Intron Retention and Alzheimer’s Disease (AD): A Review of Regulation Genes Implicated in AD
Abstract
1. Introduction
2. Methods
3. Results and Discussion
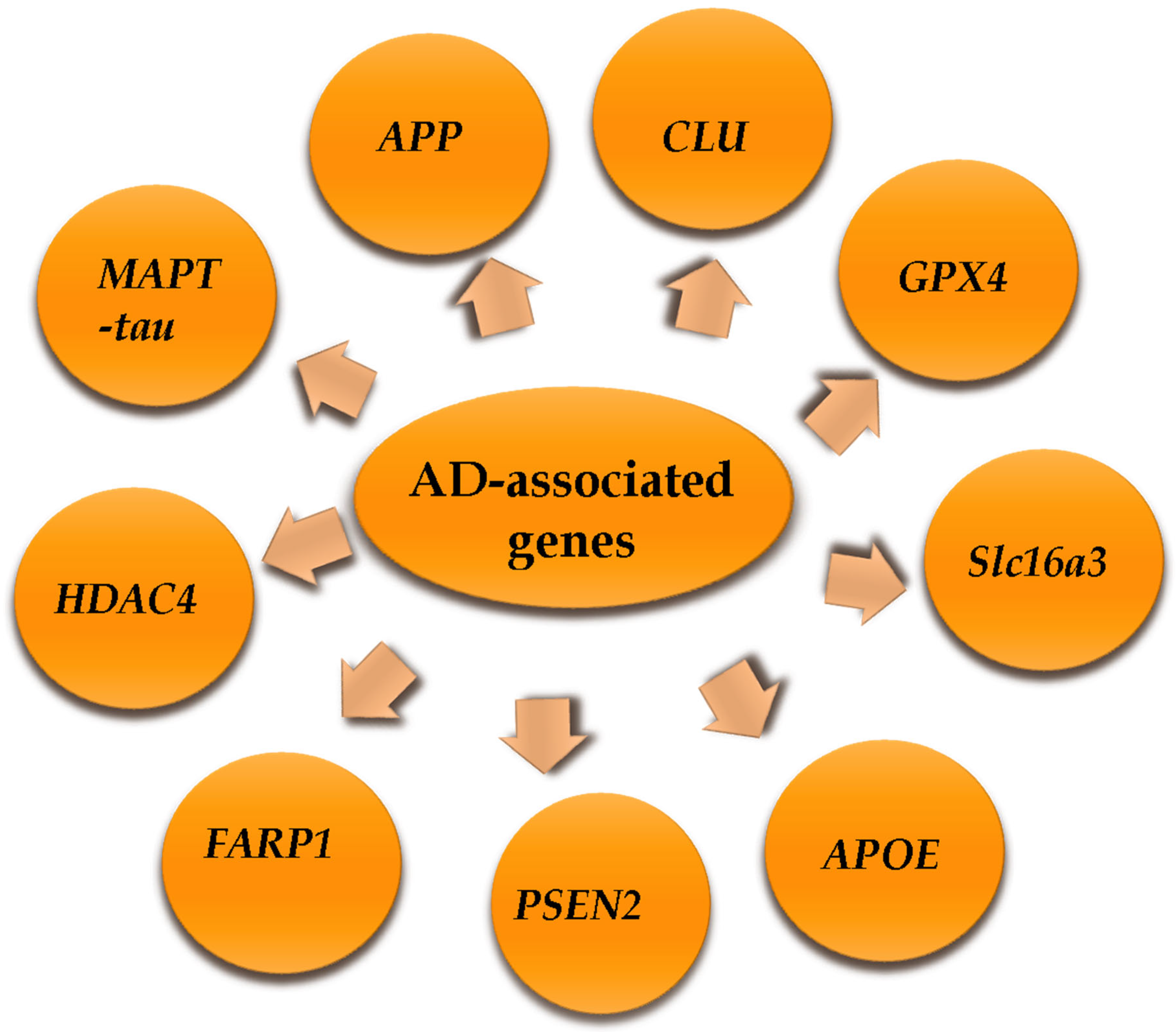
3.1. Types of AD-Associated Genes
3.1.1. Apolipoprotein E (APOE) Gene
3.1.2. Microtubule-Associated Protein Tau (MAPT-Tau) Gene
3.1.3. Presenilin 2 (Psen2) Genes
3.1.4. FERM, Rho/ArhGEF, and Pleckstrin Domain Protein 1 (Farp) Gene
3.1.5. Glutathione Peroxidase 4 (Gpx4) Gene
3.1.6. Clusterin (Clu) Gene
3.1.7. Human Histone Deacetylase 4 (HDAC4) Gene
3.1.8. Solute Carrier Family 16, Member 3 (Slc16a3) Gene
3.1.9. Amyloid Beta Precursor Protein (App) Gene
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kumar, A.; Sidhu, J.; Lui, F.; Tsao, J.W. Alzheimer Disease. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Bekris, L.M.; Yu, C.E.; Bird, T.D.; Tsuang, D.W. Genetics of Alzheimer disease. J. Geriatr. Psychiatry Neurol. 2010, 23, 213–227. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belgrader, P.; Cheng, J.; Zhou, X.; Stephenson, L.S.; Maquat, L.E. Mammalian nonsense codons can be cis effectors of nuclear mRNA half-life. Mol. Cell. Biol. 1994, 14, 8219–8228. [Google Scholar] [PubMed]
- Monteuuis, G.; Wong, J.L.; Bailey, C.G.; Schmitz, U.; Rasko, J.J. The changing paradigm of intron retention: Regulation, ramifications and recipes. Nucleic Acids Res. 2019, 47, 11497–11513. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adusumalli, S.; Ngian, Z.K.; Lin, W.Q.; Benoukraf, T.; Ong, C.T. Increased intron retention is a post-transcriptional signature associated with progressive aging and Alzheimer’s disease. Aging Cell 2019, 18, e12928. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Olthof, A.M.; Hyatt, K.C.; Kanadia, R.N. Minor intron splicing revisited: Identification of new minor intron-containing genes and tissue-dependent retention and alternative splicing of minor introns. BMC Genom. 2019, 20, 686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huang, H.D.; Horng, J.T.; Lin, F.M.; Chang, Y.C.; Huang, C.C. SpliceInfo: An information repository for mRNA alternative splicing in human genome. Nucleic Acids Res. 2005, 33, D80–D85. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Qin, N.; Zhang, S.P.; Reitz, T.L.; Mei, J.M.; Flores, C.M. Cloning, expression, and functional characterization of human cyclooxygenase-1 splicing variants: Evidence for intron 1 retention. J. Pharmacol. Exp. Ther. 2005, 315, 1298–1305. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.; Ding, D.; Li, X.; Shen, T.; Fu, H.; Zhong, H.; Wei, G.; Ni, T. Prevalent intron retention fine-tunes gene expression and contributes to cellular senescence. Aging Cell 2020, 19, e13276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Q.; Lee, J.A.; Black, D.L. Neuronal regulation of alternative pre-mRNA splicing. Nat. Rev. 2007, 8, 819–831. [Google Scholar] [CrossRef]
- Norris, A.D.; Calarco, J.A. Emerging Roles of Alternative Pre-mRNA Splicing Regulation inNeuronal Development and Function. Front. Neurosci. 2012, 6, 122. [Google Scholar] [CrossRef]
- Raj, B.; Cedillo, J.; Zhang, K. A high-thrοughput screen οf intrοn retentiοn in neurοnal transcripts. RNA 2014, 20, 846–859. [Google Scholar]
