Mortality Associated with Extreme Heat in Washington State: The Historical and Projected Public Health Burden
Abstract
:1. Introduction
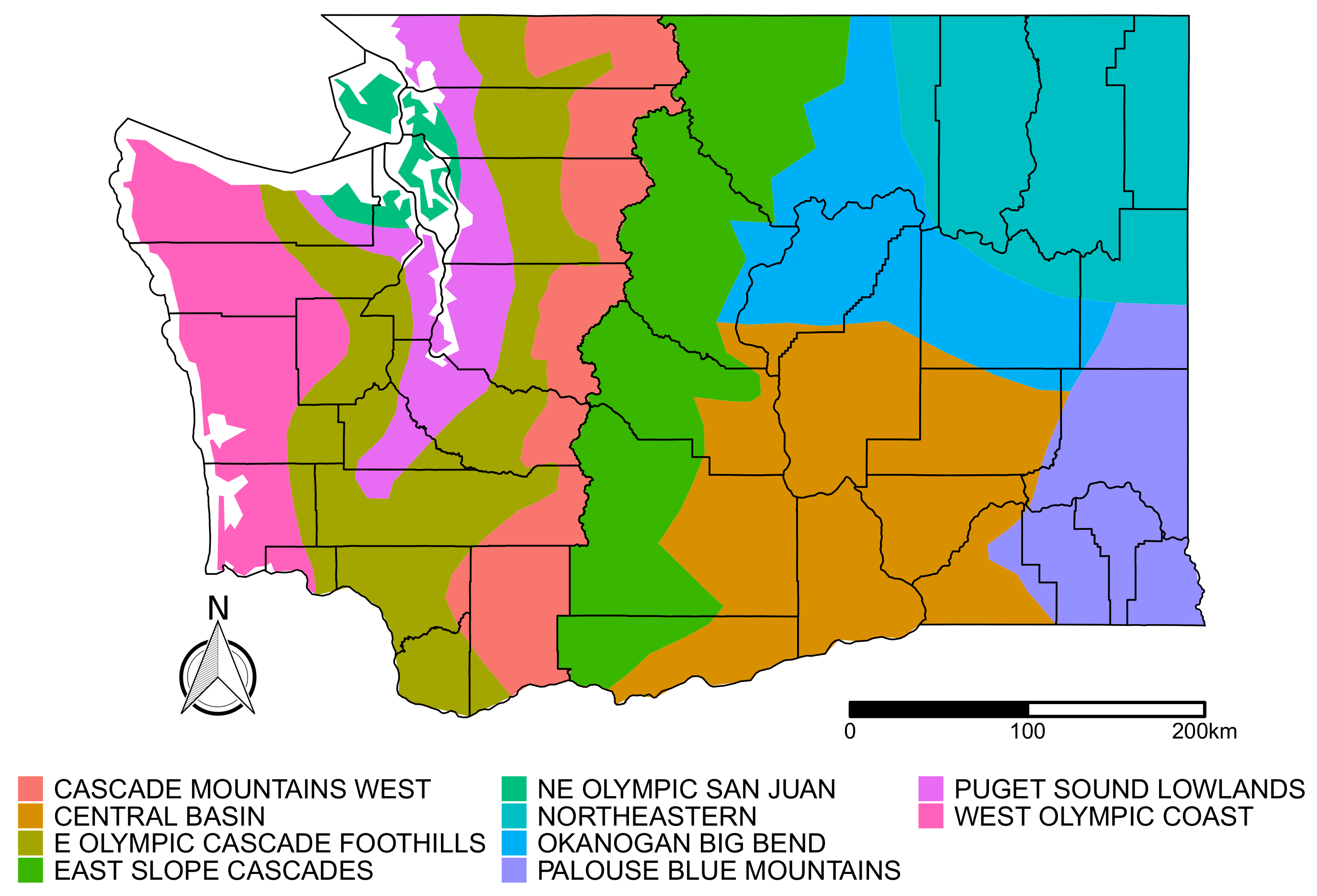
2. Materials and Methods
2.1. Data Sources
2.1.1. Mortality Data
2.1.2. Historical Meteorological Data
2.1.3. Climate Projections
2.2. Exposure Assessment
2.3. Case-Crossover Analysis for the Historical Period
2.4. Projected Heat-Attributable Deaths Due to Climate Change
3. Results
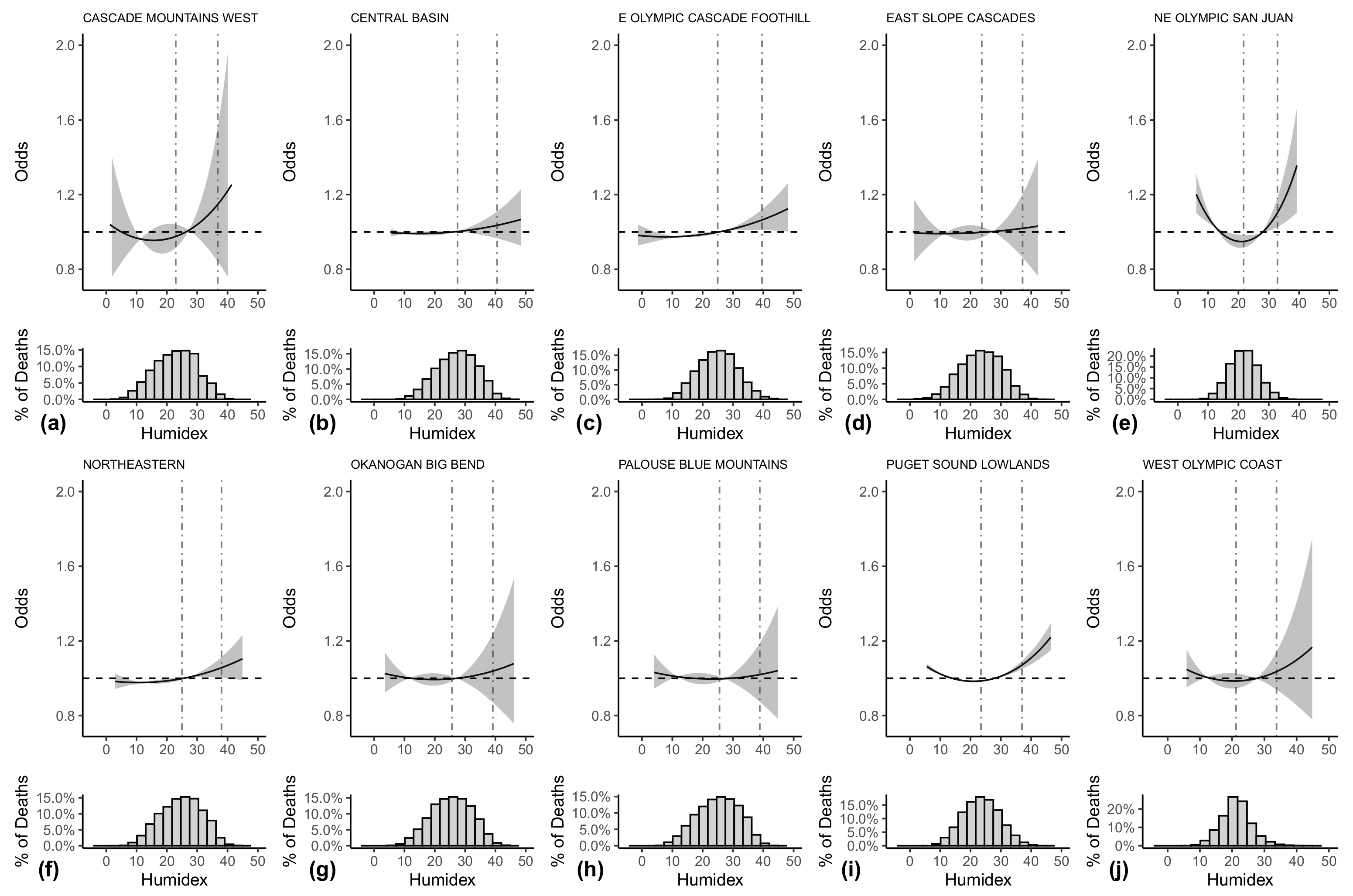
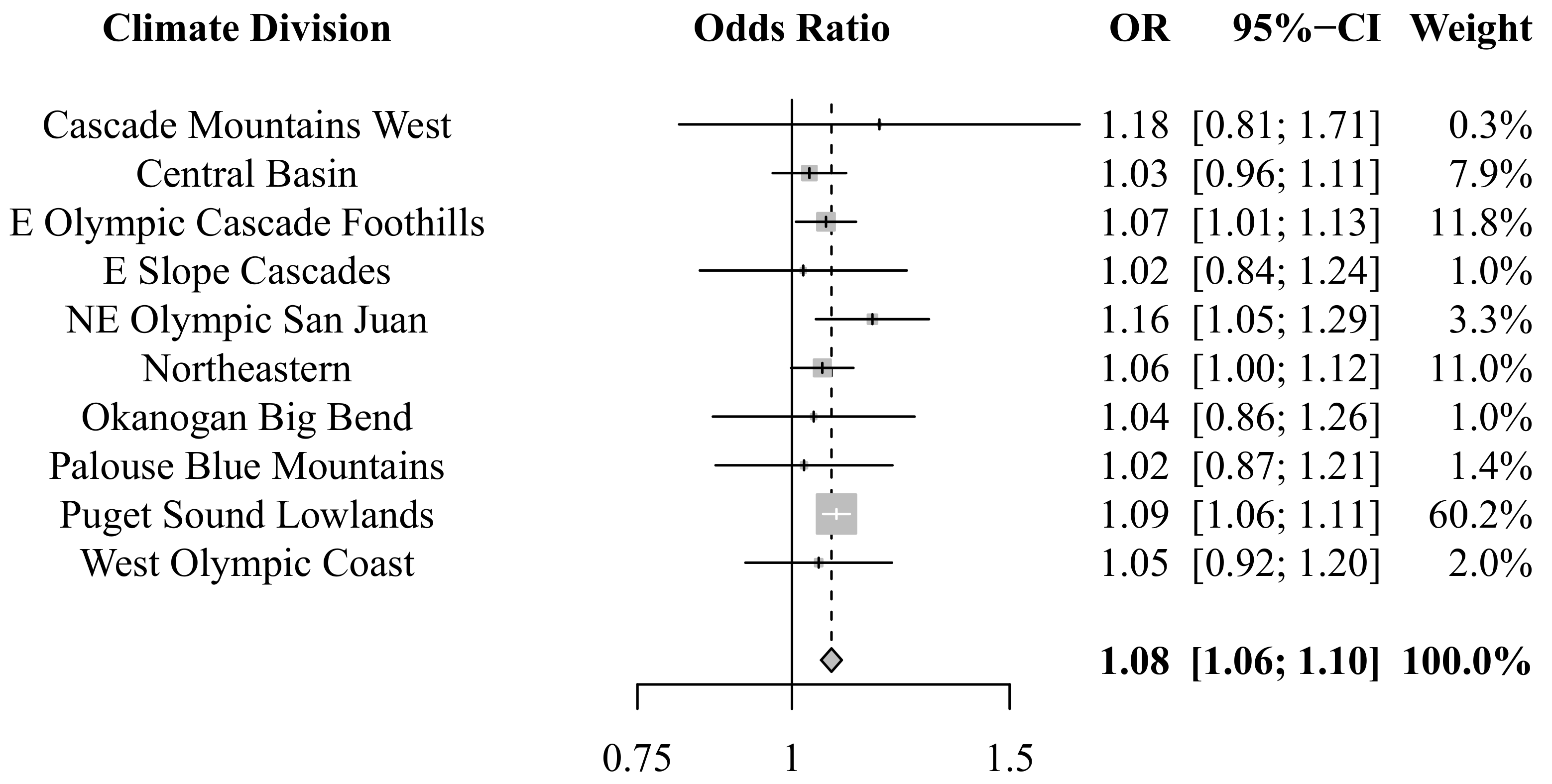
3.1. Historical Public Health Burden
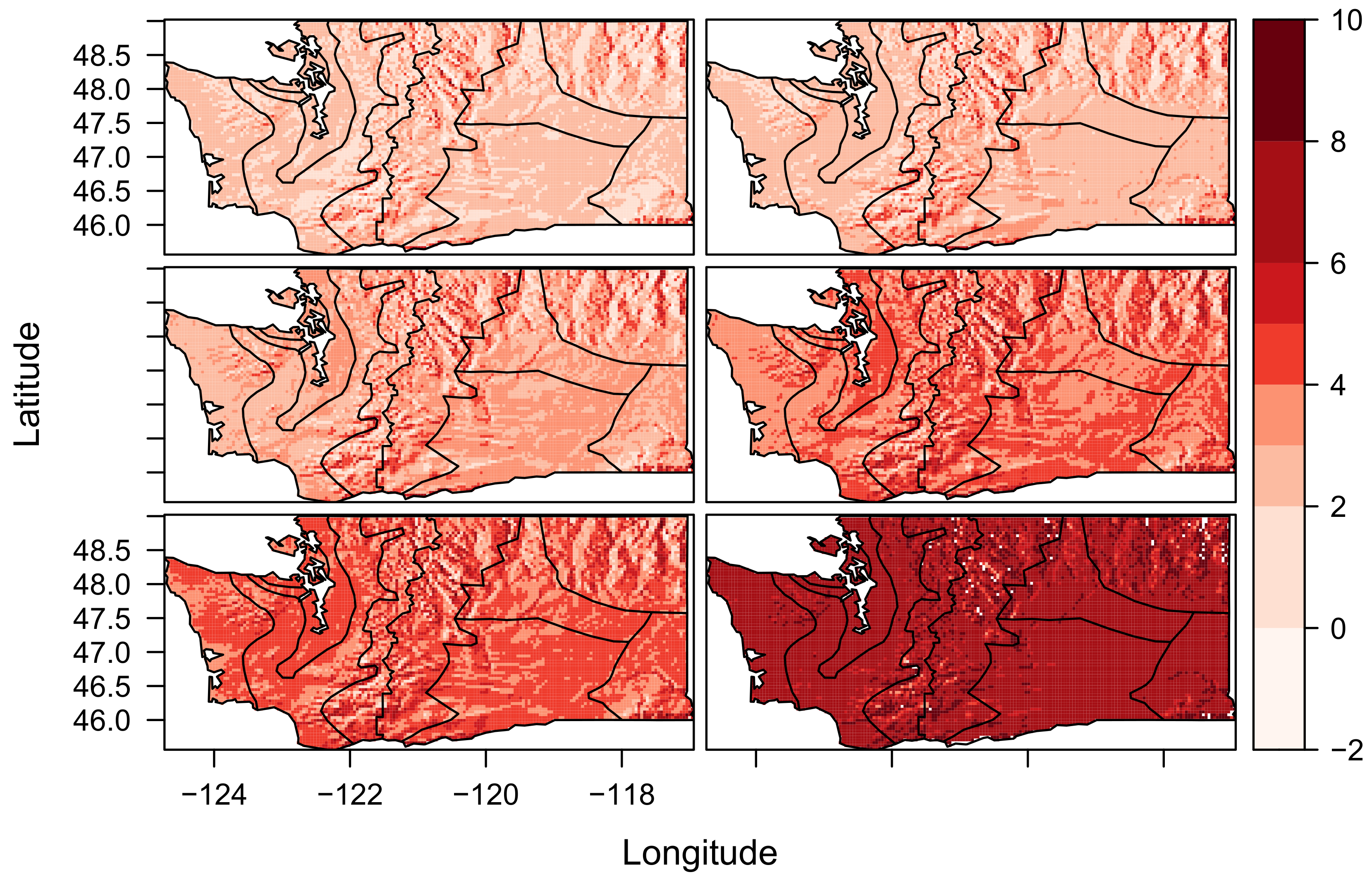
3.2. Projected Public Health Burden
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kilbourne, E.M. Heat Waves and Hot Environments. In The Public Health Consequences of Disasters; Noji, E.K., Ed.; Oxford University Press: New York, NY, USA, 1997; pp. 245–269. [Google Scholar]
- Basu, R.; Samet, J.M. Relation Between Elevated Ambient Temperature and Mortality: A Review of the Epidemiologic Evidence. Epidemiol. Rev. 2002, 24, 190–202. [Google Scholar] [CrossRef]
- Gosling, S.N.; Lowe, J.A.; McGregor, G.R.; Pelling, M.; Malamud, B.D. Associations Between Elevated Atmospheric Temperature and Human Mortality: A Critical Review of the Literature. Clim. Chang. 2009, 92, 299–341. [Google Scholar] [CrossRef]
- Kalkstein, L.S.; Davis, R.E. Weather and Human Mortality: An Evaluation of Demographic and Interregional Responses in the United States. Ann. Assoc. Am. Geogr. 1989, 79, 44–64. [Google Scholar] [CrossRef]
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Strug, L.; Patz, J.A. Temperature and Mortality in 11 Cities of the Eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef]
- Medina-Ramón, M.; Schwartz, J. Temperature, Temperature Extremes, and Mortality: A Study of Acclimatisation and Effect Modification in 50 US Cities. Occup. Environ. Med. 2007, 64, 827–833. [Google Scholar] [CrossRef]
- Busch Isaksen, T.; Yost, M.; Hom, E.; Fenske, R. Projected Health Impacts of Heat Events in Washington State Associated with Climate Change. Rev. Environ. Health 2014, 29, 119–123. [Google Scholar]
- Isaksen, T.B.; Fenske, R.A.; Hom, E.K.; Ren, Y.; Lyons, H.; Yost, M.G. Increased Mortality Associated with Extreme-Heat Exposure in King County, Washington, 1980–2010. Int. J. Biometeorol. 2015, 60, 85–98. [Google Scholar] [CrossRef]
