Abstract
Osteosarcoma prognosis has remained unchanged for the past three decades. In both humans and canines, treatment is limited to excision, radiation, and chemotherapy. Chemoresistance is the primary cause of treatment failure, and the trajectory of tumor evolution while under selective pressure from treatment is thought to be the major contributing factor in both species. We sought to understand the nature of platinum-based chemotherapy resistance by investigating cells that were subjected to repeated treatment and recovery cycles with increased carboplatin concentrations. Three HMPOS-derived cell lines, two resistant and one naïve, underwent single-cell RNA sequencing to examine transcriptomic perturbation and identify pathways leading to resistance and phenotypic changes. We identified the mechanisms of acquired chemoresistance and inferred the induced cellular trajectory that evolved with repeated exposure. The gene expression patterns indicated that acquired chemoresistance was strongly associated with a process similar to epithelial–mesenchymal transition (EMT), a phenomenon associated with the acquisition of migratory and invasive properties associated with metastatic disease. We conclude that the observed trajectory of tumor adaptability is directly correlated with chemoresistance and the phase of the EMT-like phenotype is directly affected by the level of chemoresistance. We infer that the EMT-like phenotype is a critical component of tumor evolution under treatment pressure and is vital to understanding the mechanisms of chemoresistance and to improving osteosarcoma prognosis.
1. Introduction
Osteosarcoma (OSA) treatment and prognosis have remained unchanged over the past thirty years [1]. It continues to be the most common human primary bone malignancy and comprises under 1% of adult cancers and 3–5% of pediatric cancers [2]. The current standard of care, first implemented in the 1980s, entails surgical excision, radiation, and an aggressive chemotherapy regimen [1,3]. This offers a ten-year survival rate of 60% for patients with nonmetastatic disease and 30% for patients with metastatic disease [1,3].
Canine OSA is a naturally occurring cancer and the predominant bone malignancy that affects dogs. Most dogs impacted by OSA are large or/giant breeds that experience increased cell proliferation and rapid growth in the long bones of the appendicular skeleton [4]. In addition, the rate of incidence is 10-fold greater in dogs than that in humans, and a canine’s shorter lifespan allows for more rapid data collection [4]. The canine model is particularly relevant due to mutations in the TP53, RB1, MTAP/CDKN2A, and MDM2 genes that are commonly associated with human and canine OSA [5,6,7]. However, with the exception of TP53, the specific mutations within these shared genes that infrequently occur in both species and mutations in SETD2 and DMD are unique to canine OSA [6,8,9,10].
The primary cause of OSA treatment failure is chemoresistance, which has been attributed to tumor adaptability and the trajectory of tumor cell evolution [11,12]. Tumor adaptability is driven by the key hallmarks of tumorigenesis, genomic instability, and compromised regulation of DNA replication and the cell cycle [11]. Genomic instability results in high levels of copy number variation and genotypic, transcriptomic, and phenotypic heterogeneity within cancerous tissues that can promote adaptive mechanisms for resistance to chemotherapy drugs and the production of highly resistant cancer cells [11,12]. In addition, chemotherapy-induced mutations may drive the tumor’s trajectory by selecting for drug-resistant cell populations [11,12,13].
The gold-standard chemotherapies for OSA in both humans and canines are platinum-based drugs [14]. The mechanisms of resistance are similar among platinum chemotherapeutic agents and include reduced drug accumulation, inactivation by glutathione (GSH) and metallothionein (MT), increased DNA repair, and suppression of apoptosis [13,14,15,16].
A preliminary study characterized the proteomes of canine osteosarcoma HMPOS-derived carboplatin-resistant cell lines and their exosomes, and evaluated exosome-mediated chemotherapy resistance [17]. There were differences between each cell line in the response to chemotherapeutics and in the proteins expressed [17]. Proteomic analysis indicated an association of chemotherapy resistance with the glutathione biosynthesis, conjugation, and recycling pathways, and the γ-glutamyl biosynthesis pathway [17]. These pathways minimize the effectiveness of chemotherapeutic drugs by promoting glutathione S transferase (GST) enzyme activation, which hydrolyzes the platinum agents’ active group [17,18]. Carboplatin-resistant cell lines, particularly HMPOS-10R, have high expression of β-catenin, an oncogene [17]. β-catenin plays a key role in the Wnt/β-catenin signaling pathway and promotes chemoresistance through upregulating MDR1 and inducing epithelial–mesenchymal transition (EMT) [19]. Exposure to HMPOS-2.5R exosomes was found to induce chemotherapy resistance in naïve HMPOS-S cells, while exposure to HMPOS-10R exosomes only induced β-catenin expression in naïve HMPOS-S cells [17]. The results of this study indicated the complexity of chemotherapy resistance induction and conveyance, which we will continue to investigate by evaluating the transcriptomes of these cell lines [17].
We hypothesized that OSA cancer cells develop their drug resistance by adapting to the evolutionary selective pressure resulting from increased chemotherapy concentration, either along a singular or a diversified path. The goal of this study was to examine the evolutionary trajectory, assess the results of adaptation due to selective pressure, and determine the nature of resistance mechanisms in previously induced OSA carboplatin-resistant cell lines. This in vitro approach mitigates the cellular complexity of the bone marrow niche to address the diverse tumor microenvironment, which aids in tracking the evolutionary progress of each cell population as they acquire carboplatin resistance [20].
2. Materials and Methods
2.1. Carboplatin Chemoresistant Cell Lines
For our experiment, we used a highly aggressive and malignant cell line, Highly Metastasizing POS (HMPOS). The HMPOS cells were a kind donation from the Barroga and Fujina Lab [21]. This cell line was previously derived from the canine OSA cell line POS, which was generated by harvesting cells from canine metastatic lesions passaged in mice. Cells were incubated at 37 °C with 5% CO2 in growth media (RPMI 1640 and 10% FBS supplemented with 100 units/mL penicillin and 100 μg/mL streptomycin) [21]. All cells were tested for mycoplasma prior to incubation. The cells used for this study were passaged fewer than five times before arriving in our lab. Expansion in-house entailed fewer than 3 passages prior to introducing carboplatin. Carboplatin resistance was induced at 0, 2.5 μM, and 10 μM dosages in a previous study, and clones were validated to be resistant and were used in this study (Figure 1) [21]. The HMPOS 0, 2.5 μM, and 10 μM-carboplatin-resistant cells will be referred to as HMPOS, HMPOS-2.5, and HMPOS-10, respectively.
2.2. Carboplatin Sensitivity Assay
HMPOS, HMPOS-2.5, and HMPOS-10 cell lines were grown in T-25 tissue culture flasks containing RPMI 1640 cell culture media with 10% fetal bovine serum. The flasks were incubated at 37 °C with 5% CO2 until 50% confluent. The tissue culture flasks were washed with 1× PBS and replenished with serum-free RPMI 1640 cell culture media. The cells were incubated at 37 °C and serum-starved for 24 h. After incubation, tissue culture flasks were washed with 1× PBS, and varying concentrations of carboplatin diluted in cell culture media were added to the flasks. All three cell lines were treated with carboplatin doses ranging from 0–480 µM. Conditions were set up in triplicate and cells containing drug-free RMPI 1640 with 10% fetal bovine serum were used as a negative control. All flasks were incubated for 72 h at 37 °C. After incubation, the cells were trypsinized, harvested, and centrifuged at 500× g for 5 min. The supernatant was decanted and the remaining cell pellet was resuspended in 100 µL of 1× PBS. The cell suspension was mixed 1:1 with ViaStain AOPI Staining Solution (Nexcelom Biosciences, Lawrence, MA, USA) and cell viability was determined using a Cellometer Auto 2000 (Nexcelom Biosciences, Figure S1). Three technical replicates of three biological replicates were performed. IC50 values were determined using non-linear regression and curve fit analysis. To determine the difference between curves, pairwise extra sum-of-squares F tests were performed, with the null hypothesis as IC50 being the same and the alternative hypothesis as IC50 being different. We also tested this as IC50 being different in at least one of the three replicates. For all tests, p < 0.001.
2.3. Cell Invasion and Migration Assay
The coating buffer was produced from 0.7% NaCl and 0.1 M tris in distilled water and filtered using a 0.2 µm sterile syringe filter. The Matrigel Matrix (Corning, Tewksbury, MA, USA) was diluted using chilled coating buffer to a final concentration of 250 µg/mL. Thincerts were placed in a 24-well plate (Greiner Bio-one, Kremsmünster, Austria) and coated with 100 µL of Matrigel Matrix. The plates were placed in an incubator at 37 °C for 2 h. A cell suspension was prepared using serum-free cell culture media at a concentration of 1 × 106 cells/mL. An amount of 600 uL of cell culture media containing serum was pipetted into the bottom of each test well and a coated Thincert was placed on top of the media; 200 µL of the cell suspension was pipetted into each Thincert and the plates were returned to the incubator. Positive control wells to measure migration were set up in the same manner as the test wells, but included uncoated Thincerts. Negative control wells contained uncoated Thincerts to measure invasion, but only contained serum-free media. All conditions were run in triplicate. Plates were removed after 20 h and the Thincerts were gently removed and placed in a new 24-well plate containing serum-free media and 8 µM Calcein-AM. The plates were incubated for 45 min at 37 °C. After incubation, the cell suspension was removed from the inside of the Thincert, and the Thincerts were placed in a new 24-well plate containing 500 µL of pre-warmed trypsin–EDTA. The plates were incubated for 15 min at 37 °C with occasional tapping to encourage detachment. After 15 min, the thincerts were discarded and the trypsinized cells were mixed via a pipette. A total of 200 µL of the trypsinized cells was pipetted into a 96-well plate in triplicate and the plates were read by a fluorescent plate reader (excitation 485 nm/emission 520 nm) (BioTek Synergy 2, Winooski, VT, USA). The invasion index percentage was calculated using the following formula: Invasion index % = (experimental average–negative control average)/(positive control average–negative control average) × 100%. The migration index was calculated using the following formula: Migration index% = (positive control average − negative control average)/200,000 (total number of cells that were originally plated). Analysis was performed using ANOVA single-factor analysis to evaluate the p values for the invasion and migration assays, and Tukey’s HSD test was performed for the invasion assay data (Table S1).
