Myelin Antigens and Antimyelin Antibodies
Abstract
:1. Introduction
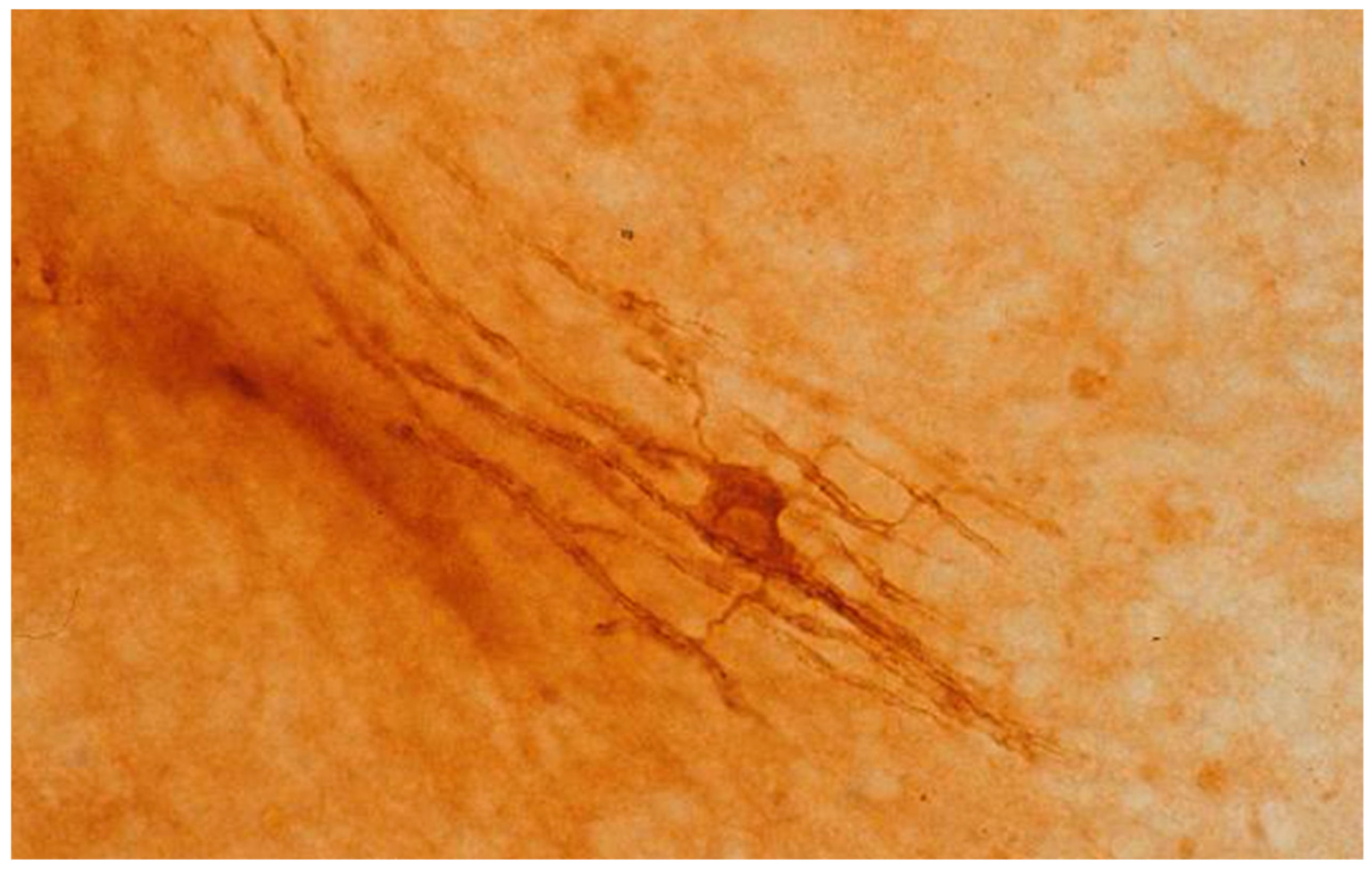
2. Myelin
3. EAE and Anti-MBP Antibodies
4. Other CNS Myelin Antigens
5. PNS Myelin Antigens and EAN
6. Significance of Antimyelin Antibodies
7. Human Demyelinating Disorders
8. Conclusions
Acknowledgments
Conflicts of Interest
References
- Bornstein, M.B.; Appel, S.H. The application of tissue culture to the study of experimental “allergic” encephalomyelitis. J. Neuropathol. Exp. Neurol. 1961, 20, 141–157. [Google Scholar] [CrossRef]
- Appel, S.H.; Bornstein, M.B. The application of tissue culture to the study of experimental allergic encephalomyelitis. II. Serum factors responsible for demyelination. J. Exp. Med. 1964, 119, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.B.; Bornstein, M.B. Myelin binding antibodies in vitro. Immunoperoxidase studies with experimental allergic encephalomyelitis, anti-galactocerebroside and multiple sclerosis sera. Brain Res. 1978, 159, 173–182. [Google Scholar] [CrossRef]
- Lebar, R.; Boutry, J.-M.; Vincent, C.; Robineaux, R.; Voisin, A. Studies on autoimmune encephalomyelitis in the guinea pig. II. An in vitro investigation on the nature, properties and specificity of the serum demyelinating factor. J. Immunol. 1976, 116, 1439–1446. [Google Scholar] [PubMed]
- Bornstein, M.B.; Raine, C.S. Experimental allergic encephalomyelitis: Antiserum inhibition of myelination in vitro. Lab. Investig. 1970, 23, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.B. A tissue culture approach to the demyelinative disorders. NCI Monogr. 1963, 11, 197–214. [Google Scholar]
- Peters, A.; Palay, S.L.; Webster, H.F. The Fine Structure of the Nervous System: The Neurons and Supporting Cells, 3rd ed.; Oxford Press: New York, NY, USA, 1991; pp. 222–265. [Google Scholar]
- Morell, P.; Quarles, R.H.; Norton, W.T. Myelin formation, structure and biochemistry. In Basic Neurochemistry, 5th ed.; Siegel, G.J., Agranoff, B.W., Albers, R.W., Molinoff, P.B., Eds.; Raven Press: New York, NY, USA, 1994; pp. 117–143. [Google Scholar]
- Eng, L.F.; Chao, F.-C.; Gerstl, B.; Pratt, D.; Tavaststjerna, M.G. The maturation of human white matter myelin. Fractionation of the myelin membrane proteins. Biochemistry 1968, 7, 4455–4465. [Google Scholar] [CrossRef] [PubMed]
- Quarles, R.H. Glycoproteins in myelin and myelin related membranes. In Complex Carbohydrates of Nervous Tissue; Margolis, R.U., Margolis, R.K., Eds.; Plenum: New York, NY, USA, 1979; pp. 209–233. [Google Scholar]
- Eylar, E.H.; Uyemura, K.; Brostoff, S.; Kitamura, K.; Ishaque, A.; Greenfield, S. Proposed nomenclature for PNS myelin proteins. Neurochem. Res. 1979, 4, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Braun, P.E.; Brostoff, S.W. Proteins of myelin. In Myelin; Morell, P., Ed.; Plenum: New York, NY, USA, 1977; pp. 201–231. [Google Scholar]
- Lumsden, C.E. Immunopathological events in multiple sclerosis. Int. Congr. Ser. Excerpta Med. 1966, 100, 231–239. [Google Scholar]
