Abstract
Nitrogen oxides (NOx) are gaseous pollutants contributing to pollution in their primary form and are also involved in reactions forming ground-level ozone and fine particulate matter. Thus, NOx is of great interest for targeted pollution reduction because of this cascade effect. Primary emissions originate from fossil fuel combustion making NOx a common outdoor and indoor air pollutant. Numerous studies documenting the observed physical health impacts of NOx were reviewed and, where available, were summarized using risk ratios. More recently, the literature has shifted to focus on the mental health implications of NOx exposure, and a review of the current literature found five main categories of mental health-related conditions with respect to NOx exposure: common mental health disorders, sleep, anxiety, depression, and suicide. All the physical and mental health effects with available risk ratios were organized in order of increasing risk. Mental health concerns emerged as those most influenced by NOx exposure, with physical health impacts, such as asthma, only beginning to surface as the fourth highest risk. Mental health conditions occupied seven of the top ten highest risk health ailments. The results summarized in this narrative review show that there are clear positive correlations between NOx and negative physical and mental health manifestations, thus strengthening the argument in support of the reduction in ambient NOx levels.
Keywords:
air pollution; air quality; mental health; nitrogen oxides; NOx; physical health; risk ratios 1. Introduction
Air pollution has become a global health crisis with no relief in the foreseeable future. In 2015, the World Health Organization (WHO) and the Organisation for Economic Co-operation and Development (OECD) identified air toxins as the form of air pollution that had the greatest impact on health [1]. Outdoor air pollution is now the fourth leading mortality risk worldwide, preceded only by high blood pressure, dietary risk, and smoking [1,2]. Exposure to atmospheric pollution occurs at all hours of the day encompassing where an individual lives and works. It is also exacerbated by the commutes people make in all modes of transportation including walking, biking, public transport, and driving [3].
Air pollutants are defined as those substances in the atmosphere that cause harm to humans, animals, vegetation, or other materials. In the case of humans, this harm occurs primarily in the form of serious illness (morbidity) and/or mortality [4]. There is substantial evidence linking repeated exposure to various air pollutants to significant health effects [5]. In general, air pollution impacts the cardiovascular and respiratory health of humans. Symptoms can range from mild coughing or irritation of airways to more serious illnesses, including lung cancer, heart disease, stroke, acute respiratory infections, and chronic obstructive pulmonary disease (COPD) [6]. The occurrence of these symptoms can also lead to hospital emergency department visits, hospitalization, and/or premature death [7].
Although air quality related health challenges are being encountered worldwide, they are significantly more apparent in urban environments, especially in lower income countries. The total estimations for 2019 point to approximately 99% of the global population living in areas exceeding WHO ambient air quality standards [8]. Low- to middle-income countries see a disproportionately high impact of poor air quality. It is estimated that over 90% of deaths attributed to outdoor air pollution occur in low- and middle- income countries [8].
Premature deaths due to exposure to both indoor and outdoor air pollutants have been estimated to encompass approximately 10% of all deaths worldwide [6]. In 2016, it was estimated that outdoor air pollution resulted in 4.2 million deaths globally, with 58% from stroke and heart disease, 18% from respiratory infections, 18% from COPD, and 6% from lung cancer [8,9]. The effects of exposure to indoor air pollutants are just as significant as exposure to outdoor air pollutants for the overall health of a population. Indoor air exposure was ranked as the ninth largest risk factor for health in the 2015 Global Burden of Disease and, in 2012, the WHO estimated that 54% of the total 8 million premature deaths associated with poor air quality resulted from indoor air exposure [10,11]. Estimates of the combined worldwide health cost related to both outdoor and indoor air pollution were assessed at USD 8.1 trillion in 2019 [12].
Most of the statistics on air pollution and human health are linked only to the impact of fine particulate matter (PM) and do not take into account the contribution from other air pollutants. PM concentrations are readily monitored, and their health effects are well established, providing a foundation for quantifying the impacts of air pollution on human health. The omission of gaseous pollutants, such as nitrogen oxides (NOx), from air pollution statistics will need to be remedied in future analyses to provide a more comprehensive view of air pollution. The physical health impacts of NOx and other gaseous air pollutants have become well established over the past two decades and are the grounds for supporting more stringent exposure guidelines [8].
Another challenge associated with air pollution statistics and messages communicated to the public is that they are solely based on the physical health impacts of air pollution and do not account for mental health effects [13]. The number of people impacted by mental health disorders globally is on the rise. In 2016, these disorders were prevalent in over one billion people, or 16% of the world’s population (Ref. [14] citing data in [15]). Given that approximately one in seven individuals around the world are impacted by mental illnesses, there is a need for a better understanding of how air pollution impacts mental health.
Historically, the repercussions of gaseous pollutant exposure have been perceived through a single lens of physical health effects, but research into the mental health implications of NOx exposure has begun to gain traction in the last decade. To achieve a holistic understanding of the correlation between NOx and human health, both the physical and mental health implications must be accounted for. As a result, the aim of this paper is to provide an overview of the health risks due to NOx exposure, by means of a risk ratio comparison, with a particular focus on the recent developments in mental wellness and how mental health risks compare to physical ailments.
2. Nitrogen Oxides (NOx) as a Targeted Pollutant
NOx is a ubiquitous pollutant due to its numerous sources (mainly from stationary and mobile fossil fuel combustion but also from natural causes such as lightning), its potential to be both a primary and secondary pollutant, and its documented impacts on human health.
NOx occurs primarily in one of two forms: nitric oxide (NO) and nitrogen dioxide (NO2). NO is generally emitted as a primary pollutant, which photochemically reacts with free radicals in the atmosphere to form NO2 [4,16]. There are instances where NO2 is emitted as a primary pollutant, but more often than not, it occurs as a result of pre-existing NO [17]. The rate of secondary oxidation of NO into NO2 depends on the solar radiation intensity, humidity, concentration, availability of free radicals, and airflow in the region of concern [18]. When no information is not provided, it can be assumed that the NO2 concentration is essentially equivalent to the NOx concentration, since any NO in the atmosphere reacts quickly to form NO2 [4,16].
NO and NO2 can rapidly cycle back and forth in the atmosphere on a minute-by-minute timescale [19]. NOx is regarded as a short-lived air pollutant with an atmospheric lifetime on the order of a day [19], although this is typically shorter in the summer (<6 h [20,21]) due to higher ozone concentrations [21]. NO2 buildup in the atmosphere can be visually seen hanging over many large urban centres as a brown haze on the horizon.
In some instances, nitrous acid (HONO) is also generated [18]. Water molecules in the atmosphere are able to dissolve the ambient NO2 to form acidic compounds contributing to acid rain, putting ecosystems at risk of acidification. Additionally, NO2 can be absorbed directly by plants causing damage or death of tissue, which can impact plant growth and yield [7].
NOx, while a significant environmental pollutant on its own, also acts as a precursor for other air pollutants. NOx typically resides close to ground level in urban environments and, through a complex set of reactions, can react to form both ground-level ozone (O3) and fine particulate matter (PM2.5) in the form of secondary organic and inorganic aerosols (SOAs and SIAs, respectively). This, in turn, contributes to smog formation [22,23,24,25]. These reactions are cyclical in nature and can result in a buildup of NOx and O3 at ground level. There is typically a lag time between when the concentration of NOx increases (during morning and evening rush hours) and when the concentration of O3 increases (mid-morning and into the afternoon during peak solar intensities) [24].
It can be quite difficult to attribute the amount of PM2.5 or O3 in the atmosphere to either primary or secondary sources. Source attribution is influenced by geographic location, season, meteorological conditions, wind directions, and surrounding air pollution releases, as these, among other conditions, influence the equilibrium for secondary reactions. Several studies from China [26,27] estimated that between 14% and 27% of the measured secondary PM2.5 was generated from nitrates, thus illustrating that the NOx secondary aerosol pathway is significant in PM2.5 generation. The authors highlight that the significant contribution of secondary PM to the atmosphere necessitates a reduction in the precursor pollutants, such as NOx, as the focal point for air pollution reduction measures. By reducing NOx in the atmosphere, not only are the direct negative effects associated with NOx minimized, but the subsequent health impacts associated with exposure to O3, PM2.5, and smog will similarly be reduced.
3. Methodology, Considerations and Contribution of Research
3.1. Methodology
3.1.1. Overview
As stated above, the intention of this work is to provide an illustrative overview of the extensive health research conducted with respect to NOx exposure, with emphasis on the newly emerging research into mental health. As a result, this work should be considered in a narrative context and not as an exhaustive or comprehensive literature review. Both original epidemiological studies and review papers were collected. Studies covered primarily single pollutant analyses, with some containing multi-pollutant regressions. A multitude of countries are represented with studies including both region-specific and multi-city study locations.
There has been an abundance of research, covering a range of NOx concentrations for both indoor and outdoor exposure, that has examined the negative physical human health impacts associated with NOx exposure. The results presented herein do not provide an exhaustive list of the physical health literature but, rather, offer an extensive effort to illustrate the findings in this field, particularly studies presenting risk ratios. Both individual longitudinal studies and also review articles on the association between NOx exposure, physical health impacts, and risk ratios were collected. One such example is Atkinson et al. [28] which analysed the results from 48 articles on the association between NO2 exposure and human mortality.
