Improving Survival in Cardiogenic Shock—A Propensity Score-Matched Analysis of the Impact of an Institutional Allocation Protocol to Short-Term Mechanical Circulatory Support
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Observed Outcomes
2.3. Data Collection
2.4. Statistical Analysis
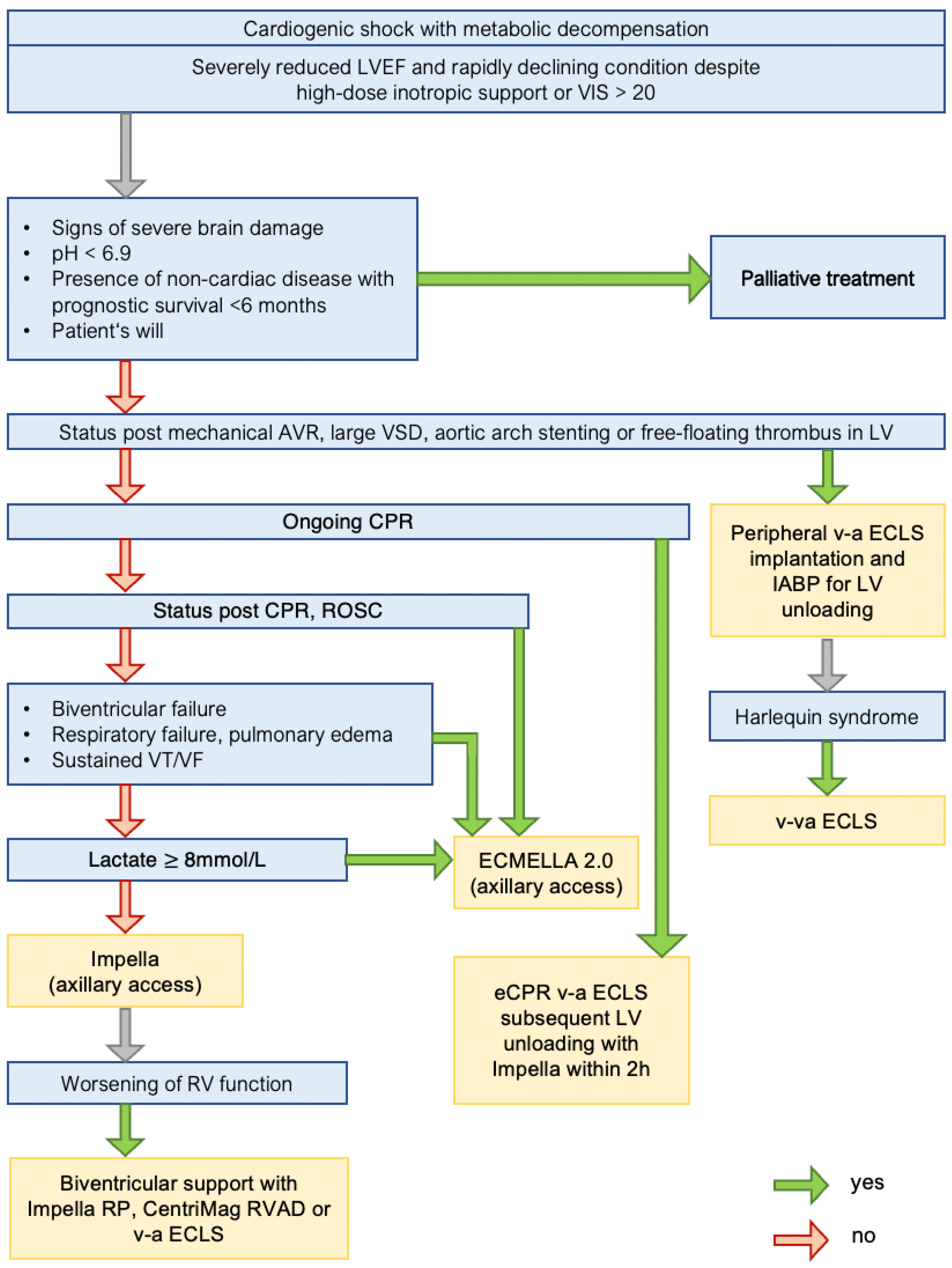
3. Standard Operating Procedure
4. Results
4.1. Study Cohort
4.2. Outcome Analysis
4.2.1. Unmatched Cohorts
4.2.2. Matched Cohorts
4.2.3. Matched Subgroups SOP-A and SOP-NA
5. Discussion
5.1. Rationale of SOP Revision
5.2. Outcome
5.3. Observed Cohort and Comparative Evaluation
5.4. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Samsky, M.D.; Morrow, D.A.; Proudfoot, A.G.; Hochman, J.S.; Thiele, H.; Rao, S.V. Cardiogenic shock after acute myocardial infarction: A review. JAMA 2021, 326, 1840–1850. [Google Scholar] [CrossRef] [PubMed]
- Freund, A.; Desch, S.; Pöss, J.; Sulimov, D.; Sandri, M.; Majunke, N.; Thiele, H. Extracorporeal Membrane Oxygenation in Infarct-Related Cardiogenic Shock. J. Clin. Med. 2022, 11, 1256. [Google Scholar] [CrossRef] [PubMed]
- Chioncel, O.; Mebazaa, A.; Harjola, V.-P.; Coats, A.J.; Piepoli, M.F.; Crespo-Leiro, M.G.; Laroche, C.; Seferovic, P.M.; Anker, S.D.; Ferrari, R.; et al. ESC Heart Failure Long-Term Registry Investigators Clinical phenotypes and outcome of patients hospitalized for acute heart failure: The ESC Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2017, 19, 1242–1254. [Google Scholar] [CrossRef] [PubMed]
- Van Diepen, S.; Katz, J.N.; Albert, N.M.; Henry, T.D.; Jacobs, A.K.; Kapur, N.K.; Kilic, A.; Menon, V.; Ohman, E.M.; Sweitzer, N.K.; et al. Contemporary management of cardiogenic shock: A scientific statement from the american heart association. Circulation 2017, 136, e232–e268. [Google Scholar] [CrossRef] [PubMed]
- Mariscalco, G.; El-Dean, Z.; Yusuff, H.; Fux, T.; Dell’Aquila, A.M.; Jónsson, K.; Ragnarsson, S.; Fiore, A.; Dalén, M.; di Perna, D.; et al. Duration of venoarterial extracorporeal membrane oxygenation and mortality in postcardiotomy cardiogenic shock. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2662–2668. [Google Scholar] [CrossRef] [PubMed]
- Schrage, B.; Dabboura, S.; Yan, I.; Hilal, R.; Neumann, J.T.; Sörensen, N.A.; Goßling, A.; Becher, P.M.; Grahn, H.; Wagner, T.; et al. Application of the SCAI classification in a cohort of patients with cardiogenic shock. Catheter. Cardiovasc. Interv. 2020, 96, E213–E219. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.H.; Puri, R.; Kalra, A. Management of cardiogenic shock complicating acute myocardial infarction: A review. Clin. Cardiol. 2019, 42, 484–493. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.L.; Etchill, E.W.; Giuliano, K.A.; Shou, B.L.; Sharma, K.; Choi, C.W.; Kilic, A. Bridge to transplantation from mechanical circulatory support: A narrative review. J. Thorac. Dis. 2021, 13, 6911–6923. [Google Scholar] [CrossRef]
