberg, E.R.; Anderson, G.L.; Morgan, D.R.; Torres, J.; Chey, W.D.; Bravo, L.E.; Dominguez, R.L.; Ferreccio, C.; Herrero, R.; Lazcano-Ponce, E.C.; et al. 14-Day Triple, 5-Day Concomitant, and 10-Day Sequential Therapies for Helicobacter pylori Infection in Seven Latin American Sites: A Randomised Trial. Lancet 2011, 378, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Butt, A.M.K.; Sarwar, S.; Nadeem, M.A. Concomitant Therapy versus Triple Therapy: Efficacy in H. pylori Eradication and Predictors of Treatment Failure. J. Coll. Physicians Surg. Pak. 2021, 31, 128–131. [Google Scholar] [CrossRef] [PubMed]
- Gisbert, J.P.; Romano, M.; Gravina, A.G.; Solís-Muñoz, P.; Bermejo, F.; Molina-Infante, J.; Castro-Fernández, M.; Ortuño, J.; Lucendo, A.J.; Herranz, M.; et al. Helicobacter pylori Second-Line Rescue Therapy with Levofloxacin- and Bismuth-Containing Quadruple Therapy, after Failure of Standard Triple or Non-Bismuth Quadruple Treatments. Aliment Pharmacol. Ther. 2015, 41, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Fallone, C.A.; Chiba, N.; van Zanten, S.V.; Fischbach, L.; Gisbert, J.P.; Hunt, R.H.; Jones, N.L.; Render, C.; Leontiadis, G.I.; Moayyedi, P.; et al. The Toronto Consensus for the Treatment of Helicobacter pylori Infection in Adults. Gastroenterology 2016, 151, 51–69.e14. [Google Scholar] [CrossRef] [PubMed]
- Efficacy and Safety of Hybrid Therapy for Helicobacter pylori Infection: A Systematic Review and Meta-Analysis; Centre for Reviews and Dissemination: Heslington, UK, 2014.
- Kim, S.Y.; Choi, D.J.; Chung, J.-W. Antibiotic Treatment for Helicobacter pylori: Is the End Coming? World J. Gastrointest. Pharmacol. Ther. 2015, 6, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Goderska, K.; Agudo Pena, S.; Alarcon, T. Helicobacter pylori Treatment: Antibiotics or Probiotics. Appl. Microbiol. Biotechnol. 2018, 102, 1–7. [Google Scholar] [CrossRef]
- Finegold, S.M. Metronidazole. Ann. Intern. Med. 1980, 93, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.S.; Woodcock, K.R. Do Ethanol and Metronidazole Interact to Produce a Disulfiram-like Reaction? Ann. Pharmacother. 2000, 34, 255–257. [Google Scholar] [CrossRef]
- Shutter, M.C.; Akhondi, H. Tetracycline. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Graham, D.Y. Transitioning of Helicobacter pylori Therapy from Trial and Error to Antimicrobial Stewardship. Antibiotics 2020, 9, 671. [Google Scholar] [CrossRef]
- Saleem, N.; Howden, C.W. Update on the Management of Helicobacter pylori Infection. Curr. Treat. Options Gastroenterol. 2020, 18, 476–487. [Google Scholar] [CrossRef]
- Gisbert, J.P.; Pajares, J.M. Stool Antigen Test for the Diagnosis of Helicobacter pylori Infection: A Systematic Review. Helicobacter 2004, 9, 347–368. [Google Scholar] [CrossRef]
- Shah, S.C.; Iyer, P.G.; Moss, S.F. AGA Clinical Practice Update on the Management of Refractory Helicobacter pylori Infection: Expert Review. Gastroenterology 2021, 160, 1831–1841. [Google Scholar] [CrossRef]
- Raina, H.; Sainani, R.; Parray, A.; wani, A.H.; Asharaf, U.; Raina, M.A. Efficacy of Levofloxacin, Omeprazole, Nitazoxanide, and Doxycycline (LOAD) Regimen Compared with Standard Triple Therapy to Eradicate Helicobacter pylori Infection: A Prospective Randomized Study from a Tertiary Hospital in India. Gastroenterol. Hepatol. Bed Bench 2021, 14, 342–348. [Google Scholar]
- Polat, Z.; Kadayifci, A.; Kantarcioglu, M.; Ozcan, A.; Emer, O.; Uygun, A. Comparison of Levofloxacin-Containing Sequential and Standard Triple Therapies for the Eradication of Helicobacter pylori. Eur. J. Intern. Med. 2012, 23, 165–168. [Google Scholar] [CrossRef]
- Yang, J.-C.; Lin, C.-J.; Wang, H.-L.; Chen, J.-D.; Kao, J.Y.; Shun, C.-T.; Lu, C.-W.; Lin, B.-R.; Shieh, M.-J.; Chang, M.-C.; et al. High-Dose Dual Therapy Is Superior to Standard First-Line or Rescue Therapy for Helicobacter pylori Infection. Clin. Gastroenterol. Hepatol. 2015, 13, 895–905.e5. [Google Scholar] [CrossRef]
