Dust Storms Are Associated with an Increase in Outpatient Visits for Rheumatoid Arthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Model
- is the daily number of RA outpatient visits.
- Trend is the time trend variable.
- is a dummy variable for the jth day after a dust storm.
- denotes the number of daily RA outpatient visits on the jth day before day t.
- Xt represents controlled exogenous variables such as SO2, and O3.
- coefficient terms.
- εt is the error term.
3. Results
3.1. Descriptive Statistics
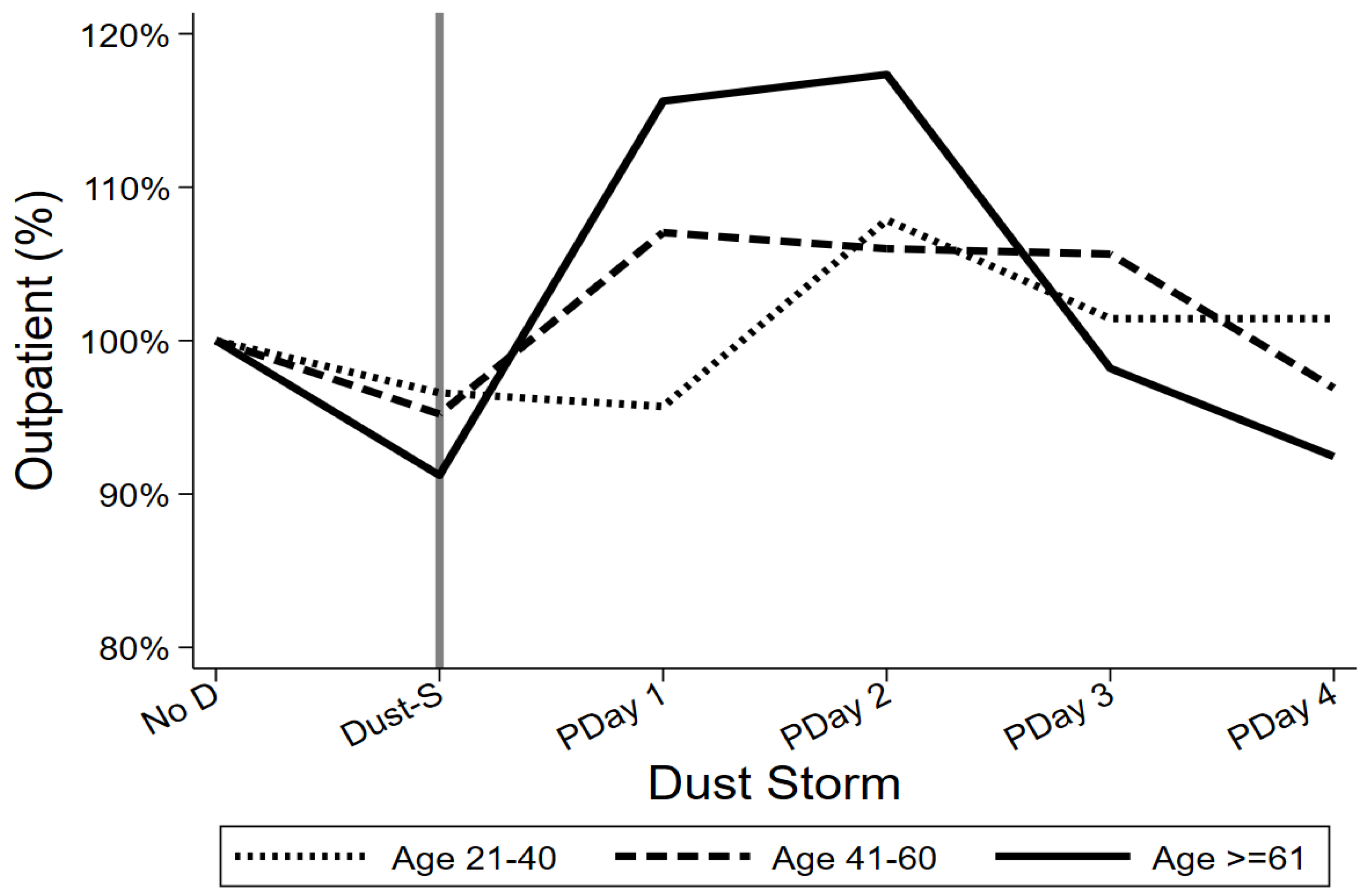
3.2. Gender- and Age-Specific Patterns
3.3. Contrast Analysis
3.4. Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smolen, J.S.; Aletaha, D.; McInnes, I.B. Rheumatoid arthritis. Lancet 2016, 388, 2023–2038. [Google Scholar] [CrossRef]
- Alamanos, Y.; Drosos, A.A. Epidemiology of adult rheumatoid arthritis. Autoimmun. Rev. 2005, 4, 130–136. [Google Scholar] [CrossRef]
- Doran, M.F.; Pond, G.R.; Crowson, C.S.; O’Fallon, W.M.; Gabriel, S.E. Trends in incidence and mortality in rheumatoid arthritis in Rochester, Minnesota, over a forty-year period. Arthritis Rheum. 2002, 46, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Rasch, E.K.; Hirsch, R.; Paulose-Ram, R.; Hochberg, M.C. Prevalence of rheumatoid arthritis in persons 60 years of age and older in the United States: Effect of different methods of case classification. Arthritis Rheum. 2003, 48, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Kato, E.; Sawada, T.; Tahara, K.; Hayashi, H.; Tago, M.; Mori, H.; Tohma, S. The age at onset of rheumatoid arthritis is increasing in Japan: A nationwide database study. Int. J. Rheum. Dis. 2017, 20, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Deane, K.D.; Demoruelle, M.K.; Kelmenson, L.B.; Kuhn, K.A.; Norris, J.M.; Holers, V.M. Genetic and environmental risk factors for rheumatoid arthritis. Best. Pract. Res. Clin. Rheumatol. 2017, 31, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Catrina, A.I.; Deane, K.D.; Scher, J.U. Gene, environment, microbiome and mucosal immune tolerance in rheumatoid arthritis. Rheumatology 2016, 55, 391–402. [Google Scholar] [CrossRef]
- Anderson, R.; Meyer, P.W.; Ally, M.M.; Tikly, M. Smoking and Air Pollution as Pro-Inflammatory Triggers for the Development of Rheumatoid Arthritis. Nicotine Tob. Res. 2016, 18, 1556–1565. [Google Scholar] [CrossRef]
