Computed Tomography Angiography (CTA) in Selected Scenarios with Risk of Possible False-Positive or False-Negative Conclusions in Diagnosing Brain Death
Abstract
1. Introduction
2. Ancillary Tests for Determination of Cerebral Blood Perfusion Arrest
3. CTA-Diagnosing Management for BD Determination
- Compared to DSA, Zampakis et al. [44] found no statistically significant difference between all CTA -4-point scores and in general, the 4-point CTA scoring system has been accepted as the most reliable scoring among other CTA scoring systems in the diagnosis of BD. However, some challenges still exist [46]. For completeness, it should be noted that there are different versions of the 4-point score [44]: the 4-point scale introduced by Frampas et al. [38] (the so-called CTA-F (by this score only the M4 branches of the middle cerebral artery and the internal cerebral vein are assessed);
- The revised 4-point scale suggested by Nunes and co-workers [47] (the so-called CTA-MF) and
- The prior revised venous 4-point scale, proposed by Marchand and colleagues [48] (the so-called CTA-M).
4. The Role of Computed Tomography Perfusion (CTP) as Adjunct in Diagnosing BD
5. General Considerations to Secure the Informative Value of CTA/CTP
6. Cerebral Perfusion Test as Diagnosing Option in False-Negative Ventilation Patterns
7. Cerebral Perfusion Tests in Case of Possible False-Positive Findings Caused by Central Nervous System (CNS) Depressant Drugs
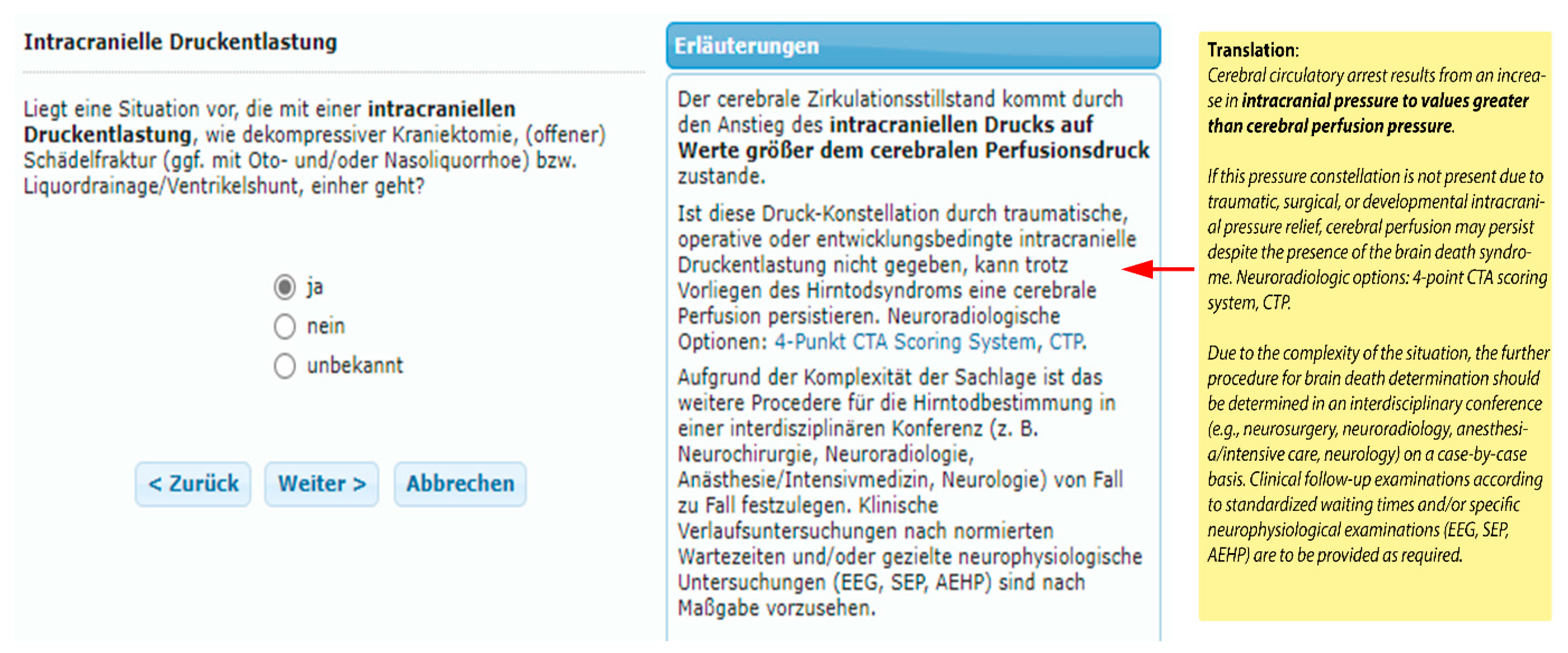
8. CTA and CTP as Contents of an Expert-System Based Training Tool for Diagnosing BD
Example of BRAINDEXweb-Workflow in the Context with False-Negative CTA-Signs Caused by Decreased Intracranial Pressure (ICP) in Suspected BD
9. Cerebral Perfusion Test as Diagnosing Option in Case of False-Negative Movement Patterns
10. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Greer, D.M.; Shemie, S.D.; Lewis, A.; Torrance, S.; Varelas, P.; Goldenberg, F.D.; Bernat, J.L.; Souter, M.; Topcuoglu, M.A.; Alexandrov, A.W.; et al. Determination of Brain Death/Death by Neurologic Criteria: The World Brain Death Project. JAMA J. Am. Med. Assoc. 2020, 324, 1078–1097. [Google Scholar] [CrossRef]
- Spears, W.; Mian, A.; Greer, D. Brain death: A clinical overview. J. Intensive Care 2022, 10, 16. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.; Wolfer, H.; Hendrickson, R.G. Toxicologic confounders of brain death determination: A narrative review. Neurocrit Care 2021, 34, 1072–1089. [Google Scholar] [CrossRef]
