Binding Sites of Anti-Lcr V Monoclonal Antibodies Are More Critical than the Avidities and Affinities for Passive Protection against Yersinia pestis Infection in a Bubonic Plague Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Strains and mAbs
2.2. Animal Studies
2.3. Binding of mAbs to V-Antigen Peptides or V-Antigens
2.4. Competitive Binding of mAbs
2.5. Avidity ELISA Assay
2.6. Biacore Surface Plasmon Resonance (SPR) Analysis of mAb Binding to V-Antigen
2.7. Statistics
3. Results
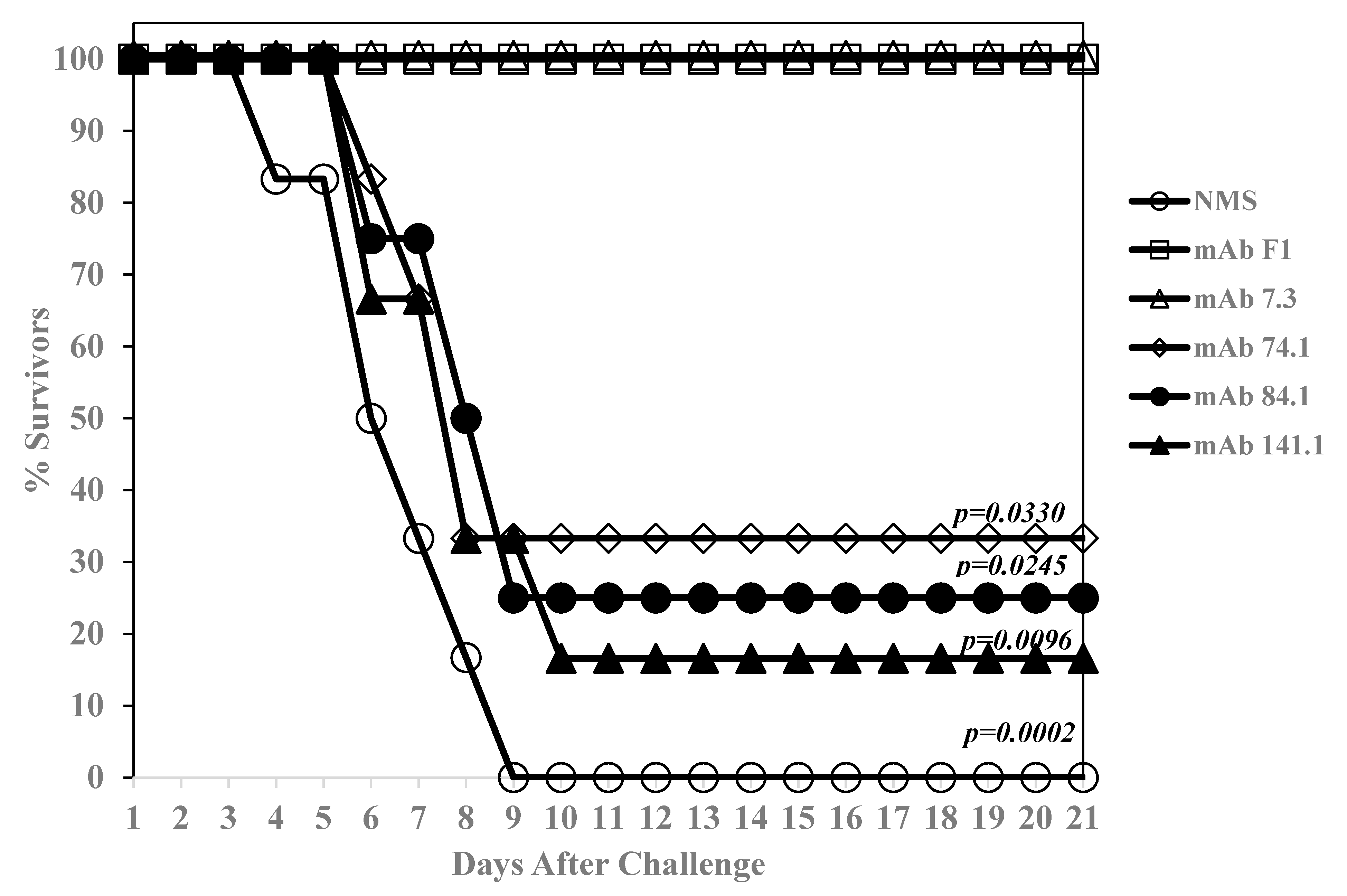
3.1. Potency of Anti-Y. Pestis mAb 7.3
3.2. Isolation of Protective Anti-V mAbs
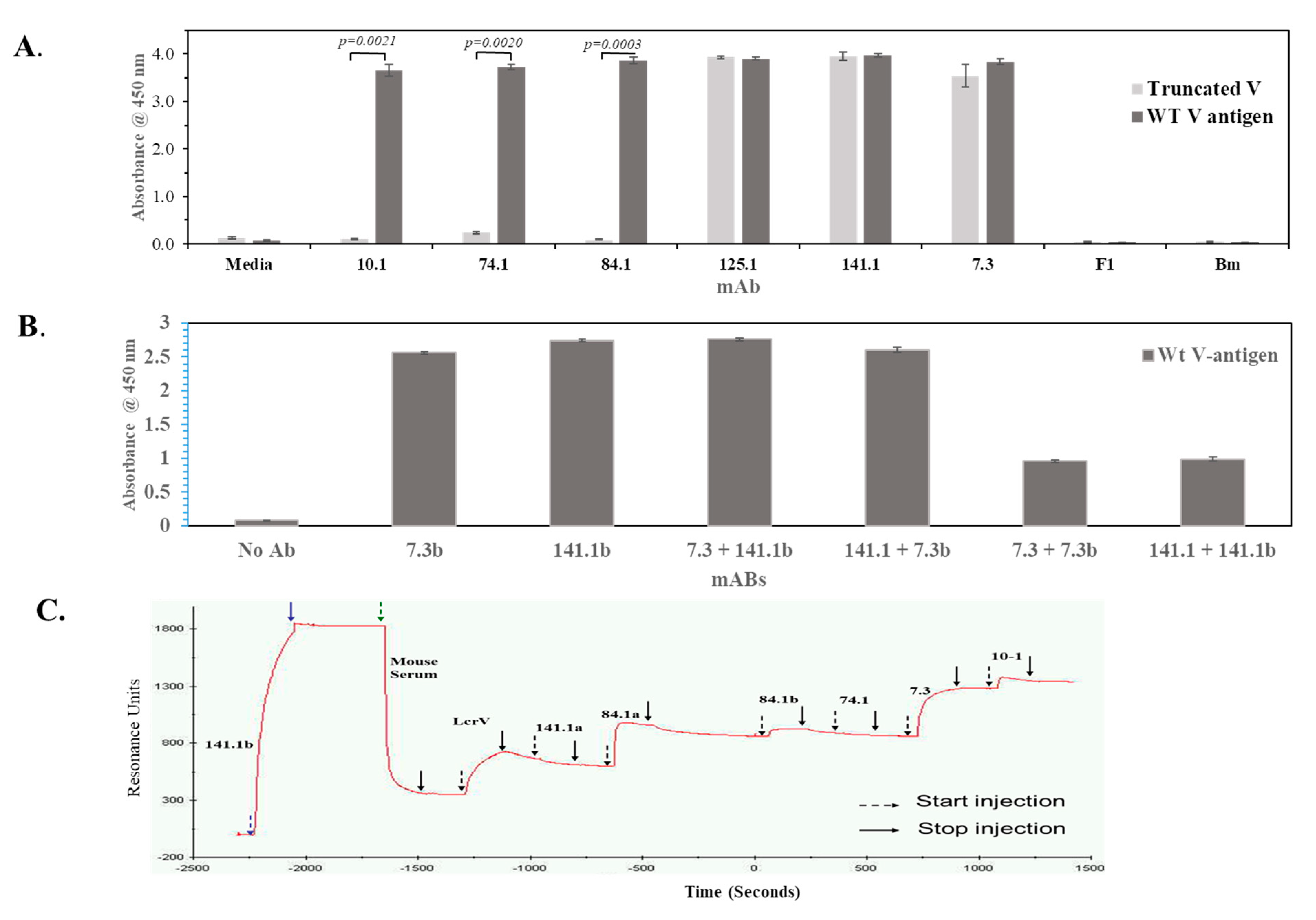
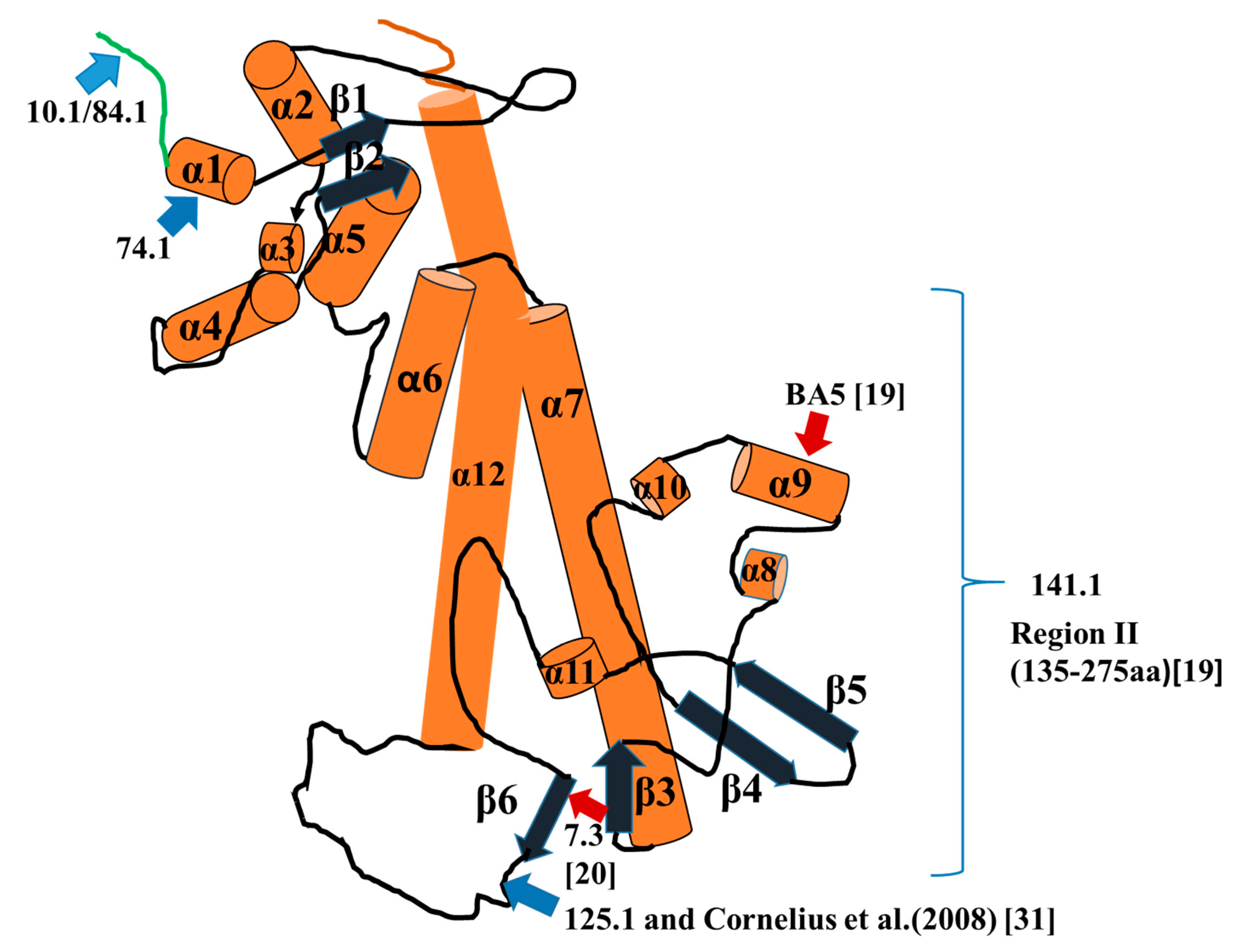
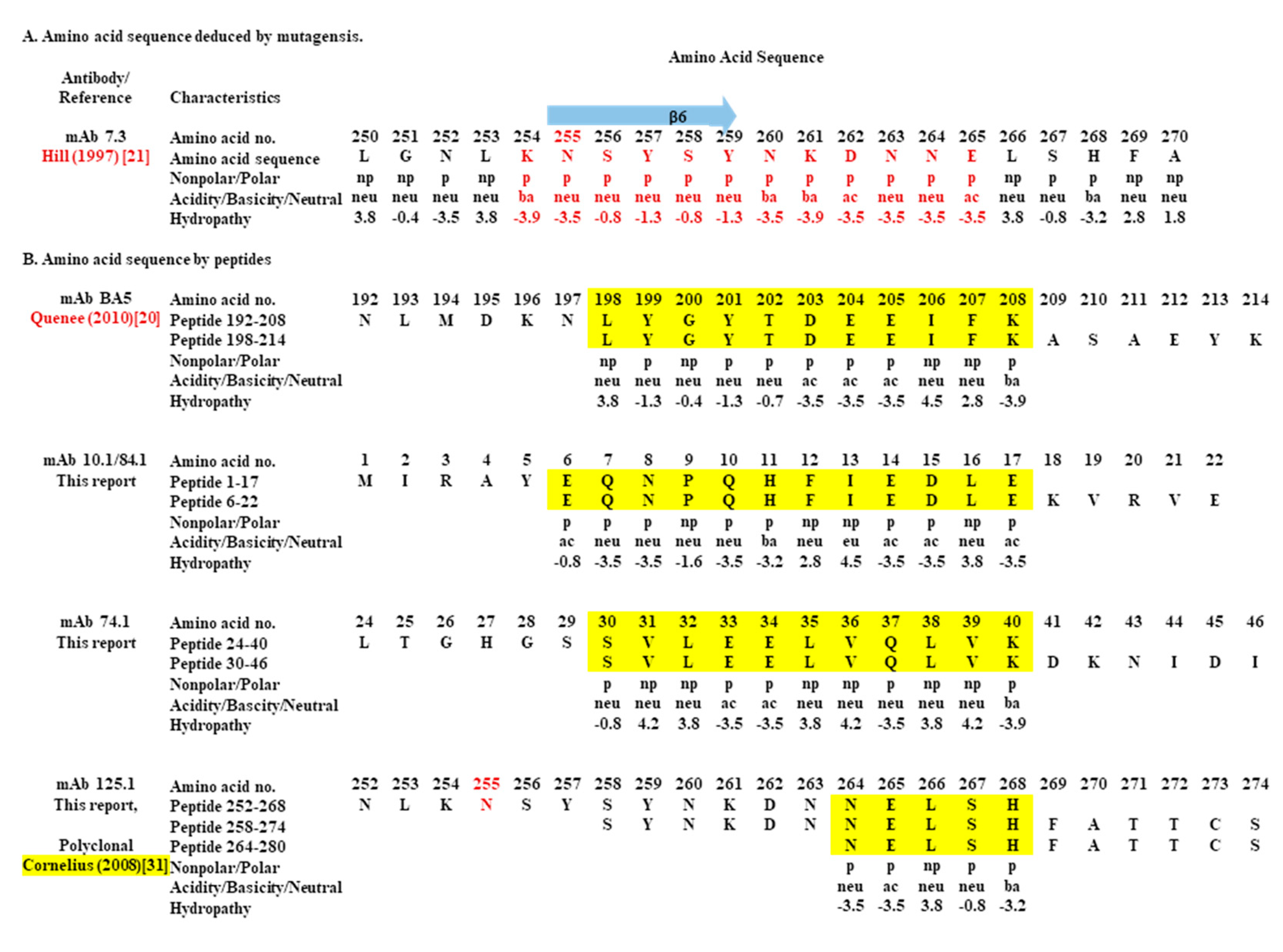
3.3. Comparison of the Binding Sites of the Protective Anti-V mAbs with that of Anti-V 7.3 mAbs on the V-Antigen
3.4. Binding of Anti-V mAbs and 7.3 to Regions of a Truncated V-Antigen
3.5. mAbs 141.1 and 7.3 do not Bind to the Same Conformational Site on the V-Antigen
3.6. mAb 7.3 Does not Have a Higher Avidity or Affinity to the V-Antigen than Less Protective mAbs
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Perry, R.D.; Fetherston, J.D. Yersinia pestis-etiologic agent of plague. Clin. Microbiol. Rev. 1997, 10, 35–66. [Google Scholar] [CrossRef]
- Demeure, C.E.; Dussurget, O.; Fiol, G.M.; Le Guern, A.-S.; Savin, C.; Pizarro-Cerda, J. Yersinia pestis and plague: An updated view on evolution, virulence determinants, immume subversion, vaccination, and diagnostics. Genes Immun. 2019, 20, 357–370. [Google Scholar] [CrossRef] [PubMed]
