1. Introduction
Adolescent idiopathic scoliosis (AIS) is the most common type of scoliosis affecting children 10 to 18 years of age. In general, AIS curves progress during the rapid growth period [
1], which leads to deformity of the whole trunk, with a negative effect on heart and lung function and a negative cosmetic result.
The most common classification system of AIS is the Lenke classification distinguishing six main scoliotic types according to the localization and number of curves [
2]. Lenke types 1A and 1B in skeletally mature patients are indicated for selective fusion surgical treatment if they exceed 40° of the Cobb angle [
3].
The X-ray imaging technique allows classification of the deformity and helps to determine the type and range of the instrumented fusion. Basic plain standing radiographs are always taken in a long format, which depicts both the lower part of the cranium and the pelvis. Side-bending scans in a supine position provide information about the flexibility of the curve and help to classify the deformity.
Selective posterior spinal instrumentation and fusion (PSIF) remains the gold standard for the surgical treatment of patients with AIS. The goal of surgical treatment is to prevent the progression of the scoliotic deformity, correct the curve, and achieve good spinal stability [
4].
The amount of correction considered sufficient and the correct instrumentation levels are still controversial [
5,
6,
7,
8]. Ideally, the lowest instrumented vertebra (LIV) should be as proximal as possible to preserve lumbar motion but also distal enough to avoid trunk imbalance.
None of the current classification systems of AIS specify the determination of the range of planned PSIF. Modern instrumentation enables effective correction of an operated part of the spine and can abbreviate the area of the necessary bone fusion. It is a global trend to maintain as many unfused spine segments as possible while achieving superior correction of the curve as well as the complex balance of the spine. Maintaining the motion range of the lumbar spine for general compensation and the future physical development of the child are the most important goals of AIS fusion surgery. Selection of the LIV is an art, and there are no official guidelines to determine the right LIV. Clues for this process may be obtained while determining the end, stable, and neutral vertebra [
9].
The right identification of the LIV leads to symmetrical loading of the first free disc below the fusion, which is an important factor for a high-quality surgical result. An excessive shift of the LIV towards the lumbar segments of the spine brings a larger restriction of mobility [
10]. On the contrary, an excessive abbreviation of the instrumentation with the LIV shifted cranially can lead to decompensation of the compensatory curve, the adding-on phenomenon, as well as an asymmetric overload of the unfused disc below fusion (UDBF) [
11].
This study aims to assess whether bending films can affect the determination of the LIV. Our hypothesis is that the higher flexibility of the main structural curve on bending films could help to determine the possible shortening of instrumentation range.
2. Materials and Methods
2.1. Study Design, Setting
This is a consecutive retrospective study based on an X-ray evaluation of patients with AIS operated between 2012 and 2016 at the University Hospital Brno, Brno, Czech Republic.
Although this is a retrospective study, patients were selected consecutively; then, the inclusion criteria were defined. To minimize the selection bias of a retrospective study a prospective study with larger groups of patients would be needed to compare with our results.
Radiographical FU was 2 years for this study and the average clinical followup was 5.8 years (maximum FU 10.8 years; minimum FU 2 years). Patients in this study were not included in randomized controlled trials. Observational data were obtained during routine clinical practice. All of the angles were measured by one experienced radiologist specialized in orthopedics to eliminate inter-observer error. This study provided real-world data.
2.2. Subjects
We set the inclusion criteria to match our ideal indication for AIS surgical treatment.
The inclusion criteria for the study were as follows: progressive AIS with insufficient previous conservative treatment with a severity more than 40° of Cobb angle in the major structural thoracic curve; adolescent age of 12–16 years; Lenke type 1A or B; Risser sign 4 or 5.
The exclusion criteria were previous surgery of the musculoskeletal system and Lenke type 1C (this type is often connected to unsatisfactory clinical outcomes and risk of revision surgery) [
5].
All study subjects underwent PSIF with transpedicular all-screw (43 patients) or hybrid fixation (25 patients). Postoperatively, all patients were examined clinically and radiologically using plain standing radiographs on the 5th day after surgery, after 4 months, one year, and two years after surgery.
2.3. Operation Technique
During screw/hooks insertion, facetectomy was performed. This allows a posterior spine release and provides autograft for bone fusion. The correction maneuver used the simultaneous double rod rotation technique [
4]. Both rods were bent into kyphosis and introduced on both sides of the curve. Set screws were applied to the anchor points but not fully tightened. Both rods were then simultaneously rotated to the concavity of the curve by 90°. Anchor points of the apical vertebra were fully tightened. Correction continued with segmental compressions on the concavity and segmental distractions of the convexity of the curve. After the final correction, the spine was decorticated, and autografts were added posterolaterally to provide a bone fusion.
