Effects of Exposure to Air Pollution and Cold Weather on Acute Myocardial Infarction Mortality
Abstract
1. Introduction
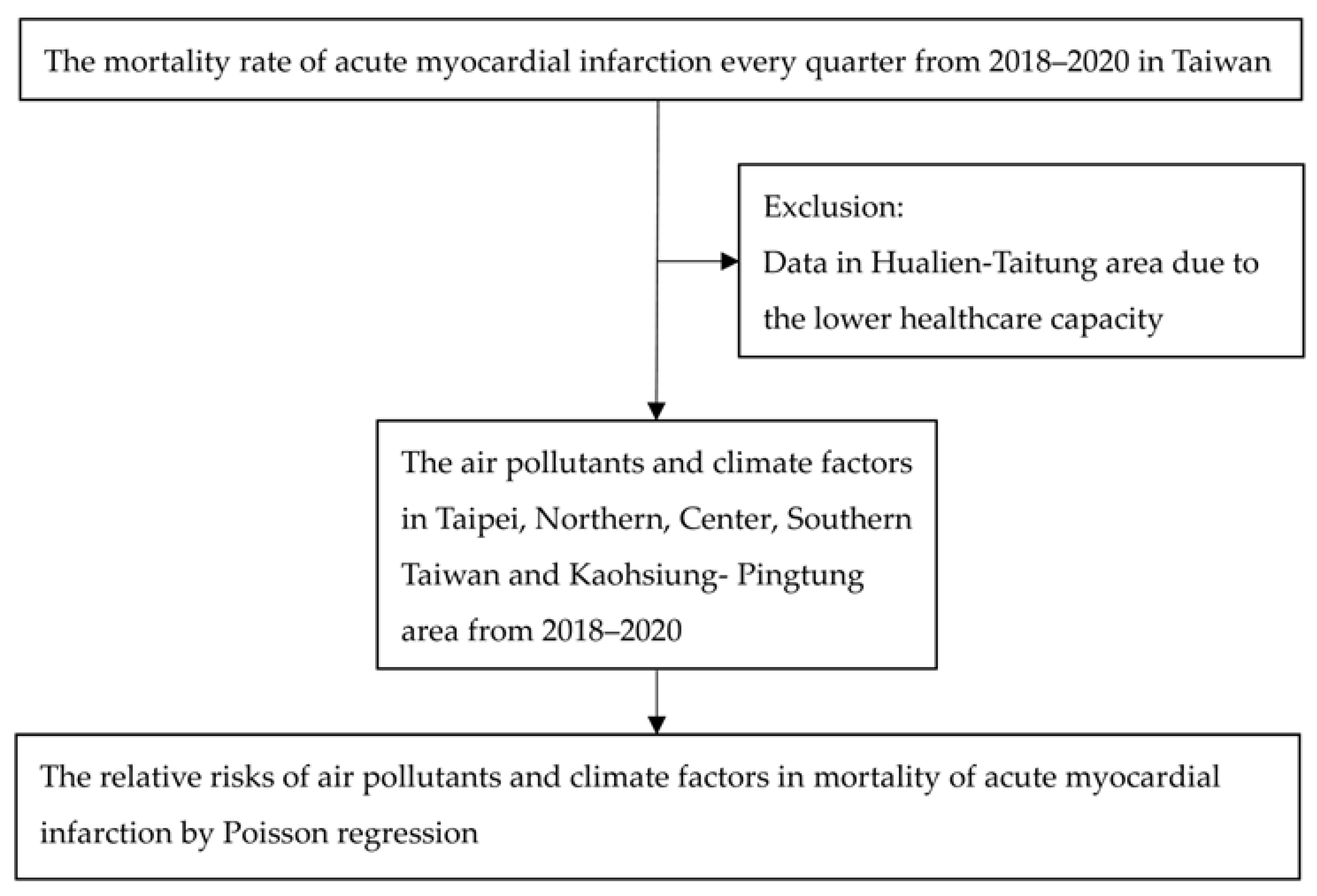
2. Materials and Methods
2.1. The Mortality of AMI
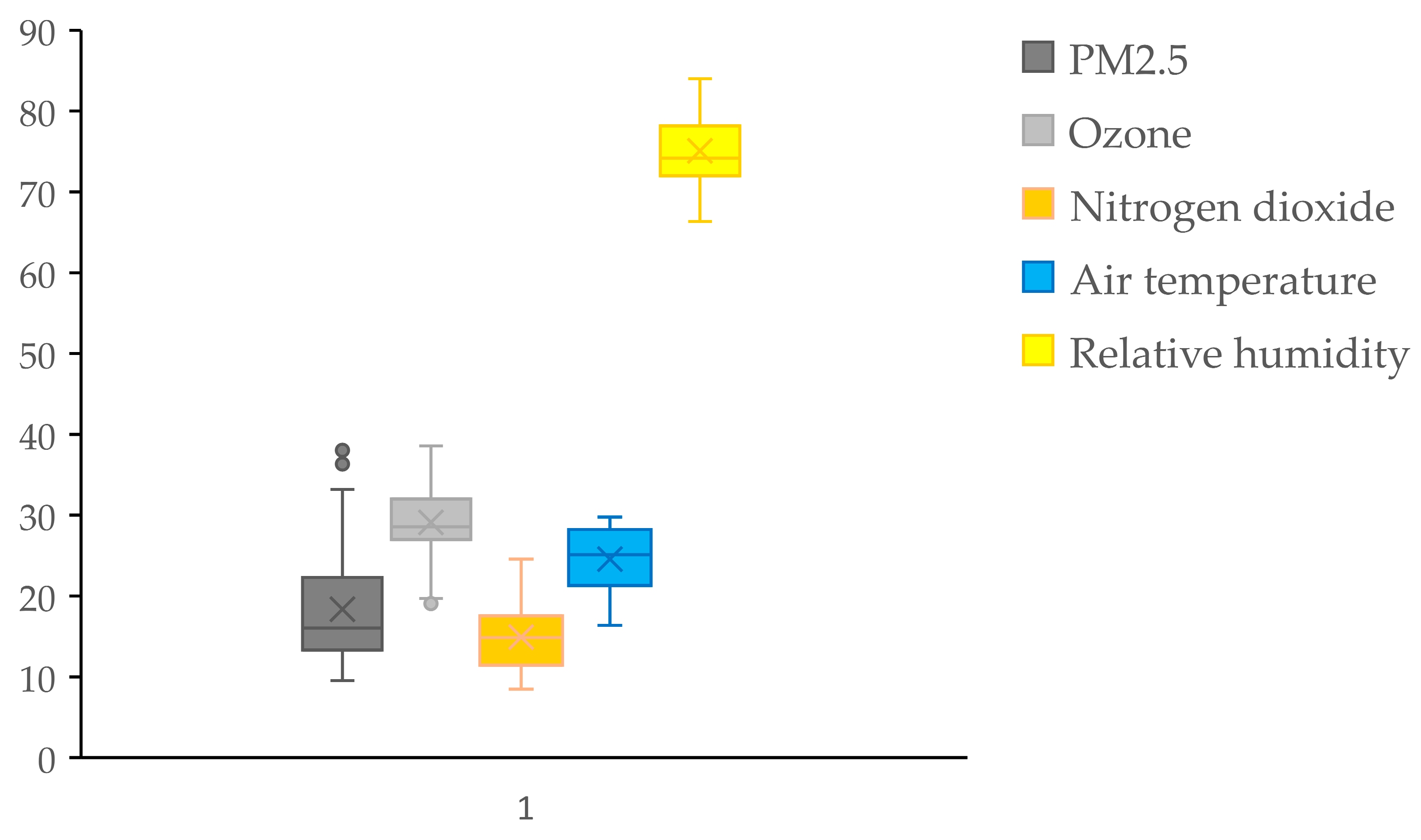
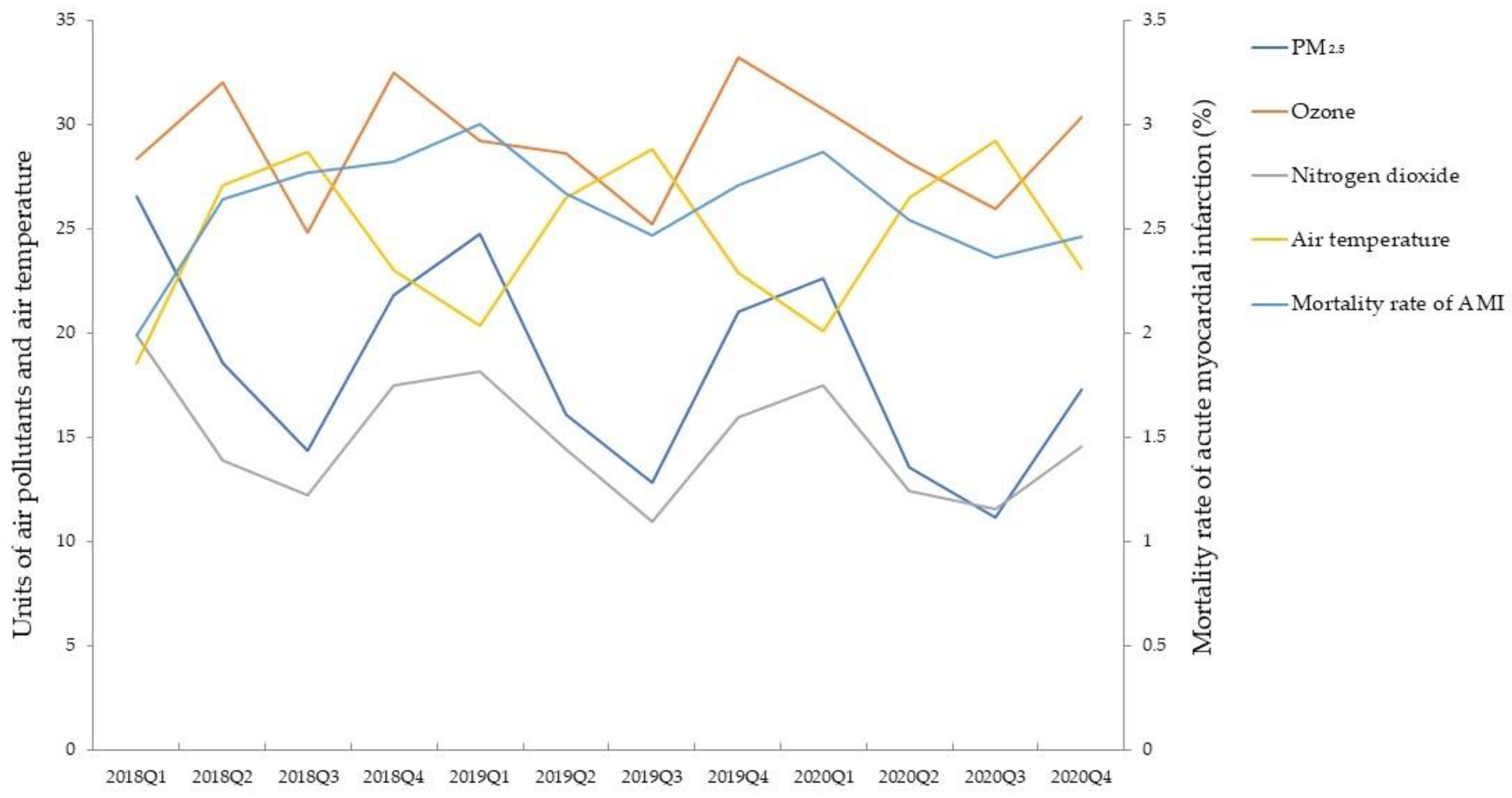
2.2. The Mean Air Pollutants and Climatic Factors
2.3. Correlation Between Air Pollutants and Climatic Factors
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CVD | cardiovascular disease |
| AMI | acute myocardial infarction |
| PM2.5 | particulate matter with a diameter less than 2.5 μm |
| O3 | ozone |
| NO2 | nitrogen dioxide |
| CO | carbon monoxide |
| WHO | World Health Organization |
| RR | relative risk |
| HR | hazard ratio |
References
- Mansoor, H.; Elgendy, I.Y.; Segal, R.; Bavry, A.A.; Bian, J. Risk prediction model for in-hospital mortality in women with ST-elevation myocardial infarction: A machine learning approach. Heart Lung 2017, 46, 405–411. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Oliveira, M.; Seringa, J.; Pinto, F.J.; Henriques, R.; Magalhães, T. Machine learning prediction of mortality in Acute Myocardial Infarction. BMC Med. Inform. Decis. Mak. 2023, 23, 70. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [PubMed]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef]
- Hsu, S.C.; Chang, J.H.; Lee, C.L.; Huang, W.C.; Hsu, Y.P.; Liu, C.T.; Jean, S.S.; Huang, S.K.; Hsu, C.W. Differential time-lag effects of ambient PM2.5 and PM2.5-bound PAHs on asthma emergency department visits. Environ. Sci. Pollut. Res. Int. 2020, 27, 43117–43124. [Google Scholar] [CrossRef]
- Huang, W.H.; Lin, J.H.; Weng, C.H.; Hsu, C.W.; Yen, T.H. Environmental NO2 and CO Exposure: Ignored Factors Associated with Uremic Pruritus in Patients Undergoing Hemodialysis. Sci. Rep. 2016, 6, 31168. [Google Scholar] [CrossRef]
