Formaldehyde Exposure and Associated Health Burdens Apportioned to Residential and Public Places Based on Personal and Environmental Measurements
Abstract
1. Introduction
2. Materials and Methods
2.1. Sampling Site and Study Design
2.2. Sampling Method and Chemical Analysis
2.3. QA/QC and Statistical Analysis
2.4. Exposure and Contribution Apportionment
2.5. Health Burden Estimation
2.6. Uncertainty and Sensitivity Analysis
3. Results and Discussion
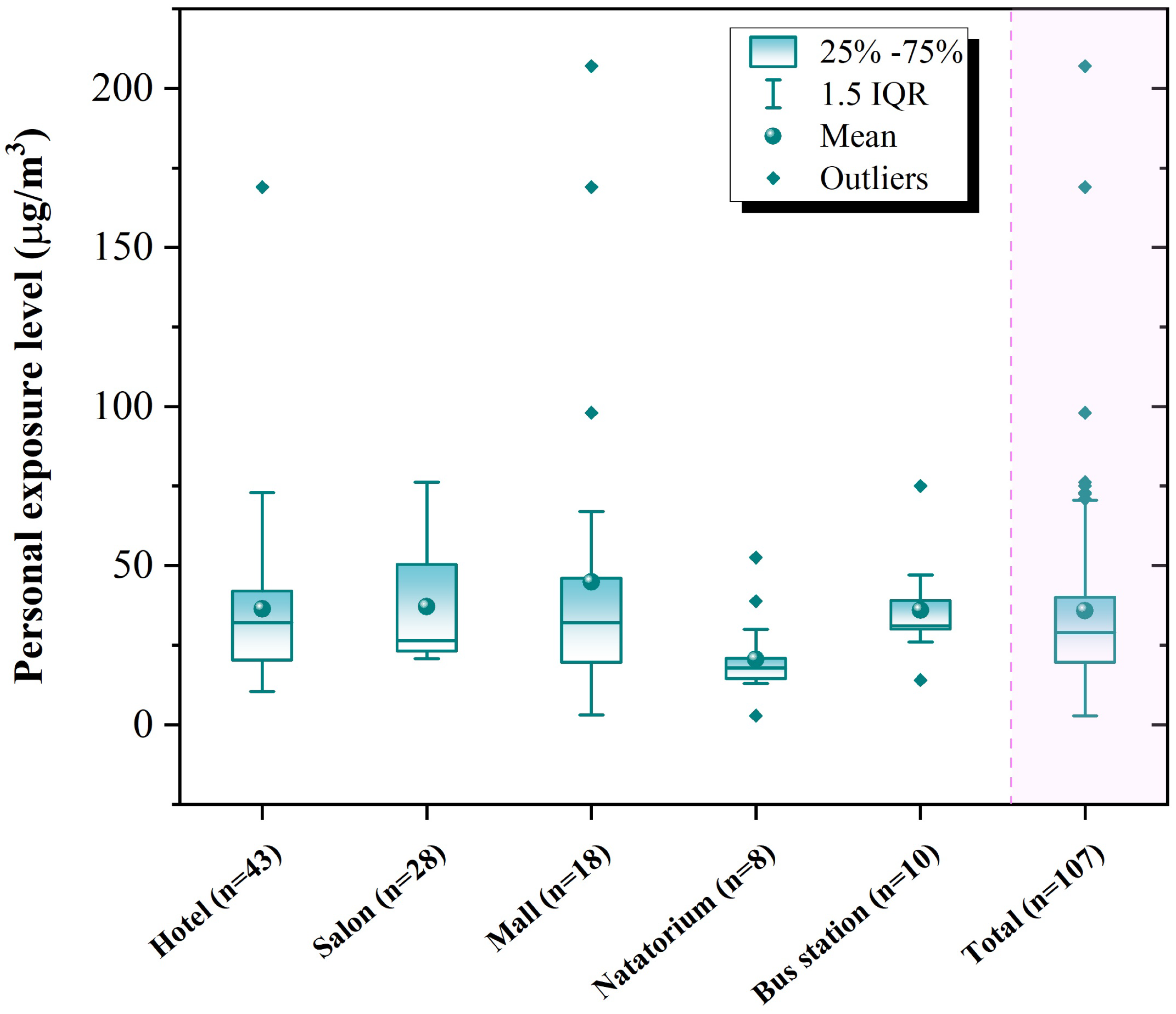
3.1. Personal Exposure Levels
3.2. Formaldehyde Concentration in Microenvironments
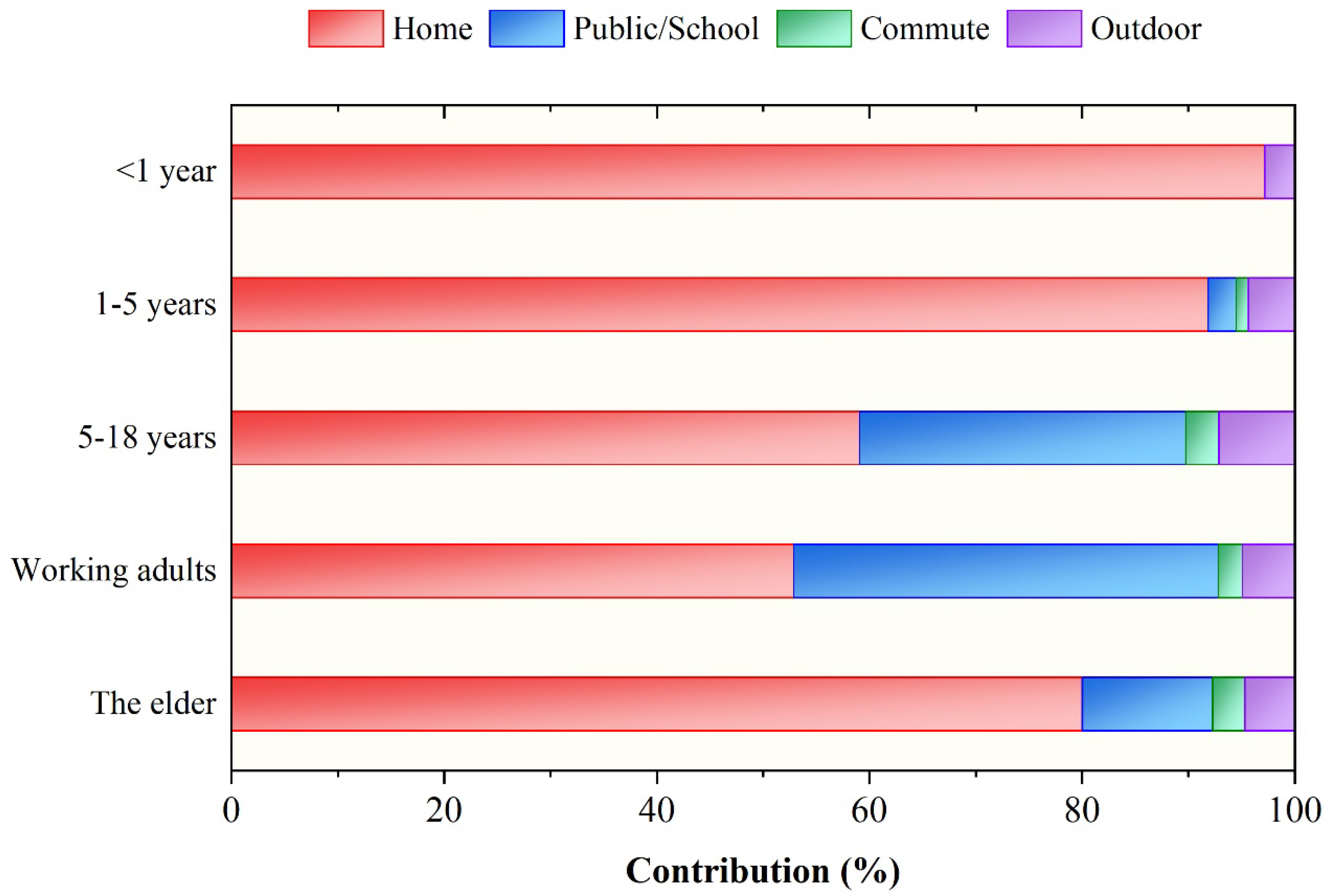
3.3. Exposure Estimates and Contribution Apportionment
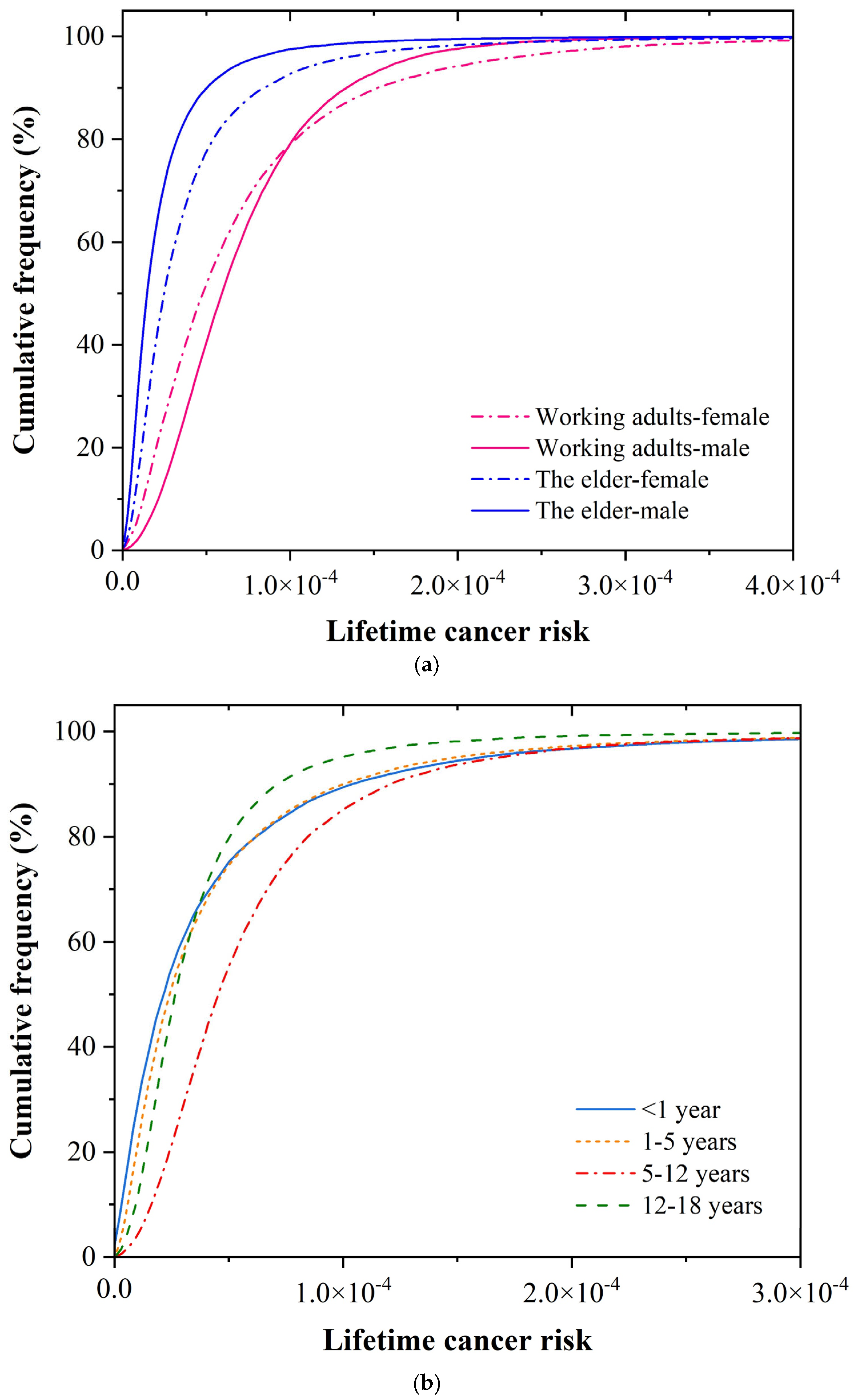
3.4. Cancer Risk and Burden of Disease
3.5. Sensitivity Analysis
3.6. Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- IARC. Formaldehyde, 2-Butoxyethanol and 1-Tert-butoxy-2-propanol. Monographs on the Evaluation of Carcinogenic Risks to Humans. 2006. Available online: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Monographs-On-The-Identification-Of-Carcinogenic-Hazards-To-Humans/Formaldehyde-2-Butoxyethanol-And-1--Em-Tert-Em–Butoxypropan-2-ol-2006 (accessed on 23 July 2025).
- Bentayeb, M.; Billionnet, C.; Baiz, N.; Derbez, M.; Kirchner, S.; Annesi-Maesano, I. Higher prevalence of breathlessness in elderly exposed to indoor aldehydes and VOCs in a representative sample of French dwellings. Respir. Med. 2013, 107, 1598–1607. [Google Scholar] [CrossRef]
- Billionnet, C.; Gay, E.; Kirchner, S.; Leynaert, B.; Annesi-Maesano, I. Quantitative assessments of indoor air pollution and respiratory health in a population-based sample of French dwellings. Environ. Res. 2011, 111, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Hulin, M.; Caillaud, D.; Annesi-Maesano, I. Indoor air pollution and childhood asthma: Variations between urban and rural areas. Indoor Air 2010, 20, 502–514. [Google Scholar] [CrossRef] [PubMed]
- Delfino, R.J.; Gong, H., Jr.; Linn, W.S.; Pellizzari, E.D.; Hu, Y. Asthma symptoms in hispanic children and daily ambient exposures to toxic and criteria air pollutants. Environ. Health Perspect. 2003, 111, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Coulburn, L.; Miller, W.; Susilawati, C. Onset characteristics and breadth of occupants’ long-lasting building-related symptoms attributed to living in damp housing conditions in Australia: Qualitative insights. Build. Environ. 2024, 255, 111432. [Google Scholar] [CrossRef]
- Locatelli, F.; Martinelli, L.; Marchetti, P.; Caliskan, G.; Badaloni, C.; Caranci, N.; de Hoogh, K.; Gatti, L.; Giorgi Rossi, P.; Guarda, L.; et al. Residential exposure to air pollution and incidence of leukaemia in the industrial area of Viadana, Northern Italy. Environ. Res. 2024, 254, 119120. [Google Scholar] [CrossRef]
- Khoshakhlagh, A.H.; Mohammadzadeh, M.; Ghobakhloo, S.; Cheng, H.; Gruszecka-Kosowska, A.; Knight, J. Health risk assessment from inhalation exposure to indoor formaldehyde: A systematic review and meta-analysis. J. Hazard. Mater. 2024, 471, 134307. [Google Scholar] [CrossRef]