- Den Uil, C.A.; Akin, S.; Jewbali, L.S.; Dos Reis Miranda, D.; Brugts, J.J.; Constantinescu, A.A.; Kappetein, A.P.; Caliskan, K. Short-term mechanical circulatory support as a bridge to durable left ventricular assist device implantation in refractory cardiogenic shock: A systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 2017, 52, 14–25. [Google Scholar] [CrossRef]
- Oren, D.; Zilinyi, R.; Lotan, D.; Uriel, M.; Uriel, N.; Sayer, G. The role of temporary mechanical circulatory support as a bridge to advanced heart failure therapies or recovery. Curr. Opin. Cardiol. 2022, 37, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Tehrani, B.N.; Truesdell, A.G.; Psotka, M.A.; Rosner, C.; Singh, R.; Sinha, S.S.; Damluji, A.A.; Batchelor, W.B. A standardized and comprehensive approach to the management of cardiogenic shock. JACC Heart Fail. 2020, 8, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Samsky, M.D.; Krucoff, M.W.; Morrow, D.A.; Abraham, W.T.; Aguel, F.; Althouse, A.D.; Chen, E.; Cigarroa, J.E.; DeVore, A.D.; Farb, A.; et al. Cardiac safety research consortium “shock II” think tank report: Advancing practical approaches to generating evidence for the treatment of cardiogenic shock. Am. Heart J. 2020, 230, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef] [PubMed]
- Koponen, T.; Karttunen, J.; Musialowicz, T.; Pietiläinen, L.; Uusaro, A.; Lahtinen, P. Vasoactive-inotropic score and the prediction of morbidity and mortality after cardiac surgery. Br. J. Anaesth. 2019, 122, 428–436. [Google Scholar] [CrossRef]
- Eulert-Grehn, J.-J.; Starck, C.; Kempfert, J.; Falk, V.; Potapov, E. ECMELLA 2.0: Single arterial access technique for a staged approach in cardiogenic shock. Ann. Thorac. Surg. 2021, 111, e135–e137. [Google Scholar] [CrossRef] [PubMed]
- Pahuja, M.; Schrage, B.; Westermann, D.; Basir, M.B.; Garan, A.R.; Burkhoff, D. Hemodynamic effects of mechanical circulatory support devices in ventricular septal defect. Circ. Heart Fail. 2019, 12, e005981. [Google Scholar] [CrossRef] [PubMed]