Similar to the physical health research, both individual longitudinal studies and review articles were collected and reviewed herein for associations between mental health and NOx exposure. With the novelty of the mental health research, limited literature reviews have been completed in this field. Of those available, Łopuszańska and Makara-Studzińska [29], Gładka et al. [30], Zeng et al. [31], and Borroni et al. [32] focus only on depression and, in the case of Gładka et al. [30], suicide. Buoli et al. [33] provides an encompassing view of many different mental health disorders. The challenge with these literature reviews is that they are now outdated, as significant research has been published on the topic since 2019. Additionally, the reviews do not provide a succinct review specifically of NOx and its impacts on mental health. Over thirty-five longitudinal studies and reviews, published between 2007 and the beginning of 2022, were found concerning NOx air pollution and mental health disorders.
3.1.2. Data Collection
In an effort to document and effectively evaluate the literature gathered from the search for the physical and mental health correlation with NOx exposure, various information was collected from the articles. The information of interest, although not always available, from each study included: initial NOx exposure level, type of health ailment, acute or chronic exposure, metric for assessing health implication (e.g., medication use, hospital admission, etc.), geographic location and context (e.g., some studies looked at multi-city analyses), exposure duration, both categorial and continuous demographic variables (e.g., age or pre-existing medical considerations), seasonality, lag-time to response, single and multi-pollutant considerations, and, ultimately, risk or odds ratio. Once the data were collected, the sheer volume of the experimental conditions used became apparent. In effort to consolidate the information into a format to allow for initial comparisons to be made, type of health ailment, acute vs. chronic exposure, metric, and exposure level were the primary pieces of information extracted from each study, along with the risk or odds ratio result.
3.1.3. Risk Ratio Conversion
Where available, researchers presented results in one of two fashions, either as the risk ratio (RR) or the odds ratio (OR). The risk ratio is the incidence of a health ailment (number with the symptom divided by the total number in group) observed in the group exposed to NOx air pollution divided by the incidence of the same health effect in the unexposed group, otherwise known as the probability. When this ratio is greater than one, it indicates that there is a higher risk of developing a defined health effect when exposed to air pollution [34]. Odds ratios, on the other hand, provide a ratio of the odds (number with the symptom divided by the number without) of the health impact for the exposed and unexposed study groups [34]. It is possible to calculate RR from OR, and vice versa, based on the following Equation (1) adapted from Viera [34].
3.2. Considerations
This research evaluation was subject to numerous variables that may have influenced the results and findings presented herein. It should be understood that the evaluation was limited by the studies included, the quality of research and results produced in each study, the types of health ailments documented, the participant groups utilized, and the exposure conditions the participants were subject to, among other variables. No manipulation of the original study data, outside of a conversion from OR to RR where applicable, was performed on the data to account for any influencing factors outside of the analysis performed by the original authors.
One of the most prevalent limitations was the ability to isolate and attribute direct causation of health ailments to NOx exposure. As previously mentioned, NOx exists in the atmosphere alongside many other air pollutants; therefore, it is difficult to definitively link an observed health ailment solely to NOx exposure. Research methodologies are advancing in the field to include multi-pollutant models that may point to causation, but the evaluations presented herein should be viewed as correlational in nature between NOx exposure and health maladies and not as direct causation.
Finally, this review provides a snapshot in time of physical and mental health correlations with NOx exposure based on the research gathered to date. The results and comparative rankings will evolve as more research is published and included in the evaluation.
3.3. Research Contribution
The breadth of literature available under both physical and mental health studies also covered an expansive set of study variables. Due to the breadth of the research documented herein, the evaluation presented in this work is an initial effort to explore the relationship between physical and mental health, NOx exposure, and the correlated relative risk associations.
The contribution being offered through this work is to provide insight into the increased likelihood of observing significant health outcomes if ambient NOx concentrations increase throughout the world or the potential benefit that may be realized as NOx levels fall. The novel side-by-side comparison of both mental and physical health correlations will provide a unique lens for air pollution and human health discussions. The unique lens presented by this paper can be then used to educate future work into the more extensive and detailed modelling and analysis.
4. Physical Health Impacts of NOx
The main route of NOx exposure for humans is via inhalation, during which 80–90% is absorbed into the body through the respiratory tract. Nitrogen oxides, both NO and NO2, are readily absorbed into the bloodstream through the respiratory tract. Once in the bloodstream, NO reacts quite quickly, on the order of three seconds, with O2 to generate NO2. NO2 can further react in the bloodstream, as it is a water-based environment. Highly reactive NO2 generates superoxide and alloxy radicals, and the ensuing nitrogen anion imbalance contributes to lipid peroxidation [35].
NO occurs naturally in the bloodstream and has essential physiological functions in the human body, including acting as a vasodilator and signalling molecule. Blood concentrations above what is considered normal trigger inflammatory responses [35,36,37,38,39].
Exposure to NO also directly affects the nitric oxide synthase (NOS) activity, generally found in the intercellular fluid or in membranes of blood vessels and can trigger changes to the respiratory system and cellular respiration leading to the formation of reactive oxygen species (ROS). The presence of ROS in the respiratory tract and lung parenchyma result in sensitive tissue damage, such as augmentation of pulmonary permeability, increased mucus secretion, damage to fatty bronchial epithelium, and damage of surfactant properties. Chronic exposure directly causes the inflammation of tracheal mucosa and is often expected to be observed with irritation of the conjunctiva and ulceration of the nasal cavity [35]. Moreover, within the human body, NO can act as a vasodilator of cerebral blood vessels, causing cytotoxic activities in the immune system, as well as acting as neurotransmitter. Within the brain, neurons produce NO during their function and, when the NO and NO-synthase equilibrium is imbalanced, this can disrupt the cerebral blood flow and brain activity connection [36].
Nitrosation is the primary indirect impact of enhanced NO in the bloodstream and leads to the formation of nitrosamines. These byproducts damage DNA leading to carcinogenesis processes as well as chronic inflammation. Another NO reaction byproduct is superoxide nitrates, strong oxidizers responsible for inflammation and lipid peroxidation, with subsequent damage to cells and tissues throughout the body [35,36,37,38,39].
The first signs of NOx exposure are generally nose and throat irritation. If exposure persists, these symptoms can progress to bronchoconstriction and dyspnea (difficult and laboured breathing), especially in individuals who suffer from asthma [4]. Symptoms can worsen and develop into bronchitis, reduced lung function, and increased susceptibility to other respiratory developments [40]. Continued direct exposure to NOx can lead to increased sensitivity to respiratory infections, allergic reactions, childhood asthma, lung cancer, cardiovascular and respiratory diseases, and potential reproductive impacts [4,7,41]. These impacts can lead to increased risk for hospital emergency room visits, hospital admissions, and mortality.
Table 1 summarizes the more specific health effects resulting from both acute and chronic NOx exposure, specifically for NO2, along with the risk ratio (where available) that represents the increased risk associated with a 10 μg·m−3 increase in concentrations of NO2. It is evident, based on the literature, that exposure to NO2 has numerous adverse health effects, many of which can be severe in nature if left untreated. In addition, many of these health effects are confounded by the simultaneous exposure to O3 and PM2.5, of which NOx is a precursor gas.

Table 1.
Human physical health effects linked to NO2 exposure.
While NOx, O3, and PM2.5 have individual health impacts [77], they coexist in the ambient atmosphere; hence, it is not possible to allocate the health impacts, or portions of the impacts, to one specific pollutant outside of a controlled laboratory setting. Based on the medical evidence to date, the WHO has established annual and 24-h mean NO2 exposure limits of 10 μg·m−3 and 25 μg·m−3, respectively [8]. Prior to 2021, the annual limit was set at 40 μg·m−3. These limits are guidelines, and many countries impose their own regulations, having not yet adopted the new WHO guidelines. In Canada, for example, the current annual and 1-h NOx exposure levels are 35 μg·m−3 and 123 μg·m−3, respectively. These limits are scheduled to be reduced to 25 μg·m−3 and 86 μg·m−3, respectively, in 2025 [7].
5. Mental Health Impacts of NOx
The mental health impacts of NOx are not as established as the physical health effects of NOx and appear to have become a major focus of research after approximately 2015. This date coincides with the emergence of a worldwide societal focus on the mental health of the population and has been a focus over the past decade [14]. Mental health has been identified in the UN Sustainable Development Goals and focuses on promoting wellbeing among global citizens [78].
Mental health is an integral part to the overall wellness of an individual and, when not cared for properly, can also contribute to detrimental physical health impacts. A recent study at the University of Washington [79] found that the prevalence of mental health disorders increased at a rate of approximately 9,876,000 cases per annum between 2000 and 2019. This means that in 2020 there were be over 976 million people, 12.6% of the world’s population, with a mental health disorder. With the high ever-increasing prevalence of mental health disorders and with air pollution being a ubiquitous challenge significantly impacting physical health, the question becomes how does air pollution, specifically NOx, impact mental health?
The evaluation of the over thirty five longitudinal studies and reviews presented herein in Table 2 found that, in all cases, air pollution was mapped to NO2 exposure (NOx levels were sometimes also included). For the purposes of this review, any OR from studies were converted to RR, and the data converted from ORs are clearly indicated. The mental health concerns investigated included common mental disorders (CMD), sleep apnea, anxiety, depression, and suicide. Sleep apnea was included in the research because of its strong association with the occurrence of many psychopathological conditions, including psychological distress, anxiety, depression, and suicidal ideation [80]. Most commonly, researchers collected data based on emergency room visits, though other metrics were used to quantify mental health impacts including self-reported assessments, medication use, hospital admissions, and number of deaths. The work was primarily collected on adults of all sexes, over numerous years, and spanning multiple seasons.

