1. Introduction
COVID-19 disease, secondary to SARS-CoV-2 infection, has caused a global pandemic since it was reported at the end of 2019 in China [
1]. Its high contagiousness has forced us to stop our lives and even our jobs completely for a few months and, in a more relaxed manner, with fewer restrictions afterwards. This impasse has also affected assisted reproduction techniques (ART) as the number of treatments was drastically reduced due to the unknown effect of COVID-19 on pregnancy and obstetric outcomes [
2].
In Europe, the first confirmed COVID-19 case was detected in France at the end of January [
3]. From this moment on, ART treatments began to decline in Spanish clinics as a significant proportion of our patients are of foreign origin. Soon after, the first COVID-19 case in Spain was detected in La Gomera [
4]. ART continued with this huge decline until the closure of all infertility clinics at the end of March, right after several professional societies around the world recommended to suspend infertility services [
2]. Clinics reopened in mid-May and, since then, the normal cycle rhythm has been gradually recovering.
Besides the huge impact on the ART industry, this pandemic is also a sanitary threat and thus it may affect pregnant women and their offspring. At the beginning of this pandemic, there were few data regarding the virus effects on pregnancy and thus the increased fear in starting any infertility treatment. Over the course of 2020 and 2021, more data on pregnant women with and without the infection became available [
5,
6]. It seems that the COVID-19 pandemic did not compromise ART early pregnancy outcomes in comparison to a pre-COVID time frame [
6], even though obstetric and perinatal complications were higher in COVID-positive pregnant women, in particular if they were symptomatic [
5]. However, apart from a physical threat, this pandemic has also exerted a great impact on the population’s psychological health. The lockdown period, fear of the unknown, uncertainty about when this situation will end, and worry about sick family members or friends are only examples of all the mental threats the whole population is currently experiencing.
Nowadays, it is believed that the mental health and psychological status of patients influences their ART cycle outcome, as well as pregnancy evolution in those who get pregnant, exerting its effect through the hypothalamus–pituitary–adrenal axis and sympathetic nervous system. Higher levels of stress in women undergoing ART treatments, measured by different biomarkers (cortisol, α-amylase, and norepinephrine) and standardized psychological questionnaires, have been related to lower pregnancy and live birth rates, as well as longer time to pregnancy [
7,
8,
9]. Given the high psychological load of this pandemic, we wanted to evaluate its impact on our pregnant patients’ mental health, how it progressed throughout pregnancy, and if this impact was somehow related to their final pregnancy outcome.
In addition, given the huge drop in the number of ART treatments performed during 2020, we wanted to compare our overall pregnancy rates to the ones registered in the previous year. In this manner, we would be able to assess if the COVID-19 pandemic only negatively affected the number of treatments or if it has also reduced the chances of achieving a successful pregnancy.
2. Materials and Methods
2.1. Design and Setting
This is a retrospective, multicentric, and double-arm study conducted in all IVI clinics in Spain, along with IVI Lisbon and IVI Rome.
The first arm includes data from all treatments performed from 12 February onwards in 2019 and 2020.
The election of 12 February as the start date is based on the fact that from that date onwards, all pregnancy tests were done while being more conscious of the critical situation in Italy, which led to harder sanitary and political actions regarding the pandemic.
The second arm includes data from pregnant patients whose first trimester coincided with the onset of the pandemic (February and March 2020) and who had responded to at least one of the three pregnancy follow-up surveys.
2.2. Study Procedures
Descriptive analysis of all infertility treatments (amount, type, success rates, etc.) performed between 12 February and 31 December 2020. Data from the same time period in 2019 has been taken as a control group in the comparative analysis.
Descriptive analysis of the psychological status of pregnant women whose first trimester coincided with the onset of the COVID-19 pandemic in Spain and the assessment of its impact in their final pregnancy outcome. This psychological status has been evaluated while taking into account several answers from their pregnancy follow-up surveys.
As part of our routine clinical practice, pregnant patients receive several phone calls during their pregnancy in order to ask about its evolution. Given the sanitary situation and the establishment of distance working, we substituted these phone calls for surveys sent over e-mail.
Data from all these surveys was exported and analyzed, as well as the final pregnancy outcome of all those patients who had answered to at least one of the surveys. The impact of the pandemic on the psychological status of pregnant women has been evaluated, as well as the subsequent impact of this psychological status on final pregnancy outcome. In addition, the evolution of their anxiety status throughout pregnancy and pandemic has been also assessed.