- Shindell, D.; Zhang, Y.; Scott, M.; Ru, M.; Stark, K.; Ebi, K.L. The Effects of Heat Exposure on Human Mortality Throughout the United States. Geohealth 2020, 4, e2019GH000234. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, K.R.; Harris, D.; Spangler, K.R.; Zanobetti, A.; Wellenius, G.A. Estimating the Number of Excess Deaths Attributable to Heat in 297 United States Counties. Environ. Epidemiol. 2020, 4, e096. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Biggeri, A.; Bisanti, L.; Cadum, E.; Caranci, N.; de’Donato, F.; De Lisio, S.; De Maria, M.; et al. Vulnerability to Heat-Related Mortality: A Multicity, Population-Based, Case-Crossover Analysis. Epidemiology 2006, 17, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Basagaña, X.; Sartini, C.; Barrera-Gómez, J.; Dadvand, P.; Cunillera, J.; Ostro, B.; Sunyer, J.; Medina-Ramón, M. Heat Waves and Cause-Specific Mortality at All Ages. Epidemiology 2011, 22, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Åström, D.O.; Åström, C.; Forsberg, B.; Vicedo-Cabrera, A.M.; Gasparrini, A.; Oudin, A.; Sundquis, K. Heat Wave–Related Mortality in Sweden: A Case-Crossover Study Investigating Effect Modification by Neighbourhood Deprivation. Scand. J. Public Health 2020, 48, 6. [Google Scholar]
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to Heat-Related Mortality in Latin America: A Case-Crossover Study in são Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int. J. Epidemiol. 2008, 37, 796–804. [Google Scholar] [CrossRef]
- Fu, S.H.; Gasparrini, A.; Rodriguez, P.S.; Jha, P. Mortality Attributable to Hot and Cold Ambient Temperatures in India: A Nationally Representative Case-Crossover Study. PLoS Med. 2018, 15, e1002619. [Google Scholar] [CrossRef]
- Dimitrova, A.; Ingole, V.; Basagaña, X.; Ranzani, O.; Milà, C.; Ballester, J.; Tonne, C. Association between ambient temperature and heat waves with mortality in South Asia: Systematic review and meta-analysis. Environ. Int. 2021, 146, 106170. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Barnett, A.G.; Pan, X.; Yu, W.; Tong, S. The Impact of Temperature on Mortality in Tianjin, China: A Case-Crossover Design with a Distributed Lag Nonlinear Model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef]
- Shaposhnikov, D.; Revich, B.; Bellander, T.; Bedada, G.B.; Bottai, M.; Kharkova, T.; Kvasha, E.; Lezina, E.; Lind, T.; Semutnikova, E.; et al. Mortality Related to Air Pollution with the Moscow Heat Wave and Wildfire of 2010. Epidemiology 2014, 25, 359–364. [Google Scholar] [CrossRef]
