Abstract
Background: Non-absorbable materials (nylon) are always used in cinch sutures to maintain nasal width and to improve harmonious facial symmetry in orthognathic surgery. However, a few drawbacks of nylon materials have been clinically reported following orthognathic surgery, such as nasal irritation and exposure of the sutures. An absorbable material (PDS) has been proposed in cinch sutures, not only to avoid the complications of nylon but also to stabilize the nasal width for a long-term follow-up. Methods: Fifty-seven patients with Angle’s malocclusion classification III receiving orthognathic surgery were enrolled in this study. A non-absorbable material (nylon) and an absorbable material (PDS) were utilized for the cinch sutures. Pre-operative (T1) and post-operative six-month (T2) craniofacial 3D images were collected for all patients to measure the alar curvature (Ac) width and the alar base (Al) width. A significance level of p < 0.05 was applied in the statistical analysis. Results: With the approval of IRB, cinch suturing was performed with nylon in 29 patients and with PDS in 28 patients. Pre-operative Ac and Al distances showed no significant difference between these two groups. There were also no significant differences between the suture materials in the peri-operative change in nasal width, including Ac (nylon: 1.999 ± 1.40; PDS: 1.484 ± 0.97; p = 0.112) and Al (nylon: 1.861 ± 1.66; PDS: 1.115 ± 0.92; p = 0.056). Conclusions: For cinch sutures in orthognathic surgery, PDS can maintain the peri-operative nasal width similarly to nylon; additionally, it can be absorbed in a timely manner without the drawbacks of non-absorbable materials.
1. Introduction
In Steiner’s definition, class III malocclusion patients present a protrusive mandible and/or retrusive maxilla with a concave lateral facial profile [1,2]. Bimaxillary orthognathic surgery is commonly performed in class III malocclusion patients to improve both occlusal function and facial esthetics and is able to provide a stable, long-term symmetric outcome [3,4]. Despite skeletal movement, a change in the related soft tissue after surgery, especially the nasolabial region, is also a major concern for patients. Nasal alar and alar base widening has been observed after superior/anterior repositioning Le Fort I osteotomy [5,6], which would tend to post-operative nasal asymmetry in the result of an unfavorable outcome. Therefore, the target is to achieve symmetrical facial esthetics by maintaining an original nasal width following the procedure.
One method for controlling post-operative nasal soft tissue change is alar cinch sutures. Cinch sutures were developed to correct the flat and flaring nose in cleft lip deformity and was later applied to avoid nasal change after Le Fort I osteotomy [7]. Classic cinch sutures pass through bilateral fibro-areolar tissue at the alar–facial junction intraorally, which tightens both sides in the middle [8,9,10]. In a recent study, the authors described several modified alar cinch methods that have been developed, such as anchoring to the dermis, alar base skin, or nasal septum, in order to provide more security [8,9,10,11,12,13].
Non-absorbable monofilament sutures, such as nylon or polypropylene (Prolene), have been used in alar cinch sutures due to their stability during wound healing. However, in clinical practice, we noticed some patients with knot exposure from the oral mucosa or palpability through the skin during post-operative follow-up. Slow-absorbable sutures of monofilament polydioxanone (PDS) have been widely used in all kinds of tissue approximation or lifting, including rhinoplasty [14], brow lift [15], and laparotomy fascial closure [16]. Using characteristics such as the smooth and slow absorption of polydioxanone suture, we tried to undertake cinch suturing with this material.
To the best of our knowledge, there is no literature comparing the different materials for alar cinch sutures. The aim of this study was to assess the effectiveness and results of alar width change by two different materials in cinch sutures after orthognathic surgery.