Anxiety levels were assessed using an adjusted Hamilton Scale, in which one of the 14 questions could not be evaluated as the evaluation did not occur in person [
10]. The choice of this scale was due to its standardization and worldwide validation in the absence of any salivary or serum biomarker measurement. Patients were then divided into three main categories: mild, mild to moderate, and moderate to severe anxiety. This scale was complemented with many other questions, in which variables could have directly or indirectly affected patients’ anxiety levels. These questions include: levels of concern regarding the pandemic, diet, exercise, family members affected by COVID-19, etc.
2.3. Statistical Analysis
A statistical analysis was performed using IBM SPSS 15.0.1 Statistics for Windows (SPSS Inc. Chicago, IL, USA). Quantitative variables are presented with the mean (95% confidence interval) and categorical variables with n (percentage). ANOVA and ꭓ2 tests were employed for comparisons between variables. A p-value < 0.05 was defined as statistically significant.
3. Results
3.1. Descriptive Analysis of Infertility Treatments in 2020 versus 2019
3.1.1. Types and Quantity of Infertility Treatments Performed
In 2019, a total of 23,078 embryo transfers or IUIs were performed between IVI clinics in Spain, IVI Lisbon, and IVI Rome, in contrast to the 19,261 performed in 2020. Cycle and demographic patients’ characteristics are summarized in
Table 1.
Table 2 presents a detailed descriptive analysis of these cycles regarding the type of treatment.
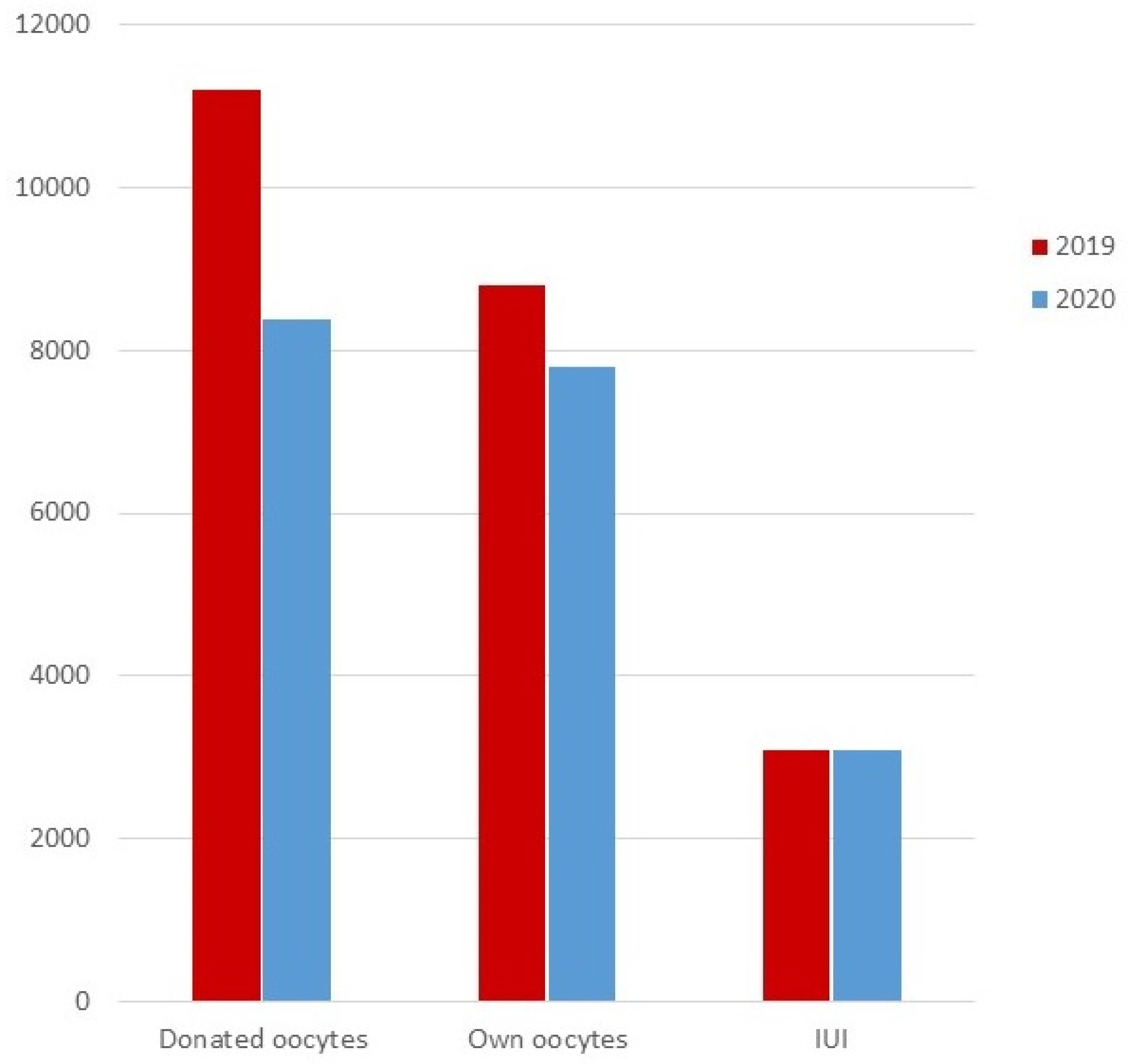
Figure 1 represents the comparison in the number of cycles performed in 2019 vs. 2020 regarding the three main categories of type of treatment (IUI and embryo transfers from own and donated oocytes).
