The Role of Mitogen-Activated Protein Kinase-Activated Protein Kinases (MAPKAPKs) in Inflammation
Abstract
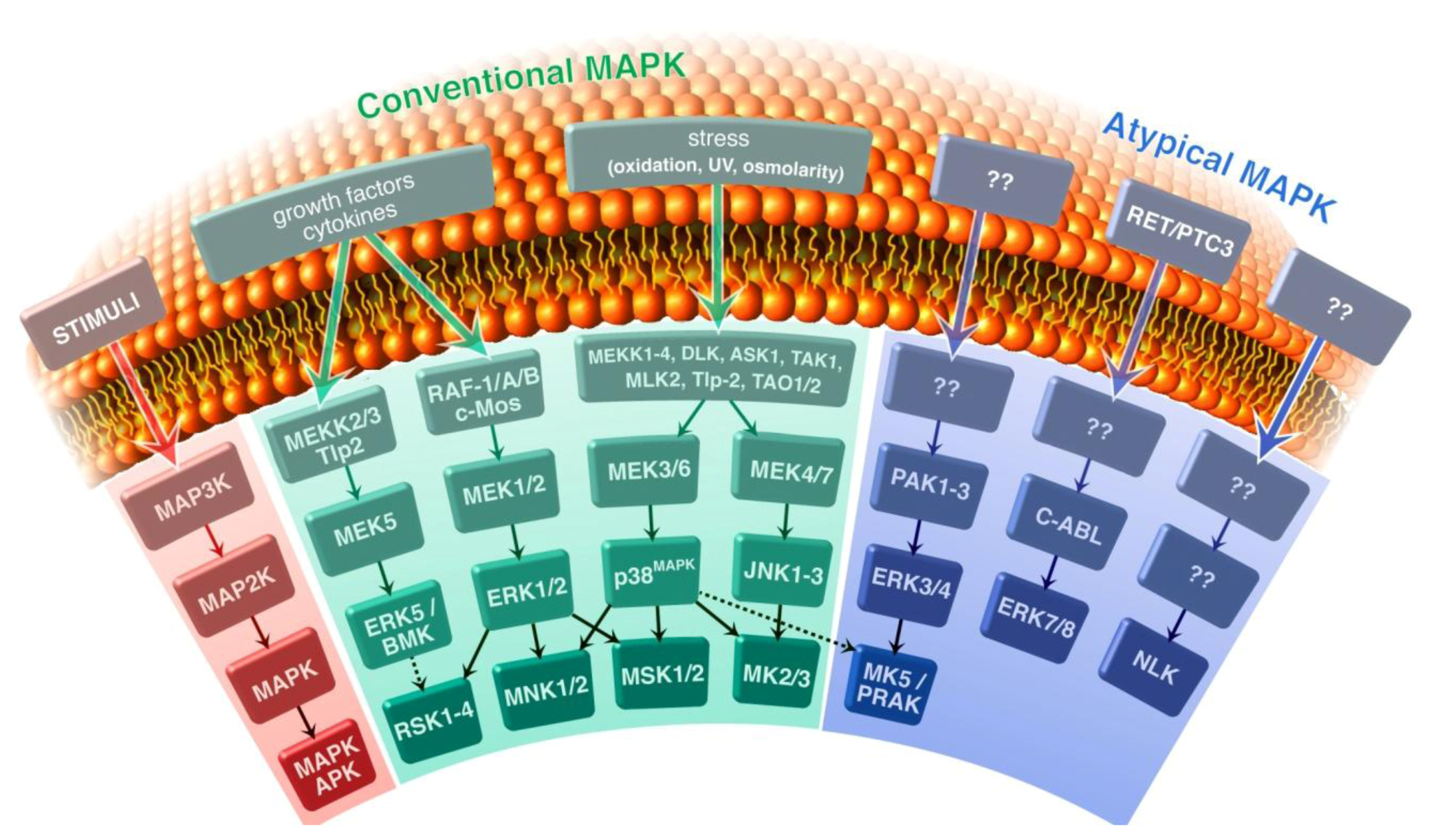
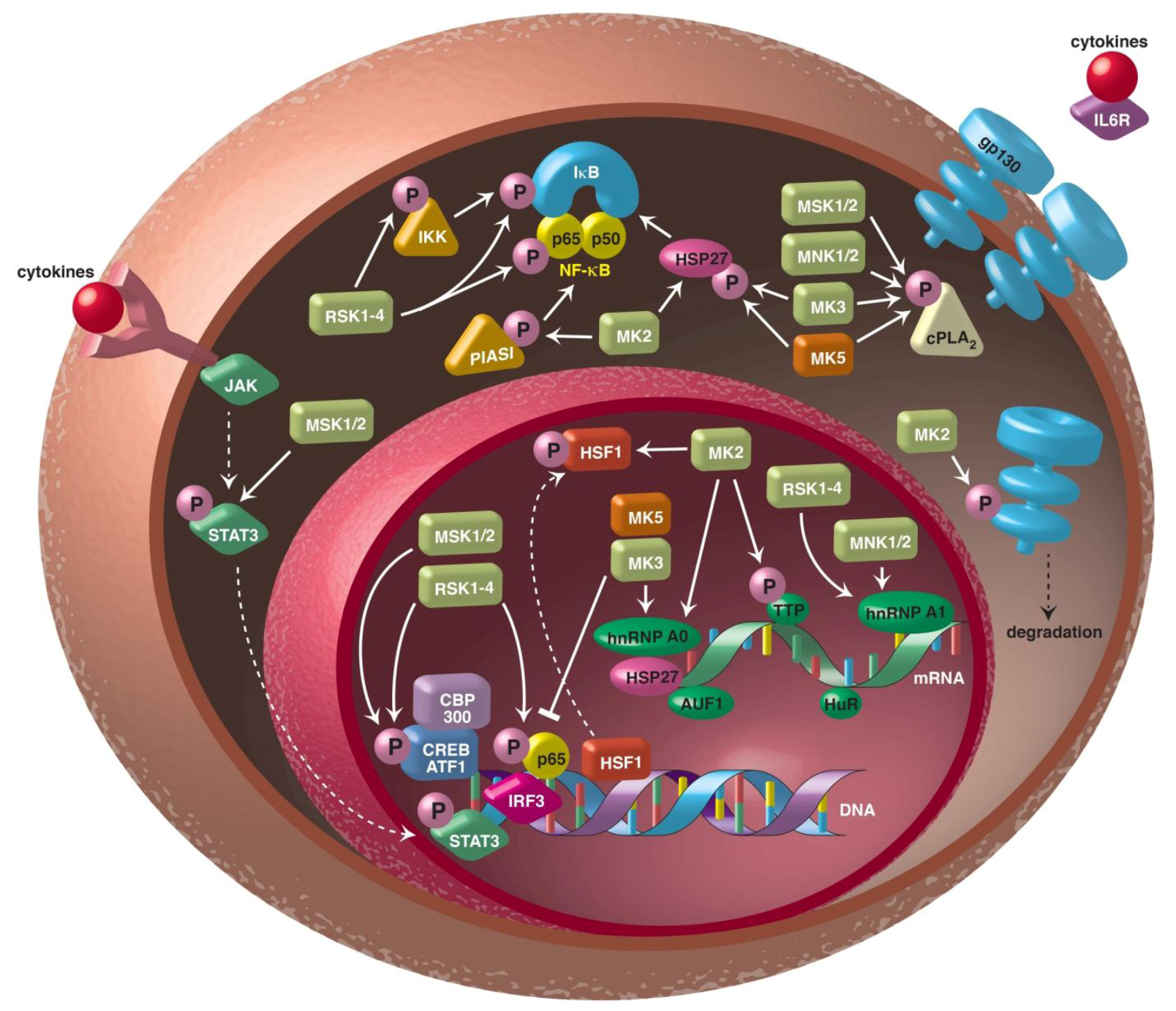
:1. Introduction
2. RSK and Inflammation
3. MSK and Inflammation
3.1. MSK and Expression of Inflammatory Regulators
3.2. MSK and In Vivo Models of Inflammation
4. MNK and Inflammation
5. MK2 and Inflammation
5.1. MK2 and Regulation of Inflammatory Mediators
5.2. Phosphorylated HSP27 and Inflammation
5.3. In Vivo Role of MK2 in Inflammation and Inflammatory Diseases
6. MK3 and Inflammation
7. MK5 and Inflammation
8. MAPKAPK Inhibitors in the Treatment of Inflammatory Diseases
8.1. RSK Inhibitors
8.2. MSK1/2 Inhibitors
8.3. MNK Inhibitors
8.4. MK2/3 Inhibitors
8.5. MK5 Inhibitors
9. Conclusions
References
- Ward, P.A. Acute and chronic inflammation. In Fundamentals of Inflammation, 1st; Serhan, C.N., Ward, P.A., Eds.; Cambridge University Press: New York, NY, USA, 2010; pp. 1–16. [Google Scholar]
- DiDonato, J.A.; Mercurio, F.; Karin, M. NF-kB and the link between inflammation and cancer. Immunol. Rev. 2012, 246, 379–400. [Google Scholar] [CrossRef]
- Kyriakis, J.M.; Avruch, J. Mammalian MAPK signal transduction pathways activated by stress and inflammation: A 10-year update. Physiol. Rev. 2012, 92, 689–737. [Google Scholar] [CrossRef]
- Newton, K.; Dixit, V.M. Signaling in innate immunity and inflammation. Cold Spring Harb. Perspect. Biol. 2012, 4, a006049. [Google Scholar] [CrossRef]
- O’Shea, J.J.; Plenge, R. JAK and STAT signaling molecules in immunoregulation and immune-mediated disease. Immunity 2012, 36, 542–550. [Google Scholar]
- Cargnello, M.; Roux, P.P. Activation and function of the MAPKs and their substrates, the MAPK-activated protein kinases. Microbiol. Mol. Biol. Rev. 2011, 75, 50–83. [Google Scholar] [CrossRef]
- Anjum, R.; Blenis, J. The RSK family of kinases: Emerging roles in cellular signaling. Nat. Rev. Mol. Cell. Biol. 2008, 9, 747–758. [Google Scholar] [CrossRef]
- Arthur, J.S. MSK activation and physiological roles. Front. Biosci. 2008, 13, 5866–5879. [Google Scholar] [CrossRef]
- Buxade, M.; Parra-Palau, J.L.; Proud, C.G. The Mnks: MAP kinase-interacting kinases (MAP kinase signal-integrating kinases). Front. Biosci. 2008, 13, 5359–5374. [Google Scholar]
- Carriere, A.; Ray, H.; Blenis, J.; Roux, P.P. The RSK factors of activating the Ras/MAPK signaling cascade. Front. Biosci. 2008, 13, 4258–4275. [Google Scholar] [CrossRef]
- Ronkina, N.; Kotlyarov, A.; Gaestel, M. MK2 and MK3—A pair of isoenzymes. Front Biosci. 2008, 13, 5511–5521. [Google Scholar] [CrossRef]
- Kostenko, S.; Dumitriu, G.; Lægreid, K.J.; Moens, U. Physiological roles of mitogen-activated-protein-kinase-activated p38-regulated/activated protein kinase. World J. Biol. Chem. 2011, 2, 73–89. [Google Scholar] [CrossRef]
- Gaestel, M. MAPKAP kinases- MKs- two’s company, three’s a crowd. Nat. Rev. Mol. Cell. Biol. 2006, 7, 120–130. [Google Scholar] [CrossRef]
- Kotlyarov, A.; Neininger, A.; Schubert, C.; Eckert, R.; Birchmeier, C.; Volk, H.D.; Gaestel, M. MAPKAP kinase 2 is essential for LPS-induced TNF-alpha biosynthesis. Nat. Cell. Biol. 1999, 1, 94–97. [Google Scholar] [CrossRef]
- Ronkina, N.; Kotlyarov, A.; Dittrich-Breiholz, O.; Kracht, M.; Hitti, E.; Milarski, K.; Askew, R.; Marusic, S.; Lin, L.L.; Gaestel, M.; Telliez, J.B. The mitogen-activated protein kinase (MAPK)-activated protein kinases MK2 and MK3 cooperate in stimulation of tumor necrosis factor biosynthesis and stabilization of p38 MAPK. Mol. Cell. Biol. 2007, 27, 170–181. [Google Scholar] [CrossRef]
- Shiryaev, A.; Moens, U. Mitogen-activated protein kinase p38 and MK2, MK3 and MK5: ménage à trois or ménage à quatre? Cell. Signal. 2010, 22, 1185–1192. [Google Scholar] [CrossRef]
- Kostenko, S.; Dumitriu, G.; Moens, U. Tumor promoting and suppressing roles of the atypical signalling pathway ERK3/4-MK5. J. Mol. Signal. 2012, 7, 9. [Google Scholar] [CrossRef]
- Shiryaev, A.; Kostenko, S.; Dumitriu, G.; Moens, U. Septin 8 is an interaction partner and in vitro substrate of MK5. World J. Biol. Chem. 2012, 3, 98–109. [Google Scholar] [CrossRef]
- Baeuerle, P.A.; Baichwal, V.R. NF-kB as a frequent target for immunosuppressive and anti-inflammatory molecules. Adv. Immunol. 1997, 65, 111–137. [Google Scholar] [CrossRef]
- Barnes, P.J.; Karin, M. Nuclear factor-kappab: A pivotal transcription factor in chronic inflammatory diseases. N. Engl. J. Med. 1997, 336, 1066–1071. [Google Scholar] [CrossRef]
- Baeuerle, P.A.; Baltimore, D. NF-kB: Ten years after. Cell 1996, 87, 13–20. [Google Scholar] [CrossRef]
- Ghoda, L.; Lin, X.; Greene, W.C. The 90-kDa ribosomal S6 kinase (pp90rsk) phosphorylates the N-terminal regulatory domain of the IkappaBalpha and stimulates its degradation in vitro. J. Biol. Chem. 1997, 272, 21281–21288. [Google Scholar] [CrossRef]
- Schouten, G.J.; Vertegaal, A.C.; Whiteside, S.T.; Israël, A.; Toebes, M.; Dorsman, J.C.; van der Eb, A.J.; Zantema, A. IkappaB alpha is a target for the mitogen-activated 90 kDa ribosomal S6 kinase. EMBO J. 1997, 16, 3133–3144. [Google Scholar] [CrossRef]
- Han, Y.; Runge, M.S.; Brasier, A.R. Angiotensin II induces interleukin-6 transcription in vascular smooth muscle cells through pleiotropic activation of nuclear factor-kappa B transcription factor. Circ. Res. 1999, 84, 695–703. [Google Scholar] [CrossRef]
- Suzuki, Y.; Ruiz-Ortega, M.; Lorenzo, O.; Ruperez, M.; Esteban, V.; Egido, J. Inflammation and angiotensin II. Int. J. Biochem. Cell Biol. 2003, 35, 881–900. [Google Scholar] [CrossRef]
- Xu, S.; Zhi, H.; Hou, X.; Jiang, B. Angiotensin II modulates interleukin-1b-induced inflammatory gene expression in vascular smooth muscle cells via interfering with ERK-NF-kB crosstalk. Biochem. Biophys. Res. Commun. 2011, 410, 543–548. [Google Scholar] [CrossRef]
- Doyen, P.; Servant, M.J. Tumor necrosis factor receptor-associated factor-6 and ribosomal S6 kinase intracellular pathways link the angiotensin II AT1 receptor to the phosphorylation and activation of the IkB kinase complex in vascular smooth muscle cells. J. Biol. Chem. 2010, 285, 30708–30718. [Google Scholar] [CrossRef]