- Arbour, R.B. Brain death: Assessment, controversy, and confounding factors. Crit. Care Nurse 2013, 33, 27–46. [Google Scholar] [CrossRef]
- Vargas, F.; Hilbert, G.; Gruson, D.; Valentino, R.; Gbikpi-Benissan, G.; Cardinaud, J.P. Fulminant Guillain-Barré syndrome mimicking cerebral death: Case report and literature review. Intensive Care Med. 2000, 26, 623–627. [Google Scholar] [CrossRef]
- Liik, M.; Puksa, L.; Lüüs, S.; Haldre, S.; Taba, P. Unusual presentation of more common disease/injury: Fulminant inflammatory neuropathy mimicking cerebral death. BMJ Case Rep. 2012, 2012, bcr1020114906. [Google Scholar] [CrossRef] [PubMed]
- Waters, C.E.; French, G.; Burt, M. Difficulty in brainstem death testing in the presence of high spinal cord injury. Br. J. Anaesth. 2004, 92, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Joffe, A.R.; Anton, N.; Blackwood, J. Brain death and the cervical spinal cord: A confounding factor for the clinical examination. Spinal Cord 2010, 48, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.; Hodgman, M.J.; Kao, L.; Tormoehlen, L.M. Baclofen overdose mimicking brain death. Clin. Toxicol. 2012, 50, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Richard, I.H.; LaPointe, M.; Wax, P.; Risher, W. Non-barbiturate, drug-induced reversible loss of brainstem reflexes. Neurology 1998, 51, 639–640. [Google Scholar] [CrossRef] [PubMed]
- Kainuma, M.; Miyake, T.; Kanno, T. Extremely prolonged vecuronium clearance in a brain death case. J. Am. Soc. Anesthesiol. 2001, 95, 1023–1024. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.L.; Dantzker, D.R. Reversible brain death: A manifestation of amitriptyline overdose. Chest 1991, 99, 1037–1038. [Google Scholar] [CrossRef][Green Version]
- Peter, J.V.; Prabhakar, A.T.; Pichamuthu, K. In-laws, insecticide—and a mimic of brain death. Lancet 2008, 371, 622. [Google Scholar] [CrossRef]
- John, J.; Gane, B.D.; Plakkal, N.; Aghoram, R.; Sampath, S. Snake bite mimicking brain death. Cases J. 2008, 1, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Wijdicks, E.F.M.; Varelas, P.N.; Gronseth, G.S.; Greer, D.M. Evidence-based guideline update: Determining brain death in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2010, 74, 1911–1918. [Google Scholar] [CrossRef]
