Characterization of Haemophilus influenzae Strains with Non-Enzymatic Resistance to β-Lactam Antibiotics Caused by Mutations in the PBP3 Gene in the Czech Republic in 2010–2018
Abstract
1. Introduction
2. Results
2.1. Phenotypic Detection
2.2. PCR and Mutation of the ftsI Gene
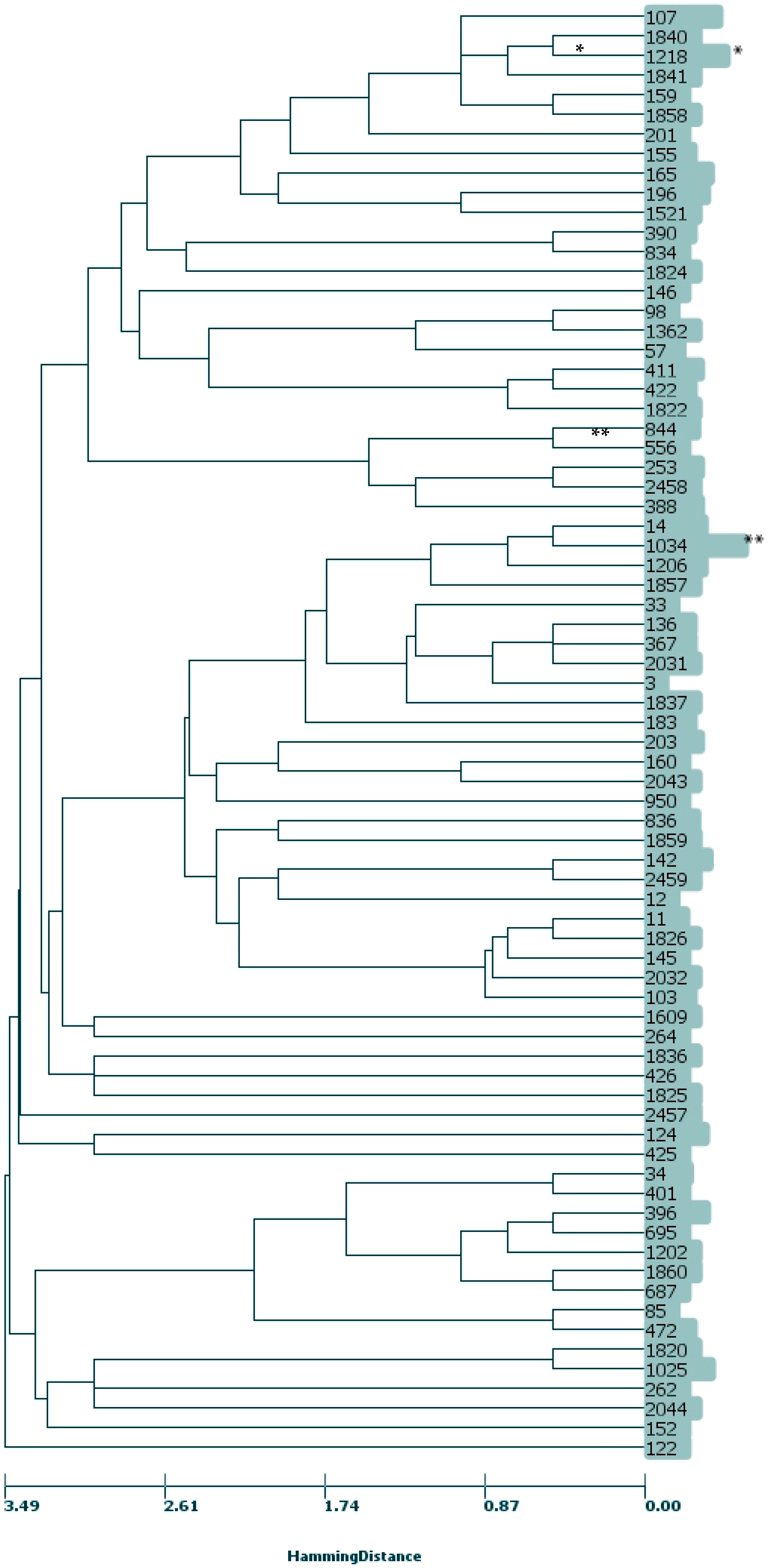
2.3. MLST, CC
3. Discussion
4. Materials and Methods
4.1. Strains
4.2. Susceptibility Testing to β-Lactams
4.3. PCR Detection of β-Lactamases
4.4. Detection of Mutations in the ftsI Gene and Comparative Analysis
4.5. Multi-Locus Sequence Typing (MLST) and Clonal Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jordens, J.Z.; Slack, M.P.E. Haemophilus influenzae: Then and now. Eur. J. Clin. Microbiol. Infect. Dis. 1995, 14, 935–948. [Google Scholar] [CrossRef]
- Niederman, M.S.; Mandell, L.A.; Anzueto, A.; Bass, J.B.; Broughton, W.A.; Campbell, G.D.; Dean, N.; File, T.; Fine, M.J.; Gross, P.A.; et al. Guidelines for the management of adults with community acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am. J. Respir. Crit. Care Med. 2001, 163, 1730–1754. [Google Scholar] [CrossRef]
- Medeiros, A.A.; O’Brien, T.F. Ampicillin-resistant Haemophilus influenzae type B possessing a TEMtype beta-lactamase but little permeability barrier to ampicillin. Lancet 1975, 1, 716–719. [Google Scholar] [CrossRef]
- Rubin, L.G.; Medeiros, A.A.; Yolken, R.H.; Moxon, E.R. Ampicillin treatment failure of apparently beta-lactamase-negative Haemophilus influenzae type b meningitis due to novel betalactamase. Lancet 1981, 2, 1008–1010. [Google Scholar] [CrossRef]
- Ubukata, K.; Shibasaki, Y.; Yamamoto, K.; Chiba, N.; Hasegawa, K.; Takeuchi, Y.; Sunakawa, K.; Inoue, M.; Konno, M. Association of amino acid substitutions in penicillin-binding protein 3 with β-lactam resistance in β-lactamase-negative ampicillin-resistant Haemophilus influenzae. Antimicrob. Agents Chemother. 2001, 45, 1693–1699. [Google Scholar] [CrossRef]
- Osaki, Y.; Sanbongi, M.; Ishikawa, H.; Kataoka, T.; Suzuki, K. Genetic approach to study the relationship between penicillin-binding protein 3 mutations and Haemophilus influenzae beta-lactam resistance by using site-directed mutagenesis and gene recombinants. Antimicrob. Agents Chemother. 2005, 49, 2834–2839. [Google Scholar] [CrossRef]
- Matic, V.; Bozdogan, B.; Jacobs, M.R.; Ubukata, K.; Appelbaum, P.C. Contribution of beta-lactamase and PBP amino acid substitutions to amoxicillin/clavulanate resistance in beta-lactamase-positive, amoxicillin/clavulanate-resistant Haemophilus influenzae. J. Antimicrob. Chemother. 2003, 52, 1018–1021. [Google Scholar] [CrossRef]