- Liu, N.; Fang, L.; Liu, W.; Kan, H.; Zhao, Z.; Deng, F.; Huang, C.; Zhao, B.; Zeng, X.; Sun, Y.; et al. Health effects of exposure to indoor formaldehyde in civil buildings: A systematic review and meta-analysis on the literature in the past 40 years. Build. Environ. 2023, 233, 110080. [Google Scholar] [CrossRef]
- Salthammer, T. Formaldehyde in the ambient atmosphere: From an indoor pollutant to an outdoor pollutant? Angew. Chem. Int. Ed. 2013, 52, 3320–3327. [Google Scholar] [CrossRef]
- Liu, C.; Miao, X.; Li, J. Outdoor formaldehyde matters and substantially impacts indoor formaldehyde concentrations. Build. Environ. 2019, 158, 145–150. [Google Scholar]
- Zhang, H.; Zheng, Z.; Yu, T.; Liu, C.; Qian, H.; Li, J. Seasonal and diurnal patterns of outdoor formaldehyde and impacts on indoor environments and health. Environ. Res. 2022, 205, 112550. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guidelines for Indoor Air Quality: Selected Pollutants; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Huang, S.; Wei, W.; Weschler, L.B.; Salthammer, T.; Kan, H.; Bu, Z.; Zhang, Y. Indoor formaldehyde concentrations in urban China: Preliminary study of some important influencing factors. Sci. Total Environ. 2017, 590–591, 394–405. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Mo, J.; Sundell, J.; Fan, Z.; Zhang, Y. Health risk assessment of inhalation exposure to formaldehyde and benzene in newly remodeled buildings, Beijing. PLoS ONE 2013, 8, e79553. [Google Scholar] [CrossRef]
- NBS. China Statistical Yearbook; National Bureau of Statistics—People’s Republic of China; China Statistics Press: Beijing, China, 2023. [Google Scholar]
- U.N.E. Programme. Global Status Report for Buildings and Construction 2024/2025; The United Nations Environment Programme: Nairobi, Kenya; Global Alliance for Buildings and Construction: Paris, France, 2025. [Google Scholar]
- Zhang, L.P.; Steinmaus, C.; Eastmond, D.A.; Xin, X.J.K.; Smith, M.T. Formaldehyde exposure and leukemia: A new meta-analysis and potential mechanisms. Mutat. Res./Rev. Mutat. Res. 2009, 681, 150–168. [Google Scholar] [CrossRef]
- Du, Z.; Mo, J.; Zhang, Y. Risk assessment of population inhalation exposure to volatile organic compounds and carbonyls in urban China. Environ. Int. 2014, 73, 33–45. [Google Scholar] [CrossRef]
- Fang, L.; Liu, N.; Liu, W.; Mo, J.; Zhao, Z.; Kan, H.; Deng, F.; Huang, C.; Zhao, B.; Zeng, X.; et al. Indoor formaldehyde levels in residences, schools, and offices in China in the past 30 years: A systematic review. Indoor Air 2022, 32, e13141. [Google Scholar] [CrossRef]
- Liu, N.; Liu, W.; Deng, F.; Liu, Y.; Gao, X.; Fang, L.; Chen, Z.; Tang, H.; Hong, S.; Pan, M.; et al. The burden of disease attributable to indoor air pollutants in China from 2000 to 2017. Lancet Planet. Health 2023, 7, e900–e911. [Google Scholar] [CrossRef]
- La Torre, G.; Vitello, T.; Cocchiara, R.A.; Della Rocca, C. Relationship between formaldehyde exposure, respiratory irritant effects and cancers: A review of reviews. Public Health 2023, 218, 186–196. [Google Scholar] [CrossRef]
- Salthammer, T.; Zhang, Y.; Mo, J.; Koch, H.M.; Weschler, C.J. Assessing Human Exposure to Organic Pollutants in the Indoor Environment. Angew. Chem. Int. Edit. 2018, 57, 12228–12263. [Google Scholar] [CrossRef]
