Laparoscopic Pancreatoduodenectomy in Elderly Patients: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Inclusion and Exclusion Criteria
2.3. Literature Search Strategy
2.4. Study Selection and Quality Assessment
2.5. Data Extraction and Analysis
3. Results
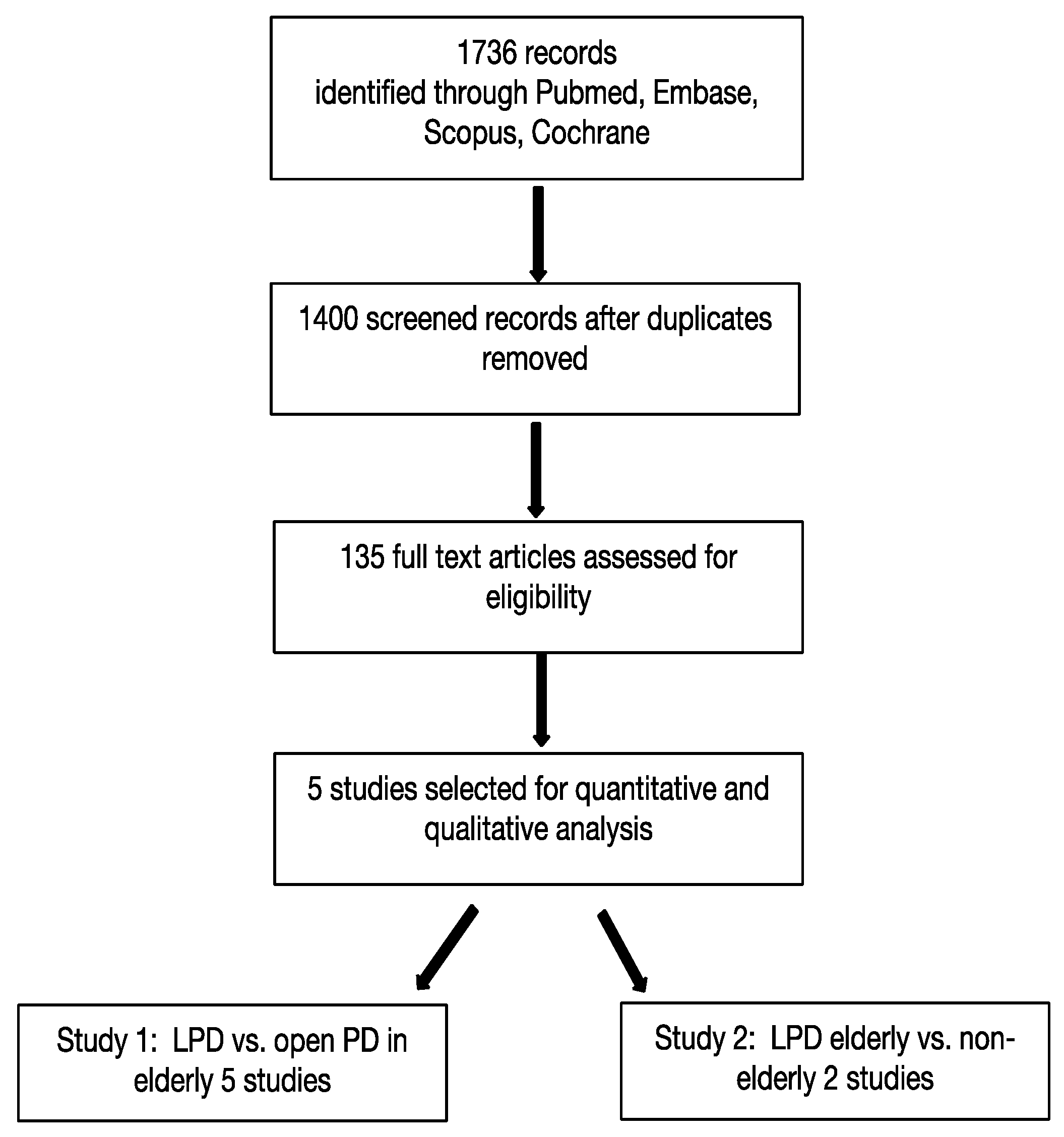
3.1. Literature Search and Selection
3.2. First Study: LPD vs. OPD in Elderly
3.3. Second Study: Outcome of LPD in the Elderly vs. Non-Elderly Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, A.S.Y.; Menon, R.; Gunnarsson, R.; de Costa, A. Risk factors for conversion of laparoscopic cholecystectomy to open surgery—A systematic literature review of 30 studies. Am. J. Surg. 2017, 214, 920–930. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Pérez, A.; Carra, M.C.; Brunetti, F.; De’Angelis, N. Pathologic Outcomes of Laparoscopic vs Open Mesorectal Excision for Rectal Cancer: A Systematic Review and Meta-analysis. JAMA Surg. 2017, 152, e165665. [Google Scholar] [CrossRef] [PubMed]
- Beyer, K.; Baukloh, A.-K.; Kamphues, C.; Seeliger, H.; Heidecke, C.-D.; Kreis, M.E.; Patrzyk, M. Laparoscopic versus open gastrectomy for locally advanced gastric cancer: A systematic review and meta-analysis of randomized controlled studies. World J. Surg. Oncol. 2019, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Bates, A.T.; Divino, C. Laparoscopic Surgery in the Elderly: A Review of the Literature. Aging Dis. 2015, 6, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Are, C.; Dhir, M.; Ravipati, L. History of pancreaticoduodenectomy: Early misconceptions, initial milestones and the pioneers. HPB 2011, 13, 377–384. [Google Scholar] [CrossRef]
