Abstract
Morphea is a rare sclerotic autoimmune disorder primary affecting the skin and subcutaneous tissues. The linear head variants involve the facial area, with asymmetries and deformities. Eighteen patients with hemifacial deformity (age range 14–75 years) were assessed before surgery (T0), and after one (T1, 18 patients) or two (T2, six patients) surgical treatments of facial autologous fat grafting. A stereophotogrammetric reconstruction of the facial surface was obtained for each patient and a group of control subjects, and facial symmetry was quantified according to the root mean square distance between homologous areas of trigeminal innervation. Values obtained from the control subjects were used to calculate z-scores for patients. At T0, all facial thirds of the patients resulted significantly more asymmetrical than those of the control subjects (Mann–Whitney test, p < 0.05), while at T1, the symmetry of the middle facial third did not differ from that of control subjects (p = 0.263). At T2, the upper and the lower facial thirds also did not differ from the control values (p > 0.05). The faster result obtained in the facial middle third was in accord with clinical findings. In conclusion, autologous fat grafting significantly improved facial asymmetry after one (middle facial third) or two (lower and upper thirds) treatments; the outcomes were efficaciously quantified by stereophotogrammetry.
1. Introduction
Morphea is a rare, clinically heterogeneous, sclerotic autoimmune disorder characterized by increased and excessive collagen deposition, whose pathogenesis, although not fully understood, is likely multifactorial. It is also recognized as localized scleroderma and includes disorders characterized by sclerosis primary affecting the skin, but it can also involve adjacent subcutaneous tissues in either a limited or extensive fashion. It begins with an initial inflammatory phase followed by subsequent sclerotic and/or atrophic phases: damage to vessels, profibrotic cytokine release, and the unbalance of collagen production and destruction represent all the culminating disease effects [1].
In literature, the actual morphea classification systems are based on clinical phenotypes and the first attempt to classify this pathological condition dates back to 1995. Peterson et al. [2] described a system including five different sub-classifications of morphea: plaque, generalized, bullous, linear and deep. Later on, other classification systems were proposed and more widely adopted in clinical settings.
Currently, one of the systems mostly accepted and used in clinics is that proposed by Laxer et al. [3] who defined five different subtypes of morphea: circumscribed (including superficial and deep variants), linear (comprising trunk/limb and head variants), generalized, pansclerotic, and mixed. Among all the subtypes, linear morphea (also called linear scleroderma) involving the head and neck can be responsible for provoking the worst social and psychological issues in the patient’s life [4]. In fact, apart from a variety of manifestations caused by morphea, such as neurological complications [4], this pathological condition is generally not a fatal disease, although causing severe deformity in the most serious cases. Indeed, for patients suffering by linear head variant sub-types of morphea, the changes in skin appearance, asymmetry, and deformities can seriously involve the craniofacial area, affecting the quality of life.
In this scenario, En Coupe de Sabre scleroderma syndrome (ECDS) and Parry–Romberg syndrome (PRS) are two different conditions classified as particular forms of the linear morphea subtypes progressive hemifacial atrophy [5,6], with an estimated prevalence of at least 1/700,000 individuals, women being slightly more affected than men.
ECDS is characterized by a linear lesion (a “sword stroke-like lesion”) [2] generally occurring in the fronto-parietal scalp or in the paramedian frontal region and sometimes also extending down the face [7]. Differently, PRS is characterized by the atrophy of the subcutaneous tissues (fat, connective tissue, muscles and sometimes also bone tissue) with minimal sclerotic manifestations of the overlying skin tissue of one side of the face. It is also known as “progressive hemifacial atrophy” and, in contrast with ECDS, presents little-to-no sclerosis of the cutaneous and subcutaneous tissue [7,8,9,10] in addition to an involvement of the deeper head and neck structures [11,12]. However, according to many authors, the clinical presentation of PRS can sometimes be very similar to ECDS, often even co-existing, making these two entities difficult to distinguish and supporting the fact that they are both subtypes of the same common underlying pathogenesis related to linear scleroderma [7,12,13,14,15,16,17].
However, regardless of the specificity of the lesions, all the head variants of the localized scleroderma determine some common facial defects which include disfiguring and loss of symmetry. Consequently, a severe psycho-social impact can affect the patients for whom only a surgical intervention can represent a valid attempt to correct the facial asymmetry once the disorder has stabilized.
Many are the surgical options that can offer benefits to patients with facial lesions caused by linear morphea syndrome: the main object for all reconstructive surgery procedures is the volume augmentation and/or the facial symmetry retrieval. Among the diverse surgical treatments that can be proposed, grafting of autologous fat for filling the facial defects has been revealed to be a promising procedure, enabling professionals to reach satisfactory outcomes in PRS patients [10,18,19]. However, regardless of the type of surgical treatment performed on patients, to date there is still not a commonly univocal way to assess the effectiveness of the adopted surgical treatments and their outcomes in treated patients.
Indeed, the evaluation of the treatment success often relays in the physician’s clinical judgment and patient satisfaction, both based on qualitative and subjective assessments rather than on quantitative and objective measurements [9]. However, in order to correctly assess whether surgical treatments can reach optimal results in terms of symmetry recovery, and to consider the treatment as an adequate and advantageous therapeutic alternative, it is indispensable to evaluate the surgical outcomes through objective analyses providing quantitative evidence. In these terms, three-dimensional (3D) stereophotogrammetry represents an ideal method for facial soft tissue evaluations since it offers precise, quantified assessments [20,21,22]. In addition, being radiation-free, it can be used longitudinally without any adverse effect, as already done for other diseases [23]. All these characteristics make this technique very suitable for conducting quantitative evaluations on outcomes deriving from the lipofilling treatment on linear morphea patients.