- Kies, M.W.; Alvord, E.C., Jr. Encephalitogenic activity in guinea pigs of water-soluble protein fractions of nervous tissue. In “Allergic” Encephalomyelitis; Kies, M.W., Alvord, E.C., Jr., Eds.; Thomas: Springfield, IL, USA, 1959; pp. 293–299. [Google Scholar]
- Roboz, E.; Henderson, N. Preparation and properties of water-soluble proteins from bovine cord with “allergic” encephalomyelitic activity. In “Allergic” Encephalomyelitis; Kies, M.W., Alvord, E.C., Jr., Eds.; Thomas: Springfield, IL, USA, 1959; pp. 281–292. [Google Scholar]
- Seil, F.J.; Falk, G.A.; Kies, M.W.; Alvord, E.C., Jr. The in vitro demyelinating activity of sera from guinea pigs sensitized with whole CNS and with purified encephalitogen. Exp. Neurol. 1968, 22, 545–555. [Google Scholar] [CrossRef]
- Kies, M.W.; Driscoll, B.F.; Seil, F.J.; Alvord, E.C., Jr. Myelination inhibition factor: Dissociation from induction of experimental allergic encephalomyelitis. Science 1973, 179, 689–690. [Google Scholar] [CrossRef] [PubMed]
- Seil, F.J.; Rauch, H.C.; Einstein, E.R.; Hamilton, A.E. Myelination inhibition factor: Its absence in sera from subhuman primates sensitized with myelin basic protein. J. Immunol. 1973, 111, 96–100. [Google Scholar] [PubMed]
- Seil, F.J.; Smith, M.E.; Leiman, A.L.; Kelly, J.M. Myelination inhibiting and neuroelectric blocking factors in experimental allergic encephalomyelitis. Science 1975, 187, 951–953. [Google Scholar] [CrossRef] [PubMed]
- Seil, F.J.; Kies, M.W.; Bacon, M.L. Neural antigens and induction of myelination inhibition factor. J. Immunol. 1975, 114, 630–634. [Google Scholar] [PubMed]
- Seil, F.J.; Kies, M.W.; Agrawal, H.C.; Quarles, R.H.; Brady, R.O. Myelin proteins dissociated from induction of antimyelin antibodies. In Tissue Culture in Neurobiology; Giacobini, E., Vernadakis, A., Shahar, A., Eds.; Raven Press: New York, NY, USA, 1980; pp. 477–488. [Google Scholar]
- Dubois-Dalcq, M.; Niedieck, B.; Buyse, M. Action of anti-cerebroside sera on myelinated tissue cultures. Pathol. Eur. 1970, 5, 331–347. [Google Scholar] [PubMed]
- Fry, J.M.; Weissbarth, S.; Lehrer, G.M.; Bornstein, M.B. Cerebroside antibody inhibits sulfatide synthesis and myelination and demyelinates in cord tissue cultures. Science 1974, 183, 540–542. [Google Scholar] [CrossRef] [PubMed]
- Saida, T.; Silberberg, D.H.; Fry, J.M.; Manning, M.C. Demyelinating antigalactocerebroside antibodies in EAN and EAE. J. Neuropathol. Exp. Neurol. 1977, 36, 627. [Google Scholar]
- Bornstein, M.B.; Raine, C.S. Multiple sclerosis and experimental allergic encephalomyelitis: Specific demyelination of CNS in culture. Neuropathol. Appl. Neurobiol. 1977, 3, 359–367. [Google Scholar] [CrossRef]
- Hruby, S.; Alvord, E.C., Jr.; Seil, F.J. Synthetic galactocerebrosides evoke myelination-inhibiting antibodies. Science 1977, 195, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Lebar, R.; Vincent, C.; Fischer-le Boubennec, E. Studies on autoimmune encephalomyelitis in the guinea pig. III. A comparative study of two autoantigens of central nervous system myelin. J. Neurochem. 1979, 33, 1451–1460. [Google Scholar] [CrossRef]