- Dabernat, H.; Delmas, C.; Seguy, M.; Pelissier, R.; Faucon, G.; Bennamani, S.; Pasquier, C. Diversity of beta-lactam resistance-conferring amino acid substitutions in penicillin-binding protein 3 of Haemophilus influenzae. Antimicrob. Agents Chemother. 2002, 46, 2208–2218. [Google Scholar] [CrossRef]
- Kaczmarek, F.S.; Gootz, T.D.; Dib-Hajj, F.; Shang, W.; Hallowell, S.; Cronan, M. Genetic and molecular characterization of beta-lactamasenegative ampicillin-resistant Haemophilus influenzae with unusually high resistance to ampicillin. Antimicrob. Agents Chemother. 2004, 48, 1630–1639. [Google Scholar] [CrossRef]
- Skaare, D.; Allum, A.G.; Anthonisen, I.L.; Jenkins, A.; Lia, A.; Strand, L.; Tveten, Y.; Kristiansen, B.E. Mutant ftsI genes in the emergence of penicillin-binding protein-mediated beta-lactam resistance in Haemophilus influenzae in Norway. Clin. Microbiol. Infect. 2010, 16, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Resman, F.; Ristovski, M.; Forsgren, A.; Kaijser, B.; Kronvall, G.; Medstrand, P.; Melander, E.; Odenholt, I.; Riesbeck, K. Increase of beta-lactam-resistant invasive Haemophilus influenzae in Sweden, 1997 to 2010. Antimicrob. Agents Chemother. 2012, 56, 4408–4415. [Google Scholar] [CrossRef]
- Dabernat, H.; Delmas, C. Epidemiology and evolution of antibiotic resistance of Haemophilus influenzae in children 5 years of age or less in France, 2001–2008: A retrospective database analysis. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 2745–2753. [Google Scholar] [CrossRef]
- Witherden, E.A.; Montgomery, J.; Henderson, B.; Tristram, S.G. Prevalence and genotypic characteristics of beta-lactamase-negative ampicillin-resistant Haemophilus influenzae in Australia. J. Antimicrob. Chemother. 2011, 66, 1013–1015. [Google Scholar] [CrossRef] [PubMed]
- Respirační Patogeny. Available online: https://apps.szu.cz/rp/respiracni_patogeny.php (accessed on 21 March 2020).
- Jakubů, V.; Urbášková, P.; Žemličková, H. First detection of cefotaxime-resistant strains of Haemophilus influenzae. Zpr. Cent. Epidemiol. Mikrobiol. 2015, 24, 387–388. [Google Scholar]
- Aguirre-Quiñonero, A.; Pérez del Molino, I.C.; García de la Fuente, C.; Sanjuán, M.C.; Agüero, J.; Martínez-Martínez, L. Phenotypic detection of clinical isolates of Haemophilus influenzae with altered penicillin-binding protein 3. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1475–1480. [Google Scholar] [CrossRef] [PubMed]
- Norskov-Lauritsen, N.; Ridderberg, W.; Erikstrup, L.T.; Fuursted, K. Evaluation of disk diffusion methods to detect low-level β-lactamase-negative ampicillin-resistant Haemophilus influenzae. APMIS 2011, 119, 385–392. [Google Scholar] [CrossRef]