2.4. X-ray Parameters and Measurements
Each patient had preoperative long format standing radiographs in posteroanterior (PA) and lateral projections, as well as side-bending radiographs, focused on the apices of each curve.
Bending films are crucial for curve flexibility assessment as well as for classifying according to Lenke rules [
2]. The bending films in our study were acquired in the supine position on the X-ray table, while the patient was instructed to perform maximum trunk inclination to the side of the convexity of the examined curve.
The severity of the deformity was measured using the Cobb angle on the PA plain standing radiographs.
The disc angle below the LIV was measured. The criteria of local decompensation were determined as wedging of the UDBF of >5° at the last check-up. This asymmetrical disc loading is a risk factor for adding-on phenomenon and degenerative disc disease [
12].
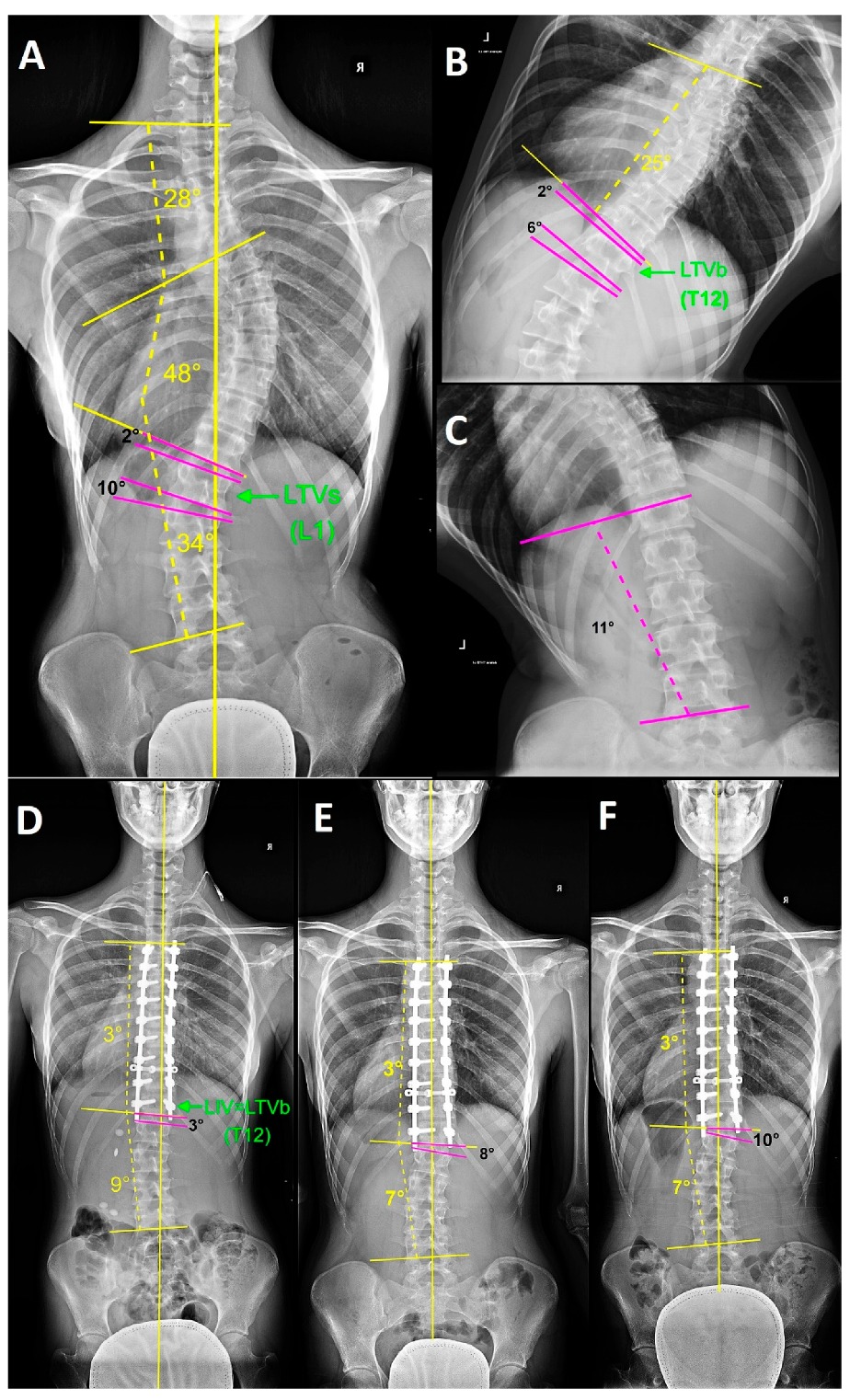
The last caudal vertebra of the main thoracic curve below which the disc opened at least 5° towards the opposite side from the main curve was identified as the lower tilted vertebra (LTV). The LTV was selected in both types of X-rays, the standing PA projection (LTVs) as well as the bending X-rays in a horizontal position (LTVb) (
Figure 1).