2. Materials and Methods
2.1. Study Design
A case–control study was conducted in Chang Gung Craniofacial Center, Taoyuan, Taiwan from January 2017 to April 2019 and was approved by the Institutional Review Board (IRB No. 202100100B0). A total of 57 consecutive patients scheduled for elective two-jaw orthognathic surgery were collected by two craniofacial surgeons performing the same techniques (one-piece Le Fort I osteotomy and bilateral sagittal splitting osteotomy) and protocols. The study’s inclusion criteria were as follows: (1) at least 18 years old, (2) Angel’s class III malocclusion and ANB angle less than 0 degrees, and (3) received orthognathic surgery involving Le Fort I osteotomy and maxillary advancement or impaction. We excluded patients who received multi-segmented Le Fort I osteotomy, or who presented with a cleft lip or palate, or who had a history of rhinoplasty or nasal bone fracture.
Among these patients, 29 patients were allocated to the nylon (Ethilon®, Johnson & Johnson Ltd.: Somerville, N.J., U.S.) group and the other 28 patients to the polydioxanone (PDS®, Johnson & Johnson Ltd.: Somerville, N.J., U.S.) group. The primary aim of this study was to compare the nasal alar base width change in alar cinch suturing after orthognathic surgery using nylon and PDS. This was achieved by measuring the differences of nasal width in three-dimensional photographs before and after OGS.
2.2. Surgical Method
Bimaxillary orthognathic surgery was carried out under general anesthesia with nasotracheal tube intubation. Before intubation, a sliding caliber was used for measuring the widest alar width (Al-Al) of the patient as the reference for post-operative alar cinch suture tightness. Bilateral sagittal split osteotomy was performed using the modified Hunsuck technique [17]. An upper buccal sulcus incision was made from one side of the lateral buttress to the other. The incision cut through the bilateral levator and depressor labii superioris and elevated the sub-periosteal plane to the pyriform edges. Le Fort I osteotomy was carried out by saw and Dautrey osteotome [18]. The final maxillomandibular complex (MMC) position was decided through pre-operative planning and also intra-operative facial profile considerations [16]. After temporarily wiring the MMC to the desired position, the Le Fort I osteotomy sites were fixed by four L-shape mini-plates over the medial and lateral buttresses. A hole was made on the anterior nasal spine (ANS) by a drill. Then, the alar cinch sutures, either non-absorbable 3-0 nylon or absorbable 3-0 PDS, passed through the perinasal musculature, up to anchoring the dermis over the alar base bilaterally, and were fixed to the hole over the ANS [19] (Figure 1). The bilateral alar bases were approximated by sutures that were the same or slightly smaller (2 mm) than the pre-operative alar width. At least five turns were made on the knot. The mucosal wound was closed by 4-0 Dexon sutures in a continuous fashion without V-Y flap advancement. The patient had a liquid diet for at least five days and a soft diet for one month post-operation.
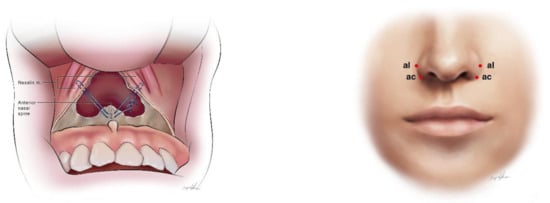
Figure 1.
(left) Cinch sutures approximating the ANS with bilateral nasalis muscles. (right) Alare (Al): The most lateral point of the alar contour; alar curvature (Ac): The point located at the facial insertion of the alar base.
2.3. Assessment of Nasal Soft Tissue Change
Three-dimensional (3D) stereophotogrammetry of the face was obtained using the 3dMD system (3dMD Inc., Atlanta, GA, USA) before surgery (T0) and six months after surgery (T1). While the images were taken, every patient was instructed to keep their facial muscles and lips relaxed, with a neutral facial expression and their head in a natural position. The 3D photography reference plane was set following the method of [20]: (1) the horizontal reference plane: the line connecting the alar and tragus plane was rotated 7.5 degrees upward on the axis connecting both tragi and translated until soft tissue nasion; (2) the sagittal reference plane: the plane perpendicular to the horizontal plane and through the soft tissue nasion; and (3) the coronal reference plane: the plane perpendicular to the other reference planes and passing through the soft tissue nasion. The definition of nasal landmarks was applied based on the method described by Farkas [21]. The two points that represented the nasal alar area were: (1) Alare (Al): the most lateral point of the alar contour and (2) alar curvature (Ac): the point located at the facial insertion of the alar base (Figure 1). The linear distance between the right and left Al (Al-Al; alar width) and Ac (Ac-Ac; alar base width) in T0 and T1 was measured by two investigators, one craniofacial fellow and one senior plastic surgery resident.
