Safety of Electrotherapy Treatment in Patients with Knee Osteoarthritis and Cardiac Diseases
Abstract
1. Introduction
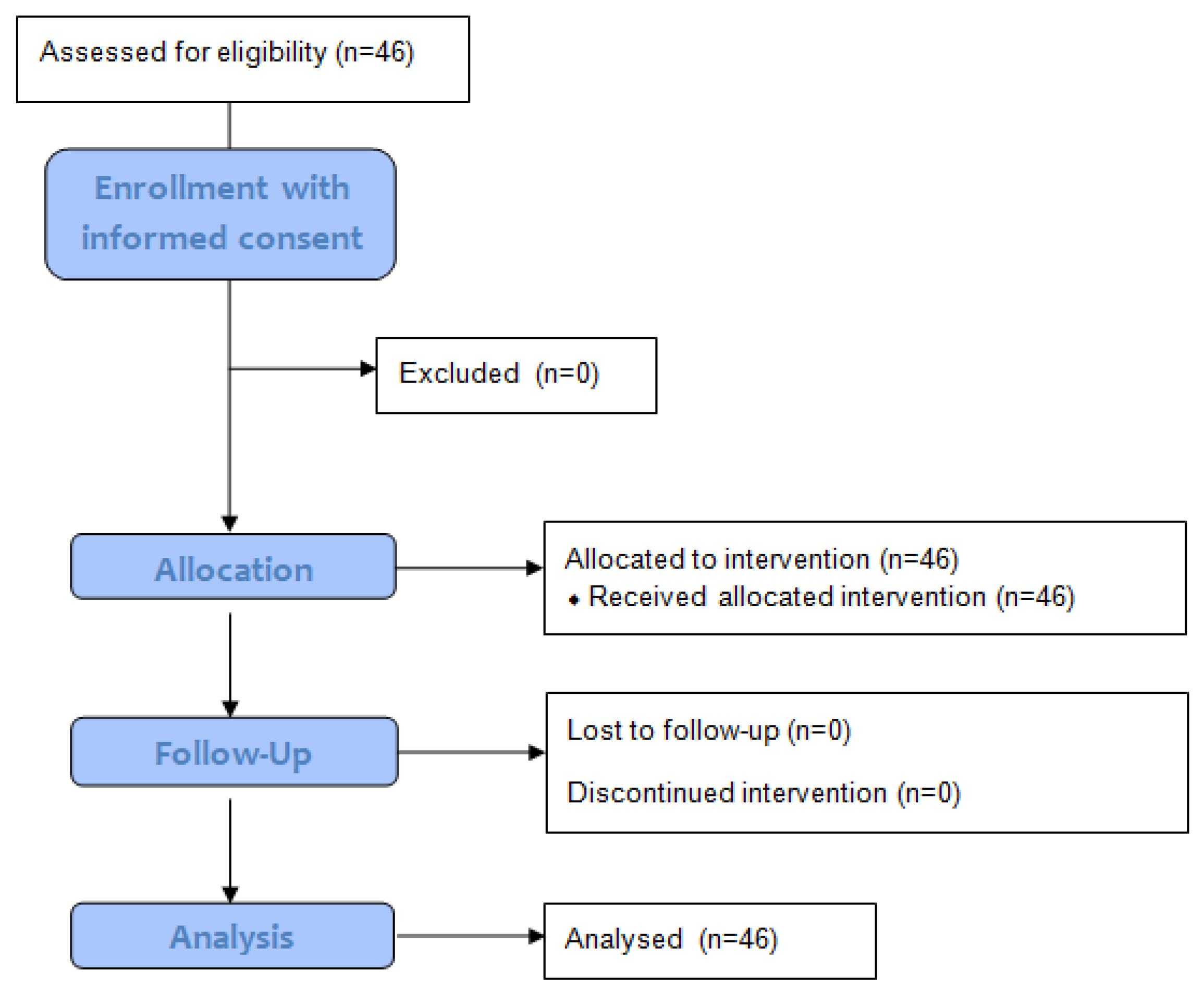
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Tiktinsky, R.; Chen, L.; Narayan, P. Electrotherapy: Yesterday, today and tomorrow. Haemophilia 2010, 16, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Watson, T. The role of electrotherapy in contemporary physiotherapy practice. Man. Ther. 2000, 5, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Ciubean, A.D.; Ungur, R.A.; Irsay, L.; Ciortea, V.M.; Borda, I.M.; Dogaru, G.B.; Trifa, A.P.; Vesa, S.C.; Buzoianu, A.D. Polymorphisms of FDPS, LRP5, SOST and VKORC1 Genes and Their Relation with Osteoporosis in Postmenopausal Romanian Women. PLoS ONE 2019, 14, e0225776. [Google Scholar] [CrossRef] [PubMed]
- Eleazu, I.C.; Jones-O’Connor, M.; Honigberg, M.C. The Impact of Premature Menopause on Future Risk of Cardiovascular Disease. Curr. Treat. Options Cardiovasc. Med. 2020, 22, 77. [Google Scholar] [CrossRef]
- Bjordal, J.M.; Johnson, M.I.; Lopes-Martins, R.A.; Bogen, B.; Chow, R.; Ljunggren, A.E. Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials. BMC Musculoskelet. Disord. 2007, 8, 51. [Google Scholar] [CrossRef] [PubMed]
- Conaghan, P.G.; Dickson, J.; Grant, R.L. Care and management of osteoarthritis in adults: Summary of NICE guidance. BMJ 2008, 336, 502–503. [Google Scholar] [CrossRef] [PubMed]
- March, L.; Amatya, B.; Osborne, R.H.; Brand, C. Developing a minimum standard of care for treating people with osteoarthritis of the hip and knee. Best Pr. Res. Clin. Rheumatol. 2010, 24, 121–145. [Google Scholar] [CrossRef]
- McAlindon, T.E.; Bannuru, R.; Sullivan, M.C.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.M.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef]
- Osiri, M.; Welch, V.; Brosseau, L.; Shea, B.; McGowan, J.L.; Tugwell, P.; Wells, G.A. Transcutaneous electrical nerve stimulation for knee osteoarthritis. Cochrane Database Syst. Rev. 2000, 4, CD002823. [Google Scholar] [CrossRef]
- Rutjes, A.W.; Nüesch, E.; Sterchi, R.; Jüni, P. Therapeutic ultrasound for osteoarthritis of the knee or hip. Cochrane Database Syst. Rev. 2010, 1, CD003132. [Google Scholar] [CrossRef]
- Ungur, R.; Dronca, M.; Crăciun, E.C.; Rusu, R.; Văleanu, M.; Onac, I.; Borda, I.M.; Irsay, L. Improvement of total antioxidant status, a possible bioeffect of the ultrasound therapy-a pilot study. Rev. Romana Med. Lab. 2011, 19, 177–183. [Google Scholar]