3.1.2. Timeline of the Amount of Infertility Treatments Performed in 2020 versus 2019
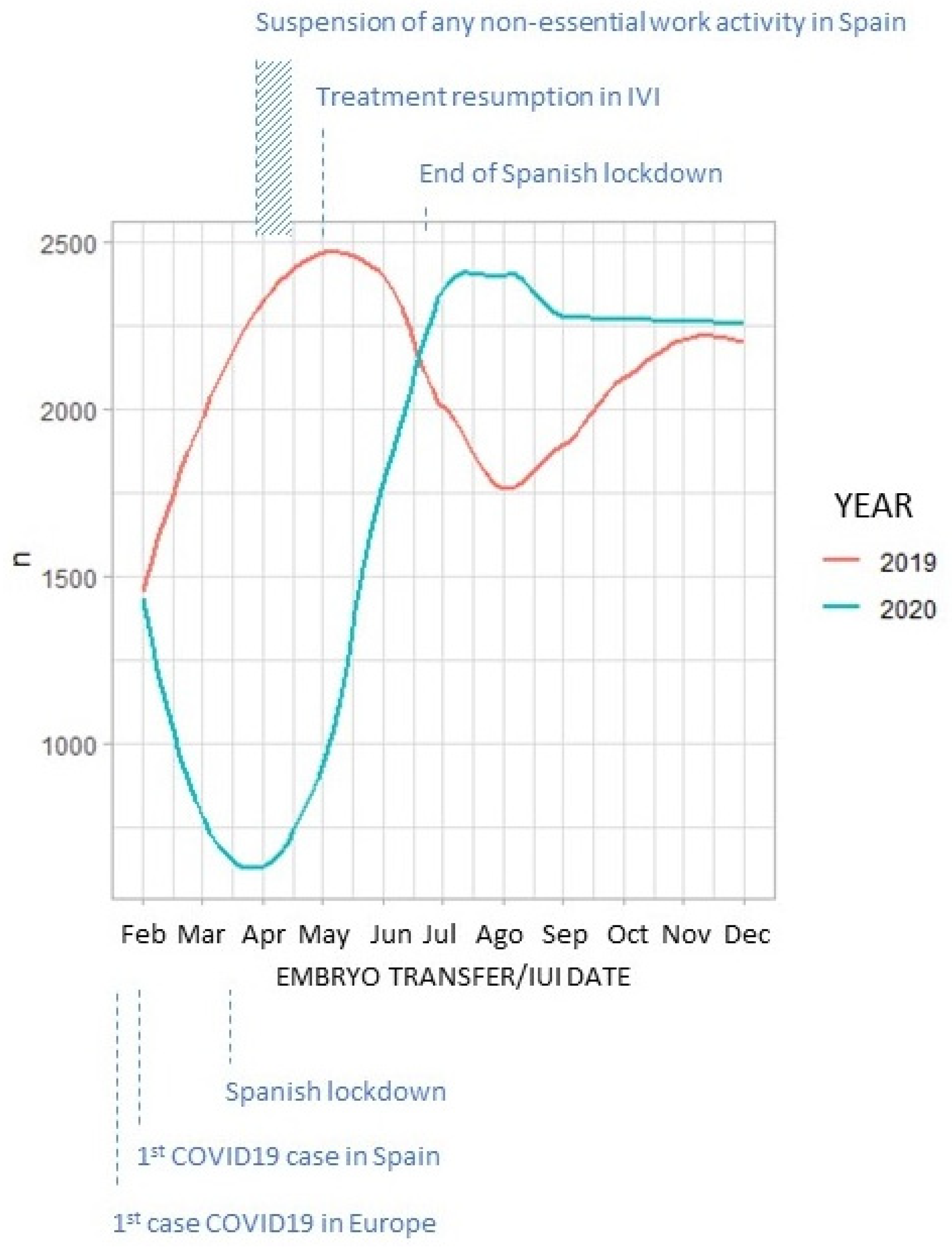
In 2020, the total number of treatments performed in our clinics per month followed a completely opposite trend to that registered in 2019. This trend corresponds to the episodes that took place in Spain during this period (
Figure 2).
