Metabolic Health, Obesity, and Renal Function: 2013–2018 National Health and Nutrition Examination Surveys
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Definition of Metabolic Phenotypes
2.3. Renal Outcome Measures
2.4. Questionnaires, Examinations, and Laboratory Data
2.5. Statistical Analysis
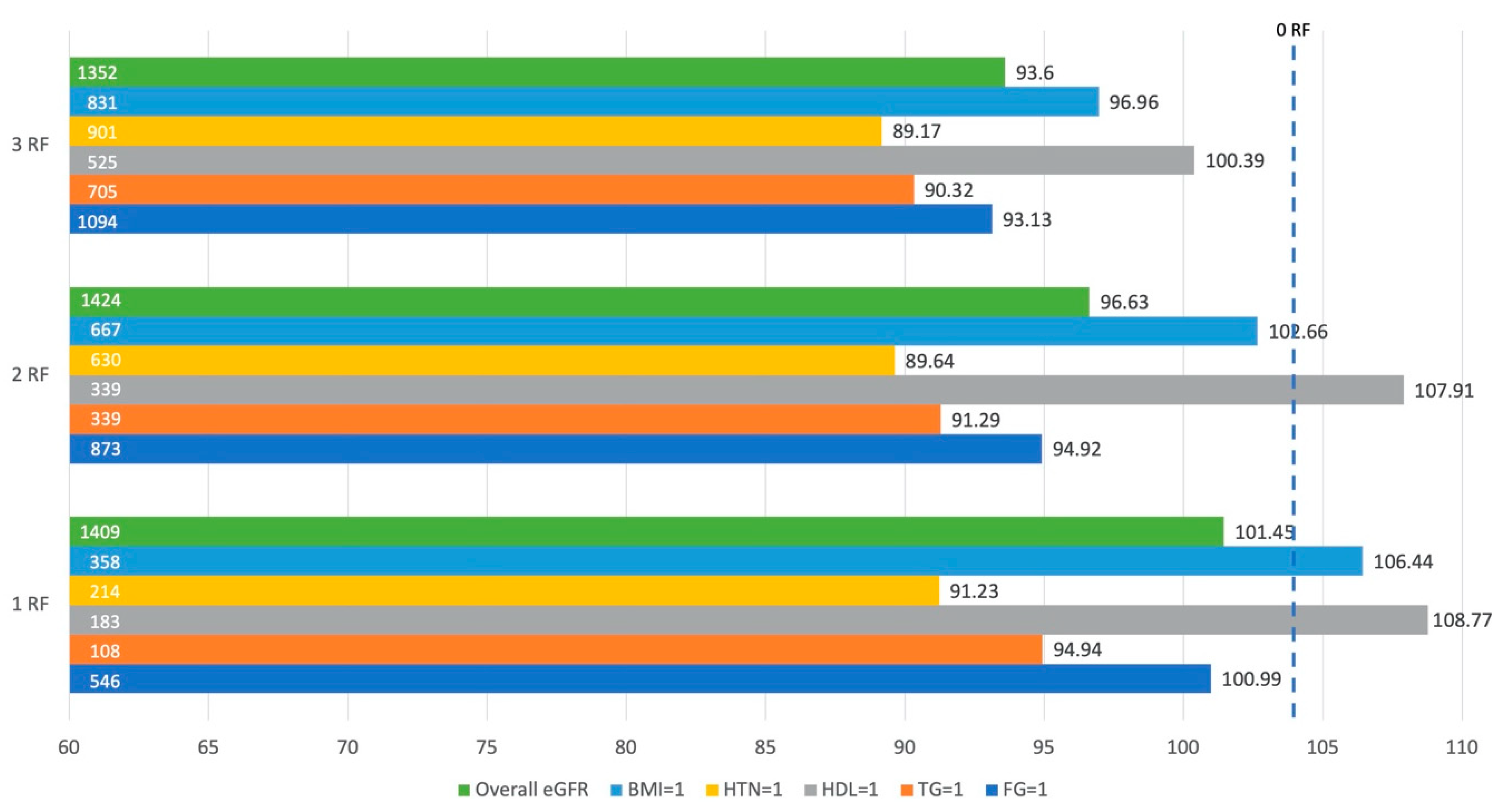
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2018.