The first step for standardizing the possible use of stereophotogrammetry for treatment planning and the evaluation of surgery outcomes in patients with linear morphea-associated facial lesions is the quantitative and objective analysis of facial asymmetry as compared to that found in the normal population (healthy subjects). In fact, to the authors’ knowledge, no studies have longitudinally quantified the symmetry of facial surfaces in patients with linear morphea by using stereophotogrammetry: most researchers primarily focused on 3D analyses of facial volume retention after specific surgical treatments and generically on the subjective assessment of aesthetics/facial symmetry improvements by a mean of physicians and patient satisfaction questionnaires [10,24]. Only few studies exist: stereophotogrammetry was used by Pucciarelli et al. to quantify the restoration of facial symmetry in a single patient [25] and by Jaing et al. to monitor fat graft retention and reliably assess the volume change of soft tissues after the surgical treatment [26]. Another few studies used CT scans to assess the restoration of facial volume following maxillo-facial surgical treatments [27,28]. However, stereophotogrammetry, being a fast and radiation-free technique, might represent the elective methodology to investigate the asymmetry of facial soft tissues and the surgery outcomes to restore facial symmetry in patients suffering of mild and moderate linear morphea where no skeletal tissues are involved.
In this perspective, our study has two aims: the first one is to investigate the possible use of a 3D stereophotogrammetry-based protocol for potentially quantifying and demonstrating facial asymmetry in patients with head-variants linear morphea before any maxillo-facial surgical treatment. The second aim focuses on the quantitative evaluation of the effectiveness of lipofilling as a surgical treatment for restoring facial symmetry on the same patients by considering different facial thirds (upper, middle and lower according to the areas of trigeminal nerve innervation) and number of performed surgical treatments (one or two).
2. Materials and Methods
2.1. Patients
Patients diagnosed with the head-variant of linear morphea (Parry–Romberg syndrome, En Coupe de Sabre syndrome, and/or linear scleroderma generically involving head) attending the multidisciplinary Maxillo-Facial and Odontostomatologic Surgery Unit of Fondazione IRCCS Ca’ Granda Ospedale Policlinico Maggiore at the University of Milan (Milano, Italy) and with complete records and long-term follow-up (>2 years) were included in this longitudinal study. All recruited patients presented unilateral involvement and/or hemifacial deformity ranging from “mild” to “moderate”, limited to soft tissues. A total of 18 patients of both sexes and aged 14 to 75 years of age were selected and followed up before surgery, after the first surgical treatment and, for one third of patients, also after the second surgical one. Clinical and demographic data of all patients are summarized in Table 1.

Table 1.
Demographic and clinical data of patients (type of syndrome, affected side and involved facial thirds) and number of treatments analyzed in the present study.
All patients were treated between 2015 and 2020 with a surgical operation, based on autologous fat tissue grafting (AFTG), the so-called lipofilling treatment. A stereophotogrammetric evaluation of facial symmetry was performed on patients before the surgical treatment and compared with data collected in a control group of 60 healthy subjects matched for sex, age and ethnicity. Accordingly, four control groups, each composed by 15 subjects, were used: female and male adolescents (aged between 14 and 18 years old), and female and male adults (with an age ranging from 30 and 75 years old). Control subjects were selected from the laboratory database; exclusion criteria were facial deformity, recent or previous surgery or traumatic injury affecting the face, and neurological impairments.
All patients, and the parents/ legal guardians of those aged less than 18 years, received a detailed explanation of the surgical procedure, and signed an informed consent agreement, in accordance with the guidelines of the Declaration of Helsinki. The experimental procedure for facial 3D analysis was approved by the local university ethical committee (26.03.14; no 92/14), and explained to all control subjects, patients and parents/ legal guardians of the subjects aged less than 18 years of age before any acquisition. They all signed the relevant informed consent agreement.
Patients underwent one surgical treatment at least; one third of them also received a second grafting, which was made at least one year after the first surgery. Three-dimensional acquisitions of patient faces were performed some days before surgery, 6–9 months after the first surgical treatment, and one year after the second one.
2.2. Surgical Procedures
In our surgical protocol, we used Coleman technique, currently dominating the practice [29]. The donor sites can be detected in the trochanteric area, the periumbilical abdominal region or the inner thighs region, since they have a sufficient amount of adipose tissue with a comfortable access. The first step consists in anesthetizing the area to be harvested with a tumescent technique by infiltrating 150 mL of local modified Klein solution (containing 100 mL of saline, 20 mL of mepivacaine 2%, 20 mL of ropivacaine 7.5 mg/mL, 1 mL of epinephrine, and 5 mL of sodium bicarbonate solution 1 mEq/mL) in the subcutaneous tissue.
Adipose tissue is suctioned through the same incision after local infiltration of anesthetic solution. The cannula (Coleman Kit 15 cm × 12 ga; Mentor™, Johnson & Johnson Company, New Brunswick, NJ, USA) used for fat harvesting is connected with a luer-lock syringe (Terumo-B.D. Troge, Nike S.r.l., Milan, Italy). The syringe plunger is pulled at the top; this creates a slight negative pressure inside the syringe, which allows the collection of adipose tissue. The area is managed with an elastic–compressive dressing, which is kept in place for 5 days to prevent hematoma formation.