According to the possibility of structural changes in the vertebral shape, this vertebra did not have to be the end vertebra. The same method was applied to the side-bending radiographs (LTVb).
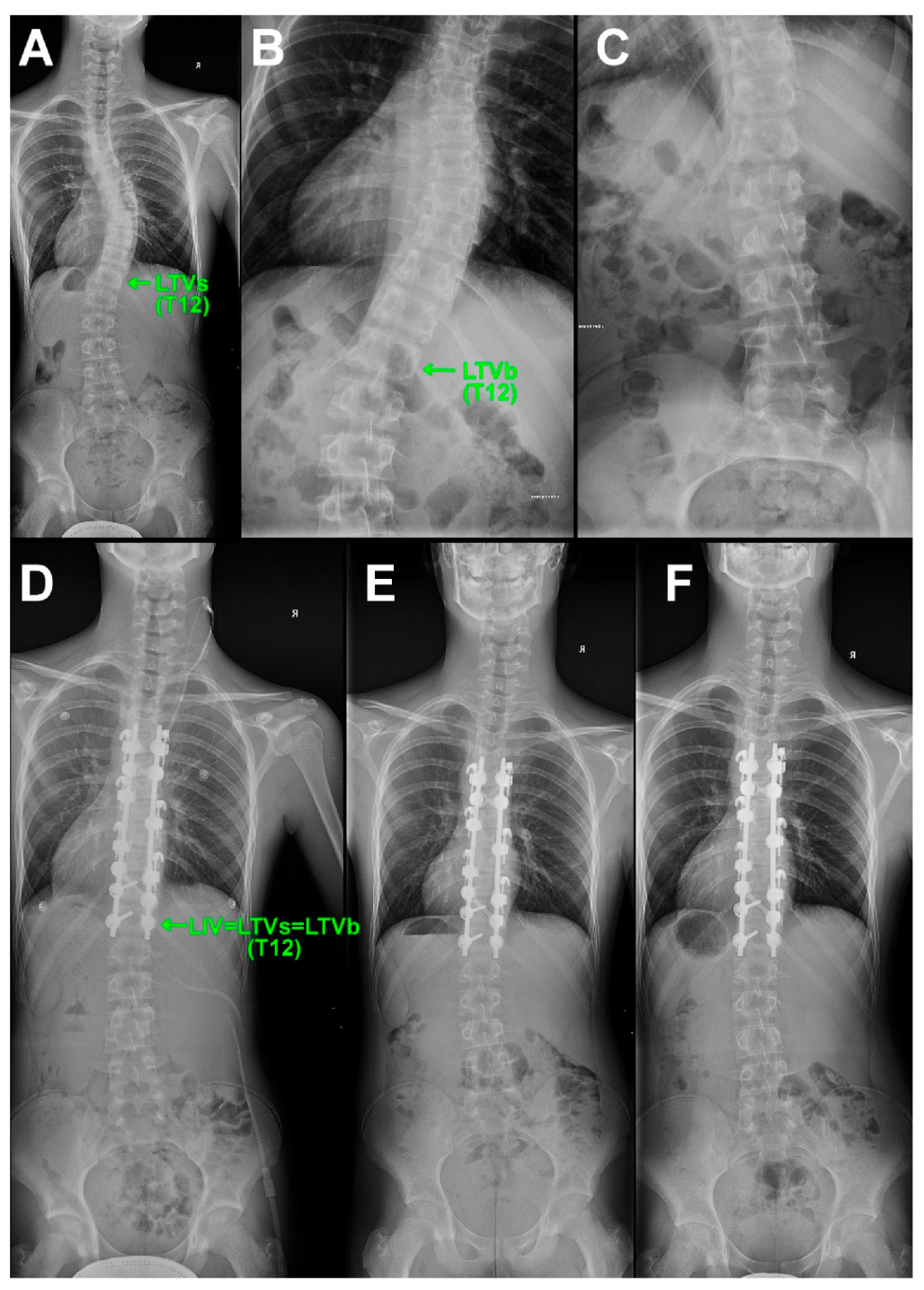
The decompensation of UDBF was demonstrated in a patient with a shorter range of instrumented spinal fusion from group C, where LIV = LTVb (
Figure 2).