Table 2.
Human mental health effects linked to NO2 exposure.
All studies found positive relationships between NO2 exposure and mental health disorders, and all but twelve of the 66 relationships were statistically significant to at least the p < 0.05 significance level. Depending on the length of the study and the data set available, some of the studies made adjustments for the sex, season, and the lag after the exposure event. There were no distinguishable trends across the literature as to whether sex or season posed any greater risk to mental health disorders due to NO2 exposure. Studies that examined the time separation between exposure event and mental health disorder manifestation did, in general, find that there was increased risk associated with shorter time scales (i.e., a mental health disorder generally had greater risk of manifestation in a zero to one day lag from the exposure event with the risk diminishing with more time passing from the exposure event). An overall observation from the body of literature reviewed points to a positive statistically significant correlation between NO2 exposure and the mental health of the global population.
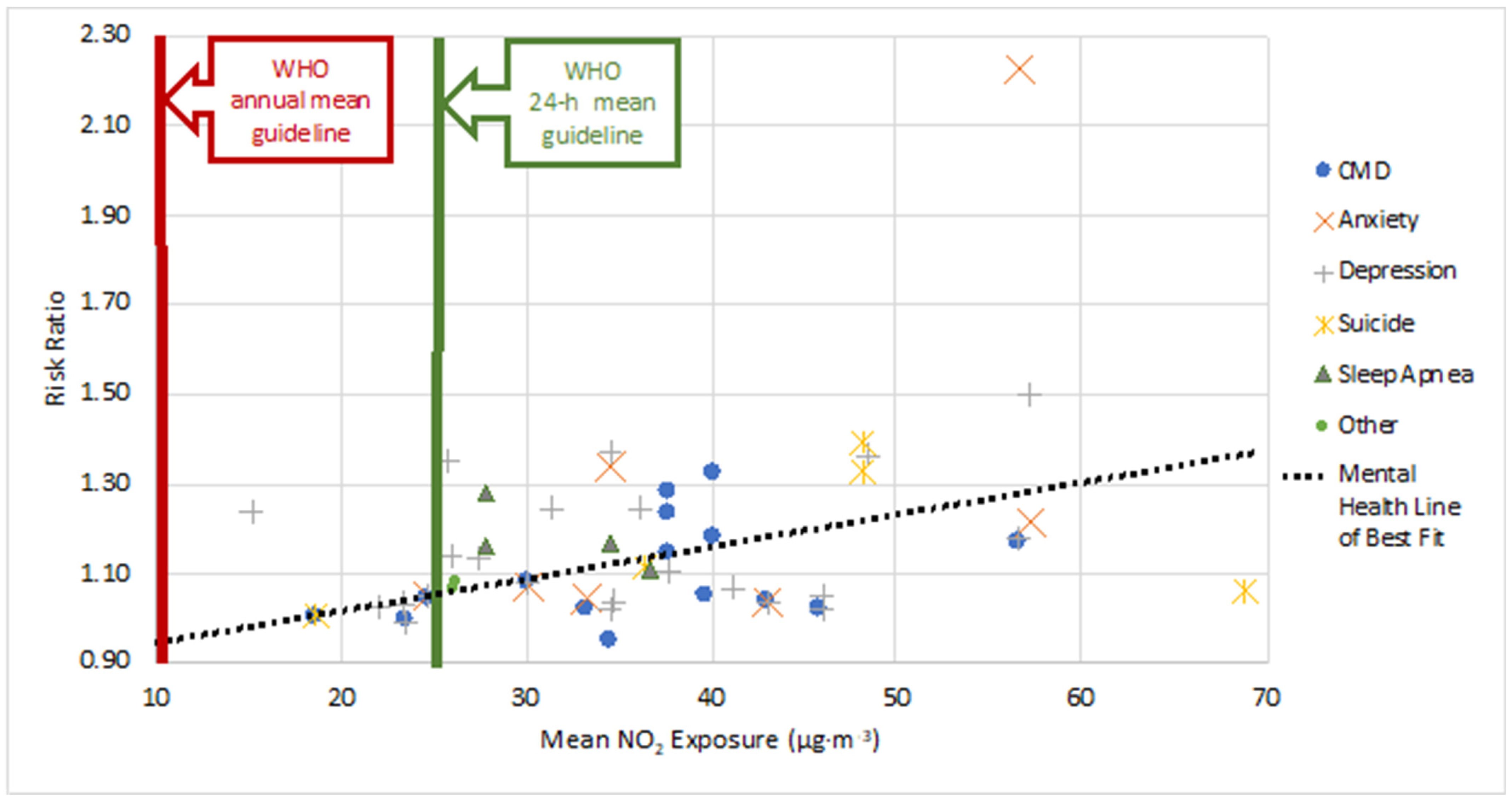
A comparison between the RR for each mental health disorder and for NO2 exposure level is presented in Figure 1. For reference, the WHO 24-h and annual mean exposure guidelines for NO2 are included on the plot. All studies had NO2 exposure concentrations that surpassed the 2021 WHO annual mean exposure guideline for NO2, and all but four exceeded the 24-h guideline. Data points are grouped based on the type of mental health disorder, and the metric used to quantify the disorder (i.e., emergency room visits, medication use, etc.) is not distinguished. The scattered nature of both data sets does not lead to any significant correlation for linking mean exposure to the level of risk of the presence of a mental health disorder. Linear trend lines were fit to the entire data set (mental health) (Equation (2)), as well subcategories with five or more data points (Equations (3)–(6)):
with RR being the risk ratio for all types of mental health disorders due to NO2 exposure, and C is the NO2 concentration (µg·m−3).
Figure 1.
Risk Ratio (RR) vs. Mean NO2 exposure (µg·m−3) for different mental health disorders. This figure provides a comparison for RR and mean exposure, when both values were provided in a study. Data are plotted from each study under the broad mental health category and the actual metric used to quantify the disorder (e.g., emergency room visit, medication use, etc.) is not distinguished. Additionally, this comparison is meant to illustrate the breadth of mental health correlations, and so both acute and chronic exposure risks are grouped together under the respective mental health category. A rough linear trend line was fit to the data set, and the equation for the line of best fit leads to the observation of a positive, though weak, association between increased NO2 exposure and increased RR.
In all instances, there were positive correlations between NO2 exposure and mental health disorders, though with low correlation coefficients. Based on the trend line slopes, anxiety carries the most risk with increased NO2 exposure levels. The subcategory of ‘sleep’ only had four data points, and ‘other’ included only Alzheimer’s and Parkinson’s diseases; thus, no trend lines were generated given the limited data. Additionally, the correlation coefficients for all the linear trend lines were very low ranging from a minimum of R2 = 0.0793 to a maximum of R2 = 0.3888. One primary reason for the large degree of scatter in the plot is that the exposure duration and concentration for each study was varied. The length of exposure and fluctuations of NO2 about the mean were not well communicated in the research and, thus, not accounted for. This makes it difficult to definitively correlate the risk ratio back to a single NO2 concentration value. While the scatter of the data may not lead to a strong fit, there is a distinct trend that increasing concentration enhances the risk of an individual manifesting a mental health disorder. This positive association, coupled with the fact all studies examined exceed the WHO annual mean NO2 guideline, leads to the observation that NO2 levels in urban areas must be reduced in order to help protect the mental health of global citizens.