- Gagner, M.; Pomp, A. Laparoscopic pylorus-preserving pancreaticoduodenectomy. Surg. Endosc. 1994, 8, 408–410. [Google Scholar] [CrossRef]
- Pugliese, R.; Scandroglio, I.; Sansonna, F. Laparoscopic pancreaticoduodenectomy: A retrospective review of 19 cases. Surg. Laparosc. Endosc. Percutaneous Tech. 2008, 18, 13–18. [Google Scholar] [CrossRef]
- Kooby, D.A.; Gillespie, T.; Bentrem, D. Left-sided pancreatectomy: A multicenter comparison of laparoscopic and open ap-proaches. Ann. Surg. 2008, 248, 438–446. [Google Scholar] [CrossRef]
- Ammori, B.J. Laparoscopic hand-assisted pancreaticoduodenectomy: Initial UK experience. Surg. Endosc. 2004, 18, 717–718. [Google Scholar] [CrossRef]
- van Hilst, J.; Brinkman, D.J.; de Rooij, T.; van Dieren, S.; Gerhards, M.F.; de Hingh, I.H.; Luyer, M.D.; Marsman, H.A.; Karsten, T.M.; Busch, O.R.; et al. The inflammatory response after laparoscopic and open pancreatoduodenectomy and the association with complications in a multicenter randomized controlled trial. HPB 2019, 21, 1453–1461. [Google Scholar] [CrossRef]
- Probst, P.; Hüttner, F.J.; Meydan, Ö.; Hilal, M.A.; Adham, M.; Barreto, S.G.; Besselink, M.G.; Busch, O.R.; Bockhorn, M.; Del Chiaro, M.; et al. Evidence Map of Pancreatic Surgery–A living systematic review with meta-analyses by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2021, 170, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- Available online: www.emps.evidencemap.surgery (accessed on 15 September 2022).
