Equal Neutralization Potency of Antibodies Raised against Abrin Subunits
Abstract
1. Introduction
2. Materials and Methods
2.1. Extraction and Purification of Abrin and Ricin
2.2. Subunit Purification
2.3. Preparation of Chimeric Toxins
2.4. Gel Electrophoresis
2.5. ELISA Titer Determination
2.6. In-Vitro Abrin Neutralization Assay
2.7. Epitope Recognition
2.8. Animal Studies
2.9. Polyclonal Anti-Chimera Antibody Production
2.10. In-Vivo Protection Assay
3. Results
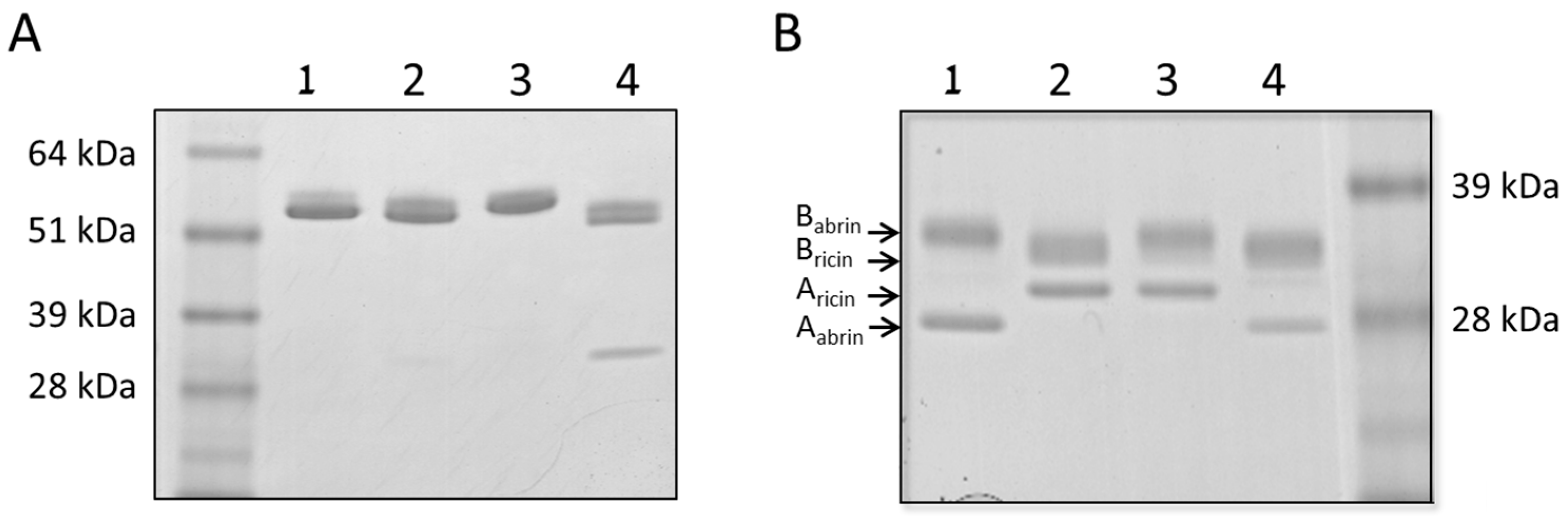
3.1. Characterization of the Chimeric Toxins
3.2. Abrin Subunit Recognition and Neutralization
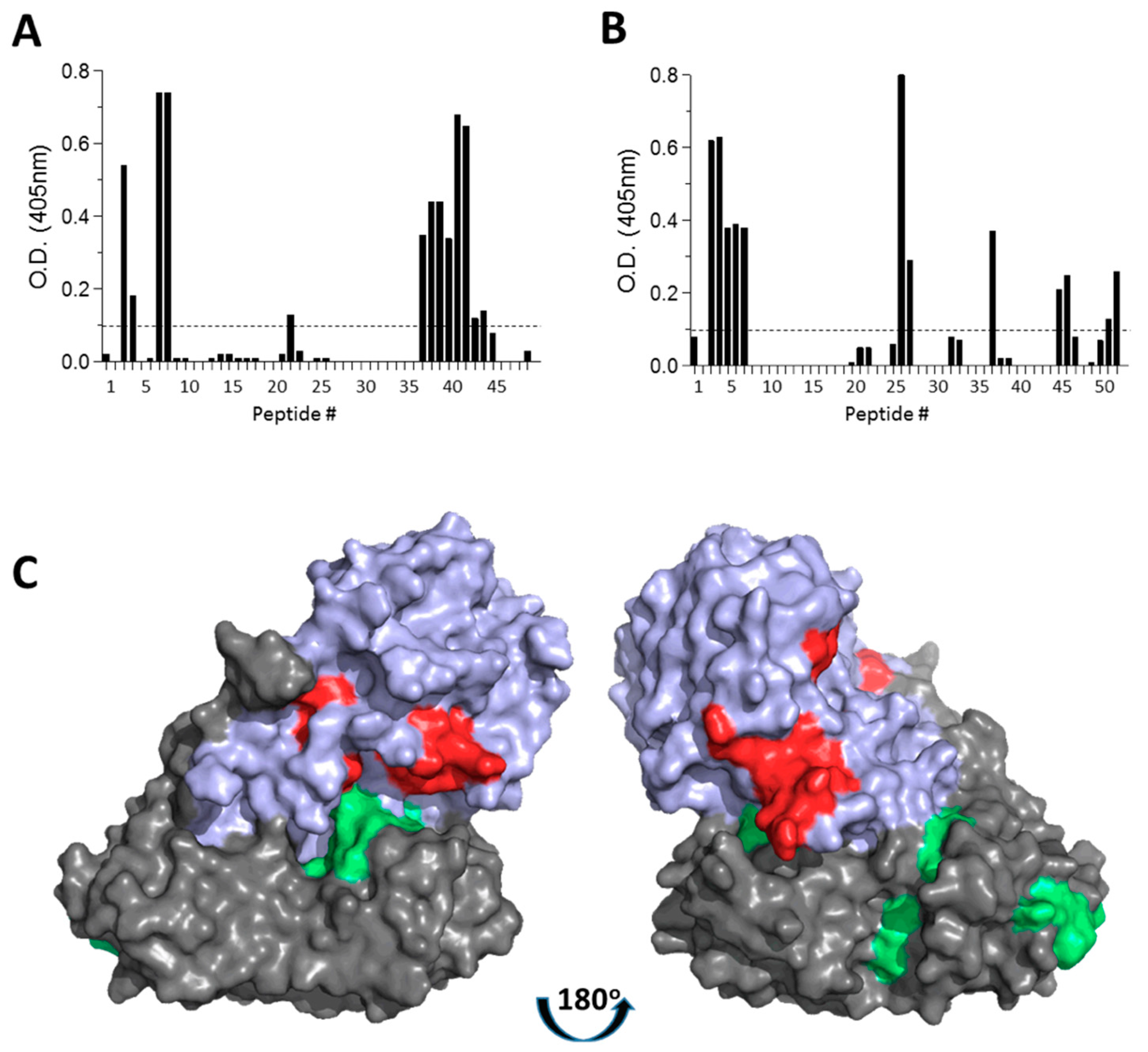
3.3. Abrin Linear-Epitope Recognition by Anti-Aabrin- and Anti-Babrin- Polyclonal Antibodies
3.4. Post-Exposure Treatment of Abrin Intoxicated Mice with Anti-Abrin Subunit-Directed Antisera
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Olsnes, S. The history of ricin, abrin and related toxins. Toxicon 2004, 44, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Audi, J.; Belson, M.; Patel, M.; Schier, J.; Osterloh, J. Ricin poisoning: a comprehensive review. JAMA 2005, 294, 2342–2351. [Google Scholar] [CrossRef] [PubMed]
- Gal, Y.; Mazor, O.; Alcalay, R.; Seliger, N.; Aftalion, M.; Sapoznikov, A.; Falach, R.; Kronman, C.; Sabo, T. Antibody/doxycycline combined therapy for pulmonary ricinosis: attenuation of inflammation improved survival of ricin-intoxicated mice. Toxicol. Rep. 2014, 1, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Sabo, T.; Kronman, C.; Mazor, O. Ricin-Holotoxin-Based Vaccines: Induction of Potent Ricin-Neutralizing Antibodies. Methods Mol. Biol. 2016, 1403, 683–694. [Google Scholar] [CrossRef] [PubMed]
- Gal, Y.; Sapoznikov, A.; Falach, R.; Ehrlich, S.; Aftalion, M.; Kronman, C.; Sabo, T. Total Body Irradiation Mitigates Inflammation and Extends the Therapeutic Time Window for Anti-Ricin Antibody Treatment against Pulmonary Ricinosis in Mice. Toxins 2017, 9, 278. [Google Scholar] [CrossRef] [PubMed]