- Wijdicks, E.F.M. Pitfalls and slip-ups in brain death determination. Neurol. Res. 2013, 35, 169–173. [Google Scholar] [CrossRef]
- Schwarz, G.; Errath, M.; Arguelles Delgado, P.; Schöpfer, A.; Cavic, T. Ventilator autotriggering. Anaesthesist 2019, 68, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Henry, N.R.; Russian, C.J.; Nespral, J. Identifying potential ventilator auto-triggering among organ procurement organization referrals. Prog. Transplant. 2016, 26, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Arbour, R.B. Confounding factors in brain death: Cardiogenic ventilator autotriggering and implications for organ transplantation. Intensive Crit. Care Nurs. 2012, 28, 321–328. [Google Scholar] [CrossRef]
- Beckmann, Y.; Çiftçi, Y.; İncesu, T.K.; Seçil, Y.; Akhan, G. Spinal reflexes in brain death. Acta Neurol. Belg. 2014, 114, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, G. Dissoziierter Hirntod: Computergestützte Verfahren in Diagnostik und Dokumentation; Springer: Berlin/Heidelberg, Germany, 1990; pp. 15–22. [Google Scholar]
- Saposnik, G.; Bueri, J.A.; Mauriño, J.; Saizar, R.; Garretto, N.S. Spontaneous and reflex movements in brain death. Neurology 2000, 54, 221. [Google Scholar] [CrossRef] [PubMed]
- Sayan, H.E. Retrospective analysis of the apnea test and ancillary test in determining brain death. Rev. Bras. Ter. Intensiva 2020, 32, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Lustbader, D.; O’Hara, D.; Wijdicks, E.F.M.; MacLean, L.; Tajik, W.; Ying, A.; Berg, E.; Goldstein, M. Second brain death examination may negatively affect organ donation. Neurology 2011, 76, 119–124. [Google Scholar] [CrossRef]
- Citerio, G.; Crippa, I.A.; Bronco, A.; Vargiolu, A.; Smith, M. Variability in brain death determination in Europe: Looking for a solution. Neurocrit. Care 2014, 21, 376–382. [Google Scholar] [CrossRef]
- ÖBIG/OSR Empfehlungen zur Durchführung der Hirntoddiagnostik bei Einer Geplanten Organentnahme. Available online: https://transplant.goeg.at/sites/transplant.goeg.at/files/2017-06/Empfehlungen%20zur%20Durchf%C3%BChrung%20der%20Hirntoddiagnostik%20bei%20einer%20geplanten%20Organentnahme%20inkl.%20Protokoll.pdf (accessed on 13 July 2022).
- SAMW Feststellung des Todes im Hinblick auf Organtransplantationen und Vorbereitung der Organentnahme. Available online: https://www.samw.ch/dam/jcr:4a69851d-bd05-49b3-a209-3ce28d66372e/richtlinien_samw_feststellung_tod_organentnahme.pdf (accessed on 23 August 2022).