- Dewoody, R.S.; Merritt, P.M.; Marketon, M.M. Regulation of the Yersinia type III secretion system: Traffic control. Front. Cell. Infect. Microbiol. 2013, 3, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cornelis, G.R. The yersinia ysc-yop type III weaponry. Nat. Rev. Mol. Cell Biol. 2002, 3, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.A.; Broz, P.; Muller, S.A.; Ringler, P.; Erne-Brand, F.; Sorg, I.; Kuhn, M.; Engel, A.; Cornelis, G.R. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science 2005, 310, 674–676. [Google Scholar] [CrossRef]
- Butler, T. Plague history: Yersin′s discovery of the causative bacterium in 1894 enabled, in the subsequent century, scientific progress in understanding the disease and the development of treatments and vaccines. Clin. Microbiol. Infect. 2014, 20, 202–209. [Google Scholar] [CrossRef]
- Baker, E.E.; Sommer, H.; Foster, L.E.; Meyer, E.; Meyer, K.F. Studies on immunization against plague: I. The isolatiom and characterizatiom of the soluble antigen of Pasterurella pestis. J. Immumol. 1952, 68, 131–145. [Google Scholar]
- Lawton, W.D.; Fukui, G.M.; Surgalla, M.J. Studies on the antigens of Pasteurella pestis and Pasteurella pseudotuberculosis. J. Immuol. 1960, 84, 475–479. [Google Scholar]
- Lawton, W.D.; Erdman, R.L.; Sugalla, M.J. Biosynthesis and purification of V ad W antigen in Pasteurella pestis. J. Immunol. 1963, 91, 179–184. [Google Scholar]
- Williamson, E.D.; Eley, S.M.; Griffin, K.F.; Green, M.; Russell, P.; Leary, S.E.C.; Oyston, P.C.F.; Easterbrook, T.; Reddin, K.M.; Robinson, A.; et al. A new improved sub-unit vaccine for plague: The basis of protection. FEMS Immunol. Med. Microbiol. 1995, 12, 223–230. [Google Scholar] [CrossRef]
