Surface Ozone Trends and Health Impacts in the Yangtze River Delta Region During 2015–2019
Abstract
1. Introduction
2. Date and Research Methods
2.1. Ground-Level O3 Data
2.2. Trend Analysis
2.3. Premature Mortality Estimation Method
3. Results Analysis
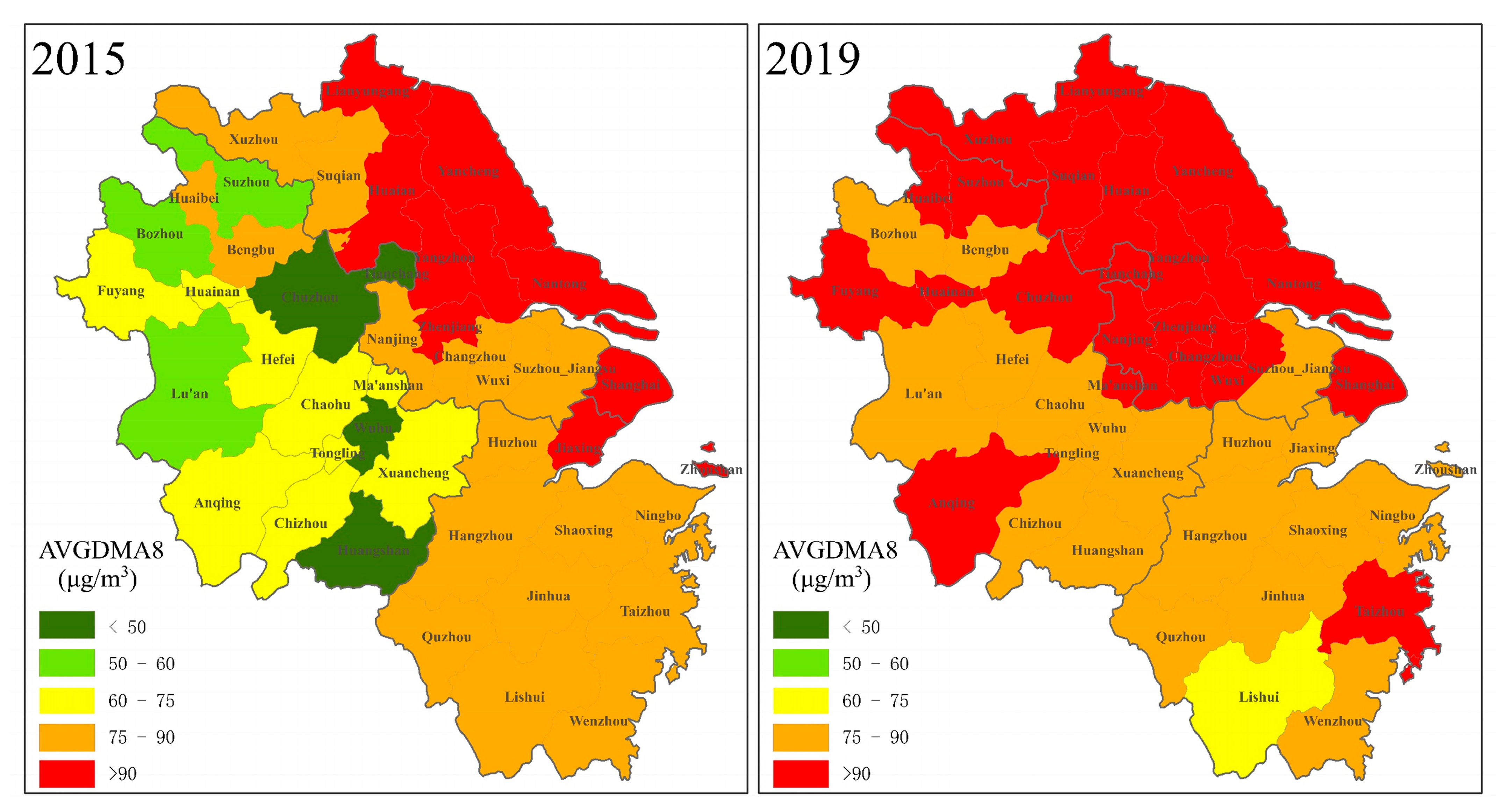
3.1. Spatial and Temporal Distribution of AVGDMA8 O3 Concentrations
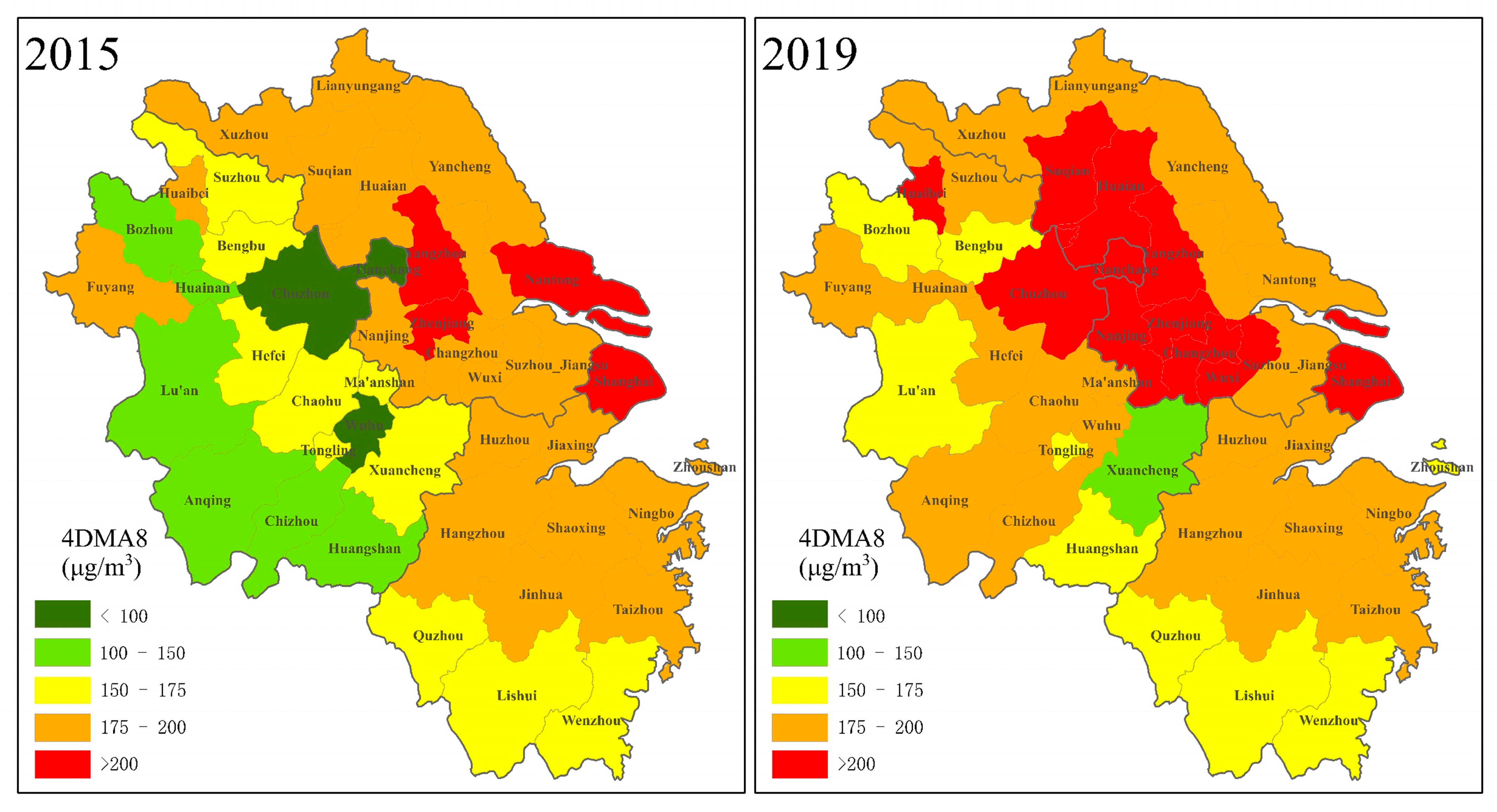
3.2. Spatial and Temporal Distribution of 4DMA8 O3 Concentrations
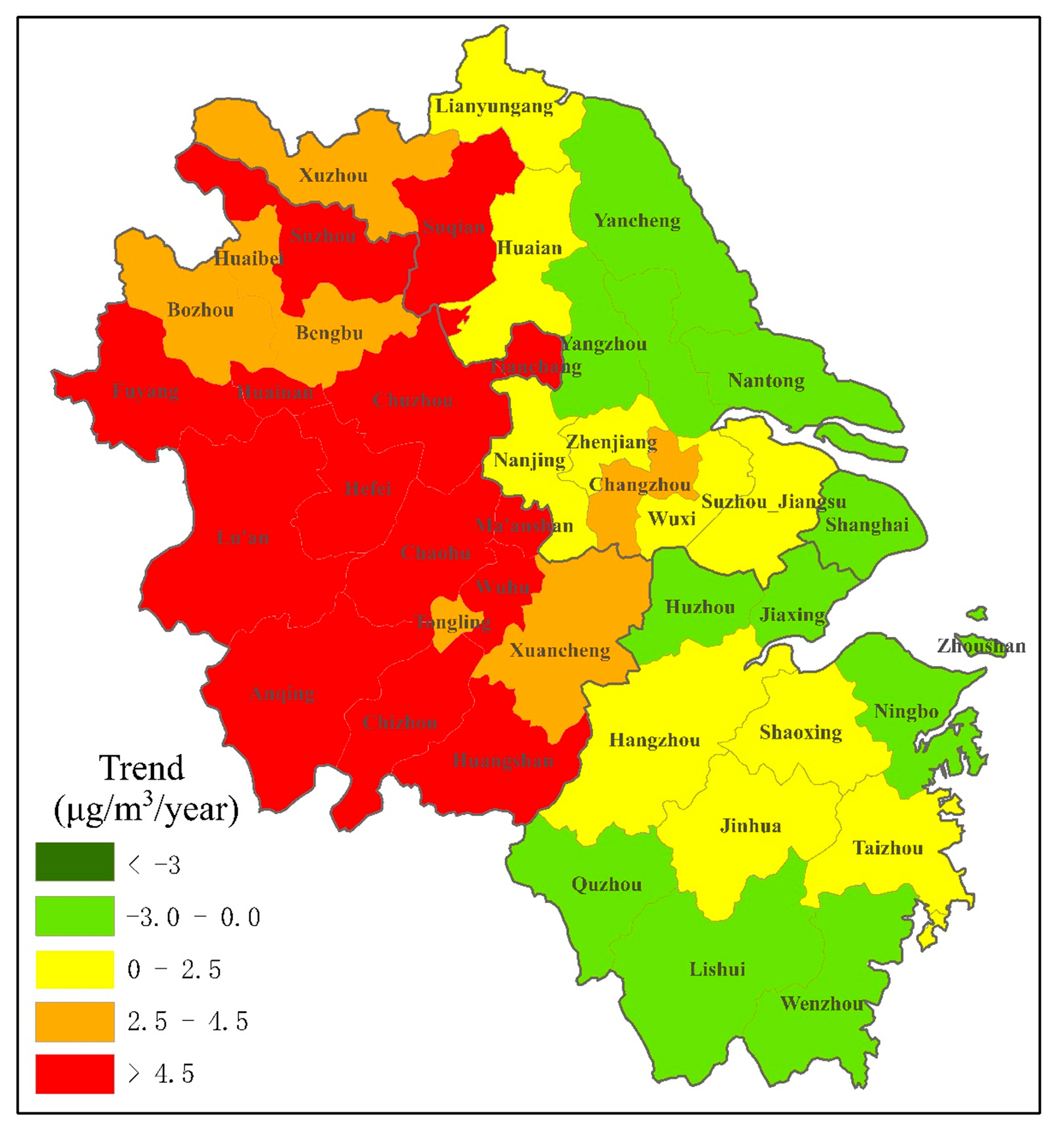
3.3. Trends in DMA8 O3 Concentrations
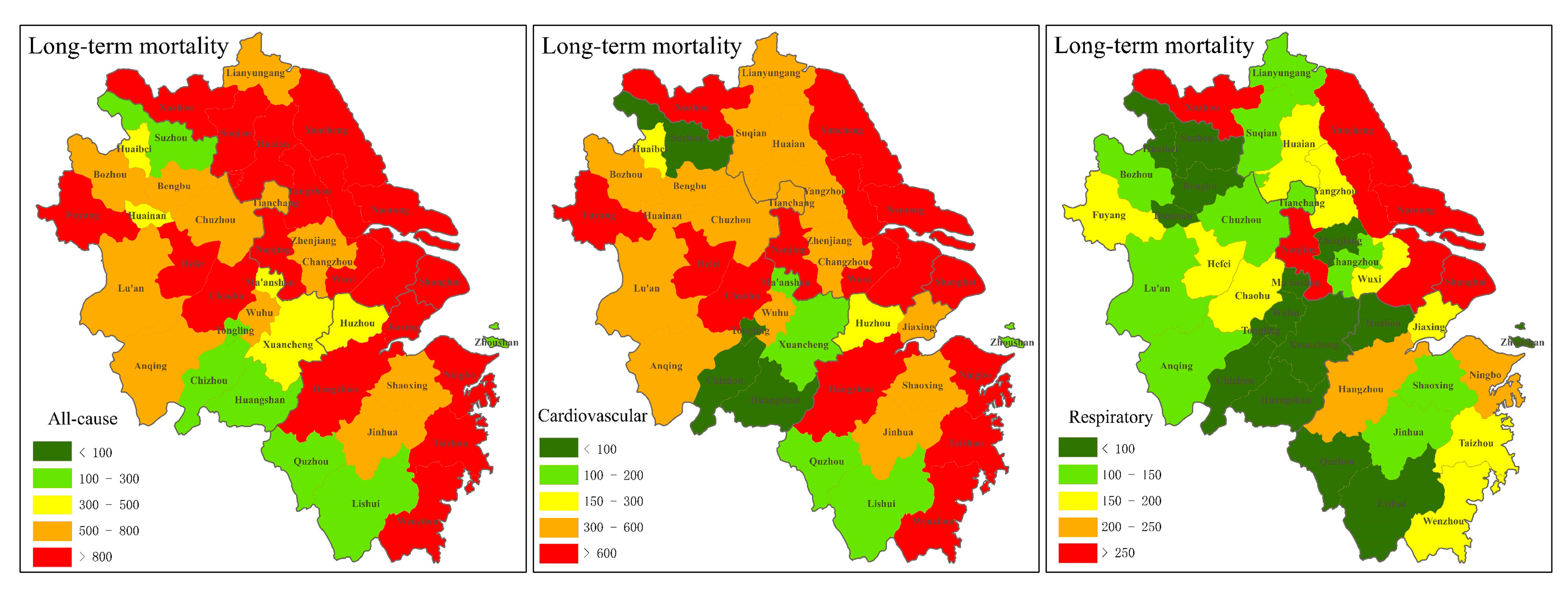
3.4. Long-Term Premature Mortality