- Bundesärztekammer Richtlinie gemäß § 16 Abs. 1 S. 1 Nr. 1 TPG für die Regeln zur Feststellung des Todes nach § 3 Abs. 1 S. 1 Nr. 2 TPG und die Verfahrensregeln zur Feststellung des endgültigen, nicht behebbaren Ausfalls der Gesamtfunktion des Großhirns, des Kleinhirns und des Hirnstamms nach § 3 Abs. 2 Nr. 2 TPG, Vierte Fortschreibung. Dtsch. Ärzteblatt 2015, 31, 1. [CrossRef]
- Bohatyrewicz, R.; Pastuszka, J.; Walas, W.; Chamier-Cieminska, K.; Poncyljusz, W.; Dabrowski, W.; Wojczal, J.; Luchowski, P.; Guzinski, M.; Jurkiewicz, E.; et al. Implementation of Computed Tomography Angiography (CTA) and Computed Tomography Perfusion (CTP) in Polish Guidelines for Determination of Cerebral Circulatory Arrest (CCA) during Brain Death/Death by Neurological Criteria (BD/DNC) Diagnosis Procedure. J. Clin. Med. 2021, 10, 4237. [Google Scholar] [CrossRef]
- Sawicki, M.; Sołek-Pastuszka, J.; Chamier-Ciemińska, K.; Walecka, A.; Bohatyrewicz, R. Accuracy of computed tomographic perfusion in diagnosis of brain death: A prospective cohort study. Med. Sci. Monit. 2018, 24, 2777–2785. [Google Scholar] [CrossRef]
- MacDonald, D.; Stewart-Perrin, B.; Shankar, J.J.S. The Role of Neuroimaging in the Determination of Brain Death. J. Neuroimaging 2018, 28, 374–379. [Google Scholar] [CrossRef]
- Donohoe, K.J.; Agrawal, G.; Frey, K.A.; Gerbaudo, V.H.; Mariani, G.; Nagel, J.S.; Shulkin, B.L.; Stabin, M.G.; Stokes, M.K. SNM practice guideline for brain death scintigraphy 2.0. J. Nucl. Med. Technol. 2012, 40, 198–203. [Google Scholar] [CrossRef]
- Sürücü, E.; Aslan, M.; Demir, Y.; Durak, H. Brain Scintigraphy in Brain Death: The Experience of Nuclear Medicine Department in Dokuz Eylul University, School of Medicine. East. J. Med. 2014, 19, 66–70. Available online: https://dergipark.org.tr/en/pub/ejm/issue/5368 (accessed on 21 May 2022).
- Ande, R.S.; Shankar, S.J.J. Ancillary Imaging Tests for Confirmation of Brain Death; Dogan, K.H., Ed.; IntechOpen: London, UK, 2019. [Google Scholar]
- Sohn, C.; Lee, H.; Park, J.B.; Chang, H.W.; Kim, E.; Kim, E.; Park, U.J.; Kim, H.; Ku, J. Imaging findings of brain death on 3-tesla MRI. Korean J. Radiol. 2012, 13, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, M.; Bohatyrewicz, R.; Walecka, A.; Sołek-Pastuszka, J.; Rowiński, O.; Walecki, J. CT angiography in the diagnosis of brain death. Pol. J. Radiol. 2014, 79, 417. [Google Scholar] [CrossRef] [PubMed]
- Bundesärztekammer, W.B. Richtlinien zur Feststellung des Hirntodes. Dtsch. Ärzteblatt 1998, 95, 53. [Google Scholar]
- Frampas, E.; Videcoq, M.; De Kerviler, E.; Ricolfi, F.; Kuoch, V.; Mourey, F.; Tenaillon, A.; Dupas, B. CT angiography for brain death diagnosis. Am. J. Neuroradiol. 2009, 30, 1566–1570. [Google Scholar] [CrossRef]
- Welschehold, S.; Kerz, T.; Boor, S.; Reuland, K.; Thömke, F.; Reuland, A.; Beyer, C.; Wagner, W.; Müller-Forell, W.; Giese, A. Detection of intracranial circulatory arrest in brain death using cranial CT-angiography. Eur. J. Neurol. 2013, 20, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Lanfermann, H.; Götz, F.; Raab, P. Einsatz der CT-Angiographie zur Feststellung des zerebralen Zirkulationsstillstandes. Clin Neuroradiol 2015, 25, 329–333. [Google Scholar] [CrossRef]
