High Risk for Attention-Deficit Hyperactive Disorder in Children with Strabismus: A Nationwide Cohort Study from the National Health Insurance Research Database
Abstract
1. Introduction
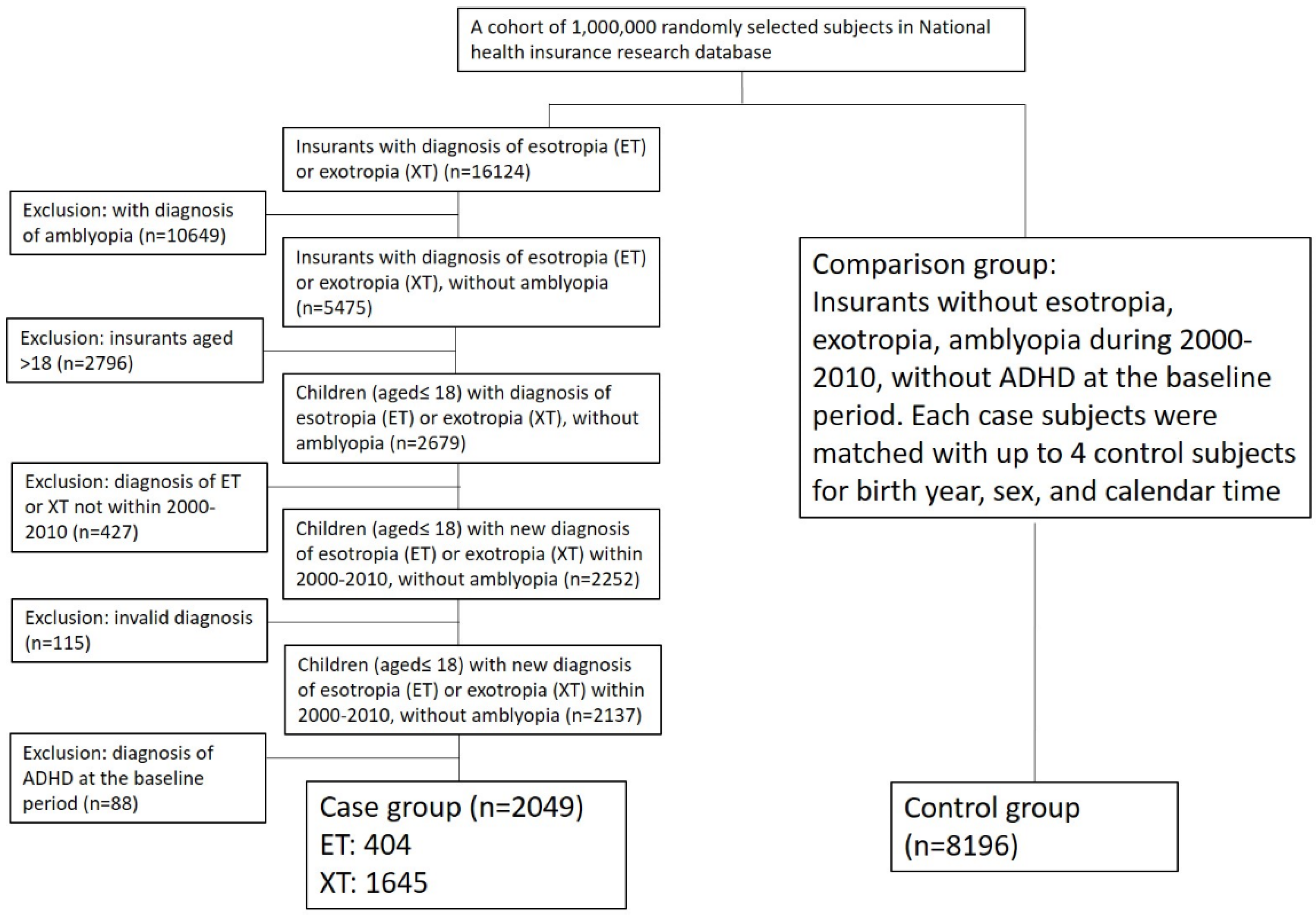
2. Materials and Methods
Statistical Analysis
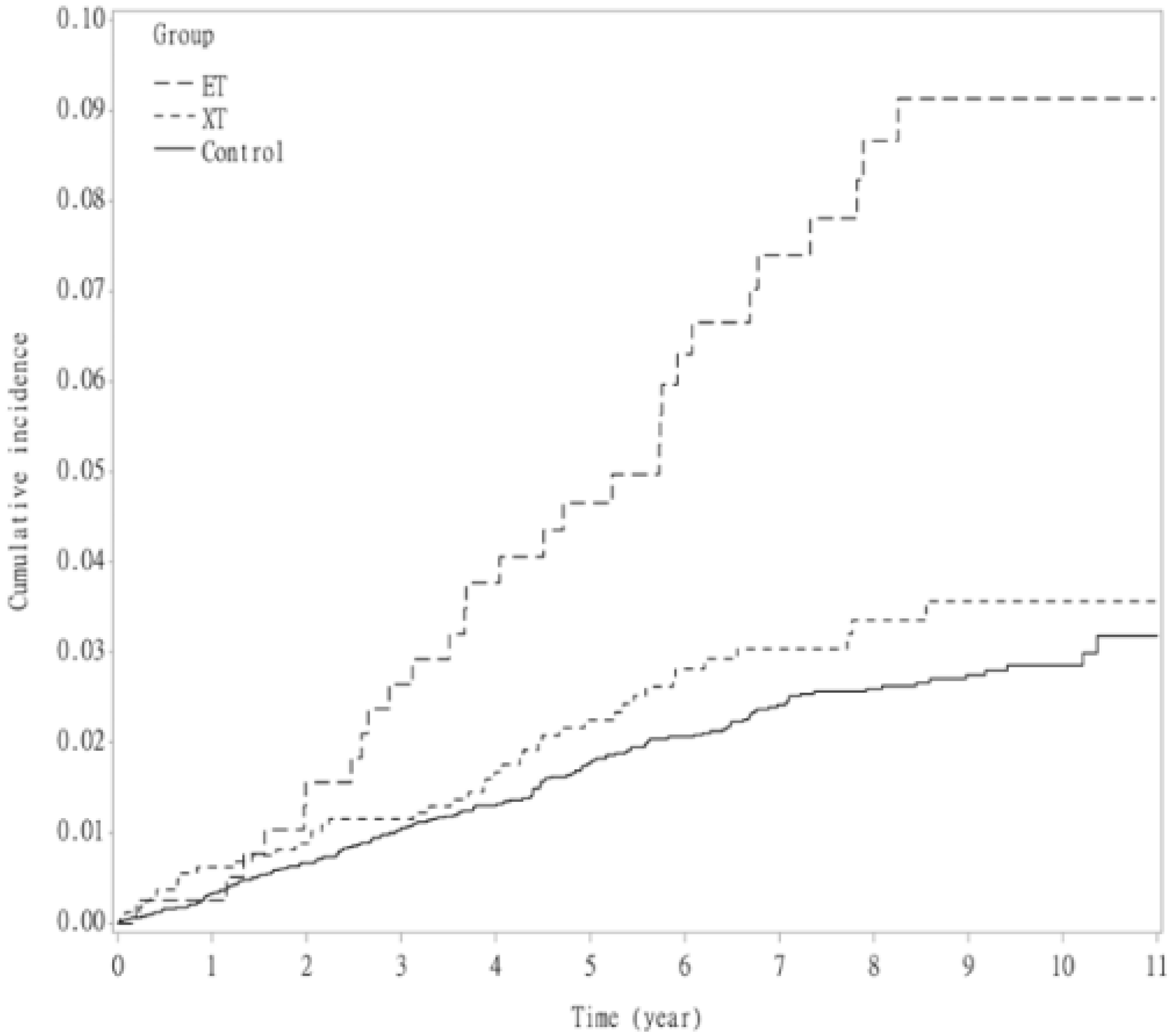
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohney, B.G.; Greenberg, A.E.; Diehl, N.N. Age at Strabismus Diagnosis in an Incidence Cohort of Children. Am. J. Ophthalmol. 2007, 144, 467–469. [Google Scholar] [CrossRef]
- McKean-Cowdin, R.; Cotter, S.A.; Tarczy-Hornoch, K.; Wen, G.; Kim, J.; Borchert, M.; Varma, R.; Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of Amblyopia or Strabismus in Asian and Non-Hispanic White Preschool Children: Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology 2013, 120, 2117–2124. [Google Scholar] [CrossRef]
- Lim, H.C.; Quah, B.L.; Balakrishnan, V.; Lim, H.C.; Tay, V.; Emmanuel, S.C. Vision Screening of 4-Year-Old Children in Singapore. Singap. Med. J. 2000, 41, 271–278. [Google Scholar]
- Ip, J.M.; Robaei, D.; Kifley, A.; Wang, J.J.; Rose, K.A.; Mitchell, P. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology 2008, 115, 678–685. [Google Scholar] [CrossRef]
- Yu, C.B.; Fan, D.S.; Wong, V.W.; Wong, C.Y.; Lam, D.S. Changing Patterns of Strabismus: A Decade of Experience in Hong Kong. Br. J. Ophthalmol. 2002, 86, 854–856. [Google Scholar] [CrossRef]
- Wu, C.; Hunter, D.G. Amblyopia: Diagnostic and Therapeutic Options. Am. J. Ophthalmol. 2006, 141, 175–184. [Google Scholar] [CrossRef]
- Fox, R.; Aslin, R.N.; Shea, S.L.; Dumais, S.T. Stereopsis in Human Infants. Science 1980, 207, 323–324. [Google Scholar] [CrossRef]
- Sim, B.; Yap, G.H.; Chia, A. Functional and Psychosocial Impact of Strabismus on Singaporean Children. J. AAPOS 2014, 18, 178–182. [Google Scholar] [CrossRef]
- Hatt, S.R.; Leske, D.A.; Castañeda, Y.S.; Wernimont, S.M.; Liebermann, L.; Cheng-Patel, C.S.; Birch, E.E.; Holmes, J.M. Association of Strabismus with Functional Vision and Eye-Related Quality of Life in Children. JAMA Ophthalmol. 2020, 138, 528–535. [Google Scholar] [CrossRef]