- Panta, G.R.; Kaur, S.; Cavin, L.G.; Cortés, M.L.; Mercurio, F.; Lothstein, L.; Sweatman, T.W.; Israel, M.; Arsura, M. ATM and the catalytic subunit of DNA-dependent protein kinase activate NF-kappaB through a common MEK/extracellular signal-regulated kinase/pp90(rsk) signaling pathway in response to distinct forms of DNA damage. Mol. Cell. Biol. 2004, 24, 1823–1835. [Google Scholar] [CrossRef]
- Zhang, L.; Ma, Y.; Zhang, J.; Cheng, J.; Du, J. A new cellular signaling mechanism for angiotensin II activation of NF-kB: An IkB-independent, RSK-mediated phosphorylation of p65. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1148–1153. [Google Scholar] [CrossRef]
- Zhang, L.; Cheng, J.; Ma, Y.; Thomas, W.; Zhang, J.; Du, J. Dual pathways for nuclear factor kappaB activation by angiotensin II in vascular smooth muscle: Phosphorylation of p65 by IkappaB kinase and ribosomal kinase. Circ. Res. 2005, 97, 975–982. [Google Scholar] [CrossRef]
- Bohuslav, J.; Chen, L.F.; Kwon, H.; Mu, Y.; Greene, W.C. p53 induces NF-kappaB activation by an IkappaB kinase-independent mechanism involving phosphorylation of p65 by ribosomal S6 kinase 1. J. Biol. Chem. 2004, 279, 26115–26125. [Google Scholar]
- Vergnolle, N.; Cellars, L.; Mencarelli, A.; Rizzo, G.; Swaminathan, S.; Beck, P.; Steinhoff, M.; Andrade-Gordon, P.; Bunnett, N.W.; Hollenberg, M.D.; et al. A role for proteinase-activated receptor-1 in inflammatory bowel disease. J. Clin. Invest. 2004, 114, 1444–1456. [Google Scholar]
- Hou, L.; Kapas, S.; Cruchley, A.T.; Macey, M.G.; Harriot, P.; Chinni, C.; Stone, S.R.; Howells, G.L. Immunolocalization of protease-activated receptor-2 in skin: Receptor activation stimulates interleukin-8 secretion by keratinocytes in vitro. Immunology 1998, 94, 356–362. [Google Scholar] [CrossRef]
- Asokananthan, N.; Graham, P.T.; Fink, J.; Knight, D.A.; Bakker, A.J.; McWilliam, A.S.; Thompson, P.J.; Stewart, G.A. Activation of protease-activated receptor (PAR)-1, PAR-2, and PAR-4 stimulates IL-6, IL-8, and prostaglandin E2 release from human respiratory epithelial cells. J. Immunol. 2002, 168, 3577–3585. [Google Scholar]
- Wang, H.; Moreau, F.; Hirota, C.L.; MacNaughton, W.K. Proteinase-activated receptors induce interleukin-8 expression by intestinal epithelial cells through ERK/RSK90 activation and histone acetylation. FASEB J. 2010, 24, 1971–1980. [Google Scholar] [CrossRef]
- Eliopoulos, A.G.; Dumitru, C.D.; Wang, C.C.; Cho, J.; Tsichlis, P.N. Induction of COX-2 by LPS in macrophages is regulated by Tpl2-dependent CREB activation signals. EMBO J. 2002, 21, 4831–4840. [Google Scholar] [CrossRef]
- Barrios-Rodiles, M.; Tiraloche, G.; Chadee, K. Lipopolysaccharide modulates cyclooxygenase-2 transcriptionally and posttranscriptionally in human macrophages independently from endogenous IL-1b and TNF-a. J. Immunol. 1999, 163, 963–969. [Google Scholar]
- Gilroy, D.W.; Colville-Nash, P.R. New insights into the role of COX2 in inflammation. J. Mol. Med. 2000, 78, 121–129. [Google Scholar] [CrossRef]
- Agarwal, S.; Reddy, G.V.; Reddanna, P. Eicosanoids in inflammation and cancer: the role of COX-2. Expert Rev. Clin. Immunol. 2009, 5, 145–165. [Google Scholar] [CrossRef]
- Zaru, R.; Ronkina, N.; Gaestel, M.; Arthur, J.S.; Watts, C. The MAPK-activated kinase Rsk controls an acute Toll-like receptor signaling response in dendritic cells and is activated through two distinct pathways. Nat. Immunol. 2007, 8, 1227–1235. [Google Scholar] [CrossRef]
- Wang, W.; Han, G.; Ye, M.; Shi, H.; Zou, H.; Huo, K. Mapping of phosphorylation sites in human MSK1 activated by a novel interaction with MRK-beta. Electrophoresis 2010, 31, 1283–1293. [Google Scholar] [CrossRef]
- Vermeulen, L.; De Wilde, G.; Van Damme, P.; Vanden Berghe, W.; Haegeman, G. Transcriptional activation of NF-kappaB p65 subunit by mitogen- and stress-activated protein kinase-1 (MSK1). EMBO J. 2003, 22, 1313–1324. [Google Scholar] [CrossRef]
- Chen, L.F.; Williams, S.A.; Mu, Y.; Nakano, H.; Duerr, J.M.; Buckbinder, L.; Greene, W.C. NF-kappaB RelA phosphorylation regulates RelA acetylation. Mol. Cell. Biol. 2005, 25, 7966–7975. [Google Scholar] [CrossRef]
- Gorska, M.M.; Liang, Q.; Stafford, S.J.; Goplen, N.; Dharajiya, N.; Guo, L.; Sur, S.; Gaestel, M.; Alam, R. MK2 controls the level of negative feedback in the NF-kB pathway and is essential for vascular permeability and airway inflammation. J. Exp. Med. 2007, 204, 1637–1652. [Google Scholar]
- Reber, L.; Vermeulen, L.; Haegeman, G.; Frossard, N. Ser276 phosphorylation of NF-kB p65 by MSK1 controls SCF expression in inflammation. PLoS One 2009, 4, e4393. [Google Scholar]
- Quivy, V.; Van Lint, C. Regulation at multiple levels of NF-kB-mediated transactivation by protein acetylation. Biochem. Pharmacol. 2004, 68, 1221–1229. [Google Scholar] [CrossRef]
- Spooren, A.; Kolmus, K.; Vermeulen, L.; Van Wesemael, K.; Haegeman, G.; Gerlo, S. Hunting for serine 276-phosphorylated p65. J. Biomed. Biotechnol. 2010, 2010, 275892. [Google Scholar]
- Gesser, B.; Johansen, C.; Rasmussen, M.K.; Funding, A.T.; Otkjaer, K.; Kjellerup, R.B.; Kragballe, K.; Iversen, L. Dimethylfumarate specifically inhibits the mitogen and stress activated kinases 1 and 2 (MSK1/2). Possible role for its anti-psoriatic effect. J. Invest. Dermatol. 2007, 127, 2129–2137. [Google Scholar]
- Seidel, P.; Roth, M.; Ge, O.; Merfort, I.; S’ng, C.T.; Ammit, A.J. IkBa glutathionylation and reduced histone H3 phosphorylation inhibit eotaxin and RANTES. Eur. Respir. J. 2011, 38, 1444–1452. [Google Scholar] [CrossRef]
- Terazawa, S.; Nakajima, H.; Shingo, M.; Niwano, T.; Imokawa, G. Astaxanthin attenuates the UVB-induced secretion of prostaglandin E2 and interleukin-8 in human keratinocytes by interrupting MSK1 phosphorylation in a ROS depletion-independent manner. Exp. Dermatol. 2012, 21, 11–17. [Google Scholar] [CrossRef]
- Ospelt, C.; Gay, S. TLRs and chronic inflammation. Int. J. Biochem. Cell. Biol. 2010, 42, 495–505. [Google Scholar] [CrossRef]
- Drexler, S.K.; Foxwell, B.M. The role of Toll-like receptors in chronic inflammation. Int. J. Biochem. Cell. Biol. 2010, 42, 506–518. [Google Scholar] [CrossRef]