- Lebar, R.; Lubetzki, C.; Vincent, C.; Lombrail, P.; Boutry, J.-M. The M2 autoantigen of central nervous sysrem myelin, a glycoprotein present in oligodendrocyte membrane. Clin. Exp. Immunol. 1986, 66, 423–443. [Google Scholar] [PubMed]
- Herndon, R.M.; Rauch, H.C.; Einstein, E.R. Immune-electron microscopic localization of the encephalitogenic basic protein in myelin. Immunol. Commun. 1973, 2, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Quarles, R.H.; Everly, J.L.; Brady, R.O. Demonstration of a glycoprotein which is associated with a purified myelin fraction from rat brain. Biochem. Biophys. Res. Commun. 1972, 47, 491–497. [Google Scholar] [CrossRef]
- Poduslo, J.F.; Quarles, R.H.; Brady, R.O. External labeling of galactose in surface membrane glycoproteins of the intact myelin sheath. J. Biol. Chem. 1976, 251, 153–158. [Google Scholar] [PubMed]
- Seil, F.J.; Quarles, R.H.; Johnson, D.; Brady, R.O. Immunization with purified myelin-associated glycoprotein does not evoke myelination-inhibiting or demyelinating antibodies. Brain Res. 1981, 209, 470–475. [Google Scholar] [CrossRef]
- Williams, R.M.; Lees, M.B.; Cambi, F.; Macklin, W.B. Chronic experimental allergic encephalomyelitis induced in rabbits with bovine white matter proteolipid apoprotein. J. Neuropathol. Exp. Neurol. 1982, 41, 508–521. [Google Scholar] [CrossRef] [PubMed]
- Cambi, F.; Lees, M.B.; Williams, R.M.; Macklin, W.B. Chronic experimental allergic encephalomyelitis produced by bovine proteolipid apoprotein: Immunological studies in rabbits. Ann. Neurol. 1983, 13, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Seil, F.J.; Agrawal, H.C. Myelin proteolipid protein does not induce demyelinating or myelination-inhibiting antibodies. Brain Res. 1980, 194, 273–277. [Google Scholar] [CrossRef]
- Mithen, F.; Bunge, R.; Agrawal, H. Proteolipid protein antiserum does not affect CNS myelin in rat spinal cord culture. Brain Res. 1980, 197, 477–483. [Google Scholar] [CrossRef]
- Nagai, Y.; Momoi, T.; Saito, M.; Mitsuzawa, E.; Ohtani, S. Ganglioside syndrome, a new autoimmune neurologic disorder, experimentally induced with brain gangliosides. Neurosci. Lett. 1976, 2, 107–111. [Google Scholar] [CrossRef]
- Cohen, O.; Schwartz, M.; Cohen, I.R.; Sela, B.-A.; Eshhar, N. Multiple sclerosis-like disease induced in rabbits by immunization with brain gangliosides. Isr. J. Med. Sci. 1981, 17, 711–714. [Google Scholar] [PubMed]
- Konat, G.; Offner, H.; Lev-Ram, V.; Cohen, O.; Schwartz, M.; Cohen, I.R.; Sela, B.A. Abnormalities of brain myelin in rabbits with experimental autoimmune multiple sclerosis-like disease induced by immunization to gangliosides. Acta Neurol. Scand. 1982, 66, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Bourdette, D.N.; Zalc, B.; Baumann, N.; Seil, F.J. Antisera to the ganglioside GM1 do not have anti-myelin or anti-axon activities in vitro. Brain Res. 1989, 478, 175–180. [Google Scholar] [CrossRef]
- Gonzales-Sastre, F. The protein composition of isolated myelin. J. Neurochem. 1970, 17, 1049–1056. [Google Scholar] [CrossRef]
- Wolfgram, F.; Kotorii, K. The composition of the myelin proteins of the central nervous system. J. Neurochem. 1968, 15, 1281–1290. [Google Scholar] [CrossRef] [PubMed]