The adipose tissue is centrifuged (Hettich EBA 20, Seneco Science, Milan, Italy) at 700× g for 3 min in sterile conditions. Exposure of the lipoaspirate to the environment should be avoided. Graft survival is improved by reducing the time between aspiration and injection. Only the intermediate layer containing adipocytes and stromal vascular component is used for AFTG and then injected using a blunt cannula (Coleman Style II, 9 cm × 17 ga; Mentor™, Johnson & Johnson Company, New Brunswick, NJ, USA) through a small incision, in a retrograde fashion at the dermal–epidermal junction level. In order to avoid coalescence, fat necrosis, resorption and oily cysts, microribbons of adipose tissue are preferred to boli.
The areas to be treated are identified before surgery, after an accurate analysis of the patient’s face and of his/her 3D-images. The amount of fat grafted is decided intraoperatively in order to symmetrize the interested area with the contralateral and to contrast the fat grafting reabsorption, which is the main pitfall of this surgical technique.
All patients underwent surgery in general anesthesia. Before surgery, antibiotic prophylaxis is performed with Cefazoline 2 g iv. Postsurgery prescriptions involve pain killer therapy (Paracetamol) and ice over the harvested area for 48–72 h after surgery.
2.3. Image Acquisition
The entire study was performed on 3D facial digital models acquired by VECTRA System (VECTRA M3; Canfield Scientific, Inc., Fairfield, NJ, USA), a stereophotogrammetric device that provides a fast, safe, and not invasive procedure. The system uses three pairs of coordinated, high-definition digital cameras configured in a Cartesian reference system; all the cameras simultaneously shot the analyzed subject from different perspectives and accurately calculate its 3D position in the space [20,21,22,30]. The data collection protocol was non-invasive, and free from pain, disturbance or risk to the subject, and involved minimal discomfort to the patient.
Regardless of whether performed on patients or control subjects, before the acquisition of the 3D model, an experienced and qualified operator detected, by a prior palpation and inspection, a set of anthropometric landmarks on the facial surface according to the protocol used in the laboratory [22,30,31]. Marking these points of interest with a biocompatible and washable black eyeliner before the acquisition increases the precision of the facial measurements and the selection of the 3D facial areas to be superimposed without affecting the quality of the image. Where needed, the subject’s hair was tied with a disposable elastic band in order to allow the upper facial third to be as properly acquired as any other facial parts. All subjects were requested to seat in front of the device during the image acquisition, in a relaxed posture and with a natural expression exhibiting open eyes, closed mouth and teeth in slight contact [31,32].
2.4. Image Analysis
For each patient, a stereophotogrammetric reconstruction of the entire facial surface was obtained for each experimental evaluation: before surgery (at T0) and after 6–9 months from the first surgical treatment (T1). For six patients who underwent also the second surgery, an additional stereophotogrammetric reconstruction obtained 12 months after the treatment (at T2) was available for the analysis. All 3D digital facial models obtained from patients and healthy subjects were further elaborated using VAM software (VECTRA Analysis Module; Canfield Scientific, Inc., Fairfield, NJ, USA). For each 3D model, facial areas of interest (FAIs) were semi-automatically selected according to a previously published protocol [22,31,32]. At first, the facial surface was encompassed by several landmarks: trichion (tr); nasale (n), pronasale (prn), columella (c), stomion (sto), sublabiale (sl), gnathion (gn) placed in the midline, and frontotemporalis (ft); zygion (zy); tragion (t); gonion (go) located bilaterally. Subsequently, each face was automatically split into two halves. according to the maximum symmetry plane; each FAI (left and right) was further divided into 3 facial thirds according to the areas of trigeminal nerve innervation: upper (trichion, nasion, pronasale, columella, alare (al), endocanthion (en), exocanthion (ex), frontotemporalis), middle (endocanthion, alare, columella, stomion, cheilion (ch), zygion, frontotemporalis, exocanthion) and lower (stomion, sublabiale, gnathion, gonion, tragion, zygion, cheilion). Figure 1 shows the positions of the three facial thirds.
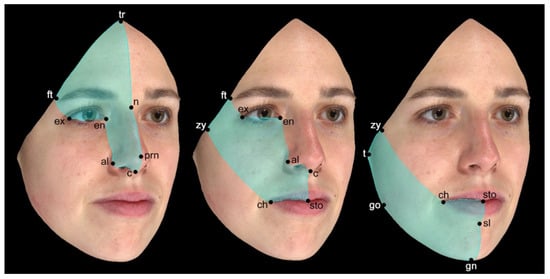
Figure 1.
Three-dimensional digital model of the face divided into its three thirds. The landmarks used to identify the thirds are listed in the text.
