An Evaluation of Risk Ratios on Physical and Mental Health Correlations due to Increases in Ambient Nitrogen Oxide (NOx) Concentrations
Abstract
:1. Introduction
2. Nitrogen Oxides (NOx) as a Targeted Pollutant
3. Methodology, Considerations and Contribution of Research
3.1. Methodology
3.1.1. Overview
3.1.2. Data Collection
3.1.3. Risk Ratio Conversion
3.2. Considerations
3.3. Research Contribution
4. Physical Health Impacts of NOx
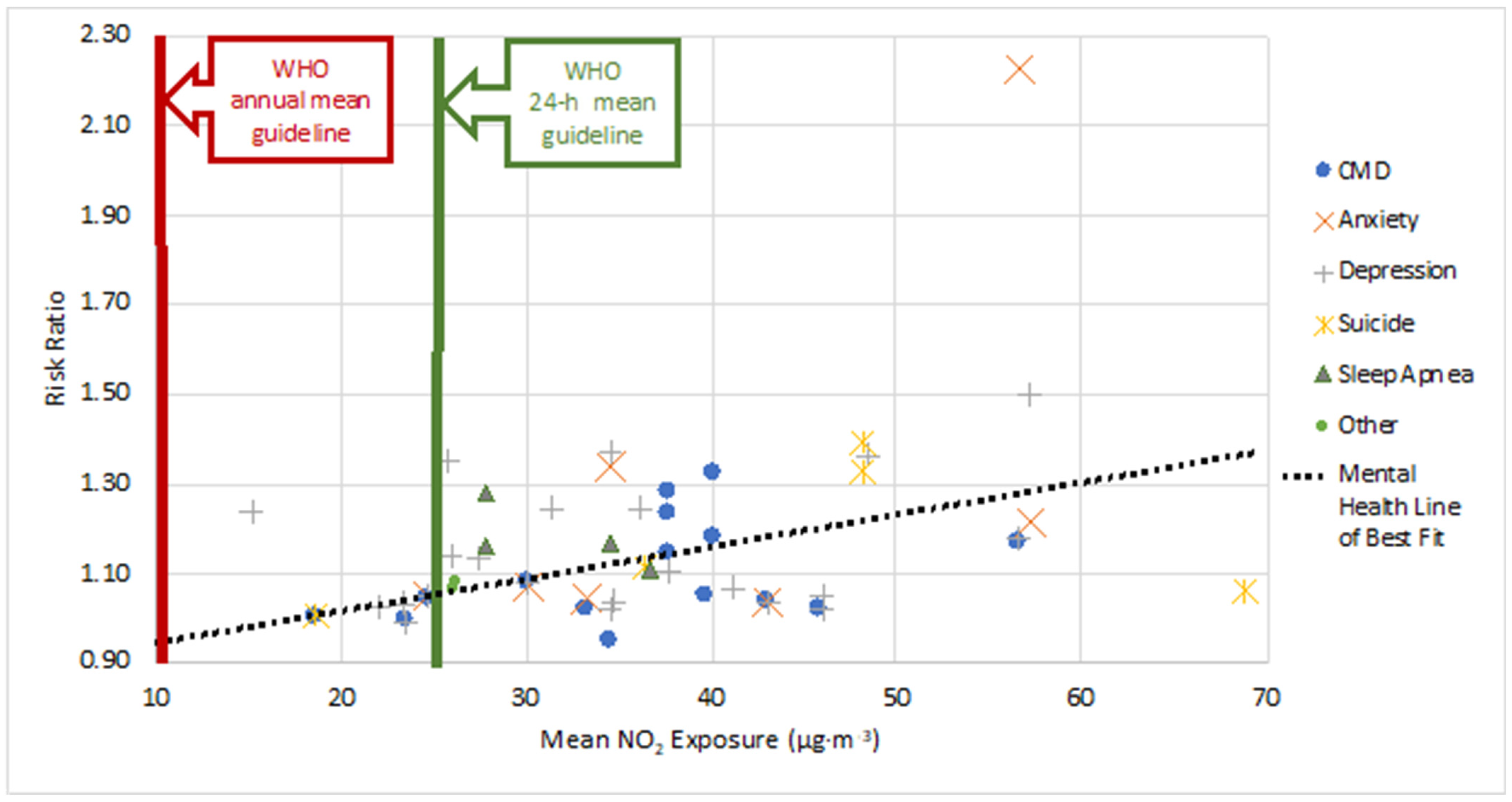
5. Mental Health Impacts of NOx
6. Physical and Mental Health with NO2 Exposure Relative Risk
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| CMD | Common Mental Disorder |
| COPD | Chronic Obstructive Pulmonary Disorder |
| HONO | Nitrous Acid |
| NOS | Nitric Oxide Synthase |
| NO | Nitric Oxide |
| NO2 | Nitrogen Dioxide |
| NOx | Nitrogen Oxides |
| O3 | Ozone |
| OR | Odds Ratio |
| PM | Particulate Matter |
| ROS | Reactive Oxygen Species |
| RR | Risk Ratio |
| SIA | Secondary Inorganic Aerosol |
| SOA | Secondary Organic Aerosol |
| UN | United Nations |
| VOC | Volatile Organic Compound |
| WHO | World Health Organization |
References
- Smith, R.; McDougal, K. Costs of Pollution in Canada: Measuring the Impacts on Families, Businesses and Governments; International Institute for Sustainable Development: Winnipeg, MB, Canada, 2017. [Google Scholar]
- Liu, G.; Xiao, M.; Zhang, X.; Gal, C.; Chen, X.; Liu, L.; Pan, S.; Wu, J.; Tang, L.; Clements-Croome, D.; et al. A review of air filtration technologies for sustainable and healthy building ventilation. Sustain. Cities Soc. 2017, 32, 375–396. [Google Scholar] [CrossRef]
- Johansson, C.; Lövenheim, B.; Schantz, P.; Wahlgren, L.; Almström, P.; Markstedt, A.; Strömgren, M.; Forsberg, B.; Sommar, J.N. Impacts on air pollution and health by changing commuting from car to bicycle. Sci. Total Environ. 2017, 584–585, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Gorai, A.K.; Kanchan Upadhyay, A.; Tuluri, F.; Goyal, P.; Tchounwou, P.B. An innovative approach for determination of air quality health index. Sci. Total Environ. 2015, 533, 495–505. [Google Scholar] [CrossRef] [Green Version]
- World Bank. The Cost of Air Pollution: Strengthening the Economic Case for Action; World Bank Group: Washington, DC, USA, 2016. [Google Scholar]
- Canadian Council of Ministers of the Environment. 2017 Air Quality, Canadian Ambient Air Quality Standards (CAAQS). Available online: http://airquality-qualitedelair.ccme.ca/en/ (accessed on 20 January 2021).