- Quarles, R.H.; Pasnak, C.F. A rapid procedure for rapidly isolating the major glycoprotein from purified rat brain myelin. Biochem. J. 1977, 163, 635–637. [Google Scholar] [CrossRef] [PubMed]
- Reig, J.A.; Rames, J.M.; Cozar, M.; Aguilar, J.S.; Criado, M.; Monreal, J. Purification and chemical characterization of a W2 protein from rat brain myelin. J. Neurochem. 1982, 39, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Brunner, C.; Lassman, H.; Waehneldt, T.V.; Matthieu, J.-M.; Linington, C. Differential ultra-structural localization of myelin basic protein, myelin/oligodendrocyte glycoprotein, and 2′, 3′-cyclic nucleotide 3′-phosphodiesterase in the CNS of adult rats. J. Neurochem. 1989, 52, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Seil, F.J.; Garwood, M.M.; Clark, H.B.; Agrawal, H.C. Demyelinating and myelination-inhibiting factors induced by chloroform-methanol insoluble proteins of myelin. Brain Res. 1983, 288, 384–388. [Google Scholar] [CrossRef]
- Seil, F.J. Effects of humoral factors on myelin in organotypic cultures. In Multiple Sclerosis: Current Status of Research and Treatment; Herndon, R.M., Seil, F.J., Eds.; Demos: New York, NY, USA, 1994; pp. 33–50. [Google Scholar]
- Armor, S.; Groome, N.; Linington, C.; Morris, M.M.; Dornmair, K.; Gardinier, M.V.; Matthieu, J.M.; Baker, D. Identification of epitopes of myelin oligodendrocyte glycoprotein for the induction of experimental allergic encephalomyelitis in SJL and AB/H mice. J. Immunol. 1994, 153, 4349–4356. [Google Scholar]
- Adelmann, M.; Wood, J.; Benzel, I.; Fiori, P.; Lassmann, H.; Matthieu, J.M.; Gardinier, M.V.; Dornmair, K.; Linington, C. The N-terminal domain of the myelin oligodendrocyte glycoprotein (MOG) induces acute demyelinating experimental autoimmune encephalomyelitis in the Lewis rat. J. Immunol. 1995, 63, 17–27. [Google Scholar] [CrossRef]
- Johns, T.J.; Kerloro de Rosbo, N.; Menon, K.K.; Abo, S.; Gonzales, M.F.; Bernard, C.C. Myelin oligodendrocyte glycoprotein induces a demyelinating encephalomyelitis resembling multiple sclerosis. J. Immunol. 1995, 154, 5536–5541. [Google Scholar] [PubMed]
- Kerloro de Rosbo, N.; Honneger, P.; Lassmann, H.; Matthieu, J.-M. Demyelination induced in aggregating brain cell cultures by a monoclonal antibody against myelin/oligodendrocyte glycoprotein. J. Neurochem. 1990, 55, 583–587. [Google Scholar] [CrossRef]
- Waksman, B.H.; Adams, R.D. Allergic neuritis—An experimental disease of rabbits induced by injection of peripheral nervous tissue and adjuvants. J. Exp. Med. 1955, 102, 213–235. [Google Scholar] [CrossRef] [PubMed]
- Carlo, D.J.; Karkhanis, Y.D.; Bailey, P.J.; Wisniewski, H.M.; Brostoff, S.W. Experimental allergic neuritis: Evidence for the involvement of the P0 and P2 proteins. Brain Res. 1975, 88, 580–584. [Google Scholar] [CrossRef]
- Kadlubowski, M.; Hughes, R.A.C. Identification of the neuritogen for experimental allergic neuritis. Nature 1979, 227, 140–141. [Google Scholar] [CrossRef]
- Yonezawa, T.; Ishihara, Y.; Matsuyama, H. Studies on experimental allergic peripheral neuritis. I. Demyelinating patterns studied in vitro. J. Neuropathol. Exp. Neurol. 1968, 27, 453–463. [Google Scholar] [CrossRef]