The left side (conventionally chosen) of each subject’s face and facial third was then automatically flipped according to the maximum symmetry plane in order to obtain a “mirror” image for the superimposition on the contralateral FAI. After the registration of the two FAIs (the original and the flipped ones), the software automatically superimposed them together and calculated the root mean square (RMS, unit: mm) point-to-point distance of the selected surfaces. This value was used to quantify the symmetry of each facial third in each subject: healthy subjects of control group and patients at T0 (considered as baseline). For the patient group, this procedure was also repeated for every follow-up time points (at T1 and T2) in order to calculate the symmetry changes due to the treatment. The higher the value, the higher the asymmetry [32,33]. The procedure was found to be highly reproducible both in the literature [33], and in our laboratory: Bland–Altman repeatability coefficients ranging from 0.9% to 1.7%, and relevant mean biases of area measurements included between −0.003 and 0.097 cm were found [31,32].
Finally, the software also produced colorimetric maps, which highlight the variations in an intuitive way.
2.5. Statistical Analysis
At T0, the 18 patients were divided into the same four age and sex classes obtained for control subjects: female adolescents (N = 4), male adolescents (N = 4), female adults (N = 7) and male adults (N = 3). For each class, descriptive statistics (mean, SD) of the RMS values obtained from the superimposition of the total face (left hemi-face flipped on the right hemi-face) and of the three thirds (the left facial third—upper, middle and lower—flipped on the respective right third—upper, middle and lower) were obtained separately for patients and control subjects. For each facial third, RMS values obtained from the relevant control groups were used to calculate a set of z-scores for patients at every experimental time point (T0, T1, T2). Z-score values were calculated as follow:
RMS patient − RMS mean controls/SD controls
Mann–Whitney test was used to compare the z-scores of the three facial thirds of patients, before and after surgery, with those of control subjects (z-scores = 0 for definition) in order to evaluate the efficacy of the treatment on the facial symmetry restoration in terms of possible changes/improvements from the initial situation (baseline at T0). Additionally, the effect size of the differences was estimated by r, calculated and interpreted according to [34], as small (r values lower than 0.30), medium (between 0.30 and 0.50) and large (larger than 0.5). The significance level was established at p < 0.05 and the statistical analyses were performed using IBM SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, USA).
3. Results
Among the 18 patients (11 females and 7 males) with a head-variant linear morphea condition, seven patients were diagnosed with ECDS, seven with PRS and four generically with linear scleroderma, involving the face, unilaterally. All patients presented unilateral involvements: upper third unilateral lesions were diagnosed in 14 patients, middle third lesions in 13 patients while the lower third resulted the less involved and only nine patients were diagnosed with skin scleroderma lesions, relating to this facial third. In six patients the lesions extended in two facial thirds, while in the other six, all facial thirds were involved. At T0, patient ages ranged from 14 to 75 years old with an average age of 33 years old (Table 1).
On average, in all the four control groups RMS mean values ranged between 0.62 and 0.88 mm and most resulted <0.78 mm with standard deviations ranging between 0.12 and 0.35 mm (Table 2).

Table 2.
RMS mean values and relevant standard deviations of total face and facial thirds (upper, middle and lower) of each class of control subjects. All values are mm.
On the contrary, when considering the RMS values of symmetry of the total face and facial thirds computed on patients at baseline (T0), values larger than those obtained in the control groups were observed. On average, patient RMS values at T0 were always larger than 0.80 mm (ranging from 0.82 to 1.59 mm). In particular, 12 out of 18 mean RMS values always resulted >1.00 mm with standard deviations ranging from 0.12 to 1.28 mm. Mean RMS values of all facial thirds of all patient groups at T1 were similar to or even larger than those observed at T0 and never inferior to 0.80 mm.
Reduced RMS values were instead found at T2, especially in the adult female patient group in which all the mean RMS values fall into the relevant mean plus 1 SD intervals of the control group (up to 0.88 mm). Only one female adolescent patient was analyzed at T2; her upper and middle third displayed a reduction in RMS point-to-point distance with values < 0.80 mm, similar to those of her class-related control group. A reduction in the RMS distance of the lower third between T0 (and T1) and T2 was observed also in male adolescent patients. RMS mean values and relevant SD at the diverse time points for each patient group are reported in Table 3, while Figure 2 shows the colorimetric maps of Patient 2, who was affected by a Parry–Romberg syndrome, involving in particular her left middle and lower facial thirds.

Table 3.
RMS mean values and relevant standard deviations of total face and facial thirds (upper, middle and lower) of patients before (T0) and after the surgical treatment (T1 and T2). All values are mm.
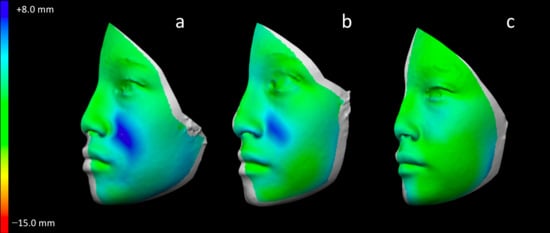
Figure 2.
Colorimetric maps showing facial asymmetry of Patient 2 before treatment (T0), (a), 6 months after the first treatment (T1), (b) and 12 months after the second treatment (T2), (c). Asymmetric areas are colored in blue (left side superimposed on the right side), while symmetrical areas are in green.
Z-score values of all facial thirds of each patient at every time point are presented in Table 4. Overall, individual values ranged from −1.62 to 9.8. At T0, 70% of the Z-scores of all facial thirds involved by sclerotic lesions (a total of 25 out of 36 facial thirds) showed values deviating more than 1 SD from the control values. Positive changes to the Z-scores, in terms of value reduction, at T1 and T2 were especially observed for the middle third, followed by the upper third; improvements for the lower third were only observable at T2.