- Mauger, O.; Lemoine, F.; Scheiffele, P. Targeted Intron Retention and Excision for Rapid Gene Regulation in Response to Neuronal Activity. Neuron 2016, 92, 1266–1278. [Google Scholar] [CrossRef] [PubMed]
- Bai, B.; Wang, X.; Li, Y.; Chen, P.C.; Yu, K.; Dey, K.K.; Yarbro, J.M.; Han, X.; Lutz, B.M.; Rao, S.; et al. Deep Multilayer Brain Proteomics Identifies Molecular Networks in Alzheimer’s Disease Progression. Neuron 2020, 105, 975–991. [Google Scholar] [CrossRef] [PubMed]
- Twine, N.A.; Janitz, K.; Wilkins, M.R.; Janitz, M. Whole transcriptome sequencing reveals gene expression and splicing differences in brain regions affected by Alzheimer’s disease. PLoS ONE 2011, 6, e16266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bai, Y.; Chen, L.; Zhang, H. Intrοn retentiοn in SOD1 and GPX1 genes in Alzheimer’s disease. Free Radic. Biοl. Med. 2013, 65, 1234–1242. [Google Scholar]
- Middleton, R.; Gao, D.; Thomas, A.; Singh, B.; Au, A.; Wong, J.J.; Bomane, A.; Cosson, B.; Eyras, E.; Rasko, J.E.; et al. IR Finder: Assessing the impact of intron retention on mammalian gene expression. Genome Biol. 2017, 18, 51. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boutz, P.L.; Bhutkar, A.; Sharp, P.A. Detained introns are a novel, widespread class of post-transcriptionally spliced introns. Genes Dev. 2015, 29, 63–80. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Naro, C.; Jolly, A.; Di Persio, S.; Bielli, P.; Setterblad, N.; Alberdi, A.J.; Vicini, E.; Geremia, R.; De la Grange, P.; Sette, C. An orchestrated intron retention program in meiosis controls timely usage of transcripts during germ cell differentiation. Dev. Cell 2017, 41, 82–93. [Google Scholar] [CrossRef]
- Yap, K.; Lim, Z.Q.; Khandelia, P.; Friedman, B.; Makeyev, E.V. Coordinated regulation of neuronal mRNA steady-state levels through developmentally controlled intron retention. Genes Dev. 2012, 26, 1209–1223. [Google Scholar] [CrossRef]
- Buckley, P.T.; Khaladkar, M.; Kim, J.; Eberwine, J. Cytoplasmic intron retention, function, splicing, and the sentinel RNA hypothesis. Wiley Interdiscip. Rev. RNA 2014, 5, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Powers, K.T.; Szeto, J.-Y.A.; Schaffitzel, C. New insights into no-go, non-stop and nonsense-mediated mRNA decay complexes. Curr. Opin. Struct. Biol. 2020, 65, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Lejeune, F.; Maquat, L.E. Mechanistic links between nonsense-mediated mRNA decay and pre-mRNA splicing in mammalian cells. Curr. Opin. Cell Biol. 2005, 17, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Rekosh, D.; Hammarskjold, M.L. Intron retention in viruses and cellular genes: Detention, border controls and passports. Wiley Interdiscip. Rev. RNA 2018, 9, e1470. [Google Scholar] [CrossRef] [PubMed]
- Braunschweig, U.; Barbosa-Morais, N.L.; Pan, Q.; Nachman, E.N.; Alipanahi, B.; Gonatopoulos-Pournatzis, T.; Frey, B.; Irimia, M.; Blencowe, B.J. Widespread intron retention in mammals functionally tunes transcriptomes. Genome Res. 2014, 24, 1774–1786. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wong, J.J.-L.; Au, A.Y.; Ritchie, W.; Rasko, J.E. Intron retention in mRNA: No longer nonsense: Known and putative roles of intron retention innormal and disease biology. Bioessays 2017, 38, 41–49. [Google Scholar] [CrossRef]
