Health-Related Quality of Life and Frailty in Chronic Liver Diseases
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Questionnaire
2.3. Our Study
2.4. Statistical Considerations
3. Results
3.1. Patient Baseline Data
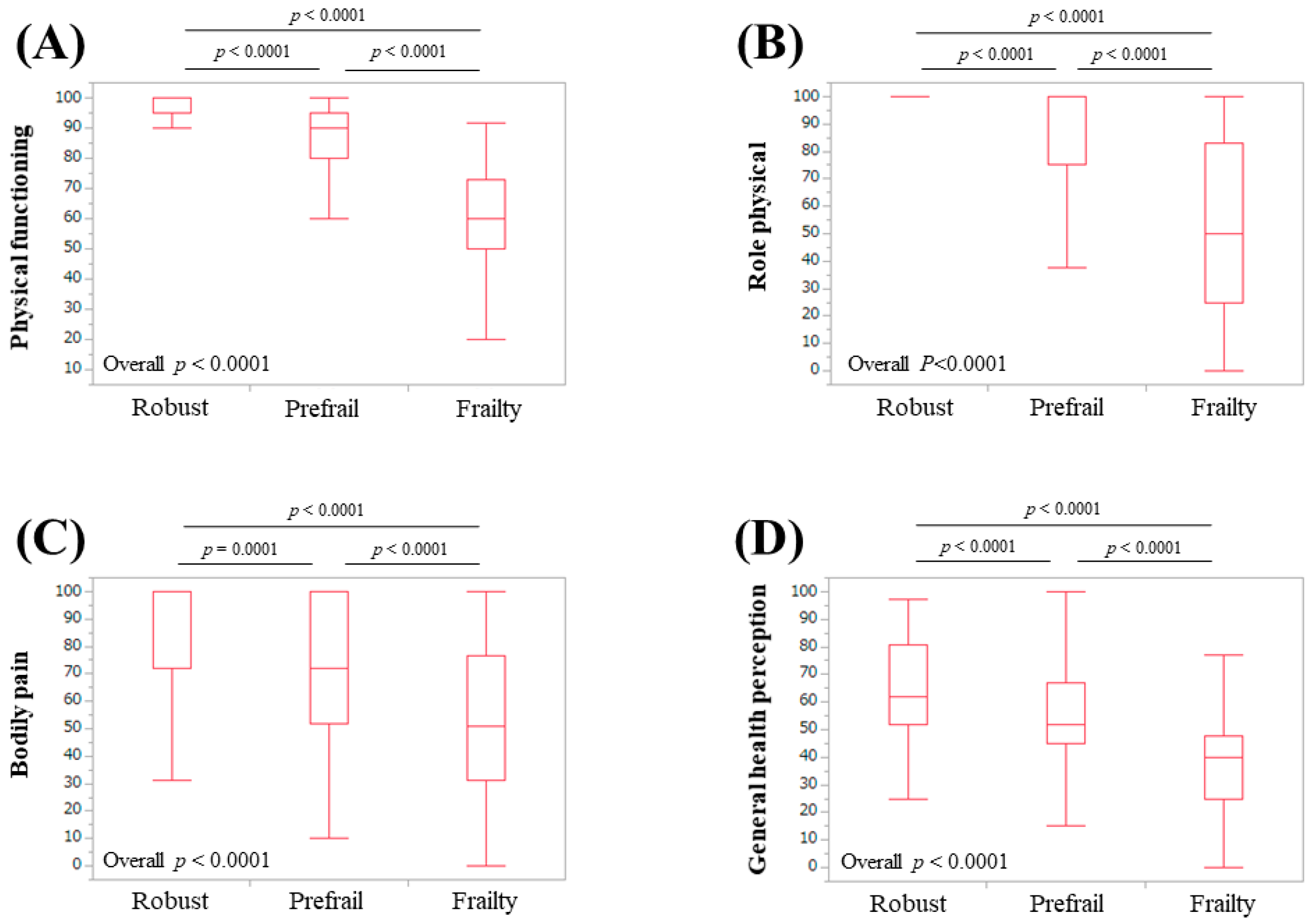
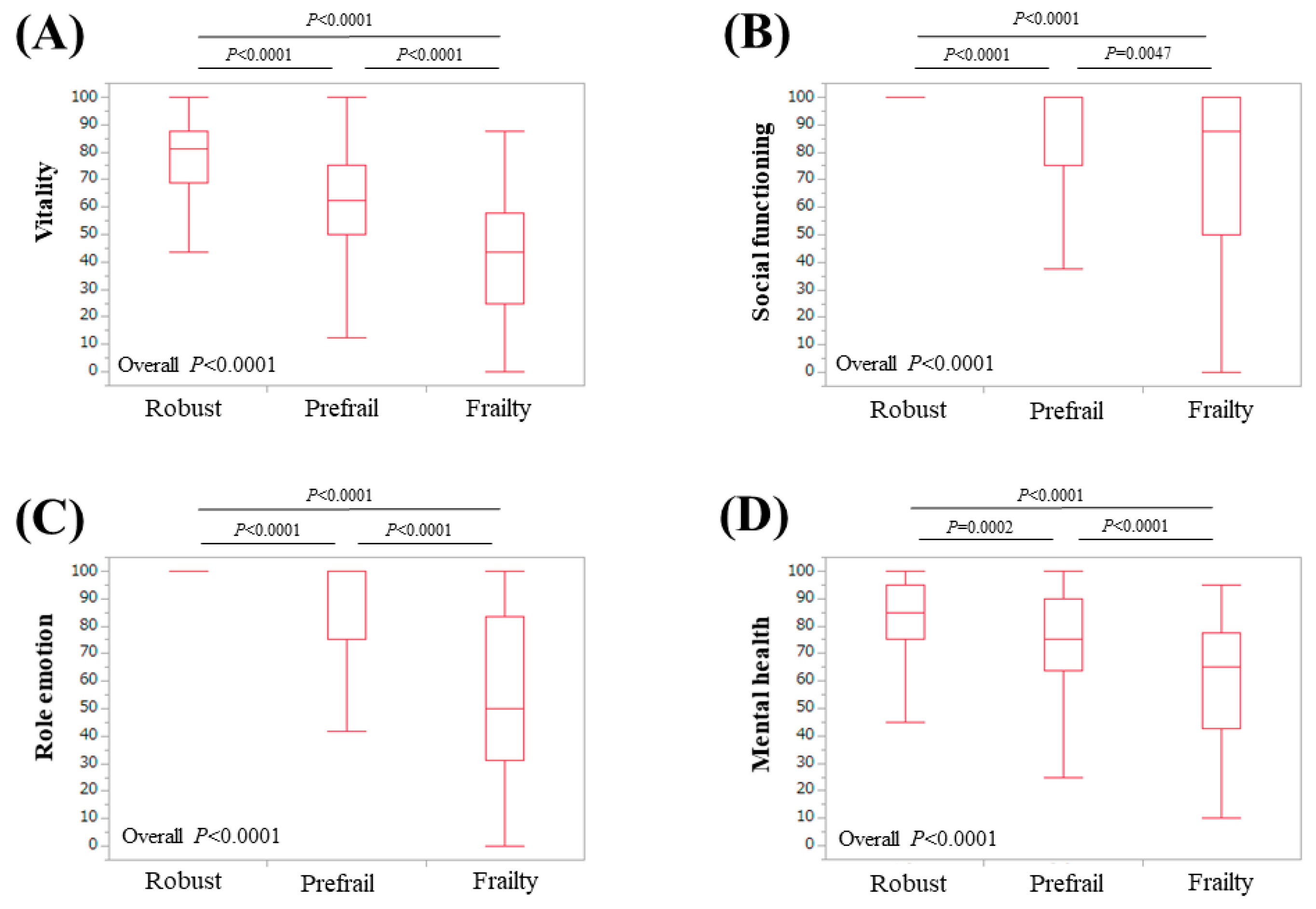
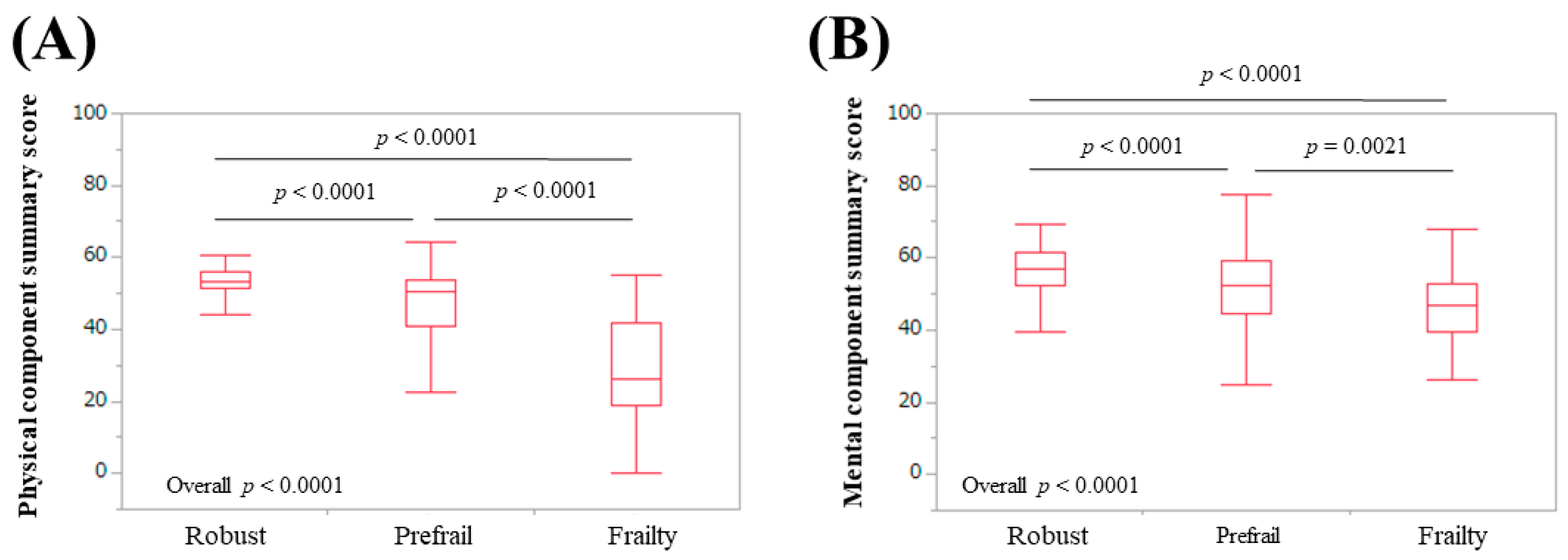
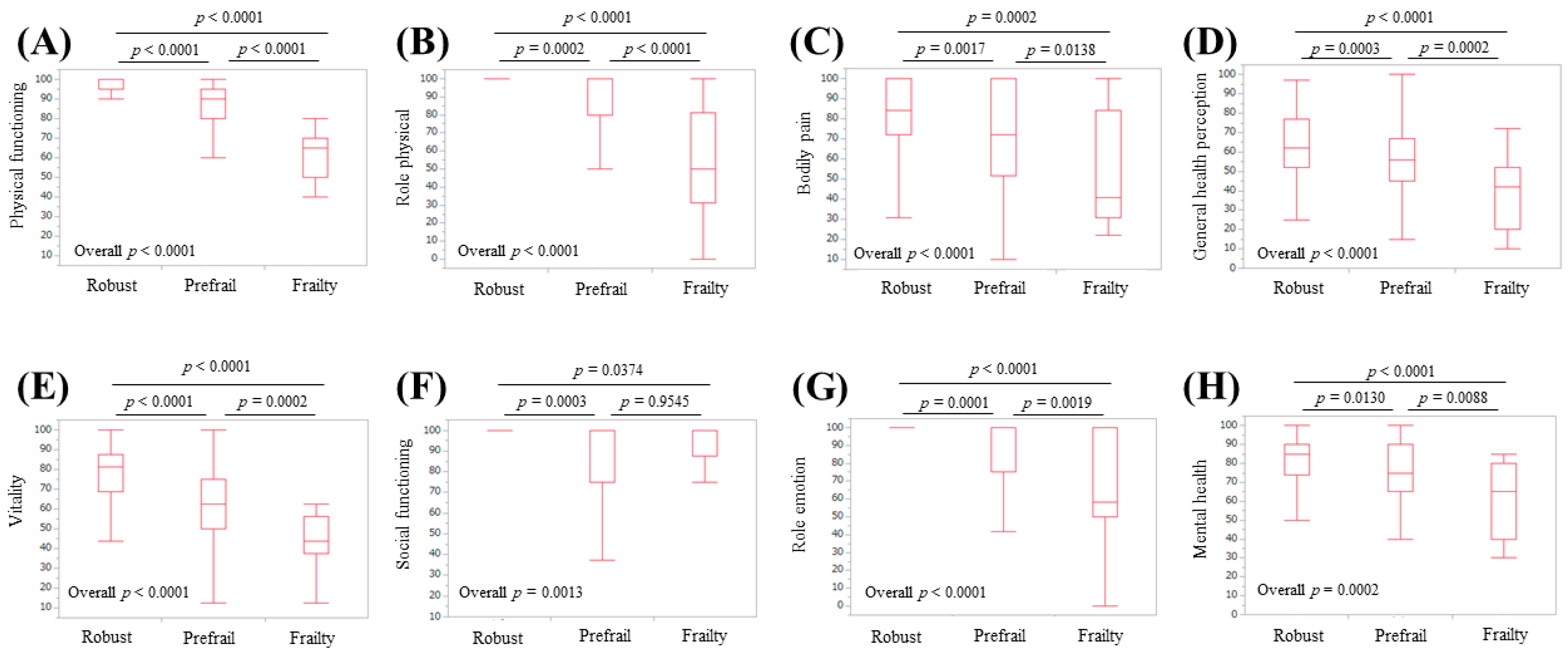
3.2. Scores of the Eight Scales of the SF-36, the PCS, and the MCS Relative to the Frailty Status
3.3. Subgroup Analysis 1: Scores of the Eight Scales of the SF-36 Relative to the Frailty Status in LC Patients
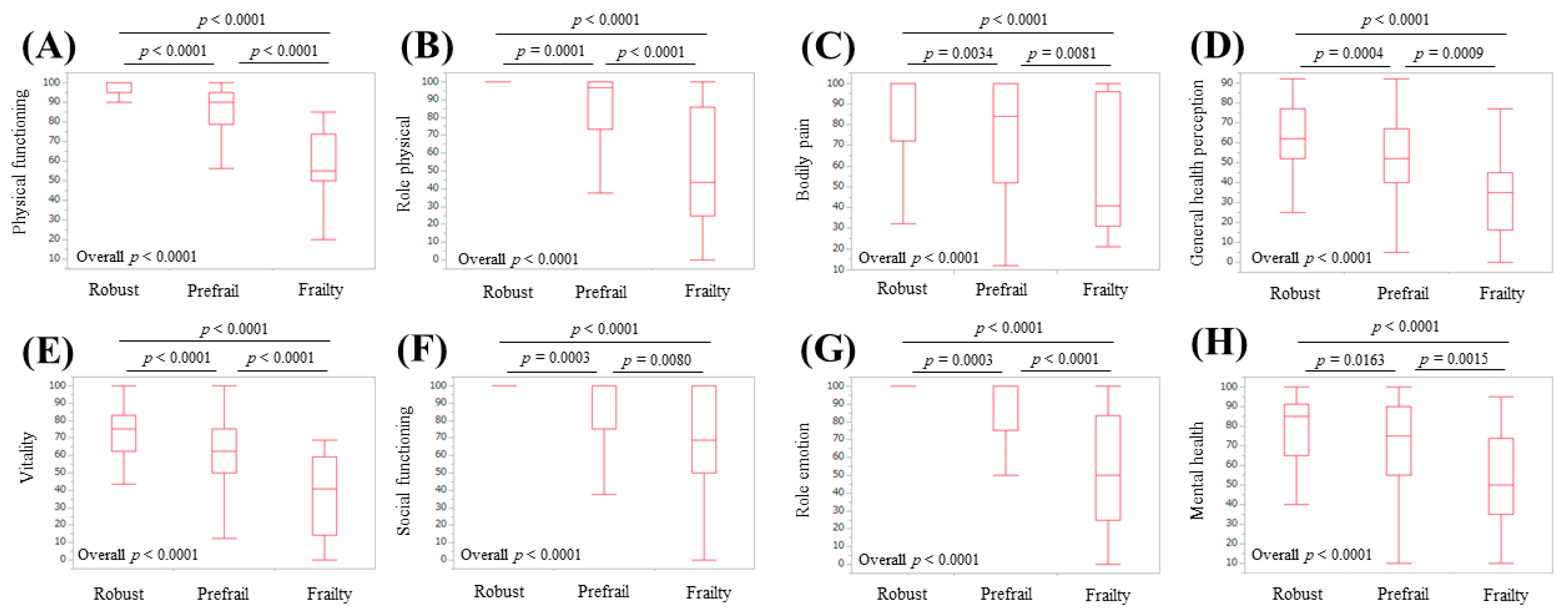
3.4. Subgroup Analysis 2: Scores of the Eight Scales of the SF-36 Relative to the Frailty Status in Non-LC Patients
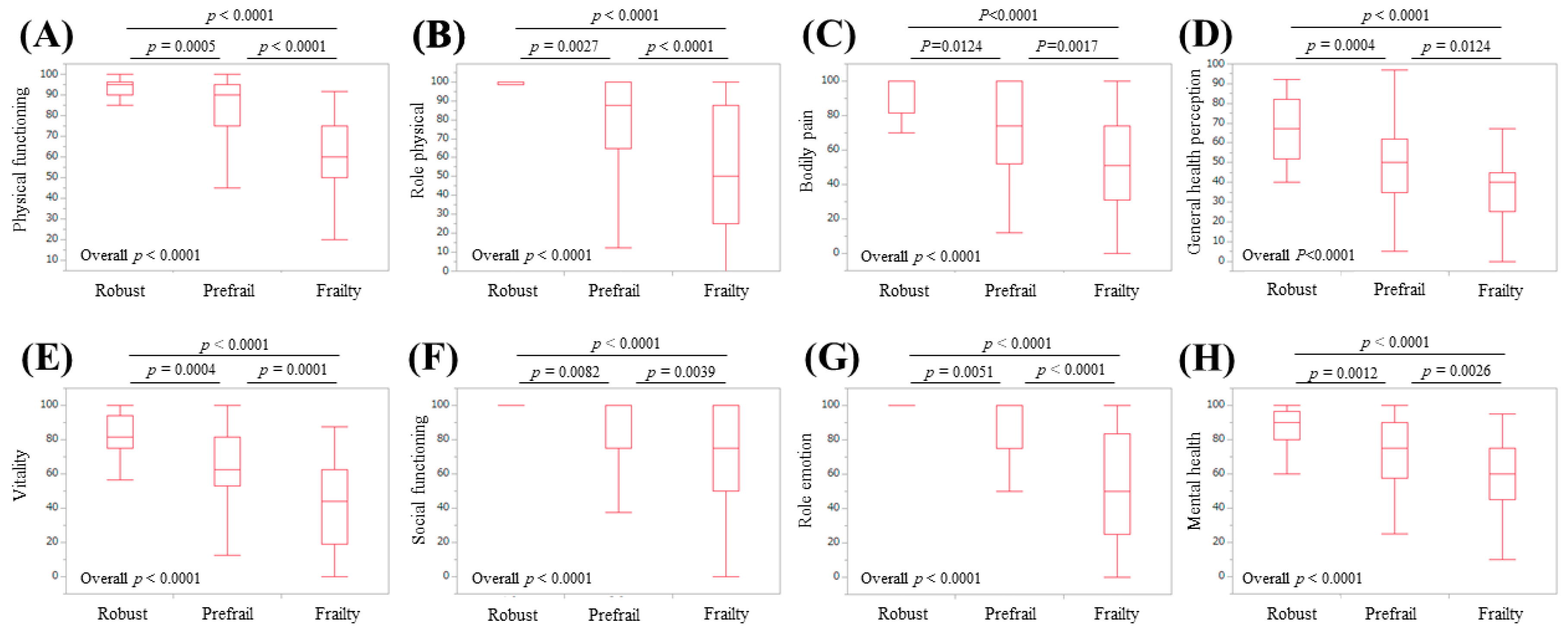
3.5. Subgroup Analysis 3: Scores of the Eight Scales of the SF-36 Relative to the Frailty Status in Male Patients
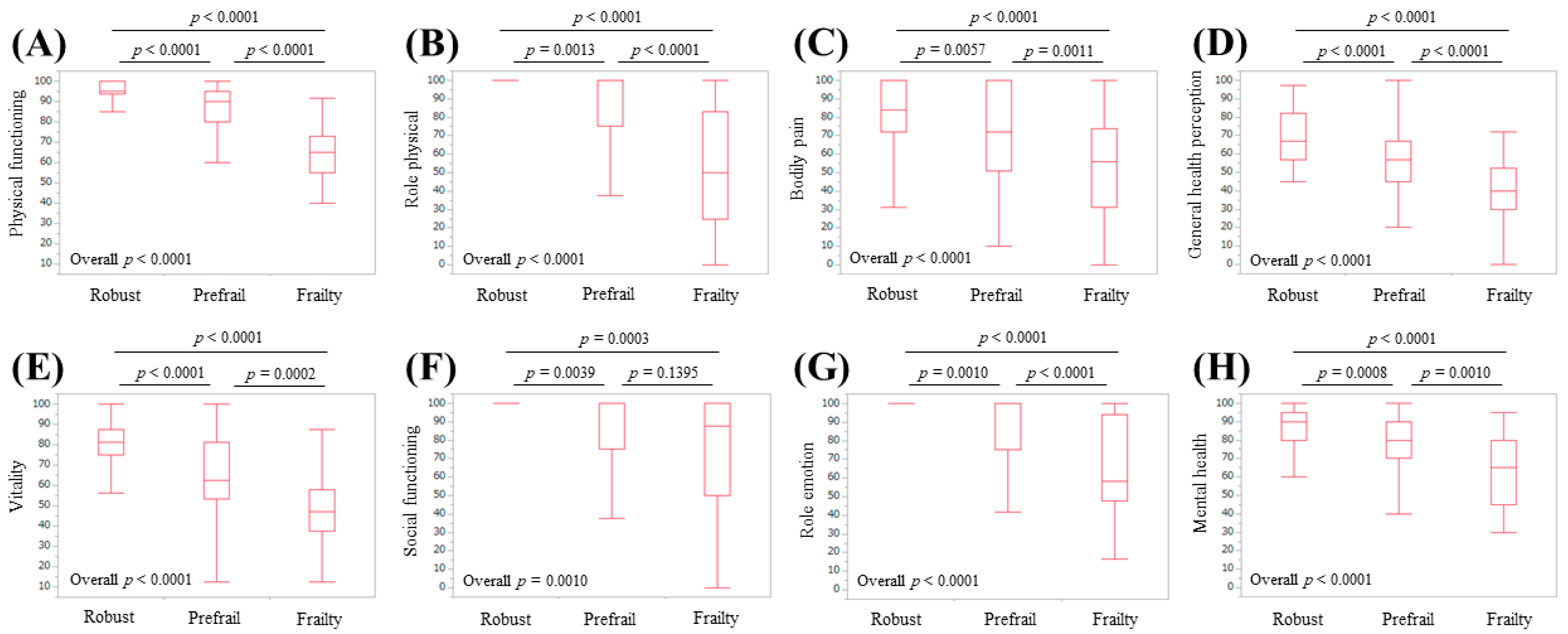
3.6. Subgroup Analysis 4: Scores of the Eight Scales of the SF-36 Relative to the Frailty Status in Female Patients
3.7. Univariate and Multivariate Analysis of Factors Linked to Frailty
4. Discussion
Author Contributions
Acknowledgments
Conflicts of Interest
Abbreviation
| Hr-QOL | health-related quality of life |
| CLDs | chronic liver diseases |
| SF-36 | 36-item Short-Form Health Survey |
| LC | liver cirrhosis |
| BW | body weight |
| GS | grip strength |
| WS | walking speed |
| CHS | Cardiovascular Health Study |
| PCS | physical component summary score |
| MCS | mental component summary score |
| IQR | interquartile range |
| ALBI | albumin-bilirubin |
References