- Via, G.; Buson, S.; Tavazzi, G.; Halasz, G.; Quagliana, A.; Moccetti, M.; Demertzis, S.; Cassina, T. Early cardiac unloading with ImpellaCPTM in acute myocardial infarction with ventricular septal defect. ESC Heart Fail. 2020, 7, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Giudicatti, L.; Silbert, B.; Xu, X.-F.; Putrino, A.; Lee, F.; Shah, A.; Larbalestier, R.; Slimani, K.; Laycock, A.; Lam, K. Post-Myocardial Infarction Ventricular Septal Defect Successfully Treated with Impella as Bridge to Cardiac Transplantation. Case Rep. Cardiol. 2022, 2022, 5690844. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, H.R.; Hochman, J.S. Cardiogenic shock: Current concepts and improving outcomes. Circulation 2008, 117, 686–697. [Google Scholar] [CrossRef] [PubMed]
- Bavaria, J.E.; Ratcliffe, M.B.; Gupta, K.B.; Wenger, R.K.; Bogen, D.K.; Edmunds, L.H. Changes in left ventricular systolic wall stress during biventricular circulatory assistance. Ann. Thorac. Surg. 1988, 45, 526–532. [Google Scholar] [CrossRef]
- Lucas, S.K.; Schaff, H.V.; Flaherty, J.T.; Gott, V.L.; Gardner, T.J. The harmful effects of ventricular distention during postischemic reperfusion. Ann. Thorac. Surg. 1981, 32, 486–494. [Google Scholar] [CrossRef]
- Griffith, B.P.; Anderson, M.B.; Samuels, L.E.; Pae, W.E.; Naka, Y.; Frazier, O.H. The RECOVER I: A multicenter prospective study of Impella 5.0/LD for postcardiotomy circulatory support. J. Thorac. Cardiovasc. Surg. 2013, 145, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Murakami, T.; Sakakura, K.; Jinnouchi, H.; Taniguchi, Y.; Tsukui, T.; Watanabe, Y.; Yamamoto, K.; Seguchi, M.; Wada, H.; Fujita, H. Complications related to veno-arterial extracorporeal membrane oxygenation in patients with acute myocardial infarction: VA-ECMO complications in AMI. J. Cardiol. 2022, 79, 170–178. [Google Scholar] [CrossRef]
- Schrage, B.; Becher, P.M.; Bernhardt, A.; Bezerra, H.; Blankenberg, S.; Brunner, S.; Colson, P.; Cudemus Deseda, G.; Dabboura, S.; Eckner, D.; et al. Left ventricular unloading is associated with lower mortality in patients with cardiogenic shock treated with venoarterial extracorporeal membrane oxygenation: Results from an international, multicenter cohort study. Circulation 2020, 142, 2095–2106. [Google Scholar] [CrossRef]
- Russo, J.J.; Aleksova, N.; Pitcher, I.; Couture, E.; Parlow, S.; Faraz, M.; Visintini, S.; Simard, T.; Di Santo, P.; Mathew, R.; et al. Left ventricular unloading during extracorporeal membrane oxygenation in patients with cardiogenic shock. J. Am. Coll. Cardiol. 2019, 73, 654–662. [Google Scholar] [CrossRef]
- Al-Fares, A.A.; Randhawa, V.K.; Englesakis, M.; McDonald, M.A.; Nagpal, A.D.; Estep, J.D.; Soltesz, E.G.; Fan, E. Optimal Strategy and Timing of Left Ventricular Venting During Veno-Arterial Extracorporeal Life Support for Adults in Cardiogenic Shock: A Systematic Review and Meta-Analysis. Circ. Heart Fail. 2019, 12, e006486. [Google Scholar] [CrossRef]