2.4. Statistics
Descriptive statistics are given as the mean ± standard deviation (SD) for continuous variables and the frequency distribution for categorical variables. The Pearson χ2 test or Fisher’s exact test were used to compare the groups with respect to categorical variables. A two-sample t-test or the Mann—Whitney U-test was performed to compare two groups with respect to variables. Intraclass correlation coefficients (ICCs) between the raters’ parameters were calculated to establish the interrater reliability. All statistical analyses were performed using SPSS software (version 19; IBM Corp., Armonk, NY, USA). A p-value <0.05 was considered to indicate a statistically significant difference.
3. Results
Of the 57 patients enrolled in this study, 29 were sutured with nylon and 28 received PDS alar cinch sutures. The demographic characteristics in both groups are presented in Table 1 and show no significant differences in age, sex ratio, or maxillary movements. The maxillary advancement/impaction amount in the nylon group was 2.37 ± 1.13/0.52 ± 1.20 mm and in the PDS group was 2.38 ± 1.59/0.16 ± 0.69 mm. There was no difference in the amount of advancement and impaction of the maxilla peri-operatively. Pre-operatively, the nasal width and alar base distance presented no difference between these two groups. Among all 57 patients, 45 (78.9%) had maxillary posterior impaction as clockwise rotation, which was able to soften the lateral profile of class III patients (Figure 2).

Table 1.
Demography of the two suture materials applied for cinch suturing.

Figure 2.
(Upper row) Patient with class III malocclusion received orthognathic surgery using nylon material for cinch suturing. Left, pre-operatively; right, post-operatively. (Lower row) Patient with class III malocclusion received orthognathic surgery using PDS material for cinch suturing. Left, pre-operatively; right, post-operatively.
The mean alar width (Al-Al) change in the nylon group was 1.861 ± 1.66 mm, and in the PDS group, it was 1.115 ± 0.92 mm; the mean alar base distance (Ac-Ac) increase in the nylon group and the PDS group was 1.999 ± 1.40 mm and 1.484 ± 0.97 mm, respectively. The changes in Al-Al and Ac-Ac before and after operation within these two groups were not significant (p > 0.05) in Table 2. The examination of two raters achieved a high correlation in the measurement of Al-Al and Ac-Ac (ICCs: 0.826/0.887).

Table 2.
Inter-group differences in nasal width change.
4. Discussion
The main purpose of this case–control study was to evaluate the effectiveness and stability of different materials in alar cinch sutures to maintain the nasal alar width after Le Fort I osteotomy. An absorbable material (PDS) and a non-absorbable material (nylon) were used in the two groups for the cinch sutures. There was no significant difference in the post-operative nasal widening by the two suture materials. However, the nasal width increase in the PDS group (Al-Al: 1.115 mm; Ac-Ac: 1.484 mm) was lower than that in the nylon group (Al-Al: 1.861 mm; Ac-Ac: 1.999 mm). It seems that the post-operative nasal width was relatively maintained from pre-operation in the PDS group.
Clinically, in previous practice, nylon materials have usually been used for cinch sutures for the maintenance of strength in approximating the nasalis muscle. However, the irritation caused by non-absorbable materials over the subnasale and alar base is often complained about after the surgery. Kolsoum et al. reported that subjects sutured with PDS were less likely to experience chronic incision pain and wound stitches, compared to nylon [22]. Durmaz et al. concluded that absorbable sutures may be preferred in the nasal cavity because of their ease of use, and non-absorbable sutures have the disadvantage of feeling discomfort [23]. This is why an absorbable material (PDS) was used in our study in order to assess its influence on the post-operative nasal width, and because the sutures would fade away afterward without irritating the soft tissue.