- Wang, M.; Li, D.; Chen, R.; Huang, X.; Li, J.; Liu, Y.; Liu, J.; Cheng, W.; Chen, X.; Zhao, W.; et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: A multicentre, open-label, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2021, 6, 438–447. [Google Scholar] [CrossRef]
- Poves, I.; Burdío, F.; Morató, O.; Iglesias, M.; Radosevic, A.; Ilzarbe, L.; Visa, L.; Grande, L. Comparison of Perioperative Outcomes Between Laparoscopic and Open Approach for Pancreatoduodenectomy: The PADULAP Randomized Controlled Trial. Ann. Surg. 2018, 268, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Palanivelu, C.; Senthilnathan, P.; Sabnis, S.C.; Babu, N.S.; Gurumurthy, S.S.; Vijai, N.A.; Nalankilli, V.P.; Raj, P.P.; Parthasarathy, R.; Rajapandian, S. Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br. J. Surg. 2017, 104, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- van Hilst, J.; de Rooij, T.; Bosscha, K.; Brinkman, D.J.; van Dieren, S.; Dijkgraaf, M.G.; Gerhards, M.F.; de Hingh, I.H.; Karsten, T.M.; Lips, D.J.; et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): A multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol. Hepatol. 2019, 4, 199–207. [Google Scholar] [CrossRef]
- Nickel, F.; Haney, C.M.; Kowalewski, K.-F.; Probst, P.; Limen, E.F.; Kalkum, E.; Diener, M.K.; Strobel, O.; Müller-Stich, B.P.; Hackert, T. Laparoscopic Versus Open Pancreaticoduodenectomy: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann. Surg. 2020, 271, 54–66. [Google Scholar] [CrossRef]
- Tan, Y.; Tang, T.; Zhang, Y.; Zu, G.; An, Y.; Chen, W.; Wu, D.; Sun, D.; Chen, X. Laparoscopic vs. open pancreaticoduodenectomy: A comparative study in elderly people. Updates Surg. 2020, 72, 701–707. [Google Scholar] [CrossRef]
- Liang, Y.; Zhao, L.; Jiang, C.; Hu, P.; Wang, H.; Cai, Z.; Wang, W. Laparoscopic pancreaticoduodenectomy in elderly patients. Surg. Endosc. 2020, 34, 2028–2034. [Google Scholar] [CrossRef]
- Chapman, B.C.; Gajdos, C.; Hosokawa, P.; Henderson, W.; Paniccia, A.; Overbey, D.M.; Gleisner, A.; Schulick, R.D.; McCarter, M.D.; Edil, B.H. Comparison of laparoscopic to open pancreaticoduodenectomy in elderly patients with pancreatic adenocarcinoma. Surg. Endosc. 2018, 32, 2239–2248. [Google Scholar] [CrossRef]
- Tee, M.C.; Croome, K.P.; Shubert, C.R.; Farnell, M.B.; Truty, M.J.; Que, F.G.; Reid-Lombardo, K.; Smoot, R.L.; Nagorney, D.M.; Kendrick, M.L. Laparoscopic pancreatoduodenectomy does not completely mitigate increased perioperative risks in elderly patients. HPB 2015, 17, 909–918. [Google Scholar] [CrossRef]
- Shin, H.; Song, K.B.; Kim, Y.I.; Lee, Y.-J.; Hwang, D.W.; Lee, J.H.; Shin, S.H.; Kwon, J.; Alshammary, S.; Park, G.; et al. Propensity score-matching analysis comparing laparoscopic and open pancreaticoduodenectomy in elderly patients. Sci. Rep. 2019, 9, 12961. [Google Scholar] [CrossRef] [PubMed]