- Chen, Y.L.; Lin, Y.Y.; Chin, P.W.; Chen, C.C.; Cheng, C.G.; Cheng, C.A. Analyzing COVID-19 and Air Pollution Effects on Pediatric Asthma Emergency Room Visited in Taiwan. Toxics 2024, 12, 79. [Google Scholar] [CrossRef]
- Cheng, C.G.; Yen, S.Y.; Hsiao, C.C.; Lin, Y.Y.; Chang, Y.H.; Chen, Y.H.; Cheng, C.A. Short-Term Exposure Effect of Ambient Fine Particulate Matter, Ozone and Cold Temperature on Emergency Room Visits for Asthma Patients. Toxics 2023, 11, 94. [Google Scholar] [CrossRef]
- Lelieveld, J.; Pozzer, A.; Pöschl, U.; Fnais, M.; Haines, A.; Münzel, T. Loss of life expectancy from air pollution compared to other risk factors: A worldwide perspective. Cardiovasc. Res. 2020, 116, 1910–1917. [Google Scholar] [CrossRef]
- de Bont, J.; Jaganathan, S.; Dahlquist, M.; Persson, Å.; Stafoggia, M.; Ljungman, P. Ambient air pollution and cardiovascular diseases: An umbrella review of systematic reviews and meta-analyses. J. Intern. Med. 2022, 291, 779–800. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Bertazzon, S.; Villeneuve, P.J.; Johnson, M.; Stieb, D.; Coward, S.; Tanyingoh, D.; Windsor, J.W.; Underwood, F.; Hill, M.D.; et al. Temporal and spatial effect of air pollution on hospital admissions for myocardial infarction: A case-crossover study. CMAJ Open 2020, 8, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Yen, C.-C.; Chen, P.-L. Effect of Short-Term Exposure to Fine Particulate Matter and Particulate Matter Pollutants on Triggering Acute Myocardial Infarction and Acute Heart Failure. Am. J. Cardiol. 2022, 175, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.O.; Jones, P.G.; Chan, P.S.; Peri-Okonny, P.A.; Hejjaji, V.; Spertus, J.A. Association of long-term exposure to particulate matter and ozone with health status and mortality in patients after myocardial infarction. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005598. [Google Scholar] [CrossRef]