- Lloyd, A.; Sawyer, W.; Hopkinson, P. Impact of long-term complications on quality of life in patients with type 2 diabetes not using insulin. Value Health 2001, 4, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Zambroski, C.H.; Moser, D.K.; Bhat, G.; Ziegler, C. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur. J. Cardiovasc. Nurs. 2005, 4, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Rebollo, P.; Ortega, F.; Baltar, J.M.; Díaz-Corte, C.; Navascués, R.A.; Naves, M.; Ureña, A.; Badía, X.; Alvarez-Ude, F.; Alvarez-Grande, J. Health-related quality of life (HRQOL) in end stage renal disease (ESRD) patients over 65 years. Geriatr. Nephrol. Urol. 1998, 8, 85–94. [Google Scholar] [CrossRef]
- Bottomley, A.; Pe, M.; Sloan, J.; Basch, E.; Bonnetain, F.; Calvert, M.; Campbell, A.; Cleeland, C.; Cocks, K.; Collette, L.; et al. Setting International Standards in Analyzing Patient-Reported Outcomes and Quality of Life Endpoints Data (SISAQOL) consortium. Analysing data from patient-reported outcome and quality of life endpoints for cancer clinical trials: A start in setting international standards. Lancet Oncol. 2016, 17, e510–e514. [Google Scholar] [PubMed]
- Gao, F.; Gao, R.; Li, G.; Shang, Z.M.; Hao, J.Y. Health-related quality of life and survival in Chinese patients with chronic liver disease. Health Qual. Life Outcomes 2013, 11, 131. [Google Scholar] [CrossRef]
- Li, L.; Yeo, W. Value of quality of life analysis in liver cancer: A clinician’s perspective. World J. Hepatol. 2017, 9, 867–883. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, B.M.; Younossi, Z.M.; Hays, R.D.; Revicki, D.; Robbins, S.; Kanwal, F. Impact of hepatitis C on health-related quality of life: A systematic review and quantitative assessment. Hepatology 2005, 41, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Stepanova, M.; Younossi, I.; Pan, C.Q.; Janssen, H.L.A.; Papatheodoridis, G.; Nader, F. Long-term Effects of Treatment for Chronic HBV Infection on Patient-Reported Outcomes. Clin. Gastroenterol. Hepatol. 2018, 17, 1641–1642. [Google Scholar] [CrossRef] [PubMed]