- Ananieva, O.; Darragh, J.; Johansen, C.; Carr, J.M.; McIlrath, J.; Park, J.M.; Wingate, A.; Monk, C.E.; Toth, R.; Santos, S.G.; et al. The kinases MSK1 and MSK2 act as negative regulators of Toll-like receptor signalling. Nat. Immunol. 2008, 9, 1028–1036. [Google Scholar] [CrossRef]
- Edwards, J.P.; Emens, L.A. The multikinase inhibitor Sorafenib reverses the suppression of IL-12 and enhancement of IL-10 by PGE2 in murine macrophages. Int. Immunopharmacol. 2010, 10, 1220–1228. [Google Scholar] [CrossRef]
- Kim, C.; Sano, Y.; Todorova, K.; Carlson, B.A.; Arpa, L.; Celada, A.; Lawrence, T.; Otsu, K.; Brissette, J.L.; Arthur, J.S.; Park, J.M. The kinase p38alpha serves cell type-specific inflammatory functions in skin injury and coordinates pro- and anti-inflammatory gene expression. Nat. Immunol. 2008, 9, 1019–1027. [Google Scholar] [CrossRef]
- Darragh, J.; Ananieva, O.; Courtney, A.; Elcombe, S.; Arthur, J.S. MSK1 regulates the transcription of IL-1ra in response to TLR activation in macrophages. Biochem. J. 2010, 425, 595–602. [Google Scholar] [CrossRef]
- Carl, V.S.; Gautam, J.K.; Comeau, L.D.; Smith, M.F., Jr. Role of endogenous IL-10 in LPS-induced STAT3 activation and IL-1 receptor antagonist gene expression. J. Leukoc. Biol. 2004, 76, 735–742. [Google Scholar] [CrossRef]
- Zheng, T.; Zhu, Z.; Wang, J.; Homer, R.J.; Elias, J.A. IL-11: Insights in asthma from overexpression transgenic modelling. J. Allergy Clin. Immunol. 2001, 108, 489–496. [Google Scholar] [CrossRef]
- Suzuki, S.; Kokubu, F.; Kawaguchi, M.; Homma, T.; Odaka, M.; Watanabe, S.; Ieki, K.; Matsukura, S.; Kurokawa, M.; Takeuchi, H.; et al. Expression of interleukin-17F in a mouse model of allergic asthma. Int. Arch. Allergy Immunol. 2007, 143, 89–94. [Google Scholar] [CrossRef]
- Barnes, P.J. Immunology of asthma and chronic obstructive pulmonary disease. Nat. Rev. Immunol. 2008, 8, 183–192. [Google Scholar] [CrossRef]
- Kawaguchi, M.; Kokubu, F.; Fujita, J.; Huang, S.K.; Hizawa, N. Role of interleukin-17F in asthma. Inflamm. Allergy Drug Targets 2009, 8, 383–389. [Google Scholar] [CrossRef]
- Kawaguchi, M.; Fujita, J.; Kokubu, F.; Hunag, S.K.; Homma, T.; Matsukura, S.; Adachi, M.; Hizawa, N. IL-17F-induced IL-11 release in bronchial epithelial cells via MSK1-CREB pathway. Am. J. Physiol. Lung Cell. Mol. Physiol. 2009, 296, L804–L810. [Google Scholar] [CrossRef]
- Hoshino, M.; Nakamura, Y.; Sim, J.J.; Yamashiro, Y.; Uchida, K.; Hosaka, K.; Isogai, S. Inhaled corticosteroid reduced lamina reticularis of the basement membrane by modulation of insulin-like growth factor (IGF)-I expression in bronchial asthma. Clin. Exp. Allergy 1998, 28, 568–577. [Google Scholar] [CrossRef]
- Kawaguchi, M.; Fujita, J.; Kokubu, F.; Ohara, G.; Huang, S.K.; Matsukura, S.; Ishii, Y.; Adachi, M.; Satoh, H.; Hizawa, N. Induction of insulin-like growth factor-I by interleukin-17F in bronchial epithelial cells. Clin. Exp. Allergy 2010, 40, 1036–1043. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, G.; Dong, Z. MSK1 and JNKs mediate phosphorylation of STAT3 in UVA-irradiated mouse epidermal JB6 cells. J. Biol. Chem. 2001, 276, 42534–42542. [Google Scholar] [CrossRef]
- Wierenga, A.T.; Vogelzang, I.; Eggen, B.J.; Vellenga, E. Erythropoietin-induced serine 727 phosphorylation of STAT3 in erythroid cells is mediated by a MEK-, ERK-, and MSK1-dependent pathway. Exp. Hematol. 2003, 31, 398–405. [Google Scholar] [CrossRef]
- Hefner, Y.; Borsch-Haubold, A.G.; Murakami, M.; Wilde, J.I.; Pasquet, S.; Schieltz, D.; Ghomashchi, F.; Yates, J.R.; Armstrong, C.G.; Paterson, A.; et al. Serine 727 phosphorylation and activation of cytosolic phospholipase A2 by MNK1-related protein kinase. J. Biol. Chem. 2000, 275, 37542–37551. [Google Scholar] [CrossRef]
- Bertelsen, T.; Iversen, L.; Riis, J.L.; Arthur, J.S.; Bibby, B.M.; Kragballe, K.; Johansen, C. The role of mitogen- and stress-activated protein kinase 1 and 2 in chronic skin inflammation in mice. Exp. Dermatol. 2011, 20, 140–145. [Google Scholar] [CrossRef]
- Chang, S.; Iversen, L.; Kragballe, K.; Arthur, J.S.; Johansen, C. Mice lacking MSK1 and MSK2 show reduced skin tumor development in a two-stage chemical carcinogenesis model. Cancer Invest. 2011, 29, 240–245. [Google Scholar] [CrossRef]
- Vermeulen, L.; Vanden Berghe, W.; Beck, I.M.; De Bosscher, K.; Haegeman, G. The versatile role of MSKs in transcriptional regulation. Trends Biochem. Sci. 2009, 34, 311–318. [Google Scholar] [CrossRef]
- Syrbu, S.I.; Waterman, W.H.; Molski, T.F.; Nagarkatti, D.; Hajjar, J.J.; Sha’afi, R.I. Phosphorylation of cytosolic phospholipase A2 and the release of arachidonic acid in human neutrophils. J. Immunol. 1999, 162, 2334–2340. [Google Scholar]
- Niknami, M.; Patel, M.; Witting, P.K.; Dong, Q. Molecules in focus: Cytosolic phospholipase A2-alpha. Int. J. Biochem. Cell Biol. 2009, 41, 994–997. [Google Scholar] [CrossRef]
- Buxadé, M.; Parra, J.L.; Rousseau, S.; Shpiro, N.; Marquez, R.; Morrice, N.; Bain, J.; Espel, E.; Proud, C.G. The Mnks are novel components in the control of TNF alpha biosynthesis and phosphorylate and regulate hnRNP A1. Immunity 2005, 23, 177–189. [Google Scholar] [CrossRef]
- Andersson, K.; Sundler, R. Posttranscriptional regulation of TNFalpha expression via eukaryotic initiation factor 4E (eIF4E) phosphorylation in mouse macrophages. Cytokine 2006, 33, 52–57. [Google Scholar] [CrossRef]
- Rowlett, R.M.; Chrestensen, C.A.; Nyce, M.; Harp, M.G.; Pelo, J.W.; Cominelli, F.; Ernst, P.B.; Pizarro, T.T.; Sturgill, T.W.; Worthington, M.T. MNK kinases regulate multiple TLR pathways and innate proinflammatory cytokines in macrophages. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 294, G452–G459. [Google Scholar]
- Ziaei, S.; Shimada, N.; Kucharavy, H.; Hubbard, K. MNK1 expression increases during cellular senescence and modulates the subcellular localization of hnRNP A1. Exp. Cell Res. 2012, 318, 500–508. [Google Scholar] [CrossRef]