- Schuster, A.K.; Elflein, H.M.; Pokora, R.; Schlaud, M.; Baumgarten, F.; Urschitz, M.S. Health-Related Quality of Life and Mental Health in Children and Adolescents With Strabismus—Results of the Representative Population-Based Survey KiGGS. Health Qual. Life Outcomes 2019, 17, 81. [Google Scholar] [CrossRef]
- Mohney, B.G.; McKenzie, J.A.; Capo, J.A.; Nusz, K.J.; Mrazek, D.; Diehl, N.N. Mental Illness in Young Adults Who Had Strabismus as Children. Pediatrics 2008, 122, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.Y.; Lee, K.M.; Hwang, J.M.; Choi, D.G.; Lee, D.S.; Park, K.H.; Yu, Y.S. Comparison Between Anisometropic and Strabismic Amblyopia Using Functional Magnetic Resonance Imaging. Br. J. Ophthalmol. 2001, 85, 1052–1056. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Li, S.H.; Zhou, F.Q.; Zhang, Y.; Zhong, Y.L.; Cai, F.Q.; Shao, Y.; Zeng, X.J. Altered Intrinsic Regional Brain Spontaneous Activity in Patients With Comitant Strabismus: A Resting-State Functional MRI Study. Neuropsychiatr. Dis. Treat. 2016, 12, 1303–1308. [Google Scholar] [CrossRef]
- Thomas, R.; Sanders, S.; Doust, J.; Beller, E.; Glasziou, P. Prevalence of Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Pediatrics 2015, 135, e994–e1001. [Google Scholar] [CrossRef]
- Hamilton, L.S.; Levitt, J.G.; O’Neill, J.; Alger, J.R.; Luders, E.; Phillips, O.R.; Caplan, R.; Toga, A.W.; McCracken, J.; Narr, K.L. Reduced White Matter Integrity in Attention-Deficit Hyperactivity Disorder. NeuroReport 2008, 19, 1705–1708. [Google Scholar]
- Loe, I.M.; Feldman, H.M. Academic and Educational Outcomes of Children With ADHD. J. Pediatr. Psychol. 2007, 32, 643–654. [Google Scholar] [CrossRef] [PubMed]
- Merrell, C.; Tymms, P.B. Inattention, Hyperactivity and Impulsiveness: Their Impact on Academic Achievement and Progress. Br. J. Educ. Psychol. 2001, 71, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Eyre, O.; Riglin, L.; Leibenluft, E.; Stringaris, A.; Collishaw, S.; Thapar, A. Irritability in ADHD: Association With Later Depression Symptoms. Eur. Child Adolesc. Psychiatry 2019, 28, 1375–1384. [Google Scholar] [CrossRef]
- Dalsgaard, S. Attention-Deficit/Hyperactivity Disorder (ADHD). Eur. Child Adolesc. Psychiatry 2013, 22 (Suppl. 1), S43–S48. [Google Scholar] [CrossRef]