- Heath, D.G.; Anderson, G.W.; Welkos, S.L.; Andrews, G.P.; Friedlander, A.M.; Mauro, J.M. A recombinant capsular F1-V antigen fusion protein vaccine protects against experimental bubonic and pneumonic plague. In Vaccines 97; Brown, F., Burton, D., Doherty, P., Mekalanos, J., Norrby, E., Eds.; Cold Spring Harbor Laboratory Press: Cold Spring Harbor, NY, USA, 1997; pp. 197–200. [Google Scholar]
- Heath, D.G.; Anderson, G.W., Jr.; Mauro, J.M.; Welkos, S.L.; Andrews, G.P.; Adamovicz, J.; Friedlander, A.M. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine 1998, 16, 1131–1137. [Google Scholar] [CrossRef]
- Williamson, E.D.; Vesey, P.M.; Gillhespy, K.J.; Eley, S.M.; Green, M.; Titball, R.W. An IgG1 titre to the F1 and V antigens correlates with protection against plague in the mouse model. Clin. Exp. Immunol. 1999, 116, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Amemiya, K.; Meyers, J.L.; Rogers, T.E.; Fast, R.L.; Bassett, A.D.; Worsham, P.L.; Powell, B.S.; Norris, S.L.; Krieg, A.M.; Adamovicz, J.J. CpG oligodeoxynucleotides augment the murine immune response to the Yersinia pestis F1-V vaccine in bubonic and pneumonic models of plague. Vaccine 2009, 27, 2220–2229. [Google Scholar] [CrossRef]
- Parent, M.A.; Berggren, K.N.; Kummer, L.W.; Wilhelm, L.B.; Szaba, F.M.; Mullarky, I.K.; Smiley, S.T. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect. Immun. 2005, 73, 7304–7310. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-S.; Park, S.; Adamovicz, J.J.; Hill, J.; Bliska, J.B.; Cote, C.K.; Perlin, D.S.; Amemiya, K.; Smiley, S.T. TNFa and IFNg contribute to F1/LcrV-targeted immune defense in mouse models of fully virulent pneumonic plague. Vaccine 2011, 29, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Dankmeyer, J.L.; Fast, R.L.; Cote, C.K.; Worsham, P.L.; Fritz, D.; Fisher, D.; Kern, S.J.; Merkel, T.; Kirschning, C.J.; Amemiya, K. Multiple