- Lee, J.C.; Laydon, J.T.; McDonnell, P.C.; Gallagher, T.F.; Kumar, S.; Green, D.; McNulty, D.; Blumenthal, M.J.; Heys, J.R.; Landvatter, S.W.; et al. A protein kinase involved in the regulation of inflammatory cytokine biosynthesis. Nature 1994, 372, 739–746. [Google Scholar] [CrossRef]
- Neininger, A.; Kontoyiannis, D.; Kotlyarov, A.; Winzen, R.; Eckert, R.; Volk, H.D.; Holtmann, H.; Kollias, G.; Gaestel, M. MK2 targets AU-rich elements and regulates biosynthesis of tumor necrosis factor and interleukin-6 independently at different post-transcriptional levels. J. Biol. Chem. 2002, 277, 3065–3068. [Google Scholar] [CrossRef]
- Culbert, A.A.; Skaper, S.D.; Howlett, D.R.; Evans, N.A.; Facci, L.; Soden, P.E.; Seymour, Z.M.; Guillot, F.; Gaestel, M.; Richardson, J.C. MAPK-activated protein kinase 2 deficiency in microglia inhibits pro-inflammatory mediator release and resultant neurotoxicity. J. Biol. Chem. 2006, 281, 23658–23667. [Google Scholar] [CrossRef]
- Thomas, T.; Timmer, M.; Cesnulevicius, K.; Hitti, E.; Kotlyarov, A.; Gaestel, M. MAPKAP kinase 2-deficiency prevents neurons from cell death by reducing neuroinflammation—relevance in a mouse model of Parkinson’s disease. J. Neurochem. 2008, 105, 2039–2052. [Google Scholar] [CrossRef]
- Tudor, C.; Marchese, F.P.; Hitti, E.; Aubareda, A.; Rawlinson, L.; Gaestel, M.; Blackshear, P.J.; Clark, A.R.; Saklatvala, J.; Dean, J.L. The p38 MAPK pathway inhibits tristetraprolin-directed decay of interleukin-10 and pro-inflammatory mediator mRNAs in murine macrophages. FEBS Lett. 2009, 583, 1933–1938. [Google Scholar] [CrossRef]
- Schottelius, A.J.; Zügel, U.; Döcke, W.D.; Zollner, T.M.; Röse, L.; Mengel, A.; Buchmann, B.; Becker, A.; Grütz, G.; Naundorf, S.; et al. The role of mitogen-activated protein kinase-activated protein kinase 2 in the p38/TNF-a pathway of systemic and cutaneous inflammation. J. Invest. Dermatol. 2010, 130, 481–491. [Google Scholar] [CrossRef]
- Bode, J.G.; Ehlting, C.; Häussinger, D. The macrophage response towards LPS and its control through the p38MAPK-STAT3 axis. Cell. Signal. 2012, 24, 1185–1194. [Google Scholar] [CrossRef]
- Johansen, C.; Funding, A.T.; Otkjaer, K.; Kragballe, K.; Jensen, U.B.; Madsen, M.; Binderup, L.; Skak-Nielsen, T.; Fjording, M.S.; Iversen, L. Protein expression of TNF-alpha in psoriatic skin is regulated at a posttranscriptional level by MAPK-activated protein kinase 2. J. Immunol. 2006, 176, 1431–1438. [Google Scholar]
- Jagielska, J.; Kapopara, P.R.; Salguero, G.; Scherr, M.; Schütt, H.; Grote, K.; Schieffer, B.; Bavendiek, U. Interleukin-1b assembles a proangiogenic signal module consisting of caveolin-1, tumor necrosis factor receptor-associated factor 6, p38-mitogen-activated protein kinase (MAPK), and MAPK-activated protein kinase 2 in endothelial cells. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 1280–1288. [Google Scholar] [CrossRef]
- Rousseau, S.; Morrice, N.; Peggie, M.; Campbell, D.G.; Gaestel, M.; Cohen, P. Inhibition of SAPK2a/p38 prevents hnRNP A0 phosphorylation by MAPKAP-K2 and its interaction with cytokine mRNAs. EMBO J. 2002, 21, 6505–6514. [Google Scholar] [CrossRef]
- Chrestensen, C.A.; Schroeder, M.J.; Shabanowitz, J.; Hunt, D.F.; Pelo, J.W.; Worthington, M.T.; Sturgill, T.W. MAPKAP kinase 2 phosphorylates tristetraprolin on in vivo sites including Ser178, a site required for 14-3-3 binding. J. Biol. Chem. 2004, 279, 10176–10184. [Google Scholar]
- Clement, S.L.; Scheckel, C.; Stoecklin, G.; Lykke-Andersen, J. Phosphorylation of tristetraprolin by MK2 impairs AU-rich element mRNA decay by preventing deadenylase recruitment. Mol. Cell. Biol. 2011, 31, 256–266. [Google Scholar] [CrossRef]
- Tran, H.; Maurer, F.; Nagamine, Y. Stabilization of urokinase and urokinase receptor mRNAs by HuR is linked to its cytoplasmic accumulation induced by mitogen-activated protein kinase-activated protein kinase 2. Mol. Cell. Biol. 2003, 23, 7177–7188. [Google Scholar] [CrossRef]
- Stoecklin, G.; Stubbs, T.; Kedersha, N.; Wax, S.; Rigby, W.F.; Blackwell, T.K.; Anderson, P. MK2-induced tristetraprolin: 14–3-3 complexes prevent stress granule association and ARE-mRNA decay. EMBO J. 2004, 23, 1313–1324. [Google Scholar] [CrossRef]
- Ronkina, N.; Menon, M.B.; Schwermann, J.; Tiedje, C.; Hitti, E.; Kotlyarov, A.; Gaestel, M. MAPKAP kinases MK2 and MK3 in inflammation: Complex regulation of TNF biosynthesis via expression and phosphorylation of tristetraprolin. Biochem. Pharmacol. 2010, 80, 1915–1920. [Google Scholar] [CrossRef]
- Tiedje, C.; Ronkina, N.; Tehrani, M.; Dhamija, S.; Laass, K.; Holtmann, H.; Kotlyarov, A.; Gaestel, M. The p38/MK2-driven exchange between tristetraprolin and HuR regulates AU-rich element-dependent translation. PLoS Genet. 2012, 8, e1002977. [Google Scholar] [CrossRef]
- Marchese, F.P.; Aubareda, A.; Tudor, C.; Clark, A.R.; Dean, J.L. MAPKAP kinase 2 blocks tristetraprolin-directed mRNA decay by inhibitingCAF1 deadenylase recruitment. J. Biol. Chem. 2010, 285, 27590–27600. [Google Scholar]
- Hitti, E.; Iakovleva, T.; Brook, M.; Deppenmeier, S.; Gruber, A.D.; Radzioch, D.; Clark, A.R.; Blackshear, P.J.; Kotlyarov, A.; Gaestel, M. Mitogen-activated protein kinase-activated protein kinase 2 regulates tumor necrosis factor mRNA stability and translation mainly by altering tristetraprolin expression, stability, and binding to adenine/uridine-rich element. Mol. Cell. Biol. 2006, 26, 2399–2407. [Google Scholar] [CrossRef]
- Ronkina, N.; Menon, M.B.; Schermann, J.; Arthur, J.S.; Legault, H.; Telliez, J.B.; Kayyali, U.S.; Nebreda, A.R.; Kotlyarov, A.; Gaestel, M. Stress induced gene expression: A direct role for MAKAPK kinases in transcriptional activation of immediate early genes. Nucleic Acids Res. 2011, 39, 2503–2518. [Google Scholar] [CrossRef]
- Winzen, R.; Kracht, M.; Ritter, B.; Wilhelm, A.; Chen, C.Y.; Shyu, A.B.; Muller, M.; Gaestel, M.; Resch, K.; Holtmann, H. The p38 MAP kinase pathway signals for cytokine-induced mRNA stabilization via MAP kinase-activated protein kinase 2 and an AU-rich region-targeted mechanism. EMBO J. 1999, 18, 4969–4980. [Google Scholar] [CrossRef]