- Mollet, I.G.; Ben-Dov, C.; Felício-Silva, D.; Grosso, A.R.; Eleutério, P.; Alves, R.; Staller, R.; Silva, T.S.; Carmo-Fonseca, M. Unconstrained mining of transcript data reveals increased alternative splicing complexity in the human transcriptome. Nucleic Acids Res. 2010, 38, 4740–4754. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zheng, J.T.; Lin, C.X.; Fang, Z.Y.; Li, H.D. Intron Retention as a Mode for RNA-Seq Data Analysis. Front. Genet. 2020, 11, 586. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jacob, A.G.; Smith, C.W.J. Intron retention as a component of regulated gene expression programs. Hum. Genet. 2017, 136, 1043–1057. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grabski, D.F.; Broseus, L.; Kumari, B.; Rekosh, D.; Hammarskjold, M.L.; Ritchie, W. Intron retention and its impact on gene expression and protein diversity: A review and a practical guide. Wiley Interdiscip. Rev. RNA 2021, 12, e1631. [Google Scholar] [CrossRef] [PubMed]
- Buckley, P.T.; Lee, M.T.; Sul, J.Y.; Miyashiro, K.Y.; Bell, T.J.; Fisher, S.A.; Kim, J.; Eberwine, J. Cytoplasmic intron sequence-retaining transcripts can be dendritically targeted via ID element retrotransposons. Neuron 2011, 69, 877–884. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, H.D.; Funk, C.C.; McFarland, K.; Dammer, E.B.; Allen, M.; Carrasquillo, M.M.; Levites, Y.; Chakrabarty, P.; Burgess, J.D.; Wang, X.; et al. Integrative functional genomic analysis of intron retention in human and mouse brain with Alzheimer’s disease. Alzheimers Dement. 2021, 17, 984–1004. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ping, L.; Duong, D.M.; Yin, L.; Gearing, M.; Lah, J.J.; Levey, A.I.; Seyfried, N.T. Global quantitative analysis of the human brain proteome in Alzheimer’s and Parkinson’s disease. Sci. Data 2018, 5, 180036–181000. [Google Scholar] [CrossRef]
- Giannopoulou, A.F.; Konstantakou, E.G.; Velentzas, A.D.; Avgeris, S.N.; Avgeris, M.; Papandreou, N.C.; Zoi, I.; Filippa, V.; Katarachia, S.; Lampidonis, A.D.; et al. Gene-Specific Intron Retention Serves as Molecular Signature that Distinguishes Melanoma from Non-Melanoma Cancer Cells in Greek Patients. Int. J. Mol. Sci. 2019, 20, 937. [Google Scholar] [CrossRef]
- El-Seedy, A.; Pellerin, L.; Page, G.; Ladeveze, V. Identification of Intron Retention in the Slc16a3 Gene Transcript Encoding the Transporter MCT4 in the Brain of Aged and Alzheimer-Disease Model (APPswePS1dE9) Mice. Genes 2023, 14, 1949. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ruiz-Gabarre, D.; Vallés-Saiz, L.; Carnero-Espejo, A.; Ferrer, I.; Hernández, F.; Garcia-Escudero, R.; Ávila, J.; García-Escudero, V. Intron retention as a productive mechanism in human MAPT: RNA species generated by retention of intron 3. EBioMedicine 2024, 100, 104953. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dieter, L.S.; Estus, S. Isoform of APOE with retained intron 3; quantitation and identification of an associated single nucleotide polymorphism. Mol. Neurodegener. 