- Barry, A.L.; Fuchs, P.C.; Brown, S.D. Identification of β-Lactamase-Negative, Ampicillin-Resistant Strains of Haemophilus influenzae with Four Methods and Eight Media. Antimicrob. Agents Chemother. 2001, 45, 1585–1588. [Google Scholar] [CrossRef] [PubMed]
- Schotte, L.; Wautier, M.; Martiny, D.; Piérard, D.; Depypere, M. Detection of beta-lactamase-negative ampicillin resistance in Haemophilus influenzae in Belgium. Diagn. Microbiol. Infect. Dis. 2019, 93, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, A.R.; Giufre, M.; Cerquetti, M.; Bajanca-Lavado, M.P. Polymorphism in ftsI gene and beta-lactam susceptibility in Portuguese Haemophilus influenzae strains: Clonal dissemination of beta-lactamase-positive isolates with decreased susceptibility to amoxicillin/clavulanic acid. J. Antimicrob. Chemother. 2011, 66, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Kishii, K.; Chiba, N.; Morozumi, M.; Hamano-Hasegawa, K.; Kurokawa, I.; Masaki, J.; Ubukata, K. Diverse mutations in the ftsI gene in ampicillin-resistant Haemophilus influenzae isolates from pediatric patients with acute otitis media. J. Infect. Chemother. 2010, 16, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Cobos, S.; Campos, J.; Lazaro, E.; Roman, F.; Cercenado, E.; Garcia-Rey, C.; Perez-Vazquez, M.; Oteo, J.; Abajo, F.d. Ampicillin-resistant non-beta-lactamaseproducing Haemophilus influenzae in Spain: Recent emergence of clonal isolates with increased resistance to cefotaxime and cefixime. Antimicrob. Agents Chemother. 2007, 51, 2564–2573. [Google Scholar] [CrossRef] [PubMed]
- Mizoguchi, A.; Hitomi, S. Cefotaxime-non-susceptibility of Haemophilus influenzae induced by additional amino acid substitutions of G555E and Y557H in altered penicillin-binding protein 3. J. Infect. Chemother. 2019, 25, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Tristram, S.; Jacobs, M.R.; Appelbaum, P.C. Antimicrobial resistance in Haemophilus influenzae. Clin. Microbiol. Rev. 2007, 20, 368–389. [Google Scholar] [CrossRef]
- Ubukata, K.; Chiba, N.; Morozumi, M.; Iwata, S.; Sunakawa, K. Longitudinal surveillance of Haemophilus influenzae isolates from pediatric patients with meningitis throughout Japan, 2000–2011. J. Infect. Chemother. 2013, 19, 34–41. [Google Scholar] [CrossRef]
- Park, C.; Kim, K.H.; Shin, N.Y.; Byun, J.H.; Kwon, E.Y.; Lee, J.W.; Kwon, H.J.; Choi, E.Y.; Lee, D.G.; Sohn, W.Y.; et al. Genetic diversity of the ftsI gene in beta-lactamase-nonproducing ampicillin-resistant and beta-lactamaseproducing amoxicillin-/clavulanic acid-resistant nasopharyngeal Haemophilus influenzae strains isolated from children in South Korea. Microb. Drug Resist. 2013, 19, 224–230. [Google Scholar] [CrossRef]