- World Health Organization. Ambient (Outdoor) Air Pollution. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 21 October 2021).
- Mason, T.G.; Schooling, C.M.; Chan, K.P.; Tian, L. An evaluation of the air quality health index program on respiratory diseases in Hong Kong: An interrupted time series analysis. Atmos. Environ. 2019, 211, 151–158. [Google Scholar] [CrossRef]
- Kumar, P.; Skouloudis, A.N.; Bell, M.; Viana, M.; Carotta, M.C.; Biskos, G.; Morawska, L. Real-time sensors for indoor air monitoring and challenges ahead in deploying them to urban buildings. Sci. Total Environ. 2016, 560–561, 150–159. [Google Scholar] [CrossRef] [Green Version]
- Patelarou, E.; Tzanakis, N.; Kelly, F.J. Exposure to indoor pollutants and wheeze and asthma development during early childhood. Int. J. Environ. Res. Public Health 2015, 12, 3993–4017. [Google Scholar] [CrossRef] [Green Version]
- World Bank. Pollution. 2021. Available online: https://www.worldbank.org/en/topic/pollution#:~:text=According%20to%20the%20World%20Bank,to%204.8%25%20of%20global%20GDP (accessed on 2 February 2021).
- Bakolis, I.; Hammoud, R.; Stewart, R.; Beevers, S.; Dajnak, D.; MacCrimmon, S.; Broadbent, M.; Pritchard, M.; Shiode, N.; Fecht, D.; et al. Mental health consequences of urban air pollution: Prospective population-based longitudinal survey. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1587–1599. [Google Scholar] [CrossRef]
- Rehm, J.; Shield, K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019, 21, 10. [Google Scholar] [CrossRef]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 30 October 2018).
- César, A.C.; Carvalho, J.A.; Nascimento, L.F. Association between NOx exposure and deaths caused by respiratory diseases in a medium-sized Brazilian city. Braz. J. Med. Biol. Res. 2015, 48, 1130–1135. [Google Scholar] [CrossRef] [Green Version]
- Chaloulakou, A.; Mavroidis, I.; Gavriil, I. Compliance with the annual NO2 air quality standard in Athens. Required NOx levels and expected health implications. Atmos. Environ. 2008, 42, 454–465. [Google Scholar] [CrossRef]
- Zouzelka, R.; Rathousky, J. Photocatalytic abatement of NOx pollutants in the air using commercial functional coating with porous morphology. Appl. Catal. B-Environ. 2017, 217, 466–476. [Google Scholar] [CrossRef]
- Jacob, D.J. Introduction to Atmospheric Chemistry; Chapter 11: Oxidizing Power of the Atmosphere; Princeton University Press: Princeton, NJ, USA, 1999; pp. 199–219. [Google Scholar]
- Liu, F.; Beirle, S.; Zhang, Q.; Dörner, S.; He, K.; Wagner, T. NOx lifetimes and emissions of cities and power plants in polluted background estimated by satellite observations. Atmos. Chem. Phys. 2016, 16, 5283–5298. [Google Scholar] [CrossRef] [Green Version]
- Shah, V.; Jacob, D.; Li, K.; Silvern, R.; Zhai, S.; Liu, M.; Lin, J.; Zhang, Q. Effect of changing NOx; lifetime on the seasonality and long-term trends of satellite-observed tropospheric NO2; columns over China. Atmos. Chem. Phys. Discuss. 2019, 670, 1–23. [Google Scholar] [CrossRef]
- Bélanger, D.; Berry, P. Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity; Health Canada: Ottawa, ON, Canada, 2008.
- Boubel, R.W.; Fox, D.L.; Turner, D.B.; Stern, A.C. Fundamentals of Air Pollution, 3rd ed.; Chapter 7 Effects on Health and Human Welfare and Chapter 12 Atmospheric Chemistry; Academic Press: Cambridge, MA, USA, 1994; pp. 99–109,165–177. [Google Scholar]
- Muilwijk, C.; Schrijvers, P.J.; Wuerz, S.; Kenjereš, S. Simulations of photochemical smog formation in complex urban areas. Atmos. Environ. 2016, 147, 470–484. [Google Scholar] [CrossRef]
- Seinfield, J.H.; Pandis, S.N. Atmospheric Chemistry and Physics, 3rd ed.; Chapter 2.7: Particulate Matter (Aerosols); John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006; pp. 48–54. [Google Scholar]
- Cheng, M.; Tang, G.; Lv, B.; Li, X.; Wu, X.; Wang, Y.; Wang, Y. Source apportionment of PM2.5 and visibility in Jinan, China. J. Environ. Sci. 2021, 102, 207–2015. [Google Scholar] [CrossRef]
- Zhao, Z.; Lv, S.; Zhang, Y.; Zhao, Q.; Shen, L.; Xu, S.; Yu, J.; Hou, J.; Jin, C. Characteristics and source apportionment of PM 2.5 in Jiaxing, China. Environ. Sci. Pollut. Res. 2019, 26, 7497–7511. [Google Scholar] [CrossRef]
- Atkinson, R.W.; Butland, B.K.; Anderson, H.R.; Maynard, R.L. Long-term concentrations of nitrogen dioxide and mortality: A meta-analysis of cohort studies. Epidemiology 2018, 29, 460–472. [Google Scholar] [CrossRef]
- Łopuszańska, U.; Makara-Studzińska, M. The correlations between air pollution and depression. Curr. Probl. Psychiatry 2017, 18, 100–109. [Google Scholar] [CrossRef] [Green Version]
- Gładka, A.; Rymaszewska, J.; Zatoński, T. Impact of air pollution on depression and suicide. Int. J. Occup. Med. Environ. 2018, 31, 711–721. [Google Scholar] [CrossRef]
- Zeng, Y.; Lin, R.; Liu, L.; Liu, Y.; Li, Y. Ambient air pollution exposure and risk of depression: A systematic review and meta-analysis of observational studies. Psychiatry Res. 2019, 276, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Borroni, E.; Pesatori, A.C.; Bollati, V.; Buoli, M.; Carugno, M. Air pollution exposure and depression: A comprehensive updated systematic review and meta-analysis. Environ. Pollut. 2022, 292, 11845. [Google Scholar] [CrossRef] [PubMed]
- Buoli, M.; Grassi, S.; Caldiroli, A.; Carnevali, G.S.; Mucci, F.; Iodice, S.; Cantone, L.; Pergoli, L.; Bollati, V. Is there a link between air pollution and mental disorders? Environ. Int. 2018, 118, 154–168. [Google Scholar] [CrossRef]