- Kalkum, E.; Klotz, R.; Seide, S.; Hüttner, F.J.; Kowalewski, K.-F.; Nickel, F.; Khajeh, E.; Knebel, P.; Diener, M.K.; Probst, P. Systematic reviews in surgery—Recommendations from the Study Center of the German Society of Surgery. Langenbeck’s Arch. Surg. 2021, 406, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Turrentine, F.E.; Wang, H.; Simpson, V.B.; Jones, R.S. Surgical risk factors, morbidity, and mortality in elderly patients. J. Am. Coll. Surg. 2006, 203, 865–877. [Google Scholar] [CrossRef] [PubMed]
- Funamizu, N.; Sakamoto, A.; Utsunomiya, T.; Uraoka, M.; Nagaoka, T.; Iwata, M.; Ito, C.; Tamura, K.; Sakamoto, K.; Ogawa, K.; et al. Geriatric nutritional risk index as a potential prognostic marker for patients with resectable pancreatic cancer: A single-center, retrospective cohort study. Sci. Rep. 2022, 12, 13644. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wu, W.; Zhang, T.; Liao, Q.; Zhao, Y.; Dai, M. Comparison of long-term benefits of organ-preserving pancreatectomy techniques for benign or low-grade malignant tumors at the pancreatic head. Medicine 2017, 96, e9420. [Google Scholar] [CrossRef]
- Narayanan, S.; Bhutiani, N.; Adamson, D.T.; Jones, C.M. Pancreatectomy, Islet Cell Transplantation, and Nutrition Considerations. Nutr. Clin. Pract. 2021, 36, 385–397. [Google Scholar] [CrossRef]
- Busquets, J.; Martín, S.; Secanella, L.; Sorribas, M.; Cornellà, N.; Altet, J.; Peláez, N.; Bajen, M.; Carnaval, T.; Videla, S.; et al. Delayed gastric emptying after classical Whipple or pylorus-preserving pancreatoduodenectomy: A randomized clinical trial (QUANUPAD). Langenbeck’s Arch. Surg. 2022, 407, 2247–2258. [Google Scholar] [CrossRef]
- Lord, A.C.; Hicks, G.; Pearce, B.; Tanno, L.; Pucher, P. Safety and outcomes of laparoscopic cholecystectomy in the extremely elderly: A systematic review and meta-analysis. Acta Chir. Belg. 2019, 119, 349–356. [Google Scholar] [CrossRef]
- Antoniou, S.A.; Antoniou, G.A.; Koch, O.O.; Pointner, R.; Granderath, F.A. Meta-analysis of laparoscopic vs. open cholecystectomy in elderly patients. World J. Gastroenterol. 2014, 20, 17626–17634. [Google Scholar] [CrossRef]
- Li, Y.; Wang, S.; Gao, S.; Yang, C.; Yang, W.; Guo, S. Laparoscopic colorectal resection versus open colorectal resection in octogenarians: A systematic review and meta-analysis of safety and efficacy. Tech. Coloproctol. 2016, 20, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, M.; Felli, E.; Roselli, S.; Altomare, D.F.; De Fazio, M.; De’Angelis, N.; Piardi, T.; Acquafredda, S.; Ammendola, M.; Verbo, A.; et al. Laparoscopic liver resection in elderly patients: Systematic review and meta-analysis. Surg. Endosc. 2019, 33, 2763–2773. [Google Scholar] [CrossRef] [PubMed]
- Caglià, P.; Tracia, A.; Buffone, A.; Amodeo, L.; Tracia, L.; Amodeo, C.; Veroux, M. Physiopathology and clinical considerations of laparoscopic surgery in the elderly. Int. J. Surg. 2016, 33, S97–S102. [Google Scholar] [CrossRef] [PubMed]