- Skaare, D.; Anthonisen, I.L.; Kahlmeter, G.; Matuschek, E.; Natås, O.B.; Steinbakk, M.; Sundsfjord, A.; Kristiansen, B.E. Emergence of clonally related multidrug resistant Haemophilus influenzae with penicillin-binding protein 3-mediated resistance to extended-spectrum cephalosporins, Norway, 2006 to 2013. Eurosurveillance 2014, 19, 20986. [Google Scholar] [CrossRef]
- Skaare, D.; Anthonisen, I.L.; Caugant, D.A.; Jenkins, A.; Steinbakk, M.; Strand, L.; Sundsfjord, A.; Tveten, Y.; Kristiansen, B.E. Multilocus sequence typing and ftsI sequencing: A powerful tool for surveillance of penicillin-binding protein 3-mediated beta-lactam resistance in nontypeable Haemophilus influenzae. BMC Microbiol. 2014, 14, 131–147. [Google Scholar] [CrossRef] [PubMed]
- Giufrè, M.; Fabiani, M.; Cardines, R.; Riccardo, F.; Caporali, M.G.; D’Ancona, F.; Pezzotti, P.; Cerquetti, M. Increasing trend in invasive non-typeable Haemophilus influenzae disease and molecular characterization of the isolates, Italy, 2012–2016. Vaccine 2018, 36, 6615–6622. [Google Scholar] [CrossRef]
- García-Cobos, S.; Arroyo, M.; Pérez-Vázquez, M.; Aracil, B.; Lara, N.; Oteo, J.; Cercenado, E.; Campos, J. Isolates of b-lactamase-negative ampicillin-resistant Haemophilus influenzae causing invasive infections in Spain remain susceptible to cefotaxime and imipenem. J. Antimicrob. Chemother. 2014, 69, 111–116. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hotomi, M.; Fujihara, K.; Billal, D.S.; Suzuki, K.; Nishimura, T.; Baba, S.; Yamanaka, N. Genetic characteristics and clonal dissemination of beta-lactamase non-producing ampicillin-resistant (BLNAR) Haemophilus influenzae isolated from the upper respiratory tract in Japan. Antimicrob. Agents Chemother. 2007, 51, 3969–3976. [Google Scholar] [CrossRef]
- Honda, H.; Sato, T.; Shinagawa, M.; Fukushima, Y.; Nakajima, C.; Suzuki, Y.; Shiraishi, T.; Kuronuma, K.; Takahashi, S.; Takahashi, H.; et al. Multiclonal Expansion and High Prevalence of Lactamase-Negative Haemophilus influenzae with High-Level Ampicillin Resistance in Japan and Susceptibility to Quinolones. Antimicrob. Agents Chemother. 2018, 62, e00851. [Google Scholar] [CrossRef] [PubMed]
- Thegerström, J.; Matuschek, E.; Su, Y.C.; Riesbeck, K.; Resman, F. A novel PBP3 substitution in Haemophilus influenzae confers reduced aminopenicillin susceptibility. BMC Microbiol. 2018, 18, 48–55. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 10.0. 2020. Available online: http://www.eucast.org (accessed on 20 May 2020).