- Viera, A.J. Odds ratios and risk ratios: What’s the difference and why does it matter? South Med. J. 2008, 101, 730–734. [Google Scholar] [CrossRef]
- Krzeszowiak, J.; Stefanow, D.; Pawlas, K. The impact of particulate matter (PM) and nitric oxides (NOx) on human health and an analysis of selected sources accounting for their emission. Med. Sr.—Environ. Med. 2016, 19, 3–15. [Google Scholar] [CrossRef]
- Anyanwu, E. Complex interconvertibility of nitrogen oxides (NOx): Impact on occupational and environmental health. Rev. Environ. Health 1999, 14, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Mohsenin, V. Human exposure to oxides of nitrogen at ambient and supra-ambient concentrations. Toxicology 1994, 89, 301–312. [Google Scholar] [CrossRef]
- Munawer, M.E. Human health and environmental impacts of coal combustion and post-combustion wastes. J. Sustain. Min. 2018, 17, 87–96. [Google Scholar] [CrossRef]
- Skouloudis, A.N.; Kassomenos, P. Combining environment and health information systems for the assessment of atmospheric pollution on human health. Sci. Total Environ. 2014, 488–489, 362–368. [Google Scholar] [CrossRef]
- Vasev, N. Governing energy while neglecting health—The case of Poland. Health Policy 2017, 121, 1147–1153. [Google Scholar] [CrossRef]
- Lu, X.; Yao, T.; Li, Y.; Fung, J.C.; Lau, A.K. Source apportionment and health effect of NOx over the Pearl River Delta region in southern China. Environ. Pollut. 2016, 212, 135–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zock, J.P.; Verheij, R.; Helbich, M.; Volker, B.; Spreeuwenberg, P.; Strak, M.; Janssen, N.A.H.; Dijst, M.; Groenewegen, P. The impact of social capital, land use, air pollution and noise on individual morbidity in Dutch neighbourhoods. Environ. Int. 2018, 121, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Palmgren, F.; Berkowicz, R.; Hertel, O.; Vignati, E. Effects of reduction of NOx on the NO2 levels in urban streets. Sci. Total Environ. 1996, 189–190, 409–415. [Google Scholar] [CrossRef]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242. [Google Scholar] [CrossRef]
- Mi, Y.H.; Norbäck, D.; Tao, J.; Mi, Y.L.; Ferm, M. Current asthma and respiratory symptoms among pupils in Shanghai, China: Influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air 2006, 16, 454–464. [Google Scholar] [CrossRef]
- Anderson, H.R.; Atkinson, R.W.; Bremmer, S.A.; Carrington, J.; Peacock, P. Quantitative Systematic Review of Short Term Associations between Ambient Air Pollution (Particulate Matter, Ozone, Nitrogen Dioxide, Sulphur Dioxide and Carbon Monoxide), and Mortality and Morbidity; Division of Community Health Sciences St George’s—University of London: London, UK, 2007. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215975/dh_121202.pdf (accessed on 26 November 2021).
- Kirsch, M.; Korth, H.G.; Sustmann, R.; de Groot, H. The pathobiochemistry of nitrogen dioxide. Biol. Chem. 2002, 383, 389–399. [Google Scholar] [CrossRef]
- McConnell, R.; Berhane, K.; Gilliland, F.; Molitor, J.; Thomas, D.; Lurmann, F.; Avol, E.; Gauderman, W.J.; Peters, J.M. Prospective study of air pollution and bronchitic symptoms in children with asthma. Am. J. Respir. Crit. Care 2003, 168, 790–797. [Google Scholar] [CrossRef] [Green Version]
- Rivas, E.; Santiago, J.L.; Lechón, Y.; Martín, F.; Ariño, A.; Pons, J.J.; Santamaría, J.M. CFD modelling of air quality in Pamplona City (Spain): Assessment, stations spatial representativeness and health impacts valuation. Sci. Total Environ. 2019, 649, 1362–1380. [Google Scholar] [CrossRef]
- Alexeeff, S.E.; Roy, A.; Shan, J.; Liu, X.; Messier, K.; Apte, J.S.; Portier, C.; Sidney, S.; Van Den Eeden, S.K. High-resolution mapping of traffic related air pollution with Google street view cars and incidence of cardiovascular events within neighborhoods in Oakland, CA. Environ. Health-Glob. 2018, 17, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Beelen, R.; Hoek, G.; van den Brandt, P.A.; Goldbohm, R.A.; Fischer, P.; Schouten, L.J. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ. Health Perspect. 2008, 116, 196–202. [Google Scholar] [CrossRef]
- Chen, H.; Goldberg, M.S.; Burnett, R.T.; Jerrett, M.; Wheeler, A.J.; Villeneuve, P.J. Long-term exposure to traffic-related air pollution and cardiovascular mortality. Epidemiology 2013, 24, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Gan, W.Q.; Koehoorn, M.; Davies, H.W.; Demers, P.A.; Tamburic, L.; Brauer, M. Long-term exposure to traffic-related air pollution and the risk of coronary heart disease hospitalization and mortality. Environ. Health Perspect. 2011, 119, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Jerrett, M.; Burnett, R.T.; Beckerman, B.S.; Turner, M.C.; Krewski, D.; Thurston, G.; Martin, R.V.; van Donkelaar, A.; Hughes, E.; Shi, Y. Spatial analysis of air pollution and mortality in California. Am. J. Respir. Crit. Care 2013, 188, 593–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raaschou-Nielsen, O.; Hermansen, M.N.; Loland, L.; Buchvald, F.; Pipper, C.B.; Sørensen, M.; Loft, S.; Bisgaard, H. Long-term exposure to indoor air pollution and wheezing symptoms in infants. Indoor Air 2010, 20, 159–167. [Google Scholar] [CrossRef]
- Rijnders, E.; Janssen, N.A.; van Vliet, P.H.; Brunekreef, B. Personal and outdoor nitrogen dioxide concentrations in relation to degree of urbanization and traffic density. Environ. Health Perspect. 2001, 109, 411–417. [Google Scholar] [CrossRef] [Green Version]