- Winzen, R.; Thakur, B.K.; Dittrich-Breiholz, O.; Shah, M.; Redich, N.; Dhamija, S.; Kracht, M.; Holtmann, H. Functional analysis of KSRP interaction with the AU-rich element of interleukin-8 and identification of inflammatory mRNA targets. Mol. Cell. Biol. 2007, 27, 8388–8400. [Google Scholar] [CrossRef]
- Stoecklin, G.; Tenenbaum, S.A.; Mayo, T.; Chittur, S.V.; George, A.D.; Baroni, T.E.; Blackshear, P.J.; Anderson, P. Genome-wide analysis identifies interleukin-10 mRNA as target of tristetraprolin. J. Biol. Chem. 2008, 283, 11689–11699. [Google Scholar] [CrossRef]
- Ogilvie, R.L.; Sternjohn, J.R.; Rattenbacher, B.; Vlasova, I.A.; Williams, D.A.; Hau, H.H.; Blackshear, P.J.; Bohjanen, P.R. Tristetraprolin mediates interferon-gamma mRNA decay. J. Biol. Chem. 2009, 284, 11216–11223. [Google Scholar]
- Zhao, W.; Liu, M.; D’Silva, N.J.; Kirkwood, K.L. Tristetraprolin regulates interleukin-6 expression through p38 MAPK-dependent affinity changes with mRNA 3’ untranslated region. J. Interferon Cytokine Res. 2011, 31, 629–637. [Google Scholar] [CrossRef]
- Xie, Y.; Chen, C.; Stevenson, M.A.; Auron, P.E.; Calderwood, S.K. Heat shock factor 1 represses transcription of the IL-1beta gene through physical interaction with the nuclear factor of interleukin 6. J. Biol. Chem. 2002, 277, 11802–11810. [Google Scholar]
- Wang, X.; Khaleque, M.A.; Zhao, M.J.; Zhong, R.; Gaestel, M.; Calderwood, S.K. Phosphorylation of HSF1 by MAPK-activated protein kinase 2 on serine 121, inhibits transcriptional activity and promotes HSP90 binding. J. Biol. Chem. 2006, 281, 782–791. [Google Scholar]
- Scheller, J.; Chalaris, A.; Schmidt-Arras, D.; Rose-John, S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim. Biophys. Acta 2011, 1813, 878–888. [Google Scholar] [CrossRef]
- Radtke, S.; Wüller, S.; Yang, X.P.; Lippok, B.E.; Mütze, B.; Mais, C.; Schmitz-Van de Leur, H.; Bode, J.G.; Gaestel, M.; Heinrich, P.C.; et al. Cross-regulation of cytokine signalling: Pro-inflammatory cytokines restrict IL-6 signalling through receptor internalisation and degradation. J. Cell Sci. 2010, 123, 947–959. [Google Scholar] [CrossRef]
- Heo, K.S.; Chang, E.; Takei, Y.; Le, N.T.; Woo, C.H.; Sullivan, M.A.; Morrell, C.; Fujiwara, K.; Abe, J.I. Phosphorylation of protein inhibitor of activated STAT1 (PIAS1) by MAPK-activated protein kinase-2 inhibits endothelial inflammation via increasing both PIAS1 transrepression and SUMO E3 ligase activity. Arteriodcler. Thromb. Vasc. Biol. 2013, 33, 321–329. [Google Scholar] [CrossRef]
- Liu, B.; Yang, R.; Wong, K.A.; Getman, C.; Stein, N.; Teitell, M.A.; Cheng, G.; Wu, H.; Shuai, K. Negative regulation of NF-kappaB signalling by PIAS1. Mol. Cell. Biol. 2005, 25, 1113–1123. [Google Scholar]
- Stokoe, D.; Engel, K.; Campbell, D.G.; Cohen, P.; Gaestel, M. Identification of MAPKAP kinase 2 as a major enzyme responsible for the phosphorylation of the small mammalian heat shock proteins. FEBS Lett. 1992, 313, 307–313. [Google Scholar] [CrossRef]
- Clifton, A.D.; Young, P.R.; Cohen, P. A comparison of the substrate specificity of MAPKAP kinase-2 and MAPKAP kinase-3 and their activation by cytokines and cellular stress. FEBS Lett. 1996, 392, 209–214. [Google Scholar] [CrossRef]
- Kostenko, S.; Moens, U. Heat shock protein 27 phosphorylation: Kinases, phosphatases, functions and pathology. Cell. Mol. Life Sci. 2009, 66, 3289–3307. [Google Scholar] [CrossRef]
- Shiryaev, A.; Dumitriu, G.; Moens, U. Distinct roles of MK2 and MK5 in cAMP/PKA- and stress/p38MAPK-induced heat shock protein 27 phosphorylation. J. Mol. Signal. 2011, 6, 4. [Google Scholar] [CrossRef]
- Kato, K.; Tokuda, H.; Mizutani, J.; Adachi, S.; Matsushima-Nishiwaki, R.; Natsume, H.; Kozawa, O.; Otsuka, T. Role of HSP27 in tumor necrosis factor-a-stimulated interleukin-6 synthesis in osteoblasts. Int. J. Mol. Med. 2011, 28, 887–893. [Google Scholar]
- Tanabe, K.; Matsushima-Nishiwaki, R.; Dohi, S.; Kozawa, O. Phosphorylation status of heat shock protein 27 regulates the interleukin-1b-induced interleukin-6 synthesis in C6 glioma cells. Neuroscience 2010, 170, 1028–1034. [Google Scholar]
- Alford, K.A.; Glennie, S.; Turrell, B.R.; Rawlinson, L.; Saklatvala, J.; Dean, J.L. Heat shock protein 27 functions in inflammatory gene expression and transforming growth factor-beta-activated kinase-1 (TAK-1)-mediated signaling. J. Biol. Chem. 2007, 282, 6232–6241. [Google Scholar]
- Lasa, M.; Mahtani, K.R.; Finch, A.; Brewer, G.; Saklatvala, J.; Clark, A.R. Regulation of cyclooxygenase 2 mRNA stability by the mitogen-activated protein kinase p38 signaling cascade. Mol. Cell. Biol. 2000, 20, 4265–4274. [Google Scholar] [CrossRef]
- De, A.K.; Kodys, K.M.; Yeh, B.S.; Miller-Graziano, C. Exaggerated human monocyte IL-10 concomitant to minimal TNF-alpha induction by heat-shock protein (Hsp27) suggests Hsp27 is primarily an antiinflammatory stimulus. J. Immunol. 2000, 165, 3951–3958. [Google Scholar]
- Park, K.J.; Gaynor, R.B.; Kwak, Y.T. Heat shock protein 27 association with the I kappa B kinase complex regulates tumor necrosis factor alpha-induced NF-kappa B activation. J. Biol. Chem. 2003, 278, 35272–35278. [Google Scholar] [CrossRef]
- Sinsimer, K.S.; Gratacós, F.M.; Knapinska, A.M.; Krause, C.D.; Wierzbowski, A.V.; Mahler, L.R.; Scrudato, S.; Rivera, Y.M.; Gupta, S.; Turrin, D.K.; et al. Chaperone Hsp27, a novel subunit of AUF1 protein complexes, functions in AU-rich element-mediated mRNA decay. Mol. Cell. Biol. 2008, 28, 5223–5237. [Google Scholar] [CrossRef]
- Kubisch, C.; Dimagno, M.J.; Tietz, A.B.; Welsh, M.J.; Ernst, S.A.; Brandt-Nedelev, B.; Diebold, J.; Wagner, A.C.; Göke, B.; Williams, J.A.; et al. Overexpression of heat shock protein Hsp27 protects against cerulean-induced pancreatitis. Gastroenterology 2004, 127, 275–286. [Google Scholar] [CrossRef]
- Funding, A.T.; Johansen, C.; Gaestel, M.; Bibby, B.M.; Lilleholt, L.L.; Kragballe, K.; Iversen, L. Reduced oxazolone-induced skin inflammation in MAPKAP kinase 2 knockout mice. J. Invest. Dermatol. 2009, 129, 891–898. [Google Scholar] [CrossRef]
- Johansen, C.; Vestergaard, C.; Kragballe, K.; Kollias, G.; Gaestel, M.; Iversen, L. MK2 regulates the early stages of skin tumor promotion. Carcinogenesis 2009, 30, 2100–2108. [Google Scholar] [CrossRef]