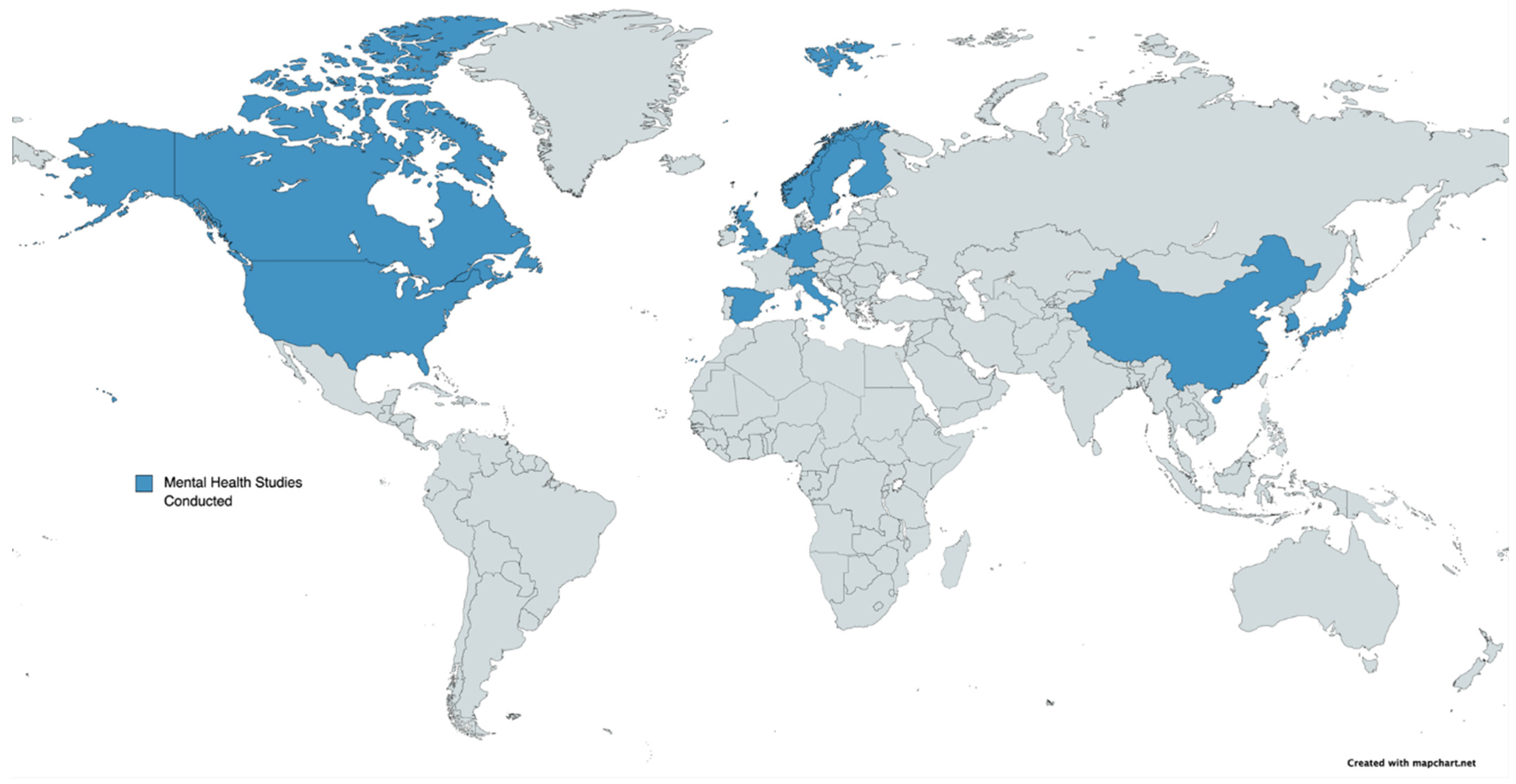
Figure 2 provides a geographical representation for where the studies on mental health have been conducted, in regard to NO2 exposure, on a world map by highlighting countries in blue. There is significant representation in North America, North and Western Europe, and some in Asia (mainly from China). Study gaps exist for Australia, South America, Africa, most of Asia, and Eastern Europe. Many of these regions are known to be heavy emitters of anthropogenic air pollution and are also highly populated. For example, ambient air quality in India (home to 1.4 billion people) can be extremely poor, with the capital city, Delhi, having the worst air quality in the world in 2020 [115]. Without mental health study data in these regions, any regional nuances and ramifications of NO2 exposure on mental health cannot be ascertained.
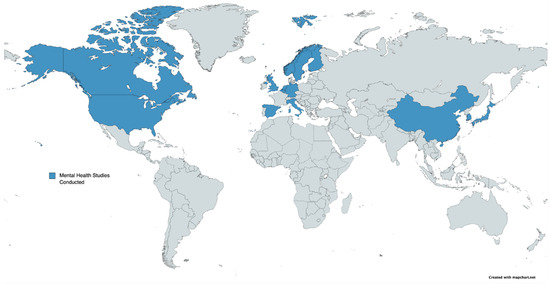
Figure 2.
World map indicating (in blue) where mental health studies in relation to NO2 exposure have been conducted. There is a significant information gap in South America, Africa, Australia, Eastern Europe, and most of Asia. Many of these regions without mental health studies are high emitters of anthropogenic air pollution and are highly populated.
6. Physical and Mental Health with NO2 Exposure Relative Risk
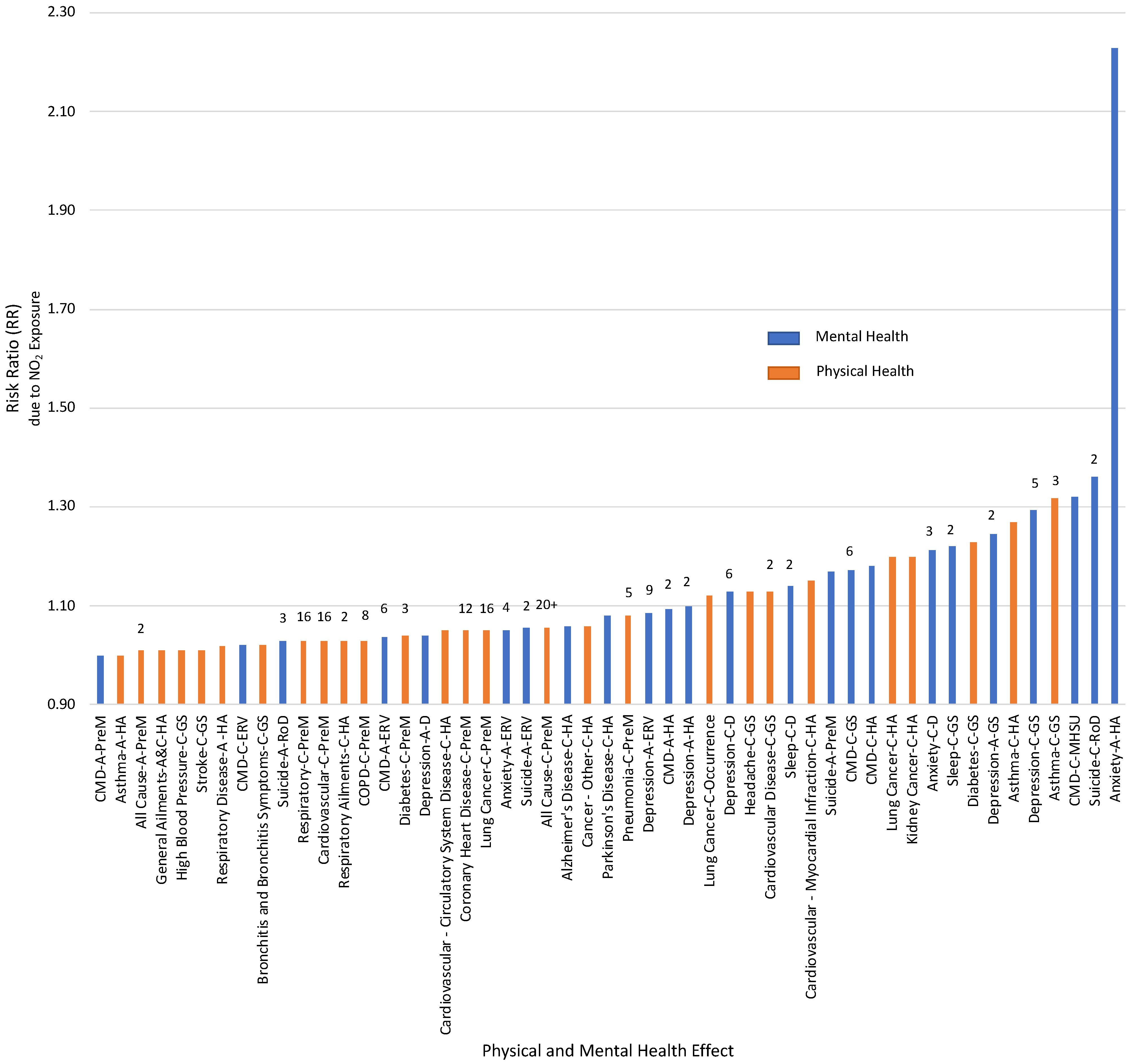
With the collected literature on the relative health risk associated with NO2 exposure, Figure 3 presents the information in a visual form that has been organized from the lowest to the highest RR. The top three highest-ranked health risks fall under the mental health category, spanning anxiety, suicide, and CMDs, with RRs ranging from 1.32 to 2.23. Seven of the top ten highest risk health ailments correlated with NOx exposure fall under the mental health category. Asthma (ranked fourth (general symptoms) and sixth (hospital admissions)) and diabetes (general symptoms, ranked eighth) are the only physical health conditions in the top ten.
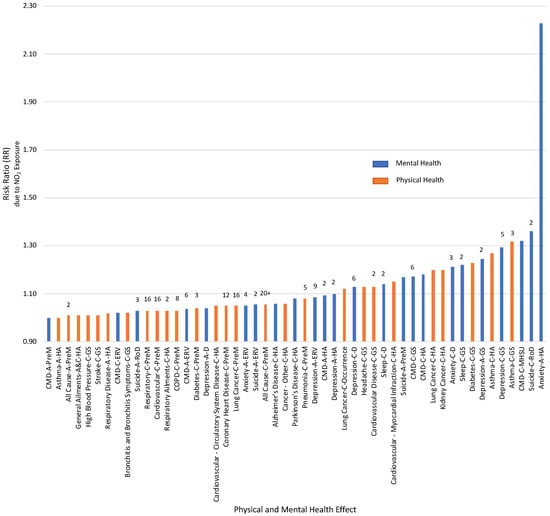
Figure 3.