- Weinmayr, G.; Romeo, E.; de Sario, M.; Weiland, S.K.; Forastiere, F. Short-Term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: A systematic review and Meta-Analysis. Environ. Health Perspect. 2010, 118, 449–457. [Google Scholar] [CrossRef] [Green Version]
- Dastoorpoor, M.; Sekhavatpour, Z.; Masoumi, K.; Mohammadi, M.J.; Aghababaeian, H.; Khanjani, N.; Hashemzadeh, B.; Vahedian, M. Air pollution and hospital admissions for cardiovascular diseases in Ahvaz, Iran. Sci. Total Environ. 2019, 652, 1318–1330. [Google Scholar] [CrossRef]
- Janke, K. Air pollution, avoidance behaviour and children’s respiratory health: Evidence from England. J. Health Econ. 2014, 38, 23–42. [Google Scholar] [CrossRef] [Green Version]
- Szyszkowicz, M. Air pollution and emergency department visits for depression in Edmonton, Canada. Int. J. Occup. Med. Environ. 2007, 20, 241–245. [Google Scholar] [CrossRef]
- Gandini, M.; Scarinzi, C.; Bande, S.; Berti, G.; Carnà, P.; Ciancarella, L.; Costa, G.; Demaria, M.; Ghigo, S.; Piersanti, A.; et al. Long term effect of air pollution on incident hospital admissions: Results from the Italian Longitudinal Study within LIFE MED HISS project. Environ. Int. 2018, 121, 1087–1097. [Google Scholar] [CrossRef]
- Fusco, D.; Forastiere, F.; Michelozzi, P.; Spadea, T.; Ostro, B.; Arcà, M.; Perucci, C.A. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur. Respir. J. 2001, 17, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Al-Ahmadi, K.; Al-Zahrani, A. NO2 and cancer incidence in Saudi Arabia. Int. J. Environ. Res. Public Health 2013, 10, 5844–5862. [Google Scholar] [CrossRef] [PubMed]
- Hystad, P.; Demers, P.A.; Johnson, K.C.; Carpiano, R.M.; Brauer, M. Long-term residential exposure to air pollution and lung cancer risk. Epidemiology 2013, 24, 762–772. [Google Scholar] [CrossRef] [PubMed]
- Nafstad, P.; Håheim, L.L.; Oftedal, B.; Gram, F.; Holme, I.; Hjermann, I.; Leren, P. Lung cancer and air pollution: A 27 year follow up of 16 209 Norwegian men. Thorax 2003, 58, 1071–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vineis, P.; Hoek, G.; Krzyzanowski, M.; Vigna-Taglianti, F.; Veglia, F.; Airoldi, L.; Autrup, H.; Dunning, A.; Garte, S.; Hainaut, P.; et al. Air pollution and risk of lung cancer in a prospective study in Europe. Int. J. Cancer 2006, 119, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Yorifuji, T.; Kashima, S.; Tsuda, T.; Ishikawa-Takata, K.; Ohta, T.; Tsuruta, K.I.; Doi, H. Long-term exposure to traffic-related air pollution and the risk of death from hemorrhagic stroke and lung cancer in Shizuoka, Japan. Sci. Total Environ. 2013, 443, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Crouse, D.L.; Goldberg, M.S.; Ross, N.A.; Chen, H.; Labrèche, F. Postmenopausal breast cancer is associated with exposure to traffic-related air pollution in Montreal, Canada: A case-control study. Environ. Health Perspect. 2010, 118, 1578–1583. [Google Scholar] [CrossRef] [Green Version]
- Samoli, E.; Aga, E.; Touloumi, G.; Nisiotis, K.; Forsberg, B.; Lefranc, A.; Pekkanen, J.; Wojtyniak, B.; Schindler, C.; Niciu, E.; et al. Short-term effects of nitrogen dioxide on mortality: An analysis within the APHEA project. Eur. Respir. J. 2006, 27, 1129–1138. [Google Scholar] [CrossRef]
- Ancona, C.; Badaloni, C.; Mataloni, F.; Bolignano, A.; Bucci, S.; Cesaroni, G.; Sozzi, R.; Davoli, M.; Forastiere, F. Mortality and morbidity in a population exposed to multiple sources of air pollution: A retrospective cohort study using air dispersion models. Environ. Res. 2015, 137, 467–474. [Google Scholar] [CrossRef] [Green Version]
- de Marco, A.; Proietti, C.; Anav, A.; Ciancarella, L.; D’Elia, I.; Fares, S.; Fornasier, M.F.; Fusaro, L.; Gualtieri, M.; Manes, F.; et al. Impacts of air pollution on human and ecosystem health, and implications for the National Emission Ceilings Directive: Insights from Italy. Environ. Int. 2019, 125, 320–333. [Google Scholar] [CrossRef]
- Faustini, A.; Rapp, R.; Forastiere, F. Nitrogen dioxide and mortality: Review and meta-analysis of long-term studies. Eur. Respir. J. 2014, 44, 744–753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoek, G.; Krishnan, R.M.; Beelen, R.; Peters, A.; Ostro, B.; Brunekreef, B.; Kaufman, J.D. Long-term air pollution exposure and cardio-respiratory mortality: A review. Environ. Health-Glob. 2013, 12, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, R.; Samoli, E.; Wong, C.M.; Huang, W.; Wang, Z.; Chen, B.; Kan, H. Associations between short-term exposure to nitrogen dioxide and mortality in 17 Chinese cities: The China Air Pollution and Health Effects Study (CAPES). Environ. Int. 2012, 45, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Sun, Z.; Cao, J.; Wang, X.; Zhong, L.; Bi, X.; Li, H.; Liu, W.; Zhu, T.; Huang, W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013, 54, 100–111. [Google Scholar] [CrossRef]
- Tao, Y.; Huang, W.; Huang, X.; Zhong, L.; Lu, S.E.; Li, Y.; Dai, L.; Zhang, Y.; Zhu, T. Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ. Health Perspect. 2012, 120, 393–398. [Google Scholar] [CrossRef]
- Malik, A.; Tauler, R. Exploring the interaction between O3 and NOx pollution patterns in the atmosphere of Barcelona, Spain using the MCR-ALS method. Sci. Total Environ. 2015, 517, 151–161. [Google Scholar] [CrossRef]
- United Nations Department of Economic and Social Affairs. Sustainable Development Goal 3: Ensure Healthy Lives and Promote Well-Being for all at all Ages. 2021. Available online: https://sdgs.un.org/goals/goal3 (accessed on 31 September 2021).
