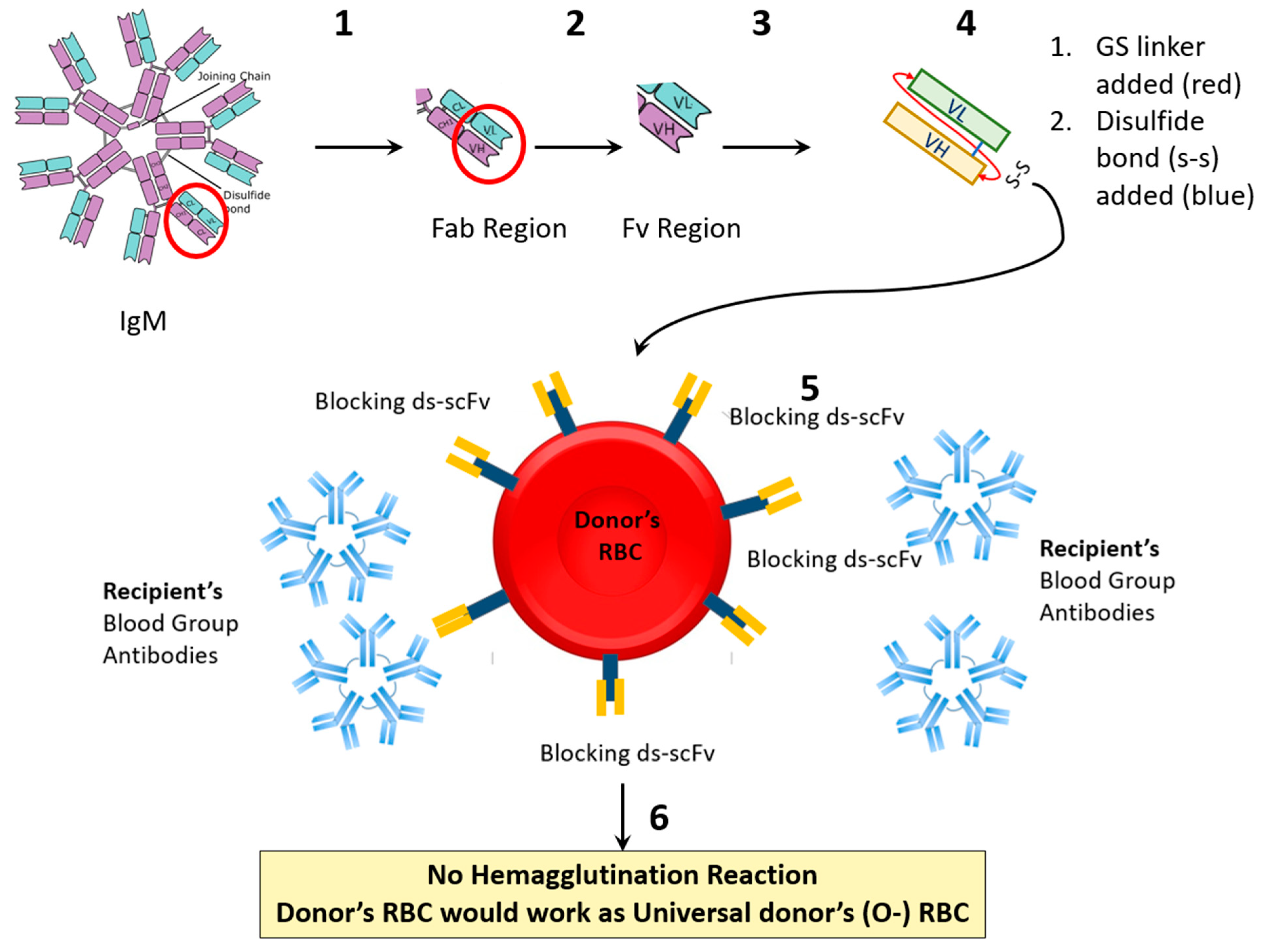
Prevention of Blood Incompatibility Related Hemagglutination: Blocking of Antigen A on Red Blood Cells Using In Silico Designed Recombinant Anti-A scFv
Highlights
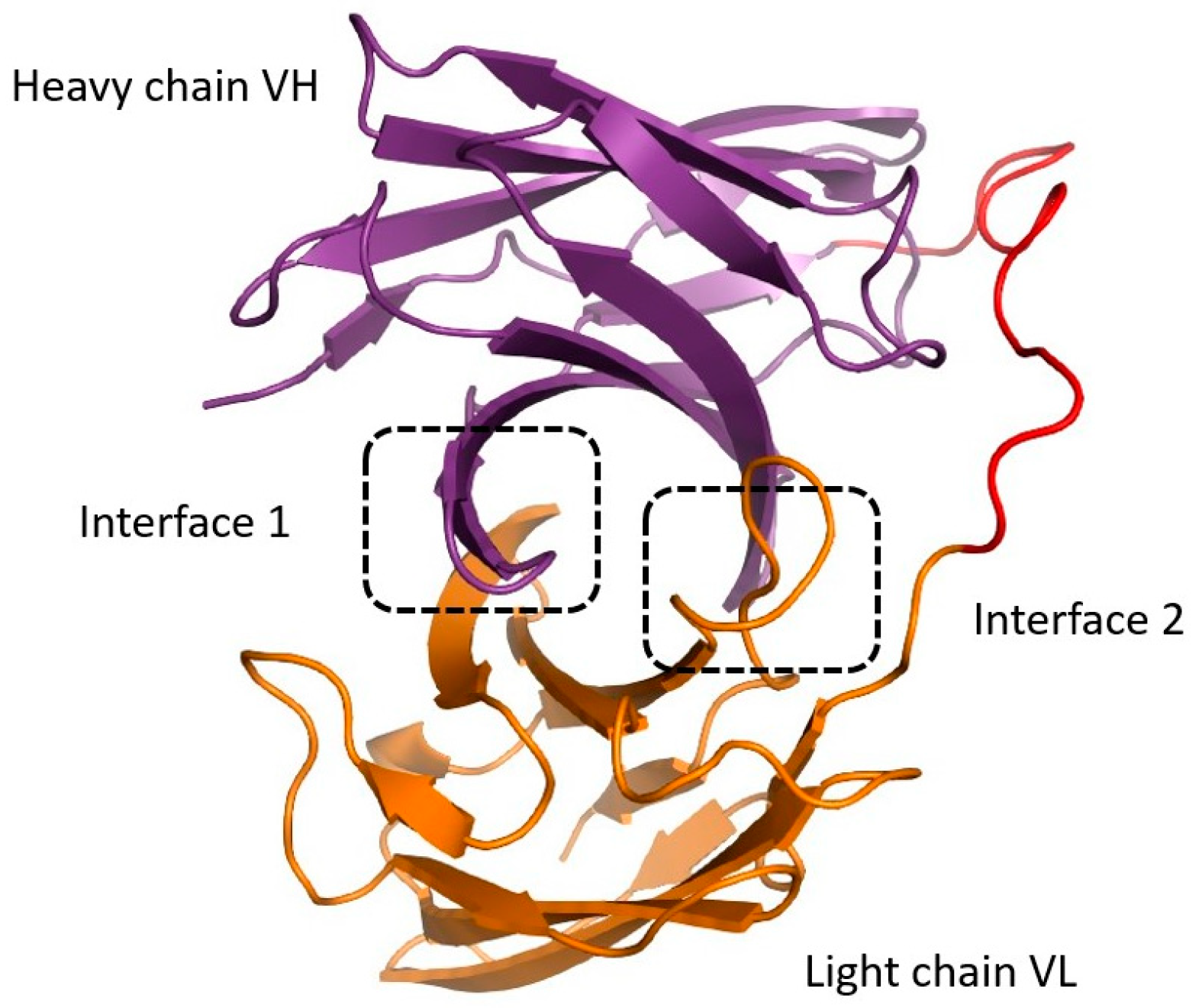