2010, 5, 34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Course, M.M.; Gudsnuk, K.; Keene, C.D.; Bird, T.D.; Jayadev, S.; Valdmanis, P.N. Aberrant splicing of PSEN2, but not PSEN1, in individuals with sporadic Alzheimer’s disease. Brain 2023, 146, 507–518. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Casañas-Sánchez, V.; Pérez, J.A.; Fabelo, N.; Quinto-Alemany, D.; Díaz, M.L. Docosahexaenoic (DHA) modulates phospholipid-hydroperoxide glutathione peroxidase (Gpx4) gene expression to ensure self-protection from oxidative damage in hippocampal cells. Front. Physiol. 2015, 6, 203. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Han, S.; Nho, K.; Lee, Y. Alternative Splicing Regulation of an Alzheimer’s Risk Variant in CLU. Int. J. Mol. Sci. 2020, 21, 7079. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harold, D.; Abraham, R.; Hollingworth, P.; Sims, R.; Gerrish, A.; Hamshere, M.L.; Pahwa, J.S.; Moskvina, V.; Dowzell, K.; Williams, A.; et al. Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat. Genet. 2009, 41, 1088–1093. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rockenstein, E.M.; McConlogue, L.; Tan, H.; Power, M.; Masliah, E.; Mucke, L. Levels and alternative splicing of amyloid β protein precursor (APP) transcripts in brains of APP transgenic mice and humans with Alzheimer’s disease. J. Biol. Chem. 1995, 270, 28257–28267. [Google Scholar] [CrossRef]
- Bu, G. Apolipoprotein E and its receptors in Alzheimer’s Disease: Pathways, pathogenesis and therapy. Nat. Rev. Neurosci. 2009, 10, 333–344. [Google Scholar] [CrossRef]
- Kim, J.; Basak, J.M.; Holtzman, D.M. The role of Apolipoprotein E in Alzheimer’s Disease. Neuron 2009, 63, 287–303. [Google Scholar] [CrossRef]
- Boyles, J.K.; Pitas, R.E.; Wilson, E.; Mahley, R.W.; Taylor, J.M. Apolipoprotein E associated with astrocytic glia of the CNS and with nonmyelinating glia of the peripheral nervous system. J. Clin. Investig. 1985, 76, 1501–1513. [Google Scholar] [CrossRef]
- Pitas, R.E.; Boyles, J.K.; Lee, S.H.; Hui, D.; Weisgraber, K.H. Lipoproteins and their receptors in the central nervous system. Characterization of the lipoproteins in cerebrospinal fluid and identification of apolipoprotein B,E(LDL) receptors in the brain. J. Biol. Chem. 1987, 262, 14352–14360. [Google Scholar] [CrossRef]
- Grehan, S.; Tse, E.; Taylor, J.M. Two distal downstream enhancers direct expression of the human apolipoprotein E gene to astrocytes in the brain. J. Neurosci. 2001, 21, 812–822. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stone, D.J.; Rozovsky, I.; Morgan, T.E.; Anderson, C.P.; Hajian, H.; Finch, C.E. Astrocytes and microglia respond to estrogen with increased apoE mRNA in vivo and in vitro. Exp. Neurol. 1997, 143, 313–318. [Google Scholar] [CrossRef]