- Kowalewski, M.; Malvindi, P.G.; Zieliński, K.; Martucci, G.; Słomka, A.; Suwalski, P.; Lorusso, R.; Meani, P.; Arcadipane, A.; Pilato, M.; et al. Left Ventricle Unloading with Veno-Arterial Extracorporeal Membrane Oxygenation for Cardiogenic Shock. Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 1039. [Google Scholar] [CrossRef]
- Lorusso, R.; Meani, P.; Raffa, G.M.; Kowalewski, M. Extracorporeal membrane oxygenation and left ventricular unloading: What is the evidence? JTCVS Tech. 2022, 13, 101–114. [Google Scholar] [CrossRef]
- Nersesian, G.; Tschöpe, C.; Spillmann, F.; Gromann, T.; Roehrich, L.; Mueller, M.; Mulzer, J.; Starck, C.; Falk, V.; Schoenrath, F.; et al. Prediction of survival of patients in cardiogenic shock treated by surgically implanted Impella 5+ short-term left ventricular assist device. Interact. Cardiovasc. Thorac. Surg. 2020, 31, 475–482. [Google Scholar] [CrossRef]
- Morris, Z.S.; Wooding, S.; Grant, J. The answer is 17 years, what is the question: Understanding time lags in translational research. J. R. Soc. Med. 2011, 104, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Westfall, J.M.; Mold, J.; Fagnan, L. Practice-based research—“Blue Highways” on the NIH roadmap. JAMA 2007, 297, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Balas, E.A.; Boren, S.A. Managing clinical knowledge for health care improvement. Yearb. Med. Inform. 2000, 9, 65–70. [Google Scholar] [CrossRef]


| Variable | Unmatched Cohort (n = 421) | Matched Groups (n = 306) | ||||
|---|---|---|---|---|---|---|
| Pre-SOP (n = 189) | SOP (n = 232) | p | Pre-SOP (n = 153) | SOP (n = 153) | p | |
| Age (years) | 60.12 {13.99} | 61.94 {13.01} | 0.165 | 60.50 {14.45} | 60.14 {13.79} | 0.842 |
| Sex (male) | 146 (77.2) | 173 (74.6) | 0.600 | 121 (79.1) | 113 (73.9) | 0.345 |
| BMI | 27.59 {5.72} | 28.37{6.64} | 0.221 | 27.99 {5.83} | 27.64 {5.37} | 0.593 |
| Diabetes | 61 (32.3) | 70 (31.0) | 0.859 | 50 (32.7) | 44 (28.8) | 0.536 |
| CKD | 45 (24.3) | 74 (32.9) | 0.073 | 44 (28.8) | 43 (28.1) | 1.000 |
| MAP (mmHg) | 66.00 [57.50, 75.00] | 69.00 [62.00, 78.00] | 0.017 | 66.00 [58.00, 76.00] | 68.00 [61.00, 77.00] | 0.12 |
| Heart rate (bpm) | 96.00 [82.00, 112.50] | 93.00 [78.00,105.00] | 0.136 | 97.00 [82.00, 111.00] | 93.00 [77.00, 104.00] | 0.178 |
| Lactate (mmol/L) | 6.11 [2.78,10.99] | 4.78 [1.72,10.1] | 0.014 | 6.05 [2.77,10.57] | 4.22 [1.44,10.19] | 0.258 |
| pH | 7.32 [7.25, 7.39] | 7.31 [7.23, 7.39] | 0.352 | 7.32 [7.25, 7.39] | 7.31 [7.22, 7.40] | 0.142 |
| VI score | 32.00 [13.00, 48.90] | 18.88 [8.00, 41.35] | 0.001 | 30.70 [13.00, 51.98] | 18.00 [7.61, 40.75] | 0.01 |