3.1.3. Infertility Treatments Conducted in Spain Regarding Patients’ Country of Residence
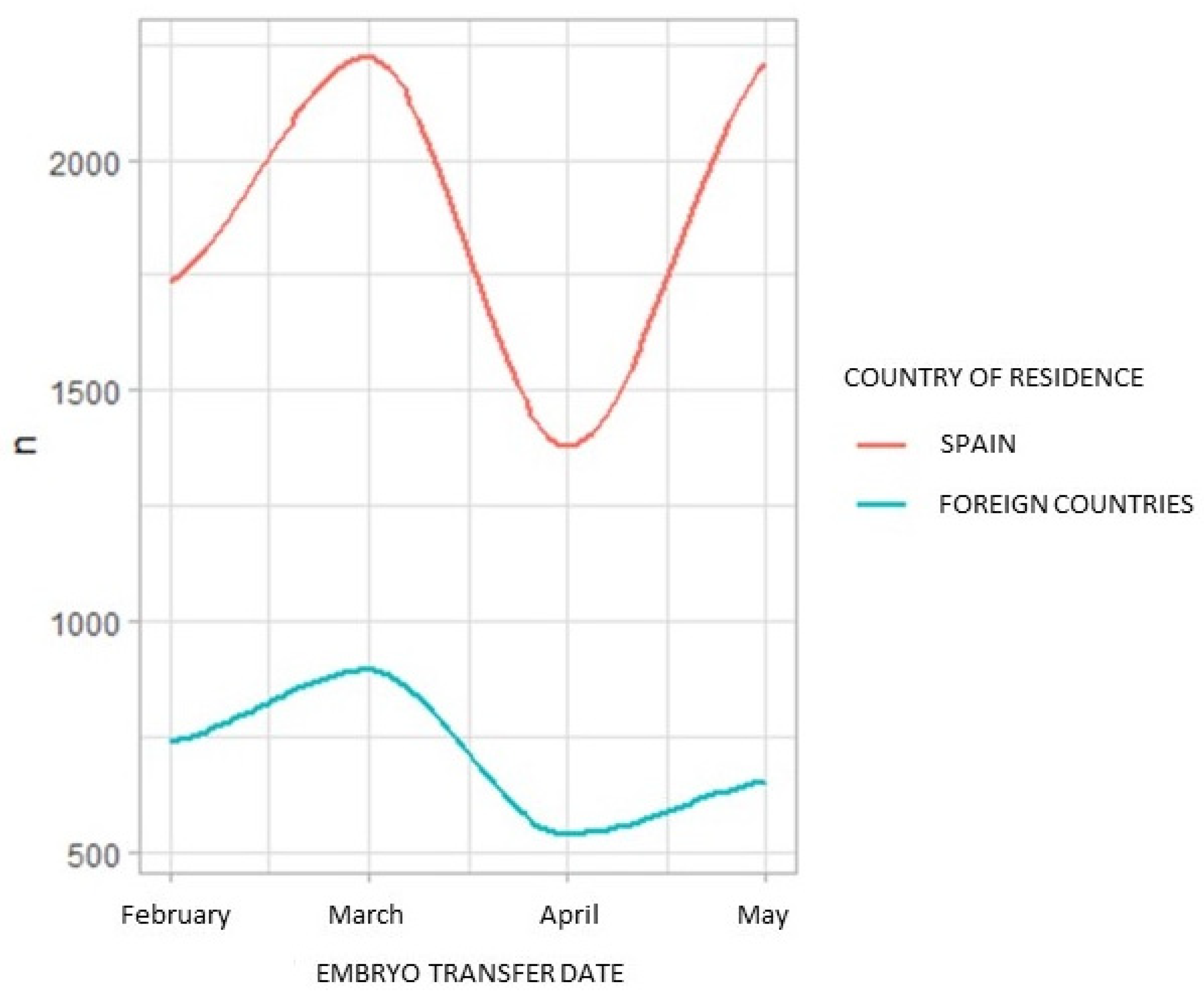
The first COVID-19 cases in Europe appeared in other countries before arriving in Spain.