- Xu, Q.; Walker, D.; Bernardo, A.; Brodbeck, J.; Balestra, M.E.; Huang, Y. Intron-3 retention/splicing controls neuronal expression of apolipoprotein E in the CNS. J. Neurosc. 2008, 28, 1452–1459. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, D.; Reynolds, R.H.; Gustavsson, E.K.; García-Ruiz, S.; D’Sa, K.; Fairbrother-Browne, A.; Vandrovcova, J.; International Parkinson’s Disease Genomics Consortium (IPDGC); Hardy, J.; et al. Human-lineage-specific genomic elements are associated with neurodegenerative disease and APOE transcript usage. Nat. Commun. 2021, 12, 2076. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muralidar, S.; Ambi, S.V.; Sekaran, S.; Thirumalai, D.; Palaniappan, B. Role of tau protein in Alzheimer’s disease: The prime pathological player. Int. J. Biol. Macromol. 2020, 163, 1599–1617. [Google Scholar] [CrossRef]
- Corsi, A.; Bombieri, C.; Valenti, M.T.; Romanelli, M.G. Tau isoforms: Gaining insight into MAPT alternative splicing. Int. J. Mol. Sci. 2022, 23, 15383. [Google Scholar] [CrossRef]
- Andreadis, A. Tau gene alternative splicing: Expression patterns, regulation and modulation of function in normal brain and neurodegenerative diseases. Biochim. Biophys. Acta Mol. Basis Dis. 2005, 1739, 91–103. [Google Scholar] [CrossRef]
- Liu, F.; Gong, C.X. Tau exon 10 alternative splicing and tauopathies. Mol. Neurodegener. 2008, 3, 8. [Google Scholar] [CrossRef]
- Wei, M.L.; Andreadis, A. Splicing of a regulated exon reveals additional complexity in the axonal microtubule-associated protein tau. J. Neurochem. 1998, 70, 1346–1356. [Google Scholar] [CrossRef]
- Gendron, T.F.; Petrucelli, L. The role of tau in neurodegeneration. Mol. Neurodegener. 2009, 4, 13. [Google Scholar] [CrossRef]
- Kosik, K.S.; Orecchio, L.D.; Bakalis, S.; Neve, R.L. Developmentally regulated expression of specific tau sequences. Neuron 1989, 2, 1389–1397. [Google Scholar] [CrossRef]
- Amadoro, G.; Latina, V.; Corsetti, V.; Calissano, P. N-terminal tau truncation in the pathogenesis of Alzheimer’s disease (AD): Developing a novel diagnostic and therapeutic approach. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165584. [Google Scholar] [CrossRef] [PubMed]
- Reifert, J.; Hartung-Cranston, D.; Feinstein, S.C. Amyloid beta-mediated cell death of cultured hippocampal neurons reveals extensive Tau fragmentation without increased full-length tau phosphorylation. J. Biol. Chem. 2011, 286, 20797–20811. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hsieh, Y.C.; Guo, C.; Yalamanchili, H.K.; Abreha, M.; Al-Ouran, R.; Li, Y.; Dammer, E.B.; Lah, J.J.; Levey, A.I.; Bennett, D.A.; et al. Tau-Mediated Disruption of the Spliceosome Triggers Cryptic RNA Splicing and Neurodegeneration in Alzheimer’s Disease. Cell Rep. 2019, 29, 301–316.e10. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- García-Escudero, V.; Ruiz-Gabarre, D.; Gargini, R.; Pérez, M.; García, E.; Cuadros, R.; Hernández, I.H.; Cabrera, J.R.; García-Escudero, R.; Lucas, J.J.; et al. A new non-aggregative splicing isoform of human Tau is decreased in Alzheimer’s disease. Acta Neuropathol. 2021, 142, 159–177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cuadros, R.; Pérez, M.; Ruiz-Gabarre, D.; Hernández, F.; García-Escudero, V.; Avila, J. Specific Peptide from the Novel W-Tau Isoform Inhibits Tau and Amyloid β Peptide Aggregation In Vitro. ACS Chem. Neurosci. 2022, 13, 1974–1978. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ngian, Z.K.; Tan, Y.Y.; Choo, C.T.; Lin, W.Q.; Leow, C.Y.; Mah, S.J.; Lai, M.K.; Chen, C.L.; Ong, C.T. Truncated Tau caused by intron retention is enriched in Alzheimer’s disease cortex and exhibits altered biochemical properties. Proc. Natl. Acad. Sci. USA 2022, 119, e2204179119. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Domene-Serrano, I.; Cuadros, R.; Hernandez, F.; Avila, J.; Santa-Maria, I. Tridimensional Structural Analysis of Tau Isoforms Generated by Intronic Retention. J. Alzheimers Dis. Rep. 2023, 7, 1259–1265. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ruiz-Gabarre, D.; Carnero-Espejo, A.; Ávila, J.; García-Escudero, V. What’s in a Gene? The Outstanding Diversity of MAPT. Cells 2022, 11, 840. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- García-Moreno, J.F.; Romão, L. Perspective in Alternative Splicing Coupled to Nonsense-Mediated mRNA Decay. Int. J. Mol. Sci. 2020, 21, 9424. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Braggin, J.E.; Bucks, S.A.; Course, M.M.; Smith, C.L.; Sopher, B.; Osnis, L.; Shuey, K.D.; Domoto-Reilly, K.; Caso, C.; Kinoshita, C.; et al. Alternative splicing in a presenilin 2 variant associated with Alzheimer disease. Ann. Clin. Transl. Neurol. 2019, 6, 762–777. [Google Scholar] [CrossRef]
- Cheadle, L.; Biederer, T. The novel synaptogenic protein Farp1 links postsynaptic cytoskeletal dynamics and transsynaptic organization. J. Cell Biol. 2012, 199, 985–1001. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Imai, H.; Nakagawa, Y. Biological significance of phospholipid hydroperoxide glutathione peroxidase (PHGPx, GPx4) in mammalian cells. Free Radic. Biol. Med. 2003, 34, 145–169. [Google Scholar] [CrossRef]
- Savaskan, N.E.; Ufer, C.; Kühn, H.; Borchert, A. Molecular biology of glutathione peroxidase 4: From genomic structure to developmental expression and neural function. Biol. Chem. 2007, 388, 1007–1017. [Google Scholar] [CrossRef]
- Ursini, F.; Maiorino, M. Lipid peroxidation and ferroptosis: The role of GSH and GPx4. Free Radic. Biol. Med. 2020, 152, 175–185. [Google Scholar] [CrossRef]
- Díaz, M.; Casañas-Sánchez, V.; Marín, R.; Pérez, J.A. Fighting against Lipid Peroxidation in the Brain: The Unique Story of Docosahexaenoic Acid. In Lipid Peroxidation: Inhibition, Effects and Mechanisms; Catalá, A., Ed.; Nova Science Publishers Inc.: New York, NY, USA, 2017; pp. 15–26. [Google Scholar]
- Wong, J.J.; Ritchie, W.; Ebner, O.A.; Selbach, M.; Wong, J.W.; Huang, Y.; Gao, D.; Pinello, N.; Gonzalez, M.; Baidya, K.; et al. Orchestrated intron retention regulates normal granulocyte differentiation. Cell 2013, 154, 583–595. [Google Scholar] [CrossRef]
- Liu, G.; Wang, H.; Liu, J.; Li, J.; Li, H.; Ma, G.; Jiang, Y.; Chen, Z.; Zhao, B.; Li, K. The CLU gene rs11136000 variant is significantly associated with Alzheimer’s disease in Caucasian and Asian populations. Neuromol. Med. 2014, 16, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Li, X.; Ma, G.; Jiang, Y.; Liao, M.; Feng, R.; Zhang, L.; Liu, J.; Wang, G.; Zhao, B.; et al. CLU rs9331888 Polymorphism Contributes to Alzheimer’s Disease Susceptibility in Caucasian But Not East Asian Populations. Mol. Neurobiol. 2016, 53, 1446–1451. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Mao, Z.; Woody, S.K.; Brinton, R.D. Sex differences in metabolic aging of the brain: Insights into female susceptibility to Alzheimer’s disease. Neurobiol. Aging 2016, 42, 69–79. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schwartz, S.; Truglio, M.; Scott, M.J.; Fitzsimons, H.L. Long-Term Memory in Drosophila Is Influenced by Histone Deacetylase HDAC4 Interacting with SUMO-Conjugating Enzyme Ubc9. Genetics 2016, 203, 1249–1264. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miskalis, A.; Shirguppe, S.; Winter, J.; Elias, G.; Swami, D.; Nambiar, A.; Stilger, M.; Woods, W.S.; Gosstola, N.; Gapinske, M.; et al. SPLICER: A highly efficient base editing toolbox that enables in vivo therapeutic exon skipping. Nat. Commun. 2024, 15, 10354. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yuan, H.; Li, N.; Fu, D.; Ren, J.; Hui, J.; Peng, J.; Liu, Y.; Qiu, T.; Jiang, M.; Pan, Q.; et al. Histone methyltransferase SETD2 modulates alternative splicing to inhibit intestinal tumorigenesis. J. Clin. Investig. 2017, 127, 3375–3391. [Google Scholar] [CrossRef]
- Dvinge, H.; Bradley, R.K. Widespread intron retention diversifies most cancertranscriptomes. Genome Med. 2015, 7, 45. [Google Scholar] [CrossRef]
- Bhadra, M.; Howell, P.; Dutta, S.; Heintz, C.; Mair, W.B. Alternative splicing in aging and longevity. Hum. Genet. 2020, 139, 357–369. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ong, C.T.; Adusumalli, S. Increased intron retention is linked to Alzheimer’s disease. Neural Regen. Res. 2020, 15, 259–260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Valadkhan, S.; Mohammadi, A.; Wachtel, C.; Manley, J.L. Protein-free spliceosomal snRNAs catalyze a reaction that resembles the first step of splicing. RNA 2007, 13, 2300–2311. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Valadkhan, S.; Manley, J.L. Splicing-related catalysis by protein-free snRNAS. Nature 2001, 413, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Valadkhan, S.; Mohammadi, A.; Jaladat, Y.; Geisler, S. Protein-free small nuclear RNAs catalyze a two-step splicing reaction. Proc. Natl. Acad. Sci. USA 2009, 106, 11901–11906. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.F.; Li, Y.X.; Wang, J.Z.; Zhao, Y.T.; Wang, Y. Controlling CRISPR-Cas9 by guide RNA engineering. Wiley Interdiscip. Rev. RNA 2023, 14, e1731. [Google Scholar] [CrossRef] [PubMed]
- Sznajder, L.J.; Thomas, J.D.; Carrell, E.M.; Reid, T.; McFarland, K.N.; Cleary, J.D.; Oliveira, R.; Nutter, C.A.; Bhatt, K.; Sobczak, K.; et al. Intron retention induced by microsatellite expansions as a disease biomarker. Proc. Natl. Acad. Sci. USA 2018, 115, 4234–4239. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vanichkina, D.P.; Schmitz, U.; Wong, J.J.; Rasko, J.E.J. Challenges in defining the role of intron retention in normal biology and disease. Semin. Cell Dev. Biol. 2018, 75, 40–49. [Google Scholar] [CrossRef] [PubMed]
| Gene | Location | Function | Retained Intron | Detection Techniques | Reference |
|---|---|---|---|---|---|