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z. Chronic Kidney Disease: Global Dimension and Perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Saran, R.; Robinson, B.; Abbott, K. US Renal Data System 2017 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 2018, 71 (Suppl. S1), A7. [Google Scholar] [CrossRef] [PubMed]
- Keith, D.S.; Nichols, G.A.; Gullion, C.M.; Brown, J.B.; Smith, D.H. Longitudinal Follow-up and Outcomes Among a Population With Chronic Kidney Disease in a Large Managed Care Organization. Arch. Intern. Med. 2004, 164, 659–663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, J.X. Metabolic Syndrome Prevalence by Race/Ethnicity and Sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev. Chronic Dis. 2017, 14, E24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hales, C.; Carroll, M.; Fryar, C.; Ogden, C. Prevalence of Obesity among Adults and Youth: United States, 2017–2018; National Center for Health Statistics: Hyattsville, MD, USA, 2020.
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2019; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019.
- Weisinger, J.R.; Kempson, R.L.; Eldridge, F.L.; Swenson, R.S. The Nephrotic Syndrome: A Complication of Massive Obesity. Ann. Intern. Med. 1974, 81, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Yarnoff, B.O.; Hoerger, T.J.; Shrestha, S.S.; Simpson, S.K.; Burrows, N.R.; Anderson, A.H.; Xie, D.; Chen, H.-Y.; Pavkov, M.E.; the CRIC Study Investigators. Modeling the Impact of Obesity on the Lifetime Risk of Chronic Kidney Disease in the United States Using Updated Estimates of GFR Progression from the CRIC Study. PLoS ONE 2018, 13, e0205530. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, S.; Esmaeili, H.; Alizadeh, M.; Daneshzad, E.; Sharifi, L.; Radfar, H.; Radaei, M.K. Metabolic Phenotypes of Obese, Overweight, and Normal Weight Individuals and Risk of Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Arch. Endocrinol. Metab. 2019, 63, 427–437. [Google Scholar] [CrossRef]
- Kouvari, M.; Panagiotakos, D.B.; Yannakoulia, M.; Georgousopoulou, E.; Critselis, E.; Chrysohoou, C.; Tousoulis, D.; Pitsavos, C.; ATTICA Study Investigators. Transition From Metabolically Benign to Metabolically Unhealthy Obesity and 10-Year Cardiovascular Disease Incidence: The ATTICA Cohort Study. Metabolism 2019, 93, 18–24. [Google Scholar] [CrossRef]
- Adair, K.E.; Padgett, R.N.; von Waaden, N.; Wilson, R.L.; Bowden, R.G. Metabolic Health, Obesity, and Cardiovascular Disease: 2015–2016 National Health and Nutrition Examination Survey. Am. J. Med. Sci. 2020, 361, 244–252. [Google Scholar] [CrossRef]
- Van Vliet-Ostaptchouk, J.V.; Nuotio, M.-L.; Slagter, S.N.; Doiron, D.; Fischer, K.; Foco, L.; Gaye, A.; Gögele, M.; Heier, M.; Hiekkalinna, T.; et al. The Prevalence of Metabolic Syndrome and Metabolically Healthy Obesity in Europe: A Collaborative Analysis of Ten Large Cohort Studies. BMC Endocr. Disord. 2014, 14, 9. [Google Scholar] [CrossRef] [Green Version]
- Caleyachetty, R.; Thomas, G.N.; Toulis, K.A.; Mohammed, N.; Gokhale, K.M.; Balachandran, K.; Nirantharakumar, K. Metabolically Healthy Obese and Incident Cardiovascular Disease Events Among 3.5 Million Men and Women. J. Am. Coll. Cardiol. 2017, 70, 1429–1437. [Google Scholar] [CrossRef]