- Weichenthal, S.; Lavigne, E.; Evans, G.; Pollitt, K.; Burnett, R.T. Ambient PM2.5 and risk of emergency room visits for myocardial infarction: Impact of regional PM2.5 oxidative potential: A case-crossover study. Environ. Health 2016, 15, 46. [Google Scholar] [CrossRef]
- Chuang, K.J.; Chan, C.C.; Su, T.C.; Lee, C.T.; Tang, C.S. The effect of urban air pollution on inflammation, oxidative stress, coagulation, and autonomic dysfunction in young adults. Am. J. Respir. Crit. Care Med. 2007, 176, 370–376. [Google Scholar] [CrossRef]
- Peters, A.; von Klot, S.; Mittleman, M.A.; Meisinger, C.; Hormann, A.; Kuch, B.; Wichmann, H.E. Triggering of acute myocardial infarction by different means of transportation. Eur. J. Prev. Cardiol. 2013, 20, 750–758. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Hajat, S.; Armstrong, B.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. The effects of hourly differences in air pollution on the risk of myocardial infarction: Case crossover analysis of the MINAP database. BMJ 2011, 343, d5531. [Google Scholar] [CrossRef]
- Cesaroni, G.; Forastiere, F.; Stafoggia, M.; Andersen, Z.J.; Badaloni, C.; Beelen, R.; Caracciolo, B.; de Faire, U.; Erbel, R.; Eriksen, K.T.; et al. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 2014, 348, f7412. [Google Scholar] [CrossRef]
- Bai, L.; Shin, S.; Burnett, R.T.; Kwong, J.C.; Hystad, P.; van Donkelaar, A.; Goldberg, M.S.; Lavigne, E.; Copes, R.; Martin, R.V.; et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: A population-based study of 5.1 million Canadian adults living in Ontario. Environ. Int. 2019, 132, 105004. [Google Scholar] [CrossRef]
- Shah, A.S.; Langrish, J.P.; Nair, H.; McAllister, D.A.; Hunter, A.L.; Donaldson, K.; Newby, D.E.; Mills, N.L. Global association of air pollution and heart failure: A systematic review and meta-analysis. Lancet 2013, 382, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.R. Oxidative stress and the cardiovascular effects of air pollution. Free Radic. Biol. Med. 2020, 151, 69–87. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Xu, X.; Chu, M.; Guo, Y.; Wang, J. Air particulate matter and cardiovascular disease: The epidemiological, biomedical and clinical evidence. J. Thorac. Dis. 2016, 8, 8–19. [Google Scholar]