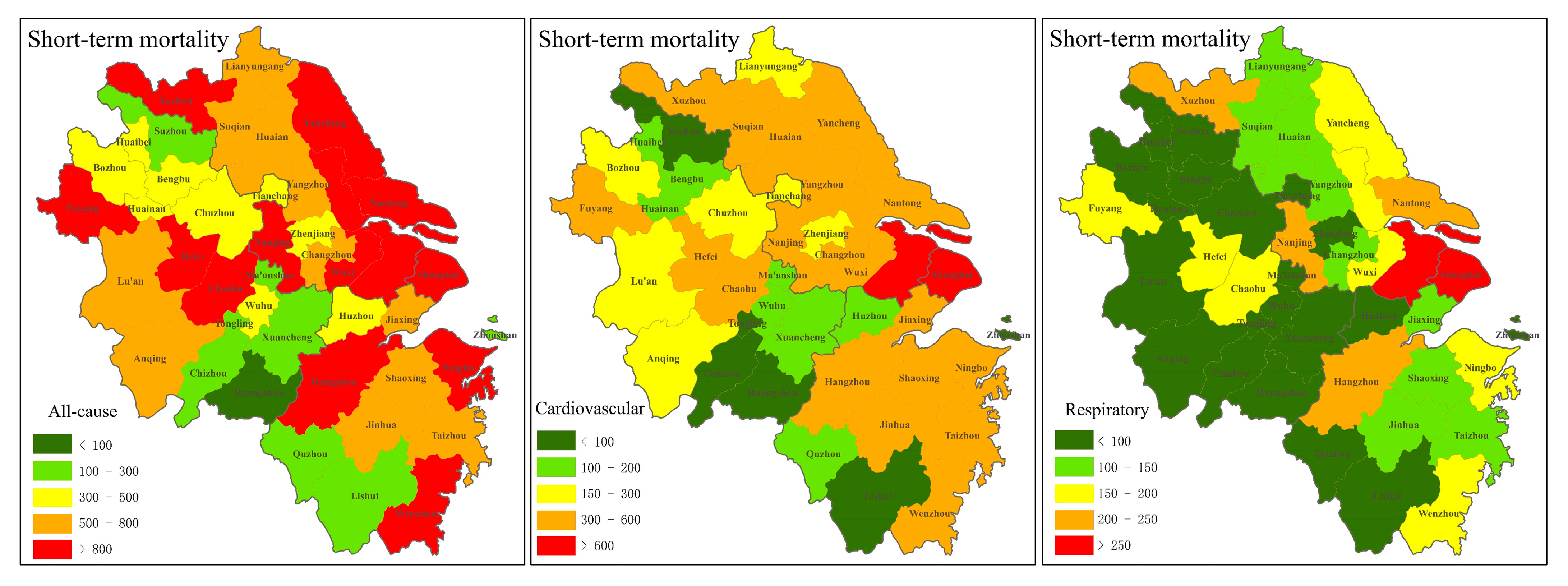
3.5. Short-Term Premature Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, Y.; Zhang, Y.; Wang, W.; Qin, P.; Li, H.; Jiao, H.; Wei, J. Estimation of health risk and economic loss attributable to PM2.5 and O3 pollution in Jilin Province, China. Sci. Rep. 2023, 13, 17717. [Google Scholar] [CrossRef]
- Ainsworth, E.A. Understanding and improving global crop response to ozone pollution. Plant J. 2017, 90, 886–897. [Google Scholar] [CrossRef]
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef]
- Xu, X. Recent advances in studies of ozone pollution and impacts in China: A short review. Curr. Opin. Environ. Sci. Health 2021, 19, 100225. [Google Scholar] [CrossRef]