- Zhang, Y.; Mo, J.; Weschler, C.J. Reducing Health Risks from Indoor Exposures in Rapidly Developing Urban China. Environ. Health Perspect. 2013, 121, 751–755. [Google Scholar] [CrossRef]
- Gong, Y.; Wei, Y.; Cheng, J.; Jiang, T.; Chen, L.; Xu, B. Health risk assessment and personal exposure to Volatile Organic Compounds (VOCs) in metro carriages—A case study in Shanghai, China. Sci. Total Environ. 2017, 574, 1432–1438. [Google Scholar] [CrossRef]
- Evtyugina, M.; Vicente, E.D.; Vicente, A.M.; Nunes, T.; Lucarelli, F.; Calzolai, G.; Nava, S.; Blanco-Alegre, C.; Calvo, A.I.; Castro, A.; et al. Air quality and particulate matter speciation in a beauty salon and surrounding outdoor environment: Exploratory study. Atmos. Pollut. Res. 2021, 12, 101174. [Google Scholar] [CrossRef]
- Lamplugh, A.; Harries, M.; Xiang, F.; Trinh, J.; Hecobian, A.; Montoya, L.D. Occupational exposure to volatile organic compounds and health risks in Colorado nail salons. Environ. Pollut. 2019, 249, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Muthalagu, A.; Serrano, V.G.; Licina, D. Human personal air pollution clouds in a naturally ventilated office during the COVID-19 pandemic. Build. Environ. 2023, 236, 110280. [Google Scholar] [CrossRef] [PubMed]
- GB/T18883-2022; Standards for Indoor Air Quality. State Administration for Market Regulation: Beijing, China, 2022. (In Chinese)
- Liang, W. Long-term indoor formaldehyde variations and health risk assessment in Chinese urban residences following renovation. Build. Environ. 2021, 206, 108402. [Google Scholar] [CrossRef]
- Pál, L.; Lovas, S.; McKee, M.; Diószegi, J.; Kovács, N.; Szűcs, S. Exposure to volatile organic compounds in offices and in residential and educational buildings in the European Union between 2010 and 2023: A systematic review and health risk assessment. Sci. Total Environ. 2024, 945, 173965. [Google Scholar] [CrossRef]
- Zhang, Z.-F.; Zhang, X.; Zhang, X.-m.; Liu, L.-Y.; Li, Y.-F.; Sun, W. Indoor occurrence and health risk of formaldehyde, toluene, xylene and total volatile organic compounds derived from an extensive monitoring campaign in Harbin, a megacity of China. Chemosphere 2020, 250, 126324. [Google Scholar] [CrossRef]
- Hänninen, O.; Knol, A.B.; Jantunen, M.; Lim, T.-A.; Conrad, A.; Rappolder, M.; Carrer, P.; Fanetti, A.-C.; Kim, R.; Buekers, J.; et al. Environmental Burden of Disease in Europe: Assessing Nine Risk Factors in Six Countries. Environ. Health Perspect. 2014, 122, 439–446. [Google Scholar] [CrossRef]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef]
- Logue, J.M.; Price, P.N.; Sherman, M.H.; Singer, B.C. A Method to Estimate the Chronic Health Impact of Air Pollutants in U.S. Residences. Environ. Health Perspect. 2012, 120, 216–222. [Google Scholar] [CrossRef]
- Levin, J.O.; Lindahl, R.; Anderson, K. A passive sampler for formaldehyde in air using 2,4-dinitrophenylhydrazine-coated glass fiber filters. Environ. Sci. Technol. 1986, 20, 1273–1276. [Google Scholar] [CrossRef]