- Fyhrquist, N.; Matikainen, S.; Lauerma, A. MK2 signaling: lessons on tissue specificity in modulation of inflammation. J. Invest. Dermatol. 2010, 130, 342–344. [Google Scholar] [CrossRef]
- Li, C.; Xu, J.; Li, F.; Chaudhary, S.C.; Weng, Z.; Wen, J.; Elmets, C.A.; Ahsan, H.; Athar, M. Unfolded protein response signaling and MAP kinase pathways underlie pathogenesis of arsenic-induced cutaneous inflammation. Cancer Prev. Res. 2011, 4, 2101–2109. [Google Scholar] [CrossRef]
- Pierce, B.L.; Argos, M.; Chen, Y.; Melkonian, S.; Parvez, F.; Islam, T.; Ahmed, A.; Hasan, R.; Rathouz, P.J.; Ahsan, H. Arsenic exposure, dietary patterns, and skin lesion risk in Bangladesh: A prospective study. Am. J. Epidemiol. 2011, 173, 345–354. [Google Scholar] [CrossRef]
- Tietz, A.B.; Malo, A.; Diebold, J.; Kotlyarov, A.; Herbst, A.; Kolligs, F.T.; Brandt-Nedelev, B.; Halangk, W.; Gaestel, M.; Göke, B.; Schäfer, C. Gene deletion of MK2 inhibits TNF-a and IL-6 and protects against cerulein-induced pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 290, G1298–G1306. [Google Scholar] [CrossRef]
- Li, Y.Y.; Ochs, S.; Gao, Z.R.; Malo, A.; Chen, C.J.; Lv, S.; Gallmeier, E.; Goke, B.; Schafer, C. Regulation of HSP60 and the role of MK2 in a new model of severe experimental pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2009, 297, G981–G989. [Google Scholar] [CrossRef]
- Michler, T.; Storr, M.; Kramer, J.; Ochs, S.; Malo, A.; Reu, S.; Göke, B.; Schäfer, C. Activation of cannabinoid receptor 2 reduces inflammation in acute experimental pancreatitis via intra-acinar activation of p38 and MK2-dependent mechanisms. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 304, G181–G192. [Google Scholar]
- Wagner, A.C.; Mazzucchelli, L.; Miller, M.; Camoratto, A.M.; Goke, B. CEP-1347 inhibits caerulein-induced rat pancreatic JNK activation and ameliorates caerulein pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 278, G165–G172. [Google Scholar]
- Yoshizuka, N.; Lai, M.; Liao, R.; Cook, R.; Xiao, C.; Han, J.; Sun, P. PRAK suppresses oncogenic ras-induced hematopoietic cancer development by antagonizing the JNK pathway. Mol. Cancer Res. 2012, 10, 810–820. [Google Scholar] [CrossRef]
- Lin, M.T.; Juan, C.Y.; Chang, K.J.; Chen, W.J.; Kuo, M.L. IL-6 inhibits apoptosis and retains oxidative DNA lesions in human gastric cancer AGS cells through up-regulation of anti-apoptotic gene mcl-1. Carcinogenesis 2001, 22, 1947–1953. [Google Scholar] [CrossRef]
- Poornima, I.G.; Parikh, P.; Shannon, R.P. Diabetic cardiomyopathy: The search for a unifying hypothesis. Circ. Res. 2006, 98, 596–605. [Google Scholar] [CrossRef]
- Thandavarayan, R.A.; Giridharan, V.V.; Sari, F.R.; Arumugam, S.; Veeraveedu, P.T.; Pandian, G.N.; Palaniyandi, S.S.; Ma, M.; Suzuki, K.; Gurusamy, N.; et al. Depletion of 14–3-3 protein exacerbates cardiac oxidative stress, inflammation and remodelling process via modulation of MAPK/NF-kB signalling pathways after streptozotocin-induced diabetes mellitus. Cell. Physiol. Biochem. 2011, 28, 911–922. [Google Scholar] [CrossRef]
- Wang, X.; Xu, L.; Wang, H.; Young, P.R.; Gaestel, M.; Feuerstein, G.Z. Mitogen-activated protein kinase-activated protein (MAPKAP) kinase 2 deficiency protects brain from ischemic injury in mice. J. Biol. Chem. 2002, 277, 43969–43972. [Google Scholar]
- Trentham, D.E.; Townes, A.S.; Kang, A.H. Autoimmunity type II collagen and experimental model of arthritis. J. Exp. Med. 1977, 146, 857–868. [Google Scholar]
- Hegen, M.; Gaestel, M.; Nickerson-Nutter, C.L.; Lin, L.L.; Telliez, J.B. MAPKAP kinase 2-deficient mice are resistant to collagen-induced arthritis. J. Immunol. 2006, 177, 1913–1917. [Google Scholar]
- Jagavelu, K.; Tietge, U.J.; Gaestel, M.; Drexler, H.; Schieffer, B.; Bavendiek, U. Systemic deficiency of the MAP kinase-activated protein kinase 2 reduces atherosclerosis in hypercholesterolemic mice. Circ. Res. 2007, 101, 1104–1112. [Google Scholar] [CrossRef]
- Ebrahimian, T.; Li, M.W.; Lemarié, C.A.; Simeone, S.M.; Pagano, P.J.; Gaestel, M.; Paradis, P.; Wassmann, S.; Schiffrin, E.L. Mitogen-activated protein kinase-activated protein kinase 2 in angiotensin II-induced inflammation and hypertension: Regulation of oxidative stress. Hypertension 2011, 57, 245–254. [Google Scholar] [CrossRef]
- Li, Q.; Yu, H.; Zinna, R.; Martin, K.; Herbert, B.; Liu, A.; Rossa, C., Jr.; Kirkwood, K.L. Silencing mitogen-activated protein kinase-activated protein kinase-2 arrests inflammatory bone loss. J. Pharmacol. Exp. Ther. 2011, 336, 633–642. [Google Scholar] [CrossRef]
- Jones, S.W.; Brockbank, S.M.; Clements, K.M.; Le Good, N.; Campbell, D.; Read, S.J.; Needham, M.R.; Newham, P. Mitogen-activated kinase-activated protein kinase 2 (MK2) modulates key biological pathways associated with OA disease pathology. Ostearthritis Cartilage 2009, 17, 124–131. [Google Scholar] [CrossRef]
- Braun, T.; Lepper, J.; Heiland, G.R.; Hofstetter, W.; Siegrist, M.; Lezuo, P.; Gaestel, M.; Rumpler, M.; Thaler, R.; Klaushofer, K.; et al. Mitogen-activated protein kinase 2 (MK2) regulates physiological and pathological bone turnover. J. Bone Miner. Res. 2012, 28, 936–947. [Google Scholar]
- Feng, Y.J.; Li, Y.Y. The role of p38 mitogen-activated protein kinase in the pathogenesis of inflammatory bowel disease. J. Dig. Dis. 2011, 12, 327–332. [Google Scholar] [CrossRef]
- Ghasemlou, N.; Lopez-Vales, R.; Lachance, C.; Thuraisingam, T.; Gaestel, M.; Radzioch, D.; David, S. Mitogen-activated protein kinase-activated protein kinase 2 (MK2) contributes to secondary damage after spinal cord injury. J. Neurosci. 2010, 30, 13750–13759. [Google Scholar]
- Ehlting, C.; Ronkina, N.; Böhmer, O.; Albrecht, U.; Bode, K.A.; Lang, K.S.; Kotlyarov, A.; Radzioch, D.; Gaestel, M.; Häussinger, D.; et al. Distinct functions of the mitogen-activated protein (MAPKAP) kinases MK2 and MK3: MK2 mediates lipopolysaccharide-induced signal transducers and activators of transcription 3 (STAT3) by preventing negative regulatory effects of MK3. J. Biol. Chem. 2011, 286, 24113–24124. [Google Scholar] [CrossRef]