- University of Washington Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2019 (GBD 2019) Data Resources. 2021. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 30 September 2021).
- Kaufmann, C.N.; Susukida, R.; Depp, C.A. Sleep apnea, psychopathology, and mental health care. Sleep Health 2017, 3, 244–249. [Google Scholar] [CrossRef]
- Kanner, J.; Pollack, A.Z.; Ranasinghe, S.; Stevens, D.R.; Nobles, C.; Rohn, M.C.; Sherman, S.; Mendola, P. Chronic exposure to air pollution and risk of mental health disorders complicating pregnancy. Environ. Res. 2021, 196, 110937. [Google Scholar] [CrossRef]
- Klompmaker, J.O.; Hoek, G.; Bloemsma, L.D.; Wijga, A.H.; van den Brink, C.; Brunekreef, B.; Lebret, E.; Gehring, U.; Janssen, N.A.H. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ. Int. 2019, 129, 525–537. [Google Scholar] [CrossRef]
- Pelgrims, I.; Devleesschauwer, B.; Guyot, M.; Keune, H.; Nawrot, T.S.; Remmen, R.; Saenen, N.D.; Trabelsi, S.; Thomas, I.; Aerts, R.; et al. Association between urban environment and mental health in Brussels, Belgium. BMC Public Health 2021, 21, 635. [Google Scholar] [CrossRef]
- Gu, H.; Yan, W.; Elahi, E.; Cao, Y. Air pollution risks human mental health: An implication of two-stages least squares estimation of interaction effects. Environ. Sci. Pollut. R 2020, 27, 2036–2043. [Google Scholar] [CrossRef] [PubMed]
- Newbury, J.B.; Stewart, R.; Fisher, H.L.; Beevers, S.; Dajnak, D.; Broadbent, M.; Pritchard, M.; Shiode, N.; Heslin, M.; Hammoud, R.; et al. Association between air pollution exposure and mental health service use among individuals with first presentations of psychotic and mood disorders: Retrospective cohort study. Br. J. Psychiatry 2021, 219, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.Y.; Lam, H.C.; So, S.H.; Goggins, W.B.; Ho, J.Y.; Liu, S.; Chung, P.P. Association between ambient temperatures and mental disorder hospitalizations in a subtropical city: A time-series study of Hong Kong special administrative region. Int. J. Environ. Res. Public Health 2018, 15, 754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Liu, C.; Chen, R.; Wang, W.; Li, W.; Kan, H.; Fu, C. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Sci. Total Environ. 2018, 613–614, 324–330. [Google Scholar] [CrossRef]
- Oudin, A.; Åström, D.O.; Asplund, P.; Steingrimsson, S.; Szabo, Z.; Carlsen, H.K. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: A case-crossover study. Environ. Health-Glob. 2018, 17, 4. [Google Scholar] [CrossRef] [Green Version]
- Wei, F.; Wu, M.; Qian, S.; Li, D.; Jin, M.; Wang, J.; Shui, L.; Lin, H.; Tang, M.; Chen, K. Association between short-term exposure to ambient air pollution and hospital visits for depression in China. Sci. Total Environ. 2020, 724, 138207. [Google Scholar] [CrossRef]
- Lu, P.; Zhang, Y.; Xia, G.; Zhang, W.; Xu, R.; Wang, C.; Guo, Y.; Li, S. Attributable risks associated with hospital outpatient visits for mental disorders due to air pollution: A multi-city study in China. Environ. Int. 2020, 143, 105906. [Google Scholar] [CrossRef]
- Thilakaratne, R.A.; Malig, B.J.; Basu, R. Examining the relationship between ambient carbon monoxide, nitrogen dioxide, and mental health-related emergency department visits in California, USA. Sci. Total Environ. 2020, 746, 140915. [Google Scholar] [CrossRef]
- Li, H.; Zhang, S.; Qian, Z.; Xie, X.H.; Luo, Y.; Han, R.; Hou, J.; Wang, C.; McMillin, S.E.; Wu, S.; et al. Short-term effects of air pollution on cause-specific mental disorders in three subtropical Chinese cities. Environ. Res. 2020, 191, 110214. [Google Scholar] [CrossRef]
- Tong, L.; Li, K.; Zhou, Q. Season, sex and age as modifiers in the association of psychosis morbidity with air pollutants: A rising problem in a Chinese metropolis. Sci. Total Environ. 2016, 541, 928–933. [Google Scholar] [CrossRef]
- Billings, M.E.; Gold, D.; Szpiro, A.; Aaron, C.P.; Jorgensen, N.; Gassett, A.; Leary, P.L.; Kaufman, J.D.; Redline, S.R. The association of ambient air pollution with sleep apnea: The multi-ethnic study of atherosclerosis. Ann. Am. Thorac. Soc. 2019, 16, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, W.R.; Yang, M.; Zhang, C.; Liu, R.Q.; Lin, S.; Wang, S.Q.; Liu, Y.; Ma, H.; Chen, D.H.; Zeng, X.W.; et al. Association between long-term exposure to air pollution and sleep disorder in Chinese children: The Seven Northeastern Cities study. Sleep 2018, 41, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Vert, C.; Sánchez-Benavides, G.; Martínez, D.; Gotsens, X.; Gramunt, N.; Cirach, M.; Molinuevo, J.L.; Sunyer, J.; Nieuwenhuijsen, M.J.; Crous-Bou, M.; et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: A cross-sectional study. Int. J. Hyg. Environ. Health 2017, 220, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Park, J.Y.; Choi, J. Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE 2018, 13, e0195607. [Google Scholar] [CrossRef] [Green Version]