- Montgomery, K.; Raymundo, L.; Drew, W.L. Chromogenic cephalosporin spot test to detect β-lactamase in clinically significant bacteria. J. Clin. Microbiol. 1979, 9, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Tristram, S.; Nichols, S. A multiplex PCR for beta-lactamase genes of Haemophilus influenzae and description of a new blaTEM promoter variant. J. Antimicrob. Chemother. 2005, 58, 183–185. [Google Scholar] [CrossRef][Green Version]
- Public Databases for Molecular Typing and Microbial Genome Diversity. Available online: https://pubmlst.org/static/organisms/haemophilus-influenzae/ftsI_sequencing_protocol_v3_01-02-2014.pdf (accessed on 11 December 2018).
- Fleischmann, R.D.; Adams, M.D.; White, O.; Clayton, R.A.; Kirkness, E.F.; Kerlavage, A.R.; Bult, C.J.; Tomb, J.F.; Dougherty, B.A.; Merrick, J.M.; et al. Whole-genome random sequencing and assembly of Haemophilus influenzae Rd. Science 1995, 269, 496–512. [Google Scholar] [CrossRef] [PubMed]
- Meats, E.; Feil, E.J.; Stringer, S.; Cody, A.J.; Goldstein, R.; Kroll, J.S.; Popovic, T.; Spratt, B.G. Characterization of Encapsulated and Noncapsulated Haemophilus influenzae and Determination of Phylogenetic Relationships by Multilocus Sequence Typing. J. Clin. Microbiol. 2003, 41, 1623–1636. [Google Scholar] [CrossRef]
- Francisco, A.P.; Bugalho, M.; Ramirez, M.; Carriço, J.A. Global optimal eBURST analysis of multilocus typing data using a graphic matroid approach. BMC Bioinform. 2009, 10, 152–167. [Google Scholar] [CrossRef]
| β-Lactamase Negative | β-Lactamase Positive | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range of Measured Values | MLST | Range of Measured Values | MLST | |||||||||||
| PBP3 Groups | AA Substitutions and Their Combinations | N | MIC AMP c (mg/L) | MIC CTX (mg/L) | PEN (mm) | AMC (mm) | CRX (mm) | AMP MIC50/MIC90 (mg/L) | ST/CC * a | N | MIC CTX (mg/L) | AMC (mm) | CRX (mm) | ST/CC * a |
| sPBP3 (n = 12) | A502S | 1 | 1 | 0.06 | 12 | 15 | 26 | 1/1 | 1218/1218 | |||||
| V511A | 1 | 0.06 | 11 | 23 | 426 | |||||||||
| D350N | 6 | 0.25–1 | 0.016–0.03 | 12–16 | 17–21 | 26–28 | 0.25/0.5 | 124 (5), 145/11 | 3 | 0.016 | 15–16 | 21–29 | 388 (3) | |
| A388V | 1 | 0.03 | 17 | 27 | 401 | |||||||||
| rPBP3 Group I (n = 15) | A502V, R517H | 13 | 1–4 | 0.03–0.125 | 6–19 | 12–19 | 14–27 | 2/4 | 1218/1218 (11), 1840/1218, 1841/1218 | 2 b | 0.016–0.06 | 13–19 | 23–31 | 146, 1218/1218 |