- Schramm, C.; Wahl, I.; Weiler-Normann, C.; Voigt, K.; Wiegard, C.; Glaubke, C.; Brähler, E.; Löwe, B.; Lohse, A.W.; Rose, M. Health-related quality of life, depression, and anxiety in patients with autoimmune hepatitis. J. Hepatol. 2014, 60, 618–624. [Google Scholar] [CrossRef]
- Dyson, J.K.; Wilkinson, N.; Jopson, L.; Mells, G.; Bathgate, A.; Heneghan, M.A.; Neuberger, J.; Hirschfield, G.M.; Ducker, S.J.; UK-PBC Consortium; et al. The inter-relationship of symptom severity and quality of life in 2055 patients with primary biliary cholangitis. Aliment. Pharmacol. Ther. 2016, 44, 1039–1050. [Google Scholar] [CrossRef]
- Younossi, Z.M. Patient-reported Outcomes and the Economic Effects of Non-Alcoholic Fatty Liver Disease and Non-alcoholic Steatohepatitis-The Value Proposition. Hepatology 2018, 68, 2405–2412. [Google Scholar] [CrossRef]
- Tapper, E.B.; Baki, J.; Parikh, N.D.; Lok, A.S. Frailty, Psychoactive Medications, and Cognitive Dysfunction Are Associated With Poor Patient-Reported Outcomes in Cirrhosis. Hepatology 2019, 69, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Kok, B.; Whitlock, R.; Ferguson, T.; Bailey, R.J.; Burak, K.W.; Kowalczewski, J.; Tangri, N.; Tandon, P. Health-Related Quality of Life: A Rapid Predictor of Hospitalization in Patients With Cirrhosis. Am. J. Gastroenterol. 2020, 115, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Williams, F.R.; Berzigotti, A.; Lord, J.M.; Lai, J.C.; Armstrong, M.J. Impact of exercise on physical frailty in patients with chronic liver disease. Aliment. Pharmacol. Ther. 2019, 50, 988–1000. [Google Scholar] [CrossRef] [PubMed]