Instead of multi-segmented Le Fort I osteotomy, the transfer of single-pieced Le Fort I osteotomy would adequately represent the maxillary movement relating to perioperative nasal change. Nasal alar and base widening after maxillary movement has been consistently found, especially when moving superiorly and anteriorly (impaction/advancement) [24,25,26,27,28]. Horizontally, compared to maxillary setback, maxillary advancement causes significant post-operative nasal alar and base widening [27,28]. In class III malocclusion correction, MMC clockwise rotation is also one of the most effective and popular methods to achieve a better esthetic profile at our center. Among all 57 patients, maxillary posterior impaction was performed in 78.5% (44/56) of them. This clockwise movement of MMC resulted in maxillary advancement and impaction with the alteration of the ANS fixation point in alar cinch sutures, which increases the nasal width. Moreover, Ryckman et al. presented that an increase in alar width is most likely related to the larger amount of advancement [26]. They found that a maxilla movement that has advanced over 4 mm has significant alar widening compared to that of advancement with less than 4 mm. However, in our study, the mean maxillary advancement was 2.37 ± 1.13 mm with a mean vertical change of 0.52 ± 1.20 mm in the nylon group and 2.38 ± 1.59/0.16 ± 0.69 mm in the PDS group. There was no obvious relationship with the amount of advancement in either group.
Classic cinch sutures were originally described by Millard, using 3-0 non-absorbable material passing through fibro-alveolar tissue and the musculature underneath the alar, and approximating in the middle [7]. Controversial results regarding the effectiveness and stability were found in previous studies [11,29,30]. Recently, craniofacial surgeons have started to modify their alar cinch suture techniques. Such modifications include fixation through the nasal septum or anchoring to the dermis or epidermis of the alar area. A systemic review in 2014 compared classic and modified methods of cinch suturing after Le Fort I osteotomy and revealed that the modified technique was more effective for maintaining the nasal width [31].
Chen et al. compared two different kinds of cinch suture methods in Taiwanese skeletal class III malocclusion patients by a randomized trial [12]. The inter-alar and alar base width showed no significant increase when using either the classic method (0.31 ± 1.31 mm) or the modified method, which involved the dermis of the alar base (0.81 ± 1.87 mm). Their study had the same population as our study and was performed in our center. A narrow alar width has become more popular in East Asia in recent years and has become a post-operative concern of OGS patients [27,28].
In this study, stereophotogrammetry was applied for image acquisition owing to its adequacy in soft-tissue imaging and measuring facial soft tissue. The craniofacial community have widely adopted 3D imaging techniques, which have been shown to be accurate when compared to manual anthropometry. Additionally, instead of 2D imaging, 3D imaging can broaden the vision, facilitate communication, and expand the applications [32]. Evaluating the properties of peri-nasal soft tissue clinically and quantitatively is the priority for contemporary optimization of surgical outcomes [33]. Many imaging techniques have been utilized to evaluate facial soft tissue, but 3D stereophotogrammetry remains the most practical modality nowadays [34].
Classic 3-0 non-absorbable sutures are commonly used, and some surgeons prefer polyglactin (Vicryl®, Johnson & Johnson Ltd.: Somerville, N.J., U.S.) and PDS for their medical practice [31,35]. In our study, we chose slow-absorbable monofilament suture made from polyester, i.e., polydioxanone (PDS) as an alternative to nylon in some characteristics, such as slowly releasing the tensile strength and becoming completely absorbed within 180 days [36]. However, some relevant comparisons between nylon and PDS have been published. Sakamoto reported that compared to nylon, absorbable sutures (PDS and VICRYL) are suitable materials for the fixation of cartilage when performing auriculoplasty. When using nylon, in two out of five cases, exposure and deformation were found [37]. In Hennessey et al.’s study of suture strength and fracture, it was found that PDS could tolerate a higher maximum tensile force than nylon, and excessive twisting could lead to a greater decrease in tensile strength in PDS than that in nylon. Namely, compared with nylon, PDS can possess a greater strength but would degrade in tensile force when over-twisted as a result of the risk of suture fracture [38].