- Crouse, D.L.; Peters, P.A.; van Donkelaar, A.; Goldberg, M.S.; Villeneuve, P.J.; Brion, O.; Khan, S.; Atari, D.O.; Jerrett, M.; Pope, C.A.; et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: A Canadian national-level cohort study. Environ. Health Perspect. 2012, 120, 708–714. [Google Scholar] [CrossRef]
- Juráň, S.; Karl, T.; Ofori-Amanfo, K.K.; Šigut, L.; Zavadilová, I.; Grace, J.; Urban, O. Drought shifts ozone deposition pathways in spruce forest from stomatal to non-stomatal flux. Environ. Pollut. 2025, 372, 126081. [Google Scholar] [CrossRef]
- Day, D.B.; Xiang, J.; Mo, J.; Li, F.; Chung, M.; Gong, J.; Weschler, C.J.; Ohman-Strickland, P.A.; Sundell, J.; Weng, W.; et al. Association of Ozone Exposure with Cardiorespiratory Pathophysiologic Mechanisms in Healthy Adults. JAMA Intern. Med. 2017, 177, 1344–1353. [Google Scholar] [CrossRef]
- Lim, C.C.; Hayes, R.B.; Ahn, J.; Shao, Y.; Silverman, D.T.; Jones, R.R.; Garcia, C.; Bell, M.L.; Thurston, G.D. Long-Term Exposure to Ozone and Cause-Specific Mortality Risk in the United States. Am. J. Respir. Crit. Care Med. 2019, 200, 1022–1031. [Google Scholar] [CrossRef]
- Zeng, J.; Lin, G.; Dong, H.; Li, M.; Ruan, H.; Yang, J. Association Between Nitrogen Dioxide Pollution and Cause-Specific Mortality in China: Cross-Sectional Time Series Study. JMIR Public Health Surveill. 2024, 10, e44648. [Google Scholar] [CrossRef]
- Ebi, K.L.; Capon, A.; Berry, P.; Broderick, C.; de Dear, R.; Havenith, G.; Honda, Y.; Kovats, R.S.; Ma, W.; Malik, A.; et al. Hot weather and heat extremes: Health risks. Lancet 2021, 398, 698–708. [Google Scholar] [CrossRef]