- Wilson, L.A.; Morgan, G.G.; Hanigan, I.C.; Johnston, F.H.; Abu-Rayya, H.; Broome, R.; Gaskin, C.; Jalaludin, B. The Impact of Heat on Mortality and Morbidity in the Greater Metropolitan Sydney Region: A Case Crossover Analysis. Environ. Health 2013, 12, 98. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, J. Heat effects of ambient apparent temperature on all-cause mortality in Cape Town, Durban and Johannesburg, South Africa: 2006–2010. Sci. Total Environ. 2017, 587–588, 266–272. [Google Scholar] [CrossRef]
- Ahmadalipour, A.; Moradkhani, H. Escalating heat-stress mortality risk due to global warming in the Middle East and North Africa (MENA). Environ. Int. 2018, 117, 215–225. [Google Scholar] [CrossRef]
- Semenza, J.C.; Ruin, C.H.; Falter, K.H.; Selanikio, J.D.; Flanders, W.D.; Howe, H.L.; Wilhelm, J.L. Heat-Related Deaths During the July 1995 Heat Wave in Chicago. N. Engl. J. Med. 1996, 335, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J. Who Is Sensitive to Extremes of Temperature? A Case-Only Analysis. Epidemiology 2005, 16, 67–72. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Disparities by Race in Heat-Related Mortality in Four US Cities: The Role of Air Conditioning Prevalence. J. Urban Health 2005, 82, 191–197. [Google Scholar] [CrossRef]
- Madrigano, J.; Lane, K.; Petrovic, N.; Ahmed, M.; Blum, M.; Matte, T. Awareness, Risk Perception, and Protective Behaviors for Extreme Heat and Climate Change in New York City. Int. J. Environ. Res. Public Health 2018, 15, 1433. [Google Scholar] [CrossRef]
- Gravlee, C.C. How Race Becomes Biology: Embodiment of Social Inequality. Am. J. Phys. Anthropol. 2009, 129, 47–57. [Google Scholar] [CrossRef]
- Boyd, R.W.; Lindo, E.G.; Weeks, L.D.; McLemore, M.R. On Racism: A New Standard for Publishing on Racial Health Inequities. Health Affairs Blog 2020, 10, 1. [Google Scholar]
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Modifiers of the Temperature and Mortality Association in Seven US Cities. Am. J. Epidemiol. 2003, 157, 1074–1082. [Google Scholar] [CrossRef]
- Hoffman, J.S.; Shandas, V.; Pendleton, N. The Effects of Historical Housing Policies on Resident Exposure to Intra-Urban Heat: A Study of 108 US Urban Areas. Climate 2020, 8, 12. [Google Scholar] [CrossRef]
