Long-Term Anatomical and Hearing Outcomes of Canal Wall down Tympanoplasty for Tympano-Mastoid Cholesteatoma: A 20-Year Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Inclusion and Exclusion Criteria
- (1)
- Preoperative assessment including otomicrotoscopy, pure tone audiometry, middle ear CT scan
- (2)
- Single-stage CWD mastoidectomy
- (3)
- No previous otological surgery
- (4)
- Age > 15 years old
- (5)
- Minimum follow-up of at least 10 years
2.3. Surgical Techniques
2.4. Follow-Up Protocol
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nadol, J.B.; Schuknecht, H.F. Surgery of the Ear and Temporal Bone, 1st ed.; Raven Press: New York, NY, USA, 1993. [Google Scholar]
- Kim, M.B.; Choi, J.; Lee, J.K.; Park, J.-Y.; Chu, H.; Cho, Y.-S.; Hong, S.H.; Chung, W.-H. Hearing outcomes according to the types of mastoidectomy: A comparison between canal wall up and canal wall down mastoidectomy. Clin. Exp. Otorhinolaryngol. 2010, 3, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Yung, M.; Tono, T.; Olszewska, E.; Yamamoto, Y.; Sudhoff, H.; Sakagami, M.; Mulder, J.; Kojima, H.; İncesulu, A.; Trabalzini, F.; et al. EAONO/JOS Joint Consensus Statements on the definitions, classification and staging of middle ear cholesteatoma. J. Int. Adv. Otol. 2017, 3, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Palva, T.; Karma, P.; Palva, A. Cholesteatoma Surgery: Canal Wall down and Mastoid Obliteration. In Cholesteatoma First International Conference; McCabe, B., Sade, J., Abramson, M., Eds.; Aesculapius: Birmingham, AL, USA, 1977; pp. 363–367. [Google Scholar]
- Smyth, G.D.L.; Hassard, T.H. The Evolution of Policies in the Surgical Treatment of Acquired Cholesteatoma of the Tubotympanic Cleft. J. Laryngol. Otol. 1981, 95, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Nyrop, M.; Bonding, P. Extensive cholesteatoma: Long-term results of three surgical techniques. J. Laryngol. Otol. 1997, 111, 521–526. [Google Scholar] [CrossRef]