2.4. Single Cell RNA Sequencing
Cell suspensions were prepared using Next Gel Bead-in-Emulsion (GEM) technology using the Chromium Controller (10× Genomics). The Chromium Single Cell 3′ Library, Gel Bead & Multiplex Kit v3 (10× Genomics) was used to construct the scRNA-seq libraries following the manufacturer’s protocols. Sequencing libraries were constructed using the Nextera XT DNA sample Pre-Kit (Illumina, San Diego, CA, USA). The final libraries were analyzed using the Agilent Bioanalyzer by running a High Sensitivity DNA Kit (Agilent Technologies, Santa Clara, CA, USA). The pooling of individual libraries was performed using 75-cycle run kits on an Illumina HiSeq X platform with 150 bp paired-end reads. The Texas A&M Institute for Genome Sciences and Society performed the scRNA sequencing (Figure 1).
2.5. Analysis and Visualization
All following computational methods were performed on a private 96-core server running Scientific Linux v7. Raw base call files (BCL) were demultiplexed using the cellranger mkfastq command to generate FASTQ files [22]. These FASTQ files were filtered and the cell barcodes and unique molecular identifiers (UMIs) were extracted using Cell Ranger v6.0 and then aligned to the canFam4 reference [23]. The “count” command then was used to group reads with the same cell barcodes, UMIs, and genes to calculate the number of UMIs per gene per cell. The Seurat package (version 4.0.0) was used to process the raw output data in R Studio software (version 3.3) for each individual tissue sampled [24,25]. Cells were filtered for bioinformatic analysis by parameters to exclude cells with the percentage of mitochondrial genes expressed over 5% and those that fell outside of the 250–2500 number of genes. The filtered cells underwent cell cycle regression to minimize cell cycle heterogeneity effects. The filtered cells were then scaled and underwent principal component analysis (PCA), nearest neighbors were computed, and clusters were found using a resolution of 0.5. The data were dimensionally reduced using both t-distributed Stochastic Neighbor Embedding (tSNE) and Uniform Manifold Approximation and Projection (UMAP). Differential expression was determined using the R package Seurat between each cell line, and genes with a p-value less than 2 × 105 were further evaluated in gene enrichment and network analyses. Pseudotime analysis was conducted using Monocle and Slingshot [24,26,27].
Each cell line was mostly homogenous, but scRNAseq was performed in order to capture small heterogeneous populations that illustrated the evolutionary trajectory that bulk RNA sequencing would not be able to detect. Differential expression testing was performed by pairwise comparison of each cell line (Tables S2–S4), between each line and all other cells (Tables S5–S7), between the three Seurat clusters within HMPOS-10 (Tables S8–S10), and between clusters 8, 10, and 11 with their respective primary cell line clusters HMPOS, HMPOS-10, and HMPOS-10, respectively (Tables S11–S13). Gene set enrichment analysis was performed on the upregulated and downregulated gene lists, comparing HMPOS with HMPOS-2.5, HMPOS with HMPOS-10, and HMPOS-2.5 with HMPOS-10 in gProfiler [28]. Network and pathway analyses were performed on all differential expression comparisons with the core analysis algorithm in Ingenuity Pathway Analysis (IPA) to compare the log fold-change (LogFC) variation for significant genes and the Bonferroni-corrected p-values within each gene list [29]. A visual overview of this experiment illustrates the pipeline from cell culture to sequence data to cell analysis (Figure 1).
Figure 1.
Visual overview of experimental design. HMPOS cell lines were previously challenged with increased concentrations of carboplatin to generate the HMPOS-2.5 μM and HMPOS-10 μM drug-resistant cell lines [23]. Single-cell RNA sequencing was performed on these two chemoresistant cell lines and the HMPOS cells. Created with BioRender.com, (accessed on 22 October, 2022) [30].
3. Results
3.1. Characterization Confirmation of the HMPOS Cell Lines
The resistance of HMPOS, HMPOS-2.5, and HMPOS-10 confirmed the results of previous carboplatin sensitivity assay characterization (Figure 2A) [17]. The HMPOS-10 cell line exhibited the highest resistance to carboplatin, followed by the HMPOS-2.5 cell line, and the HMPOS cell line was found to be the least resistant (Figure 2A). The IC50-values calculated for HMPOS, HMPOS-2.5, and HMPOS-10 were 88.10 μM, 151.99 μM, and 248.85 μM, respectively. There was no statistical difference between each group using the extra sum-of-squares F test with p-values of 0.653, 0.368, and 0.377 for HMPOS and HMPOS 2.5, HMPOS and HMPOS-10, and HMPOS-2.5 and HMPOS-10, respectively.
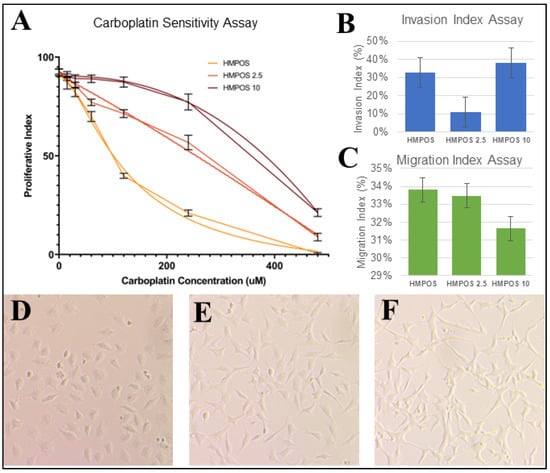
Figure 2.
(A) Proliferative index for each HMPOS cell line at carboplatin dosages of 0 μM, 15 μM, 30 μM, 60 μM, 120 μM, 240 μM, and 480 μM. Three technical replicates of three biological replicates are shown. Nonlinear regression curve for resistance to carboplatin is significant according to the extra sum-of-squares F (p < 0.001). (B) Average % of Invasion Index Assay; the p-value was significant and found to be 0.00013753 using an ANOVA single-factor test. However, the Tukey’s HSD p-values between HMPOS and HMPOS-2.5 and between HMPOS-2.5 and HMPOS-10 were 0.001 and 0.001 respectively, while it was 0.379 between HMPOS and HMPOS-10. (C) Average % of Migration Index Assay; the p-value was not significant and found to be 0.06012698 using an ANOVA single-factor test. Light microscopy photos of (D) HMPOS, (E) HMPOS-2.5, and (F) HMPOS-10 showing distinct phenotypic differences, from cuboidal to spindle morphology.
Cell morphology was visually different between the HMPOS cells, which exhibited a more cuboidal shape than the HMPOS-2.5 and 10 cells, which were comprised of a spindled morphology with a more severe shape in HMPOS-10 (Figure 2D–F). The Invasion Index Assay was statistically significant according to ANOVA analysis, but Tukey’s range test showed no statistical significance between samples, except for HMPOS-2.5 (Figure 2B). The Invasion Index assay indicated that HMPOS-10 was more invasive than HMPOS, but HMPOS-2.5 had the lowest invasion index scores of the three cell lines (Figure 2B). There was no statistically significant difference in the rate of migration between all three cell lines (Figure 2C).
3.2. Distinction in Transcriptomes between Chemoresistance Levels
Post-filtration, there were 12,644, 10,883, and 8668 cells for HMPOS, HMPOS-2.5, and HMPOS-10 respectively. The distribution across cell phases for each cell type was similar, with the exception of a lower proportion of cells in G1 in HMPOS-10 (Figure S2). Each cell line clustered distinctly using Principal Component Analysis (PCA) and Uniform Manifold Approximation and Projection (UMAP), resulting in fourteen subclone groups (Figure 3A). The inferred pseudotime values showed a trajectory in evolution from HMPOS to HMPOS-2.5, then HMPOS-10 (Figure 3C and Figure S3). A clear distinction between these three cell lines due to the differential expression was evident. In total, 688 genes were upregulated and 400 genes were downregulated in the HMPOS line in comparison with the HMPOS-2.5 cells; 1147 genes were upregulated and 1164 genes were downregulated in the HMPOS cells compared with the HMPOS-10 cells; and 976 genes were upregulated and 1465 genes were downregulated in the HMPOS-2.5 cells compared with the HMPOS-10 cells.
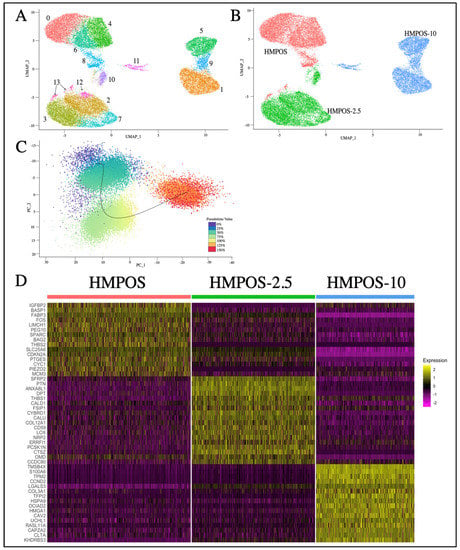
Figure 3.
(A) UMAP plot of HMPOS, HMPOS 2.5, and HMPOS 10 showing the cell lines. (B) UMAP of the Seurat clusters in which HMPOS makes up clusters 0, 4, 6, 8, and 13, while HMPOS-2.5 forms clusters 2, 3, 7, 10, and 12, and clusters 1, 5, 9, and 11 are made up of HMPOS-10 cells. (C) PCA jitter plot highlighting the different cell stages and inferred trajectory. (D) Heatmap showing the highest differentially expressed genes for each cell line. This list was put together by selecting the top 20 genes for each cell line based on avg_log2FC, which is the log fold-change in the difference in expression between groups where positive values indicate that the expression of a gene is greater in the first group. Eight genes with no gene symbol listed were dropped.