| rPBP3 Group II (n = 175) | A368T, A502T, N526K | 2 | 1–4 | 0.06 | 6–11 | 17 | 20–23 | 1/4 | 950, 1825 | |||||
| A502T, N526K | 1 | 2 | 0.125 | 6 | 13 | 21 | 2 | 12 | ||||||
| A502V, N526K | 5 | 1–2 | 0.03–0.06 | 6–11 | 11–15 | 21–25 | 2/2 | 142 (2), 411/422 (3) | 2 | 0.03–0.06 | 10–14 | 21–23 | 34, 411/422 | |
| D350N, A437S, A502V, N526K | 6 | 1–4 | 0.03–0.06 | 6–11 | 9–16 | 15–23 | 2/4 | 196 (5), 1837 | 2 | 0.03–0.06 | 10–13 | 17–23 | 836 (2) | |
| D350N, A437S, G490E, N526K, A530S | 1 | 4 | 0.06 | 6 | 7 | 21 | 1 | 390 | ||||||
| D350N, A502T, N526K | 8 | 1–4 | 0.06–0.125 | 6–11 | 10–14 | 6–21 | 2/4 | 183 (2), 1362, 1820, 1025 (4) | 1 | 0.06 | 9 | 19 | 1860/396 | |
| D350N, A502V, N526K | 1 | 4 | 0.06 | 10 | 14 | 22 | 4 | 122 | ||||||
| D350N, G490E, A502V, N526K | 1 | 2 | 0.03 | 9 | 15 | 21 | 2 | 2457 | ||||||
| D350N, G490E, A502V, N526K, A530S | 1 | 0.25 | 6 | 12 | 836 | |||||||||
| D350N, G490E, N526K, A530S | 18 | 0.25–4 | 0.008–0.06 | 6–11 | 10–18 | 17–25 | 2/4 | 107 (14), 159/1218, 201, 203, 425 | ||||||
| D350N, I449V, N526K | 1 | 1 | 0.03 | 12 | 16 | 24 | 1 | 152 | ||||||
| D350N, M377I, A502V, N526K | 74 | 0.25–16 | 0.016–0.125 | 6–11 | 6–20 | 11–29 | 2/8 | 14/14 (13), 98, 124, 136/367 (2), 145/11, 165 (6), 203 (3), 262, 367/367 (2), 422/422, 1034/14 (47), 1206/14 (2), 1218/1218 | 6 | 0.03–0.125 | 6–14 | 15–23 | 165 (5), 1206/14 | |
| D350N, M377I, G490E, A502V, N526K | 6 | 1 | 0.03–0.06 | 6–11 | 10–14 | 18–21 | 1/1 | 33, 556, 834, 844 (3) | ||||||
| D350N, M377I, I491V, A502V, N526K | 1 | 4 | 0.125 | 6 | 10 | 18 | 4 | 1034/14 | ||||||
| D350N, S357N, A502V, N526K | 1 | 2 | 0.125 | 9 | 12 | 17 | 2 | 1822/422 | ||||||
| G490E, N526K, A530S | 1 | 2 | 0.125 | 9 | 12 | 19 | 2 | 1858/1218 | ||||||
| G490E; A502V; N526K | 1 | 2 | 0.06 | 10 | 14 | 17 | 2 | 85 | ||||||
| I449V, N526K | 17 | 1–4 | 0.03–0.06 | 6–10 | 9–15 | 15–27 | 2/4 | 57, 253 (4), 390, 396/396 (7), 687/396, 695/396, 1202/396, 2458 | ||||||
| M377I, A502V, N526K | 3 | 0.03–0.06 | 11–15 | 19–20 | 165 (3) | |||||||||
| M377I, I449V, N526K | 5 | 1–4 | 0.06–0.25 | 6 | 6–14 | 12–19 | 4/4 | 11/11 (3), 1826/11, 2032/11 | ||||||
| N526K | 3 | 0.5–4 | 0.03–0.06 | 8–11 | 13–17 | 19–27 | 1/4 | 34 (3), | ||||||
| N526K, A530S | 5 | 1–4 | 0.06–0.125 | 6–11 | 12–17 | 17–25 | 2/4 | 2459, 142 (4) | ||||||
| R501L, N526K | 2 | 1 | 0.06 | 6–8 | 12–13 | 19–24 | 1/1 | 196 (2) | ||||||