- Wildman, R.P.; Muntner, P.; Reynolds, K.; McGinn, A.P.; Rajpathak, S.; Wylie-Rosett, J.; Sowers, M.R. The Obese Without Cardiometabolic Risk Factor Clustering and the Normal Weight With Cardiometabolic Risk Factor Clustering: Prevalence and Correlates of 2 Phenotypes Among the US Population (NHANES 1999–2004). Arch. Intern. Med. 2008, 168, 1617–1624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nam, K.H.; Yun, H.-R.; Joo, Y.S.; Kim, J.; Lee, S.; Lee, C.; Park, K.S.; Park, J.T.; Chang, T.-I.; Kang, E.W.; et al. Changes in Obese Metabolic Phenotypes over Time and Risk of Incident Chronic Kidney Disease. Diabetes Obes. Metab. 2018, 20, 2778–2791. [Google Scholar] [CrossRef]
- Bradshaw, P.T.; Monda, K.L.; Stevens, J. Metabolic Syndrome in Healthy Obese, Overweight, and Normal Weight Individuals: The Atherosclerosis Risk in Communities Study. Obesity 2013, 21, 203–209. [Google Scholar] [CrossRef] [Green Version]
- Yun, H.-R.; Kim, H.; Park, J.T.; Chang, T.I.; Yoo, T.-H.; Kang, S.-W.; Choi, K.H.; Sung, S.; Kim, S.W.; Lee, J.; et al. Obesity, Metabolic Abnormality, and Progression of CKD. Am. J. Kidney Dis. 2018, 72, 400–410. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Janssen, I.; Heymsfield, S.B. Metabolic Syndrome in Normal-Weight Americans: New Definition of the Metabolically Obese, Normal-Weight Individual. Diabetes Care 2004, 27, 2222–2228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Jiang, H.; Chen, J. Combined Effect of Body Mass Index and Metabolic Status on the Risk of Prevalent and Incident Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Oncotarget 2016, 8, 35619–35629. [Google Scholar] [CrossRef] [Green Version]
- Lavie, C.J.; Laddu, D.; Arena, R.; Ortega, F.B.; Alpert, M.A.; Kushner, R.F. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1506–1531. [Google Scholar] [CrossRef] [PubMed]
- Diniz, M.d.F.H.S.; Beleigoli, A.M.R.; Ribeiro, A.L.P.; Vidigal, P.G.; Bensenor, I.M.; Lotufo, P.A.; Duncan, B.B.; Schmidt, M.I.; Barreto, S.M. Factors Associated with Metabolically Healthy Status in Obesity, Overweight, and Normal Weight at Baseline of ELSA-Brasil. Medicine 2016, 95, e4010. [Google Scholar] [CrossRef] [PubMed]
- Adair, K.E.; von Waaden, N.; Rafalski, M.; Hess, B.W.; Weaver, S.P.; Bowden, R.G. Metabolic Phenotypes and Chronic Kidney Disease: A Cross-Sectional Assessment of Patients from a Large Federally Qualified Health Center. Life 2021, 11, 175. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Clark, J.; Riddles, M.; Mohadjer, L.; Fakhouri, T. National Health and Nutrition Examination Survey, 2015−2018: Sample Design and Estimation Procedures; National Center for Health Statistics: Paris, France, 2020.
- Chen, T.; Parker, J.; Clark, J.; Shin, H.; Rammon, J.; Burt, V. National Health and Nutrition Examination Survey: Estimation Procedures, 2011–2014; National Center for Health Statistics: Hyattsville, MD, USA, 2018.
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [Green Version]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Hyattsville, MD, USA, 2019. Available online: https://Wwwn.Cdc.Gov/Nchs/Nhanes/ (accessed on 12 February 2021).