Figure 3 represents the decline in the number of infertility treatments in our Spanish clinics during the first three months of the pandemic, both in patients of foreign (blue) and Spanish (red) origin.
3.1.4. Gestational Results Registered in 2020 versus 2019
Mean pregnancy rates in 2019 and 2020, as well as their comparison, are presented in
Table 3 regarding the type of treatment (IUI and IVF/ICSI with own oocytes and IVF/ICSI with donated oocytes).
3.2. Impact of COVID-19 in Gestational Results and Psychological Status of Women Whose First Trimester of Pregnancy Corresponded with the Onset of the Pandemic in Spain
In 2020, we gathered data from a total of 874 patients who got pregnant during the first three months of the pandemic and who answered to at least one of the surveys. In the first trimester, there were 439 answers from 1171 surveys sent (37.5%). In the second trimester, there were 614 answers from 2126 surveys sent (28.9%). However, only 341 from these 614 answers are from women whose first trimester coincides with the very onset of the pandemic (February and March, 2020). Finally, there were 140 answers from 719 surveys sent (21.3%) during the post-partum period. Some patients have answered more than one survey. Only 71 patients answered all three surveys.
A descriptive analysis of the final pregnancy outcome of these 874 patients is presented in
Table 4. Unfortunately, we lack information on the final pregnancy outcome of 135 ongoing pregnancies beyond the 12th week.
A descriptive analysis of the patients’ answers to our follow-up surveys is presented in
Table 5.
In order to ease the comparative analysis between the answers to the surveys and the final pregnancy outcome, this later variable was encompassed in two main categories: live birth (689/739) and miscarriage or gestational loss (50/739). Ongoing pregnancies beyond the 12th week lost to follow-up (n = 135) were withdrawn from the comparative analysis.
Regarding the Hamilton scale results, there was not any significant impact on pregnancy outcome on the first (p = 0.598) and second trimester (p = 0.745). In the post-partum survey, however, almost only pregnancies with live birth answered to these anxiety scale questions (107 answers in the live birth group vs. 1 in the miscarriage group; 30 answers in the ongoing pregnancy group, which were not analyzed due to the lack of final pregnancy outcome results). Therefore, the correlation between the Hamilton scale results assessed during the post-partum period and the final pregnancy outcome could not be analyzed.
A similar situation occurred with the data regarding levels of concern, levels of exercise, diet, if someone related died for COVID-19, or their COVID-19 symptoms/test result in the first and second trimester. In line with the general results (
Table 5), the majority of pregnant women in both the live birth and miscarriage groups had high levels of concern, their physical exercise had been reduced, their diet was unchanged, no one close died from COVID-19, and they lacked any COVID-19 symptoms (
p = 0.000). Hence, due to the high homogeneity in the answers between both pregnancy outcome groups and added to the large difference in sample size between the miscarriage (n = 24 answers) and live birth groups (n = 347 answers), the potential impact of these variables on final pregnancy outcome could not be correctly evaluated.
Finally, a descriptive analysis of the six pregnant women who tested positive for COVID-19 (one in the survey of the first trimester and five in the survey of the second trimester) showed that all of them reported mild anxiety levels as measured by the Hamilton scale and ended in live birth. In contrast, levels of concern regarding the pandemic were moderate and high in two and four of them, respectively.
4. Discussion
The onset of the COVID-19 global pandemic has forced the whole world to stop and infertility treatments were not any different. In the current study, we wanted to show an overall perspective on the impact of this pandemic in the ART sector, as well as in the reproductive outcome of those patients who got pregnant in our clinics during its most crucial months.