The limitations in our study include the strength of the cinch sutures not being identical in all patients. The extent of pre-operative minus ANB angle could be categorized for a more delicate correlated analysis. Moreover, the different sizes of the endotracheal tubes placed via the nostril for general anesthesia depending on patients’ body height would have various effects on nasal morphology. Segmental Le Fort I osteotomy increases the scarring over the nasal wound, which influences the width compared to non-segmental Le Fort I osteotomy. All of these limitations should be corrected and well designed for future studies.
5. Conclusions
The suture materials, PDS and nylon, performed similarly for cinch suturing in orthognathic surgery. No difference of post-operative nasal widening was found between the two suture materials.
Author Contributions
Conceptualization, P.-F.W. and S.-H.K.; methodology, D.C.P.; software, P.-F.W. and S.-H.K.; validation, D.C.P., Y.-A.C., and S.-H.K.; formal analysis, C.-F.Y. and S.-H.C.; writing—original draft preparation, P.-F.W. and C.-H.L.; writing—review and editing, P.-Y.C.; visualization, P.-Y.C.; supervision, P.-Y.C. and Y.-R.C.; review of the submitted version of the manuscript, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Chang Gung Memorial Hospital (IRB No. 202100100B0).
Informed Consent Statement
The patients consented to the use of their photos.
Data Availability Statement
Data available on request due to restrictions eg privacy or ethical. The data presented in this study are available on request from the corresponding author. The data are not publicly available due to consent needed for personal photography.
Acknowledgments
This work was supported in part by a grant from the Craniofacial Research Center, Taoyuan Chang Gung Memorial Hospital (CMRPG3J0823, CMRPG3L0361). The authors wish to thank Ingrid Kuo and the Center for Big Data Analytics and Statistics (Grant CLRPG3D0048) at Chang Gung Memorial Hospital for creating the illustrations used herein.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Steiner, C.C. Cephalometrics in clinical practice. Angle Orthod. 1959, 29, 8–29. [Google Scholar]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Jakobsone, G.; Stenvik, A.; Sandvik, L.; Espeland, L. Three-year follow-up of bimaxillary surgery to correct skeletal Class III malocclusion: Stability and risk factors for relapse. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 80–89. [Google Scholar] [CrossRef]
- Liao, Y.F.; Chen, Y.F.; Yao, C.F.; Chen, Y.A.; Chen, Y.R. Long-term outcomes of bimaxillary surgery for treatment of asymmetric skeletal class III deformity using surgery-first approach. Clin. Oral Investig. 2019, 23, 1685–1693. [Google Scholar] [CrossRef] [PubMed]
- Rosen, H.M. Lip-nasal aesthetics following Le Fort I osteotomy. Plast. Reconstr. Surg. 1988, 81, 171–182. [Google Scholar] [CrossRef]
- Sarver, D.M.; Weissman, S.M. Long-term soft tissue response to LeFort I maxillary superior repositioning. Angle Orthod. 1991, 61, 267–276. [Google Scholar] [CrossRef]
- Millard, D.R., Jr. The alar cinch in the flat, flaring nose. Plast. Reconstr. Surg. 1980, 65, 669–672. [Google Scholar] [CrossRef]
- Rauso, R.; Gherardini, G.; Santillo, V.; Biondi, P.; Santagata, M.; Tartaro, G. Comparison of two techniques of cinch suturing to avoid widening of the base of the nose after Le Fort I osteotomy. Br. J. Oral Maxillofac. Surg. 2010, 48, 356–359. [Google Scholar] [CrossRef]