3.3. Differential Gene Expression in Chemoresistant Cell Lines
Genes that were differentially upregulated in HMPOS compared with the induced carboplatin-resistant cell lines were found to be related to biological pathways that involved biosynthesis, metabolism, and proliferation (Figure 4A). The biological pathways upregulated in HMPOS-2.5 cells from HMPOS were in response to chemicals and morphogenesis. Catalytic activity and protein binding were the upregulated biological pathways in HMPOS-2.5 compared with HMPOS-10 cells. Protein, enzyme, and transcription factor binding were upregulated in HMPOS-10 cells compared with the naïve and HMPOS-2.5 cell lines. Further analysis of pathway differentiation using IPA implicated the EIF2 signaling pathway, the sirtuin signaling pathway, and the mTOR signaling pathway. The EIF2 signaling pathway was activated in HMPOS-2.5 compared with HMPOS, while the sirtuin and mTOR pathways were downregulated in HMPOS-2.5 compared with HMPOS (Figure 5B). In HMPOS-10, the EIF2 signaling pathway was also activated, and the mTOR pathway was downregulated when compared with HMPOS and HMPOS-2.5 (Figure 5C). In contrast, the sirtuin pathway was activated in HMPOS-10 (Figure 5C). TMSB4X, LGALS3, COL3A1, and HMGA1 increased and THBS2, BAG2, BASP1, PEG10, and NPR3 decreased in correlation with the increase in the carboplatin dosage (Figure S4). The HMPOS-10 cell line was particularly distinct and exhibited high expression of S100A6, TPM2, CCND2, TFPI2, HMGA2, and GSTT2B (Figure S5). CDKN2A, TMEM126A, TMEM126B, MTAP, COX7A1, and LTBR were downregulated in the HMPOS-10 cell line (Figure S5). For the HMPOS-2.5 cell line, PIEZO2, IGFBP2, and ACVR2A were distinctly downregulated and THBS1, SFRP2, PTN, FSIP1, DPT, OMD, OGN, COL5A2, and ENO1 were distinctly upregulated (Figure S6). Network and pathway analyses comparing HMPOS with HMPOS-2.5, HMPOS with HMPOS-10, and HMPOS-2.5 with HMPOS-10 are presented in Figures S7–S9 respectively.
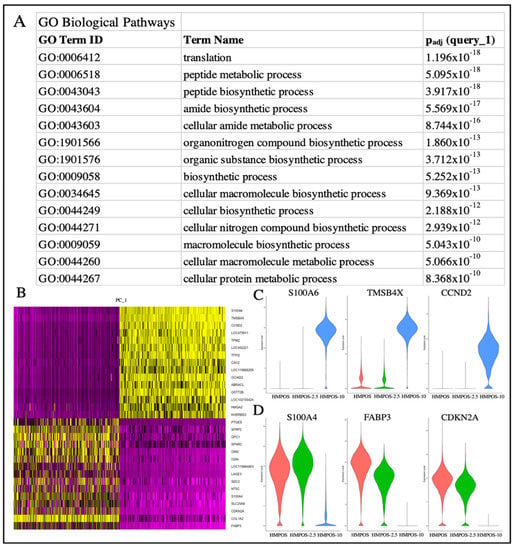
Figure 4.
(A) gProfiler analysis of the biological pathways related to the upregulated genes of the HMPOS cell line in comparison with the 2.5 and HMPOS-10 cell lines. (B) DimHeatmap showing the primary sources of heterogeneity. (C) Violin plot of genes from PC_1, i.e., the most highly differentially expressed genes that coordinate with the HMPOS-10 cell line. (D) Violin plot of genes from PC_1, i.e., the most highly differentially expressed genes that coordinate with the HMPOS-2.5 and HMPOS cell lines.
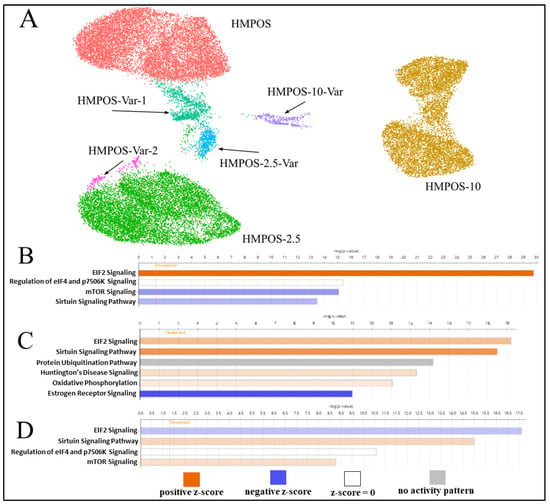
Figure 5.
(A) UMAP plot of HMPOS, HMPOS-2.5, and HMPOS-10 and the subclonal populations that were distinct from the main cell lines. HMPOS-Var-1 and HMPOS-Var-2 are variants of HMPOS, though the low cell count of 249 cells of HMPOS-Var-2 led to its exclusion from further analysis. HMPOS-2.5-Var is a variant of HMPOS-2.5 and HMPOS-10-Var is a variant of HMPOS-10. (B) Pathway analysis comparing HMPOS and HMPOS-2.5, with positive z-scores in orange indicating pathway activation and blue indicating pathway inhibition in HMPOS-2.5 compared with HMPOS. The color’s intensity represents the z score’s distance from the mean, with darker color indicating greater distance. (C) IPA comparing HMPOS-10 with HMPOS and HMPOS-2.5. (D) IPA comparing HMPOS-10 cells in clusters 1 and 5, which can be seen in Figure 3B.
3.4. Subclonal Cell Populations
For each cell line, there was a cluster distinct from the main cell population, only detectable using the single cell approach. Cluster 8 and cluster 13 were secondary clusters for HMPOS and were labeled as HMPOS-Var-1 and HMPOS-Var-2, respectively. HMPOS-Var-2 was not investigated further as it consisted of only 249 cells (Figure S10). Cluster 10 was a secondary cluster for HMPOS-2.5 and was labeled HMPOS-2.5-Var (Figure S11). Cluster 11 was a secondary cluster for HMPOS-10 and was labeled HMPOS-10-Var (Figure S12). Additionally, clusters 1 and 5 within the HMPOS-10 group were compared due to their divergent expression patterns. A comparison of HMPOS with HMPOS-Var-1 revealed the downregulation of THBS1 and LGALS3. In HMPOS-2.5-Var, FSIP1 and OMD were upregulated in comparison with HMPOS-2.5. SFRP2 and COL12A1 were downregulated and FSIP1 was upregulated in HMPOS-10-Var in comparison with HMPOS-10. Clusters 1, 5, and 9 within the main HMPOS-10 cell population were also compared using IPA and revealed the inhibition of the EIF2 signaling pathway and promotion of the sirtuin signaling pathway and the mTOR signaling pathway (Figure 5D and Figure S13).
4. Discussion
One of the main causes of treatment failure in OSA and many other cancers is chemotherapy drug resistance [11,12]. Tumor adaptability and the trajectory of cancer cell evolution play a major role in treatment evasion and the development of evasion mechanisms. It is essential to understand the trajectory of tumor adaptation in order to tailor treatment strategies to fit the genetic profile of patients in order to improve prognosis.
The cell viability assay confirmed the induction of carboplatin drug resistance, with HMPOS being the most sensitive, HMPOS-2.5 having improved survival, and HMPOS-10 exhibiting the highest resistance to carboplatin exposure. The observed morphology changed from cuboidal to spindled, correlating with the morphological changes seen in the epithelial-to-mesenchymal transition (EMT), where spindled tumor cells are more aggressive and chemoresistant [30]. The invasion and migration assays, which assessed the metastatic potential of cells via movement, were not significant between the three conditions. This was expected, as the metastatic nature of HMPOS was well established, and was not likely to change given exposure to carboplatin. However, the gene expression patterns between HMPOS, HMPOS-2.5, and HMPOS-10 were distinct from one another, with HMPOS-10 being the most phenotypically and transcriptionally divergent.
4.1. Epithelial-to-Mesenchymal Transition in Correlation with Chemotherapy Resistance
The resistance to carboplatin and change to a spindled morphology from HMPOS to HMPOS-2.5 to HMPOS-10 may indicate the induction of EMT or an EMT-like process as a result of adaptive resistance. Several lines of evidence for the resistant cell lines in this work demonstrate an evolutionary progression toward this transition. As chemoresistance increased, TMSB4X, LGALS3, COL3A1, and HMGA1 were consistently upregulated, while THBS2, BASP1, NPR3, BAG2, and PEG10 were downregulated.
The upregulation of TMSB4X (thymosin-β4 X-linked), LGALS3 (galectin 3), COL3A1 (collagen type III α 1), and HMGA1 (high-mobility group AT-hook 1) is associated with chemoresistance and poor prognosis [31,32,33,34,35,36,37,38,39,40]. thymosin-β4 is an actin-binding protein and plays a major role in the development of tissue and wound repair [32,33]. The upregulation of TMSB4X is correlated with tumor progression and induces the activation of myocardin-related transcription factors (MRTF) that regulate EMT transition and downregulate E-cadherin [31,32,33]. LGALS3 plays a role in apoptosis and cell adhesion, and stimulates bone marrow mesenchymal stem cells to express interleukin-6 (IL-6) to promote tumorigenesis, inflammation of the tumor microenvironment, and metastasis [34,35,36,37,38]. TMSB4X suppresses and LGALS3 interacts with E-cadherin, a tumor-suppressor protein that maintains cell adhesion and epithelial structural integrity, and is a key gene that is downregulated to allow EMT transition [31,35]. Collagen type III α 1 is a component of the extracellular matrix [39,40]. COL3A1 is a marker for EMT and is shown to be associated with POSTN (periostin), which activates the ERK and p38 pathways and downregulates miR-381 expression to regulate EMT [39,40]. HMGA1 is an architectural transcription factor, and its overexpression activates Akt signaling to promote survival and proliferation [41,42,43]. The HMGA1–TRIP13 axis has been shown to induce EMT when HMGA1 is overexpressed [44].
THBS2 (thrombospondin 2), BASP1 (brain acid soluble protein 1), and NPR3 (natriuretic peptide receptor 3) are tumor-suppressor genes, for which downregulation is associated with poor prognosis [45,46,47,48,49]. Deficiency of THBS2 is associated with the degradation of collagen and the extracellular matrix to allow metastasis [45]. Upregulated miR-191 expression promotes EMT and activates the Wnt pathway for tumor promotion through the inhibition of BASP1 [47,48]. POU2F1 regulates NPR3 expression to block the PI3K/Akt pathway to inhibit OSA cell proliferation and EMT [49].