- Sigaux, J.; Biton, J.; André, E.; Semerano, L.; Boissier, M.C. Air pollution as a determinant of rheumatoid arthritis. Joint Bone Spine. 2019, 86, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Bang, S.Y.; Lee, K.H.; Cho, S.K.; Lee, H.S.; Lee, K.W.; Bae, S.C. Smoking increases rheumatoid arthritis susceptibility in individuals carrying the HLA-DRB1 shared epitope, regardless of rheumatoid factor or anti-cyclic citrullinated peptide antibody status. Arthritis Rheum. 2010, 62, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, D. Impact of smoking as a risk factor for developing rheumatoid arthritis: A meta-analysis of observational studies. Ann. Rheum. Dis. 2010, 69, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Damgaard, D.; Nielsen, M.F.B.; Gaunsbaek, M.Q.; Palarasah, Y.; Svane-Knudsen, V.; Nielsen, C.H. Smoking is associated with increased levels of extracellular peptidylarginine deiminase 2 (PAD2) in the lungs. Clin. Exp. Rheumatol. 2015, 33, 405–408. [Google Scholar] [PubMed]
- Lugli, E.B.; Correia, R.E.; Fischer, R.; Lundberg, K.; Bracke, K.R.; Montgomery, A.B.; Venables, P.J. Expression of citrulline and homocitrulline residues in the lungs of non-smokers and smokers: Implications for autoimmunity in rheumatoid arthritis. Arthritis Res. Ther. 2015, 17, 9. [Google Scholar] [CrossRef]
- Alex, A.M.; Kunkel, G.; Sayles, H.; Flautero Arcos, J.D.; Mikuls, T.R.; Kerr, G.S. Exposure to ambient air pollution and autoantibody status in rheumatoid arthritis. Clin. Rheumatol. 2020, 39, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.Y.; Cheng, M.H.; Chen, C.C. Effects of Asian dust storm events on hospital admissions for congestive heart failure in Taipei, Taiwan. J. Toxicol. Environ. Health A 2009, 72, 324–328. [Google Scholar] [CrossRef]
- Chan, C.C.; Chuang, K.J.; Chen, W.J.; Chang, W.T.; Lee, C.T.; Peng, C.M. Increasing cardiopulmonary emergency visits by long-range transported Asian dust storms in Taiwan. Environ. Res. 2008, 106, 393–400. [Google Scholar] [CrossRef]
- Cha, S.; Srinivasan, S.; Jang, J.H.; Lee, D.; Lim, S.; Kim, K.S.; Seo, T. Metagenomic Analysis of Airborne Bacterial Community and Diversity in Seoul, Korea, during December 2014 Asian Dust Event. PLoS ONE 2017, 12, e0170693. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Liu, T.C.; Keller, J.; Lin, H.C. Asian dust storm events are associated with an acute increase in stroke hospitalisation. J. Epidemiol. Community Health 2013, 67, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Chen, C.S.; Lin, C.L. The threat of Asian dust storms on asthma patients: A population-based study in Taiwan. Glob. Public. Health 2014, 9, 1040–1052. [Google Scholar] [CrossRef]