- Tomlin, J.; Chang, D.; McCutcheon, B.; Harris, J. Surgical technique and recurrence in cholesteatoma: A meta-analysis. Audiol. Neurootol. 2013, 18, 135–142. [Google Scholar] [CrossRef]
- Kerckhoffs, K.G.; Kommer, M.B.; van Strien, T.H.; Visscher, S.J.A.; Bruijnzeel, H.; Smit, A.L.; Grolman, W. The disease recurrence rate after the canal wall up or canal wall down technique in adults. Laryngoscope 2016, 126, 980–987. [Google Scholar] [CrossRef]
- Toner, J.G.; Smyth, G.D.L. Surgical Treatment of Cholesteatoma: A Comparison of Three Techniques. Am. J. Otolaryngol. 1990, 11, 247–249. [Google Scholar]
- Roden, D.; Honrubia, V.F.; Wiet, R. Outcome of Residual Cholesteatoma and Hearing in Mastoid Surgery. J. Otolaryngol. 1996, 25, 178–181. [Google Scholar]
- Whittemore, K.R.; Merchant, S.N.; Rosowski, J.J. Acoustic Mechanisms: Canal Wall-Up versus Canal Wall down Mastoidectomy. Otolaryngol. Head Neck Surg. 1998, 118, 751–762. [Google Scholar] [CrossRef]
- Aslan Felek, S.; Islam, A.; Celik, H.; Demirci, M.; Samim, E.; Kose, S.K. The functional and anatomical results of the canal wall down tympanoplasty in extensive cholesteatoma. Acta Otolaryngol. 2009, 129, 1388–1394. [Google Scholar] [CrossRef]
- Cho, Y.S.; Hong, S.D.; Chung, K.W.; Hong, S.H.; Chung, W.-H.; Park, S.H. Revision surgery for chronic otitis media: Characteristics and outcomes in comparison with primary surgery. Auris Nasus Larynx 2010, 37, 18–22. [Google Scholar] [CrossRef]
- Ajalloueyan, M. Experience with surgical management of cholesteatomas. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 931–933. [Google Scholar] [CrossRef]
- Cook, J.A.; Krishnan, S.; Fagan, P.A. Hearing Results Following Modified Radical versus Canal-Up Mastoidectomy. Ann. Otol. Rhinol. Laryngol. 1996, 105, 379–383. [Google Scholar] [CrossRef]
- Chang, C.; Chen, M. Canal-Wall down Tympanoplasty with Mastoidectomy for Advanced Cholesteatoma. J. Otol. 2000, 29, 271–273. [Google Scholar]
- Artuso, A.; Di Nardo, W.; De Corso, E.; Marchese, M.R.; Quaranta, N. Canal-Wall-Down Tympanoplasty Surgery with or without Ossiculoplasty in Cholesteatoma: Hearing Results. Acta Otorhinolaryngol. Ital. 2004, 24, 2–3. [Google Scholar]