- Physical Activity Guidelines for Americans. Physical Activity Guidelines Advisory Committee Report, 2019; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Fang, J.; Zhang, Z.; Ayala, C.; Thompson-Paul, A.M.; Loustalot, F. Cardiovascular Health Among Non-Hispanic Asian Americans: NHANES, 2011–2016. J. Am. Heart Assoc. 2019, 8, e011324. [Google Scholar] [CrossRef] [Green Version]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, Without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A. Homeostasis Model Assessment: Insulin Resistance and Beta-Cell Function from Fasting Plasma Glucose and Insulin Concentrations in Man. Diabetologia 1985, 28, 412. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Abramowitz, M.K. Metabolic Acidosis and the Progression of Chronic Kidney Disease. BMC Nephrol. 2014, 15, 55. [Google Scholar] [CrossRef] [Green Version]
- Aung, K.; Lorenzo, C.; Hinojosa, M.A.; Haffner, S.M. Risk of Developing Diabetes and Cardiovascular Disease in Metabolically Unhealthy Normal-Weight and Metabolically Healthy Obese Individuals. J. Clin. Endocrinol. Metab. 2014, 99, 462–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valadez, E.; Buckley, D.; Ismaeel, A.; OLIVER, A.; Adair, K.; Papoutsi, E.; Prezioso, K.; Stamatis, A.; Koutakis, P.; Forsse, J. Is Age an Independent Factor in Assessing Renal Health and Function in Healthy Individuals? A Pilot Study. Int. J. Exerc. Sci. Conf. Proc. 2020, 2, 75. [Google Scholar]
- Wang, Y.; Chen, X.; Song, Y.; Caballero, B.; Cheskin, L.J. Association between Obesity and Kidney Disease: A Systematic Review and Meta-Analysis. Kidney Int. 2008, 73, 19–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, C.H.; Lee, M.J.; Kang, Y.M.; Hwang, J.Y.; Kim, E.H.; Park, J.-Y.; Kim, H.-K.; Lee, W.J. The Risk of Chronic Kidney Disease in a Metabolically Healthy Obese Population. Kidney Int. 2015, 88, 843–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, J.E.; Henegar, J.R.; Dwyer, T.M.; Liu, J.; Da Silva, A.A.; Kuo, J.J.; Tallam, L. Is Obesity a Major Cause of Chronic Kidney Disease? Adv. Ren. Replace. Ther. 2004, 11, 41–54. [Google Scholar] [CrossRef] [PubMed]
- Gounden, V.; Bhatt, H.; Jialal, I. Renal Function Tests. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Ärnlöv, J.; Ingelsson, E.; Sundström, J.; Lind, L. Impact of Body Mass Index and the Metabolic Syndrome on the Risk of Cardiovascular Disease and Death in Middle-Aged Men. Circulation 2010, 121, 230. [Google Scholar] [CrossRef] [PubMed]
- Kuk, J.L.; Ardern, C.I. Are Metabolically Normal but Obese Individuals at Lower Risk for All-Cause Mortality? Diabetes Care 2009, 32, 2297–2299. [Google Scholar] [CrossRef] [Green Version]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory Mechanisms Linking Obesity and Metabolic Disease. J. Clin. Investig. 2017, 127, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Cinti, S.; Mitchell, G.; Barbatelli, G.; Murano, I.; Ceresi, E.; Faloia, E.; Wang, S.; Fortier, M.; Greenberg, A.S.; Obin, M.S. Adipocyte Death Defines Macrophage Localization and Function in Adipose Tissue of Obese Mice and Humans. J. Lipid Res. 2005, 46, 2347–2355. [Google Scholar] [CrossRef] [Green Version]