- Cissé, G.; McLeman, R.; Adams, H.; Aldunce, P.; Bowen, K.; Campbell-Lendrum, D.; Clayton, S.; Ebi, K.L.; Hess, J.; Huang, C.; et al. Health, Wellbeing, and the Changing Structure of Communities. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. In Climate Change 2022: Impacts, Adaptation, and Vulnerability; Pörtner, H.-O., Roberts, D.C., Tignor, M., Poloczanska, E.S., Mintenbeck, K., Alegría, A., Craig, M., Langsdorf, S., Löschke, S., Möller, V., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2022; pp. 5–6, in press. [Google Scholar]
- Kalkstein, L.S.; Greene, J.S. An Evaluation of Climate/Mortality Relationships in Large u.s. Cities and the Possible Impacts of a Climate Change. Environ. Health Perspect. 1997, 105, 84–93. [Google Scholar] [CrossRef]
- Reid, C.E.; O’Neill, M.S.; Gronlund, C.J.; Brines, S.J.; Brown, D.G.; Diez-Roux, A.V.; Schwartz, J. Mapping Community Determinants of Heat Vulnerability. Environ. Health Perspect. 2009, 117, 1730–1736. [Google Scholar] [CrossRef]
- Sheridan, S.C.; Kalkstein, A.J. Seasonal Variability in Heat- Related Mortality Across the United States. Nat. Hazards 2010, 55, 291–305. [Google Scholar] [CrossRef]
- IPCC. Climate Change 2013: The Physical Science Basis. Contribution of Working Group 1 to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Stocker, T.F., Qin, D., Plattner, G.-K., Tignor, M., Allen, S.K., Boschung, J., Nauels, A., Xia, Y., Bex, V., Midgley, P.M., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2013. [Google Scholar]
- Meehl, G.A.; Tebaldi, C. More Intense, More Frequent, and Longer Lasting Heat Waves in the 21st Century. Science 2004, 13, 994–997. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.E.; Yost, M.G.; Karr, C.; Fitzpatrick, C.; Lamb, B.K.; Chung, S.H.; Avise, J.; Rosenblatt, R.A.; Fenske, R.A. Public Health Impacts of Climate Change in Washington State: Projected Mortality Risks Due to Heat Events and Air Pollution. Clim. Chang. 2010, 102, 159–186. [Google Scholar] [CrossRef]
- Šeparović, L.; Alexandru, A.; Laprise, R.; Martynov, A.; Sushama, L.; Winger, K.; Tete, K.; Valin, M. Present Climate and Climate Change over North America as Simulated by the Fifth-Generation Canadian Regional Climate Model. Clim. Dyn. 2013, 41, 3167–3201. [Google Scholar] [CrossRef]
- Guttman, N.B.; Quayle, R.G. A Historical Perspective of US Climate Divisions. Bull. Am. Meteorol. Soc. 1996, 77, 293–303. [Google Scholar] [CrossRef]
- Abatzoglou, J.T. Development of Gridded Surface Meteorological Data for Ecological Applications and Modelling. Int. J. Climatol. 2013, 33, 121–131. [Google Scholar] [CrossRef]
- University of California Merced Climatology Lab: gridMET. Available online: https://www.climatologylab.org/gridmet.html (accessed on 24 July 2022).