- GB/T18204.2-2014; Examinations Methods for Public Places—Part 2: Chemical Pollutants. National Health Commission of the People’s Republic of China: Beijing, China, 2014.
- OEHHA. The Air Toxics Hot Spots Program Guidance Manual for Preparation of Health Risk Assessments; California Environmental Protection Agency: Sacramento, CA, USA, 2003. [Google Scholar]
- U.S. EPA. Supplemental Guidance for Assessing Cancer Susceptibility from Early-Life Exposure to Carcinogens; EPA/630/R-03/003F; Risk Assessment Forum; U.S. Environmental Protection Agency: Washington, DC, USA, 2005. [Google Scholar]
- Zhu, Y.; Tao, S.; Sun, J.; Wang, X.; Li, X.; Tsang, D.C.W.; Zhu, L.; Shen, G.; Huang, H.; Cai, C.; et al. Multimedia modeling of the PAH concentration and distribution in the Yangtze River Delta and human health risk assessment. Sci. Total Environ. 2019, 647, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, J.C.; Woodruff, T.J.; Morello-Frosch, R.; Axelrad, D.A. Application of health information to hazardous air pollutants modeled in EPA’s Cumulative Exposure Project. Toxicol. Ind. Health 1998, 14, 429–454. [Google Scholar] [CrossRef] [PubMed]
- Global Health Data Exchange. IHME Data: GBD Results Tool. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 13 August 2025).
- Hughes, K.; Ford, K.; Bellis, M.A.; Glendinning, F.; Harrison, E.; Passmore, J. Health and financial costs of adverse childhood experiences in 28 European countries: A systematic review and meta-analysis. Lancet Public Health 2021, 6, e848–e857. [Google Scholar] [CrossRef]
- Kunshan Bureau of Statistics. Kunshan Statistical Yearbook 2024; Kunshan Bureau of Statistics: Kunshan, China, 2024. [Google Scholar]
- Zhou, J.A.; You, Y.; Bai, Z.P.; Hu, Y.D.; Zhang, J.F.; Zhang, N. Health risk assessment of personal inhalation exposure to volatile organic compounds in Tianjin, China. Sci. Total Environ. 2011, 409, 452–459. [Google Scholar] [CrossRef]
- Shinohara, N.; Okazaki, Y.; Mizukoshi, A.; Wakamatsu, S. Exposure to benzene, toluene, ethylbenzene, xylene, formaldehyde, and acetaldehyde in and around gas stations in Japan. Chemosphere 2019, 222, 923–931. [Google Scholar] [CrossRef]
- Uchiyama, S.; Noguchi, M.; Hishiki, M.; Shimizu, M.; Kunugita, N.; Isobe, T.; Nakayama, S.F. Long-term monitoring of indoor, outdoor, and personal exposure to gaseous chemical compounds. Sci. Total Environ. 2024, 906, 167830. [Google Scholar] [CrossRef]
- Lazenby, V.; Hinwood, A.; Callan, A.; Franklin, P. Formaldehyde personal exposure measurements and time weighted exposure estimates in children. Chemosphere 2012, 88, 966–973. [Google Scholar] [CrossRef]
- Choi, Y.H.; Kim, H.J.; Sohn, J.R.; Seo, J.H. Occupational exposure to VOCs and carbonyl compounds in beauty salons and health risks associated with it in South Korea. Ecotoxicol. Environ. Saf. 2023, 256, 114873. [Google Scholar] [CrossRef]
- Yen, Y.C.; Ku, C.H.; Hsiao, T.C.; Chi, K.H.; Peng, C.Y.; Chen, Y.C. Impacts of COVID-19’s restriction measures on personal exposure to VOCs and aldehydes in Taipei City. Sci. Total Environ. 2023, 880, 163275. [Google Scholar] [CrossRef]