- Saracino, I.M.; Pavoni, M.; Zullo, A.; Fiorini, G.; Saccomanno, L.; Lazzarotto, T.; Antonelli, G.; Cavallo, R.; Borghi, C.; Vaira, D. Rifabutin-Based Triple Therapy Or Bismuth-Based Quadruple Regimen As Rescue Therapies For Helicobacter pylori Infection. Eur. J. Intern. Med. 2020, 81, 50–53. [Google Scholar] [CrossRef]
- Papastergiou, V.; Georgopoulos, S.D.; Karatapanis, S. Treatment of Helicobacter pylori Infection: Meeting the Challenge of Antimicrobial Resistance. World J. Gastroenterol. 2014, 20, 9898–9911. [Google Scholar] [CrossRef]
- Pantuzza, L.L.; Ceccato, M.D.G.B.; Silveira, M.R.; Junqueira, L.M.R.; Reis, A.M.M. Association between Medication Regimen Complexity and Pharmacotherapy Adherence: A Systematic Review. Eur. J. Clin. Pharmacol. 2017, 73, 1475–1489. [Google Scholar] [CrossRef]
- Bhatia, S.J.; Kochar, N.; Abraham, P.; Nair, N.G.; Mehta, A.P. Lactobacillus Acidophilus Inhibits Growth of Campylobacter Pylori in Vitro. J. Clin. Microbiol. 1989, 27, 2328–2330. [Google Scholar] [CrossRef]
- Prescription Prices, Coupons & Pharmacy Information. Available online: https://www.goodrx.com/ (accessed on 22 November 2022).



| Regimen | Cost |
|---|---|
| Bismuth Quadruple Therapy | $85.08 |
| Pylera | $903.84 |
| Helidac | $946.89 |
| Clarithromycin Triple Therapy | $15.44 |
| Prevpac | $224.90 |
| Concomitant Therapy | $23.54 |
| Levofloxacin Triple Therapy | $14.10 |
| Rifabutin Triple Therapy | $146.33 |
| Talicia | $697.01 |
| Clinical Efficacy and Safety | |||
|---|---|---|---|
| Author and Study | Groups Studied and Intervention | Results and Findings | Conclusions |
| Study 1: Single Capsule Bismuth Quadruple Therapy for Eradication of H. pylori Infection: A Real-Life Study https://pubmed.ncbi.nlm.nih.gov/33995097/ (accessed on 11 August 2022) | A total of 250 treatment-naïve patients were given esomeprazole 40 mg bid and Pylera 3 tablets QID for 10 days. |
| Using a combination capsule is an effective strategy that improves compliance and yields high eradication rates with low incidence of side effects. |
| Study 2: Long-term changes in the gut microbiota after triple therapy, sequential therapy, bismuth quadruple therapy, and concomitant therapy for Helicobacter pylori eradication in Chinese children https://pubmed.ncbi.nlm.nih.gov/33899288/ (accessed on 11 August 2022) |
|
| Transient microbiota changes may occur following H. pylori treatment but return to normal within a year to indicate long-term safety. |
| Study 3: Half-dose clarithromycin-containing bismuth therapy is effective and economical in treating Helicobacter pylori infection: A single-center, open-label, randomized trial quadruple https://pubmed.ncbi.nlm.nih.gov/30780194/ (accessed on 11 August 2022) |
|
| A half-dose clarithromycin regimen is as effective as the full dose regimen with improved tolerability and affordability. |
| Study 4: Efficacy of Lactoferrin with Standard Triple Therapy or Sequential Therapy for Helicobacter pylori Eradication: A Randomized Controlled Trial https://pubmed.ncbi.nlm.nih.gov/34609303/ (accessed on 11 August 2022) | A total of 400 H. pylori-infected patients were either assigned to a triple therapy or sequential therapy group, and each regimen also had a separate group that added bovine lactoferrin for 2 weeks. | Bovine lactoferrin showed improved effectiveness in the sequential therapy and triple therapy (94.5% vs. 82.8% and 85.6% vs. 70.3%). | Bovine lactoferrin could help improve eradication rates as an addition to current regimens. |
| Study 5: Efficacy and safety of twice a day, bismuth-containing quadruple therapy using high-dose tetracycline and metronidazole for second-line Helicobacter pylori eradication https://pubmed.ncbi.nlm.nih.gov/32074663/ (accessed on 11 August 2022) | A total of 100 patients in each group received either bismuth subcitrate 300 mg QID or BID, tetracycline 1 g, metronidazole 750 mg, and pantoprazole 20 mg BID for 1 week. | The eradication rates between the twice daily and four times daily did not differ (93.9% vs. 92.9%), while adverse effects were more common in the four times daily than twice daily (50 vs. 36). | The twice daily regimen is as effective and safe as the four-times-daily regimen. |