- Wang, Y.C.; Lin, Y.K.; Chuang, C.Y.; Li, M.H.; Chou, C.H.; Liao, C.H.; Sung, F.C. Associating emergency room visits with first and prolonged extreme temperature event in Taiwan: A population-based cohort study. Sci. Total Environ. 2012, 416, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Zhou, M.; Li, B.; Du, C.; Yao, R.; Wang, L.; Yang, X.; Yu, W. Reducing indoor relative humidity can improve the circulation and cardiorespiratory health of older people in a cold environment: A field trial conducted in Chongqing, China. Sci. Total Environ. 2022, 817, 152695. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance. Administration Medical Quality Indicator Information Hospital Total Professional Medical Service Quality Report. 2023. Available online: https://www.nhi.gov.tw/ch/lp-3504-1.html (accessed on 15 December 2024).
- Department of Household Registration, Ministry of the Interior of Taiwan. Demographics in 2020. Available online: https://www.ris.gov.tw/app/portal/346 (accessed on 1 March 2025).
- Air Pollutants Monthly Report of Taiwan Ministry of Environment. Available online: https://airtw.moenv.gov.tw/CHT/Query/Month_Value.aspx (accessed on 15 December 2024).
- Taiwan Center Weather Administration. Climate Monthly data in Taiwan. 2023. Available online: https://www.cwa.gov.tw/V8/E/C/Statistics/monthlydata.html (accessed on 15 December 2024).
- WHO. Air Pollution Guideline Values. 2022. Available online: https://iris.who.int/bitstream/handle/10665/345329/9789240034228-eng.pdf?sequence=1&isAllowed=y (accessed on 15 December 2024).
- Ministry of Health and Welfare. Cause of Death in 2023. Available online: https://www.mohw.gov.tw/cp-6650-79055-1.html (accessed on 15 December 2024).
- National Health Insurance Administration of Ministry of Health and Welfare. National Health Insurance Annual Statistical Report 2023. Available online: https://www.nhi.gov.tw/ch/cp-15989-bd89a-3811-1.html (accessed on 15 December 2024).