- Garrett, M.P.; Williamson, R.W.; Bohl, M.A.; Bird, C.R.; Theodore, N. Computed tomography angiography as a confirmatory test for the diagnosis of brain death. J. Neurosurg. 2018, 128, 639–644. [Google Scholar] [CrossRef]
- Brasil, S.; Bor-Seng-Shu, E.; de-Lima-Oliveira, M.; Azevedo, M.K.; Teixeira, M.J.; Bernardo, L.; Bernardo, W.M. Role of computed tomography angiography and perfusion tomography in diagnosing brain death: A systematic review. J. Neuroradiol. 2015, 43, 133–140. [Google Scholar] [CrossRef]
- Sahin, H.; Pekcevik, Y. CT angiography as a confirmatory test in diagnosis of brain death: Comparison between three scoring systems. Diagn. Interv. Radiol. 2015, 21, 177–183. [Google Scholar] [CrossRef]
- Zampakis, P.; Panagiotopoulos, V.; Kalogeropoulou, C.; Karachaliou, M.; Aretha, D.; Sioulas, N.; Dimoulia, S.; Karnabatidis, D.; Fligou, F. Computed tomography angiography scoring systems and the role of skull defects in the confirmation of brain death. Sci. Rep. 2021, 11, 15081. [Google Scholar] [CrossRef]
- Kricheff, I.I.; Pinto, R.S.; George, A.E.; Braunstein, P.; Korein, J. ANGIOGRAPHIC FINDINGS IN BRAIN DEATH. Ann. N. Y. Acad. Sci. 1978, 315, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Akdogan, A.I.; Pekcevik, Y.; Sahin, H.; Pekcevik, R. Assessment of Cerebral Circulatory Arrest via CT Angiography and CT Perfusion in Brain Death Confirmation. Korean J. Radiol. 2021, 22, 395–404. [Google Scholar] [CrossRef]
- Nunes, D.M.; Maia, A.C.M., Jr.; Boni, R.C.; da Rocha, A.J. Impact of Skull Defects on the Role of CTA for Brain Death Confirmation. Am. J. Neuroradiol. AJNR 2019, 40, 1177–1183. [Google Scholar] [CrossRef]
- Marchand, A.J.; Seguin, P.; Malledant, Y.; Taleb, M.; Raoult, H.; Gauvrit, J.Y. Revised CT angiography venous score with consideration of infratentorial circulation value for diagnosing brain death. Ann. Intensive Care 2016, 6, 88. [Google Scholar] [CrossRef] [PubMed]
- Taylor, T.; Dineen, R.A.; Gardiner, D.C.; Buss, C.H.; Howatson, A.; Pace, N.L.; Taylor, T. Computed tomography (CT) angiography for confirmation of the clinical diagnosis of brain death. Cochrane Database Syst. Rev. 2014, 2018, CD009694. [Google Scholar] [CrossRef]
- Shankar, J.J.S.; Vandorpe, R. CT perfusion for confirmation of brain death. Am. J. Neuroradiol. AJNR 2013, 34, 1175–1179. [Google Scholar] [CrossRef]
- Heran, M.K.S.; Heran, N.S.; Shemie, S.D. A review of ancillary tests in evaluating brain death. Can. J. Neurol. Sci. 2008, 35, 409–419. [Google Scholar] [CrossRef]
- Kerhuel, L.; Srairi, M.; Georget, G.; Bonneville, F.; Mrozek, S.; Mayeur, N.; Lonjaret, L.; Sacrista, S.; Hermant, N.; Marhar, F.; et al. The Optimal Time between Clinical Brain Death Diagnosis and Confirmation Using CT Angiography: A Retrospective Study. Minerva Anestesiol. 2016, 82, 1180–1188. Available online: https://pubmed.ncbi.nlm.nih.gov/27625121/ (accessed on 26 May 2022).