BAG2 (BAG cochaperone 2) plays a role in the Akt/mTOR and ERK pathways to promote tumorigenesis [50,51,52]. PEG10 (paternally expressed gene 10) promotes tumor invasion and metastasis, and is a major regulator in TGFB1-induced EMT [53,54,55]. The increased chemoresistance, the cell morphology change, and the gene expression suggest that the gain of chemoresistance is associated with the transition from epithelial to mesenchymal. The downregulation of BAG2 and PEG10 with the increase in chemoresistance may indicate the effectiveness of other mechanisms in promoting tumorigenesis and resistance.
4.2. Epithelial-to-Mesenchymal Transition in HMPOS-10
HMPOS-10 exhibited high expression of genes associated with tumorigenesis and directly correlated with chemotherapy resistance, including S100A6, TPM2, CCND2, TFPI2, HMGA2, and GSTT2B. S100A6 (calcium-binding protein A6) is upregulated in breast cancer through mesenchymal stem cell-secreted exosomes to promote chemotherapy resistance [56,57]. S100A6 is involved in the Wnt/β-catenin signaling pathway and induces EMT by downregulating E-cadherin [56,57]. TPM2 (tropomyosin 2) is mainly expressed in muscle fibers and, when upregulated, decreases E-cadherin and β-catenin expression [58,59]. CCND2 (cyclin D2) is a driver of cell cycle progression and can be suppressed by miR-646 to prevent tumorigenesis and EMT [60,61,62]. TFPI2 (tissue factor pathway inhibitor-2) is a tumor-suppressor gene that induces apoptosis, but hypermethylated TFPI2 is associated with several human cancers and dysregulated TFPI2 overexpression promotes EMT through the TGF-β pathway [63,64]. HMGA2 (high-motility group AT-hook 2) overexpression activates the Dvl2/Wnt pathway to increase chemoresistance and promote EMT through the MAPK pathway [65,66]. GSTT2B (glutathione S-transferase theta 2) is a pseudogene of GSTT2, and glutathione S-transferases are associated with chemotherapy, such as platinum agents and detoxification [67].
The genes downregulated in HMPOS-10 were CDKN2A, TMEM126A, TMEM126B, MTAP, COX7A1, and LTBR. CDKN2A (cyclin-dependent kinase inhibitor 2A) is an inhibitor of cellular proliferation through the Akt/mTOR pathway, and loss-of-function correlates with chemotherapy resistance [68,69]. TMEM126A and TMEM126B (transmembrane protein 126A and transmembrane protein 126B, respectively) downregulation promotes mitochondrial and extracellular matrix dysregulation, attributed to poor prognosis, EMT, and chemoresistance [70]. EMT is also promoted by the purine metabolic enzyme MTAP (methylthioadenosine phosphorylase), which is downregulated in lung adenocarcinoma and predicts prognosis [71,72]. Knockout of MTAP was found to downregulate E-cadherin and p-GSK3β and lead to EMT progression [73]. COX7A1 (cytochrome c oxidase subunit 7A1) is involved in the mitochondrial respiratory chain and its overexpression inhibits cell proliferation and promotes apoptosis [74]. LTBR (lymphotoxin β receptor) mediates apoptosis in tumor cells and activates tumorigenesis by promoting the NF-Kβ pathway [75,76].
Analysis of HMPOS-10 showed that there were many different genes at play targeting various pathways, including the Wnt/β-catenin, TGF-β, Dvl2/Wnt, MAPK, Akt/mTOR, and NF-Kβ pathways, which are related to tumorigenesis and the induction of an EMT-like phenotype. The mechanisms of chemotherapy resistance linked to EMT include improved proliferation and maintenance, resistance to apoptosis, the overexpression of ABC transporters that remove chemotherapeutics, and the induction of a hypoxic tumor microenvironment.
4.3. Epithelial-to-Mesenchymal Transition in HMPOS-2.5
HMPOS-2.5 exhibited upregulation of THBS1, SFRP2, PTN, FSIP1, DPT, OMD, OGN, COL5A2, and ENO1 and downregulation of PIEZO2, IGFBP2, and ACVR2A. THBS1 (thrombospondin 1) upregulation activates the TGF-β pathway to promote tumorigenesis and EMT [77,78]. SFRP2 (secreted frizzled-related protein 2) modulates the Wnt/β-catenin pathway and controls WNT16B to promote acquired resistance [79,80]. In vitro and in vivo studies show that the downregulation of SFRP2 expression can reverse the EMT process [81]. PTN (pleiotrophin) is a growth factor involved in proliferation and in osteosarcoma; its overexpression promotes EMT and doxorubicin resistance [82,83,84]. The upregulation of FSIP1 (fibrous sheath interacting protein 1) correlates with poor prognosis in breast cancer and FSIP1 knockout in a mouse model has been found to improve docetaxel sensitivity [85]. DPT (dermatopontin) promotes cellular adhesion and enhances TGFB1 during the process of wound repair [86,87]. OMD (osteomodulin) is involved in osteoblast differentiation and OGN (osteoglycin) regulates bone and glucose homeostasis and has been indicated as a tumor suppressor [88,89]. In colorectal cancer, OGN upregulation has been found to induce EGFR endocytosis and inhibit EMT through the EGFR/Akt pathway [90]. EMT is accelerated and metastasis is promoted by the upregulation of COL5A2 (collagen type V α 2 chain), while its downregulation inhibits the TGF-β and Wnt/β-catenin signaling pathways in OSA [91,92]. ENO1 (enolase 1) is a glycolytic enzyme that suppresses ERK1/2 phosphorylation to inhibit EMT in vivo [93,94,95].
PIEZO2, IGFBP2, and ACVR2A upregulation is associated with the promotion of EMT [96,97,98,99,100,101]. PIEZO2 (piezo-type mechanosensitive ion channel component 2) regulates the actin cytoskeleton, and actin remodeling can alter drug response [96,97]. IGFBP2 (insulin-like growth factor-binding protein 2) promotes cellular proliferation, and its upregulation correlates with chemotherapy resistance [98,99,100]. ACVR2A (activin A receptor type 2A) mediates members of the TGF-β family and its loss-of-function results in an increase in tumorigenesis and metastasis [101].
The difference in gene expression between HMPOS-2.5 and HMPOS-10 may be due to HMPOS-2.5 being in an earlier state of EMT or an EMT-like process than HMPOS-10. There are fewer pathways associated with the gene expression patterns in HMPOS-2.5 compared with HMPOS-10. Many of the upregulated genes in HMPOS-2.5 are associated with EMT, but only implicate only the role of TGF-β, Wnt/β-catenin, and EGFR/Akt pathways. The downregulation of PIEZO2, IGFBP2, and ACVR2A may be due to HMPOS-2.5 being at an early stage of an EMT-like process or may reflect the effectiveness of other mechanisms of chemotherapy resistance.
4.4. Cell Populations Variating from the Main Cell Lines
There were small populations of cells from each identity that clustered separately from the main cell lines HMPOS, HMPOS-2.5, and HMPOS-10. These clusters were 8, 10, 11, and 13, which were renamed HMPOS-Var-1, HMPOS-2.5-Var, HMPOS-10-Var, and HMPOS-Var-2, respectively, to distinguish the cell lines that comprised these clusters. These clusters were compared with the main cell lines that they were split from, though HMPOS-Var-2 was excluded from further analysis because the cell count of 249 was too low to obtain meaningful results. Clusters 1 and 5 were also compared because of the distinction of these clusters within the HMPOS-10 cell line in comparison with the homogeneity of the HMPOS and HMPOS-2.5 cell lines.
LGALS3 and THBS1 were downregulated in HMPOS-Var-1 when compared with HMPOS. The upregulation of these two genes was shown to be correlated with chemotherapy resistance when comparing the expression of HMPOS, HMPOS-2.5, and HMPOS-10. LGALS3 and THBS1 are both associated with the promotion of tumorigenesis, metastasis, and EMT [34,35,36,77,78]. FSIP1 and OMD were upregulated in HMPOS-2.5-Var compared with HMPOS-2.5, which aligns with the pattern already seen for the upregulation of FSIP1 and OMD in HMPOS-2.5 in comparison with HMPOS. These two genes are related to docetaxel resistance and the regulation of osteoblast differentiation, respectively [85,88]. In HMPOS-10-Var, SFRP2 and COL12A1 were downregulated, while FSIP1 was upregulated in comparison with HMPOS-10. SFRP2 and another collagen, COL5A2, were previously seen to be upregulated in HMPOS-2.5 in comparison with HMPOS. SFRP2 controls the Wnt/β-catenin pathway and its upregulation promotes EMT, the upregulation of COL12A1 and other collagen genes is associated with chemotherapy resistance, and the upregulation of FSIP1 promotes chemotherapy resistance [79,80,81,85,102]. The existence of these small variant clusters from the large, homogenous main clusters for each cell line may have been the result of the divergence of each cell line as chemotherapy resistance evolved.
Clusters 1 and 5 within the main HMPOS-10 cluster were also compared using IPA and revealed the inhibition of the EIF2 signaling pathway alongside the promotion of the mTOR signaling pathway and the sirtuin signaling pathway (Figure 5D). EIF2 signaling pathway upregulation promotes tumorigenesis, metastasis, and tumor hypoxia, which results in chemotherapy resistance [103]. Oxygen is necessary for DNA damage to occur with radiation and activate chemotherapeutic agents [103]. The mTOR signaling pathway regulates cell proliferation and apoptosis, and its upregulation is associated with tumorigenesis and chemotherapy resistance [104]. DNA repair, apoptosis, and drug metastasis are controlled by the sirtuin signaling pathway and its upregulation is associated with tumorigenesis, metastasis, and drug resistance [105]. The differences in the promotion and inhibition of these pathways between these two clusters suggest that there are competing strategies for chemotherapy resistance. This is particularly because the pattern observed in cluster 5 of the downregulation of the EIF2 signaling pathway, the upregulation of the mTOR signaling pathway, and the increased upregulation of the sirtuin signaling pathway in contrast to cluster 1 was distinctively different to the pattern seen in HMPOS-2.5 compared with HMPOS.