- Berenholz, L.P.; Rizer, F.M.; Burkey, J.M.; Schuring, A.G.; Lipp, W.H. Ossiculoplasty in Canal Wall down Mastoidectomy. Otolaryngol. Head Neck Surg. 2000, 123, 30–33. [Google Scholar] [CrossRef]
- Gu, F.M.; Chi, F.L. Surgical results of modified canal wall down tympanoplasty. Acta Otolaryngol. 2017, 137, 803–806. [Google Scholar] [CrossRef]
- Bhatia, S.; Karmarkar, S.; DeDonato, G.; Mutlu, C.; Taibah, A.; Russo, A.; Sanna, M. Canal wall down mastoidectomy: Causes of failure, pitfalls and their management. J. Laryngol. Otol. 1995, 109, 583–589. [Google Scholar] [CrossRef]
- Hulka, G.F.; McElveen, J.T., Jr. A randomized, blinded study of canal wall up versus canal wall down mastoidectomy determining the differences in viewing middle ear anatomy and pathology. Am. J. Otol. 1998, 19, 574–578. [Google Scholar]
- Britze, A.; Moller, M.L.; Ovesen, T. Incidence, 10-year recidivism rate and prognostic factors for cholesteatoma. J. Laryngol. Otol. 2017, 131, 319–328. [Google Scholar] [CrossRef]
- Ferlito, S.; Allegra, E.; Grillo, C.; Fadda, G.L.; Conticello, S. Canal wall down mastoidectomy and tympanoplasty in cholesteatoma surgery: Ten years’ experience. Int. Johns 2016, 5, 195–202. [Google Scholar] [CrossRef][Green Version]
- Pareschi, R.; Lepera, D.; Nucci, R. CWD approach for tympanomastoid cholesteatoma: Long-term results and prognostic factors. Acta Otorhinolaryngol. Ital. 2019, 39, 122–129. [Google Scholar] [PubMed]
- Blom, E.F.; Gunning, M.N.; Kleinrensink, N.J.; Lokin, A.S.H.J.; Bruijnzeel, H.; Smit, A.L.; Grolman, W. Influence of Ossicular Chain Damage on Hearing After Chronic Otitis Media and Cholesteatoma Surgery: A Systematic Review and Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Strobe Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Kos, M.I.; Castrillon, R.; Montandon, P.; Guyot, J.P. Anatomic and functional long-term results of canal wall-down mastoidectomy. Ann. Otol. Rhinol. Laryngol. 2004, 113, 872–876. [Google Scholar] [CrossRef]