- Ritto, F.G.; Medeiros, P.J.; de Moraes, M.; Ribeiro, D.P. Comparative analysis of two different alar base sutures after Le Fort I osteotomy: Randomized double-blind controlled trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 111, 181–189. [Google Scholar] [CrossRef]
- Nirvikalpa, N.; Narayanan, V.; Wahab, A.; Ramadorai, A. Comparison between the classical and a modified trans-septal technique of alar cinching for Le Fort I osteotomies: A prospective randomized controlled trial. Int. J. Oral Maxillofac. Surg. 2013, 42, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.; Edler, R.J. Efficacy and stability of the alar base cinch suture. Br. J. Oral Maxillofac. Surg. 2011, 49, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Lin, C.C.; Ko, E.W. Effects of two alar base suture techniques suture techniques on nasolabial changes after bimaxillary orthognathic surgery in Taiwanese patients with class III malocclusions. Int. J. Oral Maxillofac. Surg. 2015, 44, 816–822. [Google Scholar] [CrossRef]
- Raithatha, R.; Naini, F.B.; Patel, S.; Sherriff, M.; Witherow, H. Long-term stability of limiting nasal alar base width changes with a cinch suture following Le Fort I osteotomy with submental intubation. Int. J. Oral Maxillofac. Surg. 2017, 46, 1372–1379. [Google Scholar] [CrossRef]
- Jin, H.R.; Won, T.B. Rhinoplasty in the Asian Patient. Clin. Plast. Surg. 2016, 43, 265–279. [Google Scholar] [CrossRef]
- Vaca, E.E.; Alghoul, M.S. Upper Blepharoplasty with Endoscopically Assisted Brow Lift to Restore Harmonious Upper Lid Arc Curvatures. Plast. Reconstr. Surg. 2020, 146, 565e–568e. [Google Scholar] [CrossRef]
- Sajid, M.S.; Parampalli, U.; Baig, M.K.; McFall, M.R. A systematic review on the effectiveness of slowly-absorbable versus non-absorbable sutures for abdominal fascial closure following laparotomy. Int. J. Surg. 2011, 9, 615–625. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.A.; Ng, L.S.; Ko EW, C.; Chen, Y.R. Mandibular contouring during orthognathic surgery using the modified hunsuck technique. J. Craniofacial Surg. 2017, 28, 239–240. [Google Scholar] [CrossRef]
- Chou, P.Y.; Denadai, R.; Yao, C.F.; Chen, Y.A.; Chang, C.S.; Lin CC, H.; Chen, Y.R. History and evolution of orthognathic surgery at Chang Gung Craniofacial Center: Lessons learned from 35-year experience. Ann. Plast. Surg. 2020, 84, S60–S68. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.Y.; Denadai, R.; Chou, P.Y.; Yao, C.F.; Chen, Y.A.; Wang, P.F.; Chen, Y.R. Impact of the Different Types of Le Fort I Maxillary Surgical Movement on Nasal Width Changes: A Photogrammetric Analysis. Ann. Plast. Surg. 2021, 86, S64–S69. [Google Scholar] [CrossRef] [PubMed]
- Maal, T.J.; van Loon, B.; Plooij, J.M.; Rangel, F.; Ettema, A.M.; Borstlap, W.A.; Berge, S.J. Registration of 3-dimensional facial photographs for clinical use. J. Oral Maxillofac. Surg. 2010, 68, 2391–2401. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.G. Anthropometry of the Head and Neck, 2nd ed.; Raven Press: New York, NY, USA, 1994. [Google Scholar] [CrossRef]
- Kahkhaie, K.R.; Keikhaie, K.R.; Vahed, A.S.; Shirazi, M.; Amjadi, N. Randomized comparison of nylon versus absorbing polyglactin 910 for fascial closure in caesarean section. Iran. Red Crescent Med, J. 2014, 16, e12580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durmaz, A.; Kilic, A.; Gumral, R.; Yildizoglu, U.; Polat, B. The effects of different suture materials in the nasal cavity. J. Laryngol. Otol. 2016, 130, 352–356. [Google Scholar] [CrossRef]