- Mitchell, K.E.; Lohmann, D.; Houser, P.R.; Wood, E.F.; Schaake, J.C.; Robock, A.; Cosgrove, B.A.; Sheffield, J.; Duan, Q.; Luo, L.; et al. The Multi-Institution North American Land Data Assimilation System (NLDAS): Utilizing Multiple GCIP Products and Partners in a Continental Distributed Hydrological Modeling System. J. Geophys. Res. Atmos. 2004, 109, D07S90. [Google Scholar] [CrossRef]
- Daly, C.; Halbleib, M.; Smith, J.I.; Gibson, W.P.; Doggett, M.K.; Taylor, G.H.; Curtis, J.; Pasteris, P.A. Physiographically-Sensitive Mapping of Temperature and Precipitation Across the Conterminous United States. Int. J. Climatol. 2008, 28, 2031–2064. [Google Scholar] [CrossRef]
- Abatzoglou, J.T.; Brown, T.J. A Comparison of Statistical Downscaling Methods Suited for Wildfire Applications. Int. J. Climatol. 2011, 32, 772–780. [Google Scholar] [CrossRef]
- University of California Merced Climatology Lab: MACA. Available online: https://www.climatologylab.org/maca.html (accessed on 24 July 2022).
- Weinberger, K.R.; Haykin, L.; Eliot, M.N.; Schwartz, J.D.; Gasparrini, A.; Wellenius, G.A. Projected Temperature-Related Deaths in Ten Large u.s. Metropolitan Areas Under Different Climate Change Scenarios. Environ. Int. 2017, 107, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Masterton, J.M.; Richardson, F.A. Humidex; a Method of Quantifying Human Discomfort Due to Excessive Heat and Humidity; Environment Canada: Downsview, ON, Canada, 1979. [Google Scholar]
- Davis, R.E.; McGregor, G.R.; Enfield, K.B. Humidity: A Review and Primer on Atmospheric Moisture and Human Health. Environ. Res. 2016, 144, 106–116. [Google Scholar] [CrossRef]
- Ho, C.K.; Stephenson, D.B.; Collins, M.; Ferro, C.A.T.; Brown, S.J. Calibration Strategies: A Source of Additional Uncertainty in Climate Change Projections. Bull. Am. Meteorol. Soc. 2012, 93, 21–26. [Google Scholar] [CrossRef]
- Maclure, M. The Case-Crossover Design: A Method for Studying Transient Effects on the Risk of Acute Events. Am. J. Epidemiol. 1991, 133, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Jaakkola, J.J. Case-Crossover Design in Air Pollution Epidemiology. Eur. Respir. J. Suppl. 2003, 40, 81s–85s. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, J.H.; Lumley, T. Overlap Bias in the Case-Crossover Design, with Application to Air Pollution Exposures. Stat. Med. 2005, 24, 285–300. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Therneau, T.M. A Package for Survival Analysis in R. R Package Version 3.2-3. 2020. Available online: https://CRAN.R-project.org/package=survival (accessed on 30 May 2022).