- Raine, C.S.; Bornstein, M.B. Experimental allergic neuritis. Ultrastructure of serum-induced abberations in peripheral nervous system cultures. Lab. Investig. 1979, 40, 423–432. [Google Scholar] [PubMed]
- Saida, T.; Saida, K.; Silberberg, D.H. Demyelination produced by experimental allergic neuritis serum and anti-galactocerebroside antiserum in CNS cultures. Acta Neuropathol. 1979, 48, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Seil, F.J.; Kies, M.W.; Bacon, M.L. A comparison of demyelinating and myelination-inhibiting factor induction by whole peripheral nerve tissue and P2 protein. Brain Res. 1981, 210, 441–448. [Google Scholar] [CrossRef]
- Uyemura, K.; Kitamura, K.; Ogawa, Y.; Matsuyama, H. Studies on the antigenic protein to induce experimental allergic neuritis (EAN). In The Aetiology and Pathogenesis of the Demyelinating Diseases; Shiraki, H., Yonezawa, T., Kuroiwa, Y., Eds.; Japan Science Press: Tokyo, Japan, 1976; pp. 181–192. [Google Scholar]
- Mithen, F.; Agrawal, H.; Bunge, R.; Fishman, M.; Eylar, E. Effects of antiserum against PNS myelin proteins P1 and P2 on myelinated dorsal root ganglion (DRG) cultures. J. Neuropathol. Exp. Neurol. 1980, 39, 376. [Google Scholar] [CrossRef]
- Raine, C.S.; Traugott, U.; Farooq, M.; Bornstein, M.B.; Norton, W.T. Augmentation of immune-mediated demyelination by lipid haptens. Lab. Investig. 1981, 45, 174–182. [Google Scholar] [PubMed]
- Bourdette, D.N.; Driscoll, B.F.; Seil, F.J.; Kies, M.W.; Alvord, E.C., Jr. Severity of demyelination in vivo correlates with serum myelination inhibition activity in guinea pigs having a new form of experimental allergic encephalomyelitis. Neurochem. Pathol. 1986, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Martenson, R.E.; Deibler, G.E.; Kies, M.W.; Levine, S.; Alvord, E.C., Jr. Myelin basic proteins of mammalian and submammalian vertebrates: Encephalitogenic activities in guinea pigs and rats. J. Immunol. 1972, 109, 262–270. [Google Scholar] [PubMed]
- Linington, C.; Lassmann, H. Antibody responses in chronic relapsing experimental allergic encephalomyelitis: Correlation of serum demyelinating activity with antibody titre to the myelin/oligodendrocyte glycoprotein (MOG). J. Neuroimmunol. 1987, 17, 61–69. [Google Scholar] [CrossRef]
- Linington, C.; Bradl, M.; Lassmann, H.; Brunner, C.; Vass, K. Augmentation of demyelination in rat acute encephalomyelitis by circulating mouse monoclonal antibodies directed against a myelin/oligodendrocyte glycoprotein. Am. J. Pathol. 1988, 130, 443–454. [Google Scholar] [PubMed]
- Whitham, R.H.; Nilaver, G.; Bourdette, D.N.; Seil, F.J. Serum antimyelin antibodies in chronic relapsing experimental allergic encephalomyelitis. J. Neuroimmunol. 1988, 18, 155–170. [Google Scholar] [CrossRef]
- Smith, M.E.; Sadler, R.H.; Sommer, M.A. The macrophage as the demyelinative agent: A role for antimyelin antibodies. In Multiple Sclerosis: Current Status of Research and Treatment; Herndon, R.M., Seil, F.J., Eds.; Demos: New York, NY, USA, 1994; pp. 51–66. [Google Scholar]