- Thomas, M.; Khraishah, H.; Schneider, A.; Lelieveld, J.; Daiber, A.; Rajagopalan, S. Challenges posed by climate hazards to cardiovascular health and cardiac intensive care: Implications for mitigation and adaptation. Eur. Heart J. Acute Cardiovasc. Care 2024, 13, 731–744. [Google Scholar]
- Tsao, T.M.; Hwang, J.S.; Chen, C.-Y.; Lin, S.T.; Tsai, M.J.; Su, T.C. Urban climate and cardiovascular health: Focused on seasonal variation of urban temperature, relative humidity, and PM2.5 air pollution. Ecotoxicol. Environ. Saf. 2023, 263, 115358. [Google Scholar] [CrossRef] [PubMed]
- Nemmar, A.; Hoylaerts, M.F.; Nemery, B. Effects of particulate air pollution on hemostasis. Clin. Occup. Environ. Med. 2006, 5, 865–881. [Google Scholar]
- Pope, C.A.; Burnett, R.T.; Thurston, G.D.; Thun, M.J.; Calle, E.E.; Krewski, D.; Godleski, J.J. Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004, 109, 71–77. [Google Scholar] [CrossRef]
- Hayes, R.B.; Lim, C.; Zhang, Y.; Cromar, K.; Shao, Y.; Reynolds, H.R.; Silverman, D.T.; Jones, R.R.; Park, Y.; Jerrett, M.; et al. PM2.5 air pollution and cause-specific cardiovascular disease mortality. Int. J. Epidemiol. 2020, 49, 25–35. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.; Kim, S.; Kang, S.H.; Kim, H.J.; Kim, H.; Heo, J.; Yi, S.M.; Kim, K.; Youn, T.J.; et al. Cardiovascular Effects of Long-Term Exposure to Air Pollution: A Population-Based Study with 900 845 Person-Years of Follow-up. J. Am. Heart Assoc. 2017, 6, e007170. [Google Scholar] [CrossRef]
- Kioumourtzoglou, M.A.; Schwartz, J.; James, P.; Dominici, F.; Zanobetti, A. PM2.5 and Mortality in 207 US Cities: Modification by Temperature and City Characteristics. Epidemiology 2016, 27, 221–227. [Google Scholar]
- Moon, J.; Kim, E.; Jang, H.; Song, I.; Kwon, D.; Kang, C.; Oh, J.; Park, J.; Kim, A.; Choi, M.; et al. Long-term exposure to PM2.5 and mortality: A national health insurance cohort study. Int. J. Epidemiol. 2024, 53, d140. [Google Scholar] [CrossRef]
- Liu, C.; Chen, R.; Sera, F.; Vicedo-Cabrera, A.M.; Guo, Y.; Tong, S.; Lavigne, E.; Correa, P.M.; Ortega, N.V.; Achilleos, S.; et al. Interactive effects of ambient fine particulate matter and ozone on daily mortality in 372 cities: Two stage time series analysis. BMJ 2023, 383, e075203. [Google Scholar] [CrossRef]
- Niu, Y.; Zhou, Y.; Chen, R.; Yin, P.; Meng, X.; Wang, W.; Liu, C.; Ji, J.S.; Qiu, Y.; Kan, H.; et al. Long-term exposure to ozone and cardiovascular mortality in China: A nationwide cohort study. Lancet Planet. Health 2022, 6, e496–e503. [Google Scholar] [CrossRef]
- Zimmerman, J.B.; Brooks, B.; Mills, M. The 2024 Outstanding Achievements in Environmental Science & Technology Award—The Asia Pacific Region. Environ. Sci. Technol. 2024, 58, 1–2. [Google Scholar] [PubMed]
- Li, M.; Dong, H.; Wang, B.; Zhao, W.; Zare Sakhvidi, M.J.; Li, L.; Lin, G.; Yang, J. Association between ambient ozone pollution and mortality from a spectrum of causes in Guangzhou, China. Sci. Total Environ. 2021, 754, 142110. [Google Scholar] [CrossRef] [PubMed]
- Khraishah, H.; Alahmad, B.; Ostergard, R.L.J.; AlAshqar, A.; Albaghdadi, M.; Vellanki, N.; Chowdhury, M.M.; Al-Kindi, S.G.; Zanobetti, A.; Gasparrini, A.; et al. Climate change and cardiovascular disease: Implications for global health. Nat. Rev. Cardiol. 2022, 19, 798–812. [Google Scholar] [CrossRef] [PubMed]
- Madrigano, J.; Mittleman, M.A.; Baccarelli, A.; Goldberg, R.; Melly, S.; von Klot, S.; Schwartz, J. Temperature, myocardial infarction, and mortality: Effect modification by individual- and area-level characteristics. Epidemiology 2013, 24, 439–446. [Google Scholar] [CrossRef]