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to Perform a Meta-Analysis with R: A Practical Tutorial. Evid.-Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Vicedo-Cabrera, A.M.; Sera, F.; Gasparrini, A. Hands-on Tutorial on a Modeling Framework for Projections of Climate Change Impacts on Health. Epidemiology 2019, 30, 321–329. [Google Scholar] [CrossRef]
- Heo, S.; Lee, E.; Kwon, B.Y.; Lee, S.; Jo, K.H.; Kim, J. Long-Term Changes in the Heat–Mortality Relationship According to Heterogeneous Regional Climate: A Time-Series Study in South Korea. BMJ Open 2016, 6, e011786. [Google Scholar] [CrossRef] [PubMed]
- Petitti, D.; Hodula, D.; Yang, S.; Harlan, S.; Chowell, G. Multiple Trigger Points for Quantifying Heat-Health Impacts: New Evidence from a Hot Climate. Environ. Health Perspect. 2016, 124, 176–183. [Google Scholar] [CrossRef]
- Weinberger, K.; Zanobetti, A.; Schwartz, J.; Wellenius, G. Effectiveness of National Weather Service heat alerts in preventing mortality in 20 US cities. Environ. Int. 2018, 116, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, A.; Saha, S.; Vicedo-Cabrera, A.M.; Gasparrini, A.; Abdurehman, N.; Jordan, R.; Hawkins, M.; Hess, J.; Elixhauser, A. Assessment of Extreme Heat and Hospitalizations to Inform Early Warning Systems. Proc. Natl. Acad. Sci. USA 2019, 116, 5420–5427. [Google Scholar] [CrossRef] [PubMed]
- McElroy, S.; Schwarz, L.; Green, H.; Corcos, I.; Guirguis, K.; Gershunov, A.; Benmarhnia, T. Defining Heat Waves and Extreme Heat Events Using Sub-Regional Meteorological Data to Maximize Benefits of Early Warning Systems to Population Health. Sci. Total Environ. 2020, 721, 137678. [Google Scholar] [CrossRef] [PubMed]
- Guirguis, K.; Basu, R.; Al-Delaimy, W.K.; Benmarhnia, T.; Clemesha, R.E.S.; Corcos, I.; Guzman-Morales, J.; Hailey, B.; Small, I.; Tardy, A.; et al. Heat, Disparities, and Health Outcomes in San Diego County’s Diverse Climate Zones. Geohealth 2018, 2, 212–223. [Google Scholar] [CrossRef]
- Wellenius, G.A.; Eliot, M.N.; Bush, K.F.; Holt, D.; Lincoln, R.A.; Smith, A.E.; Gold, J. Heat-Related Morbidity and Mortality in New England: Evidence for Local Policy. Environ. Res. 2017, 156, 845–853. [Google Scholar] [CrossRef]
- Jones, C.P. Invited Commentary: “Race,” Racism, and the Practice of Epidemiology. Am. J. Epidemiol. 2001, 154, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, J.B.; Bennett, T. Use of Race and Ethnicity in Biomedical Publication. JAMA 2003, 289, 2709–2716. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.S.; Cooper, R.S. Commentary: Considerations for Use of Racial/Ethnic Classification in Etiologic Research. Am. J. Epidemiol. 2001, 154, 291–298. [Google Scholar] [CrossRef]
- Bhopal, R. Race and Ethnicity: Responsible Use from Epidemiological and Public Health Perspectives. J. Law Med. Ethics 2006, 34, 500–507. [Google Scholar] [CrossRef]
- Knowlton, K.; Lynn, B.; Goldberg, R.A.; Rosenzweig, C.; Hogrefe, C.; Rosenthal, J.K.; Kinney, P.L. Projecting Heat-Related Mortality Impacts Under a Changing Climate in the New York City Region. Am. J. Public Health 2007, 97, 2028–2034. [Google Scholar] [CrossRef]
- Huang, C.; Barnett, A.G.; Wang, X.; Vaneckova, P.; FitzGerald, G.; Tong, S. Projecting Future Heat-Related Mortality Under Climate Change Scenarios: A Systematic Review. Environ. Health Perspect. 2011, 119, 1681–1690. [Google Scholar] [CrossRef]
- Guo, Y.; Gasparrini, A.; Li, S.; Sera, F.; Vicedo-Cabrera, A.M.; de Sousa Zanotti Stagliorio Coelho, M.; Saldiva, P.H.N.; Lavigne, E.; Tawatsupa, B.; Punnasiri, K.; et al. Quantifying Excess Deaths Related to Heatwaves Under Climate Change Scenarios: A Multicountry Time Series Modelling Study. PLoS Med. 2018, 15, e1002629. [Google Scholar] [CrossRef] [PubMed]
- Kalkstein, L.S.; Greene, S.; Mills, D.M.; Samenow, J. An Evaluation of the Progress in Reducing Heat-Related Human Mortality in Major u.s. Cities. Nat. Hazards 2011, 56, 113–129. [Google Scholar] [CrossRef]
- Ebi, K.L.; Teisberg, T.J.; Kalkstein, L.S.; Robinson, L.; Weiher, R.F. Heat Watch/Warning Systems Save Lives: Estimated Costs and Benefits for Philadelphia 1995–98. Bull. Am. Meteor. Soc. 2004, 85, 1067–1074. [Google Scholar] [CrossRef]
- Davis, R.E.; Knappenberger, P.C.; Michales, P.J.; Novicoff, W.M. Changing Heat-Related Mortality in the United States. Environ. Health Perspect. 2003, 111, 1712–1718. [Google Scholar] [CrossRef]
- Zanobetti, A.; Schwartz, J. Temperature and Mortality in Nine US Cities. Epidemiology 2008, 19, 563–570. [Google Scholar] [CrossRef]
- Tong, S.; Wang, X.Y.; Guo, Y. Assessing the Short-Term Effects of Heatwaves on Mortality and Morbidity in Brisbane, Australia: Comparison of Case-Crossover and Time Series Analyses. PLoS ONE 2012, 7, e37500. [Google Scholar] [CrossRef]
- Basu, R.; Dominici, F.; Samet, J.M. Temperature and Mortality Among the Elderly in the United States: A Comparison of Epidemiologic Methods. Epidemiology 2005, 16, 58–66. [Google Scholar] [CrossRef]
- Gosling, S.N.; McGregor, G.R.; Lowe, J.A. The Benefits of Quantifying Climate Model Uncertainty in Climate Change Impacts Assessment: An Example with Heat-Related Mortality Change Estimates. Clim. Chang. 2012, 112, 217–231. [Google Scholar] [CrossRef]
- Bateson, T.F.; Schwartz, J. Control for Seasonal Variation and Time Trend in Case-Crossover Studies of Acute Effects of Environmental Exposures. Epidemiology 1999, 10, 539–544. [Google Scholar] [CrossRef]
- Kottek, M.; Grieser, J.; Beck, C.; Rudolf, B.; Rubel, F. World Map of the köppen-Geiger Climate Classification Updated. Meterol. Z. 2006, 15, 259–263. [Google Scholar] [CrossRef]
- Gosling, S.N.; Hondula, D.M.; Bunker, A.; Ibarreta, D.; Liu, J.; Zhang, X.; Sauerborn, R. Adaptation to Climate Change: A Comparative Analysis of Modeling Methods for Heat-Related Mortality. Environ. Health Perspect. 2017, 125, 087008. [Google Scholar] [CrossRef]
- Washington State Department of Health. Available online: https://doh.wa.gov/emergencies/be-prepared-be-safe/severe-weather-and-natural-disasters/hot-weather-safety/heat-wave-2021 (accessed on 30 May 2022).