2.5. Groups Selection
The followed-up group of patients was divided into two basic groups. Control group A consisted of patients whose preoperative LTVs were equal to the LTVb; thus, no cranial shift of LTV appeared on the bending film. LIV = LTVs = LTVb (
Figure 3).
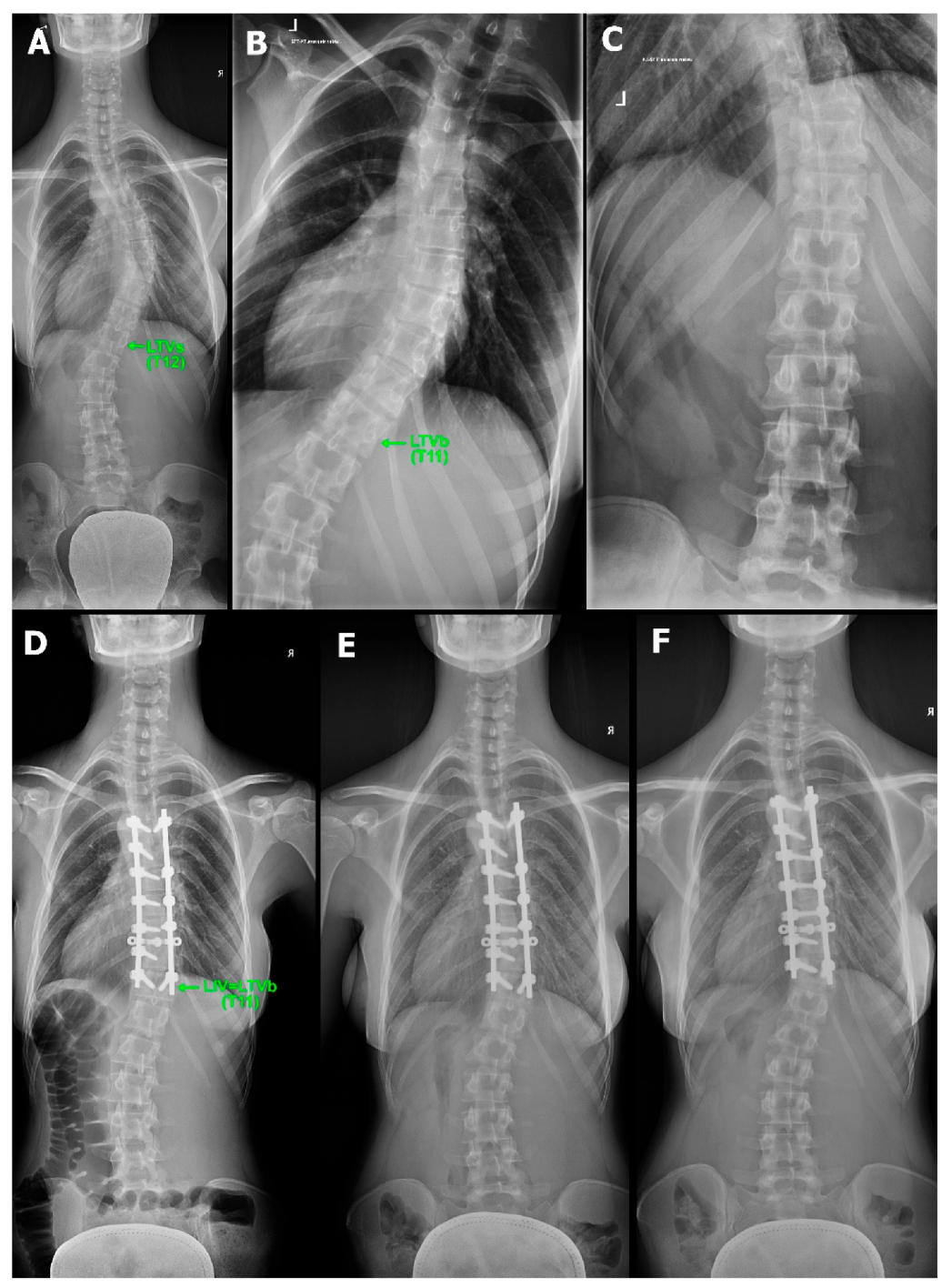
Groups B and C consisted of patients who had a cranial shift of the LTV by one segment on the bending film according to more flexible curves. Patients in group B were treated with the PSIF ending at the LIV = LTVs (despite the LTVb being one segment cranial to the LTVs) (
Figure 4).
Patients in group C were treated with shorter instrumented spinal fusion ending at the LIV = LTVb (
Figure 5).
We assumed that if the LIV was equal to the LTVb, the decompensation of the first disc below the LIV would not become significantly worse in comparison with LIV = LTVs. If this hypothesis was confirmed, it would be possible to shorten the surgical instrumentation selectively without the risk of postoperative decompensation of the UDBF.