- Krupakar, J.; Swaminathan, C.P.; Das, P.K.; Surolia, A.; Podder, S.K. Calorimetric studies on the stability of the ribosome-inactivating protein abrin II: effects of pH and ligand binding. Biochem. J. 1999, 338, 273–279. [Google Scholar] [CrossRef]
- Kumar, M.S.; Karande, A.A. A monoclonal antibody to an abrin chimera recognizing a unique epitope on abrin A chain confers protection from abrin-induced lethality. Hum. Vaccin. Immunother 2016, 12, 124–131. [Google Scholar] [CrossRef]
- Falach, R.; Sapoznikov, A.; Gal, Y.; Israeli, O.; Leitner, M.; Seliger, N.; Ehrlich, S.; Kronman, C.; Sabo, T. Quantitative profiling of the in-vivo enzymatic activity of ricin reveals disparate depurination of different pulmonary cell types. Toxicol. Lett. 2016, 258, 11–19. [Google Scholar] [CrossRef]
- Sapoznikov, A.; Falach, R.; Mazor, O.; Alcalay, R.; Gal, Y.; Seliger, N.; Sabo, T.; Kronman, C. Diverse profiles of ricin-cell interactions in the lung following intranasal exposure to ricin. Toxins 2015, 7, 4817–4831. [Google Scholar] [CrossRef]
- Mason, R.J. Biology of alveolar type II cells. Respirology 2006, 11, S12–S15. [Google Scholar] [CrossRef]
- Hegde, R.; Podder, S.K. Studies on the variants of the protein toxins ricin and abrin. Eur. J. Biochem. 1992, 204, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Olsnes, S.; Pihl, A. Isolation and properties of abrin: a toxic protein inhibiting protein synthesis. Evidence for different biological functions of its two constituent-peptide chains. Eur. J. Biochem. 1973, 35, 179–185. [Google Scholar] [CrossRef]
- Lin, J.Y.; Liu, S.Y. Studies on the antitumor lectins isolated from the seeds of Ricinus communis (castor bean). Toxicon 1986, 24, 757–765. [Google Scholar] [CrossRef]
- Luker, G.D.; Pica, C.M.; Song, J.; Luker, K.E.; Piwnica-Worms, D. Imaging 26S proteasome activity and inhibition in living mice. Nat. Med. 2003, 9, 969–973. [Google Scholar] [CrossRef] [PubMed]