- Abelmann, A.; McEwen, A.R.; Lotter, J.T.; Maskrey, J.R. Survey of 24-h personal formaldehyde exposures in geographically distributed urban office workers in the USA. Environ. Sci. Pollut. Res. 2020, 27, 17250–17257. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Zhang, J.; Song, W.; Wang, K.; Zhang, B. Formaldehyde exposure in indoor air from public places and its associated health risks in Kunshan city, China. Asia Pac. J. Public Health 2018, 30, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Mu, C.; Zhai, J.; Li, J.; Zou, T. Characteristics and personal exposures of carbonyl compounds in the subway stations and in-subway trains of Shanghai, China. J. Hazard. Mater. 2010, 183, 574–582. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Roh, J.; Park, W.M. Evaluation of PM10, CO2, airborne bacteria, TVOCs, and formaldehyde in facilities for susceptible populations in South Korea. Environ. Pollut. 2018, 242, 700–708. [Google Scholar] [CrossRef]
- Pang, X.; Mu, Y. Characteristics of carbonyl compounds in public vehicles of Beijing city: Concentrations, sources, and personal exposures. Atmos. Environ. 2007, 41, 1819–1824. [Google Scholar] [CrossRef]
- Shiohara, N.; Fernández-Bremauntz, A.A.; Blanco Jiménez, S.; Yanagisawa, Y. The commuters’ exposure to volatile chemicals and carcinogenic risk in Mexico City. Atmos. Environ. 2005, 39, 3481–3489. [Google Scholar] [CrossRef]
- Wang, Z.; Yu, T.; Ye, J.; Tian, L.; Lin, B.; Leng, W.; Liu, C. A novel low sampling rate and cost-efficient active sampler for medium/long-term monitoring of gaseous pollutants. J. Hazard. Mater. 2024, 461, 132583. [Google Scholar] [CrossRef]
- Alves, C.; Cipoli, Y.; Furst, L.; Vicente, E.; Ituamba, J.; Leitao, A. Indoor/outdoor air quality in primary schools in Luanda. Environ. Pollut. 2025, 374, 126244. [Google Scholar] [CrossRef]
- Kanjanasiranont, N.; Prueksasit, T.; Morknoy, D.; Tunsaringkarn, T.; Sematong, S.; Siriwong, W.; Zapaung, K.; Rungsiyothin, A. Determination of ambient air concentrations and personal exposure risk levels of outdoor workers to carbonyl compounds and BTEX in the inner city of Bangkok, Thailand. Atmos. Pollut. Res. 2016, 7, 268–277. [Google Scholar] [CrossRef]
- Norback, D.; Hashim, J.H.; Hashim, Z.; Ali, F. Volatile organic compounds (VOC), formaldehyde and nitrogen dioxide (NO2) in schools in Johor Bahru, Malaysia: Associations with rhinitis, ocular, throat and dermal symptoms, headache and fatigue. Sci. Total Environ. 2017, 592, 153–160. [Google Scholar] [CrossRef]
- Jia, C.; Foran, J. Air toxics concentrations, source identification, and health risks: An air pollution hot spot in southwest Memphis, TN. Atmos. Environ. 2013, 81, 112–116. [Google Scholar] [CrossRef]
- Ba’ez, A.; Padilla, H.; Garc’ıa, R.ı.; Torres, M.d.C.; Rosas, I.; Belmont, R.l. Carbonyl levels in indoor and outdoor air in Mexico City and Xalapa, Mexico. Sci. Total Environ. 2003, 302, 211–226. [Google Scholar] [CrossRef]
- Loh, M.M.; Levy, J.I.; Spengler, J.D.; Houseman, E.A.; Bennett, D.H. Ranking cancer risks of organic hazardous air pollutants in the United States. Environ. Health Perspect. 2007, 115, 1160–1168. [Google Scholar] [CrossRef]