Physical (orange) and Mental (blue) Health Effects and their relative Risk Ratios (RR) associated with NO2 exposure. Health effects, as well as the metric used to measure the impact on health, are labelled and have been organized in increasing RR order. For RR compiled from more than one study, the number of studies has been indicated above the respective bars. Abbreviations have been used in labels for ease of readability: A = Acute, C = Chronic, CMD = Common Mental Disorders, CV = Cardiovascular, D = Disorder, ERV = Emergency Room Visits, GS = General Symptoms, HA = Hospital Admissions, MHSU = Mental Health Service Use, PreM = Premature Mortality, RoD = Risk of Death.
Of the 21 health impacts with an RR of 1.10 or higher, 12 were related to mental health, and the remaining nine were physical health manifestations. The implication of this finding suggests that NO2 exposure has a significant correlation with the mental wellbeing of the global population, with a risk on par or even greater than the physical health impacts that have been extensively studied. Physical health effects have long been the basis for establishing air pollution exposure guidelines. These results advocate that, for NOx, it is essential to incorporate mental health into the discussion for setting appropriate exposure guidelines to ensure a healthy population, and solely examining physical ailments is not sufficient.
It is essential to note a few points regarding this comparison between mental and physical health implications correlated with NOx exposure. First, the evaluation presented herein is not exhaustive of all longitudinal studies conducted in either the physical or mental health realms but has primarily focused on studies that have determined a risk or odds ratio for the particular health impact. This means that there may be factors presented in other studies, which could influence the RR and ranking position. Additionally, mental health research is continuing to emerge; therefore, new studies published following the research conducted for this current work may again influence the RR and ranking for mental health manifestations. Finally, the studies and risk results collected have not been manipulated, outside of the work performed by the original authors, to account for socioeconomic status, living conditions, or other variables that may influence the correlations.
The associations drawn between NOx exposure and human health were correlations primarily based on single pollutant models and did not examine NOx pollution impacts independent from other air pollutants, such as PM, black carbon, or SOx. Causal relationships are difficult to determine as human participants are ubiquitously subject to exposure from a mixture of air pollutants. Advances in modelling and analysis are allowing for complex multi-pollutant assessments to be made. For example, Gu et al. [109] performed two-pollutant assessments and found that the impact of NO2 exposure on hospital admissions for depression remained significant even after controlling for other pollutants. Another study by Kim et al. [113] looked at the impact of single and two-pollutant models on correlations between air pollutants and suicide in citizens from ten Northeast Asian cities. Single pollutant models showed positive associations for NO2 exposure, as well as SO2 and PM10. When considering the two-pollutant models, it was found that there was a reduced RR, when NO2 was adjusted for the impacts of SO2 and PM10. A similar finding was shown by Bakolis et al. [13], where single pollutant models were positive between CMD and exposure to each of NO2, NOx, and PM2.5, though the risk was attenuated for all pollutants in two-pollutant sensitivity analyses. As more multi-pollutant studies are conducted a clearer causal association between individual air pollutants and human health may arise, though the significant correlation between air pollutants [13,113] will continue to make isolating these causal relationships difficult.
7. Conclusions
NOx is a ubiquitous primary air pollutant that contributes to the formation of additional harmful secondary pollutants. As a result, understanding how NOx impacts human health is critical for use in developing legislation and reduction strategies that may subsequently reduce the excessive exposure experienced by the global population.
The physical health impacts of the exposure to NOx have been well established over decades of research. A narrative review of some of these studies has been completed and summarized in this paper with a focus on reporting the risk ratio. In support of other bodies of knowledge on the topic, there are clear correlations between NO2 and NOx exposure and the development of health problems in the global population.
Since 2015, there has been a shift in air pollution research to examine and quantify the relationships between exposure and the mental health of the global population, but a review of the mental health research has not been completed with up-to-date research. Longitudinal research, published up to the beginning of 2022, into the impacts of NOx on mental health was collected, and the literature review completed herein found that there were positive and statistically significant correlations between NO2 exposure and the occurrence of mental health disorders. Significant gaps exist in gaining a geographically holistic understanding, as there is no current research from South America, Africa, Australia, and little in Asia and Eastern Europe on this topic.
Combining the understanding of both the physical and mental health effects of NO2 exposure into one review has allowed for the ordering of risk ratios. The results illustrated that mental health ailments correlated with the most significant risk from increasing NO2 exposure. Mental health conditions spanning anxiety, suicide, and CMDs hold the top three RR rank positions. Following these conditions, asthma was the physical health condition most impacted by NO2 exposure, and it holds the fourth and sixth rank positions. With mental health conditions presiding in the top RR positions, this signals the incredible impact that NO2 can have on mental health. Therefore, there is an imperative need for mental health to be further studied and accounted for when presenting the impact of air pollution on human health.
The evaluation of NOx exposure and correlations with both physical and mental health through a side-by-side comparison of risk ratios offers a unique lens for viewing the air pollution and human health dialogue. An initial understanding was presented of the likelihood of significant human health ailments arising with increased levels of NOx concentrations and emphasizes the need for a global reduction in NOx pollution. This preliminary exploration is not intended to be static in nature but instead provides a basis for future research to further expand and enhance the concepts presented herein.
Author Contributions
Conceptualization: S.S. and B.V.H.; investigation: S.S.; formal analysis: S.S.; writing—original draft: S.S.; writing—review and editing: S.S. and B.V.H. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Canadian Government National Science and Engineering Research Council (NSERC), the Government of Ontario Graduate Scholarship (OGS), and the University of Guelph.
Data Availability Statement
Data analysed within this study are found within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CMD | Common Mental Disorder |
| COPD | Chronic Obstructive Pulmonary Disorder |
| HONO | Nitrous Acid |
| NOS | Nitric Oxide Synthase |
| NO | Nitric Oxide |
| NO2 | Nitrogen Dioxide |
| NOx | Nitrogen Oxides |
| O3 | Ozone |
| OR | Odds Ratio |
| PM | Particulate Matter |
| ROS | Reactive Oxygen Species |
| RR | Risk Ratio |
| SIA | Secondary Inorganic Aerosol |
| SOA | Secondary Organic Aerosol |
| UN | United Nations |
| VOC | Volatile Organic Compound |
| WHO | World Health Organization |
References
- Smith, R.; McDougal, K. Costs of Pollution in Canada: Measuring the Impacts on Families, Businesses and Governments; International Institute for Sustainable Development: Winnipeg, MB, Canada, 2017. [Google Scholar]
- Liu, G.; Xiao, M.; Zhang, X.; Gal, C.; Chen, X.; Liu, L.; Pan, S.; Wu, J.; Tang, L.; Clements-Croome, D.; et al. A review of air filtration technologies for sustainable and healthy building ventilation. Sustain. Cities Soc. 2017, 32, 375–396. [Google Scholar] [CrossRef]
- Johansson, C.; Lövenheim, B.; Schantz, P.; Wahlgren, L.; Almström, P.; Markstedt, A.; Strömgren, M.; Forsberg, B.; Sommar, J.N. Impacts on air pollution and health by changing commuting from car to bicycle. Sci. Total Environ. 2017, 584–585, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Gorai, A.K.; Kanchan Upadhyay, A.; Tuluri, F.; Goyal, P.; Tchounwou, P.B. An innovative approach for determination of air quality health index. Sci. Total Environ. 2015, 533, 495–505. [Google Scholar] [CrossRef] [Green Version]
- World Bank. The Cost of Air Pollution: Strengthening the Economic Case for Action; World Bank Group: Washington, DC, USA, 2016. [Google Scholar]
- Canadian Council of Ministers of the Environment. 2017 Air Quality, Canadian Ambient Air Quality Standards (CAAQS). Available online: http://airquality-qualitedelair.ccme.ca/en/ (accessed on 20 January 2021).
- World Health Organization. Ambient (Outdoor) Air Pollution. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 21 October 2021).
- Mason, T.G.; Schooling, C.M.; Chan, K.P.; Tian, L. An evaluation of the air quality health index program on respiratory diseases in Hong Kong: An interrupted time series analysis. Atmos. Environ. 2019, 211, 151–158. [Google Scholar] [CrossRef]
- Kumar, P.; Skouloudis, A.N.; Bell, M.; Viana, M.; Carotta, M.C.; Biskos, G.; Morawska, L. Real-time sensors for indoor air monitoring and challenges ahead in deploying them to urban buildings. Sci. Total Environ. 2016, 560–561, 150–159. [Google Scholar] [CrossRef] [Green Version]
- Patelarou, E.; Tzanakis, N.; Kelly, F.J. Exposure to indoor pollutants and wheeze and asthma development during early childhood. Int. J. Environ. Res. Public Health 2015, 12, 3993–4017. [Google Scholar] [CrossRef] [Green Version]
- World Bank. Pollution. 2021. Available online: https://www.worldbank.org/en/topic/pollution#:~:text=According%20to%20the%20World%20Bank,to%204.8%25%20of%20global%20GDP (accessed on 2 February 2021).
- Bakolis, I.; Hammoud, R.; Stewart, R.; Beevers, S.; Dajnak, D.; MacCrimmon, S.; Broadbent, M.; Pritchard, M.; Shiode, N.; Fecht, D.; et al. Mental health consequences of urban air pollution: Prospective population-based longitudinal survey. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1587–1599. [Google Scholar] [CrossRef]
- Rehm, J.; Shield, K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019, 21, 10. [Google Scholar] [CrossRef]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 30 October 2018).