- Faraone, S.V.; Biederman, J. Neurobiology of Attention-Deficit Hyperactivity Disorder. Biol. Psychiatry 1998, 44, 951–958. [Google Scholar] [CrossRef]
- Leslie, L.K.; Weckerly, J.; Plemmons, D.; Landsverk, J.; Eastman, S. Implementing the American Academy of Pediatrics Attention-Deficit/Hyperactivity Disorder Diagnostic Guidelines in Primary Care Settings. Pediatrics 2004, 114, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Congdon, N.; Yam, J.C.; Huang, Y.; Qiu, K.; Ma, D.; Chen, B.; Li, L.; Zhang, M. Alcohol Use and Positive Screening Results for Depression and Anxiety Are Highly Prevalent Among Chinese Children With Strabismus. Am. J. Ophthalmol. 2014, 157, 894–900.e1. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.B.; Hodge, D.O.; Mohney, B.G. Prevalence of Mental Health Illness Among Patients with Adult-Onset Strabismus. Strabismus 2015, 23, 105–110. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mohney, B.G. Intermittent Exotropia and Mental Illness. Am. Orthopt. J. 2016, 66, 25–29. [Google Scholar] [CrossRef]
- Kilgore, K.P.; Barraza, R.A.; Hodge, D.O.; McKenzie, J.A.; Mohney, B.G. Surgical Correction of Childhood Intermittent Exotropia and the Risk of Developing Mental Illness. Am. J. Ophthalmol. 2014, 158, 788–792.e1. [Google Scholar] [CrossRef] [PubMed]
- Granet, D.B.; Gomi, C.F.; Ventura, R.; Miller-Scholte, A. The Relationship Between Convergence Insufficiency and ADHD. Strabismus 2005, 13, 163–168. [Google Scholar] [CrossRef] [PubMed]
- DeCarlo, D.K.; Bowman, E.; Monroe, C.; Kline, R.; McGwin, G., Jr.; Owsley, C. Prevalence of Attention-Deficit/Hyperactivity Disorder Among Children With Vision Impairment. J. AAPOS 2014, 18, 10–14. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Reimelt, C.; Wolff, N.; Hölling, H.; Mogwitz, S.; Ehrlich, S.; Roessner, V. The Underestimated Role of Refractive Error (Hyperopia, Myopia, and Astigmatism) and Strabismus in Children With ADHD. J. Atten. Disord. 2021, 25, 235–244. [Google Scholar] [CrossRef] [PubMed]