- S˘varcova, J.; Trnavský, K.; Zvarova, J. The influence of ultrasound, galvanic currents and shortwave diathermy on pain intensity in patients with osteoarthritis. Scand. J. Rheumatol. 1988, 17, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Alfredo, P.P.; Bjordal, J.M.; Dreyer, S.H.; Meneses, S.R.; Zaguetti, G.; Ovanessian, V.; Fukuda, T.Y.; Steagall, W., Jr.; Martins, R.Á.B.L.; Casarotto, R.A.; et al. Efficacy of low level laser therapy associated with exercises in knee osteoarthritis: A randomized double-blind study. Clin. Rehabil. 2012, 26, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Bruce-Brand, R.A.; Walls, R.J.; Ong, J.C.; Emerson, B.S.; O’Byrne, J.M.; Moyna, N.M. Effects of home-based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: A randomized controlled trial. BMC Musculoskelet. Disord. 2012, 13, 118. [Google Scholar] [CrossRef] [PubMed]
- Atamaz, F.C.; Durmaz, B.; Baydar, M.; Demircioglu, O.Y.; Iyiyapici, A.; Kuran, B.; Oncel, S.; Sendur, O.F. Comparison of the efficacy of transcutaneous electrical nerve stimulation, interferential currents, and shortwave diathermy in knee osteoarthritis: A double-blind, randomized, controlled, multicenter study. Arch. Phys. Med. Rehabil. 2012, 93, 748–756. [Google Scholar] [CrossRef]
- Ungur, R.A.; Florea, A.; Tăbăran, A.F.; Scurtu, I.C.; Onac, I.; Borda, I.M.; Irsay, L.; Ciortea, V.M.; Dronca, E.; Zdrenghea, M.T.; et al. Chondroprotective effects of pulsed shortwave therapy in rabbits with experimental osteoarthritis. Rom. J. Morphol. Embryol. 2017, 58, 465–472. [Google Scholar]
- Ioan, O.N.; Singureanu, V.; Moldovan, G.; Ungur, R. High frequency pulsatile electromagnetic fields and ultrasound pulsatile fields impact on germination dynamic at Ocimum basilicum L. and O. basilicum var. purpurascens benth., observed with open source software. Not. Bot. Horti Agrobot. Cluj-Napoca 2016, 14, 41–47. [Google Scholar]
- Csermely, M. Electroterápia. In A Fizioterápia Kézikönyve; White Golden Book: Budapest, Hungary, 2004; pp. 108–123. [Google Scholar]
- Hingorani, P.; Karnad, D.R.; Rohekar, P.; Kerkar, V.; Lokhandwala, Y.Y.; Kothari, S. Arrhythmias seen in baseline 24-hour Holter ECG recordings in healthy normal volunteers during phase 1 clinical trials. J. Clin. Pharm. 2016, 56, 885–893. [Google Scholar] [CrossRef]
- Acharya, T.; Tringali, S.; Bhullar, M.; Nalbandyan, M.; Ilineni, V.K.; Carbajal, E.; Deedwania, D. Frequent atrial premature complexes and their association with risk of atrial fibrillation. Am. J. Cardiol. 2015, 116, 1852–1857. [Google Scholar] [CrossRef]
- Conen, D.; Adam, M.; Roche, F.; Barthelemy, J.C.; Felber Dietrich, D.; Imboden, M.; Künzli, N.; von Eckardstein, A.; Regenass, S.; Hornemann, T.; et al. Premature atrial contractions in the general population: Frequency and risk factors. Circulation 2012, 126, 2302–2308. [Google Scholar] [CrossRef]
- Sideris, D.A.; Toumanidis, S.T.; Anastasiou-Nana, M.; Zakopoulos, N.; Kitsiou, A.; Tsagarakis, K.; Moulopoulos, S.D. The circadian profile of extrasystolic arrhythmia: Its relationship to heart rate and blood pressure. Int. J. Cardiol. 1992, 34, 21–31. [Google Scholar] [CrossRef]
- Man, G.S.; Mologhianu, G. Osteoarthritis pathogenesis–a complex process that involves the entire joint. J. Med. Life 2014, 7, 37. [Google Scholar] [PubMed]