- Sicard, P.; Serra, R.; Rossello, P. Spatiotemporal trends in ground-level ozone concentrations and metrics in France over the time period 1999–2012. Environ. Res. 2016, 149, 122–144. [Google Scholar] [CrossRef]
- Yang, J.; Bu, D.; Liu, J.; Du, M. Research review on urban ozone pollution control in China. Environ. Sustain. Dev. 2020, 47, 86–90. [Google Scholar]
- Yan, H.; Zhang, W.; Hou, M.; Li, Y.-S.; Gao, P.; Xia, Q.; Meng, X.-Y.; Fan, L.-Y.; Ye, D.-Q. Sources and control area division of ozone pollution in cities at prefecture level and above in China. Environ. Sci. 2020, 41, 5215–5224. [Google Scholar]
- Hong, S.Y.; Ren, Z.B.; Wang, C.C.; Zhang, P.; Guo, Y.J.; Liu, J.P.; Liu, Y. Spatial and temporal patterns of ozone pollution and its influencing factors in China in 2019. Sci. Geogr. Sin. 2024, 44, 1706–1717. [Google Scholar]
- Kuerban, M.; Waili, Y.; Fan, F.; Liu, Y.; Qin, W.; Dore, A.J.; Peng, J.; Xu, W.; Zhang, F. Spatio-temporal patterns of air pollution in China from 2015 to 2018 and implications for health risks. Environ. Pollut. 2020, 258, 113659. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Ecology and Environment of the People’s Republic of China. China Ecological and Environmental Status Bulletin 2017. Available online: https://www.mee.gov.cn/hjzl/sthjzk/zghjzkgb/201805/P020180531534645032372.pdf (accessed on 22 May 2018).
- Lu, X.; Hong, J.; Zhang, L.; Cooper, O.R.; Schultz, M.G.; Xu, X.; Wang, T.; Gao, M.; Zhao, Y.; Zhang, Y. Severe surface ozone pollution in China: A global perspective. Environ. Sci. Technol. Lett. 2018, 5, 487–494. [Google Scholar] [CrossRef]
- Ministry of Ecology and Environment of the People’s Republic of China. China Ecological and Environmental Status Bulletin 2018. Available online: https://www.mee.gov.cn/hjzl/sthjzk/zghjzkgb/201905/P020190619587632630618.pdf (accessed on 22 May 2019).