- Goggins, W.B.; Chan, E.Y.; Yang, C.Y. Weather, pollution, and acute myocardial infarction in Hong Kong and Taiwan. Int. J. Cardiol. 2013, 168, 243–249. [Google Scholar] [CrossRef]
- Huang, X.; Ma, W.; Law, C.; Luo, J.; Zhao, N. Importance of applying Mixed Generalized Additive Model (MGAM) as a method for assessing the environmental health impacts: Ambient temperature and Acute Myocardial Infarction (AMI), among elderly in Shanghai, China. PLoS ONE 2021, 16, e0255767. [Google Scholar] [CrossRef]
- Saucy, A.; Ragettli, M.S.; Vienneau, D.; de Hoogh, K.; Tangermann, L.; Schäffer, B.; Wunderli, J.M.; Probst-Hensch, N.; Röösli, M. The role of extreme temperature in cause-specific acute cardiovascular mortality in Switzerland: A case-crossover study. Sci. Total Environ. 2021, 790, 147958. [Google Scholar] [CrossRef]
- Alahmad, B.; Khraishah, H.; Royé, D.; Vicedo-Cabrera, A.M.; Guo, Y.; Papatheodorou, S.I.; Achilleos, S.; Acquaotta, F.; Armstrong, B.; Bell, M.L.; et al. Associations Between Extreme Temperatures and Cardiovascular Cause-Specific Mortality: Results From 27 Countries. Circulation 2023, 147, 35–46. [Google Scholar] [CrossRef]
- Stafoggia, M.; Oftedal, B.; Chen, J.; Rodopoulou, S.; Renzi, M.; Atkinson, R.W.; Bauwelinck, M.; Klompmaker, J.O.; Mehta, A.; Vienneau, D.; et al. Long-term exposure to low ambient air pollution concentrations and mortality among 28 million people: Results from seven large European cohorts within the ELAPSE project. Lancet Planet. Health 2022, 6, e9–e18. [Google Scholar] [CrossRef]
- Mei, Y.; Li, A.; Zhao, M.; Xu, J.; Li, R.; Zhao, J.; Zhou, Q.; Ge, X.; Xu, Q. Associations and burdens of relative humidity with cause-specific mortality in three Chinese cities. Environ. Sci. Pollut. Res. Int. 2023, 30, 3512–3526. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhou, L.; Wang, C.; Chen, R.; Ma, X.; Xu, B.; Xiong, L.; Ding, Z.; Chen, X.; Zhou, Y.; et al. Associations Between Air Quality Changes and Biomarkers of Systemic Inflammation During the 2014 Nanjing Youth Olympics: A Quasi-Experimental Study. Am. J. Epidemiol. 2017, 185, 1290–1296. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.C.; Hayes, R.B.; Ahn, J.; Shao, Y.; Silverman, D.T.; Jones, R.R.; Thurston, G.D. Mediterranean Diet and the Association Between Air Pollution and Cardiovascular Disease Mortality Risk. Circulation 2019, 139, 1766–1775. [Google Scholar] [CrossRef] [PubMed]
- Tenório, M.C.d.S.; Graciliano, N.G.; Moura, F.A.; Oliveira, A.C.M.d.; Goulart, M.O.F. N-Acetylcysteine (NAC): Impacts on Human Health. Antioxidants 2021, 10, 967. [Google Scholar] [CrossRef]
- Zivkovic, S.; Maric, G.; Cvetinovic, N.; Lepojevic-Stefanovic, D.; Bozic Cvijan, B. Anti-Inflammatory Effects of Lipid-Lowering Drugs and Supplements—A Narrative Review. Nutrients 2023, 15, 1517. [Google Scholar] [CrossRef]
- Zafeiratou, S.; Samoli, E.; Dimakopoulou, K.; Rodopoulou, S.; Analitis, A.; Gasparrini, A.; Stafoggia, M.; De’ Donato, F.; Rao, S.; Monteiro, A.; et al. EXHAUSTION project team. A systematic review on the association between total and cardiopulmonary mortality/morbidity or cardiovascular risk factors with long-term exposure to increased or decreased ambient temperature. Sci. Total Environ. 2021, 772, 145383. [Google Scholar] [CrossRef]
- Takeuchi, A.; Nishiwaki, Y.; Okamura, T.; Milojevic, A.; Ueda, K.; Asakura, K.; Takebayashi, T.; Hasegawa, S.; Sairenchi, T.; Irie, F.; et al. Long-term exposure to particulate matter and mortality from cardiovascular diseases in Japan: The Ibaraki Prefectural Health Study (IPHS). J. Atheroscler. Thromb. 2021, 28, 230–240. [Google Scholar] [CrossRef]
| SO2 | CO | O3 | NO2 | PM10 | PM2.5 | Air Temperature (°C) | Relative Humidity (%) | ||
|---|---|---|---|---|---|---|---|---|---|