- César, A.C.; Carvalho, J.A.; Nascimento, L.F. Association between NOx exposure and deaths caused by respiratory diseases in a medium-sized Brazilian city. Braz. J. Med. Biol. Res. 2015, 48, 1130–1135. [Google Scholar] [CrossRef] [Green Version]
- Chaloulakou, A.; Mavroidis, I.; Gavriil, I. Compliance with the annual NO2 air quality standard in Athens. Required NOx levels and expected health implications. Atmos. Environ. 2008, 42, 454–465. [Google Scholar] [CrossRef]
- Zouzelka, R.; Rathousky, J. Photocatalytic abatement of NOx pollutants in the air using commercial functional coating with porous morphology. Appl. Catal. B-Environ. 2017, 217, 466–476. [Google Scholar] [CrossRef]
- Jacob, D.J. Introduction to Atmospheric Chemistry; Chapter 11: Oxidizing Power of the Atmosphere; Princeton University Press: Princeton, NJ, USA, 1999; pp. 199–219. [Google Scholar]
- Liu, F.; Beirle, S.; Zhang, Q.; Dörner, S.; He, K.; Wagner, T. NOx lifetimes and emissions of cities and power plants in polluted background estimated by satellite observations. Atmos. Chem. Phys. 2016, 16, 5283–5298. [Google Scholar] [CrossRef] [Green Version]
- Shah, V.; Jacob, D.; Li, K.; Silvern, R.; Zhai, S.; Liu, M.; Lin, J.; Zhang, Q. Effect of changing NOx; lifetime on the seasonality and long-term trends of satellite-observed tropospheric NO2; columns over China. Atmos. Chem. Phys. Discuss. 2019, 670, 1–23. [Google Scholar] [CrossRef]
- Bélanger, D.; Berry, P. Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity; Health Canada: Ottawa, ON, Canada, 2008.
- Boubel, R.W.; Fox, D.L.; Turner, D.B.; Stern, A.C. Fundamentals of Air Pollution, 3rd ed.; Chapter 7 Effects on Health and Human Welfare and Chapter 12 Atmospheric Chemistry; Academic Press: Cambridge, MA, USA, 1994; pp. 99–109,165–177. [Google Scholar]
- Muilwijk, C.; Schrijvers, P.J.; Wuerz, S.; Kenjereš, S. Simulations of photochemical smog formation in complex urban areas. Atmos. Environ. 2016, 147, 470–484. [Google Scholar] [CrossRef]
- Seinfield, J.H.; Pandis, S.N. Atmospheric Chemistry and Physics, 3rd ed.; Chapter 2.7: Particulate Matter (Aerosols); John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006; pp. 48–54. [Google Scholar]
- Cheng, M.; Tang, G.; Lv, B.; Li, X.; Wu, X.; Wang, Y.; Wang, Y. Source apportionment of PM2.5 and visibility in Jinan, China. J. Environ. Sci. 2021, 102, 207–2015. [Google Scholar] [CrossRef]
- Zhao, Z.; Lv, S.; Zhang, Y.; Zhao, Q.; Shen, L.; Xu, S.; Yu, J.; Hou, J.; Jin, C. Characteristics and source apportionment of PM 2.5 in Jiaxing, China. Environ. Sci. Pollut. Res. 2019, 26, 7497–7511. [Google Scholar] [CrossRef]
- Atkinson, R.W.; Butland, B.K.; Anderson, H.R.; Maynard, R.L. Long-term concentrations of nitrogen dioxide and mortality: A meta-analysis of cohort studies. Epidemiology 2018, 29, 460–472. [Google Scholar] [CrossRef]
- Łopuszańska, U.; Makara-Studzińska, M. The correlations between air pollution and depression. Curr. Probl. Psychiatry 2017, 18, 100–109. [Google Scholar] [CrossRef] [Green Version]
- Gładka, A.; Rymaszewska, J.; Zatoński, T. Impact of air pollution on depression and suicide. Int. J. Occup. Med. Environ. 2018, 31, 711–721. [Google Scholar] [CrossRef]
- Zeng, Y.; Lin, R.; Liu, L.; Liu, Y.; Li, Y. Ambient air pollution exposure and risk of depression: A systematic review and meta-analysis of observational studies. Psychiatry Res. 2019, 276, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Borroni, E.; Pesatori, A.C.; Bollati, V.; Buoli, M.; Carugno, M. Air pollution exposure and depression: A comprehensive updated systematic review and meta-analysis. Environ. Pollut. 2022, 292, 11845. [Google Scholar] [CrossRef] [PubMed]
- Buoli, M.; Grassi, S.; Caldiroli, A.; Carnevali, G.S.; Mucci, F.; Iodice, S.; Cantone, L.; Pergoli, L.; Bollati, V. Is there a link between air pollution and mental disorders? Environ. Int. 2018, 118, 154–168. [Google Scholar] [CrossRef]
- Viera, A.J. Odds ratios and risk ratios: What’s the difference and why does it matter? South Med. J. 2008, 101, 730–734. [Google Scholar] [CrossRef]
- Krzeszowiak, J.; Stefanow, D.; Pawlas, K. The impact of particulate matter (PM) and nitric oxides (NOx) on human health and an analysis of selected sources accounting for their emission. Med. Sr.—Environ. Med. 2016, 19, 3–15. [Google Scholar] [CrossRef]
- Anyanwu, E. Complex interconvertibility of nitrogen oxides (NOx): Impact on occupational and environmental health. Rev. Environ. Health 1999, 14, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Mohsenin, V. Human exposure to oxides of nitrogen at ambient and supra-ambient concentrations. Toxicology 1994, 89, 301–312. [Google Scholar] [CrossRef]
- Munawer, M.E. Human health and environmental impacts of coal combustion and post-combustion wastes. J. Sustain. Min. 2018, 17, 87–96. [Google Scholar] [CrossRef]
- Skouloudis, A.N.; Kassomenos, P. Combining environment and health information systems for the assessment of atmospheric pollution on human health. Sci. Total Environ. 2014, 488–489, 362–368. [Google Scholar] [CrossRef]
- Vasev, N. Governing energy while neglecting health—The case of Poland. Health Policy 2017, 121, 1147–1153. [Google Scholar] [CrossRef]
- Lu, X.; Yao, T.; Li, Y.; Fung, J.C.; Lau, A.K. Source apportionment and health effect of NOx over the Pearl River Delta region in southern China. Environ. Pollut. 2016, 212, 135–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zock, J.P.; Verheij, R.; Helbich, M.; Volker, B.; Spreeuwenberg, P.; Strak, M.; Janssen, N.A.H.; Dijst, M.; Groenewegen, P. The impact of social capital, land use, air pollution and noise on individual morbidity in Dutch neighbourhoods. Environ. Int. 2018, 121, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Palmgren, F.; Berkowicz, R.; Hertel, O.; Vignati, E. Effects of reduction of NOx on the NO2 levels in urban streets. Sci. Total Environ. 1996, 189–190, 409–415. [Google Scholar] [CrossRef]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242. [Google Scholar] [CrossRef]
- Mi, Y.H.; Norbäck, D.; Tao, J.; Mi, Y.L.; Ferm, M. Current asthma and respiratory symptoms among pupils in Shanghai, China: Influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air 2006, 16, 454–464. [Google Scholar] [CrossRef]
- Anderson, H.R.; Atkinson, R.W.; Bremmer, S.A.; Carrington, J.; Peacock, P. Quantitative Systematic Review of Short Term Associations between Ambient Air Pollution (Particulate Matter, Ozone, Nitrogen Dioxide, Sulphur Dioxide and Carbon Monoxide), and Mortality and Morbidity; Division of Community Health Sciences St George’s—University of London: London, UK, 2007. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215975/dh_121202.pdf (accessed on 26 November 2021).