- Olsnes, S.; Pappenheimer, A.M., Jr.; Meren, R. Lectins from Abrus precatorius and Ricinus communis. II. Hybrid toxins and their interaction with chain-specific antibodies. J. Immunol. 1974, 113, 842–847. [Google Scholar] [PubMed]
- Gal, Y.; Alcalay, R.; Sabo, T.; Noy-Porat, T.; Epstein, E.; Kronman, C.; Mazor, O. Rapid assessment of antibody-induced ricin neutralization by employing a novel functional cell-based assay. J. Immunol. Methods 2015, 424, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Mechaly, A.; Alcalay, R.; Noy-Porat, T.; Epstein, E.; Gal, Y.; Mazor, O. Novel Phage Display-Derived Anti-Abrin Antibodies Confer Post-Exposure Protection against Abrin Intoxication. Toxins 2018, 10, 80. [Google Scholar] [CrossRef]
- Teter, K. Toxin instability and its role in toxin translocation from the endoplasmic reticulum to the cytosol. Biomolecules 2013, 3, 997–1029. [Google Scholar] [CrossRef]
- Lord, J.M.; Roberts, L.M.; Lencer, W.I. Entry of protein toxins into mammalian cells by crossing the endoplasmic reticulum membrane: co-opting basic mechanisms of endoplasmic reticulum-associated degradation. Curr. Top. Microbiol. Immunol. 2005, 300, 149–168. [Google Scholar] [CrossRef]
- Wesche, J.; Rapak, A.; Olsnes, S. Dependence of ricin toxicity on translocation of the toxin A-chain from the endoplasmic reticulum to the cytosol. J. Biol. Chem. 1999, 274, 34443–34449. [Google Scholar] [CrossRef]
- Spooner, R.A.; Hart, P.J.; Cook, J.P.; Pietroni, P.; Rogon, C.; Hohfeld, J.; Roberts, L.M.; Lord, J.M. Cytosolic chaperones influence the fate of a toxin dislocated from the endoplasmic reticulum. Proc. Natl. Acad. Sci. USA 2008, 105, 17408–17413. [Google Scholar] [CrossRef] [PubMed]
- Bagaria, S.; Ponnalagu, D.; Bisht, S.; Karande, A.A. Mechanistic insights into the neutralization of cytotoxic abrin by the monoclonal antibody D6F10. PLoS ONE 2013, 8, e70273. [Google Scholar] [CrossRef] [PubMed]
- Surendranath, K.; Karande, A.A. A neutralizing antibody to the a chain of abrin inhibits abrin toxicity both in-vitro and in-vivo. Clin. Vaccine Immunol. 2008, 15, 737–743. [Google Scholar] [CrossRef] [PubMed]