Table 4.
Z-score values of the symmetry of facial thirds (upper, middle and lower) of all patients at T0 (baseline, before surgery), at T1 (6–8 months after the first treatment) and T2 (1 year after the second treatment). Values relative to facial thirds involved by scleroderma according to the clinical diagnosis are in bold italic type.
Finally, Mann–Whitney test allowed the comparison of the symmetry of the three facial third between the control group and the patients sample: at baseline (T0) all facial thirds of the patients resulted significantly more asymmetrical than those of the control subjects, while after the first surgery (also maintained after the second surgical treatment) the symmetry of the middle facial third did not differ from that of control subjects. At T0, the effect size of the differences was either medium or large (lower third of the face). At T1, the effect sizes of the three facial thirds were, respectively, medium, small and large. At T2, both the upper and the lower facial thirds presented p values > 0.05 indicating that once the second surgical treatment was performed, no significant differences in the symmetry of these thirds was detected in comparison with that found on healthy individuals. Effect sizes were large (upper third) and small (middle and lower third). Descriptive statistics of the Z-scores values, and results (p value and effect size) from Mann–Whitney Test are summarized in Table 5.

Table 5.
Z-score mean values and relevant standard deviations of the total face and facial thirds (upper, middle and lower) of all patients before surgery (baseline, T0) and at different follow-up time points (T1 and T2). p values refer to Mann–Whitney test (patients values compared to healthy control subjects).
4. Discussion
In our study, we aimed to test the application of a 3D optical instrument to the detection and longitudinal quantification of facial asymmetry in patients affected by head variants of linear morphea and treated with autologous fat grafting. The treatment was intended to improve their facial symmetry and, consequently, their quality of life, in terms of social and personal acceptance. Lipofilling allows patients to reach a good esthetic result, with a minimally invasive approach [29,35], and a 3D quantitative assessment can actually measure the effectiveness of this surgical treatment in reducing facial asymmetry [36].
Indeed, restoring facial symmetry is the main challenge of surgery in patients affected by morphea of the cervico-facial district. Many different surgical procedures can be performed in order to obtain the fixed endpoint and they can be listed from osteotomies to free flaps to autologous fat grafting, involving both bones and soft tissues. Recently, Anderson et al. proposed an algorithm to restore facial contour symmetry in pediatric populations, but it can be used also for adult patients: when the disease is limited to the soft tissues, AFTG is the treatment of choice due to its biocompatibility, efficiency, low cost and limited side effects [36]. Among the complications, scarring and contractions of the donor site have been reported [36]. Indeed, the trochanteric area, the periumbilical abdominal region, the gluteal area and the inner thighs region, can all be used because they offer an adequate quantity of adipose tissue that can be easily harvested. There is not a consensus about which area is more suitable for better outcomes in lipofilling: Balaji supports the hypothesis that donor gluteal fat is better than abdominal fat [37]. On the contrary, Lim et al. found no differences in results comparing the different donor regions [38].
Before treatment, our patients had faces that, on average, were about three SDs more asymmetrical than those of the control group subjects, with individual z-scores up to 9.8 SDs. The quantification and localization of the areas of major asymmetry was performed semiautomatically on the digital models of the patients’ faces obtained by stereophotogrammetry, and used to plan the surgical treatment. The longitudinal, post-surgical analysis allowed to quantify the modifications in facial asymmetry separately for the three facial thirds, supporting the clinical decisions without submitting the patients to potentially harmful or painful procedures [32]. Additionally, the colorimetric presentation of facial asymmetry can be usefully shared with the patients helping to better explain the baseline situation and its longitudinal modifications [31].
Indeed, photogrammetry methods were originally developed within engineering and physical sciences, and they are widely employed by production engineering for a variety of industrial applications, ranging for instance from car manufacturing and ship building to health industries. Among the others, photogrammetry is used to generate 3D models of objects, for measurements of both large and small scale manufacts, for surface characterization of parts and quality assurance of objects obtained by manufacturing processes [39,40]. More recently, they were implemented for medical imaging applications with suitable hardware and software solutions [41]. These instruments are becoming more and more diffuse for patient diagnosis, treatment planning and follow-up, especially where surface information plays a key role [20,21,22,23,25,30,31,32,33]. Additionally, surface information can be fused with volumetric information obtained by ultrasonography, computerized tomography or magnetic resonance imaging [41], and both can be used for fabrication and performance verification of medical devices and prostheses [40], thus going back to one of the original applications of the method.
As seen in our results, we can affirm that the middle third of the face, if compared with the superior and the inferior ones, showed an improvement of the symmetry already after the first treatment, which, moreover, was maintained and enhanced with the second one. This can be explained because variable results can be seen in different facial regions [19]. First of all, we can assume that a similia similibus reconstruction is more appropriate and it leads to better results, since the middle third of the face is mainly composed by soft tissue. Furtherly, adipose tissue preservation and post-operative outcomes are more promising in the malar and cheek areas because mobile zones are less likely to retain the graft [38]; also, the perioral and temporal areas are known to have less favorable results [38,42].