- Vartiainen, E.; Nuutinen, J. Long-term results of surgical treatment in different cholesteatoma types. Am. J. Otol. 1993, 14, 507–511. [Google Scholar] [CrossRef]
- Committee on Hearing and Equilibrium. Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol. Head Neck Surg. 1995, 113, 186–187. [Google Scholar] [CrossRef]
- De Zinis, L.O.; Tonni, D.; Barezzani, M.G. Single-stage canal wall-down tympanoplasty: Long-term results and prognostic factors. Ann. Otol. Rhinol. Laryngol. 2010, 119, 304–312. [Google Scholar] [CrossRef]
- Schraff, S.A.; Strasnick, B. Pediatric cholesteatoma: A retrospective review. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 385–393. [Google Scholar] [CrossRef]
- Shirazi, M.A.; Muzaffar, K.; Leonetti, J.P.; Marzo, S. Surgical treatment of pediatric cholesteatomas. Laryngoscope 2006, 116, 1603–1607. [Google Scholar] [CrossRef]
- Okada, M.; Gyo, K.; Takagi, T.; Fujiwara, T.; Takahashi, H.; Hakuba, N.; Hato, N. Air-bone gap in ears with a well-repaired tympanic membrane after Type III and Type IV tympanoplasty. Auris Nasus Larynx 2014, 41, 153–159. [Google Scholar] [CrossRef]
| Features | Total (n = 176) | Group A (n = 35) | Group B (n = 141) | p-Value |
|---|---|---|---|---|
| Residual Cholesteatoma | 10/176 (5.68%) | 2/35 (5.71%) | 8/141 (5.67%) | 0.993 |
| Recurrent Cholesteatoma | 4/176 (2.27%) | 1/35 (2.85%) | 3/141 (2.18%) | 0.516 |
| Total (n = 176) | Group A (n = 35) | Group B (n = 141) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 6 Months | 10 Years | p-Value | 6 Months | 10 Years | p-Value | 6 Months | 10 Years | p-Value | |
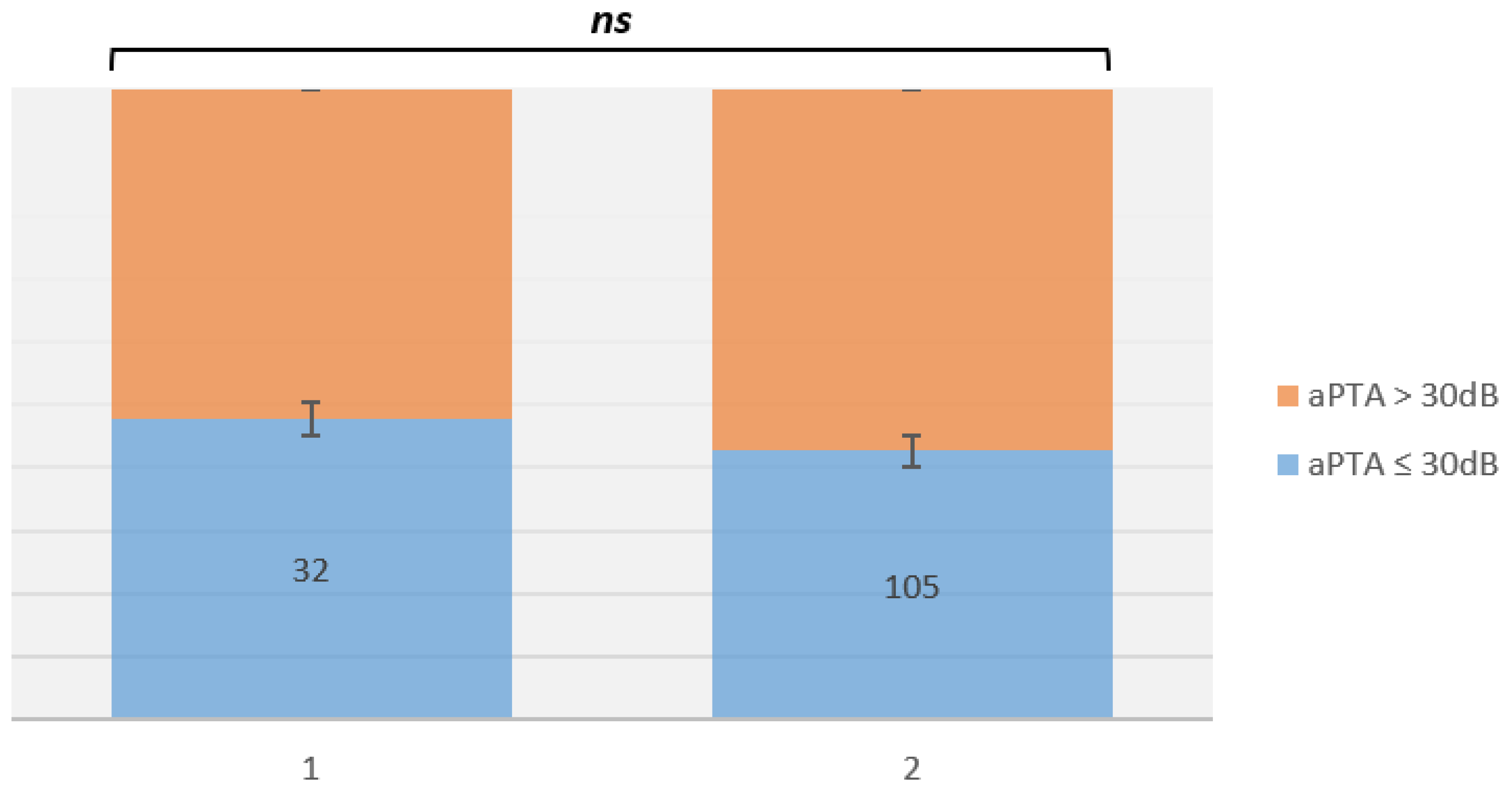
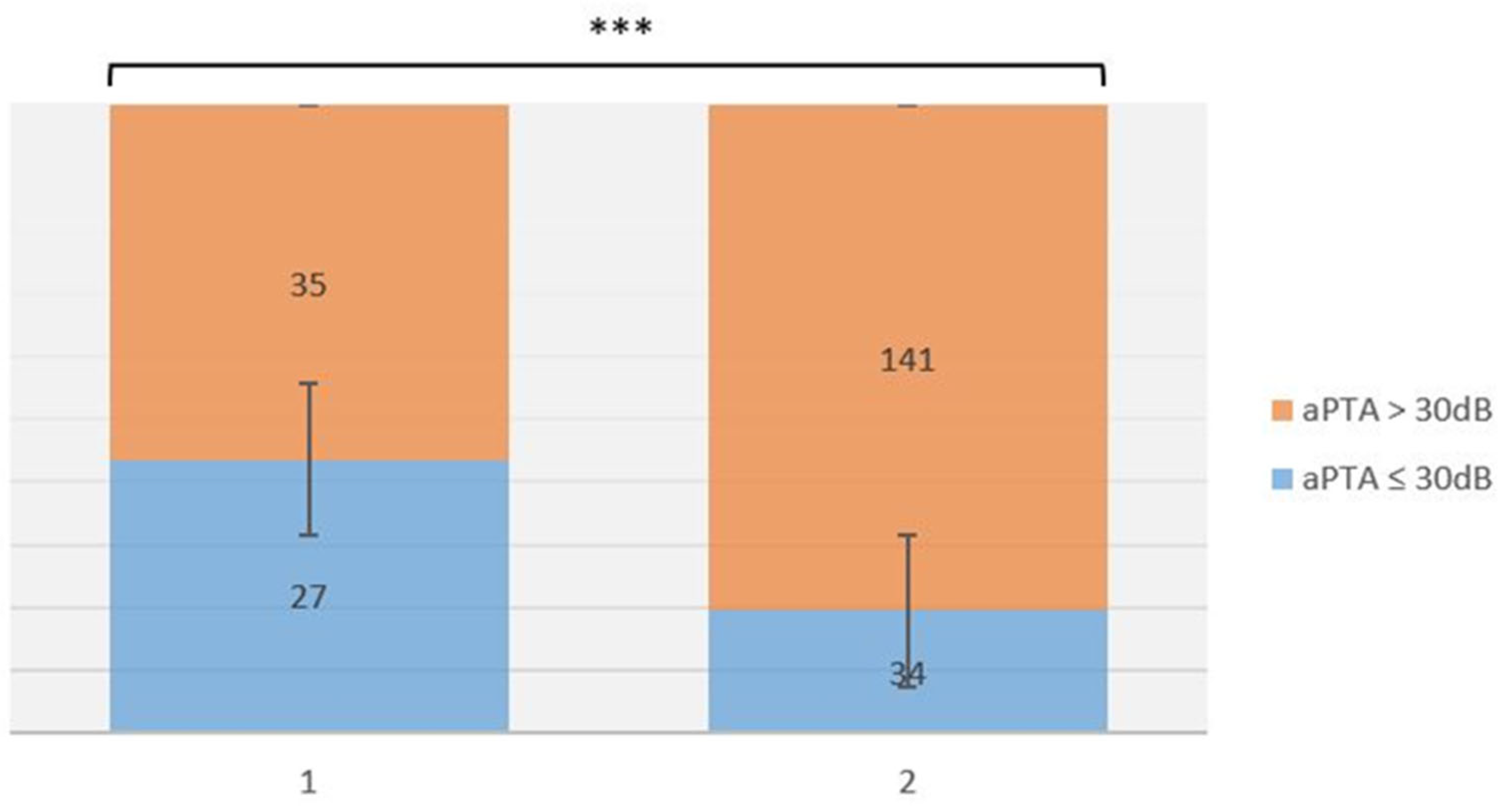
| ≤30 dB | 137 (77.84%) | 61 (34.65%) | p < 0.001 | 32 (91.42%) | 27 (77.14%) | p = 0.001 | 105 (74.46%) | 34 (24.11%) | p < 0.001 |
| >30 dB | 39 (22.15%) | 115 (65.34%) | 3 (8.57%) | 8 (22.85%) | 36 (25.53%) | 107 (75.88%) | |||
| Hearing Outcomes | Residual Rate | Recurrence Rate | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Square | F | Sig. | Mean Square | F | Sig. | Mean Square | F | Sig. | |