- DeCarlo, D.K.; Swanson, M.; McGwin, G.; Visscher, K.; Owsley, C. ADHD and Vision Problems in the National Survey of Children’s Health. Optom. Vis. Sci. 2016, 93, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Dirani, M.; Chan, Y.H.; Gazzard, G.; Au Eong, K.G.; Selvaraj, P.; Ling, Y.; Quah, B.L.; Young, T.L.; Mitchell, P.; et al. Prevalence of Amblyopia and Strabismus in Young Singaporean Chinese Children. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3411–3417. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.W.; Zhu, H.; Yu, J.J.; Ding, H.; Bai, J.; Chen, J.; Yu, R.-B.; Liu, H. Epidemiology of Intermittent Exotropia in Preschool children in China. Optom. Vis. Sci. 2016, 93, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.H.; Wang, A.H.; Hu, F.R.; Tsai, T.H. Exploring the Divergence Range for Stereopsis Maintenance With a Computer-Simulated Troposcope in Patients With Intermittent Exotropia. Investig. Ophthalmol. Vis. Sci. 2016, 57, 4493–4497. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, A.E.; Mohney, B.G.; Diehl, N.N.; Burke, J.P. Incidence and Types of Childhood Esotropia: A Population-Based Study. Ophthalmology 2007, 114, 170–174. [Google Scholar] [CrossRef]
- Atkinson, J.; Braddick, O. Visual Development. Handb. Clin. Neurol. 2020, 173, 121–142. [Google Scholar] [CrossRef] [PubMed]
- Hakim, R.B.; Tielsch, J.M. Maternal cigarette smoking during pregnancy: A risk factor for childhood strabismus. Arch. Ophthalmol. 1992, 110, 1459–1462. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.L., 3rd; Hung, L.F.; Arumugam, B.; Wensveen, J.M.; Chino, Y.M.; Harwerth, R.S. Observations on the Relationship Between Anisometropia, Amblyopia and Strabismus. Vis. Res. 2017, 134, 26–42. [Google Scholar] [CrossRef] [PubMed]
- Su, C.C.; Tsai, C.Y.; Tsai, T.H.; Tsai, I.J. Incidence and Risk of Attention-Deficit Hyperactivity Disorder in Children With Amblyopia: A Nationwide Cohort Study. Clin. Exp. Ophthalmol. 2019, 47, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Konrad, K.; Eickhoff, S.B. Is the ADHD Brain Wired Differently? A Review on Structural and Functional Connectivity in Attention Deficit Hyperactivity Disorder. Hum. Brain Mapp. 2010, 31, 904–916. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Norcia, A.M.; Yeatman, J.D.; Mezer, A. The Structural Properties of Major White Matter Tracts in Strabismic Amblyopia. Investig. Ophthalmol. Vis. Sci. 2015, 56, 5152–5160. [Google Scholar] [CrossRef] [PubMed]