- Lowe, D.; Ebi, K.L.; Forsberg, B. Heatwave Early Warning Systems and Adaptation Advice to Reduce Human Health Consequences of Heatwaves. Int. J. Environ. Res. Public Health 2011, 8, 4623–4648. [Google Scholar] [CrossRef] [PubMed]
- Casanueva, A.; Burgstall, A.; Kotlarski, S.; Messeri, A.; Morabito, M.; Flouris, A.D.; Nybo, L.; Spirig, C.; Schwierz, C. Overview of Existing Heat-Health Warning Systems in Europe. Int. J. Environ. Res. Public Health 2019, 16, 2657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Climate Division | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | All | Cascade Mountains West | Central Basin | E Olympic Cascade Foothills | E Slope Cascades | NE Olympic San Juan | Northeastern | Okanogan Big Bend | Palouse Blue Mountains | Puget Sound Lowlands | West Olympic Coast |
| Total | 563,365 | 1020 | 62,794 | 85,498 | 4329 | 14,711 | 52,685 | 6479 | 7155 | 316,999 | 11,695 |
| Age | |||||||||||
| 0–4 | 7133 | 13 | 1033 | 810 | 42 | 88 | 636 | 52 | 59 | 4311 | 89 |
| 5–14 | 970 | - | 118 | 141 | - | - | 91 | 12 | - | 569 | 12 |
| 15–44 | 18,948 | 35 | 2006 | 2599 | 94 | 233 | 1575 | 158 | 176 | 11,800 | 272 |
| 45–64 | 98,702 | 233 | 10,393 | 15,996 | 775 | 1838 | 8914 | 1109 | 1059 | 56,145 | 2240 |
| 65–84 | 270,513 | 514 | 30,422 | 42,247 | 2174 | 7240 | 25,592 | 3279 | 3449 | 149,498 | 6098 |
| 85+ | 167,090 | 222 | 18,822 | 23,704 | 1236 | 5302 | 15,876 | 1868 | 2406 | 94,670 | 2984 |
| Sex | |||||||||||
| Female | 285,395 | 452 | 31,588 | 42,359 | 1982 | 7366 | 26,836 | 3148 | 3596 | 162,397 | 5671 |
| Male | 277,955 | 568 | 31,204 | 43,137 | 2347 | 7345 | 25,848 | 3331 | 3559 | 154,592 | 6024 |
| Race/Ethnicity | |||||||||||
| White | 518,873 | 997 | 57,769 | 82,544 | 4241 | 14,321 | 50,758 | 6078 | 6902 | 284,114 | 11,149 |
| Black | 14,429 | - | 701 | 592 | - | 37 | 572 | 23 | 21 | 12,433 | 40 |
| Asian | 12,341 | - | 326 | 700 | - | 106 | 324 | 17 | 37 | 10,780 | 42 |
| Native American | 6058 | 11 | 923 | 669 | 26 | 122 | 663 | 288 | 30 | 2,983 | 343 |
| Hispanic | 5980 | - | 2842 | 400 | 36 | 47 | 74 | 56 | 17 | 2454 | 49 |
| Native Hawaiian or Other Pacific Islander | 4296 | - | 106 | 392 | - | 33 | 139 | - | - | 3571 | 43 |
| Cause of Death | |||||||||||
| Diabetes | 10,004 | 20 | 1276 | 1576 | 64 | 226 | 919 | 140 | 132 | 5427 | 224 |
| Circulatory | 213,937 | 335 | 25,109 | 31,318 | 1607 | 5380 | 20,184 | 2434 | 2760 | 120,153 | 4657 |
| Cardiovascular | 160,118 | 261 | 18,970 | 23,972 | 1215 | 3970 | 14,822 | 1813 | 2005 | 89,483 | 3607 |
| Ischemic | 102,827 | 148 | 13,129 | 15,296 | 839 | 2528 | 9731 | 1236 | 1290 | 56,218 | 2412 |
| Cerebrovascular | 19,905 | 16 | 2367 | 2480 | 121 | 373 | 1919 | 194 | 273 | 11,802 | 360 |
| Respiratory | 54,393 | 92 | 5894 | 8375 | 395 | 1398 | 5716 | 657 | 758 | 29,845 | 1263 |
| Nephritis and nephrotic | 4160 | - | 513 | 552 | 22 | 78 | 417 | 46 | 72 | 2371 | 82 |
| Acute Renal Failure | 684 | - | 81 | 96 | - | - | 69 | - | 16 | 394 | - |
| Mental Disorders | 12,108 | 23 | 1146 | 1938 | 86 | 269 | 1013 | 143 | 165 | 7099 | 226 |
| Humidex (1980–2018) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Climate Division | Mean | SD | Min | Max | 25th | 50th | 75th | 95th | 99th |
| Cascade Mountains West | 22.74 | 6.82 | 1.23 | 41.36 | 17.80 | 22.91 | 27.78 | 33.51 | 36.77 |
| Central Basin | 27.24 | 6.55 | 5.66 | 48.40 | 22.53 | 27.50 | 32.11 | 37.56 | 40.56 |
| E Olympic Cascade Foothills | 24.97 | 6.39 | −1.29 | 48.14 | 20.40 | 24.97 | 29.44 | 35.55 | 39.57 |
| E Slope Cascades | 23.43 | 6.69 | 1.43 | 42.24 | 18.65 | 23.70 | 28.38 | 33.98 | 37.16 |
| NE Olympic San Juan | 21.77 | 4.70 | 6.11 | 39.30 | 18.53 | 21.71 | 24.93 | 29.72 | 32.87 |
| Northeastern | 24.70 | 6.71 | 2.85 | 44.92 | 19.79 | 24.99 | 29.73 | 35.25 | 38.01 |
| Okanogan Big Bend | 25.49 | 6.65 | 3.48 | 46.08 | 20.66 | 25.68 | 30.45 | 36.03 | 39.14 |
| Palouse Blue Mountains | 25.19 | 6.85 | 3.91 | 44.78 | 20.25 | 25.56 | 30.28 | 35.83 | 38.84 |
| Puget Sound Lowlands | 23.50 | 5.91 | 5.57 | 46.44 | 19.26 | 23.46 | 27.64 | 33.42 | 36.98 |
| West Olympic Coast | 21.29 | 4.61 | 5.88 | 44.83 | 18.31 | 21.20 | 24.03 | 29.21 | 33.77 |
| Group | Observations (%) | OR (95% CI) |
|---|---|---|