- Lim, Y.H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.C. Air Pollution and Symptoms of Depression in Elderly Adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Eliot, M.N.; Koutrakis, P.; Gryparis, A.; Schwartz, J.D.; Coull, B.A.; Mittleman, M.A.; Milberg, W.P.; Lipsitz, L.A.; Wellenius, G.A. Ambient air pollution and depressive symptoms in older adults: Results from the MOBILIZE Boston study. Environ. Health Perspect. 2014, 122, 553–558. [Google Scholar] [CrossRef]
- Zijlema, W.L.; Wolf, K.; Emeny, R.; Ladwig, K.H.; Peters, A.; Kongsgård, H.; Hveem, K.; Kvaløy, K.; Yli-Tuomi, T.; Partonen, T.; et al. The association of air pollution and depressed mood in 70,928 individuals from four European cohorts. Int. J. Hyg. Environ. Health 2016, 219, 212–219. [Google Scholar] [CrossRef] [Green Version]
- Altuğ, H.; Fuks, K.B.; Hüls, A.; Mayer, A.K.; Tham, R.; Krutmann, J.; Schikowski, T. Air pollution is associated with depressive symptoms in elderly women with cognitive impairment. Environ. Int. 2020, 136, 105448. [Google Scholar] [CrossRef]
- Kim, S.Y.; Bang, M.; Wee, J.H.; Min, C.; Yoo, D.M.; Han, S.M.; Kim, S.; Choi, H.G. Short- and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: A nested case-control study using meteorological data and national sample cohort data. Sci. Total Environ. 2021, 757, 143960. [Google Scholar] [CrossRef]
- Lo, K.; Chiang, L.L.; Hsu, S.M.; Tsai, C.Y.; Wu, D.; Chou, C.J.; Chuang, H.C.; Liu, W.T. Association of short-term exposure to air pollution with depression in patients with sleep-related breathing disorders. Sci. Total Environ. 2021, 786, 147291. [Google Scholar] [CrossRef]
- Latham, R.M.; Kieling, C.; Arseneault, L.; Botter-Maio Rocha, T.; Beddows, A.; Beevers, S.; Danese, A.; De Oliveira, K.; Kohrt, B.A.; Moffitt, T.E.; et al. Childhood exposure to ambient air pollution and predicting individual risk of depression onset in UK adolescents. J. Psychiatry Res. 2021, 138, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Rowe, B.; Colman, I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. 2009, 22, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Kousha, T.; Kingsbury, M.; Colman, I. Air Pollution and Emergency Department Visits for Depression: A Multicity Case-Crossover Study. Environ. Health Insights 2016, 10, 155–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, J.; Choi, Y.J.; Suh, M.; Sohn, J.; Kim, H.; Cho, S.K.; Ha, K.H.; Kim, C.; Shin, D.C. Air pollution as a risk factor for depressive episode in patients with cardiovascular disease, diabetes mellitus, or asthma. J. Affect. Disord. 2014, 157, 45–51. [Google Scholar] [CrossRef]
- Zhou, Y.M.; An, S.J.; Tang, E.J.; Xu, C.; Cao, Y.; Liu, X.L.; Yao, C.Y.; Xiao, H.; Zhang, Q.; Liu, F.; et al. Association between short-term ambient air pollution exposure and depression outpatient visits in cold seasons: A time-series analysis in northwestern China. J. Toxicol. Environ. Health A 2021, 84, 389–398. [Google Scholar] [CrossRef]
- Gu, X.; Guo, T.; Si, Y.; Wang, J.; Zhang, W.; Deng, F.; Chen, L.; Wei, C.; Lin, S.; Guo, X.; et al. Association between ambient air pollution and daily hospital admissions for depression in 75 Chinese cities. Am. J. Psychiatry 2020, 177, 735–743. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Willey, J.B.; Grafstein, E.; Rowe, B.H.; Colman, I. Air Pollution and Emergency Department Visits for Suicide Attempts in Vancouver, Canada. Environ. Health Insights 2010, 4, 79–86. [Google Scholar] [CrossRef]
- Min, J.; Kim, H.J.; Min, K. Long-term exposure to air pollution and the risk of suicide death: A population-based cohort study. Sci. Total Environ. 2018, 628–629, 573–579. [Google Scholar] [CrossRef]
- Ng, C.F.; Stickley, A.; Konishi, S.; Watanabe, C. Ambient air pollution and suicide in Tokyo, 2001–2011. J. Affect. Disord. 2016, 201, 194–202. [Google Scholar] [CrossRef]
- Kim, Y.; Ng, C.F.; Chung, Y.; Kim, H.; Honda, Y.; Guo, Y.L.; Lim, Y.H.; Chen, B.Y.; Page, L.A.; Hashizume, M. Air pollution and suicide in 10 cities in Northeast Asia: A time-stratified case-crossover analysis. Environ. Health Perspect. 2018, 126, 037002. [Google Scholar] [CrossRef] [Green Version]
- Bakian, A.; Huber, R.S.; Coon, H.; Gray, D.; Wilson, P.; McMahon, W.M.; Renshaw, P.F. Acute air pollution exposure and risk of suicide completion. Am. J. Epidemiol. 2015, 181, 295–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IQAir. 2020 World Air Quality Report: Region & City PM2.5 Ranking. Available online: https://www.iqair.com/ca/world-most-polluted-countries (accessed on 10 December 2021).