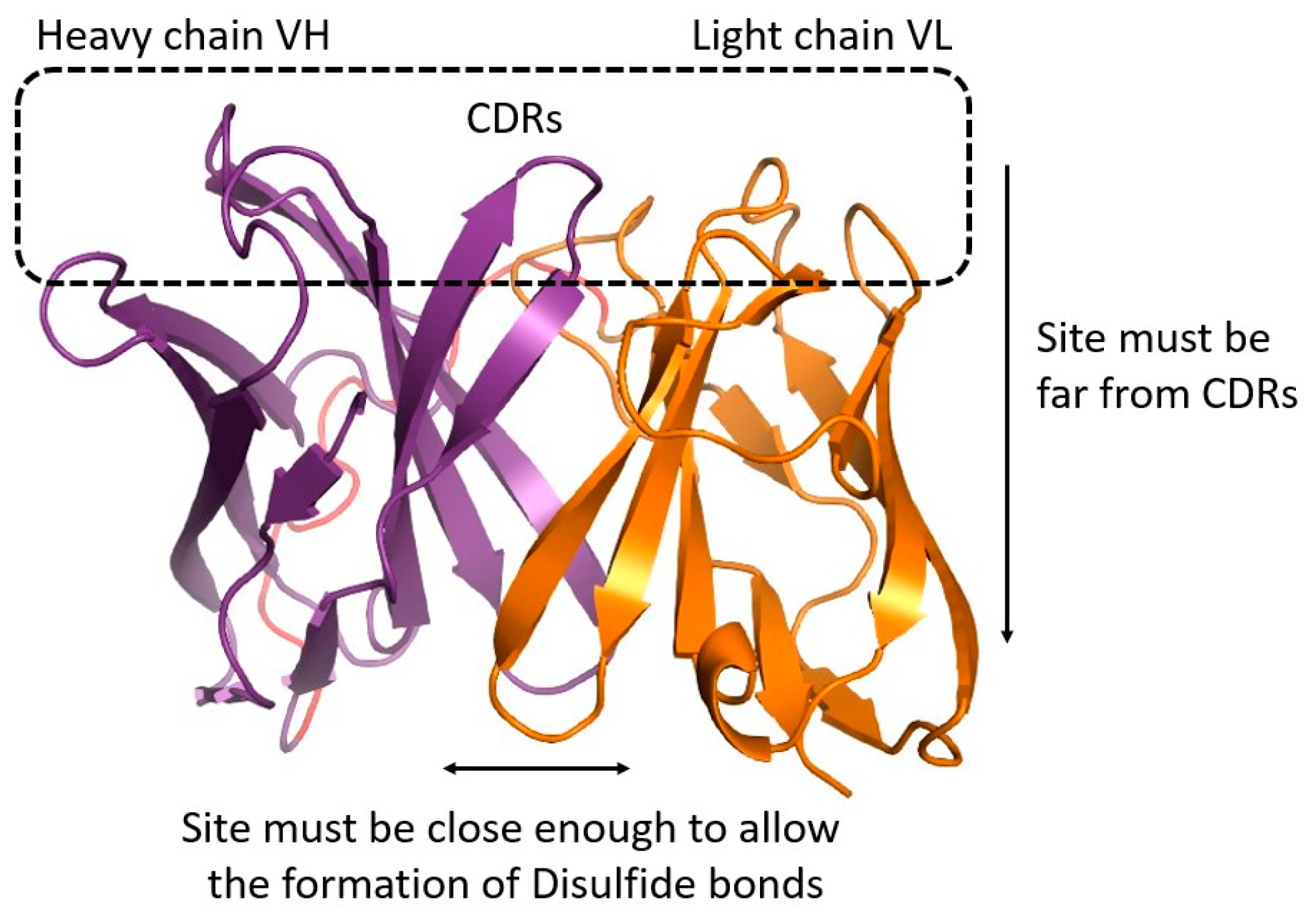
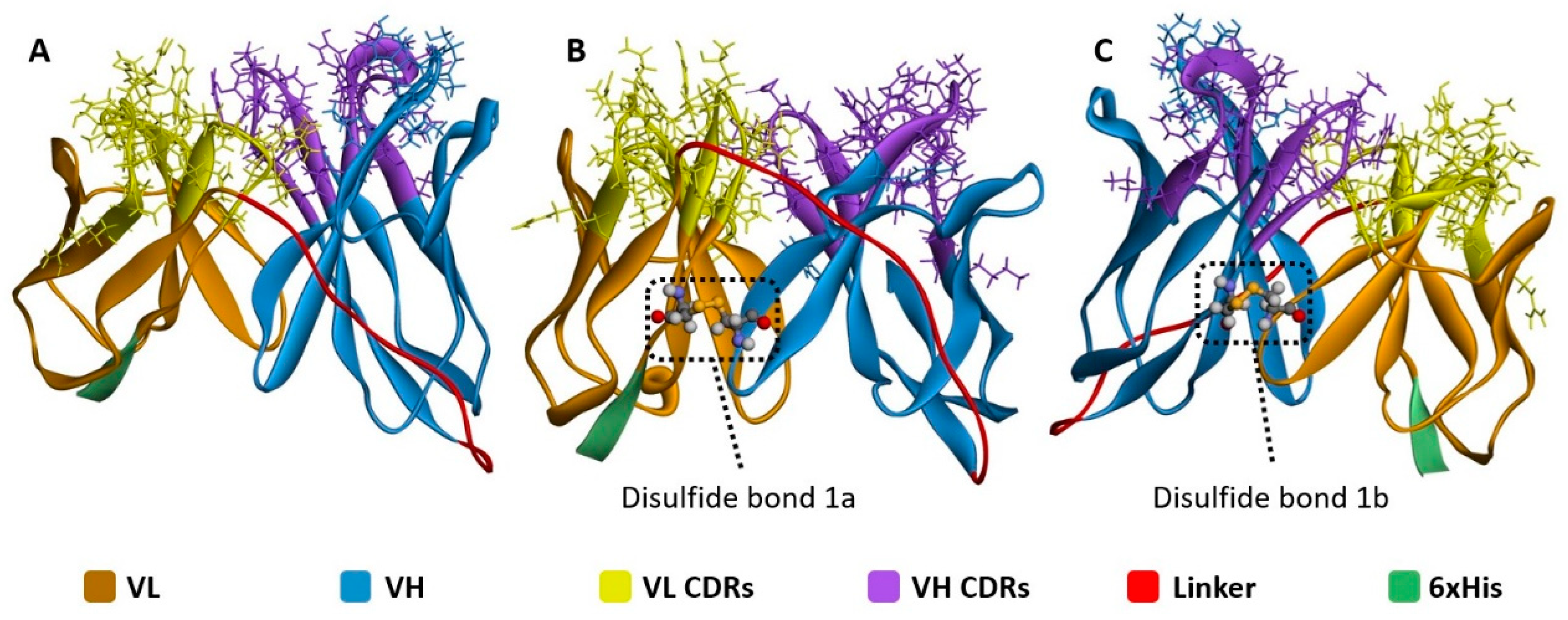
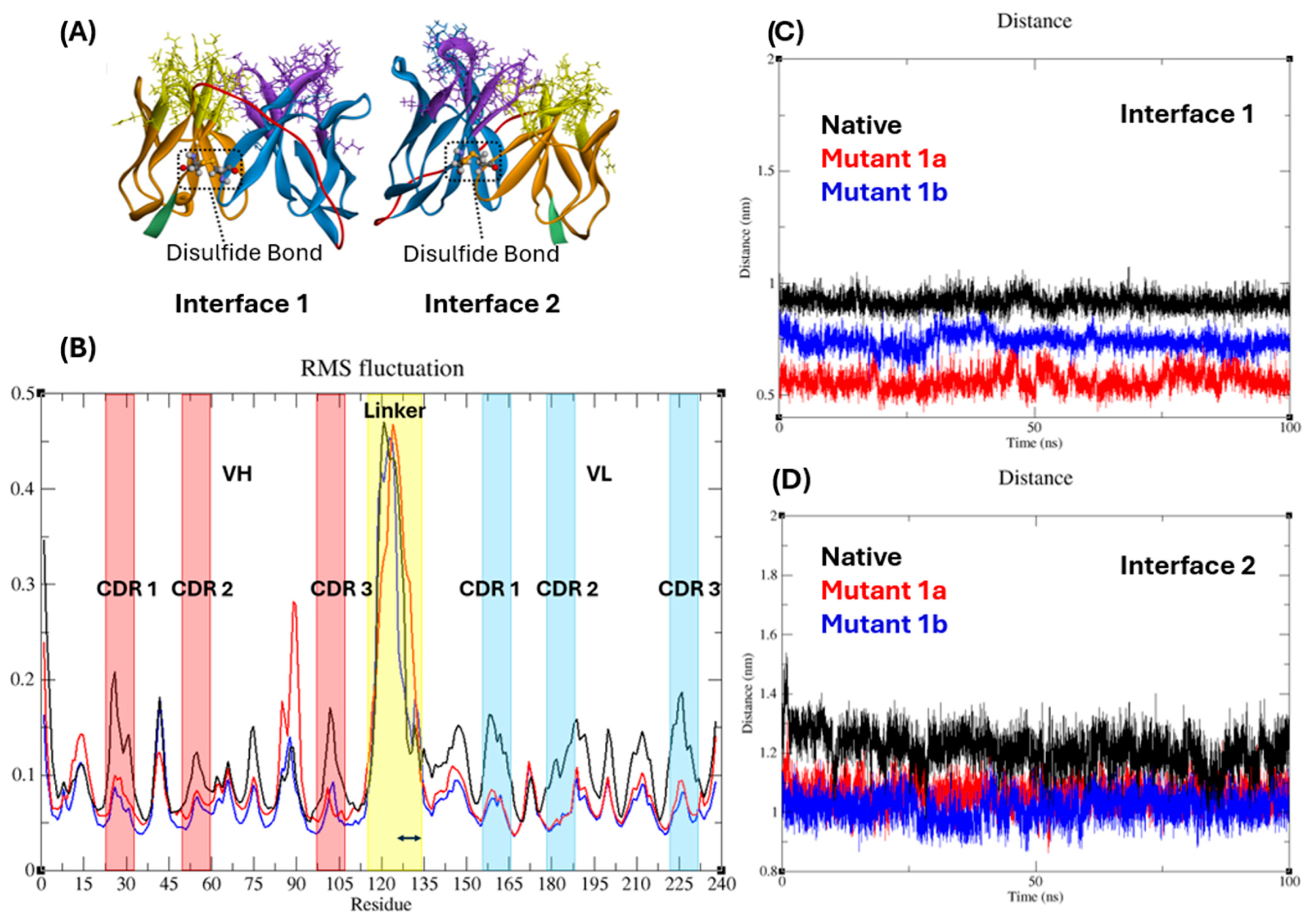
- The location of the interdomain disulfide bond affects the positioning of CDR amino acids.