- Modification of Diet in Renal Disease Study Group; Hunsicker, L.G.; Adler, S.; Caggiula, A.; England, B.K.; Greene, T.; Kusek, J.W.; Rogers, N.L.; Teschan, P.E.; Beck, G. Predictors of the Progression of Renal Disease in the Modification of Diet in Renal Disease Study. Kidney Int. 1997, 51, 1908–1919. [Google Scholar] [CrossRef] [Green Version]
- Muntner, P.; Coresh, J.; Smith, J.C.; Eckfeldt, J.; Klag, M.J. Plasma Lipids and Risk of Developing Renal Dysfunction: The Atherosclerosis Risk in Communities Study. Kidney Int. 2000, 58, 293–301. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Zhou, S.; Wu, B.; Zhao, Y.; Liu, X.; Liang, Y.; Shao, X.; Holthöfer, H.; Zou, H. Association between Metabolically Unhealthy Overweight/Obesity and Chronic Kidney Disease: The Role of Inflammation. Diabetes Metab. 2014, 40, 423–430. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Krishnaswami, S.; Harris, T.B.; Katsiaras, A.; Kritchevsky, S.B.; Simonsick, E.M.; Nevitt, M.; Holvoet, P.; Newman, A.B. Obesity, Regional Body Fat Distribution, and the Metabolic Syndrome in Older Men and Women. Arch. Intern. Med. 2005, 165, 777. [Google Scholar] [CrossRef] [Green Version]
- Thomas, G.; Sehgal, A.R.; Kashyap, S.R.; Srinivas, T.R.; Kirwan, J.P.; Navaneethan, S.D. Metabolic Syndrome and Kidney Disease: A Systematic Review and Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2011, 6, 2364–2373. [Google Scholar] [CrossRef] [Green Version]
- Madsen, C.M.; Varbo, A.; Nordestgaard, B.G. Extreme High High-Density Lipoprotein Cholesterol Is Paradoxically Associated with High Mortality in Men and Women: Two Prospective Cohort Studies. Eur. Heart J. 2017, 38, 2478–2486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zanoni, P.; Khetarpal, S.A.; Larach, D.B.; Hancock-Cerutti, W.F.; Millar, J.S.; Cuchel, M.; DerOhannessian, S.; Kontush, A.; Surendran, P.; Saleheen, D.; et al. Rare Variant in Scavenger Receptor BI Raises HDL Cholesterol and Increases Risk of Coronary Heart Disease. Science 2016, 351, 1166–1171. [Google Scholar] [CrossRef] [Green Version]
- Corsetti, J.P.; Ryan, D.; Rainwater, D.L.; Moss, A.J.; Zareba, W.; Sparks, C.E. Cholesteryl Ester Transfer Protein Polymorphism (TaqIB) Associates With Risk in Postinfarction Patients With High C-Reactive Protein and High-Density Lipoprotein Cholesterol Levels. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 1657–1664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Category | Classification | Values |
|---|---|---|
| Metabolic Risk Factor | Obesity | Non-Asian BMI ≥ 30 kg/m2, Asian BMI ≥ 25 kg/m2 |
| Hyperglycemia | Fasting glucose ≥100 mg/dL or Rx | |
| Dyslipidemia (2nd criteria) | TG ≥ 150 mg/dL or Rx | |
| HDL < 40 mg/dL (M), <50 mg/dL (F); or Rx | ||
| Hypertension | >130 mmHg systolic or >85 mmHg diastolic or Rx | |
| Metabolic Phenotype | MHN | Non-obese and <1 metabolic risk factor |
| MHO | Obese and <1 metabolic risk factor | |
| MUN | Non-obese and >1 metabolic risk factor | |