4.5. Overlap in Proteomics and Transcriptomics
In our previous paper investigating the proteomics of these HMPOS-derived cell lines and their exosomes, there were several genes that were expressed in similar patterns to the transcriptomic work performed [17]. FSTL1 (follistatin-related protein 1) was upregulated in both HMPOS-2.5 and HMPOS-10 in the previous proteomic data and the scRNAseq results [17]. GLUL (glutamine synthetase) and ENO2 (γ-enolase) were only upregulated in HMPOS-10 in parallel to the proteomics results [17]. CDH2 (N-Cadherin) was upregulated in both HMPOS-2.5 and HMPOS-10 in the proteomics study, but only in the HMPOS-10 transcriptomics [17]. FSTL1 is a marker of EMT and invasion, GLUL plays a role in glutamine metabolism, ENO2 increases glycolysis, and CDH2 is a marker of EMT [17,106,107,108,109].
CTNNB1 (β-catenin) was seen to be upregulated in the previous proteomic analysis in HMPOS-10 and in the naïve HMPOS cell line when treated with exosomes derived from the chemoresistant cell lines [17]. These results and the difference in the expression of dephosphorylated and phosphorylated β-catenin between cell lines indicated the importance of CTNNB1 in chemotherapy resistance [17]. The scRNAseq results showed a downregulation of CTNNB1 in HMPOS-10 in comparison with HMPOS and HMPOS-2.5, which is not in line with the proteomic results [17]. As has been recurrently documented in proteome–transcriptome integration approaches, these data do not always align. The transient nature of the expressed genes tends to be more dynamic, and the proteome more static [110,111]. Future multiomic approaches provide promise for better understanding the covariation in these mechanisms [112]. However, the observed upregulation of SFRP2 and COL5A2 in HMPOS-2.5 and S100A6 and TPM2 in HMPOS-10 indicates the importance of the Wnt/β-catenin signaling pathway in chemoresistance [17,56,58,79,91].
5. Conclusions
There are clear distinctions in the stage of the EMT-like phenotype and the mechanisms of tumorigenesis and chemotherapy resistance between HMPOS, HMPOS-2.5, and HMPOS-10. The differentiation of HMPOS-2.5 and HMPOS-10 from HMPOS demonstrates the ability of cancer cells to acquire resistance when under selection pressure from exposure to chemotherapy drugs. The contrast between the mechanisms of the HMPOS-2.5 and HMPOS-10 cell lines shows the complexity of chemotherapy resistance and the evolution of the adaptative mechanisms of cancer cells. The investigation of subclonal populations of each cell line helps to explore to evolution and acquisition of chemotherapy resistance. The EIF2 signaling pathway, the mTOR pathway, and the sirtuin pathway particularly seem to play important roles in chemotherapy resistance and the differentiation of HMPOS-10. The sirtuin pathway is known to play an essential role in maintaining malignancy, affecting cell longevity [113]. The role of sirtuins is complex and varies between cancer types, though evidence suggests that sirtuins have an inhibitory effect on cell viability. Interestingly, the member SIRT1 induces EMT and enhances prostate cancer cell migration and metastasis [114]. The gene expression patterns of each cell line indicate the correlation of the EMT-like phenotype with chemotherapy resistance. Fifteen genes that were upregulated and five genes that were downregulated were strongly associated with EMT in the previous literature. Nine of these genes, TMSB4X, LGALS3, COL3A1, HMGA1, S100A6, TPM2, CCND2, TFPI2, and HMGA2, were either upregulated or only expressed in HMPOS-10. The previous proteomic analysis performed using these HMPOS-derived cell lines showed that the EMT marker FSTL1 was upregulated in both HMPOS-2.5 and HMPOS-10, as previously observed, but CDH2 was only upregulated in HMPOS-10 in this experiment. This indicates that HMPOS-10 is further involved in the EMT-like process in comparison with HMPOS-2.5.
This study was only able to evaluate the transcriptome of each cell and does not provide a full picture of the genetic landscape between these cell lines, nor the cell surface protein complement. This experiment also does not encapsulate the effects of the tumor microenvironment or transmissible chemotherapy resistance. A lack of correlation in expression between the previous proteomics and the present transcriptomics data may be due to annotation differences. The genetic divergence of these three cell lines will be explored in the future, along with the potential causative mutations that are affecting the regulation of genes associated with these varying levels of chemotherapy resistance. Another limitation of this study is the use of a long-established cell line, which may mean that the results do not fully reflect the mechanisms involved in vivo, though it allowed us to clearly see the genetic divergence from a very homogenous cell line. This can be rectified in future investigations by developing primary cell lines from tumor samples that have and have not been treated with chemotherapy to compare the expression of the tumor pre- and post-treatment. Additionally, comparisons of the tumor microenvironment, bone marrow distal to the tumor, and healthy bone marrow could be utilized for expression analysis using the methods in this work. Examining transcriptomics at the time of excision between cell populations of the heterogeneous tumor tissue and homogeneous cell lines would add to future experimental designs in the context of conveying chemotherapy drug resistance.
These results indicate the importance of the EMT-like process in the evolution of chemotherapy resistance. This analysis provides insight into potential treatment targets and illustrates the importance of accounting for the tumor evolution trajectory at the start of and over the progression of treatment to combat chemotherapy resistance in OSA.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/genes14030558/s1, Figure S1. Condition averages of triplicates for each HMPOS cell line ate each carboplatin dosage with standard error bars; Figure S2. A UMAP of the distribution of cell phases for the three HMPOS cell lines; Figure S3. A monocle pseudotime trajectory plot showing the progress of each cell in differentiating from a beginning state to a terminal state; Figure S4. Violin plots of gene expression of genes that showed an increase with an increase or decrease in expression in correlation with the increase in chemotherapy respectively; Figure S5. Violin plots of expression of genes that were highly upregulated or downregulated in HMPOS 10; Figure S6. Violin plots of gene expression of genes that were highly upregulated or downregulated for HMPOS 2.5; Figure S7. Network representation of the core analysis results for the differential expression gene list comparing HMPOS to HMPOS-2.5 and Pathway analysis for the same list; Figure S8. Network representation of the core analysis results for the differential expression gene list comparing HMPOS to HMPOS-10 and Pathway analysis for the same list; Figure S9. Network representation of the core analysis results for the differential expression gene list comparing HMPOS-2.5 to HMPOS-10 and Pathway analysis for the same list; Figure S10. Network representation of the core analysis results for the differential expression gene list comparing HMPOS to HMPOS-Var1 and Pathway analysis for the same list; Figure S11. Network representation of the core analysis results for the differential expression gene list comparing HMPOS-2.5 to HMPOS-2.5-Var and Pathway analysis for the same list; Figure S12. Network representation of the core analysis results for the differential expression gene list comparing HMPOS-10 to HMPOS-10-Var and Pathway analysis for the same list; Figure S13. Network representation of the core analysis results for the differential expression gene list comparing the subclusters within HMPOS-10 (clusters 5 to 1) and Pathway analysis for the same list. Table S1. Invasion and migration assay indices; Table S2. Differential expression between HMPOS-CTRL and HMPOS-2.5; Table S3. Differential expression between HMPOS-CTRL and HMPOS-10; Table S4. Differential expression between HMPOS-2.5 and HMPOS-10; Table S5. Differential expression between HMPOS-CTRL and all other cells; Table S6. Differential expression between HMPOS-2.5 and all other cells; Table S7. Differential expression between HMPOS-10 and all other cells; Table S8. Differential expression between Cluster 5 and Cluster 1; Table S9. Differential expression between Cluster 5 and Cluster 9; Table S10. Differential expression between Cluster 9 and Cluster 1; Table S11. Differential expression between Cluster 8 and Clusters 0, 4, 6; Table S12. Differential expression between Cluster 10 and Clusters 2, 3, 7, and 12; Table S13. Differential expression between Cluster 11 and Clusters 1, 5, and 9.
Author Contributions
Conceptualization, S.B. and B.W.D.; methodology, M.A.W. and B.W.D.; formal analysis, M.A.H. and B.W.D.; investigation, M.A.H., T.M. and B.W.D.; resources, M.A.W., B.W.-J. and S.B.; data curation, B.W.D.; writing—original draft preparation, M.A.H. and B.W.D.; writing—review and editing, M.A.H., T.M., S.B. and B.W.D.; visualization, M.A.H.; supervision, S.B. and B.W.D.; project administration, B.W.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
All raw sequencing data have been submitted to the NCBI Sequence Read Archive (SRA) under BioProject PRJNA934861. The codes used in all analyses are available at www.github.com/EvoMedLab/HMPOS/.