- Anderson, A.S.; Loeser, R.F. Why is osteoarthritis an age-related disease? Best Pr. Res. Clin. Rheumatol. 2010, 24, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Lespasio, M.J.; Piuzzi, N.S.; Husni, M.E.; Muschler, G.F.; Guarino, A.J.; Mont, M.A. Knee osteoarthritis: A primer. Perm. J. 2017, 21, 16–183. [Google Scholar] [CrossRef]
- Ferreira, R.M.; Duarte, J.A.; Goncalves, R.S. Non-pharmacological and non-surgical interventions to manage patients with knee osteoarthritis: An umbrella review. Acta Reum. Port 2018, 43, 182–200. [Google Scholar]
- Robertson, V.J.; Ward, A.R.; Low, J.; Reed, A. Electrotherapy Explained: Principles and Practice, 4th ed.; Butterworth-Heinemann: Oxford, UK, 2006. [Google Scholar]
- Batavia, M. Contraindications in Physical Rehabilitation-Doing No Harm; Saunders Elsevier: Amsterdam, The Netherlands, 2006; Available online: https://evolve.elsevier.com/cs/product/9781455735266?role=student&CT=RO (accessed on 14 September 2022).
- Shields, N.; Gormley, J.; O’Hare, N. Contraindications to continuous and pulsed short-wave diathermy. Phys. Ther. Rev. 2002, 7, 133–143. [Google Scholar] [CrossRef]
- Batavia, M. Contraindications for superficial heat and therapeutic ultrasound: Do sources agree? Arch. Phys. Med. Rehabil. 2004, 85, 1006–1012. [Google Scholar] [CrossRef]
- Drca, N.; Wolk, A.; Jensen-Urstad, M.; Larsson, S.C. Atrial fibrillation is associated with different levels of physical activity levels at different ages in men. Heart 2014, 100, 1037–1042. [Google Scholar] [CrossRef]
- Drca, N.; Wolk, A.; Jensen-Urstad, M.; Larsson, S.C. Physical activity is associated with a reduced risk of atrial fibrillation in middle-aged and elderly women. Heart 2015, 101, 1627–1630. [Google Scholar] [CrossRef]
- Iliescu, M.G.; Ionescu, E.V.; Tica, I.; Prazaru, M.D.; Popa, F.L.; Popescu, M.N.; Berteanu, M.; Irsay, L.; Ciortea, V.M.; Voinea, F.; et al. The role of natural biotherapeutic factors in pain and functional management of knee osteoarthritis. Farmacia 2022, 70, 65–69. [Google Scholar] [CrossRef]
| n = 46 | ||
| Age (years) | Mean | Median |
| 62.7 (95% CI [59.25–66.05] | 66 | |
| Sex | Female | Male |
| n = 33 | n = 13 | |
| Ischemic cardiac disease | Present | Not present |
| n = 19 | n = 27 | |
| Extrasystolic Arrhythmia | Present | Not present |
| n = 20 | n = 26 | |
| Extrasystoles (n = 46) | Mean (95% CI) | Median | p-Value * | |
|---|---|---|---|---|
| Number of ventricular extraystoles/24 h | Day 1 | 35.17 [9.6–60.75] | 3 | 0.974 |
| Day 2 | 38.9 [3.68–72.5] | 3.5 | ||
| Number of supraventricular extrasystoles/24 h | Day 1 | 91.7 [51.69–131.7] | 36 | 0.642 |
| Day 2 | 110.48 [48.59–172.36] | 29.5 | ||
| Number of total extrasystoles/24 h | Day 1 | 126.87 [76.63–177.11] | 55 | 0.407 |
| Day 2 | 148.57 [75.57–221.56] | 41 | ||
| Heart Rate/Minute (n = 46) | Median | p-Value * | |
|---|---|---|---|
| Minimal | Day 1 | 49 [44–53.5] | 0.969 |