- Castellanos, F.X.; Margulies, D.S.; Kelly, C.; Uddin, L.Q.; Ghaffari, M.; Kirsch, A.; Shaw, D.; Shehzad, Z.; Di Martino, A.; Biswal, B.; et al. Cingulate-Precuneus Interactions: A New Locus of Dysfunction in Adult Attention-Deficit/Hyperactivity Disorder. Biol. Psychiatry 2008, 63, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Vogt, B.A. Cingulate Impairments in ADHD: Comorbidities, Connections, and Treatment. Handb. Clin. Neurol. 2019, 166, 297–314. [Google Scholar]
- Ten Tusscher, M.P.M.; Houtman, A.C.; De Mey, J.; Van Schuerbeek, P. Cortical Visual Connections via the Corpus Callosum Are Asymmetrical in Human Infantile Esotropia. Strabismus 2018, 26, 22–27. [Google Scholar] [CrossRef]
- Cao, Q.; Sun, L.; Gong, G.; Lv, Y.; Cao, X.; Shuai, L.; Zhu, C.; Zang, Y.; Wang, Y. The Macrostructural and Microstructural Abnormalities of Corpus Callosum in Children With Attention Deficit/Hyperactivity Disorder: A Combined Morphometric and Diffusion Tensor MRI Study. Brain Res. 2010, 1310, 172–180. [Google Scholar] [CrossRef]
- Gilliam, M.; Stockman, M.; Malek, M.; Sharp, W.; Greenstein, D.; Lalonde, F.; Clasen, L.; Giedd, J.; Rapoport, J.; Shaw, P. Developmental Trajectories of the Corpus Callosum in Attention-Deficit/Hyperactivity Disorder. Biol. Psychiatry 2011, 69, 839–846. [Google Scholar] [CrossRef][Green Version]
- Lin, L.Y.; Warren-Gash, C.; Smeeth, L.; Chen, P.C. Data Resource Profile: The National Health Insurance Research Database (NHIRD). Epidemiol. Health 2018, 40, e2018062. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total | Strabismus Group | Esotropia | Exotropia | Non-Strabismus Group | p-Value * |
|---|---|---|---|---|---|---|
| n = 44330 | n = 2049 | n = 404 | n = 1645 | n = 8196 | ||
| Age, no. (%) | ||||||
| ≤7 | 3197 (31.2) | 650 (31.7) | 233 (57.7) | 417 (25.3) | 2547 (31.1) | 0.7168 |
| 7– ≤ 12 | 4180 (40.8) | 820 (40.0) | 100 (24.8) | 720 (43.8) | 3360 (41.0) | |
| 12– ≤ 18 | 2868 (28.0) | 579 (28.3) | 71 (17.6) | 508 (30.9) | 2289 (27.9) | |
| Mean (SD) | 9.2 (4.2) | 9.2 (4.2) | 6.9 (4.7) | 9.8 (3.8) | 9.2 (4.2) | 0.9987 |