- Kirsch, M.; Korth, H.G.; Sustmann, R.; de Groot, H. The pathobiochemistry of nitrogen dioxide. Biol. Chem. 2002, 383, 389–399. [Google Scholar] [CrossRef]
- McConnell, R.; Berhane, K.; Gilliland, F.; Molitor, J.; Thomas, D.; Lurmann, F.; Avol, E.; Gauderman, W.J.; Peters, J.M. Prospective study of air pollution and bronchitic symptoms in children with asthma. Am. J. Respir. Crit. Care 2003, 168, 790–797. [Google Scholar] [CrossRef] [Green Version]
- Rivas, E.; Santiago, J.L.; Lechón, Y.; Martín, F.; Ariño, A.; Pons, J.J.; Santamaría, J.M. CFD modelling of air quality in Pamplona City (Spain): Assessment, stations spatial representativeness and health impacts valuation. Sci. Total Environ. 2019, 649, 1362–1380. [Google Scholar] [CrossRef]
- Alexeeff, S.E.; Roy, A.; Shan, J.; Liu, X.; Messier, K.; Apte, J.S.; Portier, C.; Sidney, S.; Van Den Eeden, S.K. High-resolution mapping of traffic related air pollution with Google street view cars and incidence of cardiovascular events within neighborhoods in Oakland, CA. Environ. Health-Glob. 2018, 17, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Beelen, R.; Hoek, G.; van den Brandt, P.A.; Goldbohm, R.A.; Fischer, P.; Schouten, L.J. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ. Health Perspect. 2008, 116, 196–202. [Google Scholar] [CrossRef]
- Chen, H.; Goldberg, M.S.; Burnett, R.T.; Jerrett, M.; Wheeler, A.J.; Villeneuve, P.J. Long-term exposure to traffic-related air pollution and cardiovascular mortality. Epidemiology 2013, 24, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Gan, W.Q.; Koehoorn, M.; Davies, H.W.; Demers, P.A.; Tamburic, L.; Brauer, M. Long-term exposure to traffic-related air pollution and the risk of coronary heart disease hospitalization and mortality. Environ. Health Perspect. 2011, 119, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Jerrett, M.; Burnett, R.T.; Beckerman, B.S.; Turner, M.C.; Krewski, D.; Thurston, G.; Martin, R.V.; van Donkelaar, A.; Hughes, E.; Shi, Y. Spatial analysis of air pollution and mortality in California. Am. J. Respir. Crit. Care 2013, 188, 593–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raaschou-Nielsen, O.; Hermansen, M.N.; Loland, L.; Buchvald, F.; Pipper, C.B.; Sørensen, M.; Loft, S.; Bisgaard, H. Long-term exposure to indoor air pollution and wheezing symptoms in infants. Indoor Air 2010, 20, 159–167. [Google Scholar] [CrossRef]
- Rijnders, E.; Janssen, N.A.; van Vliet, P.H.; Brunekreef, B. Personal and outdoor nitrogen dioxide concentrations in relation to degree of urbanization and traffic density. Environ. Health Perspect. 2001, 109, 411–417. [Google Scholar] [CrossRef] [Green Version]
- Weinmayr, G.; Romeo, E.; de Sario, M.; Weiland, S.K.; Forastiere, F. Short-Term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: A systematic review and Meta-Analysis. Environ. Health Perspect. 2010, 118, 449–457. [Google Scholar] [CrossRef] [Green Version]
- Dastoorpoor, M.; Sekhavatpour, Z.; Masoumi, K.; Mohammadi, M.J.; Aghababaeian, H.; Khanjani, N.; Hashemzadeh, B.; Vahedian, M. Air pollution and hospital admissions for cardiovascular diseases in Ahvaz, Iran. Sci. Total Environ. 2019, 652, 1318–1330. [Google Scholar] [CrossRef]
- Janke, K. Air pollution, avoidance behaviour and children’s respiratory health: Evidence from England. J. Health Econ. 2014, 38, 23–42. [Google Scholar] [CrossRef] [Green Version]
- Szyszkowicz, M. Air pollution and emergency department visits for depression in Edmonton, Canada. Int. J. Occup. Med. Environ. 2007, 20, 241–245. [Google Scholar] [CrossRef]
- Gandini, M.; Scarinzi, C.; Bande, S.; Berti, G.; Carnà, P.; Ciancarella, L.; Costa, G.; Demaria, M.; Ghigo, S.; Piersanti, A.; et al. Long term effect of air pollution on incident hospital admissions: Results from the Italian Longitudinal Study within LIFE MED HISS project. Environ. Int. 2018, 121, 1087–1097. [Google Scholar] [CrossRef]
- Fusco, D.; Forastiere, F.; Michelozzi, P.; Spadea, T.; Ostro, B.; Arcà, M.; Perucci, C.A. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur. Respir. J. 2001, 17, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Al-Ahmadi, K.; Al-Zahrani, A. NO2 and cancer incidence in Saudi Arabia. Int. J. Environ. Res. Public Health 2013, 10, 5844–5862. [Google Scholar] [CrossRef] [PubMed]
- Hystad, P.; Demers, P.A.; Johnson, K.C.; Carpiano, R.M.; Brauer, M. Long-term residential exposure to air pollution and lung cancer risk. Epidemiology 2013, 24, 762–772. [Google Scholar] [CrossRef] [PubMed]
- Nafstad, P.; Håheim, L.L.; Oftedal, B.; Gram, F.; Holme, I.; Hjermann, I.; Leren, P. Lung cancer and air pollution: A 27 year follow up of 16 209 Norwegian men. Thorax 2003, 58, 1071–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vineis, P.; Hoek, G.; Krzyzanowski, M.; Vigna-Taglianti, F.; Veglia, F.; Airoldi, L.; Autrup, H.; Dunning, A.; Garte, S.; Hainaut, P.; et al. Air pollution and risk of lung cancer in a prospective study in Europe. Int. J. Cancer 2006, 119, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Yorifuji, T.; Kashima, S.; Tsuda, T.; Ishikawa-Takata, K.; Ohta, T.; Tsuruta, K.I.; Doi, H. Long-term exposure to traffic-related air pollution and the risk of death from hemorrhagic stroke and lung cancer in Shizuoka, Japan. Sci. Total Environ. 2013, 443, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Crouse, D.L.; Goldberg, M.S.; Ross, N.A.; Chen, H.; Labrèche, F. Postmenopausal breast cancer is associated with exposure to traffic-related air pollution in Montreal, Canada: A case-control study. Environ. Health Perspect. 2010, 118, 1578–1583. [Google Scholar] [CrossRef] [Green Version]
- Samoli, E.; Aga, E.; Touloumi, G.; Nisiotis, K.; Forsberg, B.; Lefranc, A.; Pekkanen, J.; Wojtyniak, B.; Schindler, C.; Niciu, E.; et al. Short-term effects of nitrogen dioxide on mortality: An analysis within the APHEA project. Eur. Respir. J. 2006, 27, 1129–1138. [Google Scholar] [CrossRef]
- Ancona, C.; Badaloni, C.; Mataloni, F.; Bolignano, A.; Bucci, S.; Cesaroni, G.; Sozzi, R.; Davoli, M.; Forastiere, F. Mortality and morbidity in a population exposed to multiple sources of air pollution: A retrospective cohort study using air dispersion models. Environ. Res. 2015, 137, 467–474. [Google Scholar] [CrossRef] [Green Version]
- de Marco, A.; Proietti, C.; Anav, A.; Ciancarella, L.; D’Elia, I.; Fares, S.; Fornasier, M.F.; Fusaro, L.; Gualtieri, M.; Manes, F.; et al. Impacts of air pollution on human and ecosystem health, and implications for the National Emission Ceilings Directive: Insights from Italy. Environ. Int. 2019, 125, 320–333. [Google Scholar] [CrossRef]
- Faustini, A.; Rapp, R.; Forastiere, F. Nitrogen dioxide and mortality: Review and meta-analysis of long-term studies. Eur. Respir. J. 2014, 44, 744–753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoek, G.; Krishnan, R.M.; Beelen, R.; Peters, A.; Ostro, B.; Brunekreef, B.; Kaufman, J.D. Long-term air pollution exposure and cardio-respiratory mortality: A review. Environ. Health-Glob. 2013, 12, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, R.; Samoli, E.; Wong, C.M.; Huang, W.; Wang, Z.; Chen, B.; Kan, H. Associations between short-term exposure to nitrogen dioxide and mortality in 17 Chinese cities: The China Air Pollution and Health Effects Study (CAPES). Environ. Int. 2012, 45, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Sun, Z.; Cao, J.; Wang, X.; Zhong, L.; Bi, X.; Li, H.; Liu, W.; Zhu, T.; Huang, W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013, 54, 100–111. [Google Scholar] [CrossRef]
- Tao, Y.; Huang, W.; Huang, X.; Zhong, L.; Lu, S.E.; Li, Y.; Dai, L.; Zhang, Y.; Zhu, T. Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ. Health Perspect. 2012, 120, 393–398. [Google Scholar] [CrossRef]
- Malik, A.; Tauler, R. Exploring the interaction between O3 and NOx pollution patterns in the atmosphere of Barcelona, Spain using the MCR-ALS method. Sci. Total Environ. 2015, 517, 151–161. [Google Scholar] [CrossRef]
- United Nations Department of Economic and Social Affairs. Sustainable Development Goal 3: Ensure Healthy Lives and Promote Well-Being for all at all Ages. 2021. Available online: https://sdgs.un.org/goals/goal3 (accessed on 31 September 2021).
- University of Washington Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2019 (GBD 2019) Data Resources. 2021. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 30 September 2021).