roles of MyD88 in the immune response to the plague F1-V vaccine and in protection against an aerosol challenge of Yersinia pestis CO92 in mice. J. Immumol. Res. 2014, 2014, 1–13. [Google Scholar] [CrossRef]
- Anderson, G.W.; Worsham, P.L.; Bolt, C.R.; Andrews, G.P.; Welkos, S.L.; Friedlander, A.M.; Burans, J.P. Protection of mice from fatal bubonic and pneumonic plague by passive immunization with monoclonal antibodies against the F1 protein of Yersinia pestis. Am. J. Trop. Med. Hyg. 1997, 56, 471–473. [Google Scholar] [CrossRef]
- Hill, J.; Leary, S.E.C.; Griffin, K.F.; Williamson, E.D.; Titball, R.W. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect. Immun. 1997, 65, 4476–4482. [Google Scholar] [CrossRef] [PubMed]
- Quenee, L.E.; Berube, B.J.; Segal, J.; Elli, D.; Ciletti, N.A.; Anderson, D.; Schneewind, O. Amino acid residues 196–225 of LcrV represent a plague protective epitope. Vaccine 2010, 28, 1870–1876. [Google Scholar] [CrossRef][Green Version]
- Hill, J.; Leary, S.; Smither, S.; Best, A.; Petterson, J.; Forsberg, A.; Lingard, B.; Lipka, A.; Brown, K.A.; Williamson, E.D.; et al. N255 is a key residue for recognition by a monoclonal antibody which protects against Yersinia pestis infection. Vaccine 2009, 27, 7073–7079. [Google Scholar] [CrossRef]
- Hill, J.; Copse, C.; Leary, S.; Stagg, A.J.; Williamson, E.D.; Titball, R.W. Synergistic protection of mice against plague with monoclonal antibodies specific for the F1 and V antigens of Yersinia pestis. Infect. Immun. 2003, 71, 2234–2238. [Google Scholar] [CrossRef] [PubMed]