| RRT prior to tMCS | 21 (11.2) | 27 (11.7) | 1.000 | 20 (13.2) | 19 (12.5) | 0.982 |
| Cause of CS | ||||||
| AMICS | 34 (18.0) | 24 (10.3) | 0.034 | 21 (13.7) | 22 (14.4) | 1.000 |
| Acute-on-chronic CMP | 56 (29.6) | 90 (38.8) | 0.063 | 49 (32.0) | 51 (33.3) | 0.903 |
| PCCS | 80 (42.3) | 100 (43.1) | 0.951 | 69 (45.1) | 67 (43.8) | 0.912 |
| Other | 18 (10.1) | 18 (7.8) | 0.502 | 14 (9.2) | 13 (8.5) | 0.840 |
| Previous cardiac arrest | 71 (37.6) | 58 (25.0) | 0.007 | 48 (31.4) | 45 (29.4) | 0.731 |
| Duration of CPR (min) | 20.00 [10.00, 58.75] | 20.00 [10.00, 50.75] | 0.459 | 17.50 [10.00, 40.00] | 19.50 [10.50, 53.75] | 0.401 |
| eCPR | 30 (18.5) | 36 (20.9) | 0.667 | 21 (16.3) | 26 (23.4) | 0.22 |
| Mechanical aortic valve | 2 (1.2) | 0 (0) | 0.465 | 2 (1.5) | 0 (0.0) | 0.559 |
| Aortic arch stent | 1 (0.6) | 4 (2.3) | 0.385 | 1 (0.8) | 1 (0.9) | 1.000 |
| Free-floating LV thrombus | 0 (0) | 1 (0.6) | 1.000 | 0 (0.0) | 1 (0.9) | 0.928 |
| MCS type | ||||||
| v-a ECLS | 139 (73.5) | 109 (47.0) | <0.001 | 109 (71.2) | 70 (45.8) | <0.001 |
| Impella | 26 (13.8) | 61 (26.3) | 0.002 | 20 (13.1) | 41 (26.8) | 0.004 |
| ECMELLA | 24 (12.7) | 62 (26.7) | 0.001 | 23 (15.0) | 42 (27.5) | 0.012 |
| Variable | Unmatched Cohort (n = 230) | Matched Groups (n = 144) | ||||
|---|---|---|---|---|---|---|
| SOP-A (n = 120) | SOP-NA (n = 110) | p | SOP-A (n = 72) | SOP-NA (n = 72) | p | |
| Age (years) | 59.63 {13.06} | 64.44 {12.53} | 0.005 | 62.07 {12.17} | 62.58 {12.38} | 0.802 |
| Sex (male) | 97 (80.8) | 74 (67.3) | 0.028 | 56 (77.8) | 57 (79.2) | 1.000 |
| BMI | 28.11 {7.24} | 28.71 {5.95} | 0.506 | 28.72 {7.67} | 28.88 {5.64} | 0.888 |
| Diabetes | 37 (31.6) | 32 (29.9) | 0.894 | 24 (33.3) | 23 (31.9) | 1.000 |
| CKD | 39 (33.6) | 35 (32.7) | 0.998 | 23 (31.9) | 25 (34.7) | 0.860 |
| MAP (mmHg) | 71.00 [63.00, 77.00] | 68.00 [60.50, 77.50] | 0.571 | 69.00 [63.00, 76.00] | 67.00 [59.25, 81.00] | 0.661 |
| Heart rate (bpm) | 93.00 [79.00, 105.00] | 94.00 [78.00, 105.50] | 0.698 | 91.00 [77.00, 105.00] | 98.50 [87.00, 108.00] | 0.335 |
| Lactate (mmol/L) | 2.99 [1.44, 6.13] | 7.55 [3.77, 10.93] | <0.001 | 3.05 [1.55, 6.05] | 8.55 [4.17, 10.88] | <0.001 |
| pH | 7.34 [7.26, 7.40] | 7.29 [7.20, 7.37] | 0.018 | 7.33 [7.24, 7.40] | 7.29 [7.20, 7.37] | 0.087 |
| VI score | 18.00 [8.89, 37.75] | 21.60 [8.00, 42.25] | 0.504 | 19.00 [9.79, 40.00] | 26.45 [10.50, 51.30] | 0.331 |
| RRT prior to tMCS | 10 (8.3) | 16 (14.7) | 0.193 | 8 (11.1) | 14 (19.7) | 0.232 |
| Cause of CS | ||||||
| AMICS | 17 (14.2) | 7 (6.4) | 0.086 | 7 (9.7) | 5 (6.9) | 0.763 |