| MUO | Obese and >1 metabolic risk factor |
| Unweighted Total (n = 6610) | Weighted Total (n = 220,388,819) | MHN (19.11%) | MHO (5.59%) | MUN (38.40%) | MUO (36.90%) | p-Value | |
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | ||
| Age (years) | 47.03 (17.04) | 45.61 (0.37) | 35.72 (0.58) | 36.22 (0.86) | 49.31 (0.57) | 48.31 (0.52) | <0.001 |
| BMI (kg/m2) | 29.4 (7.33) | 29.40 (0.18) | 23.42 (0.13) | 33.48 (0.28) | 25.33 (0.09) | 36.10 (0.24) | <0.001 |
| Waist Circumference (cm) | 99.35 (17.15) | 99.83 (0.43) | 83.75 (0.40) | 105.93 (0.84) | 92.25 (0.30) | 115.19 (0.50) | <0.001 |
| Caloric Intake (Kcal/day) | 2048 (853) | 2087 (17) | 2083 (43) | 2032 (56) | 2123 (25) | 2058 (27) | 0.207 |
| Fasting Glucose (mg/dL) | 110.71 (37.50) | 107.74 (0.49) | 91.54 (0.26) | 92.41 (0.38) | 108.35 (0.65) | 117.83 (0.83) | <0.001 |
| Triglycerides (mg/dL) | 115.59 (112.38) | 114.16 (1.70) | 66.21 (1.21) | 75.35 (1.81) | 117.73 (2.03) | 141.14 (3.20) | <0.001 |
| HDL (mg/dL) | 53.75 (16.11) | 54.29 (0.36) | 64.82 (0.65) | 59.06 (1.07) | 54.49 (0.53) | 47.90 (0.37) | <0.001 |
| LDL (mg/dL) | 111.22 (35.56) | 111.38 (0.72) | 100.91 (1.32) | 109.55 (1.79) | 113.90 (1.13) | 114.55 (1.01) | <0.001 |
| Systolic BP (mmHg) | 123.31 (18.00) | 121.41 (0.29) | 110.05 (0.40) | 113.55 (0.49) | 122.64 (0.44) | 127.19 (0.37) | <0.001 |
| Diastolic BP (mmHg) | 70.13 (12.28) | 70.30 (0.29) | 65.32 (0.32) | 68.11 (0.62) | 70.49 (0.42) | 73.01 (0.33) | <0.001 |
| eGFR (mL/min/1.73 m2) | 97.7 (22.17) | 97.16 (0.50) | 103.93 (0.91) | 106.44 (1.25) | 94.34 (0.64) | 95.19 (0.61) | <0.001 |
| hs-CRP (mg/L) | 4.15 (8.25) | 3.80 (0.18) | 1.39 (0.07) | 4.49 (0.52) | 2.92 (0.26) | 5.68 (0.28) | <0.001 |
| ACR (mg/g) | 41.66 (291.46) | 29.14 (2.78) | 16.70 (2.33) | 10.49 (3.07) | 23.34 (2.93) | 44.45 (6.20) | <0.001 |
| HOMA-IR | 4.22 (8.52) | 3.77 (0.10) | 1.35 (0.03) | 2.51 (0.10) | 2.63 (0.07) | 6.43 (0.22) | <0.001 |
| SCr (mg/dL) | 0.86 (0.28) | 0.86 (0.00) | 0.83 (0.00) | 0.84 (0.01) | 0.86 (0.00) | 0.87 (0.01) | <0.001 |
| BUN (mg/dL) | 13.74 (5.24) | 13.84 (0.12) | 13.03 (0.16) | 12.61 (0.31) | 14.16 (0.18) | 14.12 (0.16) | <0.001 |
| n (%) | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | p-value | |
| Male Sex | 3205 (48.49) | 49.39 (0.67) | 40.14 (2.28) | 36.76 (3.24) | 56.72 (1.48) | 47.01 (1.44) | <0.001 |
| Race/Ethnicity | |||||||
| Mexican American | 1041 (15.75) | 9.49 (1.12) | 8.02 (1.09) | 8.97 (2.29) | 9.06 (1.10) | 10.78 (1.30) | <0.001 |
| Other Hispanic | 731 (11.06) | 6.49 (0.79) | 6.87 (1.34) | 7.29 (1.75) | 6.99 (0.85) | 5.66 (0.65) | |
| NH White | 2353 (35.60) | 63.36 (1.98) | 68.02 (2.66) | 48.17 (4.57) | 67.21 (1.89) | 59.23 (2.44) | |
| NH Black | 1376 (20.82) | 11.29 (1.11) | 6.77 (0.98) | 30.32 (3.53) | 3.54 (0.52) | 18.81 (1.89) | |
| NH Asian | 849 (12.84) | 5.55 (0.52) | 7.45 (0.76) | 2.15 (0.63) | 8.97 (0.97) | 1.52 (0.16) | |
| Other/Multi-Racial | 260 (3.93) | 3.83 (0.40) | 2.88 (0.58) | 3.10 (1.01) | 4.24 (0.59) | 4.00 (0.61) | |
| Low SES | 1355 (22.69) | 15.43 (1.05) | 13.10 (1.46) | 16.56 (1.99) | 15.22 (1.23) | 16.67 (1.47) | 0.143 |