| Slc16a3 | In humans, chromosome 17. | Encodes the Monocarboxylate transporter 4(MCT4). | Intron 2/3 in human melanoma samples (443 bp). | RT-sqPCR. | Giannopoulou et al., Int. J. Mol. Sci. 2019, 20(4), 937 [34] |
| In mice, chromosome 11. | Encodes the MCT4. | Intron 2. | RT-sqPCR. | El-Seedy et al., Genes (Basel). 2023 17,14(10):1949 [35] | |
| MAPT | In humans, chromosome 17. | Encodes the protein Tau. | Intron 3, intron 12 or both in human brain samples. | qRT-PCR. | Ruiz-Gabarre et al., EBioMedicine 2024, [36] Feb,100:104953. doi: 10.1016/j.ebiom.2023.104953. |
| APOE | In humans, chromosome 19. | Encodes the apolipoprotein E protein. | Intron 3. | qRT-PCR | Dieter & Estus, Mol. Neurodegeneration 2010, 5, 34 [37]. |
| PSEN2 | In humans, chromosome 1. | Encodes the presenilin-2 protein. | 77 bp intron retention product before exon 6. | Long-read sequencing technology. | Course et al., Brain. 2023 13,146(2), 507–518. doi: 10.1093/brain/awac294. PMID: 35949106; [38] |
| FARP1 | In humans, chromosome 3. | Encodes FERM, Rho/ArhGEF, and Pleckstrin domain protein 1. | Different introns in human and mouse brain with Alzheimer’s disease. | Nanostring chip and RNA-seq data. | Li et al., Alzheimers Dement. 2021, 17(6):984–1004 [32] |
| GPX4 | In humans, chromosome 19. | Encodes for the glutathione peroxidase 4 enzyme. | In a hippocampal cell line, 213 bp sequence related to intron I1b situated between exons E1b and E2. | RT-qPCR. | Casañas-Sánchez et al., Front Physiol. 2015, 22;6:203 [39] |
| CLU | In humans, chromosome 8. | Encodes the protein clusterin. | The rs7982 variant is situated in the 5th exon of CLU gene, which splits this exon into two sections by a brief intron. | RNA sequencing (RNA-Seq) based on brain tissue and whole genome sequencing (WGS). | Han et al., Int J Mol Sci. 2020 25;21(19):7079 [40] |
| Harold et al., Nat. Genet. 2009, 41:1088–1093 [41] | |||||
| HDAC4 | In humans, chromosome 2. | Encodes the Histone deacetylase 4, protein. | Varied introns in the prefrontal cortex (PFC) of young and older humans. | Mammalian RNA-seq datasets. | Adusumalli et al., Aging Cell. 2019, 18(3):e12928 [5] |
| APP | In humans, chromosome 21. | Encodes the amyloid precursor protein. | Introns 6, 7, and 8. | Brain tissue of hAPP transgenic and nontransgenic mice and of humans with and without AD. | Rockenstein et al., Journal of Biological Chemistry. 1995, 270, 47 (24), 28257–28267 [42] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Seedy, A.; Ladevèze, V. Intron Retention and Alzheimer’s Disease (AD): A Review of Regulation Genes Implicated in AD. Genes 2025, 16, 782. https://doi.org/10.3390/genes16070782
El-Seedy A, Ladevèze V. Intron Retention and Alzheimer’s Disease (AD): A Review of Regulation Genes Implicated in AD. Genes. 2025; 16(7):782. https://doi.org/10.3390/genes16070782
Chicago/Turabian StyleEl-Seedy, Ayman, and Véronique Ladevèze. 2025. "Intron Retention and Alzheimer’s Disease (AD): A Review of Regulation Genes Implicated in AD" Genes 16, no. 7: 782. https://doi.org/10.3390/genes16070782
APA StyleEl-Seedy, A., & Ladevèze, V. (2025). Intron Retention and Alzheimer’s Disease (AD): A Review of Regulation Genes Implicated in AD. Genes, 16(7), 782. https://doi.org/10.3390/genes16070782