- Bunchorntavakul, C.; Reddy, K.R. Malnutrition/sarcopenia and frailty in patients with cirrhosis. Aliment. Pharmacol. Ther. 2020, 51, 64–77. [Google Scholar] [CrossRef] [PubMed]
- Aber, A.; Howard, A.; Woods, H.B.; Jones, G.; Michaels, J. Impact of Carotid Artery Stenosis on Quality of Life: A Systematic Review. Patient 2019, 12, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Mikdashi, J. Measuring and monitoring health-related quality of life responsiveness in systemic lupus erythematosus patients: Current perspectives. Patient Relat. Outcome Meas. 2018, 9, 339–343. [Google Scholar] [CrossRef]
- Gerth, A.M.J.; Hatch, R.A.; Young, J.D.; Watkinson, P.J. Changes in health-related quality of life after discharge from an intensive care unit: A systematic review. Anaesthesia 2019, 74, 100–108. [Google Scholar] [CrossRef]
- Paracha, N.; Abdulla, A.; MacGilchrist, K.S. Systematic review of health state utility values in metastatic non-small cell lung cancer with a focus on previously treated patients. Health Qual. Life Outcomes 2018, 16, 179. [Google Scholar] [CrossRef]
- Behboodi Moghadam, Z.; Fereidooni, B.; Saffari, M.; Montazeri, A. Measures of health-related quality of life in PCOS women: A systematic review. Int. J. Womens Health 2018, 10, 397–408. [Google Scholar] [CrossRef]
- Ribeiro, A.R.; Howlett, S.E.; Fernandes, A. Frailty-A promising concept to evaluate disease vulnerability. Mech. Ageing Dev. 2020, 187, 111217. [Google Scholar] [CrossRef] [PubMed]
- Satake, S.; Arai, H. Implications of frailty screening in clinical practice. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 4–10. [Google Scholar] [CrossRef]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Dunn, M.A.; Rogal, S.S.; Duarte-Rojo, A.; Lai, J.C. Physical Function, Physical Activity, and Quality of Life after Liver Transplantation. Liver Transpl. 