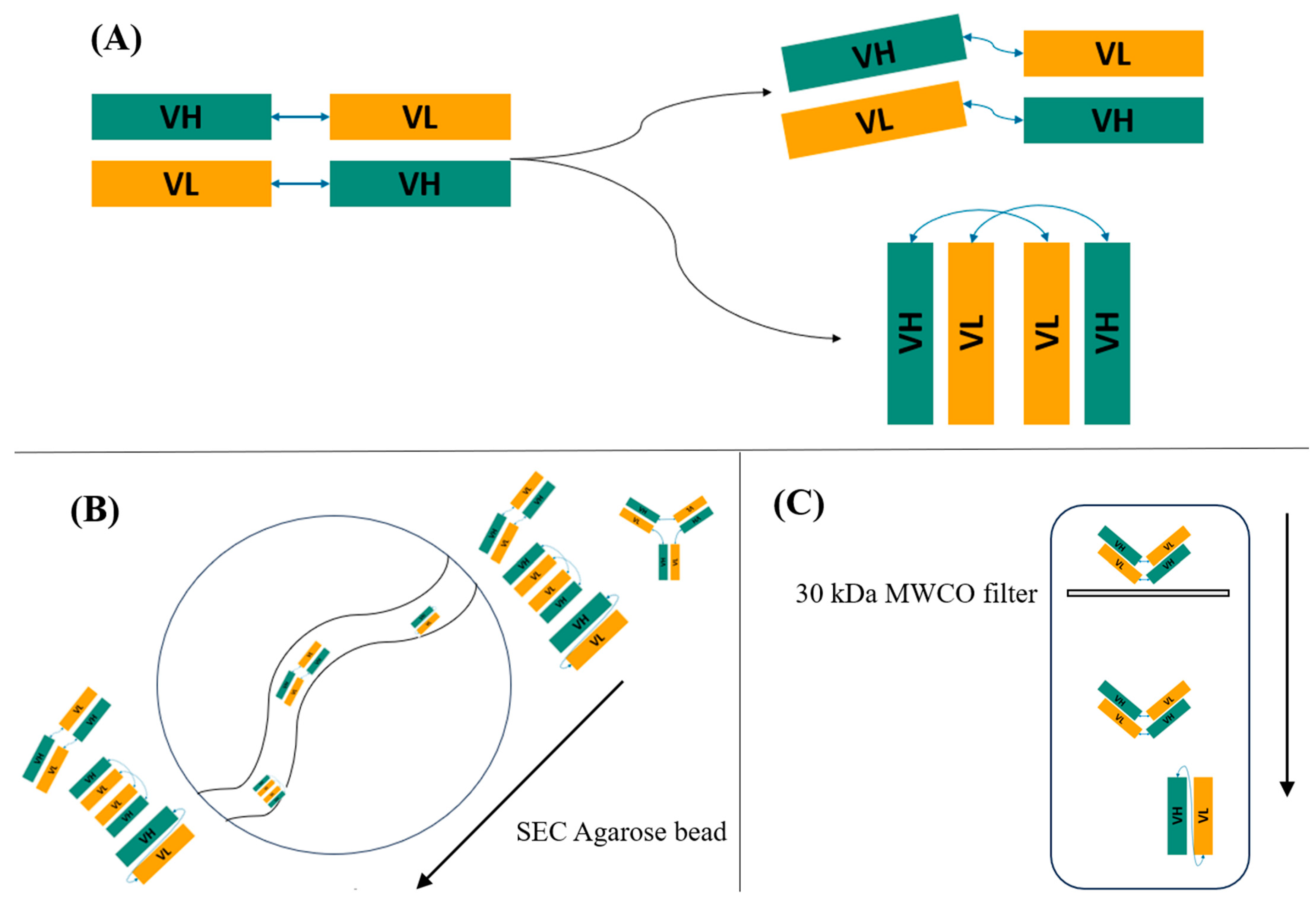
- Multimers of scFv are observed when repetitive linkers are used.
- Domain-swapping in opposite orientation leads to non-functional dimers.
- Antigen-blocked RBCs can be given to other incompatible blood groups.
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Modelling and Molecular Dynamics Simulations of Anti-A scFvs
2.3. Molecular Docking and Molecular Dynamics Simulations
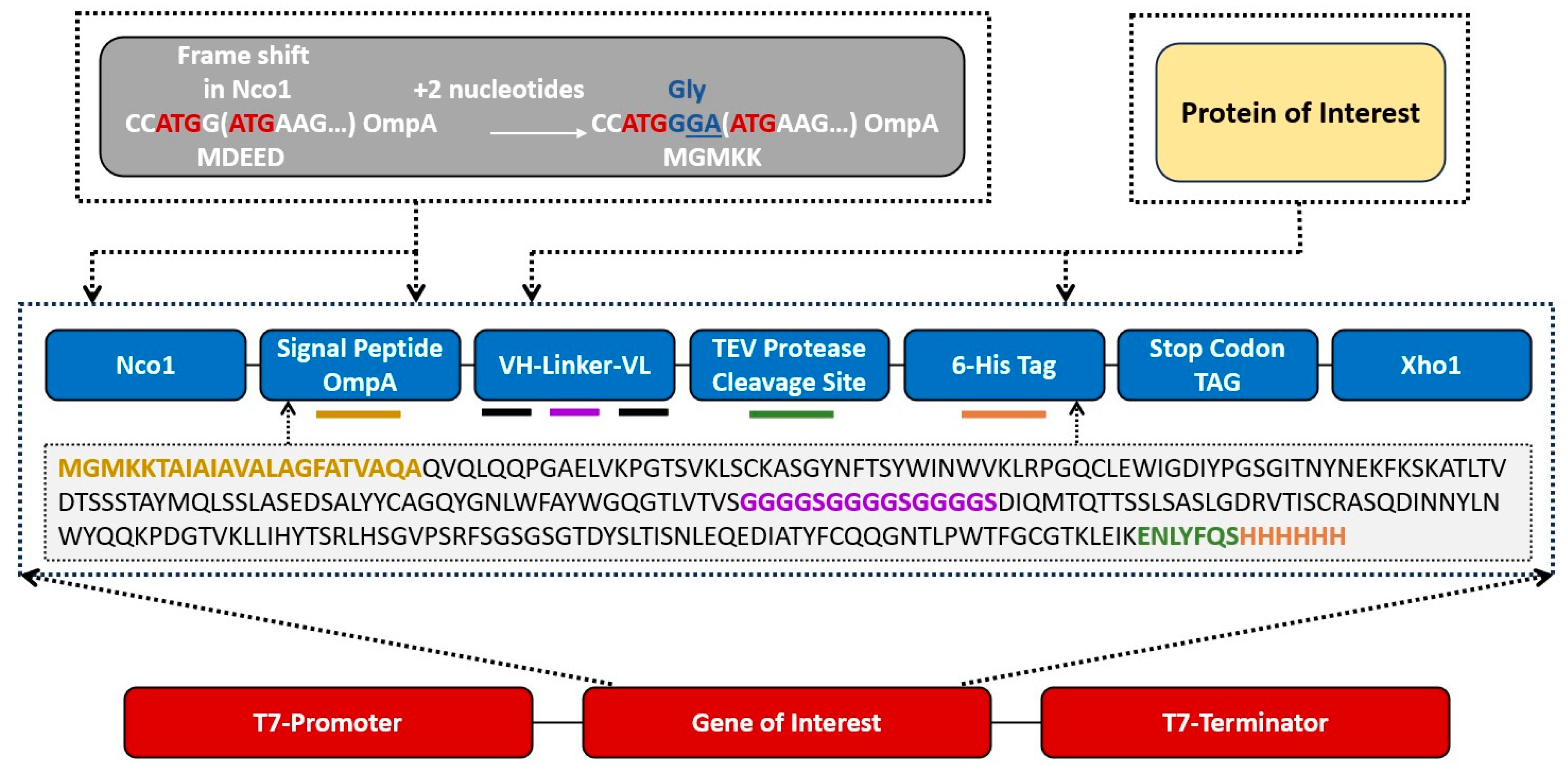
2.4. Designing and Transformation of Recombinant scFv-plasmid pET-28a (+)
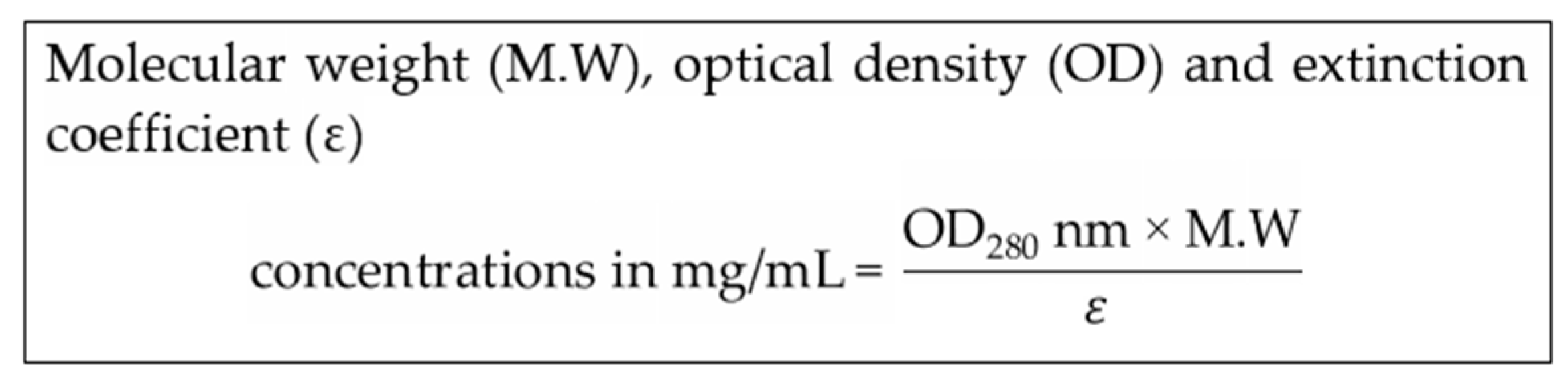
2.5. Expression and Purification of Recombinant Anti-A scFv