- Shin, T.H.; Friedrich, S.; Brat, G.A.; Rudolph, M.I.; Sein, V.; Munoz-Acuna, R.; Houle, T.T.; Ferrone, C.R.; Eikermann, M. Effects of laparoscopic vs open abdominal surgery on costs and hospital readmission rate and its effect modification by surgeons’ case volume. Surg. Endosc. 2020, 34, 1–12. [Google Scholar] [CrossRef]
- Liu, M.; Ji, S.; Xu, W.; Liu, W.; Qin, Y.; Hu, Q.; Sun, Q.; Zhang, Z.; Yu, X.; Xu, X. Laparoscopic pancreaticoduodenectomy: Are the best times coming? World J. Surg. Oncol. 2019, 17, 81. [Google Scholar] [CrossRef]
- Sharpe, S.M.; Talamonti, M.S.; Wang, C.E.; Prinz, R.A.; Roggin, K.K.; Bentrem, D.J.; Winchester, D.J.; Marsh, R.D.; Stocker, S.J.; Baker, M.S. Early National Experience with Laparoscopic Pancreaticoduodenectomy for Ductal Adenocarcinoma: A Comparison of Laparoscopic Pancreaticoduodenectomy and Open Pancreaticoduodenectomy from the National Cancer Data Base. J. Am. Coll. Surg. 2015, 221, 175–184. [Google Scholar] [CrossRef]
- Adam, M.A.; Choudhury, K.; Dinan, M.A.; Reed, S.D.; Scheri, R.P.; Blazer, D.; Roman, S.A.; Sosa, J.A. Minimally Invasive Versus Open Pancreaticoduodenectomy for Cancer: Practice Patterns and Short-term Outcomes Among 7061 Patients. Ann. Surg. 2015, 262, 372–377. [Google Scholar] [CrossRef]
- Torphy, R.J.; Friedman, C.; Halpern, A.; Chapman, B.C.; Ahrendt, S.S.; McCarter, M.M.; Edil, B.H.; Schulick, R.D.; Gleisner, A. Comparing Short-term and Oncologic Outcomes of Minimally Invasive Versus Open Pancreaticoduodenectomy Across Low and High Volume Centers. Ann. Surg. 2019, 270, 1147–1155. [Google Scholar] [CrossRef]
- Wang, Q.; Chen, C.; Li, H. Laparoscopic Pancreaticoduodenectomy in Elderly Patients: Systematic Review and Meta-Analysis. Front. Surg. 2022, 9, 807940. [Google Scholar] [CrossRef]
- Zhang, W.; Huang, Z.; Zhang, J.; Che, X. Effect of Laparoscopic Pancreaticoduodenectomy in Elderly People: A Meta-analysis. Pancreas 2021, 50, 1154–1162. [Google Scholar] [CrossRef]
- Yin, T.; Qin, T.; Wei, K.; Shen, M.; Zhang, Z.; Wen, J.; Pan, S.; Guo, X.; Zhu, F.; Wang, M.; et al. Comparison of safety and effectiveness between laparoscopic and open pancreatoduodenectomy: A systematic review and meta-analysis. Int. J. Surg. 2022, 105, 106799. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Choi, M.; Kim, S.H.; Choi, S.H.; Kang, C.M. Safety and feasibility of laparoscopic pancreaticoduodenectomy in octogenarians. Asian J. Surg. 2022, 45, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Jiang, N.; Tian, E.; Li, M.; Zhang, H.; Zhao, G.; Tan, X.; Wang, W.; Han, B.; Yuan, J.; et al. Short-term outcomes of robotic versus open pancreaticoduodenectomy in elderly patients: A multicenter retrospective cohort study. Int. J. Surg. 2022, 104, 106819. [Google Scholar] [CrossRef]