| Antiserum (Relevant Abrin Subunit) | ELISA-Antibody Titers (× 105) | Neutralizing-Antibody Titers (× 103) |
|---|---|---|
| Anti-AabrinBricin (A) | 4.5 ± 0.1 | 1.1 ± 0.1 |
| Anti-AricinBabrin (B) | 8.1 ± 0.2* | 0.9 ± 0.3 |
| Epitope No. | Subunit | Epitope Sequence | Epitope Location |
|---|---|---|---|
| 1 | Aabrin | KQFIEALR | 18–25 |
| 2 | IPVLPDP | 36–42 | |
| 3 | YGTYGDL | 110–116 | |
| 4 | QPDAAMISLE | 186–195 | |
| 5 | LTIRN | 219–223 | |
| 6 | Babrin | VRIGGRDG | 16–23 |
| 7 | NGYHNG | 31–36 | |
| 8 | QGWRTGN | 134–140 | |
| 9 | DGSI | 183–186 | |
| 10 | WVKFNDGSI | 221–229 | |
| 11 | QIWLTLF | 261–267 |
| Survival | ||
|---|---|---|
| Antibody treatment | % | Survivors/Total |
| Control | 0 | 0/10 |
| Anti-Abrin | 90 | 9/10 |
| Anti-AabrinBricin | 90 | 9/10 |
| Anti-AricinBabrin | 95 | 19/20 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gal, Y.; Sapoznikov, A.; Falach, R.; Mazor, O.; Alcalay, R.; Elhanany, E.; Aftalion, M.; Ehrlich, S.; Kronman, C.; Sabo, T. Equal Neutralization Potency of Antibodies Raised against Abrin Subunits. Antibodies 2020, 9, 4. https://doi.org/10.3390/antib9010004
Gal Y, Sapoznikov A, Falach R, Mazor O, Alcalay R, Elhanany E, Aftalion M, Ehrlich S, Kronman C, Sabo T. Equal Neutralization Potency of Antibodies Raised against Abrin Subunits. Antibodies. 2020; 9(1):4. https://doi.org/10.3390/antib9010004
Chicago/Turabian StyleGal, Yoav, Anita Sapoznikov, Reut Falach, Ohad Mazor, Ron Alcalay, Eytan Elhanany, Moshe Aftalion, Sharon Ehrlich, Chanoch Kronman, and Tamar Sabo. 2020. "Equal Neutralization Potency of Antibodies Raised against Abrin Subunits" Antibodies 9, no. 1: 4. https://doi.org/10.3390/antib9010004
APA StyleGal, Y., Sapoznikov, A., Falach, R., Mazor, O., Alcalay, R., Elhanany, E., Aftalion, M., Ehrlich, S., Kronman, C., & Sabo, T. (2020). Equal Neutralization Potency of Antibodies Raised against Abrin Subunits. Antibodies, 9(1), 4. https://doi.org/10.3390/antib9010004