2.6. Blocking of Antigen-A on RBCs of Blood Groups A+ and AB+ with Recombinant Anti-A scFv
2.7. Detection of the Presence of Recombinant Anti-A scFv on RBCs and in Supernatant
2.8. Purification of Functional Anti-A scFvs and Determination of Dissociation Constant KD
Direct Ligand-Receptor Interaction Assay (LRA)
3. Results
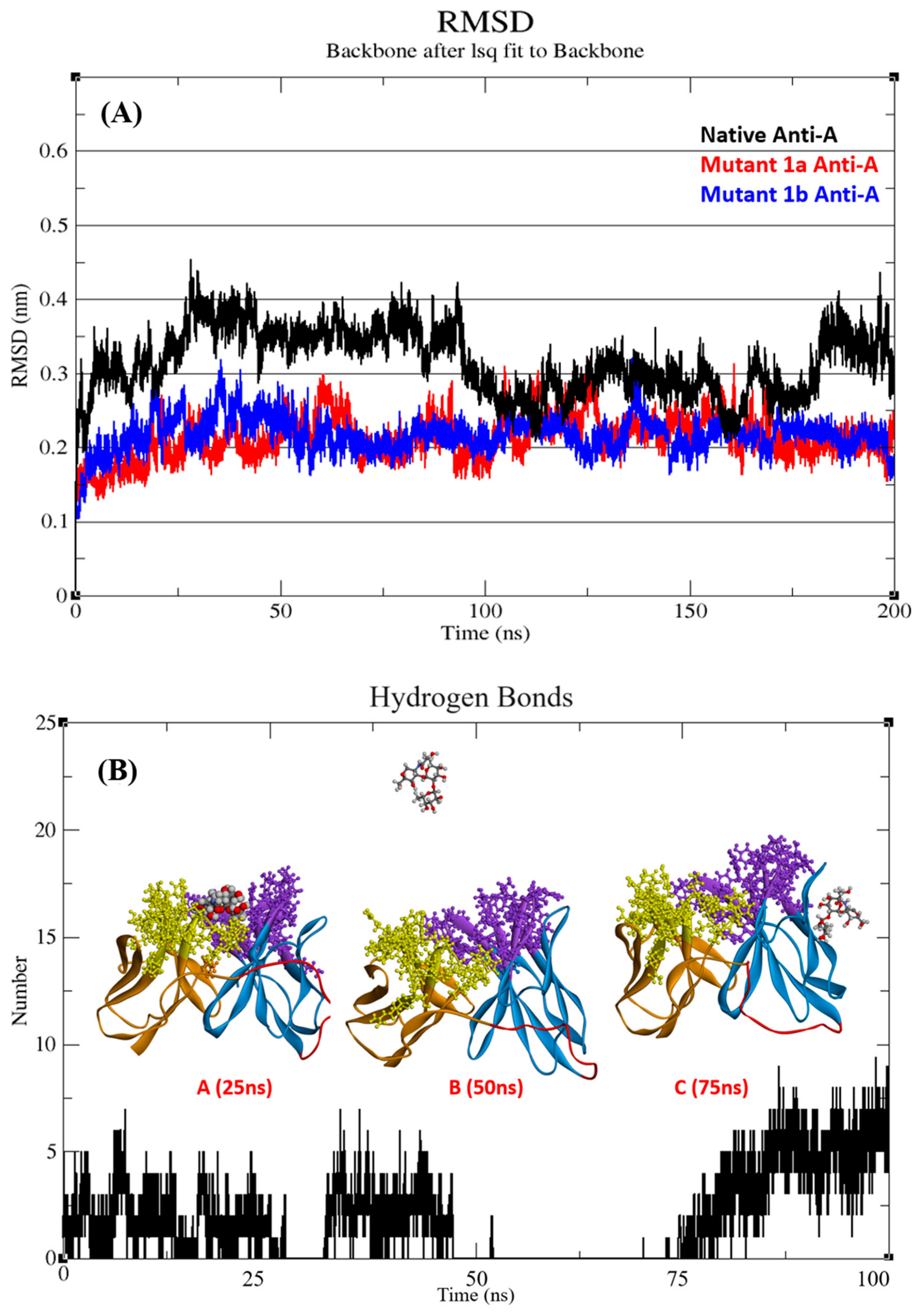
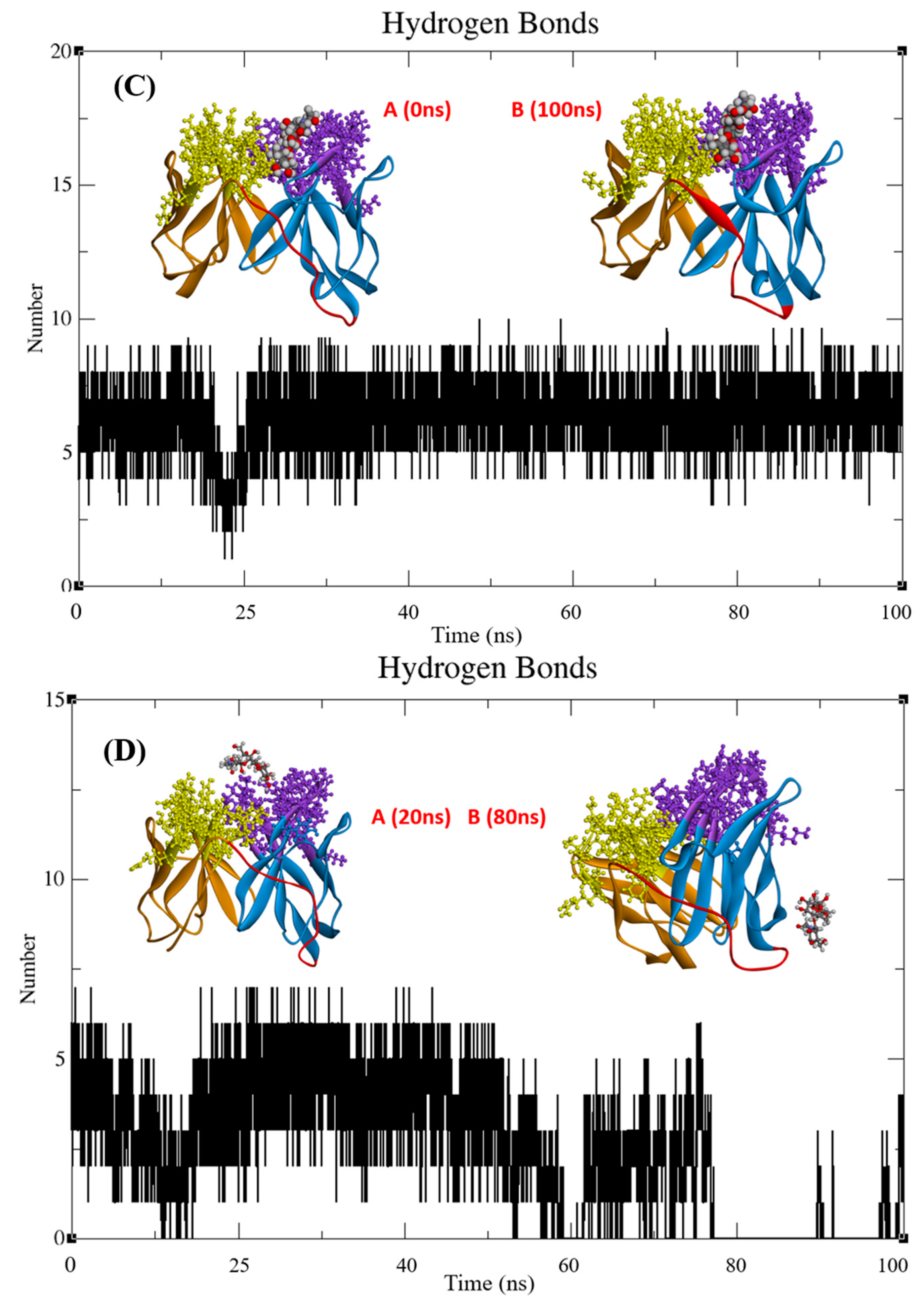
3.1. Structure Stability Analysis of scFvs
3.2. Functional Analysis of scFvs
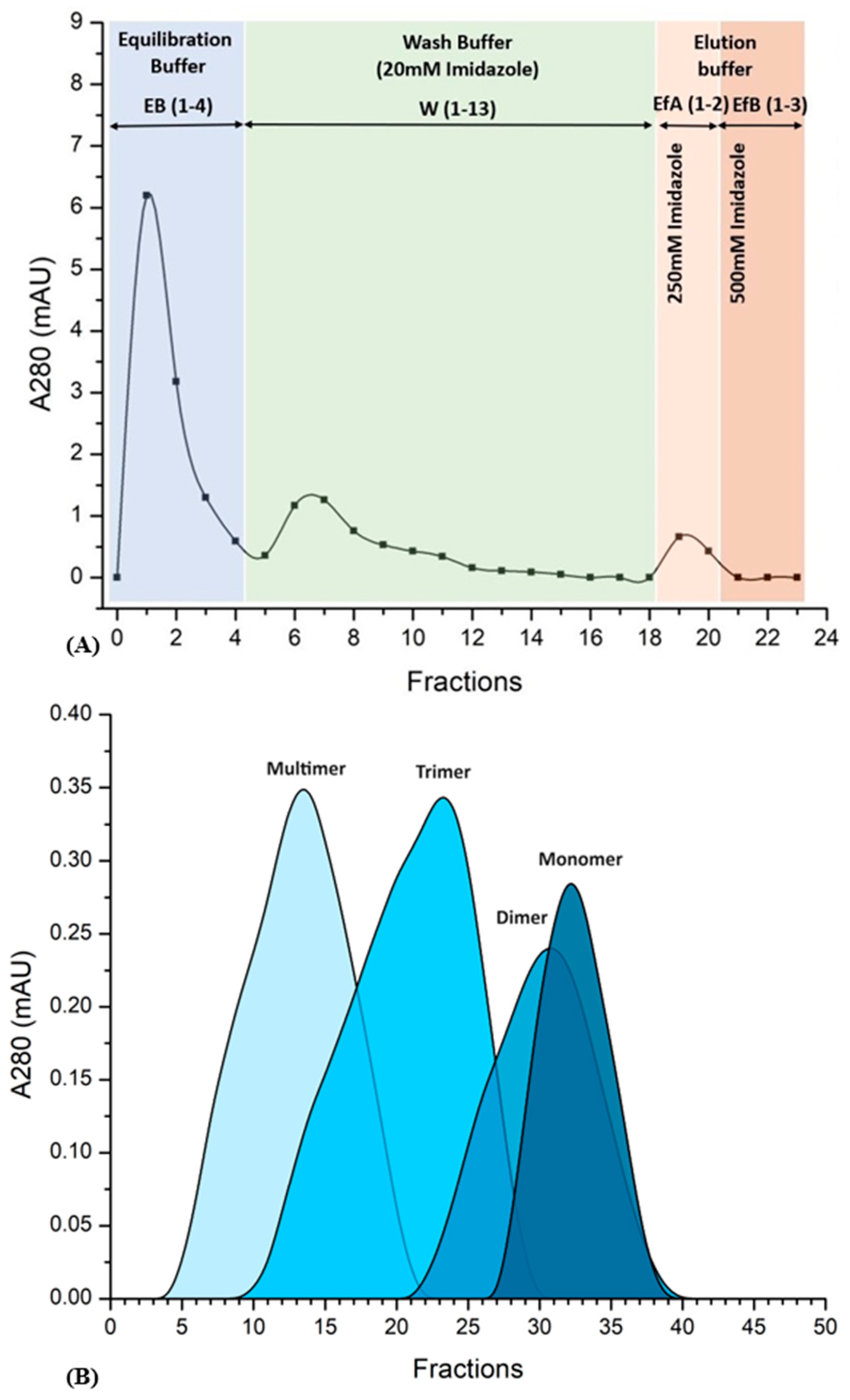
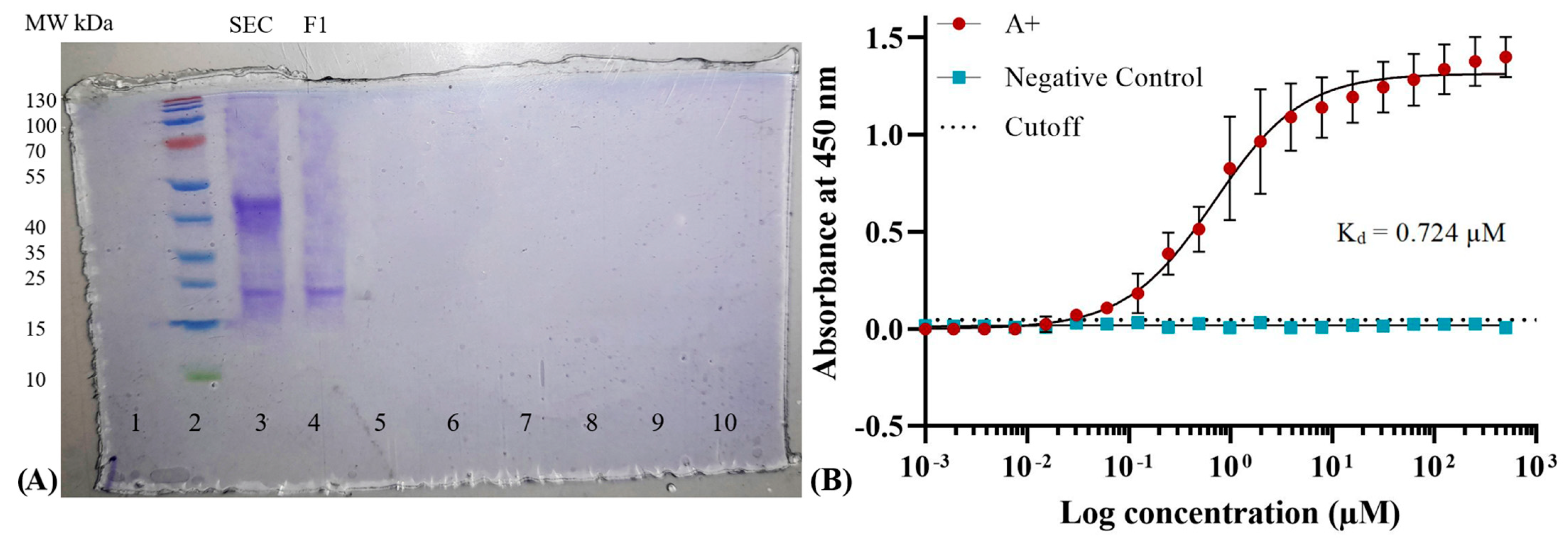
3.3. Expression and Purification of Mutant-1a scFv
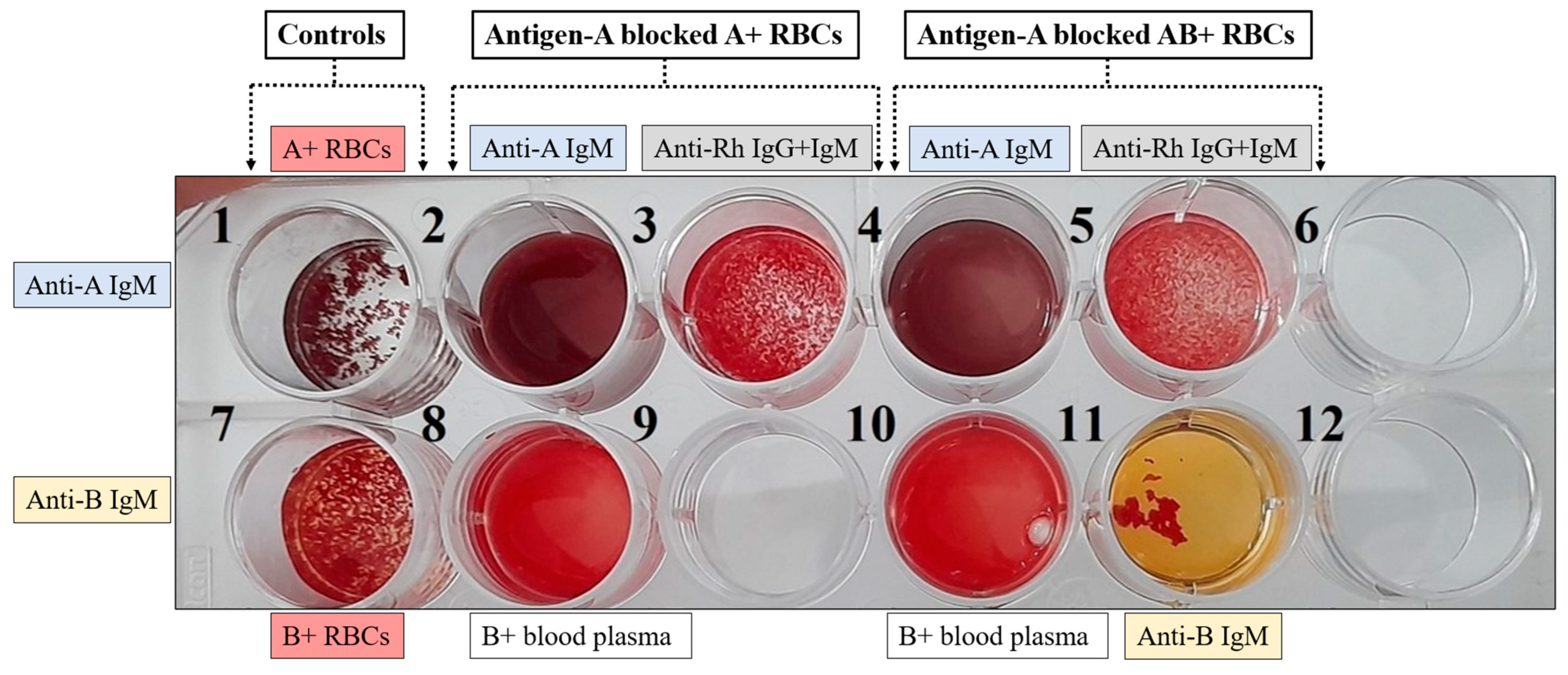
3.4. Blocking of Antigen-A on RBCs of Blood Groups A+ and AB+ with Recombinant anti-A scFv