| rPBP3 Group III (n = 26) | D350N, M377I, S385T, L389F, I519L, N526K | 1 | 4 | 0.5 | 6 | 6 | 6 | 4 | 2044 | |||||
| D350N, S357N, M377I, S385T, L389F, G490E, N526K, A530S | 2 | 4–8 | 0.5 | 6 | 6–12 | 6–12 | 4/8 | 107, 1859 | 2 | 0.5 | 6–16 | 8–16 | 107 (2) | |
| D350N, S357N, M377I, S385T, L389F, N526K | 2 | 4–16 | 1 | 6 | 6 | 6 | 4/16 | 472 (2) | ||||||
| D350N, S357N, M377I, S385T, L389F, P393L, R517H, T532S | 1 | 1 | 6 | 6 | 388 | |||||||||
| D350N, S357N, M377I, S385T, L389F, R517H | 1 | 1 | 12 | 16 | 422/422 | |||||||||
| D350N, S357N, M377I, S385T, R517H, T532S | 5 | 1–8 | 0.125–1 | 6–11 | 8–15 | 6–21 | 4/8 | 57, 155 (2), 1857, 2031/367 | ||||||
| D350N, S357N, M377I, S385T, L389F, R517H, T532S | 3 | 16 | 1–2 | 6 | 6–11 | 6–17 | 16/16 | 142, 264, 2043 | 6 | 1–2 | 6–12 | 6 | 3/367, 103/11 (2), 160, 1521, 1824 | |
| M377I, S385T, L389F, R517H | 1 | 8 | 1 | 6 | 6 | 6 | 8/8 | 142 | 1 | 1 | 6 | 6 | 1836 | |
| V329I, D350N, S357N, M377I, S385T, L389F, N526K | 1 | 8 | 2 | 6 | 13 | 15 | 8/8 | 1609 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakubu, V.; Malisova, L.; Musilek, M.; Pomorska, K.; Zemlickova, H. Characterization of Haemophilus influenzae Strains with Non-Enzymatic Resistance to β-Lactam Antibiotics Caused by Mutations in the PBP3 Gene in the Czech Republic in 2010–2018. Life 2021, 11, 1260. https://doi.org/10.3390/life11111260
Jakubu V, Malisova L, Musilek M, Pomorska K, Zemlickova H. Characterization of Haemophilus influenzae Strains with Non-Enzymatic Resistance to β-Lactam Antibiotics Caused by Mutations in the PBP3 Gene in the Czech Republic in 2010–2018. Life. 2021; 11(11):1260. https://doi.org/10.3390/life11111260
Chicago/Turabian StyleJakubu, Vladislav, Lucia Malisova, Martin Musilek, Katarina Pomorska, and Helena Zemlickova. 2021. "Characterization of Haemophilus influenzae Strains with Non-Enzymatic Resistance to β-Lactam Antibiotics Caused by Mutations in the PBP3 Gene in the Czech Republic in 2010–2018" Life 11, no. 11: 1260. https://doi.org/10.3390/life11111260
APA StyleJakubu, V., Malisova, L., Musilek, M., Pomorska, K., & Zemlickova, H. (2021). Characterization of Haemophilus influenzae Strains with Non-Enzymatic Resistance to β-Lactam Antibiotics Caused by Mutations in the PBP3 Gene in the Czech Republic in 2010–2018. Life, 11(11), 1260. https://doi.org/10.3390/life11111260