| Age | 0.305 | 1.396 | 0.239 | 0.004 | 0.019 | 0.89 | 0.757 | 3.508 | 0.063 |
| Gender | 0.003 | 0.013 | 0.909 | 0.073 | 0.305 | 0.581 | 0.056 | 0.235 | 0.628 |
| Stapes involvement | 5.256 | 38.958 | <0.001 | 0.0003 | 0.002 | 0.964 | 0.008 | 0.049 | 0.826 |
| Otorrea | 0.001 | 0.012 | 0.914 | 4.306 | 124.08 | <0.001 | 3.595 | 92.643 | <0.001 |
| Perforation | 0.0004 | 0.01 | 0.922 | 3.192 | 103.296 | <0.001 | 1.998 | 52.848 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferlito, S.; La Mantia, I.; Merlino, F.; Cocuzza, S.; Di Stadio, A.; Cammaroto, G.; Bartel, R.; Fadda, G.; Iannella, G.; Mat, Q.; et al. Long-Term Anatomical and Hearing Outcomes of Canal Wall down Tympanoplasty for Tympano-Mastoid Cholesteatoma: A 20-Year Retrospective Study. Life 2022, 12, 1745. https://doi.org/10.3390/life12111745
Ferlito S, La Mantia I, Merlino F, Cocuzza S, Di Stadio A, Cammaroto G, Bartel R, Fadda G, Iannella G, Mat Q, et al. Long-Term Anatomical and Hearing Outcomes of Canal Wall down Tympanoplasty for Tympano-Mastoid Cholesteatoma: A 20-Year Retrospective Study. Life. 2022; 12(11):1745. https://doi.org/10.3390/life12111745
Chicago/Turabian StyleFerlito, Salvatore, Ignazio La Mantia, Federico Merlino, Salvatore Cocuzza, Arianna Di Stadio, Giovanni Cammaroto, Ricardo Bartel, Gianluca Fadda, Giannicola Iannella, Quentin Mat, and et al. 2022. "Long-Term Anatomical and Hearing Outcomes of Canal Wall down Tympanoplasty for Tympano-Mastoid Cholesteatoma: A 20-Year Retrospective Study" Life 12, no. 11: 1745. https://doi.org/10.3390/life12111745
APA StyleFerlito, S., La Mantia, I., Merlino, F., Cocuzza, S., Di Stadio, A., Cammaroto, G., Bartel, R., Fadda, G., Iannella, G., Mat, Q., Gargula, S., Michel, J., Fakhry, N., & Maniaci, A. (2022). Long-Term Anatomical and Hearing Outcomes of Canal Wall down Tympanoplasty for Tympano-Mastoid Cholesteatoma: A 20-Year Retrospective Study. Life, 12(11), 1745. https://doi.org/10.3390/life12111745