- Bohatyrewicz, R.; Walecka, A.; Bohatyrewicz, A.; Zukowski, M.; Kępiński, S.; Marzec-Lewenstein, E.; Sawicki, M.; Kordowski, J. Unusual Movements,“Spontaneous” Breathing, and Unclear Cerebral Vessels Sonography in a Brain-Dead Patient: A Case Report; Transplantation Proceedings; Elsevier: New York, NY, USA, 2007; Volume 39, pp. 2707–2708. [Google Scholar]
- Wijdicks, E.F. 10 questions about the clinical determination of brain death. Neurologist 2007, 13, 380–381. [Google Scholar] [CrossRef]
- Sherrington, A.; Smith, M. International perspectives in the diagnosis of brain death in adults. Trends Anaesth. Crit. Care 2012, 2, 48–52. [Google Scholar] [CrossRef]
- López-Navidad, A.; Caballero, F.; Domingo, P.; Marruecos, L.; Estorch, M.; Kulisevsky, J.; Mora, J. Early Diagnosis of Brain Death in Patients Treated with Central Nervous System Depressant Drugs. Transplantation 2000, 70, 131–135. Available online: https://journals.lww.com/transplantjournal/Fulltext/2000/07150/RENAL_TRANSPLANTATION_WITH_LIMIT_DONORS__To_What.26.aspx (accessed on 12 February 2022). [PubMed]
- Kruse, W.H. Problems and pitfalls in the use of benzodiazepines in the elderly. Drug Saf. 1990, 5, 328–344. [Google Scholar] [CrossRef] [PubMed]
- Pelkonen, O.; Mäeenpäeä, J.; Taavitsainen, P.; Rautio, A.; Raunio, H. Inhibition and induction of human cytochrome P450 (CYP) enzymes. Xenobiotica 1998, 28, 1203–1253. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.D.; Mogali, S.; Comer, S.D. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012, 125, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Hirata, K.; Matsumoto, Y.; Kurokawa, A.; Onda, M.; Shimizu, M.; Fukuoka, M.; Hirano, M.; Yamamoto, Y. Possibility of Influence of Midazolam Sedation on the Diagnosis of Brain Death: Concentrations of Active Metabolites after Cessation of Midazolam. Yakugaku Zasshi 2003, 123, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Meinitzer, A.; Zink, M.; März, W.; Baumgartner, A.; Halwachs-Baumann, G. Midazolam and its metabolites in brain death diagnosis. Int. J. Clin. Pharmacol. Ther. 2005, 43, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Spivey, W.H. Flumazenil and seizures: Analysis of 43 cases. Clin. Ther. 1992, 14, 292–305. [Google Scholar] [PubMed]
- Chiolero, R.L.; Ravussin, P.; Anderes, J.P.; Ledermann, P.; de Tribolet, N. The effects of midazolam reversal by Ro 15-1788 on cerebral perfusion pressure in patients with severe head injury. Intensive Care Med. 1988, 14, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Seger, D.L. Flumazenil-Treatment or Toxin. J. Toxicol. Clin. Toxicol. 2004, 42, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Kamijo, Y.; Masuda, T.; Nishikawa, T.; Tsuruta, H.; Ohwada, T. Cardiovascular response and stress reaction to flumazenil injection in patients under infusion with midazolam. Crit. Care Med. 2000, 28, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Soleimanpour, H.; Ziapour, B.; Negargar, S.; Taghizadieh, A.; Shadvar, K. Ventricular tachycardia due to flumazenil administration. Pak. J. Biol. Sci. PJBS 2010, 13, 1161–1163. [Google Scholar] [CrossRef][Green Version]
- Academy of Medical Royal Colleges. A Code of Practice for the Diagnosis and Confirmation of Death. Available online: https://www.aomrc.org.uk/wp-content/uploads/2016/04/Code_Practice_Confirmation_Diagnosis_Death_1008-4.pdf (accessed on 13 July 2022).
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Real Decreto 1723/2012, de 28 de Diciembre, por el que se Regulan las Actividades de Obtención, Utilización Clínica y Coordinación Territorial de los Órganos Humanos Destinados al Trasplante y se Establecen Requisitos de Calidad y Seguridad. Available online: https://www.boe.es/eli/es/rd/2012/12/28/1723 (accessed on 13 July 2022).