- Paolini, C.; Bencini, L.; Gabellini, L.; Urciuoli, I.; Pacciani, S.; Tribuzi, A.; Moraldi, L.; Calistri, M.; Coratti, A. Robotic versus open pancreaticoduodenectomy: Is there any difference for frail patients? Surg. Oncol. 2021, 37, 101515. [Google Scholar] [CrossRef] [PubMed]
| Source | Period | Type of Study | Nr of Pt | Age of Cut Off | Approach | Median Age | ASA Score Class or Mean ± SD | Type of Pathology | Tumour Size (cm, IQR or ±SD) |
|---|---|---|---|---|---|---|---|---|---|
| Tan [18] | 2015–2019 | R | 56/28 | ≥0 | LPD OPD | 75.2 (±4.4) 74.7 (±4.6) | II 37/19 III 19/9 | PC 21/11 CC 31/4 AC 2/3 DC 8/4 | 2.5 (1.9–4.3) 3.3 (2.0–4.0) |
| Liang [19] | 2015–2018 | R | 27/19 | ≥70 | LPD OPD | 74 (±4) 76 (±5) | II 19/8 III 18/8 | PC 12/15 AC 12/2 | 2.6 (±1) 3.1 (±1) |
| Chapman [20] | 2010–2013 | R | 248/1520 | ≥75 | LPD OPD | 79.6 (±3.5) 79.5 (±3.4) | N/A | PC 248/1520 | <2: 25/125 2–4: 169/1002 >4: 49/329 |
| Tee [21] | 2007–2014 | R | 113/225 | ≥70 | LPD OPD | 76.5 (±4.3) 76.4 (±4.5) | I-II 30/67 III-IV 83/158 | PC 53/121 CC 4/15 AC 9/33 DC 2/11 | N/A |
| Shin [22] | 2014–2017 | R | 56/270 | ≥70 | LPD OPD | 74.8 (±3.7) 74.6 (±3.5) | 2.1± 0.5 2.1±0.4 | PC 14/115 CC 19/92 | N/A |
| Source | Period | Type of Study | Nr of Pt | Age of Cut Off | Median Age | Type of Pathology | ASA Score Class or Mean ± SD | Tumor Size (cm, IQR or ±SD) |
|---|---|---|---|---|---|---|---|---|
| Tan [18] | 2015–2019 | R | 56/84 | ≥70 | 75.2 (±4.4) 60.7 (±7.5) | PC 21/22 CC 31/20 AC 2/1 DC 8/13 | II 37/66 III 19/18 | 2.5 (1.9–4.3) 2.2 (1.7–3.0) |
| Liang [19] | 2015–2018 | R | 27/55 | ≥70 | 74 (±4) 59 (±9) | PC 12/18 AC 12/17 | II 19/42 III 8/1 | 2.6 (±1) 2.8 (±1.4) |
| (a) | Postoperative mortality rate at 30 days |  |
| (b) | Readmission rate in hospital |  |
| (c) | Mortality rate at 90 days | 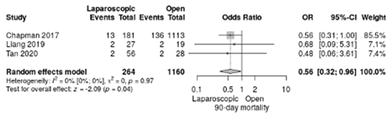 |
| (d) | Clavien–Dindo I/II complications | 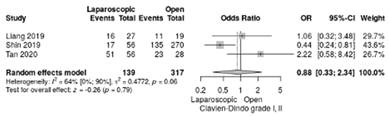 |
| (e) | Clavien–Dindo III-V complications |  |
| (f) | Delayed gastric emptying | 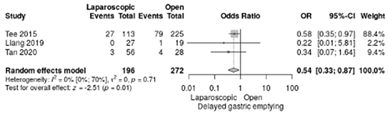 |
| (g) | Pancreatic fistula grade B/C | 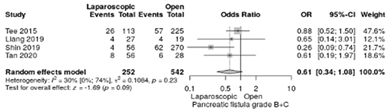 |
| (h) | Complete resection (R0) | 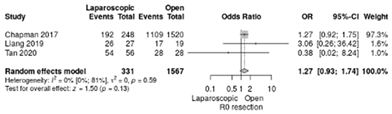 |
| (i) | Reoperation for complications |  |
| (j) | Blood loss | 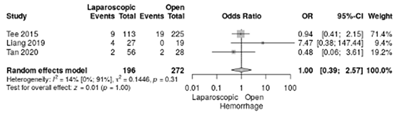 |
| (a) | Mortality rate at 90 days | 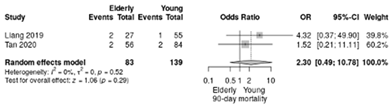 |
| (b) | Readmission rate in hospital | 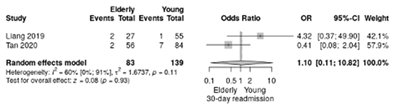 |
| (c) | Clavien–Dindo III-V complications | 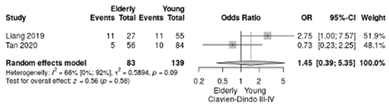 |
| (d) | Clavien–Dindo I/II complications | 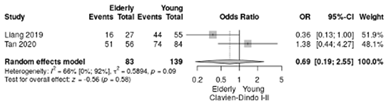 |
| (e) | Conversion rate | 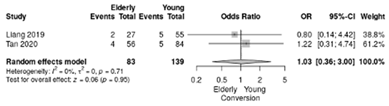 |
| (f) | Delayed gastric emptying | 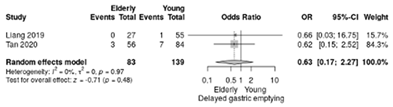 |