- Doll, J.M.; Zeitz, P.A.; Ettestad, P.; Bucholtz, A.L.; Davis, T.; Gage, K. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am. J. Trop. Med. Hyg. 1994, 51, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Worsham, P.L.; Stein, M.-P.; Welkos, S.L. Construction of defined F1 negative mutants of virulent Yersinia pestis. Contrib. Microbiol. Immunol. 1995, 13, 325–328. [Google Scholar] [PubMed]
- Anderson, G.W.; Leary, S.E.C.; Williamson, E.D.; Titball, R.W.; Welkos, S.L.; Worsham, P.L.; Friedlander, A.M. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect. Immun. 1996, 64, 4580–4585. [Google Scholar] [CrossRef]
- Xiao, X.; Zhu, Z.; Dankmeyer, J.L.; Wormald, M.M.; Fast, R.L.; Worsham, P.L.; Cote, C.L.; Amemiya, K.; Dimitrov, D.S. Human anti-plague monoclonal antibodies protect mice from Yersinia pestis in a bubonic plague model. PLoS ONE 2010, 5, e13047. [Google Scholar] [CrossRef]
- Welkos, S.L.; Davis, K.M.; Pitt, L.M.; Worsham, P.L.; Friedlander, A.M. Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib. Microbiol. Immunol. 1995, 13, 299–305. [Google Scholar]
- Heine, H.S.; Louie, A.; Sorgel, F.; Bassett, J.; Miller, L.; Sullivan, L.J.; Kinzig-Schippers, M.; Drusano, G.L. Comparison of 2 antibiotics that inhibit protein synthesis for the treatment of infecrion with Yersina pestis delivered by aerosol in a mouse model of pneumonic plague. J. Infect. Dis. 2007, 196, 782–787. [Google Scholar] [CrossRef][Green Version]
- Amemiya, K.; Bush, G.V.; DeShazer, D.S.; Waag, D.M. Nonviable Burkholderia mallei induces a mixed Th1- and Th2-like cytokine response in BALB/c mice. Infect. Immun. 2002, 74, 2319–2325. [Google Scholar] [CrossRef]