| Comparative Studies | |||
|---|---|---|---|
| Study | Groups Studied and Intervention | Results and Findings | Conclusions |
| Study 1: High Effective of 14-Day High-Dose PPI- Bismuth-Containing Quadruple Therapy with Probiotics Supplement for Helicobacter Pylori Eradication: A Double Blinded-Randomized Placebo-Controlled Study https://pubmed.ncbi.nlm.nih.gov/31554388/ (accessed on 11 August 2022) | A total of 100 patients randomized to receive 7 or 14-day bismuth quadruple therapy with or without probiotic supplement. | Overall eradication rates were 68% and 96% for the 7- and 14-day probiotics group and reduced side effects compared to placebo (26% vs. 6%). | Adding probiotics can improve eradication rates and reduce side effects. |
| Study 3: Rifabutin-Based Triple Therapy or Bismuth-Based Quadruple Regimen As Rescue Therapies For Helicobacter pylori Infection https://pubmed.ncbi.nlm.nih.gov/32646659/ (accessed on 11 August 2022) | A total of 270 patients received rifabutin-based triple therapy for 12 days, and 153 patients received quadruple therapy with Pylera for 10 days. | Pylera therapy produced a greater eradication rate than rifabutin (88.3% vs. 61.9%). | Pylera is a good option over rifabutin, despite previous treatment failures. |
| Study 4: Two-week bismuth-containing quadruple therapy and concomitant therapy are effective first-line treatments for Helicobacter pylori eradication: A prospective open-label randomized trial https://pubmed.ncbi.nlm.nih.gov/31857780/ (accessed on 11 August 2022) | A total 68 patients in each group received either quadruple or concomitant therapy for 2 weeks. | The eradication rate of the quadruple therapy was higher than the concomitant group (88.2% vs. 79.4%) and had lower adverse events (33.8% vs. 51.5%). | Quadruple therapy was found to have higher eradication rates and better tolerability. |
| Study 5: Concomitant Therapy versus Triple Therapy: Efficacy in H. pylori Eradication and Predictors of Treatment Failure https://pubmed.ncbi.nlm.nih.gov/33645176/ (accessed on 11 August 2022) | A total 105 patients were treated with concomitant therapy and 106 with triple therapy for two weeks each. | Concomitant therapy achieved eradication rates of 91.9% and 77.2% for triple therapy. | Concomitant therapy achieved higher eradication rates than triple therapy. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roberts, L.T.; Issa, P.P.; Sinnathamby, E.S.; Granier, M.; Mayeux, H.; Eubanks, T.N.; Malone, K.; Ahmadzadeh, S.; Cornett, E.M.; Shekoohi, S.; et al. Helicobacter Pylori: A Review of Current Treatment Options in Clinical Practice. Life 2022, 12, 2038. https://doi.org/10.3390/life12122038
Roberts LT, Issa PP, Sinnathamby ES, Granier M, Mayeux H, Eubanks TN, Malone K, Ahmadzadeh S, Cornett EM, Shekoohi S, et al. Helicobacter Pylori: A Review of Current Treatment Options in Clinical Practice. Life. 2022; 12(12):2038. https://doi.org/10.3390/life12122038
Chicago/Turabian StyleRoberts, Logan T., Peter P. Issa, Evan S. Sinnathamby, Mallory Granier, Holly Mayeux, Treniece N. Eubanks, Kevin Malone, Shahab Ahmadzadeh, Elyse M. Cornett, Sahar Shekoohi, and et al. 2022. "Helicobacter Pylori: A Review of Current Treatment Options in Clinical Practice" Life 12, no. 12: 2038. https://doi.org/10.3390/life12122038
APA StyleRoberts, L. T., Issa, P. P., Sinnathamby, E. S., Granier, M., Mayeux, H., Eubanks, T. N., Malone, K., Ahmadzadeh, S., Cornett, E. M., Shekoohi, S., & Kaye, A. D. (2022). Helicobacter Pylori: A Review of Current Treatment Options in Clinical Practice. Life, 12(12), 2038. https://doi.org/10.3390/life12122038