- Liu, T.C.; Tang, H.H.; Lei, S.Y.; Peng, Y.I. Asian dust storms result in a higher risk of the silicosis hospital admissions. J. Environ. Health Sci. Eng. 2022, 20, 305–314. [Google Scholar] [CrossRef]
- Kang, J.H.; Keller, J.J.; Chen, C.S.; Lin, H.C. Asian dust storm events are associated with an acute increase in pneumonia hospitalization. Ann. Epidemiol. 2012, 22, 257–263. [Google Scholar] [CrossRef]
- Yang, C.Y.; Chen, Y.S.; Chiu, H.F.; Goggins, W.B. Effects of Asian dust storm events on daily stroke admissions in Taipei, Taiwan. Environ. Res. 2005, 99, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.-T.; Liu, J.-F.; Chiang, Y.-C.; Chen, P.-C.; Chiang, M.-H.; Shih, H.-N.; Chang, P.-J.; Lee, C.-W. Particulate matter exposure aggravates osteoarthritis severity. Clin. Sci. 2019, 133, 2171–2187. [Google Scholar] [CrossRef]
- Bai, L.; Su, X.; Zhao, D.; Zhang, Y.; Cheng, Q.; Zhang, H.; Wang, S.; Xie, M.; Su, H. Exposure to traffic-related air pollution and acute bronchitis in children: Season and age as modifiers. J. Epidemiol. Community Health 2018, 72, 426–433. [Google Scholar] [CrossRef]
- Yuan, Q.; Chen, Y.; Li, X.; Zhang, Z.; Chu, H. Ambient fine particulate matter (PM(2.5)) induces oxidative stress and pro-inflammatory response via up-regulating the expression of CYP1A1/1B1 in human bronchial epithelial cells in vitro. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2019, 839, 40–48. [Google Scholar] [CrossRef]
- van Eeden, S.F.; Sin, D.D. Chronic obstructive pulmonary disease: A chronic systemic inflammatory disease. Respiration 2008, 75, 224–238. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.T.; Lin, Y.C.; Chio, C.P.; Wang, C.F.; Kuo, C.Y. Characteristics of aerosols collected in central Taiwan during an Asian dust event in spring 2000. Chemosphere 2005, 61, 1439–1450. [Google Scholar] [CrossRef] [PubMed]
- Patberg, W.R.; Rasker, J.J. Weather effects in rheumatoid arthritis: From controversy to consensus. A review. J. Rheumatol. 2004, 31, 1327–1334. [Google Scholar]
- Pradeepkiran, J.A. Insights of rheumatoid arthritis risk factors and associations. J. Transl. Autoimmun. 2019, 2, 100012. [Google Scholar] [CrossRef]

| Average Daily RA Outpatient Visits | |||||||
|---|---|---|---|---|---|---|---|