- Kaufmann, C.N.; Susukida, R.; Depp, C.A. Sleep apnea, psychopathology, and mental health care. Sleep Health 2017, 3, 244–249. [Google Scholar] [CrossRef]
- Kanner, J.; Pollack, A.Z.; Ranasinghe, S.; Stevens, D.R.; Nobles, C.; Rohn, M.C.; Sherman, S.; Mendola, P. Chronic exposure to air pollution and risk of mental health disorders complicating pregnancy. Environ. Res. 2021, 196, 110937. [Google Scholar] [CrossRef]
- Klompmaker, J.O.; Hoek, G.; Bloemsma, L.D.; Wijga, A.H.; van den Brink, C.; Brunekreef, B.; Lebret, E.; Gehring, U.; Janssen, N.A.H. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ. Int. 2019, 129, 525–537. [Google Scholar] [CrossRef]
- Pelgrims, I.; Devleesschauwer, B.; Guyot, M.; Keune, H.; Nawrot, T.S.; Remmen, R.; Saenen, N.D.; Trabelsi, S.; Thomas, I.; Aerts, R.; et al. Association between urban environment and mental health in Brussels, Belgium. BMC Public Health 2021, 21, 635. [Google Scholar] [CrossRef]
- Gu, H.; Yan, W.; Elahi, E.; Cao, Y. Air pollution risks human mental health: An implication of two-stages least squares estimation of interaction effects. Environ. Sci. Pollut. R 2020, 27, 2036–2043. [Google Scholar] [CrossRef] [PubMed]
- Newbury, J.B.; Stewart, R.; Fisher, H.L.; Beevers, S.; Dajnak, D.; Broadbent, M.; Pritchard, M.; Shiode, N.; Heslin, M.; Hammoud, R.; et al. Association between air pollution exposure and mental health service use among individuals with first presentations of psychotic and mood disorders: Retrospective cohort study. Br. J. Psychiatry 2021, 219, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Lam, H.C.; So, S.H.; Goggins, W.B.; Ho, J.Y.; Liu, S.; Chung, P.P. Association between ambient temperatures and mental disorder hospitalizations in a subtropical city: A time-series study of Hong Kong special administrative region. Int. J. Environ. Res. Public Health 2018, 15, 754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Liu, C.; Chen, R.; Wang, W.; Li, W.; Kan, H.; Fu, C. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Sci. Total Environ. 2018, 613–614, 324–330. [Google Scholar] [CrossRef]
- Oudin, A.; Åström, D.O.; Asplund, P.; Steingrimsson, S.; Szabo, Z.; Carlsen, H.K. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: A case-crossover study. Environ. Health-Glob. 2018, 17, 4. [Google Scholar] [CrossRef] [Green Version]
- Wei, F.; Wu, M.; Qian, S.; Li, D.; Jin, M.; Wang, J.; Shui, L.; Lin, H.; Tang, M.; Chen, K. Association between short-term exposure to ambient air pollution and hospital visits for depression in China. Sci. Total Environ. 2020, 724, 138207. [Google Scholar] [CrossRef]
- Lu, P.; Zhang, Y.; Xia, G.; Zhang, W.; Xu, R.; Wang, C.; Guo, Y.; Li, S. Attributable risks associated with hospital outpatient visits for mental disorders due to air pollution: A multi-city study in China. Environ. Int. 2020, 143, 105906. [Google Scholar] [CrossRef]
- Thilakaratne, R.A.; Malig, B.J.; Basu, R. Examining the relationship between ambient carbon monoxide, nitrogen dioxide, and mental health-related emergency department visits in California, USA. Sci. Total Environ. 2020, 746, 140915. [Google Scholar] [CrossRef]
- Li, H.; Zhang, S.; Qian, Z.; Xie, X.H.; Luo, Y.; Han, R.; Hou, J.; Wang, C.; McMillin, S.E.; Wu, S.; et al. Short-term effects of air pollution on cause-specific mental disorders in three subtropical Chinese cities. Environ. Res. 2020, 191, 110214. [Google Scholar] [CrossRef]
- Tong, L.; Li, K.; Zhou, Q. Season, sex and age as modifiers in the association of psychosis morbidity with air pollutants: A rising problem in a Chinese metropolis. Sci. Total Environ. 2016, 541, 928–933. [Google Scholar] [CrossRef]
- Billings, M.E.; Gold, D.; Szpiro, A.; Aaron, C.P.; Jorgensen, N.; Gassett, A.; Leary, P.L.; Kaufman, J.D.; Redline, S.R. The association of ambient air pollution with sleep apnea: The multi-ethnic study of atherosclerosis. Ann. Am. Thorac. Soc. 2019, 16, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, W.R.; Yang, M.; Zhang, C.; Liu, R.Q.; Lin, S.; Wang, S.Q.; Liu, Y.; Ma, H.; Chen, D.H.; Zeng, X.W.; et al. Association between long-term exposure to air pollution and sleep disorder in Chinese children: The Seven Northeastern Cities study. Sleep 2018, 41, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Vert, C.; Sánchez-Benavides, G.; Martínez, D.; Gotsens, X.; Gramunt, N.; Cirach, M.; Molinuevo, J.L.; Sunyer, J.; Nieuwenhuijsen, M.J.; Crous-Bou, M.; et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: A cross-sectional study. Int. J. Hyg. Environ. Health 2017, 220, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Park, J.Y.; Choi, J. Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE 2018, 13, e0195607. [Google Scholar] [CrossRef] [Green Version]
- Lim, Y.H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.C. Air Pollution and Symptoms of Depression in Elderly Adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Eliot, M.N.; Koutrakis, P.; Gryparis, A.; Schwartz, J.D.; Coull, B.A.; Mittleman, M.A.; Milberg, W.P.; Lipsitz, L.A.; Wellenius, G.A. Ambient air pollution and depressive symptoms in older adults: Results from the MOBILIZE Boston study. Environ. Health Perspect. 2014, 122, 553–558. [Google Scholar] [CrossRef]
- Zijlema, W.L.; Wolf, K.; Emeny, R.; Ladwig, K.H.; Peters, A.; Kongsgård, H.; Hveem, K.; Kvaløy, K.; Yli-Tuomi, T.; Partonen, T.; et al. The association of air pollution and depressed mood in 70,928 individuals from four European cohorts. Int. J. Hyg. Environ. Health 2016, 219, 212–219. [Google Scholar] [CrossRef] [Green Version]
- Altuğ, H.; Fuks, K.B.; Hüls, A.; Mayer, A.K.; Tham, R.; Krutmann, J.; Schikowski, T. Air pollution is associated with depressive symptoms in elderly women with cognitive impairment. Environ. Int. 2020, 136, 105448. [Google Scholar] [CrossRef]
- Kim, S.Y.; Bang, M.; Wee, J.H.; Min, C.; Yoo, D.M.; Han, S.M.; Kim, S.; Choi, H.G. Short- and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: A nested case-control study using meteorological data and national sample cohort data. Sci. Total Environ. 2021, 757, 143960. [Google Scholar] [CrossRef]
- Lo, K.; Chiang, L.L.; Hsu, S.M.; Tsai, C.Y.; Wu, D.; Chou, C.J.; Chuang, H.C.; Liu, W.T. Association of short-term exposure to air pollution with depression in patients with sleep-related breathing disorders. Sci. Total Environ. 2021, 786, 147291. [Google Scholar] [CrossRef]
- Latham, R.M.; Kieling, C.; Arseneault, L.; Botter-Maio Rocha, T.; Beddows, A.; Beevers, S.; Danese, A.; De Oliveira, K.; Kohrt, B.A.; Moffitt, T.E.; et al. Childhood exposure to ambient air pollution and predicting individual risk of depression onset in UK adolescents. J. Psychiatry Res. 2021, 138, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Rowe, B.; Colman, I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. 2009, 22, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Kousha, T.; Kingsbury, M.; Colman, I. Air Pollution and Emergency Department Visits for Depression: A Multicity Case-Crossover Study. Environ. Health Insights 2016, 10, 155–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, J.; Choi, Y.J.; Suh, M.; Sohn, J.; Kim, H.; Cho, S.K.; Ha, K.H.; Kim, C.; Shin, D.C. Air pollution as a risk factor for depressive episode in patients with cardiovascular disease, diabetes mellitus, or asthma. J. Affect. Disord. 2014, 157, 45–51. [Google Scholar] [CrossRef]
- Zhou, Y.M.; An, S.J.; Tang, E.J.; Xu, C.; Cao, Y.; Liu, X.L.; Yao, C.Y.; Xiao, H.; Zhang, Q.; Liu, F.; et al. Association between short-term ambient air pollution exposure and depression outpatient visits in cold seasons: A time-series analysis in northwestern China. J. Toxicol. Environ. Health A 2021, 84, 389–398. [Google Scholar] [CrossRef]
- Gu, X.; Guo, T.; Si, Y.; Wang, J.; Zhang, W.; Deng, F.; Chen, L.; Wei, C.; Lin, S.; Guo, X.; et al. Association between ambient air pollution and daily hospital admissions for depression in 75 Chinese cities. Am. J. Psychiatry 2020, 177, 735–743. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Willey, J.B.; Grafstein, E.; Rowe, B.H.; Colman, I. Air Pollution and Emergency Department Visits for Suicide Attempts in Vancouver, Canada. Environ. Health Insights 2010, 4, 79–86. [Google Scholar] [CrossRef]
- Min, J.; Kim, H.J.; Min, K. Long-term exposure to air pollution and the risk of suicide death: A population-based cohort study. Sci. Total Environ. 2018, 628–629, 573–579. [Google Scholar] [CrossRef]
- Ng, C.F.; Stickley, A.; Konishi, S.; Watanabe, C. Ambient air pollution and suicide in Tokyo, 2001–2011. J. Affect. Disord. 2016, 201, 194–202. [Google Scholar] [CrossRef]
- Kim, Y.; Ng, C.F.; Chung, Y.; Kim, H.; Honda, Y.; Guo, Y.L.; Lim, Y.H.; Chen, B.Y.; Page, L.A.; Hashizume, M. Air pollution and suicide in 10 cities in Northeast Asia: A time-stratified case-crossover analysis. Environ. Health Perspect. 2018, 126, 037002. [Google Scholar] [CrossRef] [Green Version]
- Bakian, A.; Huber, R.S.; Coon, H.; Gray, D.; Wilson, P.; McMahon, W.M.; Renshaw, P.F. Acute air pollution exposure and risk of suicide completion. Am. J. Epidemiol. 2015, 181, 295–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IQAir. 2020 World Air Quality Report: Region & City PM2.5 Ranking. Available online: https://www.iqair.com/ca/world-most-polluted-countries (accessed on 10 December 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).