| Health Effect Resulting from NOx Exposure | Exposure Duration | Risk Ratios (Per 10 μg·m−3 Increase in NO2 Exposure) | References | |
|---|---|---|---|---|
| General | Diabetes | Chronic | 1.23 | [42] |
| High Blood Pressure | Chronic | 1.01 | [42] | |
| Headache | Chronic | 1.13 | [42] | |
| Stroke | Chronic | 1.01 | [42] | |
| Nose and Throat Irritation | Acute | [4] | ||
| Increased sensitivity and susceptibility to respiratory illness and disease | Chronic | [4,7,17,40,41,43] | ||
| Respiratory Illness | Chronic | [39] | ||
| Chest Colds, Chronic Cough and Wheezing, Chest Cough | Acute and Chronic | [7,11,37,39,44,45] | ||
| Dyspnea | Chronic | [4] | ||
| Reduced Lung Function | Acute and Chronic | [7,37,40,44] | ||
| Bronchitis and Bronchitis Symptoms | Chronic | 1.021 | [4,16,39,40,46,47,48,49] | |
| Allergic Reactions | Chronic | [4,7,41] | ||
| Inflammatory Responses | Chronic | [11,16,35,36,37,38,39,47] | ||
| Potential Reproductive Impacts | Chronic | [4,7,41] | ||
| Cell Damage | Chronic | [11,16,35,36,37,38,39,47] | ||
| Cardiovascular Disease (CVD) | Chronic | 1.04–1.22 | [4,7,17,41,43,50,51,52,53,54] | |
| Respiratory Disease | Chronic | [4,7,16,17,41] | ||
| Asthma | Chronic | 1.05–1.5 | [4,7,11,41,42,45,55,56,57] | |
| Hospital Admissions | General | Acute and Chronic | 1.01 | [46,48,49,58,59] |
| Emergency Room | Chronic | 1.1 | [17,60] | |
| Stroke | Chronic | 1.14 | [61] | |
| Asthma | Acute and Chronic | 1.001–1.27 | [35,59,61] | |
| Respiratory Ailments | Chronic | 1.009–1.05 | [9,59,61,62] | |
| Respiratory Disease | Acute | 1.018 | [46,49] | |
| Chronic Obstructive Pulmonary Disease (COPD) | Acute | [35] | ||
| Blood Poisoning | Acute | [35] | ||
| Cardiovascular-Circulatory System Disease | Chronic | 1.05 | [61] | |
| Cardiovascular-Myocardial Infraction | Chronic | 1.15 | [61] | |
| Cancer-Lung | Chronic | 1.2 | [61] | |
| Cancer-Kidney | Chronic | 1.2 | [61] | |
| Cancer-Other | Chronic | 1.06 | [61] | |
| Cancer | Lung | Chronic | 1.12 | [3,4,7,41,55,63,64,65,66,67] |
| Brain | Chronic | [55,68] | ||
| Cervical | Chronic | [55,68] | ||
| Breast | Chronic | [55,63,68] | ||
| Prostate | Chronic | [63] | ||
| Premature Mortality | All-Cause | Acute | 1.003–1.016 | [41,49,69] |
| All-Cause | Chronic | 1.003–1.06 | [16,17,28,46,48,49,69,70,71,72,73] | |
| Cardiovascular | Chronic | 1.004–1.03 | [28,52,69] | |
| Respiratory | Chronic | 1.004–1.03 | [16,28,69,74,75,76] | |
| Lung Cancer | Chronic | 1.05 | [28,41] | |
| Coronary Heart Disease | Chronic | 1.05 | [28] | |
| COPD | Chronic | 1.03 | [28] | |
| Pneumonia | Chronic | 1.08 | [28] | |
| Diabetes | Chronic | 1.04 | [28] | |
| Category | Symptom | Exposure Duration | Risk Ratio (95% CI) per 10 μg·m−3 Increase in NO2 (Unless Otherwise Specified) *-Calculated from OR | Mean NO2 Exposureug μg·m−3 | Reference |
|---|---|---|---|---|---|
| Common Mental Disorders (CMD) | CMD | Chronic | 1.35 (1.26, 1.35)* for NO2 1.23 (1.19, 1.27)* for NOx | [81] | |
| CMD | Chronic | 1.28 (1.05, 1.46)* for NO2 1.27 (1.04, 1.45)* for NOx | 35.8–39.6 (NO2) 57.0–67.4 (NOx) | [13] | |
| Physical Symptoms | Chronic | 1.23 (1.02, 1.39)* for NO2 1.22 (1.02, 1.38)* for NOx | |||
| Self-Rated Health | Chronic | 1.15 (0.94, 1.32)* for NO2 1.13 (0.93, 1.30)* for NOx | |||
| Chronic | 1.07 (1.05, 1.10)* per IQR | 23.4 | [82] | ||
| Chronic | 0.95 (0.39, 1.31)* highest vs. lowest tertile range | 34.64 | [83] | ||
| Psychological Distress | Chronic | Positive, statistically significant relationship with NOx | [84] | ||
| Mental Health Service Use | Chronic | 1.32 (1.25, 1.38) per IQR for NO2 1.31 (1.24, 1.37) per IQR for NOx | 40.2 (NO2) 71.1 (NOx) | [85] | |
| Hospital Admissions | Acute | 1.17 (1.00, 1.36) | 56.75 | [86] | |
| Hospital Admissions | Acute | 1.0188 (−0.40,4.16) for 1-day lag, moving average concentration | 46 | [87] | |
| Hospital Admissions | Chronic | 1.18 (1.05, 1.34) per IQR for NO2 1.18 (1.05, 1.34) per IQR for NOx | 40.2 (NO2) 71.1 (NOx) | [85] | |
| Emergency Room Visits | Chronic | 1.02 (−0.6, 4.6) | [88] | ||
| Acute | 1.0494 (1.0203, 1.0792) per IQR | 39.8 | [89] | ||
| Acute | 1.0377 (1.0278, 1.0478) | 32.79–53.23 | [90] | ||
| Acute | 0.9966 (0.9873, 1.0061) per IQR | 23.57 | [91] | ||
| Acute | 1.0445 (1.0290, 1.0604) | 24.69 | [92] | ||
| Acute | 1.0794 (1.0628, 1.0962) | 30.13 | [92] | ||
| Acute | 1.0219 (0.0051, 1.0389) | 33.35 | [92] | ||
| Psychosis Mortality | Acute | 1.0010 (0.9999, 1.0021) | 18.7 | [93] | |
| Sleep | Low Sleep Efficiency | Chronic | 1.16 (1.07, 1.25)* | 27.82 | [94] |
| Sleep Apnea | Chronic | 1.28 (1.03, 1.47)* | 27.82 | [94] | |
| Sleep Disorder | Chronic | 1.11 (1.02, 1.19)* per IQR | 36.78 | [95] | |