- Derewenda, U.; Mateja, A.; Devedjiev, Y.; Routzahn, K.M.; Evdokimov, A.G.; Derewenda, Z.S.; Waugh, D.S. The structure of Yersinia pestis V-antigen, an essential virulence factor and mediator of immunity against plague. Structure 2004, 12, 301–306. [Google Scholar] [CrossRef]
- Cornelius, C.A.; Quenee, L.E.; Overheim, K.A.; Koster, F.; Brasel, T.L.; Elli, D.; Ciletti, N.A.; Schneewind, O. Immunization with recombinant V10 protects cynomolgus macaques from lethal pneumonic plague. Infect. Immun. 2008, 76, 5588–5597. [Google Scholar] [CrossRef]
- Vernazza, C.; Lingard, B.; Flick-Smith, H.C.; Baillie, L.W.J.; Hill, J.; Atkins, H.S. Small protective fragments of the Yersinia pestis V antigen. Vaccine 2009, 27, 2775–2780. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Trincado, J.L.; Gomez-Perosanz, M.; Reche, P.A. Fundamentals and methods for T- and B-cell epitope prediction. J. Immunol. Res. 2017, 2017, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.A.; Broz, P.; Cornelis, G.R. The type III secretion system tip complex and translocation. Mol. Microbiol. 2008, 68, 1085–1095. [Google Scholar] [CrossRef]
- Nilles, M.L.; Williams, A.W.; Skrzypek, E.; Straley, S.C. Yersinia pestis LcrV forma a stable complex with LcrG and may have a secretion-related regulatory role in the low-Ca2+ response. J. Bacteriol. 1997, 179, 1307–1316. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Matson, J.S.; Nilles, M.L. LcrG-LcrV interacrion is required for control of Yops secretion in Yersinia pestis. J. Bacteriol. 2001, 183, 5082–5091. [Google Scholar] [CrossRef]
- Lawton, D.G.; Longstaffs, C.; Wallace, B.A.; Hill, J.; Leary, S.E.C.; Titball, R.W.; Brown, K.A. Interactions of the type III secretion pathway proteins LcrV and LcrG from Yersinia pestis are mediated by coiled-coil domains. J. Biol. Chem. 2002, 41, 38714–38722. [Google Scholar] [CrossRef] [PubMed]