Indeed, the inferior and the superior facial thirds did not show a statistically significant improvement of the symmetry after the first treatment, that was documented after the following ones. This conduct can be explained by the larger mobility of these regions, as previously illustrated, and by the altered growth of the maxillo-facial complex of the studied patients leading to a reduced maintenance of the fat grafted and the subsequent need to repeat the lipofilling process. Frequently, a standalone lipofilling session does not offer a satisfying result; numerous procedures seem to mainly fulfill the final outcome [42]. Fortunately, AFTG is a safe, repeatable and mini-invasive method to restore facial symmetry; additionally, the maxillofacial areas is well vascularized and it can sustain multiple lipofilling procedures [43], tailoring the therapy for each patient and each facial area [36]. Evidently, the more serious the clinical condition is, the more adipose tissue is needed to restore the facial contour, with a higher number of surgical appointments and a progressive filling of the area. Some authors proposed 3 months as an ideal period between subsequent surgeries in patients affected by PRS [44], nevertheless there is not a conclusive agreement about the best interval between lipofilling procedures [45]. The current timing was selected also considering our previous clinical experience [25]. From our experience, we can affirm that lipofilling is a valid and reliable surgical technique to restore facial symmetry and, additionally, that 3D stereophotogrammetry allows for an extremely reliable and precise analysis of symmetry pre- and post-operatively. The instrument is safe, requires a minimal collaboration from the patient, and can provide a quantitative assessment of total and localized facial asymmetry in a reduced time [32]. It has already been used to quantitatively assess longitudinal modifications during surgical and reconstructive treatments in the facial area [23,25,31].
At last, we have to underline the limitations of this article. First of all, our patient population is quite heterogeneous, but, since facial morphea is a rare disease, we have tried to make it uniform by dividing the face into thirds. Moreover, only one third of the patients underwent the second surgery; some of them ended their treatment achieving a final adequate facial symmetry, other ones were lost to follow up (the COVID-19 pandemic being one of the reasons), and some are still waiting for the appropriate timing of their second lipofilling. Therefore, the results showed at T2 should be taken with caution, and a larger patient group is needed to better understand the more appropriate treatment options.
Indeed, together with the assessment of statistical significance, we also calculated the effect size that can inform about the practical/clinical meaning of the differences. At baseline, together with the statistically significant facial asymmetries, we observed medium or large effect sizes: the differences were clinically relevant. After the first treatment, the middle third of the face regained its symmetry but with a small effect size; the same was observed at T2. In contrast, the differences measured in the upper facial third had a large effect size. Therefore, also considering the reduced number of patients analyzed at T2, we underline that the results of the statistical tests should be considered with caution. In conclusion, we can affirm that the efficacy of lipofilling in terms of symmetry improvement is noticeable after the first treatment in the middle facial third, while two procedures seem to be needed to measure an enhancement in the lower and upper third. Furthermore, 3D stereophotogrammetry is confirmed to be a valid method to analyze symmetry modifications.
Author Contributions
Conceptualization, A.B.G. and C.S.; methodology, C.B., A.C., D.M.G., R.S., C.D., F.C.; formal analysis, C.B., A.C., D.M.G., C.D.; investigation, C.B., A.C., D.M.G., R.S., C.D., F.C.; A.B.G., C.S.; resources, A.B.G. and C.S.; data curation, C.B., A.C., D.M.G., C.D.; writing—original draft preparation, A.C., C.B. and C.S.; writing—review and editing, D.M.G., C.D., A.B.G.; supervision, A.B.G. and C.S.; project administration, A.B.G. and C.S.; funding acquisition, A.B.G. and C.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fett, N.; Werth, V.P. Update on morphea. J. Am. Acad. Dermatol. 2011, 64, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Peterson, L.S.; Nelson, A.M.; Su, W.P.; Mason, T.; O’Fallon, W.M.; Gabriel, S.E. The epidemiology of morphea (localized scleroderma) in Olmsted County 1960–1993. J. Rheumatol. 1997, 24, 73–80. [Google Scholar] [PubMed]
- Laxer, R.M.; Zulian, F. Localized scleroderma. Curr. Opin. Rheumatol. 2006, 18, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Tolkachjov, S.N.; Patel, N.G.; Tollefson, M. Progressive hemifacial atrophy: A review. Orphanet J. Rare Dis. 2015, 10, 1–13. [Google Scholar] [CrossRef]
- ORPHA. Available online: https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=EN&data_id=1460&Disease_Disease_Search_diseaseGroup=1214&Disease_Disease_Search_diseaseType=ORPHA&Disease(s)/group%20of%20diseases=Progressive-hemifacial-atrophy&title=Progressive%20hemifacial%20atrophy&search=Disease_Search_Simple (accessed on 15 November 2020).
- OMIM. Available online: https://www.omim.org/entry/141300 (accessed on 15 November 2020).