- Betts, N.J.; Vig, K.W.; Vig, P.; Spalding, P.; Fonseca, R.J. Changes in the nasal and labial soft tissues after surgical repositioning of the maxilla. Int. J. Adult Orthodon. Orthognath. Surg. 1993, 8, 7–23. [Google Scholar] [CrossRef]
- Mitchell, C.; Oeltjen, J.; Panthaki, Z.; Thaller, S.R. Nasolabial aesthetics. J. Craniofac. Surg. 2007, 18, 756–765. [Google Scholar] [CrossRef]
- Ryckman, M.S.; Harrison, S.; Oliver, D.; Sander, C.; Boryor, A.A.; Hohmann, A.A.; Kilic, F.; Kim, K.B. Soft-tissue changes after maxillomandibular advancement surgery assessed with cone-beam computed tomography. Am. J. Orthod. Dentofacial. Orthop. 2010, 137, S86–S93. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Lin, Y.Y.; Yao, C.F.; Chen, Y.A.; Huang, C.S.; Chen, Y.R. Type of maxillary segment mobilization affects three-dimensional nasal morphology. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 592–604. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Yao, C.F.; Chen, Y.A.; Lin, Y.Y.; Huang, C.S.; Chen, Y.R. Effect of Le Fort I Maxillary Repositioning on Three-Dimensional Nasal Tip Rotation: A Comparative Study with Implication for the Asian Nose. Plast. Reconstr. Surg. 2021, 147, 903–914. [Google Scholar] [CrossRef]
- Howley, C.; Ali, N.; Lee, R.; Cox, S. Use of the alar base cinch suture in Le Fort I osteotomy: Is it effective? Br. J. Oral Maxillofac. Surg. 2011, 49, 127–130. [Google Scholar] [CrossRef]
- Shoji, T.; Muto, T.; Takahashi, M.; Akizuki, K.; Tsuchida, Y. The stability of an alar cinch suture after Le Fort I and mandibular osteotomies in Japanese patients with Class III malocclusions. Br. J. Oral Maxillofac. Surg. 2012, 50, 361–364. [Google Scholar] [CrossRef]
- Liu, X.; Zhu, S.; Hu, J. Modified versus classic alar base sutures after LeFort I osteotomy: A systematic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Dindaroğlu, F.; Kutlu, P.; Duran, G.S.; Görgülü, S.; Aslan, E. Accuracy and reliability of 3D stereophotogrammetry: A comparison to direct anthropometry and 2D photogrammetry. Angle Orthod. 2016, 86, 487–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denadai, R.; Chou, P.Y.; Seo, H.J.; Lonic, D.; Lin, H.H.; Pai, B.C.; Lo, L.J. Patient-and 3D morphometry-based nose outcomes after skeletofacial reconstruction. Sci. Rep. 2020, 10, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Chou, P.Y.; Hallac, R.R.; Ajiwe, T.; Xie, X.J.; Liao, Y.F.; Kane, A.A.; Park, Y.J. The role of Nasoalveolar molding: A 3D Prospective analysis. Sci. Rep. 2017, 7, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Adams, B.; Levy, R.; Rademaker, A.E.; Goldberg, L.H.; Alam, M. Frequency of use of suturing and repair techniques preferred by dermatologic surgeons. Dermatol. Surg. 2006, 32, 682–689. [Google Scholar] [CrossRef]
- Gupta, D.; Sharma, U.; Chauhan, S.; Sahu, S.A. Improved outcomes of scar revision with the use of polydioxanone suture in comparison to polyglactin 910: A randomized controlled trial. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 1159–1163. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, A.; Kiyokawa, K.; Rikimaru, H.; Watanabe, K.; Nishi, Y. An investigation of the fixation materials for cartilage frames in microtia. J. Plast. Reconstr. Aesthetic Surg. 2012, 65, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Hennessey, D.B.; Carey, E.; Simms, C.K.; Hanly, A.; Winter, D.C. Torsion of monofilament and polyfilament sutures under tension decreases suture strength and increases risk of suture fracture. J. Mech. Behav. Biomed. Mater. 2012, 12, 168–173. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).