| Female | 5440 (53.1) | 1088 (53.1) | 219 (54.2) | 869 (52.8) | 4352 (53.1) | 1.0000 |
| Duration of follow-up (year) | ||||||
| Mean (SD) | 6.5 (2.9) | 6.5 (2.9) | 7.2 (3.0) | 6.4 (2.9) | 6.5 (2.9) | 0.7877 |
| Median (interquartile range) | 6.9 (4.4, 9.1) | 6.9 (4.3, 9.1) | 8.1 (5.1, 9.8) | 6.7 (4.2, 8.9) | 6.9 (4.4, 9.1) | |
| Comorbiditities **, no. (%) | ||||||
| Autism spectrum disorder | 7 (0.1) | 7 (0.3) | 1 (0.2) | 6 (0.4) | 0 (0.0) | <0.0001 |
| Tourette syndrome (Tics) | 3 (0.0) | 2 (0.1) | 0 (0.0) | 2 (0.1) | 1 (0.0) | 0.1040 |
| oppositional defiant disorder | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| depression | 4 (0.0) | 3 (0.1) | 1 (0.2) | 2 (0.1) | 1 (0.0) | 0.0272 |
| Delayed development | 48 (0.5) | 37 (1.8) | 12 (3.0) | 25 (1.5) | 11 (0.1) | <0.0001 |
| Intellectual disability | 10 (0.1) | 7 (0.3) | 1 (0.2) | 6 (0.4) | 3 (0.0) | 0.0009 |
| Stuttering | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) | |
| Obsessive compulsive disorder | 1 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) | 0.6171 |
| Conduct disorder | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) | |
| Encopresis | 6 (0.1) | 4 (0.2) | 0 (0.0) | 4 (0.2) | 2 (0.0) | 0.0043 |
| Feeding and eating disorder | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Prematurity, low birth weight | 7 (0.1) | 6 (0.3) | 2 (0.5) | 4 (0.2) | 1 (0.0) | 0.0004 |
| Perinatal infection | 5 (0.0) | 5 (0.2) | 5 (1.2) | 0 (0.0) | 0 (0.0) | 0.0003 |
| Fetal and newborn respiratory condition | 1 (0.0) | 1 (0.0) | 0 (0.0) | 1 (0.1) | 0 (0.0) | 0.2000 |
| Birth condition | 2 (0.0) | 1 (0.0) | 0 (0.0) | 1 (0.1) | 1 (0.0) | 0.3600 |
| Birth trauma | 1 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) | 1.0000 |
| Intrauterine hypoxia and birth asphyxia | 1 (0.0) | 1 (0.0) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 0.2000 |
| Lower respiratory tract infection | 1846 (18.0) | 597 (29.1) | 159 (39.4) | 438 (26.6) | 1249 (15.2) | <0.0001 |
| Paralysis | 29 (0.3) | 26 (1.3) | 4 (1.0) | 22 (1.3) | 3 (0.0) | <0.0001 |
| Headaches | 74 (0.7) | 40 (2.0) | 8 (2.0) | 32 (1.9) | 34 (0.4) | <0.0001 |
| Epilepsy | 28 (0.3) | 16 (0.8) | 0 (0.0) | 16 (1.0) | 12 (0.1) | <0.0001 |