- NLM-DailyMed Flumazenil Injection. Available online: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8175c1eb-80af-48f1-813c-c8f0e736d894 (accessed on 13 July 2022).
- Park, G.R. Editorial I: Death and its diagnosis by doctors. Br. J. Anaesth. 2004, 92, 625–628. [Google Scholar] [CrossRef][Green Version]
- Elliot, J. Brain death. Trauma 2003, 5, 23–42. [Google Scholar] [CrossRef]
- Johnston, A.J.; Matta, B.F. Brainstem death. Surgery 2007, 25, 134–137. [Google Scholar] [CrossRef]
- Machado, C. Diagnosis of brain death. Neurol. Int. 2010, 2, e2. [Google Scholar] [CrossRef] [PubMed]
- Oram, J.; Murphy, P. Diagnosis of death. Contin. Educ. Anaesth. Crit. Care Pain 2011, 11, 77–81. [Google Scholar] [CrossRef]
- Bosnell, R.; Madder, H. Concepts of brain death. Surgery 2011, 29, 289–294. [Google Scholar] [CrossRef]
- O’Sullivan, F.; Miles, B. Brainstem death. Anaesth. Intensive Care Med. 2012, 13, 249–251. [Google Scholar] [CrossRef]
- Bodenham, A.; Park, G.R. Care of the multiple organ donor. Intensive Care Med. 1989, 15, 340–348. [Google Scholar] [CrossRef]
- Hallbach, J.; von Meyer, L.; Maurer, H.H. Empfehlungen des Arbeitskreises Klinische Toxikologie der Gesellschaft für Toxikologische und Forensische Chemie (GTFCh) für die toxikologische Analytik im Rahmen der Hirntod-Feststellung. Toxichem Krimtech 2002, 69, 124–127. Available online: https://orion.gtfch.org/cms/images/stories/media/tk/tk69_3/Hallbach.pdf (accessed on 30 March 2022).
- Ghoshal, S.; Greer, D.M. Why is diagnosing brain death so confusing? Curr. Opin. Crit. Care 2015, 21, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Bartscher, J.F.; Varelas, P.N. Determining brain death: No room for error. AMA J. Ethics 2010, 12, 879–884. [Google Scholar] [CrossRef]
- Field, D.; Wee, B. Preparation for palliative care: Teaching about death, dying and bereavement in UK medical schools 2000–2001. Med. Educ. 2002, 36, 561–567. [Google Scholar] [CrossRef]
- Da Silva, I.R.F.; Frontera, J.A. Worldwide barriers to organ donation. JAMA Neurol. 2015, 72, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Pfurtscheller, G.; Schwarz, G.; Moik, H.; Haase, V. Braindex--an expert system for the diagnosis of brain death. Biomed. Technik. Biomed. Eng. 1989, 34, 3–8. [Google Scholar] [CrossRef]
- Schwarz, G.; Pfurtscheller, G.; Litscher, G.; Grims, R.; Rom, G.; Rumpl, E.; Seitlinger, H.; Fuchs, G. Computer controlled brain death documentation in the intensive care unit. Anaesthesist 1993, 42, 793–799. [Google Scholar]
- Jain, S.; DeGeorgia, M. Brain Death-Associated Reflexes and Automatisms. Neurocrit. Care 2005, 3, 122–126. [Google Scholar] [CrossRef]
- Rady, M.Y.; Verheijde, J.L. Movements after the clinical diagnosis of brain death: Supraspinal motor responses or spinal reflexes. Crit. Care 2013, 17, 469. [Google Scholar] [CrossRef]
- Ramachandran, S.; Venkatesh, H.; Foley, R.W. How should we use imaging in the determination of brainstem death? BJR Open 2018, 1, 20180013. [Google Scholar] [CrossRef]