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong-Neto, H.J.; Novakova, S.; Steiropoulos, P.; Kowal, K. Impact of air pollution on asthma outcomes. Int. J. Environ. Res. Public Health 2020, 17, 6212. [Google Scholar] [CrossRef] [PubMed]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and health impacts of air pollution: A review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef]
- Liu, N.; Lin, W.; Ma, J.; Xu, W.; Xu, X. Seasonal variation in surface ozone and its regional characteristics at global atmosphere watch stations in China. J. Environ. Sci. 2019, 77, 291–302. [Google Scholar] [CrossRef]
- Zhao, H.; Chen, K.Y.; Liu, Z.; Zhang, Y.X.; Shao, T.; Zhang, H.L. Coordinated control of PM2.5 and O3 is urgently needed in China after implementation of the “Air pollution prevention and control action plan”. Chemosphere 2021, 270, 129441. [Google Scholar] [CrossRef]
- Dai, Y.; Qiu, H.; Sun, S.; Yang, Y.; Lin, H.; Tian, L. Age-dependent effect of ambient ozone on emergency asthma hospitalizations in Hong Kong. J. Allergy Clin. Immunol. 2018, 141, 1532–1534. [Google Scholar] [CrossRef]
- Stevens, E.L.; Rosser, F.; Forno, E.; Peden, D.; Celedón, J.C. Can the effects of outdoor air pollution on asthma be mitigated? J. Allergy Clin. Immunol. 2019, 143, 2016–2018. [Google Scholar] [CrossRef]
- Chatkin, J.; Correa, L.; Santos, U. External environmental pollution as a risk factor for asthma. Clin. Rev. Allergy Immunol. 2022, 62, 72–89. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Zanobetti, A.; Dominici, F. Who is more affected by ozone pollution? A systematic review and meta-analysis. Am. J. Epidemiol. 2014, 180, 15–28. [Google Scholar] [CrossRef]
- Tian, Y.; Xiang, X.; Juan, J.; Song, J.; Cao, Y.; Huang, C.; Li, M.; Hu, Y. Short-term effect of ambient ozone on daily emergency room visits in Beijing, China. Sci. Rep. 2018, 8, 2775. [Google Scholar] [CrossRef] [PubMed]
- Raza, A.; Dahlquist, M.; Lind, T.; Ljungman, P.L. Susceptibility to short-term ozone exposure and cardiovascular and respiratory mortality by previous hospitalizations. Environ. Health 2018, 17, 37. [Google Scholar] [CrossRef]
- Zhan, Y.; Luo, Y.; Deng, X.; Grieneisen, M.L.; Zhang, M.; Di, B. Spatiotemporal prediction of daily ambient ozone levels across China using random forest for human exposure assessment. Environ. Pollut. 2018, 233, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Li, X.; Teng, Y.; Fu, H.; Chen, L.; Mao, J.; Zhang, H.; Gao, S.; Sun, Y.; Ma, Z. Estimation of health and economic benefits based on ozone exposure level with high spatial-temporal resolution by fusing satellite and station observations. Environ. Pollut. 2019, 255, 113267. [Google Scholar] [CrossRef]
- Li, K.; Jacob, D.J.; Liao, H.; Shen, L.; Zhang, Q.; Bates, K.H. Anthropogenic drivers of 2013–2017 trends in summer surface ozone in China. Proc. Natl. Acad. Sci. USA 2019, 116, 422–427. [Google Scholar] [CrossRef]
- Wang, T.; Xue, L.; Brimblecombe, P.; Lam, Y.F.; Li, L.; Zhang, L. Ozone pollution in China: A review of concentrations, meteorological influences, chemical precursors, and effects. Sci. Total Environ. 2017, 575, 1582–1596. [Google Scholar] [CrossRef]
- Gao, R.; Li, Q.; Che, F.; Zhang, Y.P.; Zu, Y.G.; Liu, F. Spatial and Temporal Distribution Characteristics of Ozone Concentration and Health Benefit Assessment in the Beijing-Tianjin-Hebei Region from 2015 to 2020. Environ. Sci. 2024, 45, 2525–2536. [Google Scholar]
- Sinha, B.; Singh Sangwan, K.; Maurya, Y.; Kumar, V.; Sarkar, C.; Chandra, B.; Sinha, V. Assessment of crop yield losses in Punjab and Haryana using 2 years of continuous in situ ozone measurements. Atmos. Chem. Phys. 2015, 15, 9555–9576. [Google Scholar] [CrossRef]
- Schultz, M.G.; Schröder, S.; Lyapina, O.; Cooper, O.R.; Galbally, I.; Petropavlovskikh, I.; Von Schneidemesser, E.; Tanimoto, H.; Elshorbany, Y.; Naja, M. Tropospheric Ozone Assessment Report: Database and metrics data of global surface ozone observations. Elem. Sci. Anthr. 2017, 5, 58. [Google Scholar] [CrossRef]