- Lang, R. Tuning of macrophage responses by Stat3-inducing cytokines: molecular mechanisms and consequences in infection. Immunobiology 2005, 210, 63–76. [Google Scholar] [CrossRef]
- Shi, Y.; Kotlyarov, A.; Laass, K.; Gruber, A.D.; Butt, E.; Marcus, K.; Meyer, H.; Friedrich, A.; Volk, H.D.; Gaestel, M. Elimination of protein kinase MK5/PRAK activity by targeted homologous recombination. Mol. Cell. Biol. 2003, 23, 7732–7741. [Google Scholar] [CrossRef]
- Cohen, P. Targeting protein kinases for the development of anti-inflammatory drugs. Curr. Opin. Vell Biol. 2009, 21, 317–324. [Google Scholar] [CrossRef]
- Gaestel, M.; Kotlyarov, A.; Kracht, M. Targeting innate immunity protein kinase signaling in inflammation. Nat. Rev. Drug Discov. 2009, 8, 480–499. [Google Scholar] [CrossRef]
- Cohen, M.S.; Zhang, C.; Shokat, K.M.; Tauton, J. Structural bioinformatics-based design of selective, irreversible kinase inhibitors. Science 2005, 308, 1318–1321. [Google Scholar] [CrossRef]
- Maloney, D.J.; Hecht, S.M. Synthesis of a potent and selective inhibitor of p90 Rsk. Org. Lett. 2005, 7, 1097–1099. [Google Scholar] [CrossRef]
- Nguyen, T.L.; Gussio, R.; Smith, J.A.; Lannigan, D.A.; Hecht, S.M.; Scudiero, D.A.; Shoemaker, R.H.; Zaharevitz, D.W. Homology model of RSK2 N-terminal kinase domain, structure-based identification of novel RSK2 inhibitors, and preliminary common pharmacophore. Bioorg. Med. Chem. 2006, 14, 6097–6105. [Google Scholar] [CrossRef]
- Smith, J.A.; Maloney, D.J.; Clark, D.E.; Xu, Y.; Hecht, S.M.; Lannigan, D.A. Influence of rhamnose substituents on the potency of SL0101, an inhibitor of the Ser/thr kinase, RSK. Bioorg. Med. Chem. 2006, 14, 6034–6042. [Google Scholar] [CrossRef]
- Sapkota, G.P.; Cummings, L.; Newell, F.S.; Armstrong, C.; Bain, J.; Frodin, M.; Grauert, M.; Hoffmann, M.; Schnapp, G.; Steegmaier, M.; Cohen, P.; Alessi, D.R. BI-D1870 is a specific inhibitor of the p90 RSK (ribosomal S6 kinase) isoforms in vitro and in vivo. Biochem. J. 2007, 401, 29–38. [Google Scholar] [CrossRef]
- Shan, M.; O’Doherty, G.A. Synthesis of SL0101 carbasugar analogues: carbasugars via Pd-catalyzed cyclitolization and post-cyclitolization transformations. Org. Lett. 2010, 12, 2986–2989. [Google Scholar] [CrossRef]
- Hilinski, M.K.; Mrozowski, R.M.; Clark, D.E.; Lannigan, D.A. Analogs of the RSK inhibitor SL0101: Optimization of in vitro biological stability. Bioorg. Med. Chem. Lett. 2012, 22, 3244–3247. [Google Scholar]
- Bain, J.; Plater, L.; Elliott, M.; Shpiro, N.; Hastie, C.J.; McLauchlan, H.; Klevernic, I.; Arthur, J.S.; Alessi, D.R.; Cohen, P. The selectivity of protein kinase inhibitors: A further update. Biochem. J. 2007, 408, 297–315. [Google Scholar] [CrossRef]
- Bamford, M.J.; Alberti, M.J.; Bailey, N.; Davies, S.; Dean, D.K.; Gaiba, A.; Garland, S.; Harling, J.D.; Jung, D.K.; Panchal, T.A.; Parr, C.A.; Steadman, J.G.; Takle, A.K.; Townsend, J.T.; Wilson, D.M.; Witherington, J. (1H-imidazo[4,5-c]pyridine-2-yl)-1,2,5-oxadiazol-3-ylamine derivatives: A novel class of potent MSK-1-inhibitors. Bioorg. Med. Chem. Lett. 15, 3402–3406.
- Bamford, M.J.; Bailey, N.; Davies, S.; Dean, D.K.; Francis, L.; Panchal, T.A.; Parr, C.A.; Sehmi, S.; Steadman, J.G.; Takle, A.K.; Townsend, J.T. (1H-imidazo[4,5-c]pyridine-2-yl)-1,2,5-oxadiazol-3-ylamine derivatives: Further optimisation as highly potent and selective MSK-1-inhibitors. Bioorg. Med. Chem. Lett. 15, 3407–3411.
- Naqvi, S.; Macdonald, A.; McCoy, C.E.; Darragh, J.; Reith, A.D.; Arthur, J.S. Characterization of the cellular action of the MSK inhibitor SB-747651A. Biochem. J. 2012, 441, 347–357. [Google Scholar] [CrossRef]
- Beck, I.M.; Vanden Berghe, W.; Vermeulen, L.; Bougarne, N.; Vander Cruyssen, B.; Haegeman, G.; De Bosscher, K. Altered subcellular distribution induced by glucocorticoids contributes to NF-kappaB inhibition. EMBO J. 2008, 27, 1682–1693. [Google Scholar] [CrossRef]
- Barnes, P.J.; Adcock, I.M. Glucocorticoid resistance in inflammatory diseases. Lancet 2009, 373, 1905–1917. [Google Scholar] [CrossRef]
- Knauf, U.; Tschopp, C.; Gram, H. Negative regulation of protein translation by mitogen-activated protein kinase-interacting kinases 1 and 2. Mol. Cell. Biol. 2001, 21, 5500–5011. [Google Scholar] [CrossRef]
- Cherla, R.P.; Lee, S.Y.; Mees, P.L.; Tesh, V.L. Shiga toxin 1-induced cytokine production is mediated by MAP kinase pathways and translation initiation factor eIF4E in the macrophage-like THP-1 cells line. J. Leukoc. Biol. 2006, 79, 397–407. [Google Scholar] [CrossRef]
- Kjellerup, R.B.; Kragballe, K.; Iversen, L.; Johansen, C. Pro-inflammatory cytokines release in keratinocytes is mediated through the MAPK signal-integrating kinases. Exp. Dermatol. 2008, 17, 498–504. [Google Scholar] [CrossRef]
- Mourey, R.J.; Burnette, B.L.; Brustkern, S.J.; Daniels, J.S.; Hirsch, J.L.; Hood, W.F.; Meyers, M.J.; Mnich, S.J.; Pierce, B.S.; Saabye, M.J.; Schindler, J.F.; South, S.A.; Webb, E.G.; Zhang, J.; Anderson, D.R. A benzothiophene inhibitor of mitogen-activated protein kinase-activated protein kinase 2 inhibits tumor necrosis factor alpha and has oral anti-inflammatory efficacy in acute and chronic models of inflammation. J. Pharmacol. Exp. Ther. 2010, 333, 797–807. [Google Scholar] [CrossRef]
- Kosugi, T.; Mitchell, D.R.; Fujino, A.; Imai, M.; Kambe, M.; Kobayashi, S.; Makino, H.; Matsueda, Y.; Oue, Y.; Komatsu, K.; Imaizumi, K.; Sakai, Y.; Sugiura, S.; Takenouchi, O.; Unoki, G.; Yamakoshi, Y.; Cunliffe, V.; Frearson, J.; Gordon, R.; Harris, C.J.; Kalloo-Hosein, H.; Le, J.; Patel, G.; Simpson, D.J.; Sherborne, B.; Thomas, P.S.; Suzuki, N.; Takimoto-Kamimura, M.; Kataoka, K.I. Mitogen-activated protein kinase-activated protein kinase 2 (MAPKAP-K2) as an anti-inflammatory target: discovery and in vivo activity of selective pyrazolo[1,5-a]pyrimidine inhibitors using a focused library and structure-based optimization approach. J. Med. Chem. 2012, 55, 6700–6715. [Google Scholar] [CrossRef]
- Wu, J.P.; Wang, J.; Abeywardane, A.; Andersen, D.; Emmanuel, M.; Gautschi, E.; Goldberg, D.R.; Kashem, M.A.; Lukas, S.; Mao, W.; Martin, L.; Morwick, T.; Moss, N.; Pargellis, C.; Patel, U.R.; Patnaude, L.; Peet, G.W.; Skow, D.; Snow, R.J.; Ward, Y.; Werneburg, B.; White, A. The discovery of carboline analogs as potent MAPKAP-K2 inhibitors. Bioorg. Med. Chem. Lett. 2007, 17, 4664–4669. [Google Scholar] [CrossRef]