Acknowledgments
The authors would like to thank Edward F Barroga and Toru Fujina for providing the HMPOS cells.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Smrke, A.; Anderson, P.M.; Gulia, A.; Gennatas, S.; Huang, P.H.; Jones, R.L. Future Directions in the Treatment of Osteosarcoma. Cells 2021, 10, 172. [Google Scholar] [CrossRef]
- Mirabello, L.; Troisi, R.J.; Savage, S.A. International Osteosarcoma Incidence Patterns in Children and Adolescents, Middle Ages and Elderly Persons. Int. J. Cancer 2009, 125, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Whelan, J.; Seddon, B.; Perisoglou, M. Management of Osteosarcoma. Curr. Treat. Options Oncol. 2006, 7, 444–455. [Google Scholar] [CrossRef] [PubMed]
- Vail, D.M.; MacEwen, E.G. Spontaneously Occurring Tumors of Companion Animals as Models for Human Cancer. Cancer Investig. 2000, 18, 781–792. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Mirabello, L. Using Epidemiology and Genomics to Understand Osteosarcoma Etiology. Sarcoma 2011, 2011, 548151. [Google Scholar] [CrossRef]
- Lorenz, S.; Barøy, T.; Sun, J.; Nome, T.; Vodák, D.; Bryne, J.-C.; Håkelien, A.-M.; Fernandez-Cuesta, L.; Möhlendick, B.; Rieder, H.; et al. Unscrambling the Genomic Chaos of Osteosarcoma Reveals Extensive Transcript Fusion, Recurrent Rearrangements and Frequent Novel TP53 Aberrations. Oncotarget 2016, 7, 5273–5288. [Google Scholar] [CrossRef]
- Yang, Y.; Basu, S.; Mirabello, L.; Spector, L.; Zhang, L. A Bayesian Gene-Based Genome-Wide Association Study Analysis of Osteosarcoma Trio Data Using a Hierarchically Structured Prior. Cancer Inform. 2018, 17, 1176935118775103. [Google Scholar] [CrossRef]
- Makielski, K.M.; Mills, L.J.; Sarver, A.L.; Henson, M.S.; Spector, L.G.; Naik, S.; Modiano, J.F. Risk Factors for Development of Canine and Human Osteosarcoma: A Comparative Review. Vet. Sci. 2019, 6, 48. [Google Scholar] [CrossRef]
- Sakthikumar, S.; Elvers, I.; Kim, J.; Arendt, M.L.; Thomas, R.; Turner-Maier, J.; Swofford, R.; Johnson, J.; Schumacher, S.E.; Alföldi, J.; et al. SETD2 Is Recurrently Mutated in Whole-Exome Sequenced Canine Osteosarcoma. Cancer Res. 2018, 78, 3421–3431. [Google Scholar] [CrossRef]
- Gardner, H.L.; Sivaprakasam, K.; Briones, N.; Zismann, V.; Perdigones, N.; Drenner, K.; Facista, S.; Richholt, R.; Liang, W.; Aldrich, J.; et al. Canine Osteosarcoma Genome Sequencing Identifies Recurrent Mutations in DMD and the Histone Methyltransferase Gene SETD2. Commun. Biol. 2019, 2, 266. [Google Scholar] [CrossRef]
- Dagogo-Jack, I.; Shaw, A.T. Tumour Heterogeneity and Resistance to Cancer Therapies. Nat. Rev. Clin. Oncol. 2018, 15, 81–94. [Google Scholar] [CrossRef]
- Crucitta, S.; Cucchiara, F.; Mathijssen, R.; Mateo, J.; Jager, A.; Joosse, A.; Passaro, A.; Attili, I.; Petrini, I.; van Schaik, R.; et al. Treatment-Driven Tumour Heterogeneity and Drug Resistance: Lessons from Solid Tumours. Cancer Treat. Rev. 2022, 104, 102340. [Google Scholar] [CrossRef]
- Stewart, D.J. Mechanisms of Resistance to Cisplatin and Carboplatin. Crit. Rev. Oncol. Hematol. 2007, 63, 12–31. [Google Scholar] [CrossRef]
- Zhou, J.; Kang, Y.; Chen, L.; Wang, H.; Liu, J.; Zeng, S.; Yu, L. The Drug-Resistance Mechanisms of Five Platinum-Based Antitumor Agents. Front. Pharmacol. 2020, 11, 343. [Google Scholar] [CrossRef]
- Geller, D.S.; Gorlick, R. Osteosarcoma: A Review of Diagnosis, Management, and Treatment Strategies. Clin. Adv. Hematol. Oncol. 2010, 8, 705–718. [Google Scholar]
- Ohmichi, M.; Hayakawa, J.; Tasaka, K.; Kurachi, H.; Murata, Y. Mechanisms of Platinum Drug Resistance. Trends Pharmacol. Sci. 2005, 26, 113–116. [Google Scholar] [CrossRef]
- Weinman, M.A.; Ramsey, S.A.; Leeper, H.J.; Brady, J.V.; Schlueter, A.; Stanisheuski, S.; Maier, C.S.; Miller, T.; Ruby, C.E.; Bracha, S. Exosomal Proteomic Signatures Correlate with Drug Resistance and Carboplatin Treatment Outcome in a Spontaneous Model of Canine Osteosarcoma. Cancer Cell. Int. 2021, 21, 245. [Google Scholar] [CrossRef]
- Tew, K.D.; Manevich, Y.; Grek, C.; Xiong, Y.; Uys, J.; Townsend, D.M. The Role of Glutathione S-Transferase P in Signaling Pathways and S-Glutathionylation in Cancer. Free Radic. Biol. Med. 2011, 51, 299–313. [Google Scholar] [CrossRef]
- Liu, L.; Zhu, H.; Liao, Y.; Wu, W.; Liu, L.; Liu, L.; Wu, Y.; Sun, F.; Lin, H.-W. Inhibition of Wnt/β-Catenin Pathway Reverses Multi-Drug Resistance and EMT in Oct4+/Nanog+ NSCLC Cells. Biomed. Pharmacother. 2020, 127, 110225. [Google Scholar] [CrossRef]
- Navin, N.; Kendall, J.; Troge, J.; Andrews, P.; Rodgers, L.; McIndoo, J.; Cook, K.; Stepansky, A.; Levy, D.; Esposito, D.; et al. Tumour Evolution Inferred by Single-Cell Sequencing. Nature 2011, 472, 90–94. [Google Scholar] [CrossRef]
- Barroga, E.F.; Kadosawa, T.; Okumura, M.; Fujinaga, T. Establishment and Characterization of the Growth and Pulmonary Metastasis of a Highly Lung Metastasizing Cell Line from Canine Osteosarcoma in Nude Mice. J. Vet. Med. Sci. 1999, 61, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.X.Y.; Terry, J.M.; Belgrader, P.; Ryvkin, P.; Bent, Z.W.; Wilson, R.; Ziraldo, S.B.; Wheeler, T.D.; McDermott, G.P.; Zhu, J.; et al. Massively Parallel Digital Transcriptional Profiling of Single Cells. Nat. Commun. 2017, 8, 14049. [Google Scholar] [CrossRef]
- Wang, C.; Wallerman, O.; Arendt, M.-L.; Sundström, E.; Karlsson, Å.; Nordin, J.; Mäkeläinen, S.; Pielberg, G.R.; Hanson, J.; Ohlsson, Å.; et al. A Novel Canine Reference Genome Resolves Genomic Architecture and Uncovers Transcript Complexity. Commun. Biol. 2021, 4, 185. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Hao, S.; Andersen-Nissen, E.; Mauck, W.M.; Zheng, S.; Butler, A.; Lee, M.J.; Wilk, A.J.; Darby, C.; Zager, M.; et al. Integrated Analysis of Multimodal Single-Cell Data. Cell 2021, 184, 3573–3587.e29. [Google Scholar] [CrossRef] [PubMed]
- R Core Team R: A Language and Environment for Statistical Computing. 2020. Available online: https://www.R-project.org/ (accessed on 1 February 2021).
- Trapnell, C.; Cacchiarelli, D.; Grimsby, J.; Pokharel, P.; Li, S.; Morse, M.; Lennon, N.J.; Livak, K.J.; Mikkelsen, T.S.; Rinn, J.L. The Dynamics and Regulators of Cell Fate Decisions Are Revealed by Pseudotemporal Ordering of Single Cells. Nat. Biotechnol. 2014, 32, 381–386. [Google Scholar] [CrossRef]
- Street, K.; Risso, D.; Fletcher, R.B.; Das, D.; Ngai, J.; Yosef, N.; Purdom, E.; Dudoit, S. Slingshot: Cell Lineage and Pseudotime Inference for Single-Cell Transcriptomics. BMC Genom. 2018, 19, 477. [Google Scholar] [CrossRef]
- Raudvere, U.; Kolberg, L.; Kuzmin, I.; Arak, T.; Adler, P.; Peterson, H.; Vilo, J. G:Profiler: A Web Server for Functional Enrichment Analysis and Conversions of Gene Lists (2019 Update). Nucleic Acids Res. 2019, 47, W191–W198. [Google Scholar] [CrossRef]
- Krämer, A.; Green, J.; Pollard, J.; Tugendreich, S. Causal Analysis Approaches in Ingenuity Pathway Analysis. Bioinformatics 2014, 30, 523–530. [Google Scholar] [CrossRef]
- Ramesh, V.; Brabletz, T.; Ceppi, P. Targeting EMT in Cancer with Repurposed Metabolic Inhibitors. Trends Cancer 2020, 6, 942–950. [Google Scholar] [CrossRef]
- Morita, T.; Hayashi, K. Tumor Progression Is Mediated by Thymosin-Β4 through a TGFβ/MRTF Signaling Axis. Mol. Cancer Res. 2018, 16, 880–893. [Google Scholar] [CrossRef]
- Sosne, G.; Qiu, P.; Goldstein, A.L.; Wheater, M. Biological Activities of Thymosin Beta4 Defined by Active Sites in Short Peptide Sequences. FASEB J. 2010, 24, 2144–2151. [Google Scholar] [CrossRef]