| (g) | Pancreatic fistula grade B/C |  |
| (h) | Complete resection (R0) |  |
| (i) | Reoperation for complications | 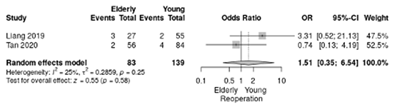 |
| (j) | Blood loss |  |
| Article | Selection | Comparability | Outcome | Score (Risk of Bias) | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| Tan et al. | ☆ | ☆ | ☆ | / | ☆ | ☆ | ☆ | ☆ | 7 (low) |
| Liang et al. | ☆ | ☆ | ☆ | / | ☆ | ☆ | ☆ | ☆ | 7 (low) |
| Chapman et al. | ☆ | ☆ | ☆ | / | ☆ | ☆ | ☆ | ☆ | 7 (low) |
| Tee et al. | ☆ | ☆ | ☆ | / | ☆ | ☆ | ☆ | ☆ | 7 (low) |
| Shin et al. | ☆ | ☆ | ☆ | / | ☆ | ☆ | ☆ | ☆ | 7 (low) |
| Benefits | Disadvantages | |
|---|---|---|
| Laparoscopic approach | Reduced postoperative pain Decreased hospital length of stay Improved mobilization Faster return to normal activity Fewer abdominal wall complications Lower rates of readmissions related to gastrointestinal, wound complications and malignancy and subsequently lower costs | More challenging based on technical aspects, with a longer learning curve for surgeons experienced with open approach Carbon dioxide pneumoperitoneum used in laparoscopic approach might lead to acidosis, produce changes in pulmonary mechanics, induce alteration in hemodynamic function and increase the risk of aspiration |
| Open surgery | Standardized procedures Established training | More blood loss compared with laparoscopy Increased postoperative pain, considering the large incision of abdominal wall Increased hospital length of stay Abdominal wall complications Increased recovery time compared with laparoscopy |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartos, A.; Mărgărit, S.; Bocse, H.; Krisboi, I.; Iancu, I.; Breazu, C.; Plesa-Furda, P.; Brînzilă, S.; Leucuta, D.; Iancu, C.; et al. Laparoscopic Pancreatoduodenectomy in Elderly Patients: A Systematic Review and Meta-Analysis. Life 2022, 12, 1810. https://doi.org/10.3390/life12111810
Bartos A, Mărgărit S, Bocse H, Krisboi I, Iancu I, Breazu C, Plesa-Furda P, Brînzilă S, Leucuta D, Iancu C, et al. Laparoscopic Pancreatoduodenectomy in Elderly Patients: A Systematic Review and Meta-Analysis. Life. 2022; 12(11):1810. https://doi.org/10.3390/life12111810
Chicago/Turabian StyleBartos, Adrian, Simona Mărgărit, Horea Bocse, Iulia Krisboi, Ioana Iancu, Caius Breazu, Patricia Plesa-Furda, Sandu Brînzilă, Daniel Leucuta, Cornel Iancu, and et al. 2022. "Laparoscopic Pancreatoduodenectomy in Elderly Patients: A Systematic Review and Meta-Analysis" Life 12, no. 11: 1810. https://doi.org/10.3390/life12111810
APA StyleBartos, A., Mărgărit, S., Bocse, H., Krisboi, I., Iancu, I., Breazu, C., Plesa-Furda, P., Brînzilă, S., Leucuta, D., Iancu, C., Puia, C., Al Hajjar, N., & Ciobanu, L. (2022). Laparoscopic Pancreatoduodenectomy in Elderly Patients: A Systematic Review and Meta-Analysis. Life, 12(11), 1810. https://doi.org/10.3390/life12111810