- Tollefson, M.; Witman, P.M. En coup de sabre morphea and Parry-Romberg syndrome: A retrospective review of 54 patients. J. Am. Acad. Dermatol. 2007, 56, 257–263. [Google Scholar] [CrossRef]
- Stone, J. Parry-Romberg syndrome: A global survey of 205 patients using the Internet. Neurology 2003, 61, 674–676. [Google Scholar] [CrossRef]
- Palmero, M.L.H.; Uziel, Y.; Laxer, R.M.; Forrest, C.R.; Pope, E. En Coup de Sabre Scleroderma and Parry-Romberg Syndrome in Adolescents: Surgical Options and Patient-related Outcomes. J. Rheumatol. 2010, 37, 2174–2179. [Google Scholar] [CrossRef]
- Rodby, K.A.; Kaptein, Y.E.; Roring, J.; Jacobs, R.J.; Kang, V.; Quinn, K.P.; Antony, A.K. Evaluating Autologous Lipofilling for Parry-Romberg Syndrome–Associated Defects: A Systematic Literature Review and Case Report. Cleft Palate Craniofacial J. 2016, 53, 339–350. [Google Scholar] [CrossRef]
- Khan, M.; Khan, M.; Negi, R.; Gupta, N. Parry Romberg syndrome with localized scleroderma: A case report. J. Clin. Exp. Dent. 2014, 6, e313–e316. [Google Scholar] [CrossRef]
- Wong, M.; Phillips, C.; Hagiwara, M.; Shatzkes, D.R. Parry Romberg Syndrome: 7 Cases and Literature Review. Am. J. Neuroradiol. 2015, 36, 1355–1361. [Google Scholar] [CrossRef]
- El-Kehdy, J.; Abbas, O.; Rubeiz, N. A review of Parry-Romberg syndrome. J. Am. Acad. Dermatol. 2012, 67, 769–784. [Google Scholar] [CrossRef] [PubMed]
- Paprocka, J.; Jamroz, E.; Adamek, D.; Marszal, E.; Mandera, M. Difficulties in differentiation of Parry–Romberg syndrome, unilateral facial sclerodermia, and Rasmussen syndrome. Childs Nerv. Syst. 2006, 22, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.E.; Vora, S.S.; Kwon, E.-K.M.; Maheshwari, M. A Significant Proportion of Children with Morphea En Coup De Sabre and Parry-Romberg Syndrome Have Neuroimaging Findings. Pediatr. Dermatol. 2012, 29, 738–748. [Google Scholar] [CrossRef] [PubMed]
- Lehman, T.J. The Parry Romberg syndrome of progressive facial hemiatrophy and linear scleroderma en coup de sabre. Mistaken diagnosis or overlapping conditions? J. Rheumatol. 1992, 19, 844–845. [Google Scholar]
- Kister, I.; Inglese, M.; Laxer, R.M.; Herbert, J. Neurologic manifestations of localized scleroderma: A case report and literature review. Neurology 2008, 71, 1538–1545. [Google Scholar] [CrossRef]
- Glaser, D.H.; Schutt, C.; Schollaert-Fitch, K.; Torok, K. Linear Scleroderma of the Head—Updates in management of Parry Romberg Syndrome and En coup de sabre: A rapid scoping review across subspecialties. Eur. J. Rheumatol. 2020, 7, S48–S57. [Google Scholar] [CrossRef]
- Wan, D.C.; Lim, A.T.; Longaker, M.T. Craniofacial Autologous Fat Transfer. J. Craniofacial Surg. 2009, 20, 273–274. [Google Scholar] [CrossRef]
- Gibelli, D.; Pucciarelli, V.; Cappella, A.; Dolci, C.; Sforza, C. Are Portable Stereophotogrammetric Devices Reliable in Facial Imaging? A Validation Study of VECTRA H1 Device. J. Oral Maxillofac. Surg. 2018, 76, 1772–1784. [Google Scholar] [CrossRef]
- Gibelli, D.; Dolci, C.; Cappella, A.; Sforza, C. Reliability of optical devices for three-dimensional facial anatomy description: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2020, 49, 1092–1106. [Google Scholar] [CrossRef]
- Gibelli, D.; Tarabbia, F.; Restelli, S.; Allevi, F.; Dolci, C.; Orabona, G.D.; Cappella, A.; Codari, M.; Sforza, C.; Biglioli, F. Three-dimensional assessment of restored smiling mobility after reanimation of unilateral facial palsy by triple innervation technique. Int. J. Oral Maxillofac. Surg. 2020, 49, 536–542. [Google Scholar] [CrossRef]
- Tse, R.W.; Mercan, E.; Fisher, D.M.; Hopper, R.A.; Birgfeld, C.B.; Gruss, J.S. Unilateral Cleft Lip Nasal Deformity. Plast. Reconstr. Surg. 2019, 144, 1138–1149. [Google Scholar] [CrossRef] [PubMed]
- Slack, G.C.; Tabit, C.J.; Allam, K.A.; Kawamoto, H.K.; Bradley, J.P. Parry-Romberg Reconstruction. J. Craniofacial Surg. 2012, 23, S27–S31. [Google Scholar] [CrossRef] [PubMed]
- Pucciarelli, V.; Baserga, C.; Codari, M.; Beltramini, G.A.; Sforza, C.; Giannì, A.B. Three-Dimensional Stereophotogrammetric Evaluation of the Efficacy of Autologous Fat Grafting in the Treatment of Parry-Romberg Syndrome. J. Craniofacial Surg. 2018, 29, 2124–2127. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Xie, Y.; Zhu, M.; Zhao, P.; Chen, Z.; Cheng, C.; Huang, R.; Liu, K.; Li, Q. The second fat graft has significantly better outcome than the first fat graft for Romberg syndrome: A study of three-dimensional volumetric analysis. J. Plast. Reconstr. Aesthetic Surg. 2016, 69, 1621–1626. [Google Scholar] [CrossRef]