- Chi, L.-H.; Chang, W.-M.; Chang, Y.-C.; Chan, Y.-C.; Tai, C.-C.; Leung, K.-W.; Chen, C.-L.; Wu, A.T.; Lai, T.-C.; Li, Y.-C.J.; et al. Global Proteomics-Based Identification and Validation of Thymosin Beta-4 X-Linked as a Prognostic Marker for Head and Neck Squamous Cell Carcinoma. Sci. Rep. 2017, 7, 9031. [Google Scholar] [CrossRef]
- He, X.; Zhang, S.; Chen, J.; Li, D. Increased LGALS3 Expression Independently Predicts Shorter Overall Survival in Patients with the Proneural Subtype of Glioblastoma. Cancer Med. 2019, 8, 2031–2040. [Google Scholar] [CrossRef]
- Nangia-Makker, P.; Hogan, V.; Raz, A. Galectin-3 and Cancer Stemness. Glycobiology 2018, 28, 172–181. [Google Scholar] [CrossRef]
- Fukumori, T.; Kanayama, H.-O.; Raz, A. The Role of Galectin-3 in Cancer Drug Resistance. Drug Resist. Updat. 2007, 10, 101–108. [Google Scholar] [CrossRef]
- Silverman, A.M.; Nakata, R.; Shimada, H.; Sposto, R.; DeClerck, Y.A. A Galectin-3-Dependent Pathway Upregulates Interleukin-6 in the Microenvironment of Human Neuroblastoma. Cancer Res. 2012, 72, 2228–2238. [Google Scholar] [CrossRef]
- Wang, D.; You, D.; Li, L. Galectin-3 Regulates Chemotherapy Sensitivity in Epithelial Ovarian Carcinoma via Regulating Mitochondrial Function. J. Toxicol. Sci. 2019, 44, 47–56. [Google Scholar] [CrossRef]
- Zhang, S.-W.; Zhang, N.; Wang, N. Role of COL3A1 and POSTN on Pathologic Stages of Esophageal Cancer. Technol. Cancer Res. Treat. 2020, 19, 1533033820977489. [Google Scholar] [CrossRef]
- Engqvist, H.; Parris, T.Z.; Kovács, A.; Nemes, S.; Werner Rönnerman, E.; de Lara, S.; Biermann, J.; Sundfeldt, K.; Karlsson, P.; Helou, K. Immunohistochemical Validation of COL3A1, GPR158 and PITHD1 as Prognostic Biomarkers in Early-Stage Ovarian Carcinomas. BMC Cancer 2019, 19, 928. [Google Scholar] [CrossRef]
- Pádua, D.; Pinto, D.F.; Figueira, P.; Pereira, C.F.; Almeida, R.; Mesquita, P. HMGA1 Has Predictive Value in Response to Chemotherapy in Gastric Cancer. Curr. Oncol. 2021, 29, 56–67. [Google Scholar] [CrossRef]
- Song, J.; Cui, D.; Wang, J.; Qin, J.; Wang, S.; Wang, Z.; Zhai, X.; Ma, H.; Ma, D.; Liu, Y.; et al. Overexpression of HMGA1 Confers Radioresistance by Transactivating RAD51 in Cholangiocarcinoma. Cell Death Discov. 2021, 7, 322. [Google Scholar] [CrossRef]
- Liau, S.-S.; Whang, E. HMGA1 Is a Molecular Determinant of Chemoresistance to Gemcitabine in Pancreatic Adenocarcinoma. Clin. Cancer Res. 2008, 14, 1470–1477. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Liu, J.; Chen, T.; Sun, R.; Liu, Z.; Qiu, B.; Xu, Y.; Zhang, Z. HMGA1-TRIP13 Axis Promotes Stemness and Epithelial Mesenchymal Transition of Perihilar Cholangiocarcinoma in a Positive Feedback Loop Dependent on c-Myc. J. Exp. Clin. Cancer Res. 2021, 40, 86. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.-Y.; Shea, Q.T.; Wong, T.-L.; Luk, S.T.; Tong, M.; Lo, C.-M.; Man, K.; Yun, J.-P.; Guan, X.-Y.; Lee, T.K.; et al. Chemotherapy-Enriched THBS2-Deficient Cancer Stem Cells Drive Hepatocarcinogenesis through Matrix Softness Induced Histone H3 Modifications. Adv. Sci. 2021, 8, 2002483. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Yang, H.; Xiang, X.; Liu, L.; Huang, H.; Tang, G. THBS2 Is Closely Related to the Poor Prognosis and Immune Cell Infiltration of Gastric Cancer. Front. Genet. 2022, 13, 803460. [Google Scholar] [CrossRef]
- Lin, C.-C.; Huang, Y.-K.; Cho, C.-F.; Lin, Y.-S.; Lo, C.-C.; Kuo, T.-T.; Tseng, G.-C.; Cheng, W.-C.; Chang, W.-C.; Hsiao, T.-H.; et al. Targeting Positive Feedback between BASP1 and EGFR as a Therapeutic Strategy for Lung Cancer Progression. Theranostics 2020, 10, 10925–10939. [Google Scholar] [CrossRef]
- Li, L.; Meng, Q.; Li, G.; Zhao, L. BASP1 Suppresses Cell Growth and Metastasis through Inhibiting Wnt/β-Catenin Pathway in Gastric Cancer. BioMed Res. Int. 2020, 2020, 8628695. [Google Scholar] [CrossRef]
- Li, S.; Guo, R.; Peng, Z.; Quan, B.; Hu, Y.; Wang, Y.; Wang, Y. NPR3, Transcriptionally Regulated by POU2F1, Inhibits Osteosarcoma Cell Growth through Blocking the PI3K/AKT Pathway. Cell. Signal. 2021, 86, 110074. [Google Scholar] [CrossRef]
- Yue, X.; Zhao, Y.; Liu, J.; Zhang, C.; Yu, H.; Wang, J.; Zheng, T.; Liu, L.; Li, J.; Feng, Z.; et al. BAG2 Promotes Tumorigenesis through Enhancing Mutant P53 Protein Levels and Function. eLife 2015, 4, e08401. [Google Scholar] [CrossRef]
- Sun, L.; Chen, G.; Sun, A.; Wang, Z.; Huang, H.; Gao, Z.; Liang, W.; Liu, C.; Li, K. BAG2 Promotes Proliferation and Metastasis of Gastric Cancer via ERK1/2 Signaling and Partially Regulated by MiR186. Front. Oncol. 2020, 10, 31. [Google Scholar] [CrossRef]
- Tu, R.; Kang, W.; Kang, Y.; Chen, Z.; Zhang, P.; Xiong, X.; Ma, J.; Du, R.-L.; Zhang, C. C-MYC-USP49-BAG2 Axis Promotes Proliferation and Chemoresistance of Colorectal Cancer Cells in Vitro. Biochem. Biophys. Res. Commun. 2022, 607, 117–123. [Google Scholar] [CrossRef]
- Li, X.; Xiao, R.; Tembo, K.; Hao, L.; Xiong, M.; Pan, S.; Yang, X.; Yuan, W.; Xiong, J.; Zhang, Q. PEG10 Promotes Human Breast Cancer Cell Proliferation, Migration and Invasion. Int. J. Oncol. 2016, 48, 1933–1942. [Google Scholar] [CrossRef]
- Xie, T.; Pan, S.; Zheng, H.; Luo, Z.; Tembo, K.M.; Jamal, M.; Yu, Z.; Yu, Y.; Xia, J.; Yin, Q.; et al. PEG10 as an Oncogene: Expression Regulatory Mechanisms and Role in Tumor Progression. Cancer Cell. Int. 2018, 18, 112. [Google Scholar] [CrossRef]
- Zhang, M.; Sui, C.; Dai, B.; Shen, W.; Lu, J.; Yang, J. PEG10 Is Imperative for TGF-Β1-Induced Epithelial-Mesenchymal Transition in Hepatocellular Carcinoma. Oncol. Rep. 2017, 37, 510–518. [Google Scholar] [CrossRef]
- Li, Y.; Wagner, E.R.; Yan, Z.; Wang, Z.; Luther, G.; Jiang, W.; Ye, J.; Wei, Q.; Wang, J.; Zhao, L.; et al. The Calcium-Binding Protein S100A6 Accelerates Human Osteosarcoma Growth by Promoting Cell Proliferation and Inhibiting Osteogenic Differentiation. Cell Physiol. Biochem. 2015, 37, 2375–2392. [Google Scholar] [CrossRef]
- Luo, T.; Liu, Q.; Tan, A.; Duan, L.; Jia, Y.; Nong, L.; Tang, J.; Zhou, W.; Xie, W.; Lu, Y.; et al. Mesenchymal Stem Cell-Secreted Exosome Promotes Chemoresistance in Breast Cancer via Enhancing MiR-21-5p-Mediated S100A6 Expression. Mol. Ther. Oncolytics 2020, 19, 283–293. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, J.; Xu, S.; Zhang, X.; Wang, P.; Wu, H.; Xia, B.; Zhang, G.; Lei, B.; Wan, L.; et al. Hypoxia-Induced TPM2 Methylation Is Associated with Chemoresistance and Poor Prognosis in Breast Cancer. Cell Physiol. Biochem. 2018, 45, 692–705. [Google Scholar] [CrossRef]
- Shin, H.; Kim, D.; Helfman, D.M. Tropomyosin Isoform Tpm2.1 Regulates Collective and Amoeboid Cell Migration and Cell Aggregation in Breast Epithelial Cells. Oncotarget 2017, 8, 95192–95205. [Google Scholar] [CrossRef]
- Wang, J.; Shu, H.; Guo, S. MiR-646 Suppresses Proliferation and Metastasis of Non-small Cell Lung Cancer by Repressing FGF2 and CCND2. Cancer Med. 2020, 9, 4360–4370. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, Y.; Che, Y.-Q. CCND2 MRNA Expression Is Correlated With R-CHOP Treatment Efficacy and Prognosis in Patients With ABC-DLBCL. Front. Oncol. 2020, 10, 1180. [Google Scholar] [CrossRef]
- Tan, Y.; Zhang, T.; Zhou, L.; Liu, S.; Liang, C. MiR-34b-3p Represses the Multidrug-Chemoresistance of Bladder Cancer Cells by Regulating the CCND2 and P2RY1 Genes. Med. Sci. Monit. 2019, 25, 1323–1335. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Chen, X.; Wang, C.; Jiang, Y.; Li, J.; Ying, X.; Yang, Y.; Li, B.; Zhou, C.; Zhong, J.; et al. The Role of TFPI2 Hypermethylation in the Detection of Gastric and Colorectal Cancer. Oncotarget 2017, 8, 84054–84065. [Google Scholar] [CrossRef] [PubMed]