Cycle and demographic characteristics of our patients in 2020 were comparable to the ones in 2019. In 2020, however, women undergoing ovarian stimulation protocols needed more days of stimulation and thus received higher FSH doses. These differences, although statistically significant, were not clinically relevant. In addition, estradiol levels in the triggering day were significantly lower in 2020, suggesting that these women had a slower response to ovarian stimulation and thus the higher days of FSH exposure (
Table 1).
In general, the total number of infertility treatments performed in 2020 suffered a huge decline in comparison to the ones performed in 2019 regardless of the type of treatment. Indeed, the proportion of the different types of treatments remained practically the same in both years (
Table 2 and
Figure 1). Fresh embryo transfers with donated oocytes were slightly reduced in 2020 probably due to the added difficulty of synchronizing donor and patient.
Additionally, this decline followed a trend that corresponds to the episodes that took place in Spain during this period. Hence, there was an initial huge drop in the number of procedures during the first months of the pandemic. Once infertility treatments resumed in the spring, however, the number of procedures exceeded the ones registered during the same period in 2019, as a substantial drop in the number of treatments performed is usually experienced due to the holiday season (
Figure 2).
The specific situation of foreign patients coming to IVI Spain in order to undergo an infertility treatment is of particular interest. COVID-19 cases began to appear in other European countries before they did in Spain, thus patients coming from abroad also began to decline with the onset of the pandemic. Furthermore, the closure of country borders totally stopped reproductive tourism in our country (
Figure 3).
Despite the evident negative effect on the number of infertility procedures, the pandemic and its associated sanitary crisis did not seem to affect pregnancy success rates. Differences in pregnancy and clinical pregnancy, although significant due to the high sample size, were not clinically relevant. In contrast, ongoing pregnancy (defined as ongoing pregnancies with a gestational sac that did not suffer any miscarriage) and live birth rates, as well as biochemical and clinical miscarriages, did not show any statistically significant difference between 2019 and 2020 (
Table 3). Hence, despite the lower total number of treatments, those couples who decided to undergo an infertility treatment in 2020 had the same chances of success as the previous year.
Along with successful pregnancy rates, answers to our follow-up surveys showed that these patients were not suffering from high levels of stress. This situation did not vary as pregnancy evolved, even though they did acknowledge high levels of concern regarding the pandemic during the first and second trimester (
Table 5).
In general, patients’ lifestyle did not change much as a result of this sanitary crisis. Their physical exercise was reduced, whereas their diet remained unchanged. Our study population did not suffer the death of someone close due to COVID-19 and they did not have any symptoms themselves (
Table 5).
However, it was not possible to evaluate the impact of these answers on final pregnancy outcome due to the far-from-heterogeneous distribution of these variables, as the majority of patients showed a clear trend towards one specific common answer. In addition, almost only good prognosis pregnancies are represented in our study population (
Table 4). It is understandable that pregnancy losses and pregnancies with early worse prognosis were not in a good place to fill these surveys. Hence, our results have an important bias and they almost describe those pregnancies with good final outcomes.
It is important to take into account that patients with any kind of miscarriage or arrested pregnancy may not have answered our surveys. Most patients with a biochemical miscarriage might have received the questionnaire from the first trimester after their loss. In addition, these patients have not answered the second and third surveys, as they were not pregnant anymore. This explains the reduced sample size regarding this pregnancy outcome. A similar situation occurred with clinical miscarriages and arrested pregnancies.
Additionally, any attempt to assess the evolution in time of psychological status and levels of concern in those patients who answered all of the surveys (n = 71) failed. As expected, these patients correspond to those with live birth or ongoing pregnancies, thus good prognosis patients and again a bias was observed.
Finally, the sub-analysis performed in the sub-population of COVID-19-positive pregnant women, although of very low sample size (n = 6), does not suggest any impact of the disease in these patients’ psychological status and final pregnancy outcome. In this sub-population, high levels of concern were not translated into an increased anxiety or impaired final pregnancy outcome.
In any case, results from the first arm clearly show no significant clinical difference in pregnancy outcome between two consecutive years with and without a huge source of stress, as it is the case of the COVID-19 pandemic. Therefore, regardless of the bias described in the second arm of the study, the overall pregnancy outcome in infertility treatments was not affected by the COVID-19 pandemic and stress generated by this situation.