- Cook, S.D.; Dowling, P.C.; Murray, M.R.; Whitaker, J.N. Circulating demyelinating factors in acute idiopathic polyneuropathy. Arch. Neurol. 1971, 24, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Dubois-Dalcq, M.; Buyse, M.; Buyse, G.; Gorce, F. The action of Guillain-Barré syndrome serum on myelin. A tissue culture and electron microscope analysis. J. Neurol. Sci. 1971, 13, 67–83. [Google Scholar] [CrossRef]
- Bornstein, M.B.; Hummelgard, A. Multiple sclerosis: Serum induced demyelination in tissue culture. In The Aetiology and Pathogenesis of the Demyelinating Diseases; Shiraki, H., Yonezawa, T., Kuroiwa, Y., Eds.; Japan Science Press: Tokyo, Japan, 1976; pp. 341–350. [Google Scholar]
- Ulrich, J.; Lardi, H. Multiple sclerosis: Demyelination and myelin inhibition of organotypic tissue cultures of spinal cord by sera of patients with multiple sclerosis and other neurological diseases. J. Neurol. 1978, 218, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Seil, F.J.; Westall, F.C.; Romine, J.S.; Salk, J. Serum demyelinating factors in multiple sclerosis. Ann. Neurol. 1983, 13, 664–667. [Google Scholar] [CrossRef] [PubMed]
- Dau, P.C.; Petajan, J.H.; Johnson, K.P.; Panitch, H.S.; Bornstein, M.B. Plasmapheresis in multiple sclerosis: Preliminary findings. Neurology 1980, 30, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, K.; Aparicio, S.R.; Sumner, D.W.; Macfie, A.; Sagar, P.; Griffin, N.R.; Bird, C.C. Comparison of in vitro demyelination and cytotoxicity of humoral factors in multiple sclerosis and other neurological diseases. J. Neurol. Sci. 1985, 70, 167–181. [Google Scholar] [CrossRef]
- Hughes, D.; Field, E.J. Myelinotoxicity of serum and spinal fluid in multiple sclerosis: A critical assessment. Clin. Exp. Immunol. 1967, 2, 295–309. [Google Scholar] [PubMed]
- Wolfgram, F.; Duquette, P. Demyelinating antibodies in multiple sclerosis. Neurology 1976, 26 Pt 2, 68–69. [Google Scholar] [CrossRef] [PubMed]
- Grundke-Iqbal, I.; Bornstein, M.B. Multiple sclerosis: Immunochemical studies on the demyelinating serum factor. Brain Res. 1979, 160, 489–503. [Google Scholar] [CrossRef]
- Grundke-Iqbal, I.; Bornstein, M.B. Multiple sclerosis: Serum gamma globulin and demyelination in organ culture. Neurology 1980, 30, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Genain, C.P.; Cannella, B.; Hauser, S.L.; Raine, C.S. Identification of autoantibodies associated with myelin damage in multiple sclerosis. Nat. Med. 1999, 5, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Raine, C.S.; Cannella, B.; Hauser, S.L.; Genain, C.P. Demyelination in primate autoimmune encephalomyelitis and acute multiple sclerosis: A case for antigen-specific antibody mediation. Ann. Neurol. 1999, 46, 144–160. [Google Scholar] [CrossRef]
- Storch, M.; Lassmann, H. Pathology and pathogenesis of demyelinating diseases. Curr. Opin. Neurol. 1997, 10, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Luchinetti, C.F.; Brück, W.; Rodriguez, M.; Lassmann, H. Distinct patterns of multiple sclerosis pathology indicates heterogeneity in pathogenesis. Brain Pathol. 1996, 6, 259–274. [Google Scholar] [CrossRef]