| SO2 | Pearson Correlation | 1 | −0.015 | 0.022 | −0.123 | 0.144 | 0.083 | −0.008 | 0.371 |
| p | 0.908 | 0.867 | 0.348 | 0.272 | 0.530 | 0.950 | 0.004 | ||
| CO | Pearson Correlation | −0.015 | 1 | 0.172 | 0.876 | 0.524 | 0.587 | −0.818 | −0.077 |
| p | 0.908 | 0.189 | <0.001 * | <0.001 * | <0.001 * | <0.001 * | 0.558 | ||
| O3 | Pearson Correlation | 0.022 | 0.172 | 1 | −0.056 | 0.718 | 0.650 | −0.171 | −0.394 |
| p | 0.867 | 0.189 | 0.668 | <0.001 * | <0.001 * | 0.191 | 0.002 * | ||
| NO2 | Pearson Correlation | −0.123 | 0.876 | −0.056 | 1 | 0.253 | 0.317 | −0.725 | −0.069 |
| p | 0.348 | <0.001 * | 0.668 | 0.051 * | 0.014 * | <0.001 * | 0.598 | ||
| PM10 | Pearson Correlation | 0.144 | 0.524 | 0.718 | 0.253 | 1 | 0.939 | −0.350 | −0.384 |
| p | 0.272 | <0.001 * | <0.001 * | 0.051 | <0.001 * | 0.006 * | 0.002 * | ||
| PM2.5 | Pearson Correlation | 0.083 | 0.587 | 0.650 | 0.317 | 0.939 | 1 | −0.429 | −0.323 |
| p | 0.530 | <0.001 * | <0.001 * | 0.014 * | <0.001 * | 0.001 * | 0.012 * | ||
| Air temperature (°C) | Pearson Correlation | −0.008 | −0.818 | −0.171 | −0.725 | −0.350 | −0.429 | 1 | −0.109 |
| p | 0.950 | <0.001 * | 0.191 | <0.001 * | 0.006 * | 0.001 * | 0.406 | ||
| Relative humidity (%) | Pearson Correlation | 0.371 | −0.077 | −0.394 | −0.069 | −0.384 | −0.323 | −0.109 | 1 |
| p | 0.004 * | 0.558 | 0.002 * | 0.598 | 0.002 * | 0.012 * | 0.406 | ||
| Adjusted Relative Risk | p | |
|---|---|---|
| The highest PM2.5 | 1.13 (95% CI: 1.04–1.229) | 0.004 * |
| The middle PM2.5 | 1.086 (95% CI: 1.033–1.142) | 0.001 * |
| The lowest PM2.5 | Reference | |
| The highest ozone | 1.095 (95% CI: 1.011–1.185) | 0.025 * |
| The middle ozone | 1.038 (95% CI: 0.981–1.099) | 0.194 |
| The lowest ozone | Reference | |
| Warm season | Reference | |
| Cold season | 1.087 (95% CI: 1.024–1.154) | 0.006 * |
| The highest NO2 | 0.761 (95% CI: 0.707–0.819) | <0.001 * |
| The middle NO2 | 0.861 (95% CI: 0.804–0.922) | <0.001 * |
| The lowest NO2 | Reference | |
| The highest RH | 1.068 (95% CI: 1.00–1.141) | 0.051 |
| The middle RH | 1.026 (95% CI: 0.973–1.081) | 0.344 |
| The lowest RH | Reference |
| Warm Season | Cold Season | ||||
|---|---|---|---|---|---|
| Relative Risk | p | Relative Risk | p | ||
| PM2.5 | 1.017 (95% CI: 1.002–1.031) | 0.025 * | 1 (95% CI: 0.994–1.005) | 0.902 | |
| Ozone | 0.998 (95% CI: 0.987–1.009) | 0.68 | 1.032 (95% CI: 1.016–1.048) | <0.001 * | |
| NO2 | 0.97 (95% CI: 0.959–0.982) | <0.001 * | 0.986 (95% CI: 0.973–0.999) | 0.035 * | |
| Air temperature | 0.985 (95% CI: 0.955–1.016) | 0.337 | 0. 981 (95% CI: 0.961–1.002) | 0.083 | |
| Relative humidity | 1.005 (95% CI: 0.997–1.013) | 0.238 | 1.011 (95% CI: 1–1.022) | 0.061 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-H.; Liu, I.-H.; Hsiao, C.-C.; Cheng, C.-G.; Cheng, C.-A. Effects of Exposure to Air Pollution and Cold Weather on Acute Myocardial Infarction Mortality. Atmosphere 2025, 16, 469. https://doi.org/10.3390/atmos16040469
Chen Y-H, Liu I-H, Hsiao C-C, Cheng C-G, Cheng C-A. Effects of Exposure to Air Pollution and Cold Weather on Acute Myocardial Infarction Mortality. Atmosphere. 2025; 16(4):469. https://doi.org/10.3390/atmos16040469
Chicago/Turabian StyleChen, Yu-Hsuan, I-Hsing Liu, Chih-Chun Hsiao, Chun-Gu Cheng, and Chun-An Cheng. 2025. "Effects of Exposure to Air Pollution and Cold Weather on Acute Myocardial Infarction Mortality" Atmosphere 16, no. 4: 469. https://doi.org/10.3390/atmos16040469
APA StyleChen, Y.-H., Liu, I.-H., Hsiao, C.-C., Cheng, C.-G., & Cheng, C.-A. (2025). Effects of Exposure to Air Pollution and Cold Weather on Acute Myocardial Infarction Mortality. Atmosphere, 16(4), 469. https://doi.org/10.3390/atmos16040469