2020, 26, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Dodge, J.L.; Kappus, M.R.; Dunn, M.A.; Volk, M.L.; Duarte-Rojo, A.; Ganger, D.R.; Rahimi, R.S.; McCulloch, C.E.; Haugen, C.E.; et al. Changes in frailty are associated with waitlist mortality in patients with cirrhosis. J. Hepatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Dodge, J.L.; McCulloch, C.E.; Covinsky, K.E.; Singer, J.P. Frailty and the Burden of Concurrent and Incident Disability in Patients with Cirrhosis: A Prospective Cohort Study. Hepatol. Commun. 2019, 4, 126–133. [Google Scholar] [CrossRef]
- Kojima, G.; Iliffe, S.; Jivraj, S.; Walters, K. Association between frailty and quality of life among community-dwelling older people: A systematic review and meta-analysis. J. Epidemiol. Community Health 2016, 70, 716–721. [Google Scholar] [CrossRef]
- Derck, J.E.; Thelen, A.E.; Cron, D.C.; Friedman, J.F.; Gerebics, A.D.; Englesbe, M.J.; Sonnenday, C.J. In ESLD patient referred for liver transplant, diminished QoL appears to be significantly negatively associated with frailty and not with severity of liver disease as measured MELD. Transplantation 2015, 99, 340–344. [Google Scholar] [CrossRef]
- Nixon, A.C.; Bampouras, T.M.; Pendleton, N.; Mitra, S.; Brady, M.E.; Dhaygude, A.P. Frailty is independently associated with worse health-related quality of life in chronic kidney disease: A secondary analysis of the Frailty Assessment in Chronic Kidney Disease study. Clin. Kidney J. 2019, 13, 85–94. [Google Scholar] [CrossRef]
- Satake, S.; Arai, H. Chapter 1 Frailty: Definition, diagnosis, epidemiology. Geriatr. Gerontol. Int. 2020, 20 (Suppl. 1), 7–13. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Nishikawa, H.; Shiraki, M.; Hiramatsu, A.; Moriya, K.; Hino, K.; Nishiguchi, S. Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol. Res. 2016, 46, 951–963. [Google Scholar] [CrossRef]