| Sleep Disorder | Chronic | 1.17 (0.77, 1.44)* highest vs. lowest tertile range | 34.64 | [83] | |
| Anxiety | Anxiety Disorder | Chronic | 1.09 (0.90, 1.25)* | 27.5 | [43] |
| Chronic | 1.34 (0.85, 1.62)* highest vs. lowest tertile range | 34.64 | [83] | ||
| Medication Use | Chronic | 1.21 (0.90, 1.44)* for NO2 1.13 (0.89, 1.32)* for NOx | 57.3 | [96] | |
| Hospital Admissions | Acute | 2.23 (1.02, 4.91) | 56.75 | [86] | |
| Emergency Room Visits | Acute | 1.0342 (1.0210, 1.0475) | 32.79–53.23 | [90] | |
| Acute | 1.0506 (1.0233, 1.0786) | 24.69 | [92] | ||
| Acute | 1.0740 (1.0545, 1.0938) | 30.13 | [92] | ||
| Acute | 1.0429 (1.0217, 1.0645) | 33.35 | [92] | ||
| Depression | Depressive Symptoms | Chronic | 1.50 (1.27, 1.67)* per 10 μg·m−3 increase NO2 1.38 (1.18, 1.53)* per 20 μg·m−3 increase NOx | 57.3 (NO2) 92.8 (NOx) | [96] |
| Chronic | 1.33 (1.27, 1.39)* for highest quartile exposure | [97] | |||
| Acute | 1.25 (1.11, 1.36)* | 36.2 | [98] | ||
| Acute | 1.24 (0.99, 1.43)* per IQR | 31.4 | [99] | ||
| Chronic | 1.24 (1.06, 1.39)* | 11.7–18.8 | [100] | ||
| Chronic | 1.35 (1.07, 1.52)* for NO2 1.27 (0.94, 1.50)* for NOx | 25.9 (NO2) 39.6 (NOx) | [101] | ||
| Chronic | 1.05 (0.98, 1.11)* for NO2 1.05 (0.99, 1.09)* for NOx | [81] | |||
| Medication Use | Chronic | 1.03 (1.00, 1.05)* per IQR | 23.4 | [82] | |
| Depressive Disorder | Chronic | 1.13 (0.95, 1.28)* | 27.5 | [43] | |
| Chronic | 1.05 (0.86, 1.20)* per 188 μg·m−3-30 days before indexing date | 46 | [102] | ||
| Chronic | 1.05 (0.78, 1.21)* per 188 μg·m−3-365 days before indexing date | 46.1 | [102] | ||
| Acute | 1.04 (0.99, 1.08)* per IQR | 34.78 | [103] | ||
| Chronic | 1.37 (0.99, 1.60)* highest vs. lowest tertile range | 34.64 | [83] | ||
| Major Depressive Disorder | Chronic | 1.14 (0.72, 1.41)* highest IQR for NO2 1.30 (0.96, 1.53)* highest IQR for NOx | 26.04 (NO2), 35.19 (NOx)–mean 39.85 (NO2), 59.71 (NOx)–Q4 | [104] | |
| Emergency Room Visits | Acute | 1.039 (1.013, 1.066)-Cold Season 1.066 (1.012, 1.124)-Warm Season | 41.17 | [105] | |
| Acute | 1.10 (1.066, 1.136) per 20.1 ppb NO2-All Season 1.20 (1.133, 1.272) per 20.1 ppb NO2-Warm Season 1.064 (1.021, 1.108) per 20.1 ppb NO2-Cold Season | 37.79 | [105] | ||
| Acute | 1.03 (0.98, 1.04)*-Warm Season, Male 1.03 (1.00, 1.05)*-Warm Season, Female | 22.18 | [106] | ||
| Acute | 1.0369 (1.0224, 1.052) | 32.79–53.23 | [90] | ||
| Acute | 1.08 (1.03, 1.12)* | [107] | |||
| Acute | 0.9875 (0.9704, 1.0049) per IQR | 23.57 | [91] | ||
| Acute | 1.36 (0.44, 2.28) | 48.5 | [108] | ||
| Acute | 1.0494 (1.0270, 1.0723) | 24.69 | [92] | ||
| Acute | 1.0802 (1.0623, 1.0984) | 30.13 | [92] | ||
| Hospital Admissions | Acute | 1.18 (0.55, 2.53) | 56.75 | [86] | |
| Acute | 1.0178 (1.0073, 1.0283)-1-day Lag | 34.6 | [109] | ||
| Suicide | Emergency Room Visits | Acute | 1.112 (1.006, 1.228) All Seasons, Male, 1-day Lag 1.239 (1.078, 1.424)-Cold Season, Male, 1-day Lag | 36.47 | [110] |
| Acute | 0.9990 (0.9730, 1.0258) per IQR | 23.57 | [91] | ||
| Risk of Death by Suicide | Chronic | 1.33 (1.09, 1.64) | 48.20 | [111] | |
| 1.39 (1.03, 1.87)-for individuals with pre-existing physical or mental disease | 48.20 | [111] | |||
| Acute | 1.06 (1.01, 1.12)*-All Gender, Under 30 years old, 0-day Lag 1.04 (1.00, 1.08)*-All Age, Warm Season, 0-day Lag | 68.94 | [112] | ||
| Acute | 1.019 (0.999, 1.039)-0–1 day Lag | [113] | |||
| Acute | 1.0057 (1.0023, 1.0081) | 18.7 | [93] | ||
| Completed Suicide | Acute | 1.17 (1.04, 1.29)*-all 1.26 (1.09, 1.40)*-Spring and Fall Transitions | [114] | ||
| Alzheimer’s Disease | Hospital Admissions | Chronic | 1.06 (0.96, 1.17) | 26.2 | [61] |
| Parkinson’s Disease | Parkinson’s Disease | Chronic | 1.08 (0.94, 1.24) | 26.2 | [61] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shaw, S.; Van Heyst, B. An Evaluation of Risk Ratios on Physical and Mental Health Correlations due to Increases in Ambient Nitrogen Oxide (NOx) Concentrations. Atmosphere 2022, 13, 967. https://doi.org/10.3390/atmos13060967
Shaw S, Van Heyst B. An Evaluation of Risk Ratios on Physical and Mental Health Correlations due to Increases in Ambient Nitrogen Oxide (NOx) Concentrations. Atmosphere. 2022; 13(6):967. https://doi.org/10.3390/atmos13060967
Chicago/Turabian StyleShaw, Stephanie, and Bill Van Heyst. 2022. "An Evaluation of Risk Ratios on Physical and Mental Health Correlations due to Increases in Ambient Nitrogen Oxide (NOx) Concentrations" Atmosphere 13, no. 6: 967. https://doi.org/10.3390/atmos13060967
APA StyleShaw, S., & Van Heyst, B. (2022). An Evaluation of Risk Ratios on Physical and Mental Health Correlations due to Increases in Ambient Nitrogen Oxide (NOx) Concentrations. Atmosphere, 13(6), 967. https://doi.org/10.3390/atmos13060967