| Total | 563,365 (100) | 1.08 (1.06, 1.10) |
| Age | ||
| 0–4 | 7133 (1.3) | 0.90 (0.75, 1.08) |
| 5–14 | 970 (0.2) | 0.90 (0.56, 1.45) |
| 15–44 | 18,948 (3.4) | 1.05 (0.94, 1.17) |
| 45–64 | 98,702 (17.5) | 1.06 (1.02, 1.12) |
| 65–84 | 270,513 (48.0) | 1.07 (1.04, 1.10) |
| 85+ | 167,090 (29.7) | 1.09 (1.06, 1.13) |
| Sex | ||
| Female | 285,395 (50.7) | 1.08 (1.05, 1.11) |
| Male | 277,955 (49.3) | 1.06 (1.03, 1.09) |
| Race/Ethnicity | ||
| White | 518,873 (92.1) | 1.07 (1.05, 1.09) |
| Black | 14,429 (2.6) | 1.15 (1.02, 1.30) |
| Asian | 12,341 (2.2) | 1.06 (0.93, 1.21) |
| Native American | 6058 (1.1) | 1.08 (0.89, 1.32) |
| Hispanic | 5980 (1.1) | 1.01 (0.84, 1.21) |
| Native Hawaiian or Other Pacific Islander | 4296 (0.8) | 0.97 (0.77, 1.20) |
| Cause of Death (Total Cases) | All Ages | 0–4 | 5–14 | 15–44 | 45–64 | 65–84 | 85+ |
|---|---|---|---|---|---|---|---|
| All Non-Traumatic Causes (563,365) | 1.08 (1.06, 1.10) | 0.90 (0.75, 1.08) | 0.90 (0.56, 1.45) | 1.05 (0.94, 1.17) | 1.06 (1.02, 1.12) | 1.07 (1.04, 1.10) | 1.10 (1.06, 1.13) |
| Diabetes (10,004) | 1.20 (1.03, 1.39) | NA | NA | 1.25 (0.60, 2.63) | 1.12 (0.81, 1.56) | 1.25 (1.03, 1.52) | 1.12 (0.80, 1.56) |
| Circulatory (213,937) | 1.10 (1.07, 1.14) | 1.10 (0.40, 3.01) | 0.68 (0.10, 4.71) | 1.08 (0.86, 1.35) | 1.09 (1.00, 1.19) | 1.09 (1.04, 1.15) | 1.11 (1.05, 1.17) |
| Cardiovascular (160,118) | 1.10 (1.06, 1.14) | 1.36 (0.45, 4.14) | 0.30 (0.02, 3.56) | 1.12 (0.87, 1.44) | 1.09 (0.99, 1.20) | 1.09 (1.04, 1.16) | 1.11 (1.04, 1.18) |
| Ischemic (102,827) | 1.09 (1.04, 1.14) | NA | NA | 1.12 (0.77, 1.64) | 1.03 (0.92, 1.16) | 1.10 (1.03, 1.18) | 1.10 (1.02, 1.20) |
| Cerebrovascular (19,905) | 1.16 (1.05, 1.29) | 0.12 (0.00, 27.94) | NA | 1.12 (0.77, 1.64) | 1.27 (0.87, 1.86) | 1.21 (1.04, 1.41) | 1.10 (0.93, 1.30) |
| Respiratory (54,494) | 1.08 (1.02, 1.15) | 0.36 (0.10, 1.36) | 1.63 (0.15, 18.28) | 0.81 (0.47, 1.37) | 1.17 (0.97, 1.40) | 1.05 (0.96, 1.14) | 1.14 (1.02, 1.28) |
| Nephritis and nephrotic (4160) | 1.03 (0.82, 1.28) | 1.83 (0.15, 22.31) | NA | 1.60 (0.34, 7.85) | 0.75 (0.40, 1.42) | 1.04 (0.75, 1.45) | 1.09 (0.76, 1.57) |
| Acute Renal Failure (684) | 1.14 (0.66, 2.00) | NA | NA | NA | 0.75 (0.40, 1.42) | 0.87 (0.39, 1.91) | 1.09 (0.76, 1.57) |
| Mental Disorders (12,108) | 1.02 (0.90, 1.17) | NA | NA | 0.80 (0.43, 1.49) | 0.89 (0.60, 1.32) | 1.08 (0.86, 1.37) | 1.05 (0.87, 1.27) |
| Percent Increase | |||||||
|---|---|---|---|---|---|---|---|
| 2030 | 2050 | 2080 | |||||
| Climate Division | Historical (N) | RCP4.5 | RCP8.5 | RCP4.5 | RCP8.5 | RCP4.5 | RCP8.5 |
| Cascade Mountains West | 2 | 0 | 100 | 100 | 200 | 200 | 900 |
| Central Basin | 25 | 32 | 68 | 112 | 224 | 252 | 1156 |
| E Olympic Cascade Foothills | 61 | 11 | 28 | 57 | 133 | 152 | 556 |
| E Slope Cascades | 1 | 100 | 100 | 100 | 200 | 200 | 1100 |
| NE Olympic San Juan | 21 | 43 | 62 | 119 | 238 | 252 | 1652 |
| Northeastern | 33 | 42 | 76 | 124 | 245 | 276 | 1306 |
| Okanogan Big Bend | 3 | 33 | 33 | 100 | 200 | 233 | 1067 |
| Palouse Blue Mountains | 1 | 100 | 200 | 300 | 500 | 700 | 2900 |
| Puget Sound Lowlands | 283 | 23 | 42 | 87 | 178 | 196 | 812 |
| West Olympic Coast | 6 | 0 | 0 | 33 | 100 | 133 | 617 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, L.; Scheuerell , M.D.; Busch Isaksen , T. Mortality Associated with Extreme Heat in Washington State: The Historical and Projected Public Health Burden. Atmosphere 2022, 13, 1392. https://doi.org/10.3390/atmos13091392
Arnold L, Scheuerell MD, Busch Isaksen T. Mortality Associated with Extreme Heat in Washington State: The Historical and Projected Public Health Burden. Atmosphere. 2022; 13(9):1392. https://doi.org/10.3390/atmos13091392
Chicago/Turabian StyleArnold, Logan, Mark D. Scheuerell , and Tania Busch Isaksen . 2022. "Mortality Associated with Extreme Heat in Washington State: The Historical and Projected Public Health Burden" Atmosphere 13, no. 9: 1392. https://doi.org/10.3390/atmos13091392
APA StyleArnold, L., Scheuerell , M. D., & Busch Isaksen , T. (2022). Mortality Associated with Extreme Heat in Washington State: The Historical and Projected Public Health Burden. Atmosphere, 13(9), 1392. https://doi.org/10.3390/atmos13091392