2.6. Statistical Methods
According to the null hypothesis, there is no difference between merged groups A and B (LIV = LTVs) compared to group C (LIV = LTVb). The followed-up parameters were statistically analyzed by Fisher’s exact test and the chi-square test; the level of significance was set to 5% (p < 0.05). The test aimed to determine the dependence between the representation of decompensations between merged groups A and B and group C. The difference was statistically significant in Fischer´s exact test (p = 0.033) and the chi-square test (p = 0.027). The null hypothesis was rejected. Data were analyzed using IBM SPSS Statistics for Windows, Version 28.0.0.0 (IBM Corp. Released 2021, Armonk, NY, USA: IBM Corp).
3. Results
The study group comprised 68 retrospectively consecutively evaluated patients with AIS operated between 2012 and 2016, 10 males and 58 females. Our subjects were 14.7 years of age on average at the time of surgery (range 12–16). In total, 35 patients were Lenke type 1A, and 33 patients were Lenke type 1B. Risser sign 4 had 54 patients, and Risser sign 5 had 14 patients. The average Cobb angle of the main thoracic curve preoperatively was 49.1° (range 40–79°) and postoperatively 9.9° (range 0–31°). The average Cobb angle of the compensatory lumbar curve preoperatively was 30.7° (range 16–43°) and postoperatively 9° (range 8.5–28°).
In group A (36 patients), the achieved correction of the main operated scoliotic curve was from 50° on average (range: 41–79°) before surgery to 10.3° on average (range 0–35°), with a median value of 76% correction after the surgery.
The loss of correction at 12 and 24 months of the followup was 1.4° on average (3%) and 2.2° (4%), respectively. The disc wedging below the LTVs was on average −5.4° preoperatively, +0.4° after the operation, +2.9° four months after the operation, +3.3° one year postoperatively, and +3.5° two years after surgery. Radiologically significant decompensation, according to the decompensation criteria, was found in 11 cases.
In group B (12 patients), the main operated scoliotic curve was corrected from 52° (range 43–66°) before the surgery to 13.8° (range 8–24°), with a median of 73% correction after the surgery. At the 12- and 24-months followup, the loss of correction reached 1.6° (3%) and 2.1° (4%), respectively. The disc wedging below the LTVb was on average −5.8° preoperatively, +1.0° after the surgery, +3.7° four months after the surgery, +3.6° one year after the surgery, and +3.6° two years after the surgery. Radiologically significant decompensation, according to the decompensation criteria, was found in 4 cases.
In group C (20 patients), the reached correction of the main operated scoliotic curve was from 45.7° (41–54) before the surgery to 8.2° (0–20), with a median of 82% correction after the surgery. At the 12- and 24-months followup, the loss of correction reached 0.9° (2%) and 1.5° (3%), respectively. The disc wedging below the LTVb was on average −2.2° preoperatively, +2.2° after the surgery, +4.3° four months after the operation, +5.3° one year after the surgery, and +6.2° two years after surgery. Radiologically significant decompensation, according to the decompensation criteria, was found in 12 cases.
One patient from group C was indicated for reoperation with the necessity of prolonging the instrumented fusion caudally, based on the decompensation on X-ray examination with clinical correlation.
Based on the previously stated criteria, the decompensation of the UDBF appeared in 31% in group A and 33% in group B. In contrast, in group C, where the instrumented fusion was shortened according to the side-bending radiographs, the decompensation appeared in 60% of the patients (
Figure 6).
4. Discussion
This study aimed to assess whether bending films could affect the determination of the LIV and at the same time prevent the decompensation of non-operated spinal segments in the postoperative followup period in patients with Lenke types 1A and 1B AIS. The study results showed that in more flexible curves shortening of the PSIF to LIV = LTVb should be avoided. The risk of decompensation in the UDBF with the possibility to develop into the adding-on phenomenon was 60%. Our recommendation is to consider using this method of LIV selection along with other LIV selection criteria [
13,
14,
15,
16].
The findings of this study have to be seen in the light of two major limitations. First, according to the retrospective study concept, selection bias cannot be ruled out. Second, the inclusion criteria of this study mentioned above were to present a typical patient who underwent a selective thoracic spinal fusion. According to the strict inclusion criteria, the final group of patients was relatively small. A prospective study with larger groups of patients would be needed to compare with our results.
Polly and Vaughan concluded that supine bending films have greater importance in curves up to 50°, and traction films more effectively ensure genuine flexibility in curves over 50° [
17,
18].