| No Dust Storm | Day of Dust Storm | Post-Dust Day 1 | Post-Dust Day 2 | Post-Dust Day 3 | Post-Dust Day 4 | Observations (%) | |
| Total | 71.50 | 66.92 | 78.39 | 79.56 | 72.83 | 68.22 | 182,899 (100.00%) |
| Gender | |||||||
| Male | 15.89 | 15.49 | 18.94 | 16.06 | 15.50 | 13.56 | 40,626 (22.21%) |
| Female | 55.61 | 51.43 | 59.44 | 63.50 | 57.33 | 54.67 | 142,273 (77.79%) |
| Age | |||||||
| 21–40 | 7.78 | 7.51 | 7.44 | 8.39 | 7.89 | 7.89 | 19,887 (10.87%) |
| 41–60 | 31.82 | 30.30 | 34.06 | 33.72 | 33.61 | 30.83 | 81,388 (44.50%) |
| ≥61 | 31.91 | 29.11 | 36.89 | 37.44 | 31.33 | 29.5 | 81,624 (44.63%) |
| Number of Daily RA Outpatient Visits | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | ||||||||||
| Independent Variable | B | SE | p Value | B | SE | p Value | B | SE | p Value | |||
| Intercept | −31.9486 | 11.5864 | 0.0060 | ** | −9.2184 | 3.4727 | 0.0080 | ** | −26.3849 | 9.3630 | 0.0050 | ** |
| Time since dust storm | ||||||||||||
| Day of dust storm | −8.0146 | 6.1632 | 0.1930 | −0.8260 | 1.4500 | 0.5690 | −7.4038 | 4.8788 | 0.1290 | |||
| Post-dust day 1 | 9.9511 | 6.8482 | 0.1460 | 3.6872 | 1.7164 | 0.0320 | * | 5.9697 | 5.3157 | 0.2610 | ||
| Post-dust day 2 | 7.8515 | 10.9950 | 0.4750 | 0.1625 | 3.3663 | 0.9620 | 7.7731 | 7.5873 | 0.3060 | |||
| Post-dust day 3 | −5.5288 | 7.1822 | 0.4410 | −1.1538 | 2.0556 | 0.5750 | −3.5710 | 5.6192 | 0.5250 | |||
| Post-dust day 4 | 0.8573 | 8.6572 | 0.9210 | −1.4477 | 2.3987 | 0.5460 | 1.6578 | 6.3635 | 0.7940 | |||
| Temperature | 0.8059 | 0.0916 | 0.0000 | *** | 0.2207 | 0.0299 | 0.0000 | *** | 0.6078 | 0.0753 | 0.0000 | *** |
| Humidity | 0.1905 | 0.1089 | 0.0800 | 0.0400 | 0.0324 | 0.2180 | 0.1623 | 0.0881 | 0.0650 | |||
| Rainfall | −1.2244 | 1.1345 | 0.2800 | −0.1737 | 0.3570 | 0.6270 | −1.0949 | 0.9115 | 0.2300 | |||
| SO2 | 6.3050 | 0.6534 | 0.0000 | *** | 1.7411 | 0.1952 | 0.0000 | *** | 5.0236 | 0.5273 | 0.0000 | *** |
| O3 | −0.0266 | 0.0621 | 0.6680 | −0.0243 | 0.0187 | 0.1930 | −0.0225 | 0.0505 | 0.6560 | |||
| Trend | 1.1431 | 0.0627 | 0.0000 | *** | 0.2638 | 0.0201 | 0.0000 | *** | 0.9023 | 0.0515 | 0.0000 | *** |
| MA1 | 0.1038 | 0.0168 | 0.0000 | *** | 0.1153 | 0.0194 | 0.0000 | *** | 0.1000 | 0.0175 | 0.0000 | *** |
| MA2 | −0.4895 | 0.0178 | 0.0000 | *** | −0.2936 | 0.0192 | 0.0000 | *** | −0.4600 | 0.0182 | 0.0000 | *** |
| Number of Daily RA Outpatient Visits | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 21–40 | 41–60 | ≥61 | ||||||||||