- Ye, J.; Wang, Z.; Yu, T.; Zhuang, W.; Lai, W.; Tian, L.; Leng, W.; Song, Y.; Huang, S.; Zhang, Y.; et al. Long-term characteristics of formaldehyde concentrations in four Chinese residences and estimation of annual average. Build. Environ. 2025, 278, 113024. [Google Scholar] [CrossRef]
- Yang, M.; Ye, J.; Yu, T.; Song, Y.; Qian, H.; Liu, T.; Chen, Y.; Wang, J.; Cao, S.-J.; Liu, C. Smartphone-based colorimetric detection of formaldehyde in the air. Build. Simul. 2024, 17, 2007–2015. [Google Scholar] [CrossRef]
- U.S. EPA. Exposure Factors Handbook: 2011 Edition (Final); Envrionmental Protection Agency: Washington, DC, USA, 2011. [Google Scholar]
- Hadei, M.; Hopke, P.K.; Rafiee, M.; Rastkari, N.; Yarahmadi, M.; Kermani, M. Indoor and outdoor concentrations of BTEX and formaldehyde in Tehran, Iran: Effects of building characteristics and health risk assessment. Environ. Sci. Pollut. Res. 2018, 25, 27423–27437. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.H.; Cheng, Y.; Bai, Y.; Ho, K.F.; Dai, W.T.; Cao, J.J.; Lee, S.C.; Huang, Y.; Ip, H.S.S.; Deng, W.J.; et al. Risk Assessment of Indoor Formaldehyde and Other Carbonyls in Campus Environments in Northwestern China. Aerosol. Air Qual. Res. 2016, 16, 1967–1980. [Google Scholar] [CrossRef]
- Rovira, J.; Roig, N.; Nadal, M.; Schuhmacher, M.; Domingo, J.L. Human health risks of formaldehyde indoor levels: An issue of concern. J. Environ. Sci. Health Part A 2016, 51, 357–363. [Google Scholar] [CrossRef]
- Villanueva, F.; Tapia, A.; Amo-Salas, M.; Notario, A.; Cabanas, B.; Martínez, E. Levels and sources of volatile organic compounds including carbonyls in indoor air of homes of Puertollano, the most industrialized city in central Iberian Peninsula. Estimation of health risk. Int. J. Hyg. Environ. Health 2015, 218, 522–534. [Google Scholar] [CrossRef]
- Zeng, L.; Li, K.; Guo, H.; Zhou, B.; Lyu, X.; Huo, Y.; Uhde, E.; Yang, J.; Zeren, Y.; Lu, H.; et al. Contributions of indoor household activities to inhalation health risks induced by gaseous air pollutants in Hong Kong home. Aerosol Air Qual. Res. 2023, 23, 230063. [Google Scholar] [CrossRef]
- Bu, Z.; Mmereki, D.; Wang, J.; Dong, C. Exposure to commonly-used phthalates and the associated health risks in indoor environment of urban China. Sci. Total Environ. 2019, 658, 843–853. [Google Scholar] [CrossRef]
- Office of the Leading Group of Jiangsu province for the Seventh National Population Census (OJC). Jiangsu Population Census Yearbook 2020; China Statistics Press: Beijing, China.
- Office of the Leading Group of the State Council for the Seventh National Population Census (OSC). China Population Census Yearbook 2020; China Statistics Press: Beijing, China.
- Duan, X. Research Methods of Exposure Factors and its Application in Environmental Health Risk Assessment; Science Press: Beijing, China, 2012. (in Chinese) [Google Scholar]
- Duan, X. Highlights of the Chinese Exposure Factors Handbook—Children; Environment Press: Beijing, China, 2016. (In Chinese) [Google Scholar]
- Fang, L. Indoor Airborne VOCs: Evaluation of Disease Burden and Control Effects. Ph.D. Thesis, Tsinghua University, Beijing, China, 2020. [Google Scholar]