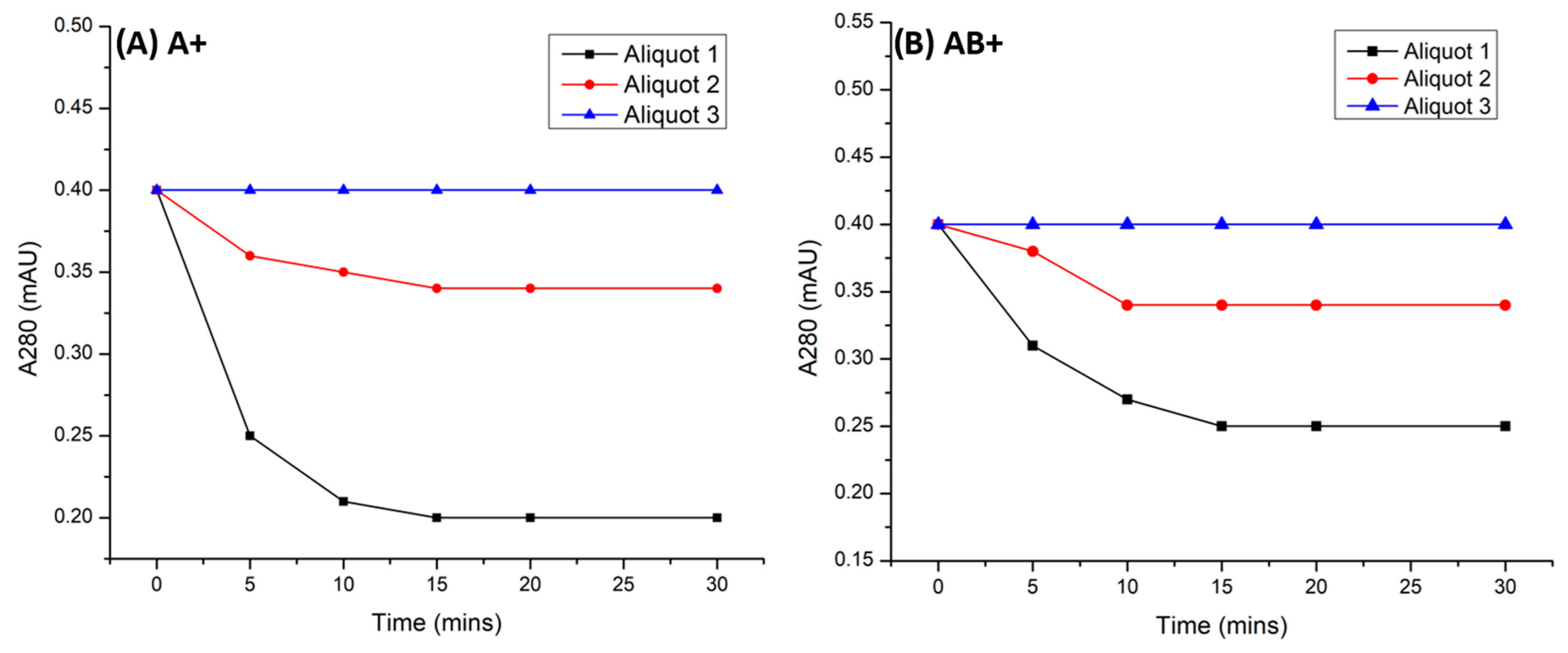
3.5. Detection of the Presence of Recombinant Anti-A scFv on RBCs and in Supernatant
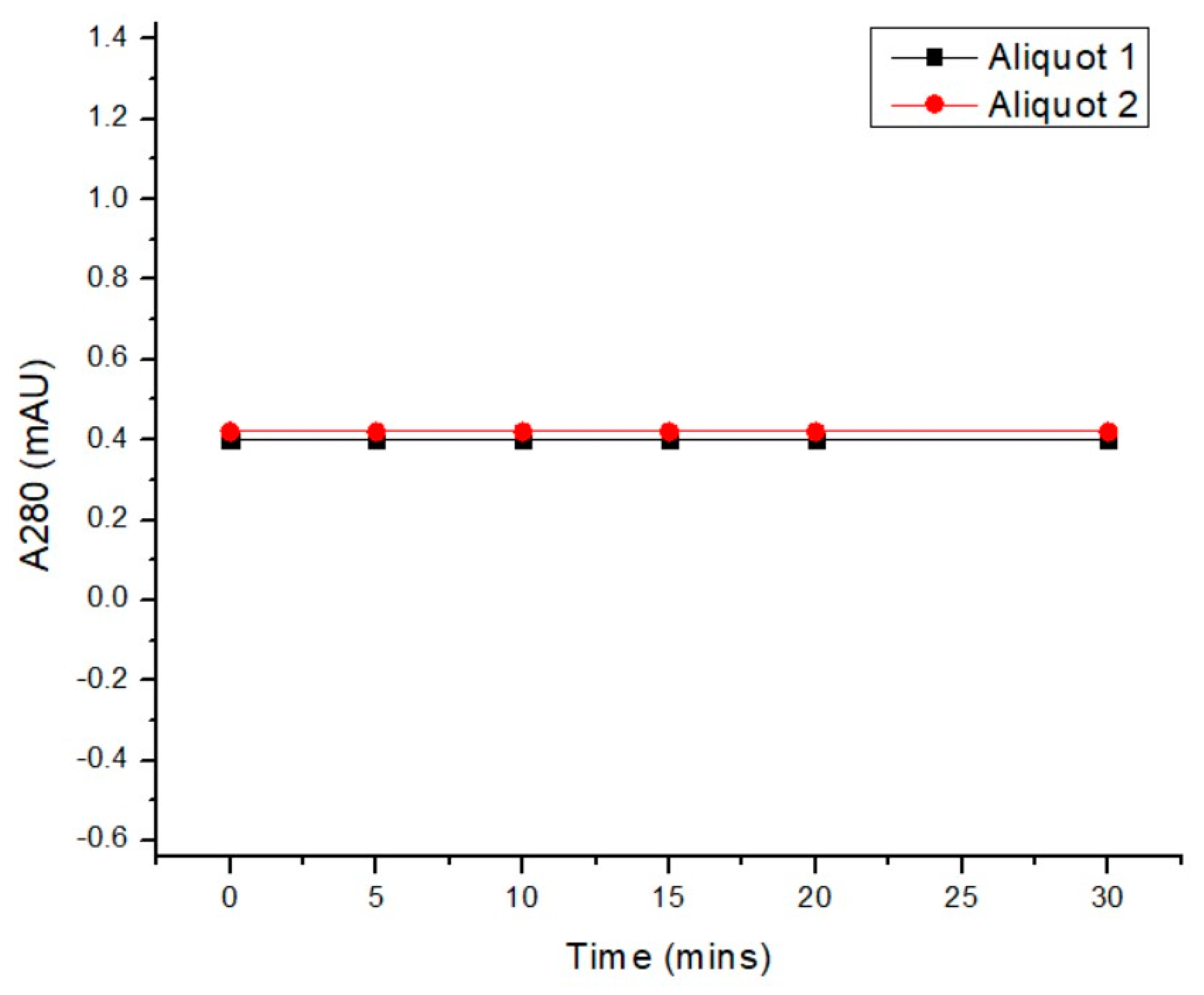
3.6. Purification of Functional Anti-A scFvs and Determination of Dissociation Constant KD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Single Chain Fragment Variable | Pose | Location | Interacting Residues | Interacting Saccharide | Binding Energies (kcal/mol) |
|---|---|---|---|---|---|
| Native Anti-A | 4 | CDR | VH CDR 1: TRP-33, ASN-35 VH CDR 2: ASP-50 VH CDR 3: ASN-102, PHE-105 | Fuc, Gal, GalNAc | −5.7 |
| VL CDR 1: TYR-164, ASN-166 VL CDR 2: HIS-181 VL CDR 3: TRP-228, PRO-227, LEU-226 | |||||
| Mutant-1a Anti-A | 1 | CDR | VH CDR 1: TRP-33, TRP-36 VH CDR 2: ASP-50, Glu-62, ASN-61 VH CDR 3: GLN-99, ASN-102, LEU-103 | Fuc, Gal, GalNAc | −7.4 |
| VL CDR 1: TYR-164 VL CDR 2: HIS-181 VL CDR 3: TRP-228, PRO-227 | |||||
| Mutant-1b Anti-A | 7 | CDR | VH CDR 1: TRP-33 VH CDR 2: ASP-50, ASN-59, TYR-60 VH CDR 3: GLN-99, ASN-102, LEU-103, PHE-105 | Fuc, Gal, GalNAc | −5.3 |
| VL CDR 1: ASN-162, TYR-164 VL CDR 2: HIS-181 VL CDR 3: GLY-223, TRP-228 |

References
- Global Status Report on Blood Safety and Availability. 2017. Available online: https://apps.who.int/iris/handle/10665/254987 (accessed on 13 March 2023).