- Lefohn, A.S.; Malley, C.S.; Smith, L.; Wells, B.; Hazucha, M.; Simon, H.; Naik, V.; Mills, G.; Schultz, M.G.; Paoletti, E. Tropospheric ozone assessment report: Global ozone metrics for climate change, human health, and crop/ecosystem research. Elem. Sci. Anthr. 2018, 6, 27. [Google Scholar] [CrossRef]
- The R Core Team. R: A Language and Environment for Statistical Computing; The R Foundation for Statistical Computing: Vienna, Austria, 2010. [Google Scholar]
- Carslaw, D. The OpenAir manual–open-source tools for analysing air pollution data. Man. Version 2015, 27–28, 52–61. [Google Scholar]
- Turner, M.C.; Jerrett, M.; Pope, C.A., III; Krewski, D.; Gapstur, S.M.; Diver, W.R.; Beckerman, B.S.; Marshall, J.D.; Su, J.; Crouse, D.L. Long-term ozone exposure and mortality in a large prospective study. Am. J. Respir. Crit. Care Med. 2016, 193, 1134–1142. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.C.; Hayes, R.B.; Ahn, J.; Shao, Y.; Silverman, D.T.; Jones, R.R.; Garcia, C.; Bell, M.L.; Thurston, G.D. Long-term exposure to ozone and cause-specific mortality risk in the United States. Am. J. Respir. Crit. Care Med. 2019, 200, 1022–1031. [Google Scholar] [CrossRef]
- Henschel, S.; Chan, G. Health Risks of Air Pollution in Europe-HRAPIE Project: New Emerging Risks to Health From Air Pollution-Results from the Survey of Experts; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Yin, P.; Chen, R.; Wang, L.; Meng, X.; Liu, C.; Niu, Y.; Lin, Z.; Liu, Y.; Liu, J.; Qi, J. Ambient ozone pollution and daily mortality: A nationwide study in 272 Chinese cities. Environ. Health Perspect. 2017, 125, 117006. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Liu, X.; Zhang, B.; Wang, J.; Shang, K. Meta-analysis of association between short-term ozone exposure and population mortality in China. Acta Sci. Circumst. 2016, 36, 1477–1485. [Google Scholar]
- He, J.; Gong, S.; Yu, Y.; Yu, L.; Wu, L.; Mao, H.; Song, C.; Zhao, S.; Liu, H.; Li, X. Air pollution characteristics and their relation to meteorological conditions during 2014–2015 in major Chinese cities. Environ. Pollut. 2017, 223, 484–496. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.G.; Shao, T.J.; Zhao, J.B.; Cao, J.J.; Song, Y.Y. Spatio-temporal Differentiation of Ozone Concentration and Its Driving Factors in Yangtze River Delta Urban Agglomeration. Resour. Environ. Yangtze Basin 2019, 28, 1434–1445. [Google Scholar]
- Jerrett, M.; Burnett, R.T.; Pope, C.A., III; Ito, K.; Thurston, G.; Krewski, D.; Shi, Y.; Calle, E.; Thun, M. Long-term ozone exposure and mortality. N. Engl. J. Med. 2009, 360, 1085–1095. [Google Scholar] [CrossRef]
- Li, M.; Zhang, Q.; Zheng, B.; Tong, D.; Lei, Y.; Liu, F.; Hong, C.; Kang, S.; Yan, L.; Zhang, Y. Persistent growth of anthropogenic non-methane volatile organic compound (NMVOC) emissions in China during 1990–2017: Drivers, speciation and ozone formation potential. Atmos. Chem. Phys. 2019, 19, 8897–8913. [Google Scholar] [CrossRef]
- Han, H.; Liu, J.; Shu, L.; Wang, T.; Yuan, H. Local and synoptic meteorological influences on daily variability in summertime surface ozone in eastern China. Atmos. Chem. Phys. 2020, 20, 203–222. [Google Scholar] [CrossRef]
- Silver, B.; Reddington, C.; Arnold, S.; Spracklen, D. Substantial changes in air pollution across China during 2015–2017. Environ. Res. Lett. 2018, 13, 114012. [Google Scholar] [CrossRef]
- Chen, H.; Zhuang, B.; Liu, J.; Wang, T.; Li, S.; Xie, M.; Li, M.; Chen, P.; Zhao, M. Characteristics of ozone and particles in the near-surface atmosphere in the urban area of the Yangtze River Delta, China. Atmos. Chem. Phys. 2019, 19, 4153–4175. [Google Scholar] [CrossRef]
- Liu, C.W.; Lian, X.B.; Huang, J.P. Research Review on the Spatio-temporal Distribution of Ozone Pollution and Its Causes in China. Arid. Meteorol. 2020, 38, 355–361. [Google Scholar]