| Independent Variable | B | SE | p Value | B | SE | p Value | B | SE | p Value | |||
| Intercept | −2.0692 | 2.0735 | 0.3180 | −9.6212 | 5.6262 | 0.0870 | −27.0921 | 6.2422 | 0.0000 | *** | ||
| Time since dust storm | ||||||||||||
| Day of dust storm | −0.3984 | 0.8270 | 0.6300 | −3.4476 | 2.8730 | 0.2300 | −4.0518 | 2.7657 | 0.1430 | |||
| Post-dust day 1 | −0.0417 | 1.1997 | 0.9720 | 3.4115 | 3.2733 | 0.2970 | 6.1803 | 3.0370 | 0.0420 | * | ||
| Post-dust day 2 | 0.6337 | 1.3752 | 0.6450 | 1.8200 | 5.2086 | 0.7270 | 5.5197 | 4.4043 | 0.2100 | |||
| Post-dust day 3 | −0.0079 | 0.9761 | 0.9940 | −0.9062 | 3.4209 | 0.7910 | −2.8862 | 3.4281 | 0.4000 | |||
| Post-dust day 4 | 0.3864 | 1.4128 | 0.7840 | 0.6251 | 3.8322 | 0.8700 | −0.9059 | 3.7836 | 0.8110 | |||
| Temperature | 0.1155 | 0.0196 | 0.0000 | *** | 0.4457 | 0.0455 | 0.0000 | *** | 0.2815 | 0.0526 | 0.0000 | *** |
| Humidity | 0.0181 | 0.0196 | 0.3550 | 0.0644 | 0.0527 | 0.2210 | 0.1328 | 0.0587 | 0.0240 | * | ||
| Rainfall | −0.1750 | 0.2206 | 0.4280 | −0.1802 | 0.4989 | 0.7180 | −0.9077 | 0.6366 | 0.1540 | |||
| SO2 | 0.7693 | 0.1139 | 0.0000 | *** | 3.0136 | 0.3167 | 0.0000 | *** | 3.3433 | 0.3479 | 0.0000 | *** |
| O3 | −0.0178 | 0.0115 | 0.1210 | −0.0130 | 0.0300 | 0.6640 | −0.0292 | 0.0344 | 0.3970 | |||
| Trend | 0.0785 | 0.0128 | 0.0000 | *** | 0.3527 | 0.0302 | 0.0000 | *** | 0.7529 | 0.0371 | 0.0000 | *** |
| MA1 | 0.1095 | 0.0212 | 0.0000 | *** | 0.0581 | 0.0187 | 0.0020 | ** | 0.1692 | 0.0172 | 0.0000 | *** |
| MA2 | −0.1196 | 0.0197 | 0.0000 | *** | −0.4175 | 0.0182 | 0.0000 | *** | −0.3877 | 0.0192 | 0.0000 | *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.; Chen, C.-S.; Liu, T.-C. Dust Storms Are Associated with an Increase in Outpatient Visits for Rheumatoid Arthritis. Atmosphere 2024, 15, 1059. https://doi.org/10.3390/atmos15091059
Chen C, Chen C-S, Liu T-C. Dust Storms Are Associated with an Increase in Outpatient Visits for Rheumatoid Arthritis. Atmosphere. 2024; 15(9):1059. https://doi.org/10.3390/atmos15091059
Chicago/Turabian StyleChen, Conmin, Chin-Shyan Chen, and Tsai-Ching Liu. 2024. "Dust Storms Are Associated with an Increase in Outpatient Visits for Rheumatoid Arthritis" Atmosphere 15, no. 9: 1059. https://doi.org/10.3390/atmos15091059
APA StyleChen, C., Chen, C.-S., & Liu, T.-C. (2024). Dust Storms Are Associated with an Increase in Outpatient Visits for Rheumatoid Arthritis. Atmosphere, 15(9), 1059. https://doi.org/10.3390/atmos15091059