- Weeks, S.; Hill, J.; Friedlander, A.; Welkos, S. Anti-V antigen antibody protects macrophages from Yersinia pestis-induced cell death and promotes phagocytosis. Microb. Pathog. 2002, 32, 227–237. [Google Scholar] [CrossRef]

| mAb | Amount Given (i.p.) b | Challenge Dose No. LD50 c (s.c.) d | No. Survivors (after 28 Days) | Mean Time to Death (MTD (Days) e |
|---|---|---|---|---|
| 7.3 | 500 µg | 21 | 8/8 | >28 |
| 7.3 | 50 µg | 21 | 8/8 | >28 |
| 7.3 | 10 µg | 21 | 6/8 | 14.5 |
| 7.3 | 5.0 µg | 21 | 1/8 (p = 0.0061) | 15.1 |
| 7.3 | 1.0 µg | 21 | 0/8 (p < 0.0001) | 7.3 |
| Bm (Neg Con) a | 1.0 mg | 21 | 0/8 (p < 0.0001) | 7.3 |
| Rab 3–89 (Pos Con) | 0.5 mg | 21 | 7/8 | 12.0 |
| Isotype | Amount Given (mg) c | Challenge Dose (LD50) d | No. Survivors (after 15 Days) | MTD (Days) e | |
|---|---|---|---|---|---|
| 10.1 a | IgG1 | 5.0 | 25 | 3/6 | 5.7 |
| 74.1 a | IgG1 | 5.0 | 25 | 4/6 | 6.0 |
| 84.1 a | IgG2a | 5.0 | 25 | 3/6 | 6.3 |
| 125.1 a | IgG1 | 5.0 | 25 | 3/6 | 7.3 |
| 141.1 a | IgG1 | 5.0 | 25 | 3/6 | 5.3 |
| 7H12 (Neg Con) b | IgG1 | 3.0 | 25 | 1/6 | 6.0 |
| Rab 3–89 (Pos Con) b | NA | 5.0 | 25 | 6/6 | >15 |
| mAb a | KD (nM) ± SE | ka × 104 (1/Ms) ± SE | kd × 10−4 (1/s) ± SE |
|---|---|---|---|
| 10.1 | 24.3 ± 0.9 b | 5.67 ± 0.42 | 13.8 ± 1.05 |
| 84.1a | 10.7 ± 0.5 b,c | 9.11 ± 0.35 | 9.66 ± 0.2 |
| 84.1b | 25.4 ± 1.5 b,c | 7.73 ± 0.33 | 19.3 ± 0.43 |
| 7.3 | 4.03 ± 0.27 | 16.9 ± 0.47 | 6.98 ± 0.56 |
| 141.1a | 2.46 ± 0.06 b,c | 22.8 ± 0.49 | 5.64 ± 0.10 |