- Huang, Y.; Su, T.; Wang, L.; Wang, N.; Xue, Y.; Dai, W.; Lee, S.C.; Cao, J.; Ho, S.S.H. Evaluation and characterization of volatile air toxics indoors in a heavy polluted city of northwestern China in wintertime. Sci. Total Environ. 2019, 662, 470–480. [Google Scholar] [CrossRef]
- Liang, X.; Ji, X.; Geng, Z.; Zhang, H.; Sun, Q.; Zhao, P.; Zhu, C. Indoor formaldehyde pollution characteristics in newly decorated residences in Kunshan of Jiangsu Province. J. Environ. Occup. Med. 2020, 37, 994–998. (In Chinese) [Google Scholar]
- McKone, T.E. CalTOX, A Multimedia Total-Exposure Model for Hazardous-Wastes 232 Sites Part II: The Dynamic Multimedia Transport and Transformation Model; Lawerence 233 Livermore National Laboratory, Department of Toxic Substances Control, California Environmental Protection Agency: Livermore, CA, USA, 1993. [Google Scholar]
- MEP. Exposure Factors Handbook of Chinese Population—Adults; Environment Press: Beijing, China, 2013. (In Chinese) [Google Scholar]

| Category | Number (n) |
|---|---|
| Sex | |
| Male | 30 |
| Female | 82 |
| Age | |
| <30 years | 15 |
| 30~45 years | 60 |
| >45 years | 37 |
| Working places | |
| Hotel | 46 |
| Mall | 29 |
| Natatorium | 19 |
| Salon | 8 |
| Bus station | 10 |
| Annual household income (RMB) | |
| <40 thousand | 25 |
| 40~60 thousand | 43 |
| 60~100 thousand | 27 |
| >100 thousand | 17 |
| Ocular irritation during the last month | |
| Yes | 32 |
| No | 80 |
| Respiratory irritation during the last month | |
| Yes | 42 |
| No | 70 |
| Country | Time | Subjects | Sampling Method | Sampling Duration | Personal Level (μg/m3) | |
|---|---|---|---|---|---|---|
| Shinohara et al. (2019) [46] | Japan | May, 2015; February, 2016 | Gas station workers | Personal pumps | 2 h | 5.1 (spring) 11.6 (winter) |
| Uchiyama et al. (2024) [47] | Japan | March, 2017–March, 2022 | Residents | Passive sampler | 1 week | 24 |
| Lazenby et al. (2012) [48] | Australia | November–December, 2006; June–August, 2007 | Children (9–12 years old) | Passive sampling badge | 24 h | 13.6 |
| Yang et al. (2023) [28] | Switzerland | November, 2020 | Office workers | Passive sampling badge | Daily working hours | 74.7 |
| Choi et al. (2023) [49] | Korea | November–December, 2021 | Salon technicians | Passive sampling badge | 8 h | 49.7 |
| Yen et al. (2023) [50] | China | May–August, 2021; February–March, 2022 | University students | Passive sampler | 3 days | 16.4~21.8 |
| Abelmann et al. (2020) [51] | USA | October, 2017 | Office workers | Passive sampling badge | 24 h | 12 |
| This study | China | June–August, 2024 | Working adults | Passive sampling badge | 24 h | 36.0 |
| Public Places (n = 84) | Residences (n = 84) | Vehicles (n = 16) | Outdoor (n = 16) | |
|---|---|---|---|---|
| Formaldehyde (μg/m3) | 46.1 ± 16.1 | 41.3 ± 61.7 | 28.2 ± 19.7 | 16.1 ± 6.8 |
| Temperature (°C) | 25.4 ± 0.9 | 27.8 ± 2.7 | 27.9 ± 2.3 | 29.8 ± 2.9 |
| Relative humidity | 75.0 ± 10.5% | 71.9 ± 10.5% | 51.0 ± 13.7% | 71.4 ± 16.6% |
| Microenvironment | Country | Sampling Site | Concentration |
|---|---|---|---|
| Public/office | |||
| Shinohara et al. (2019) [46] | Japan | Office | 10.1 (spring) 24.1 (winter) |