- Van Der Cruyssen, F.; Meeus, J.; Schoenaers, J.; Politis, C. Parry Romberg syndrome: A long-term retrospective cohort study of 10 patients. Oral Maxillofac. Surg. Cases 2018, 4, 73–83. [Google Scholar] [CrossRef]
- Abdullaev, K.F.; Orlova, E.V.; Yadav, M.K.; Vasilyev, E.A.; Mokhirev, M.A.; Gileva, K.S. Preoperative planning for advanced modelling of anterolateral thigh flaps in the treatment of severe haemifacial atrophy in Parry–Romberg and Goldenhar syndrome. JPRAS Open 2018, 16, 36–49. [Google Scholar] [CrossRef]
- Coleman, S.R. Structural Fat Grafting: More Than a Permanent Filler. Plast. Reconstr. Surg. 2006, 118, 108S–120S. [Google Scholar] [CrossRef]
- De Menezes, M.; Rosati, R.; Ferrario, V.F.; Sforza, C. Accuracy and Reproducibility of a 3-Dimensional Stereophotogrammetric Imaging System. J. Oral Maxillofac. Surg. 2010, 68, 2129–2135. [Google Scholar] [CrossRef]
- Pucciarelli, V.; Tarabbia, F.; Codari, M.; Guidugli, G.A.; Colletti, G.; Orabona, G.D.; Bianchi, B.; Sforza, C.; Biglioli, F. Stereophotogrammetric Evaluation of Labial Symmetry After Surgical Treatment of a Lymphatic Malformation. J. Craniofacial Surg. 2017, 28, e355–e358. [Google Scholar] [CrossRef]
- Codari, M.; Pucciarelli, V.; Stangoni, F.; Zago, M.; Tarabbia, F.; Biglioli, F.; Sforza, C. Facial thirds–based evaluation of facial asymmetry using stereophotogrammetric devices: Application to facial palsy subjects. J. Craniomaxillofacial Surg. 2017, 45, 76–81. [Google Scholar] [CrossRef]
- Wermker, K.; Kleinheinz, J.; Jung, S.; Dirksen, D. Soft tissue response and facial symmetry after orthognathic surgery. J. Craniomaxillofacial Surg. 2014, 42, e339–e345. [Google Scholar] [CrossRef] [PubMed]
- Mangiafico, S.S. Summary and Analysis of Extension Program Evaluation in R, Version 1.18.1. 2016. Available online: www.rcompanion.org/handbook/ (accessed on 13 December 2020).
- Piombino, P.; Marenzi, G.; Dell’Aversana Orabona, G.; Califano, L.; Sammartino, G. Autologous Fat Grafting in Facial Volumetric Restoration. J. Craniofacial Surg. 2015, 26, 756–759. [Google Scholar] [CrossRef]
- Anderson, C.; Jahromi, A.H.; Miller, E.J.; Konofaos, P. The Current Status of the Autologous Fat Grafting for Pediatric Craniofacial Patients. Ann. Plast. Surg. 2020, 85, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Balaji, S.M. Subdermal fat grafting for Parry-Romberg syndrome. Ann. Maxillofac. Surg. 2014, 4, 55–59. [Google Scholar] [CrossRef]
- Lim, A.A.; Fan, K.L.; Allam, K.A.; Wan, D.; Tabit, C.; Liao, E.; Kawamoto, H.K.; Bradley, J.P. Autologous Fat Transplantation in the Craniofacial Patient. J. Craniofacial Surg. 2012, 23, 1061–1066. [Google Scholar] [CrossRef]
- Thevara, D.J.; Kumar, C.V. Application of photogrammetry to automated finishing operations. IOP Conf. Ser. Mater. Sci. Eng. 2018, 402, 012025. [Google Scholar] [CrossRef]
- Guerra, M.G.; De Chiffre, L.; Lavecchia, F.; Galantucci, L.M. Use of Miniature Step Gauges to Assess the Performance of 3D Optical Scanners and to Evaluate the Accuracy of a Novel Additive Manufacture Process. Sensors 2020, 20, 738. [Google Scholar] [CrossRef]
- Sforza, C.; De Menezes, M.; Ferrario, V. Soft- and hard-tissue facial anthropometry in three dimensions: What’s new. J. Anthr. Sci. 2013, 91, 159–184. [Google Scholar] [CrossRef]
- Clauser, L.; Tieghi, R.; Galiè, M.; Carinci, F. Structural Fat Grafting. J. Craniofacial Surg. 2011, 22, 1695–1701. [Google Scholar] [CrossRef]
- Wang, Y.-C.; Wallace, C.G.; Pai, B.C.-J.; Chen, H.-L.; Lee, Y.-T.; Hsiao, Y.-C.; Chang, C.-S.; Liao, Y.-F.; Chen, P.K.-T.; Chen, Y.-R. Orthognathic Surgery with Simultaneous Autologous Fat Transfer for Correction of Facial Asymmetry. Plast. Reconstr. Surg. 2017, 139, 693–700. [Google Scholar] [CrossRef]
- Qiao, J.; Gui, L.; Fu, X.; Niu, F.; Liu, J.; Chen, Y.; Wang, M.; Chen, J.; You, Y. A Novel Method of Mild to Moderate Parry–Romberg Syndrome Reconstruction. J. Craniofacial Surg. 2017, 28, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Denadai, R.; Raposo-Amaral, C.A.; Buzzo, C.L.; Raposo-Amaral, C.E. Autologous Free Fat Grafting for Management of the Facial Contour Asymmetry. J. Craniofacial Surg. 2018, 29, 878–886. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).