- Schlapbach, A.; Feifel, R.; Hawtin, S.; Heng, R.; Koch, G.; Moebitz, H.; Revesz, L.; Scheufler, C.; Velcicky, J.; Waelchli, R.; Huppertz, C. Pyrrolo-pyrimidones: a novel class of MK2 inhibitors with potent cellular activity. Bioorg. Med. Chem. Lett. 2008, 18, 6142–6146. [Google Scholar] [CrossRef]
- Revesz, L.; Schlapbach, A.; Aichholz, R.; Feifel, R.; Hawtin, S.; Heng, R.; Hiestand, P.; Jahnke, W.; Koch, G.; Kroemer, M.; Möbitz, H.; Scheufler, C.; Velcicky, J.; Huppertz, C. In vivo and in vitro SAR of tetracyclic MAPKAP-K2 (MK2) inhibitors, Part I. Bioorg. Med. Chem. Lett. 2010, 20, 4715–4718. [Google Scholar] [CrossRef]
- Velcicky, J.; Feifel, R.; Hawtin, S.; Heng, R.; Huppertz, C.; Koch, G.; Kroemer, M.; Moebitz, H.; Revesz, L.; Scheufler, C.; Schlapbach, A. Novel 3-aminopyrazole inhibitors of MK-2 discovered by scaffold hopping strategy. Bioorg. Med. Chem. Lett. 2010, 20, 1293–1297. [Google Scholar] [CrossRef]
- Kaptein, A.; Oubrie, A.; de Zwart, E.; Hoogenboom, N.; de Wit, J.; van de Kar, B.; van Hoek, M.; Vogel, G.; de Kimpe, V.; Schultz-Fademrecht, C.; Borsboom, J.; van Zeeland, M.; Versteegh, J.; Kazemier, B.; de Roos, J.; Wijnands, F.; Dulos, J.; Jaeger, M.; Leandro-Garcia, P.; Barf, T. Discovery of selective and orally available spiro-3-piperidyl ATP-competitive MK2 inhibitors. Bioorg. Med. Chem. Lett. 2011, 21, 3823–3827. [Google Scholar] [CrossRef]
- Huang, X.; Zhu, X.; Chen, X.; Zhou, W.; Xiao, D.; Degrado, S.; Aslanian, R.; Fossetta, J.; Lundell, D.; Tian, F.; Trivedi, P.; Palani, A. A three-step protocol for lead optimization: quick identification of key conformational features and functional groups in the SAR studies of non-ATP competitive MK2 (MAPKAPK2) inhibitors. Bioorg. Med. Chem. Lett. 2012, 22, 65–70. [Google Scholar] [CrossRef]
- Coxon, P.Y.; Rane, M.J.; Uriarte, S.; Powell, D.W.; Singh, S.; Butt, W.; Chen, Q.; McLeish, K.R. MAPK-activated protein kinase-2 participates in p38 MAPK-dependent and ERK-dependent functions in human neutrophils. Cell. Signal. 2003, 15, 993–1001. [Google Scholar] [CrossRef]
- Lopes, L.B.; Flynn, C.; Komalavilas, P.; Panitch, A.; Brophy, C.M.; Seal, B.L. Inhibition of HSP27 phosphorylation by a cell-permeant MAPKAP kinase 2 inhibitor. Biochem. Biophys. Res. Commun. 2009, 382, 539–539. [Google Scholar]
- Brugnano, J.L.; Chan, B.K.; Seal, B.L.; Panitch, A. Cell-penetrating peptides can confer biological function: regulation of inflammatory cytokines in human monocytes by MK2 inhibitor peptides. J. Control Release 2011, 155, 128–133. [Google Scholar] [CrossRef]
- Muto, A.; Panitch, A.; Kim, N.; Park, K.; Komalavilas, P.; Brophy, C.M.; Dardik, A. Inhibition of mitogen activated protein kinase activated protein kinase II with MMI-0100 reduces intimal hyperplasia ex vivo and in vivo. Vascul. Pharmacol. 2012, 56, 47–55. [Google Scholar] [CrossRef]
- Kostenko, S.; Khan, M.T.; Sylte, I.; Moens, U. The diterpenoid alkaloid noroxoaconitine is a Mapkap kinase 5 (MK5/PRAK) inhibitor. Cell. Mol. Life Sci. 2011, 68, 289–301. [Google Scholar] [CrossRef]
- Andrews, M.; Brys, R.; Vandeghinste, N.; Pujuguet, P.; Namour, F.; Lorenzon, G.; Chambers, M.; Schmidt, W.; Clase, A.; Birault, V.; Dixon, G. Small molecules against the novel target MAPKAPK5 show bone protection and anti-inflammatory activity in in vivo models of rheumatoid arthritis. Ann. Rheum. Dis. 2009, 68, 590. [Google Scholar]
- Anwar, A.; Hosoya, T.; Leong, K.M.; Onogi, H.; Okuno, Y.; Hiramatsu, T.; Koyama, H.; Suzuki, M.; Hagiwara, M.; Garcia-Blanco, M.A. The kinase inhibitor SFV785 dislocates dengue virus envelope protein from the replication complex and blocks virus assembly. PLoS One 2011, 6, e23246. [Google Scholar] [CrossRef]
- Andrews, M.J.; Clase, J.A.; Bar, G.; Tricarico, G.; Edwards, P.J.; Brys, R.; Chambers, M.; Schmidt, W.; MacLeod, A.; Hirst, K.; Allen, V.; Birault, V.; Le, J.; Harris, J.; Self, A.; Nash, K.; Dixon, G. Discovery of a series of imidazopyrazine small molecule inhibitors of the kinase MAPKAPK5, that show activity using in vitro and in vivo models of rheumatoid arthritis. Bioorg. Med. Chem. Lett. 2012, 22, 2266–2270. [Google Scholar] [CrossRef]
- Namour, F.; Vanhoutte, F.P.; Beetens, J.; Blockhuys, S.; De Weer, M.; Wigerinck, P. Pharmacokinetics, safety, and tolerability of GLPG0259, a mitogen-activated protein kinase-activated protein kinase 5 (MAPKAPK5) inhibitor, given as single and multiple doses to healthy male subject. Drugs R D 2012, 12, 141–163. [Google Scholar]
- Westhovens, R.; De Keyser, F.; Rekalov, D.; Nasonov, E.L.; Beetens, J.; Van der Aa, A.; Wigerinck, P.; Namour, F.; Vanhoutte, F.; Durez, P. Oral administration of GLPG0259, an inhibitor of MAPKAPK5, a new target for the treatment of rheumatoid arthritis: A phase II, randomised double-blind, placebo-controlled, multicentre trial. Ann. Rheum. Dis. 2012. [Google Scholar] [CrossRef]
- Dong, J.; Jimi, E.; Zhong, H.; Hayden, M.S.; Ghosh, S. Repression of gene expression by unphosphorylated NF-kappaB p65 through epigenetic mechanisms. Genes Dev. 2008, 22, 1159–1173. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Moens, U.; Kostenko, S.; Sveinbjørnsson, B. The Role of Mitogen-Activated Protein Kinase-Activated Protein Kinases (MAPKAPKs) in Inflammation. Genes 2013, 4, 101-133. https://doi.org/10.3390/genes4020101
Moens U, Kostenko S, Sveinbjørnsson B. The Role of Mitogen-Activated Protein Kinase-Activated Protein Kinases (MAPKAPKs) in Inflammation. Genes. 2013; 4(2):101-133. https://doi.org/10.3390/genes4020101
Chicago/Turabian StyleMoens, Ugo, Sergiy Kostenko, and Baldur Sveinbjørnsson. 2013. "The Role of Mitogen-Activated Protein Kinase-Activated Protein Kinases (MAPKAPKs) in Inflammation" Genes 4, no. 2: 101-133. https://doi.org/10.3390/genes4020101
APA StyleMoens, U., Kostenko, S., & Sveinbjørnsson, B. (2013). The Role of Mitogen-Activated Protein Kinase-Activated Protein Kinases (MAPKAPKs) in Inflammation. Genes, 4(2), 101-133. https://doi.org/10.3390/genes4020101