- Barnes, L.S.; Stanley, J.; Bloch, E.M.; Pagano, M.B.; Ipe, T.S.; Eichbaum, Q.; Wendel, S.; Indrikovs, A.; Cai, W.; Delaney, M. Status of hospital-based blood transfusion services in low-income and middle-income countries: A cross-sectional international survey. BMJ Open 2022, 12, e055017. [Google Scholar] [CrossRef] [PubMed]
- Arshad Ali, S.; Azim, D.; Hassan, H.; Iqbal, A.; Ahmed, N.; Kumar, S.; Nasim, S. The impact of COVID-19 on transfusion-dependent thalassemia patients of Karachi, Pakistan: A single-center experience. Transfus. Clin. Biol. 2021, 28, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Barnes, L.S.; Al-Riyami, A.Z.; Ipe, T.S.; Bloch, E.M.; Sibinga, C.S.; Eichbaum, Q.G. COVID-19 and the impact on blood availability and transfusion practices in low- and middle-income countries. Transfusion 2022, 62, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Lal, A.; Wong, T.; Keel, S.; Pagano, M.; Chung, J.; Kamdar, A.; Rao, L.; Ikeda, A.; Puthenveetil, G.; Shah, S.; et al. The transfusion management of beta thalassemia in the United States. Transfusion 2021, 61, 3027–3039. [Google Scholar] [CrossRef]
- Nordmeyer, D.; Forestner, J.E.; Wall, M.H. Advances in transfusion medicine. Adv. Anesth. 2007, 25, 41–58. [Google Scholar] [CrossRef]
- Pham, H.P.; Shaz, B.H. Update on massive transfusion. Br. J. Anaesth. 2013, 111, 7182. [Google Scholar] [CrossRef] [PubMed]
- Rahfeld, P.; Withers, S.G. Toward universal donor blood: Enzymatic conversion of A and B to O type. J. Biol. Chem. 2020, 295, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Luyten, U.; Peeraer, S.; Pirlet, C.; Khaouch, Y.; Streel, C.; Deneys, V. O-negative blood shortage management in a University Hospital: Impact of transfusing RHD-positive red blood cells to RHD-negative patients. Transfus. Clin. Biol. 2023, 30, 402–409. [Google Scholar] [CrossRef]
- Hafeez, S.; Zaidi, N.S.S. Red blood cell substitutes: Liposome encapsulated hemoglobin and magnetite nanoparticle conjugates as oxygen carriers. Int. J. Mol. Sci. 2023, 24, 1618. [Google Scholar] [CrossRef]
- Olsson, M.L.; Hill, C.A.; de la Vega, H.; Liu, Q.P.; Stroud, M.R.; Valdinocci, J. Universal red blood cells enzymatic conversion of blood group A and B antigens. Transfus. Clin. Biol. 2004, 11, 33–39. [Google Scholar] [CrossRef]
- Mohammadi, M.; Nejatollahi, F.; Bemani, P. Production of scFvs as anti-ABO antibodies antagonist for prevention of hemolytic transfusion reactions resulting ABO blood groups incompatibility between donor and recipient. Hypothesis 2016, 14, 1–6. [Google Scholar] [CrossRef]
- Thomas, R.; Patenaude, S.I.; MacKenzie, C.R.; To, R.; Hirama, T.; Young, N.M.; Evans, S.V. Structure of an anti-blood group A FV and improvement of its binding affinity without loss of specificity. J. Biol. Chem. 2002, 277, 2059–2064. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Yang, L.; Gu, Z.; Chen, H.; Tian, F.; Chen, Y.; Zhang, H.; Chen, W. Stabilization of the single-chain fragment variable by an interdomain disulfide bond and its effect on antibody affinity. Int. J. Mol. Sci. 2010, 12, 1–11. [Google Scholar] [CrossRef]
- Yang, J.; Yan, R.; Roy, A.; Xu, D.; Poisson, J.; Zhang, Y. The I-TASSER suite: Protein structure and function prediction. Nat. Methods 2015, 12, 7–8. [Google Scholar] [CrossRef]
- Martínez-Rosell, G.; Giorgino, T.; De Fabritiis, G. Playmolecule ProteinPrepare: A web application for protein preparation for molecular dynamics simulations. J. Chem. Inf. Model. 2017, 57, 1511–1516. [Google Scholar] [CrossRef]
- Abraham, M.J.; Murtola, T.; Schulz, R.; Páll, S.; Smith, J.C.; Hess, B.; Lindahl, E. Gromacs: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX 2015, 1, 19–25. [Google Scholar] [CrossRef]
- Woods Group. GLYCAM Web. Complex Carbohydrate Research Center, University of Georgia, Athens, GA. 2005–2023. Available online: http://glycam.org (accessed on 21 February 2023).
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. Autodock4 and AutoDockTools4: Automated docking with selective receptor flexiblity. J. Comput. Chem. 2009, 16, 2785–2791. [Google Scholar] [CrossRef] [PubMed]
- Case, D.A.; Cheatham, T.E.; Darden, T.; Gohlke, H.; Luo, R.; Merz, K.M.; Onufriev, A.; Simmerling, C.; Wang, B.; Woods, R.J. The Amber Biomolecular Simulation Programs. J. Comput. Chem. 2005, 26, 1668–1688. [Google Scholar] [CrossRef] [PubMed]
- BIOVIA, Version 21.1.0; Dassault Systèmes, Discovery Studio Visualizer; Dassault Systèmes: San Diego, CA, USA, 2021; Available online: https://www.3ds.com/ (accessed on 26 July 2023).
- Pope, B.; Kent, H.M. High efficiency 5 min transformation of Escherichia coli. Nucleic Acids Res. 1996, 24, 536–537. [Google Scholar] [CrossRef][Green Version]
- Laemmli, U.K. Cleavage of structural proteins during the Assembly of the head of bacteriophage T4. Nature 1970, 227, 680–685. [Google Scholar] [CrossRef]
- Syedbasha, M.; Linnik, J.; Santer, D.; O’Shea, D.; Barakat, K.; Joyce, M.; Khanna, N.; Tyrrell, D.L.; Houghton, M.; Egli, A. An ELISA based binding and competition method to rapidly determine ligand-receptor interactions. JoVE 2016, 109, e53575. [Google Scholar]
- Koganei, A.; Tsuchiya, T.; Samura, K.; Nishikibe, M. Use of whole sheep red blood cells in Elisa to assess immunosuppressionin vivo. J. Immunotoxicol. 2007, 4, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Nonlinear Regression Curve Fitting was Performed Using GraphPad Prism Version 9.5.1; GraphPad Software: San Diego, CA, USA, 2023; Available online: https://www.graphpad.com/ (accessed on 18 June 2024).
- de Marco, A. Strategies for successful recombinant expression of disulfide bond-dependent proteins in Escherichia coli. Microb. Cell Factories 2009, 8, 26. [Google Scholar] [CrossRef]
- Shen, Z.; Yan, H.; Zhang, Y.; Mernaugh, R.L.; Zeng, X. Engineering peptide linkers for scFv immunosensors. Anal. Chem. 2008, 80, 1910–1917. [Google Scholar] [CrossRef] [PubMed]
- Arslan, M.; Karadag, M.; Onal, E.; Gelinci, E.; Cakan-Akdogan, G.; Kalyoncu, S. Effect of non-repetitive linker on in vitro and in vivo properties of an anti-VEGF scfv. Sci. Rep. 2022, 12, 5449. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Mesh Browser. U.S. National Library of Medicine. 2005. Available online: https://meshb.nlm.nih.gov/record/ui?name=Blocking+Antibodies (accessed on 20 July 2022).
- Weatherill, E.E.; Cain, K.L.; Heywood, S.P.; Compson, J.E.; Heads, J.T.; Adams, R.; Humphreys, D.P. Towards a universal disulphide stabilised single chain FV format: Importance of interchain disulphide bond location and VL-VH orientation. PEDS 2012, 25, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Dean, L. Blood Groups and Red Cell Antigens; NCBI: Bethesda, MD, USA, 2005. Available online: https://www.ncbi.nlm.nih.gov/books/NBK2261/ (accessed on 13 October 2023).