Curve flexibility in adolescent idiopathic scoliosis has been one of the major concerns of spinal surgeons since the evolution of surgical correction techniques [
19]. All surgeons have been trying to identify which criteria are the most important for curve flexibility assessment. Since the beginning of segmental instrumentations, interest in the effective range of instrumentation and possibilities of further examinations of flexibility has increased.
Three-dimensional correction of the lateral bending of the trunk was proved in a kinematic study in vivo by Fujimori [
20]. Coupled axial rotation generally occurred in the same direction as lateral bending. The standing side-bending images of the EOS device contributed the same results as the supine images, with a five times lower radiation dose [
21]. Nevertheless, none of these techniques were referred to specify the LIV.
The patients from this study underwent PSIF at our institution either with hybrid constructs or with all screw constructs. Between 2012 and 2016, the correction maneuver was achieved by derotation of the rod and further compressions and distractions. During this period, vertebral column manipulation and direct vertebral rotation were not included in the correction maneuver.
The modern correction methods, direct vertebral rotation (DVR) and vertebral column manipulation (VCM), are very powerful in the correction of the deformity and help us to shorten the range of PSIF. Horizontalization of the UDBF is also a good prognostic parameter. On the contrary, there can be a risk of overloading the UDBF with derotation forces [
22,
23,
24].
Whether VCM and DVR correction techniques can lead to preserving more motion segments in selective spinal fusion should be the next step in further research.
Burton et al., chose the LIV according to the ability of a vertebra to become horizontal on convexity bending radiographs, which would subsequently be determined as the caudal foundation vertebra [
8]. Determination of the optimal parameters of the measurement, as well as the postulation of an eventual unsatisfactory result, can vary. Kim [
25] measured the lowest instrumented vertebral tilt (LIVT), and he defined an unsatisfactory result as a LIVT of more than 10° or a coronal balance of more than 15 mm. Clement [
12] monitored changes in the tilt of the first distal non-instrumented vertebra. He found that the main variables associated with tilt ≤5° were a final correction percentage of ≥60% and an absence of correction loss between the postoperative period and the last followup. Minimal progression of UDBF decompensation in groups A and B compared to group C was also confirmed in our study. Patients from group C with a UDBF > 5° had a higher rate of decompensation.
In this study, the disc wedging angle below the fusion was evaluated and compared with the compensation of the whole spine measured by CSVL at the same time. This method is being used in our institution for followup of the further state and disc loading below the fusion. The criteria of the disc decompensation, wedging of the UDBF of 5° or more at the last check-up after the surgery, is purposely strict for better evaluation of the case collection.
The importance of symmetric loading of the first free disc below the fusion has been pointed out in several studies. Violas [
26] concluded that the recovery of balanced positioning and inherent biomechanical loads could induce restored hydration of the disc, which should favor the remodeling of free segments. In another prospective magnetic resonance imaging (MRI) study, Abelin-Genevois [
27] found significant and sustainable improvement in the MRI T2 hyper signal of the disc, indirectly indicating an improvement of disc hydration after AIS surgery. Green [
28] followed up on the long-term status of non-fused segments after operation using MRI scans. In their long-term MRI followup study, they reached good functional scores and maintenance of correction over 10 years after fusion. Disc degeneration was found remote to the lowest instrumented vertebra.
5. Conclusions
The bending films can distinguish between rigid and flexible curves. Excessive shortening of instrumented fusion in flexible curves should be avoided. The risk of UDBF decompensation in more flexible curves with instrumentation ending at LIV = LTVb was two times higher. Ending the instrumentation at LIV = LTVs is the method of choice. The method described in this study should be added as one of the factors for correct LIV selection.
Author Contributions
Conceptualization, M.P. and M.R.; Methodology, M.P. and M.R.; Data curation, R.V.; Formal analysis, M.P.; Investigation, J.S. and A.S.-P.; Project administration, J.K.; Resources, J.K. and A.S.-P.; Software, A.S.-P.; Supervision, M.R.; Validation, M.F.; Writing—original draft preparation, M.P.; Writing—review & editing, R.V. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Ministry of Health, Czech Republic—Conceptual Development of Research Organization (FNBr, 65269705). The funder had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Institutional Review Board Statement
All procedures performed in studies involving human participants followed the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical committee name: Etická komise, Fakultní nemocnice Brno, Jihlavská 20, 62500 Brno, Czech Republic; Evidence number of ethical approval: 02-100112/EK; Date of approval: 10 January 2012.