| Rheumatic disease | 2 (0.0) | 2 (0.1) | 0 (0.0) | 2 (0.1) | 0 (0.0) | 0.0400 |
| Chronic pulmonary disease | 376 (3.7) | 112 (5.5) | 23 (5.7) | 89 (5.4) | 264 (3.2) | <0.0001 |
| asthma | 289 (2.8) | 90 (4.4) | 18 (4.5) | 72 (4.4) | 199 (2.4) | <0.0001 |
| allergic rhinitis | 606 (5.9) | 245 (12.0) | 49 (12.1) | 196 (11.9) | 361 (4.4) | <0.0001 |
| allergic conjunctivitis | 191 (1.9) | 91 (4.4) | 8 (2.0) | 83 (5.0) | 100 (1.2) | <0.0001 |
| Deficiency anemias | 6 (0.1) | 4 (0.2) | 0 (0.0) | 4 (0.2) | 2 (0.0) | 0.0169 |
| ADHD Events | PY | Incidence † | Hazard Ratio (95% C.I.) | ||
|---|---|---|---|---|---|
| Crude | Adjusted | ||||
| Comparison group | 173 | 53615 | 3.23 | 1 (reference) | 1 (reference) |
| All patients | 72 | 13370 | 5.39 | 1.67 (1.27, 2.20) ** | 1.64 (1.23, 2.17) ** |
| Patients with ET | 29 | 2920 | 9.93 | 3.14 (2.12, 4.65) ** | 2.04 (1.36, 3.06) ** |
| Patients with XT | 43 | 10450 | 4.11 | 1.27 (0.91, 1.77) | 1.44 (1.03, 2.03) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, C.-Y.; Su, C.-C.; Liu, Y.-L.; Tsai, I.-J.; Tsai, T.-H. High Risk for Attention-Deficit Hyperactive Disorder in Children with Strabismus: A Nationwide Cohort Study from the National Health Insurance Research Database. Life 2021, 11, 1139. https://doi.org/10.3390/life11111139
Tsai C-Y, Su C-C, Liu Y-L, Tsai I-J, Tsai T-H. High Risk for Attention-Deficit Hyperactive Disorder in Children with Strabismus: A Nationwide Cohort Study from the National Health Insurance Research Database. Life. 2021; 11(11):1139. https://doi.org/10.3390/life11111139
Chicago/Turabian StyleTsai, Chia-Ying, Chien-Chia Su, Yao-Lin Liu, I-Ju Tsai, and Tzu-Hsun Tsai. 2021. "High Risk for Attention-Deficit Hyperactive Disorder in Children with Strabismus: A Nationwide Cohort Study from the National Health Insurance Research Database" Life 11, no. 11: 1139. https://doi.org/10.3390/life11111139
APA StyleTsai, C.-Y., Su, C.-C., Liu, Y.-L., Tsai, I.-J., & Tsai, T.-H. (2021). High Risk for Attention-Deficit Hyperactive Disorder in Children with Strabismus: A Nationwide Cohort Study from the National Health Insurance Research Database. Life, 11(11), 1139. https://doi.org/10.3390/life11111139