- Arndt, K.M.; Müller, K.M.; Plückthun, A. Factors influencing the dimer to monomer transition of an antibody single-chain FV fragment. Biochemistry 1998, 37, 12918–12926. [Google Scholar] [CrossRef]
- Dolezal, O.; Pearce, L.A.; Lawrence, L.J.; McCoy, A.J.; Hudson, P.J.; Kortt, A.A. ScFv multimers of the anti-neuraminidase antibody NC10: Shortening of the linker in single-chain FV fragment assembled in VL to VH orientation drives the formation of dimers, trimers, tetramers and higher molecular mass multimers. Protein Eng. Des. Sel. 2000, 13, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Kipriyanov, S.M.; Moldenhauer, G.; Braunagel, M.; Reusch, U.; Cochlovius, B.; Le Gall, F.; Kouprianova, O.A.; Von der Lieth, C.-W.; Little, M. Effect of domain order on the activity of bacterially produced bispecific single-chain FV antibodies. J. Mol. Biol. 2003, 330, 99–111. [Google Scholar] [CrossRef]
- Kastritis, P.L.; Bonvin, A.M. On the binding affinity of macromolecular interactions: Daring to ask why proteins interact. J. R. Soc. Interface 2013, 10, 20120835. [Google Scholar] [CrossRef]
- Chen, H.T.; Kabat, E.A.; Lundblad, A.; Ratcliffe, R.M. Nucleotide and translated amino acid sequences of cDNA coding for the variable regions of the light and heavy chains of mouse hybridoma antibodies to blood group A and B substances. J. Biol. Chem. 1987, 262, 13579–13583. [Google Scholar] [CrossRef] [PubMed]
- Muthana, S.M.; Xia, L.; Campbell, C.T.; Zhang, Y.; Gildersleeve, J.C. Competition between serum IgG, IgM, and IgA Anti-Glycan antibodies. PLoS ONE 2015, 10, e0119298. [Google Scholar] [CrossRef] [PubMed]
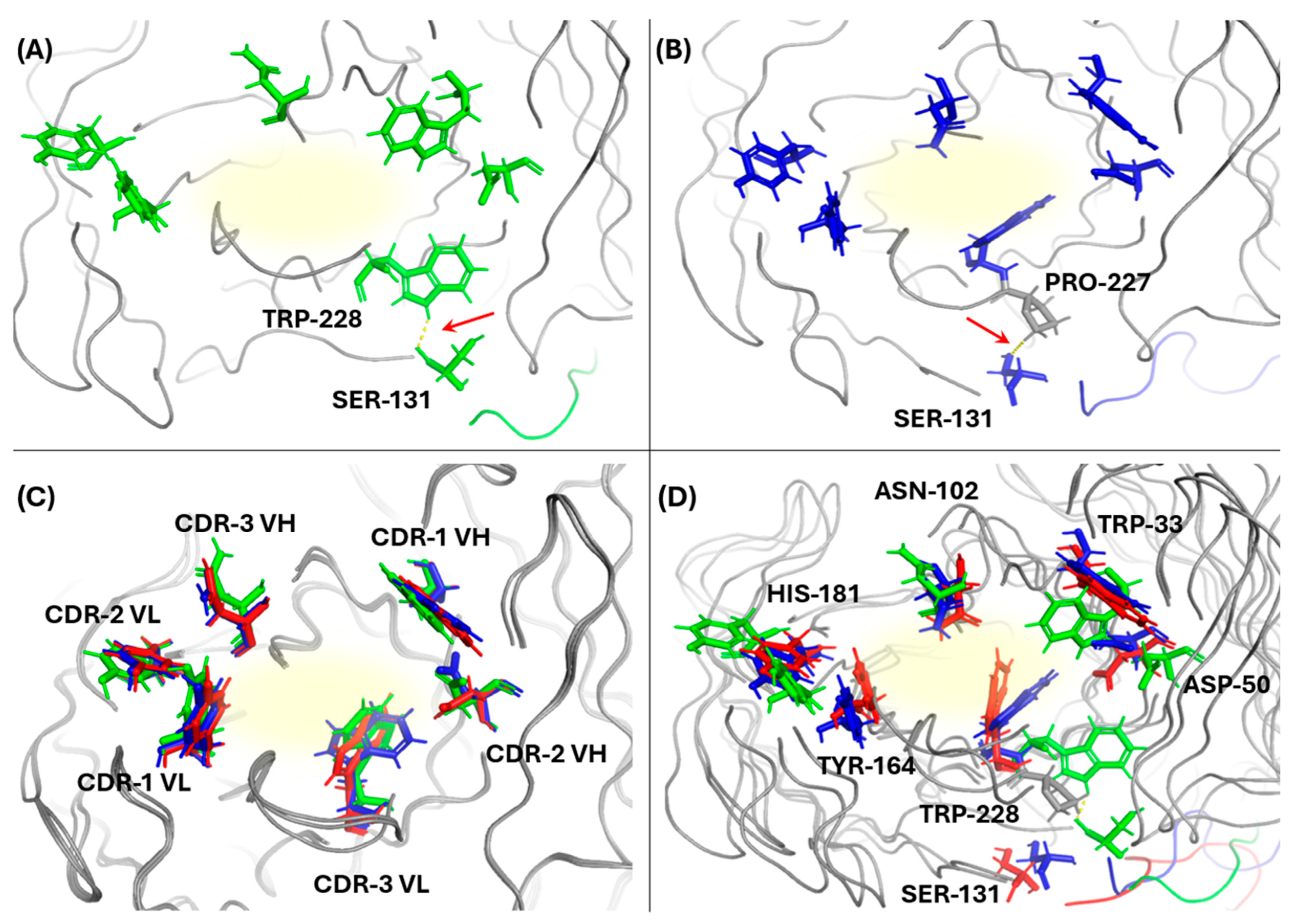



| Single Chain Fragment Variable | Pose | Location | Interacting Saccharide | Binding Energies (kcal/mol) |
|---|---|---|---|---|
| Native Anti-A | 1 | Framework | Fuc, Gal, GalNAc | −6.0 |
| 2 | Framework | Fuc, GalNAc | −6.0 | |
| 3 | Framework | Gal, GalNAc | −6.0 | |
| 4 | CDR | Fuc, Gal, GalNAc | −5.7 | |
| 5 | Framework | Fuc, Gal, GalNAc | −5.6 | |
| 6 | CDR | Fuc, Gal, GalNAc | −5.6 | |
| 7 | Framework | Fuc, Gal, GalNAc | −5.6 | |
| 8 | Framework | Fuc, Gal | −5.6 | |
| 9 | Framework | Fuc, GalNAc | −5.5 | |
| Mutant-1a Anti-A | 1 | CDR | Fuc, Gal, GalNAc | −7.4 |
| 2 | CDR | Fuc, Gal, GalNAc | −6.7 | |
| 3 | CDR | Fuc, Gal | −6.7 | |
| 4 | CDR | Fuc, Gal, GalNAc | −6.6 | |
| 5 | CDR | Fuc, GalNAc | −6.3 | |
| 6 | CDR | Gal, GalNAc | −6.2 | |
| 7 | CDR | Fuc, Gal, GalNAc | −6.2 | |
| 8 | Framework | Fuc, Gal, GalNAc | −5.9 | |
| 9 | CDR | Gal | −5.8 | |
| Mutant-1b Anti-A | 1 | Framework | GalNAc | −6.2 |
| 2 | Framework | Fuc, Gal, GalNAc | −5.5 | |
| 3 | CDR | Gal, GalNAc | −5.4 | |
| 4 | Framework | Fuc, GalNAc | −5.4 | |
| 5 | Framework | Fuc, Gal, GalNAc | −5.4 | |
| 6 | Framework | Fuc, Gal | −5.4 | |
| 7 | CDR | Fuc, Gal, GalNAc | −5.3 | |
| 8 | Framework | Fuc, Gal | −5.2 | |
| 9 | Framework | Fuc, GalNAc | −5.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hafeez, S.; Zaidi, N.U.S.S. Prevention of Blood Incompatibility Related Hemagglutination: Blocking of Antigen A on Red Blood Cells Using In Silico Designed Recombinant Anti-A scFv. Antibodies 2024, 13, 64. https://doi.org/10.3390/antib13030064
Hafeez S, Zaidi NUSS. Prevention of Blood Incompatibility Related Hemagglutination: Blocking of Antigen A on Red Blood Cells Using In Silico Designed Recombinant Anti-A scFv. Antibodies. 2024; 13(3):64. https://doi.org/10.3390/antib13030064
Chicago/Turabian StyleHafeez, Saleha, and Najam Us Sahar Sadaf Zaidi. 2024. "Prevention of Blood Incompatibility Related Hemagglutination: Blocking of Antigen A on Red Blood Cells Using In Silico Designed Recombinant Anti-A scFv" Antibodies 13, no. 3: 64. https://doi.org/10.3390/antib13030064
APA StyleHafeez, S., & Zaidi, N. U. S. S. (2024). Prevention of Blood Incompatibility Related Hemagglutination: Blocking of Antigen A on Red Blood Cells Using In Silico Designed Recombinant Anti-A scFv. Antibodies, 13(3), 64. https://doi.org/10.3390/antib13030064