- Mchorney, C.A.; Ware, J.E.; Raczek, A.E. The MOS 36-item Short-Form Health Survey (SF-36): Ⅱ. Psychometric and Clinical Tests of Validity in Measuring Physical and Mental Health Constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Mchorney, C.A.; Ware, J.E.; Raczek, A.E. The MOS 36-item Short-Form Health Survey (SF-36): Ⅲ. Tests of Data Quality, scaling Assumptions, and Reliability across Diverse Patient Groups. Med. Care 1994, 32, 40–66. [Google Scholar] [CrossRef] [PubMed]
- Fukuhara, S.; Bito, S.; Green, J.; Hsiao, A.; Kurokawa, K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J. Clin. Epidemiol. 1998, 51, 1037–1044. [Google Scholar] [CrossRef]
- Fukuhara, S.; Ware, J.E.; Kosinski, M.; Wada, S.; Gandek, B. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J. Clin. Epidemiol. 1998, 51, 1045–1053. [Google Scholar] [CrossRef]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef]
- Bunt, S.; Steverink, N.; Olthof, J.; van der Schans, C.P.; Hobbelen, J.S.M. Social frailty in older adults: A scoping review. Eur. J. Ageing 2017, 14, 323–334. [Google Scholar] [CrossRef]
- Nishikawa, H.; Enomoto, H.; Yoh, K.; Iwata, Y.; Sakai, Y.; Kishino, K.; Ikeda, N.; Takashima, T.; Aizawa, N.; Takata, R.; et al. Health-Related Quality of Life in Chronic Liver Diseases: A Strong Impact of Hand Grip Strength. J. Clin. Med. 2018, 7, 553. [Google Scholar] [CrossRef]
- Nishikawa, H.; Osaki, Y. Clinical significance of therapy using branched-chain amino acid granules in patients with liver cirrhosis and hepatocellular carcinoma. Hepatol. Res. 2014, 44, 149–158. [Google Scholar] [CrossRef]