Informed Consent Statement
Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Conflicts of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- Ylikoski, M. Growth and progression of adolescent idiopathic scoliosis in girls. J. Pediatr. Orthop. B 2005, 14, 320. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G. Lenke classification system of adolescent idiopathic scoliosis: Treatment recommendations. Instr. Course Lect. 2005, 54, 537–542. [Google Scholar] [PubMed]
- Westrick, E.R.; Ward, W.T. Adolescent Idiopathic Scoliosis: 5-Year to 20-Year Evidence-based Surgical Results. J. Pediatr. Orthop. 2011, 31, S61. [Google Scholar] [CrossRef] [PubMed]
- Theruvath, A.S.; Mahajan, R.; Gururaj, M.; Chhabra, H.S.; Tandon, V.; Nanda, A. Correction maneuvers in scoliosis surgery—An overview. Kerala J. Orthop. 2012, 25, 73–77. [Google Scholar]
- Wang, Y.; Bünger, C.E.; Wu, C.; Zhang, Y.; Hansen, E.S. Postoperative trunk shift in Lenke 1C scoliosis: What causes it? How can it be prevented? Spine 2012, 37, 1676–1682. [Google Scholar] [CrossRef] [PubMed]
- Atici, Y.; Erdogan, S.; Akman, Y.E.; Mert, M.; Carkci, E.; Tuzuner, T. The Surgical Overcorrection of Lenke Type 1 Deformities with Selective Fusion Segments: What Happens to the Coronal Balance? Korean J. Spine 2016, 13, 151–156. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Takahashi, J.; Newton, P.O.; Ugrinow, V.L.; Bastrom, T.P. Selective thoracic fusion in adolescent idiopathic scoliosis: Factors influencing the selection of the optimal lowest instrumented vertebra. Spine 2011, 36, 1131–1141. [Google Scholar] [CrossRef]
- Burton, D.C.; Asher, M.A.; Lai, S.-M. The Selection of Fusion Levels Using Torsional Correction Techniques in the Surgical Treatment of Idiopathic Scoliosis. Spine 1999, 24, 1728. [Google Scholar] [CrossRef][Green Version]
- Ni, H.-J.; Su, J.C.; Lu, Y.H.; Zhu, X.D.; He, S.S.; Wu, D.J.; Xu, J.; Yang, C.W.; Wang, C.F.; Zhao, Y.C.; et al. Using Side-bending Radiographs to Determine the Distal Fusion Level in Patients with Single Thoracic Idiopathic Scoliosis Undergoing Posterior Correction with Pedicle Screws. Clin. Spine Surg. 2011, 24, 437. [Google Scholar] [CrossRef]
- Udoekwere, U.I.; Krzak, J.J.; Graf, A.; Hassani, S.; Tarima, S.; Riordan, M.; Sturm, P.F.; Hammerberg, K.W.; Gupta, P.; Anissipour, A.K.; et al. Effect of Lowest Instrumented Vertebra on Trunk Mobility in Patients with Adolescent Idiopathic Scoliosis Undergoing a Posterior Spinal Fusion. Spine Deform. 2014, 2, 291–300. [Google Scholar] [CrossRef]
- Suk, S.-I.; Lee, S.-M.; Chung, E.-R.; Kim, J.-H.; Kim, W.-J.; Sohn, H.-M. Determination of Distal Fusion Level with Segmental Pedicle Screw Fixation in Single Thoracic Idiopathic Scoliosis. Spine 2003, 28, 484. [Google Scholar] [CrossRef]
- Clément, J.-L.; Solla, F.; Tran, A.; Morin, C.; Lakhal, W.; de Gauzy, J.S.; Leroux, J.; Gennari, J.M.; Parent, F.H.; Kreichati, G.; et al. Five-year outcomes of the First Distal Uninstrumented Vertebra after posterior fusion for Adolescent Idiopathic Scoliosis Lenke 1 or 2. Orthop. Traumatol. Surg. Res. OTSR 2017, 103, 727–731. [Google Scholar] [CrossRef]
- Qin, X.; Qiu, Y.; He, Z.; Yin, R.; Liu, Z.; Zhu, Z. Can We Stop Distally at LSTV-1 for Adolescent Idiopathic Scoliosis with Lenke 1A/2A Curves? Spine 2022, 47, 624–631. [Google Scholar] [CrossRef]
- Ifthekar, S.; Ahuja, K.; Sudhakar, P.V.; Mittal, S.; Yadav, G.; Kandwal, P.; Sarkar, B.; Goyal, N. Is it Safe to Save Levels and Choose the Lowest Instrumented Vertebra as Touched Vertebra While Selectively Fusing Lenke 1/2 Curves? A Proportional Meta-Analysis of Existing Evidence. Glob. Spine J. 2022, 21925682221091744. [Google Scholar] [CrossRef]