- Luchinetti, C.F.; Brück, W.; Parisi, J.; Scheithauer, B.; Rodriguez, M.; Lassmann, H. Heterogeneity of multiple sclerosis lesions: Implications for the pathogenesis of demyelination. Ann. Neurol. 2000, 47, 707–717. [Google Scholar] [CrossRef]
- Archelos, J.J.; Storch, M.K.; Hartnung, H.-P. The role of B cells and autoantibodies in multiple sclerosis. Ann. Neurol. 2000, 47, 465–471. [Google Scholar] [CrossRef]
- Seil, F.J. Demyelinating antibodies in multiple sclerosis. Ann. Neurol. 2000, 48, 948. [Google Scholar] [CrossRef]
- Elliott, C.; Lindner, M.; Arthur, A.; Brennan, K.; Jarius, S.; Hussey, J.; Chan, A.; Stroet, A.; Olsson, T.; Willison, H.; et al. Functional identification of pathogenic autoantibody responses in patients with multiple sclerosis. Brain 2012, 135, 1819–1833. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K.A.; Chitnis, T.; Newcombe, J.; Franz, B.; Kennedy, J.; McArdel, S.; Kuhle, J.; Kappos, L.; Rostasy, K.; Pohl, D.; et al. Age-dependent B cell autoimmunity to a myelin surface antigen in pediatric multiple sclerosis. J. Immunol. 2009, 183, 4067–4076. [Google Scholar] [CrossRef] [PubMed]
- Probstatel, A.-K.; Dornmair, K.; Bittner, R.; Sperl, P.; Jenne, D.; Magalhaes, S.; Villalobos, A.; Breithaupt, C.; Weissert, R.; Jacob, U.; et al. Antibodies to MOG are transient in childhood acute disseminated encephalomyelitis. Neurology 2011, 77, 580–588. [Google Scholar] [CrossRef] [PubMed]
- Kitley, J.; Woodhall, M.; Waters, P.J.; Leite, M.I.; Devenney, E.; Craig, J.; Palace, J.; Vincent, A. Myelin oligodendrocyte glycoprotein antibodies in adults with a neuromyelitis optica phenotype. Neurology 2012, 79, 1273–1277. [Google Scholar] [CrossRef] [PubMed]
- Lennon, V.A.; Wingerchuck, D.M.; Kryzer, T.J.; Pittock, S.J.; Lucchinetti, C.F.; Fujihara, K.; Nakashima, I.; Weinshenker, B.G. A serum autoantibody marker of neuromyelitis optica: Distinction from multiple sclerosis. Lancet 2004, 364, 2106–2112. [Google Scholar] [CrossRef]
| Antigens | EAE/EAN | Antibodies | |||
|---|---|---|---|---|---|
| Demyelinating | Myelination Inhibiting | ||||
| CNS | PNS | CNS | PNS | ||
| CNS Antigens | |||||
| Whole CNS | + | + | - | + | - |
| MBP | + | - | - | - | ND |
| GC | - | + | + | + | + |
| M2 | ND | + | ND | ND | ND |
| MAG | - | - | - | - | ND |
| PLP | + | - | - | - | ND |
| GM1 | ± a | - | - | - | - |
| CMIP | ± b | + | - | + | ND |
| MOG | + | + | ND | ND | ND |
| PNS Antigens | |||||
| Whole PNS | + | ± | + | + | + |
| P2 protein | ± | - | - | - | - |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seil, F.J. Myelin Antigens and Antimyelin Antibodies. Antibodies 2018, 7, 2. https://doi.org/10.3390/antib7010002
Seil FJ. Myelin Antigens and Antimyelin Antibodies. Antibodies. 2018; 7(1):2. https://doi.org/10.3390/antib7010002
Chicago/Turabian StyleSeil, Fredrick J. 2018. "Myelin Antigens and Antimyelin Antibodies" Antibodies 7, no. 1: 2. https://doi.org/10.3390/antib7010002
APA StyleSeil, F. J. (2018). Myelin Antigens and Antimyelin Antibodies. Antibodies, 7(1), 2. https://doi.org/10.3390/antib7010002