| Variables | All Cases (n = 341) |
|---|---|
| Age (years) | 66 (55, 72) |
| Gender, male/female | 164/177 |
| Liver disease etiology HCV-related/HBV-related/HBV- and HCV-related/NBNC-related | 174/61/7/99 |
| Presence of frailty, yes/no | 46/295 |
| Presence of LC, yes/no | 122/219 |
| Body mass index (kg/m2) | 22.7 (20.5, 25.65) |
| Walking speed (m/s) | 1.303 (1.1005, 1.4445) |
| Grip strength (kg), male | 33.3 (27.925, 38.925) |
| Grip strength (kg), female | 20.8 (17.6, 24.45) |
| Total bilirubin (mg/dL) | 0.8 (0.6, 1.1) |
| Serum albumin (g/dL) | 4.3 (4.0, 4.5) |
| ALBI score | −2.9 (−3.12, −2.6) |
| ALBI grade, 1/2/3 | 256/78/7 |
| Prothrombin time (%) | 91.2 (80.55, 99.05) |
| Platelet count (×104/mm3) | 17.5 (12.6, 22.0) |
| AST (IU/L) | 25 (19, 34) |
| ALT (IU/L) | 19 (14, 33) |
| Total cholesterol (mg/dL) | 181 (151.25, 213) |
| HbA1c (NGSP) | 5.7 (5.4, 6.1) |
| Scales of SF-36 | |
| Physical functioning | 90 (80, 95) |
| Role physical | 100 (75, 100) |
| Bodily pain | 74 (52, 100) |
| General health perception | 55 (45, 71) |
| Vitality | 68.8 (56.2, 81.3) |
| Social functioning | 100 (75, 100) |
| Role emotion | 100 (75, 100) |
| Mental health | 80 (65, 90) |
| Physical component summary score | 51.1 (41.2, 54.3) |
| Mental component summary score | 53.6 (46.0, 59.2) |
| Variables | Univariate Analysis p-Value | Multivariate Analysis | ||
|---|---|---|---|---|
| Estimates | SE | p-Value | ||
| Age (years) | 0.0002 | −0.0499 | 0.020 | 0.0126 |
| Gender | 0.5292 | |||
| Presence of LC | <0.0001 | −0.484 | 0.265 | 0.0685 |
| Body mass index | 0.3701 | |||
| Total bilirubin | 0.9042 | |||
| Serum albumin | <0.0001 | 0.259 | 0.413 | 0.5308 |
| Prothrombin time | 0.2037 | |||
| Platelet count | 0.0543 | |||
| AST | 0.0992 | |||
| ALT | 0.6717 | |||