- Tao, F.; Shi, Z.; Xie, Y.; Pan, F.; Wu, Y.; Zhang, Y.; Wang, Z.; Li, M. Determination of lowest instrumented vertebra by the location of apical vertebra in Lenke type 1 adolescent idiopathic scoliosis. Int. Orthop. 2011, 35, 561–567. [Google Scholar] [CrossRef][Green Version]
- Hyun, S.-J.; Lenke, L.G.; Kim, Y.; Bridwell, K.H.; Cerpa, M.; Blanke, K.M. Adolescent Idiopathic Scoliosis Treated by Posterior Spinal Segmental Instrumented Fusion: When Is Fusion to L3 Stable? J. Korean Neurosurg. Soc. 2021, 64, 776–783. [Google Scholar] [CrossRef]
- Polly, D.W.; Sturm, P.F. Traction versus supine side bending. Which technique best determines curve flexibility? Spine 1998, 23, 804–808. [Google Scholar] [CrossRef]
- Vaughan, J.J.; Winter, R.B.; Lonstein, J.E. Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. J. Pediatr. Orthop. 1997, 17, 416. [Google Scholar] [CrossRef]
- Ameri, E.; Behtash, H.; Mobini, B.; Daraie, A. Predictors of curve flexibility in adolescent idiopathic scoliosis: A retrospective study of 100 patients. Acta Med. Iran. 2015, 53, 182–185. [Google Scholar]
- Fujimori, T.; Iwasaki, M.; Nagamoto, Y.; Matsuo, Y.; Ishii, T.; Sugiura, T.; Kashii, M.; Murase, T.; Sugamoto, K.; Yoshikawa, H. Kinematics of the thoracic spine in trunk lateral bending: In vivo three-dimensional analysis. Spine J. 2014, 14, 1991–1999. [Google Scholar] [CrossRef]
- Hirsch, C.; Ilharreborde, B.; Mazda, K. Flexibility analysis in adolescent idiopathic scoliosis on side-bending images using the EOS imaging system. Orthop. Traumatol. Surg. Res. 2016, 102, 495–500. [Google Scholar] [CrossRef]
- Lee, S.-M.; Suk, S.-I.; Chung, E.-R. Direct Vertebral Rotation: A New Technique of Three-Dimensional Deformity Correction with Segmental Pedicle Screw Fixation in Adolescent Idiopathic Scoliosis. Spine 2004, 29, 343–349. [Google Scholar] [CrossRef]
- Pankowski, R.; Roclawski, M.; Ceynowa, M.; Mikulicz, M.; Mazurek, T.; Kloc, W. Direct Vertebral Rotation Versus Single Concave Rod Rotation: Low-dose Intraoperative Computed Tomography Evaluation of Spine Derotation in Adolescent Idiopathic Scoliosis Surgery. Spine 2016, 41, 864–871. [Google Scholar] [CrossRef]
- Obeid, I.; Aurouer, N.; Hauger, O.; Gille, O.; Pointillart, V.; Vital, J.M. 209. Axial Vertebral Rotation (AVR) Correction in All Screws Posterior Construct for Adolescent Idiopathic Scoliosis (AIS): Does Vertebral Column Manipulation (VCM) Help? Spine J. 2009, 9, 110S–111S. [Google Scholar] [CrossRef]
- Kim, S.-S.; Lim, D.J.; Kim, J.H.; Kim, J.W.; Um, K.S.; Ahn, S.H.; Suk, S.I. Determination of the Distal Fusion Level in the Management of Thoracolumbar and Lumbar Adolescent Idiopathic Scoliosis Using Pedicle Screw Instrumentation. Asian Spine J. 2014, 8, 804–812. [Google Scholar] [CrossRef]
- Violas, P.; Estivalezes, E.; Briot, J.; de Gauzy, J.S.; Swider, P. Quantification of Intervertebral Disc Volume Properties Below Spine Fusion, Using Magnetic Resonance Imaging, in Adolescent Idiopathic Scoliosis Surgery. Spine 2007, 32, E405. [Google Scholar] [CrossRef]
- Abelin-Genevois, K.; Estivalezes, E.; Briot, J.; Sévely, A.; de Gauzy, J.S.; Swider, P. Spino-pelvic alignment influences disc hydration properties after AIS surgery: A prospective MRI-based study. Eur. Spine J. 2015, 24, 1183–1190. [Google Scholar] [CrossRef]
- Green, D.W.; Lawhorne, T.W., III; Widmann, R.F.; Kepler, C.K.; Ahern, C.; Mintz, D.N.; Rawlins, B.A.; Burke, S.W.; Boachie-Adjei, O. Long-Term Magnetic Resonance Imaging Follow-up Demonstrates Minimal Transitional Level Lumbar Disc Degeneration After Posterior Spine Fusion for Adolescent Idiopathic Scoliosis. Spine 2011, 36, 1948. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).