| Day 2 | 50 [45–53.75] | ||
| Average | Day 1 | 67 [59–75] | 0.599 |
| Day 2 | 68 [61.25–72] | ||
| Maximal | Day 1 | 114 [100.5–136] | 0.729 |
| Day 2 | 115 [101.75] | ||
| n = 46 | History of Extrasystolic Arrhythmias | History of Ischemic Heart Disease | |||||
|---|---|---|---|---|---|---|---|
| Negative (n = 26) | Negative (n = 27) | ||||||
| Mean (95% CI) | Median | p-Value | Mean (95% CI) | Median | p-Value | ||
| Number of ventricular extrasystoles/24 h | Day 1 | 26.46 [−4.82–57.74] | 1 | 0.395 | 34.3 [−1.18–69.78] | 3 | 0.576 |
| Day 2 | 13.58 [0.49–26.66] | 1.5 | 44.52 [−11.69–100.73] | 3 | |||
| Number of supraventricular extrasystoles/24 h | Day 1 | 51.35 [23.87–78.83] | 30 | 0.989 | 63.41 [22.01–104.8] | 12 | 0.731 |
| Day 2 | 45.31 [21.12–69.5] | 23.5 | 67.33 [1.68–132.99] | 29 | |||
| Number of total extrasystoles/24 h | Day 1 | 77.81 [32.91–122.7] | 36 | 0.426 | 97.7 [39.19–156.22] | 36 | 0.475 |
| Day 2 | 58.88 [28.78–88.99] | 27.5 | 111.85 [21.45–202.25] | 37 | |||
| Positive (n = 20) | Positive (n = 19) | ||||||
| Number of ventricular extrasystoles/24 h | Day 1 | 46.5 [1.05–91.95] | 6 | 0.393 | 36.42 [−3.66–76.5] | 5 | 0.489 |
| Day 2 | 69.95 [−9.09–148.99] | 20.5 | 28.95 [−2.46–60.36] | 8 | |||
| Number of supraventricular extrasystoles/24 h | Day 1 | 144.15 [60.73–227.57] | 45.5 | 0.528 | 131.89 [53.21–210.58] | 56 | 0.546 |
| Day 2 | 195.2 [58.94–331.46] | 44 | 171.79 [51.76–291.82] | 77 | |||
| Number of total extrasystoles/24 h | Day 1 | 190.65 [92.54–288.76] | 74 | 0.061 | 168.32 [75.79–260.84] | 62 | 0.494 |
| Day 2 | 265.15 [109.6–420.7] | 88 | 200.74 [72.57–328.91] | 85 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Irsay, L.; Ungur, R.A.; Borda, I.M.; Tica, I.; Iliescu, M.G.; Ciubean, A.D.; Popa, T.; Cinteza, D.; Popa, F.L.; Bondor, C.I.; et al. Safety of Electrotherapy Treatment in Patients with Knee Osteoarthritis and Cardiac Diseases. Life 2022, 12, 1690. https://doi.org/10.3390/life12111690
Irsay L, Ungur RA, Borda IM, Tica I, Iliescu MG, Ciubean AD, Popa T, Cinteza D, Popa FL, Bondor CI, et al. Safety of Electrotherapy Treatment in Patients with Knee Osteoarthritis and Cardiac Diseases. Life. 2022; 12(11):1690. https://doi.org/10.3390/life12111690
Chicago/Turabian StyleIrsay, Laszlo, Rodica Ana Ungur, Ileana Monica Borda, Irina Tica, Mădălina Gabriela Iliescu, Alina Deniza Ciubean, Theodor Popa, Delia Cinteza, Florina Ligia Popa, Cosmina Ioana Bondor, and et al. 2022. "Safety of Electrotherapy Treatment in Patients with Knee Osteoarthritis and Cardiac Diseases" Life 12, no. 11: 1690. https://doi.org/10.3390/life12111690
APA StyleIrsay, L., Ungur, R. A., Borda, I. M., Tica, I., Iliescu, M. G., Ciubean, A. D., Popa, T., Cinteza, D., Popa, F. L., Bondor, C. I., & Ciortea, V. M. (2022). Safety of Electrotherapy Treatment in Patients with Knee Osteoarthritis and Cardiac Diseases. Life, 12(11), 1690. https://doi.org/10.3390/life12111690