- Wang, Y.; Wild, O.; Chen, X.; Wu, Q.; Gao, M.; Chen, H.; Qi, Y.; Wang, Z. Health impacts of long-term ozone exposure in China over 2013–2017. Environ. Int. 2020, 144, 106030. [Google Scholar] [CrossRef]
- Malley, C.S.; Henze, D.K.; Kuylenstierna, J.C.; Vallack, H.W.; Davila, Y.; Anenberg, S.C.; Turner, M.C.; Ashmore, M.R. Updated global estimates of respiratory mortality in adults ≥ 30 years of age attributable to long-term ozone exposure. Environ. Health Perspect. 2017, 125, 087021. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, L.; Wang, X.; Gao, M.; Li, K.; Zhang, Y.; Yue, X.; Zhang, Y. Rapid increases in warm-season surface ozone and resulting health impact in China since 2013. Environ. Sci. Technol. Lett. 2020, 7, 240–247. [Google Scholar] [CrossRef]
- Zhan, C.; Xie, M.; Liu, J.; Wang, T.; Xu, M.; Chen, B.; Li, S.; Zhuang, B.; Li, M. Surface ozone in the Yangtze River Delta, China: A synthesis of basic features, meteorological driving factors, and health impacts. J. Geophys. Res. Atmos. 2021, 126, e2020JD033600. [Google Scholar] [CrossRef]
- Yang, L.; Hong, S.; Mu, H.; Zhou, J.; He, C.; Wu, Q.; Gong, X. Ozone exposure and health risks of different age structures in major urban agglomerations in the People’s Republic of China from 2013 to 2018. Environ. Sci. Pollut. Res. 2023, 30, 42152–42164. [Google Scholar] [CrossRef]
- Ghude, S.D.; Chate, D.; Jena, C.; Beig, G.; Kumar, R.; Barth, M.; Pfister, G.; Fadnavis, S.; Pithani, P. Premature mortality in India due to PM2.5 and ozone exposure. Geophys. Res. Lett. 2016, 43, 4650–4658. [Google Scholar] [CrossRef]
- Feng, Z.; De Marco, A.; Anav, A.; Gualtieri, M.; Sicard, P.; Tian, H.; Fornasier, F.; Tao, F.; Guo, A.; Paoletti, E. Economic losses due to ozone impacts on human health, forest productivity and crop yield across China. Environ. Int. 2019, 131, 104966. [Google Scholar] [CrossRef]
- Seltzer, K.M.; Shindell, D.T.; Malley, C.S. Measurement-based assessment of health burdens from long-term ozone exposure in the United States, Europe, and China. Environ. Res. Lett. 2018, 13, 104018. [Google Scholar] [CrossRef]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Chen, C. Changes in the spatial distribution of the employed population in the Yangtze River Delta region since the 21st century: An analysis and discussion based on census data. Land 2023, 12, 1249. [Google Scholar] [CrossRef]
- Lin, Y.; Jiang, F.; Zhao, J.; Zhu, G.; He, X.; Ma, X.; Li, S.; Sabel, C.E.; Wang, H. Impacts of O3 on premature mortality and crop yield loss across China. Atmos. Environ. 2018, 194, 41–47. [Google Scholar] [CrossRef]
- Liu, H.; Liu, S.; Xue, B.; Lv, Z.; Meng, Z.; Yang, X.; Xue, T.; Yu, Q.; He, K. Ground-level ozone pollution and its health impacts in China. Atmos. Environ. 2018, 173, 223–230. [Google Scholar] [CrossRef]

| Exposure Duration | Cause-Specific Mortality | Relative Risk |
|---|---|---|
| Long-term mortality | All-cause mortality | 1.02 (1.01–1.04) |
| cardiovascular | 1.03 (1.01–1.06) | |
| respiratory | 1.04 (1.00–1.09) | |
| Short-term mortality | All-cause mortality | 1.0024 (1.0013–1.0035) |
| cardiovascular | 1.0027 (1.0010–1.0044) | |
| respiratory | 1.0046 (1.0023–1.0070) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.; Cai, M.; Zhao, H. Surface Ozone Trends and Health Impacts in the Yangtze River Delta Region During 2015–2019. Atmosphere 2025, 16, 995. https://doi.org/10.3390/atmos16090995
Huang J, Cai M, Zhao H. Surface Ozone Trends and Health Impacts in the Yangtze River Delta Region During 2015–2019. Atmosphere. 2025; 16(9):995. https://doi.org/10.3390/atmos16090995
Chicago/Turabian StyleHuang, Jing, Mohan Cai, and Hui Zhao. 2025. "Surface Ozone Trends and Health Impacts in the Yangtze River Delta Region During 2015–2019" Atmosphere 16, no. 9: 995. https://doi.org/10.3390/atmos16090995
APA StyleHuang, J., Cai, M., & Zhao, H. (2025). Surface Ozone Trends and Health Impacts in the Yangtze River Delta Region During 2015–2019. Atmosphere, 16(9), 995. https://doi.org/10.3390/atmos16090995