| 141.1b | 0.77 ± 0.06 b,c | 40.1 ± 0.51 | 3.07 ± 0.19 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amemiya, K.; Dankmeyer, J.L.; Keasey, S.L.; Trevino, S.R.; Wormald, M.M.; Halasohoris, S.A.; Ribot, W.J.; Fetterer, D.P.; Cote, C.K.; Worsham, P.L.; et al. Binding Sites of Anti-Lcr V Monoclonal Antibodies Are More Critical than the Avidities and Affinities for Passive Protection against Yersinia pestis Infection in a Bubonic Plague Model. Antibodies 2020, 9, 37. https://doi.org/10.3390/antib9030037
Amemiya K, Dankmeyer JL, Keasey SL, Trevino SR, Wormald MM, Halasohoris SA, Ribot WJ, Fetterer DP, Cote CK, Worsham PL, et al. Binding Sites of Anti-Lcr V Monoclonal Antibodies Are More Critical than the Avidities and Affinities for Passive Protection against Yersinia pestis Infection in a Bubonic Plague Model. Antibodies. 2020; 9(3):37. https://doi.org/10.3390/antib9030037
Chicago/Turabian StyleAmemiya, Kei, Jennifer L. Dankmeyer, Sarah L. Keasey, Sylvia R. Trevino, Michael M. Wormald, Stephanie A. Halasohoris, Wilson J. Ribot, David P. Fetterer, Christopher K. Cote, Patricia L. Worsham, and et al. 2020. "Binding Sites of Anti-Lcr V Monoclonal Antibodies Are More Critical than the Avidities and Affinities for Passive Protection against Yersinia pestis Infection in a Bubonic Plague Model" Antibodies 9, no. 3: 37. https://doi.org/10.3390/antib9030037
APA StyleAmemiya, K., Dankmeyer, J. L., Keasey, S. L., Trevino, S. R., Wormald, M. M., Halasohoris, S. A., Ribot, W. J., Fetterer, D. P., Cote, C. K., Worsham, P. L., Adamovicz, J. J., & Ulrich, R. G. (2020). Binding Sites of Anti-Lcr V Monoclonal Antibodies Are More Critical than the Avidities and Affinities for Passive Protection against Yersinia pestis Infection in a Bubonic Plague Model. Antibodies, 9(3), 37. https://doi.org/10.3390/antib9030037