| CKD | 966 (14.61) | 12.07 (0.52) | 6.31 (1.05) | 3.60 (1.05) | 11.73 (0.77) | 16.70 (0.83) | <0.001 |
| Physically Active | 2317 (69.98) | 69.38 (1.08) | 77.93 (1.83) | 76.24 (3.30) | 67.79 (1.98) | 62.88 (2.03) | <0.001 |
| Smoker | 2981 (45.10) | 46.28 (1.26) | 37.38 (2.46) | 40.78 (3.55) | 49.76 (1.57) | 48.09 (1.43) | <0.001 |
| Glucose Medication | 797 (12.06) | 9.14 (0.53) | 0 | 0 | 8.57 (0.76) | 15.86 (1.00) | <0.001 |
| Cholesterol Medication | 1206 (18.25) | 17.27 (0.67) | 0 | 0 | 21.64 (1.20) | 24.29 (1.31) | 0.158 |
| Hypertension Medication | 1678 (25.39) | 22.09 (0.88) | 0 | 0 | 23.23 (1.47) | 35.69 (1.51) | <0.001 |
| Coefficient | Model 1 a | Model 2 b | Model 3 c | |||
|---|---|---|---|---|---|---|
| B | SE B | B | SE B | B | SE B | |
| Intercept (MHN) | 103.93 | 0.91 | 101.98 | 0.79 | 99.43 | 0.73 |
| MHO | 2.50 | 1.42 | 2.03 | 1.15 | 1.54 | 0.80 |
| MUN | −9.60 ** | 0.80 | −12.30 ** | 1.09 | −12.33 ** | 1.20 |
| MUO | −8.74 ** | 0.96 | −9.55 ** | 1.01 | −10.53 ** | 0.96 |
| R2 | 0.042 | 0.077 | 0.059 | |||
| Overall eGFR | Overall SCr | MHO eGFR | MHO SCr | MUN eGFR | MUN SCr | |
|---|---|---|---|---|---|---|
| FG, r | −0.119 ** | 0.026 * | 0.015 | −0.023 | −0.069 ** | −0.020 |
| n | 6610 | 6588 | 367 | 366 | 2537 | 2529 |
| TG, r | −0.083 ** | 0.040 * | −0.159 * | 0.042 | −0.044 * | 0.034 |
| n | 6610 | 6588 | 367 | 366 | 2537 | 2529 |
| HDL, r | −0.002 | −0.123 ** | −0.065 | −0.172 * | −0.088 ** | −0.126 ** |
| n | 6610 | 6588 | 367 | 366 | 2537 | 2529 |
| SBP, r | −0.25 ** | 0.105 ** | 0.008 | 0.078 | −0.269 ** | 0.106 ** |
| n | 6610 | 6588 | 367 | 366 | 2537 | 2529 |
| DPB, r | −0.023 | 0.011 | −0.084 | −0.067 | 0.00 | 0.020 |
| n | 6610 | 6588 | 367 | 366 | 2537 | 2529 |
| BMI, r | −0.056 ** | 0.011 | 0.049 | −0.165 * | −0.124 ** | 0.061 * |
| n | 6610 | 6588 | 367 | 366 | 2537 | 2529 |
| WC, r | −0.175 ** | 0.096 ** | −0.033 | −0.123 * | −0.282 ** | 0.187 ** |
| n | 6445 | 6424 | 358 | 357 | 2481 | 2473 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adair, K.E.; Bowden, R.G.; Funderburk, L.K.; Forsse, J.S.; Ylitalo, K.R. Metabolic Health, Obesity, and Renal Function: 2013–2018 National Health and Nutrition Examination Surveys. Life 2021, 11, 888. https://doi.org/10.3390/life11090888
Adair KE, Bowden RG, Funderburk LK, Forsse JS, Ylitalo KR. Metabolic Health, Obesity, and Renal Function: 2013–2018 National Health and Nutrition Examination Surveys. Life. 2021; 11(9):888. https://doi.org/10.3390/life11090888
Chicago/Turabian StyleAdair, Kathleen E., Rodney G. Bowden, LesLee K. Funderburk, Jeffrey S. Forsse, and Kelly R. Ylitalo. 2021. "Metabolic Health, Obesity, and Renal Function: 2013–2018 National Health and Nutrition Examination Surveys" Life 11, no. 9: 888. https://doi.org/10.3390/life11090888
APA StyleAdair, K. E., Bowden, R. G., Funderburk, L. K., Forsse, J. S., & Ylitalo, K. R. (2021). Metabolic Health, Obesity, and Renal Function: 2013–2018 National Health and Nutrition Examination Surveys. Life, 11(9), 888. https://doi.org/10.3390/life11090888