- Urasaki, E.; Tokimura, T.; Kumai, J.; Wada, S.; Yokota, A. Preserved spinal dorsal horn potentials in a brain-dead patient with Lazarus’ sign. Case report. J. Neurosurg. 1992, 76, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Döşemeci, L.; Cengiz, M.; Yılmaz, M.; Ramazanoĝlu, A. Frequency of spinal reflex movements in brain-dead patients. Transplant. Proc. 2004, 36, 17–19. [Google Scholar] [CrossRef]




| Target Components | Ancillary Tests | Advantages | Disadvantages/Limitations |
|---|---|---|---|
| Cerebral bioelectrical activity | Electroencephalogram (EEG) |
|
|
| Evoked potentials: Somatory evoked potentials (SEP), Brainstem auditory evoked potentials (BAEP) |
|
| |
| Cerebral Circulation | Transcranial Doppler sonography (TCD)/Color-coded duplex sonography (CCDS) |
|
|
| Digital subtraction angiography (DSA) |
|
| |
| Computer tomography angiography (CTA) |
|
| |
| Computed tomography perfusion (CTP) |
|
| |
| Radionuclide cerebral blood perfusion imaging |
|
| |
| Magnetic resonance imaging (MRI) |
|
|
| CTA-Scoring Systems | Cerebral Arterial and Venous Vessels (Quantity of Assessed Vessels) | Total Number of Assessed Vessels | ||||||
|---|---|---|---|---|---|---|---|---|
| 10-point scoring | MCA-M4: (2) | ACA-A3: (2) | PCA-P2: (2) | BA: (1) | ICV: (2) | GCV: (1) | (-) | 10 |
| 7-point scoring | MCA-M4: (2) | ACA-A3: (2) | (-) | (-) | ICV: (2) | GCV: (1) | (-) | 7 |
| 4-point scoring (CTA-F) | MCA-M4: (2) | (-) | (-) | (-) | ICV: (2) | (-) | (-) | 4 |
| 4-point scoring (CTA-M) | (-) | (-) | (-) | (-) | (-) | GCV: (2) | SPV: (2) | 4 |
| 4-point scoring (CTA-MF) | MCA-M4: (2, a) | ICV: (2, b) | 4 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwarz, G.; Errath, M.; Argüelles Delgado, P.; Wießpeiner, U.; Voit-Augustin, H.; Grims, R.; Kaltenböck, F.; Kober, E.M.; Schöpfer, A.; Fuchs, G. Computed Tomography Angiography (CTA) in Selected Scenarios with Risk of Possible False-Positive or False-Negative Conclusions in Diagnosing Brain Death. Life 2022, 12, 1551. https://doi.org/10.3390/life12101551
Schwarz G, Errath M, Argüelles Delgado P, Wießpeiner U, Voit-Augustin H, Grims R, Kaltenböck F, Kober EM, Schöpfer A, Fuchs G. Computed Tomography Angiography (CTA) in Selected Scenarios with Risk of Possible False-Positive or False-Negative Conclusions in Diagnosing Brain Death. Life. 2022; 12(10):1551. https://doi.org/10.3390/life12101551
Chicago/Turabian StyleSchwarz, Gerhard, Maximilian Errath, Placido Argüelles Delgado, Ulrike Wießpeiner, Henrika Voit-Augustin, Robert Grims, Friedrich Kaltenböck, Eva Maria Kober, Andreas Schöpfer, and Gottfried Fuchs. 2022. "Computed Tomography Angiography (CTA) in Selected Scenarios with Risk of Possible False-Positive or False-Negative Conclusions in Diagnosing Brain Death" Life 12, no. 10: 1551. https://doi.org/10.3390/life12101551
APA StyleSchwarz, G., Errath, M., Argüelles Delgado, P., Wießpeiner, U., Voit-Augustin, H., Grims, R., Kaltenböck, F., Kober, E. M., Schöpfer, A., & Fuchs, G. (2022). Computed Tomography Angiography (CTA) in Selected Scenarios with Risk of Possible False-Positive or False-Negative Conclusions in Diagnosing Brain Death. Life, 12(10), 1551. https://doi.org/10.3390/life12101551