| Total cholesterol | 0.0815 | |||
| HbA1c (NGSP) | 0.1741 | |||
| Physical functioning | <0.0001 | 0.0434 | 0.0125 | 0.0005 |
| Role physical | <0.0001 | 0.00769 | 0.0102 | 0.4531 |
| Bodily pain | <0.0001 | −0.000804 | 0.0095 | 0.9327 |
| General health perception | <0.0001 | 0.00357 | 0.0139 | 0.7976 |
| Vitality | <0.0001 | 0.0349 | 0.0155 | 0.0246 |
| Social functioning | <0.0001 | −0.0169 | 0.0117 | 0.1481 |
| Role emotion | <0.0001 | 0.0158 | 0.0106 | 0.1384 |
| Mental health | <0.0001 | −0.00394 | 0.0146 | 0.7877 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishikawa, H.; Yoh, K.; Enomoto, H.; Iwata, Y.; Sakai, Y.; Kishino, K.; Shimono, Y.; Ikeda, N.; Takashima, T.; Aizawa, N.; et al. Health-Related Quality of Life and Frailty in Chronic Liver Diseases. Life 2020, 10, 76. https://doi.org/10.3390/life10050076
Nishikawa H, Yoh K, Enomoto H, Iwata Y, Sakai Y, Kishino K, Shimono Y, Ikeda N, Takashima T, Aizawa N, et al. Health-Related Quality of Life and Frailty in Chronic Liver Diseases. Life. 2020; 10(5):76. https://doi.org/10.3390/life10050076
Chicago/Turabian StyleNishikawa, Hiroki, Kazunori Yoh, Hirayuki Enomoto, Yoshinori Iwata, Yoshiyuki Sakai, Kyohei Kishino, Yoshihiro Shimono, Naoto Ikeda, Tomoyuki Takashima, Nobuhiro Aizawa, and et al. 2020. "Health-Related Quality of Life and Frailty in Chronic Liver Diseases" Life 10, no. 5: 76. https://doi.org/10.3390/life10050076
APA StyleNishikawa, H., Yoh, K., Enomoto, H., Iwata, Y., Sakai, Y., Kishino, K., Shimono, Y., Ikeda, N., Takashima, T., Aizawa, N., Takata, R., Hasegawa, K., Koriyama, T., Yuri, Y., Nishimura, T., Nishiguchi, S., & Iijima, H. (2020). Health-Related Quality of Life and Frailty in Chronic Liver Diseases. Life, 10(5), 76. https://doi.org/10.3390/life10050076