| Feng et al. (2010) [53] | China | Subway station | 21.2–31.7 |
| Yang et al. (2023) [28] | Switzerland | Office | 58 |
| Evtyugina et al. (2021) [26] | Spain | Salon | 11.5 |
| Lamplugh et al. (2019) [27] | USA | Salon | 5.3–20.6 |
| Hwang et al. (2018) [54] | South Korea | Hospital, personal care center | 24.4 |
| This study | China | Hotel, salon | 46.1 |
| Commuting | |||
| Feng et al. (2010) [53] | China | Metro carriage | 12.3 |
| Gong et al. (2017) [25] | China | Metro carriage | 4.5–23.3 |
| Pang et al. (2007) [55] | China | Vehicle | 16–40 |
| Shinohara et al. (2005) [56] | Mexico | Vehicle, metro | 19.4–40.2 |
| This study | China | Vehicle | 28.2 |
| Outdoor | |||
| Shinohara et al. (2019) [46] | Japan | Gas station | 4.3 (spring) 6.0 (winter) |
| Feng et al. (2010) [53] | China | Roadside | 10.8 |
| Wang et al. (2024) [57] | China | Urban area | 14.1 |
| Alves et al. (2025) [58] | Angola | School | 2.3 |
| Kanjanasiranont et al. (2015) [59] | Thailand | Roadside | 20.1 |
| Norbäck et al. (2017) [60] | Malaysia | School | 5.5 |
| Jia et al. (2013) [61] | USA | Residential region | 2.97 |
| Baez et al. (2003) [62] | Mexico | Metropolitan zone | 4–32 |
| This study | China | Urban area | 16.1 |
| Disability-Adjusted Life Years (DALYs) | Economic Losses (Million CNY) | Change in Losses a | |||||
|---|---|---|---|---|---|---|---|
| <5 Years | 5–19 Years | 20–59 Years | ≥60 Years | Total | |||
| Baseline | 60 (12–146) | 168 (63–344) | 217 (64–502) | 125 (23–338) | 571 (258–1055) | 136 (62–245) | / |
| 15% reduction | 55 (11–143) | 153 (56–329) | 194 (55–475) | 113 (20–327) | 515 (229–995) | 123 (55–232) | −9.6% |
| 30% reduction | 49 (9–137) | 137 (49–308) | 169 (47–433) | 99 (18–311) | 454 (200–926) | 108 (48–215) | −20.6% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mo, D.; Zhang, H.; Wang, Y.; Tuo, F.; Chen, M.; Cao, Z.; Xu, Y.; Lin, L.; Liang, X.; Mmereki, D.; et al. Formaldehyde Exposure and Associated Health Burdens Apportioned to Residential and Public Places Based on Personal and Environmental Measurements. Atmosphere 2025, 16, 1165. https://doi.org/10.3390/atmos16101165
Mo D, Zhang H, Wang Y, Tuo F, Chen M, Cao Z, Xu Y, Lin L, Liang X, Mmereki D, et al. Formaldehyde Exposure and Associated Health Burdens Apportioned to Residential and Public Places Based on Personal and Environmental Measurements. Atmosphere. 2025; 16(10):1165. https://doi.org/10.3390/atmos16101165
Chicago/Turabian StyleMo, Donghui, Huimin Zhang, Yuan Wang, Fei Tuo, Mengyao Chen, Zhen Cao, Yirui Xu, Lvyan Lin, Xiaojun Liang, Daniel Mmereki, and et al. 2025. "Formaldehyde Exposure and Associated Health Burdens Apportioned to Residential and Public Places Based on Personal and Environmental Measurements" Atmosphere 16, no. 10: 1165. https://doi.org/10.3390/atmos16101165
APA StyleMo, D., Zhang, H., Wang, Y., Tuo, F., Chen, M., Cao, Z., Xu, Y., Lin, L., Liang, X., Mmereki, D., Li, T., & Bu, Z. (2025). Formaldehyde Exposure and Associated Health Burdens Apportioned to Residential and Public Places Based on Personal and Environmental Measurements. Atmosphere, 16(10), 1165. https://doi.org/10.3390/atmos16101165