| Acute-on-chronic CMP | 50 (41.7) | 38 (34.5) | 0.330 | 31 (43.1) | 27 (37.5) | 0.610 |
| PCCS | 48 (40.0) | 52 (47.3) | 0.328 | 29 (40.0) | 32 (44.4) | 0.742 |
| Other | 5 (4.1) | 13 (11.8) | 5 (7.2) | 8 (11.2) | 0.356 | |
| Previous cardiac arrest | 31 (25.8) | 27 (24.5) | 0.942 | 17 (23.6) | 16 (22.2) | 1.000 |
| Duration of CPR (min) | 20.00 [10.00, 51.25] | 21.50 [10.50, 60.00] | 0.814 | 35.00 [10.00, 57.75] | 14.00 [6.00, 51.25] | 0.279 |
| eCPR | 11 (15.5) | 25 (24.8) | 0.176 | 6 (14.6) | 19 (27.9) | 0.133 |
| Mechanical aortic valve | 0 (0.0) | 0 (0.0) | NaN | 0 (0.0) | 0 (0.0) | NaN |
| Aortic arch stent | 3 (4.2) | 1 (1.0) | 0.383 | 2 (4.9) | 1 (1.5) | 0.653 |
| Free-floating LV thrombus | 1 (1.4) | 0 (0.0) | 0.859 | 1 (2.4) | 0 (0.0) | 0.797 |
| MCS type | MCS type | |||||
| v-a ECLS | 8 (6.7) | 101 (91.8) | <0.001 | 6 (8.3) | 68 (94.4) | <0.001 |
| Impella | 50 (41.7) | 9 (8.2) | <0.001 | 32 (44.4) | 4 (5.6) | <0.001 |
| ECMELLA | 62 (51.7) | 0 (0) | <0.001 | 34 (47.2) | 0 (0.0) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ott, S.; Lewin, D.; Nersesian, G.; Stein, J.; Just, I.A.; Hommel, M.; Schoenrath, F.; Starck, C.T.; O’Brien, B.; Falk, V.; et al. Improving Survival in Cardiogenic Shock—A Propensity Score-Matched Analysis of the Impact of an Institutional Allocation Protocol to Short-Term Mechanical Circulatory Support. Life 2022, 12, 1931. https://doi.org/10.3390/life12111931
Ott S, Lewin D, Nersesian G, Stein J, Just IA, Hommel M, Schoenrath F, Starck CT, O’Brien B, Falk V, et al. Improving Survival in Cardiogenic Shock—A Propensity Score-Matched Analysis of the Impact of an Institutional Allocation Protocol to Short-Term Mechanical Circulatory Support. Life. 2022; 12(11):1931. https://doi.org/10.3390/life12111931
Chicago/Turabian StyleOtt, Sascha, Daniel Lewin, Gaik Nersesian, Julia Stein, Isabell A. Just, Matthias Hommel, Felix Schoenrath, Christoph T. Starck, Benjamin O’Brien, Volkmar Falk, and et al. 2022. "Improving Survival in Cardiogenic Shock—A Propensity Score-Matched Analysis of the Impact of an Institutional Allocation Protocol to Short-Term Mechanical Circulatory Support" Life 12, no. 11: 1931. https://doi.org/10.3390/life12111931
APA StyleOtt, S., Lewin, D., Nersesian, G., Stein, J., Just, I. A., Hommel, M., Schoenrath, F., Starck, C. T., O’Brien, B., Falk, V., Potapov, E., & Lanmueller, P. (2022). Improving Survival in Cardiogenic Shock—A Propensity Score-Matched Analysis of the Impact of an Institutional Allocation Protocol to Short-Term Mechanical Circulatory Support. Life, 12(11), 1931. https://doi.org/10.3390/life12111931