- Guan, G.; Xie, J.; Dai, Y.; Han, H. TFPI2 Suppresses the Interaction of TGF-Β2 Pathway Regulators to Promote Endothelial–Mesenchymal Transition in Diabetic Nephropathy. J. Biol. Chem. 2022, 298, 101725. [Google Scholar] [CrossRef]
- Mansoori, B.; Mohammadi, A.; Ditzel, H.J.; Duijf, P.H.G.; Khaze, V.; Gjerstorff, M.F.; Baradaran, B. HMGA2 as a Critical Regulator in Cancer Development. Genes 2021, 12, 269. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Wang, Y.; Deng, H.; Liu, C.; Wu, J.; Lai, M. HMGA2 Enhances 5-Fluorouracil Chemoresistance in Colorectal Cancer via the Dvl2/Wnt Pathway. Oncotarget 2018, 9, 9963–9974. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Torres, D.; Nancarrow, D.J.; Steinberg, H.; Wang, Z.; Kuick, R.; Weh, K.M.; Mills, R.E.; Ray, D.; Ray, P.; Lin, J.; et al. Constitutively Higher Level of GSTT2 in Esophageal Tissues From African Americans Protects Cells Against DNA Damage. Gastroenterology 2019, 156, 1404–1415. [Google Scholar] [CrossRef]
- Gutiontov, S.I.; Turchan, W.T.; Spurr, L.F.; Rouhani, S.J.; Chervin, C.S.; Steinhardt, G.; Lager, A.M.; Wanjari, P.; Malik, R.; Connell, P.P.; et al. CDKN2A Loss-of-Function Predicts Immunotherapy Resistance in Non-Small Cell Lung Cancer. Sci. Rep. 2021, 11, 20059. [Google Scholar] [CrossRef]
- Malarikova, D.; Berkova, A.; Obr, A.; Blahovcova, P.; Svaton, M.; Forsterova, K.; Kriegova, E.; Prihodova, E.; Pavlistova, L.; Petrackova, A.; et al. Concurrent TP53 and CDKN2A Gene Aberrations in Newly Diagnosed Mantle Cell Lymphoma Correlate with Chemoresistance and Call for Innovative Upfront Therapy. Cancers 2020, 12, 2120. [Google Scholar] [CrossRef]
- Sun, H.-F.; Yang, X.; Zhao, Y.; Tian, Q.; Chen, M.-T.; Zhao, Y.; Jin, W. Loss of TMEM126A Promotes Extracellular Matrix Remodeling, Epithelial-to-Mesenchymal Transition, and Breast Cancer Metastasis by Regulating Mitochondrial Retrograde Signaling. Cancer Lett. 2019, 440–441, 189–201. [Google Scholar] [CrossRef]
- Jing, W.; Zhu, H.; Liu, W.; Zhai, X.; Tian, H.; Yu, J. MTAP-Deficiency Could Predict Better Treatment Response in Advanced Lung Adenocarcinoma Patients Initially Treated with Pemetrexed-Platinum Chemotherapy and Bevacizumab. Sci. Rep. 2020, 10, 843. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, T.-T.; Gao, L.; Tan, Y.-N.; Li, Y.-T.; Tan, X.-Y.; Huang, T.-X.; Li, H.-H.; Bai, F.; Zou, C.; et al. Downregulation of MTAP Promotes Tumor Growth and Metastasis by Regulating ODC Activity in Breast Cancer. Int. J. Biol. Sci. 2022, 18, 3034–3047. [Google Scholar] [CrossRef]
- Cheng, X.-Y.; Liu, Z.; Shang, L.; Cai, H.-Q.; Zhang, Y.; Cai, Y.; Xu, X.; Hao, J.-J.; Wang, M.-R. Deletion and Downregulation of MTAP Contribute to the Motility of Esophageal Squamous Carcinoma Cells. OncoTargets Ther. 2017, 10, 5855–5862. [Google Scholar] [CrossRef]
- Zhao, L.; Chen, X.; Feng, Y.; Wang, G.; Nawaz, I.; Hu, L.; Liu, P. COX7A1 Suppresses the Viability of Human Non-Small Cell Lung Cancer Cells via Regulating Autophagy. Cancer Med. 2019, 8, 7762–7773. [Google Scholar] [CrossRef]
- Fernandes, M.T.; Ghezzo, M.N.; Silveira, A.B.; Kalathur, R.K.; Póvoa, V.; Ribeiro, A.R.; Brandalise, S.R.; Dejardin, E.; Alves, N.L.; Ghysdael, J.; et al. Lymphotoxin-β Receptor in Microenvironmental Cells Promotes the Development of T-Cell Acute Lymphoblastic Leukaemia with Cortical/Mature Immunophenotype. Br. J. Haematol. 2015, 171, 736–751. [Google Scholar] [CrossRef]
- Hu, X.; Zimmerman, M.A.; Bardhan, K.; Yang, D.; Waller, J.L.; Liles, G.B.; Lee, J.R.; Pollock, R.; Lev, D.; Ware, C.F.; et al. Lymphotoxin β Receptor Mediates Caspase-Dependent Tumor Cell Apoptosis in Vitro and Tumor Suppression in Vivo despite Induction of NF-ΚB Activation. Carcinogenesis 2013, 34, 1105–1114. [Google Scholar] [CrossRef]
- Zhang, X.; Huang, T.; Li, Y.; Qiu, H. Upregulation of THBS1 Is Related to Immunity and Chemotherapy Resistance in Gastric Cancer. Int. J. Gen. Med. 2021, 14, 4945–4957. [Google Scholar] [CrossRef]
- Jayachandran, A.; Anaka, M.; Prithviraj, P.; Hudson, C.; McKeown, S.J.; Lo, P.-H.; Vella, L.J.; Goding, C.R.; Cebon, J.; Behren, A. Thrombospondin 1 Promotes an Aggressive Phenotype through Epithelial-to-Mesenchymal Transition in Human Melanoma. Oncotarget 2014, 5, 5782–5797. [Google Scholar] [CrossRef]
- Sun, Y.; Zhu, D.; Chen, F.; Qian, M.; Wei, H.; Chen, W.; Xu, J. SFRP2 Augments WNT16B Signaling to Promote Therapeutic Resistance in the Damaged Tumor Microenvironment. Oncogene 2016, 35, 4321–4334. [Google Scholar] [CrossRef]
- Huang, C.; Ye, Z.; Wan, J.; Liang, J.; Liu, M.; Xu, X.; Li, L. Secreted Frizzled-Related Protein 2 Is Associated with Disease Progression and Poor Prognosis in Breast Cancer. Dis. Markers 2019, 2019, 6149381. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Xu, H.; Zhang, T.; Xue, Y.; An, R. Secreted Frizzled Related Protein 2 Modulates Epithelial-Mesenchymal Transition and Stemness via Wnt/β-Catenin Signaling in Choriocarcinoma. Cell Physiol. Biochem. 2018, 50, 1815–1831. [Google Scholar] [CrossRef]
- Qin, T.; Zhu, W.; Kan, X.; Li, L.; Wu, D. Luteolin Attenuates the Chemoresistance of Osteosarcoma through Inhibiting the PTN/β-Catenin/MDR1 Signaling Axis by Upregulating MiR-384. J. Bone Oncol. 2022, 34, 100429. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Liu, L.; Yan, X.; Wang, C.; Wang, Y.; Han, K.; Lin, S.; Gan, Z.; Min, D. Pleiotrophin Promotes Chemoresistance to Doxorubicin in Osteosarcoma by Upregulating P-Glycoprotein. Oncotarget 2017, 8, 63857–63870. [Google Scholar] [CrossRef] [PubMed]
- Perez-Pinera, P.; Alcantara, S.; Dimitrov, T.; Vega, J.A.; Deuel, T.F. Pleiotrophin Disrupts Calcium-Dependent Homophilic Cell-Cell Adhesion and Initiates an Epithelial-Mesenchymal Transition. Proc. Natl. Acad. Sci. USA 2006, 103, 17795–17800. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.; Wang, J.; Ren, Y.; Li, L.; He, W.; Zhang, Y.; Liu, T.; Li, Z. Over-Expression of FSIP1 Promotes Breast Cancer Progression and Confers Resistance to Docetaxel via MRP1 Stabilization. Cell Death Dis. 2019, 10, 204. [Google Scholar] [CrossRef] [PubMed]
- Xi, L.; Ji, Y.; Yin, D.; Zhao, Z.; Huang, S.; Yu, S.; Liu, B.; Li, H. Effects of Dermatopontin Gene Silencing on Apoptosis and Proliferation of Osteosarcoma MG-63 Cells. Mol. Med. Rep. 2017, 17, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Sadr-Nabavi, A.; Bouromand-Noughabi, S.; Tayebi-Meybodi, N.; Dadkhah, K.; Amini, N.; Meindl, A.; Abbaszadegan, M.R. Non-Collagenous Extracellular Matrix Protein Dermatopontin May Play a Role as Another Component of Transforming Growth Factor-β Signaling Pathway in Colon Carcinogenesis. Iran. J. Basic Med. Sci. 2021, 24, 444–450. [Google Scholar] [CrossRef]
- Lin, W.; Zhu, X.; Gao, L.; Mao, M.; Gao, D.; Huang, Z. Osteomodulin Positively Regulates Osteogenesis through Interaction with BMP2. Cell Death Dis. 2021, 12, 147. [Google Scholar] [CrossRef]
- Xu, T.; Zhang, R.; Dong, M.; Zhang, Z.; Li, H.; Zhan, C.; Li, X. Osteoglycin (OGN) Inhibits Cell Proliferation and Invasiveness in Breast Cancer via PI3K/Akt/MTOR Signaling Pathway. Onco Targets Ther. 2019, 12, 10639–10650. [Google Scholar] [CrossRef]
- Hu, X.; Li, Y.-Q.; Li, Q.-G.; Ma, Y.-L.; Peng, J.-J.; Cai, S.-J. Osteoglycin (OGN) Reverses Epithelial to Mesenchymal Transition and Invasiveness in Colorectal Cancer via EGFR/Akt Pathway. J. Exp. Clin. Cancer Res. 2018, 37, 41. [Google Scholar] [CrossRef]
- Han, Y.-L.; Luo, D.; Habaxi, K.; Tayierjiang, J.; Zhao, W.; Wang, W.; Aikebaier, W.; Wang, L. COL5A2 Inhibits the TGF-β and Wnt/β-Catenin Signaling Pathways to Inhibit the Invasion and Metastasis of Osteosarcoma. Front. Oncol. 2022, 12, 813809. [Google Scholar] [CrossRef]
- Meng, X.-Y.; Shi, M.-J.; Zeng, Z.-H.; Chen, C.; Liu, T.-Z.; Wu, Q.-J.; Li, S.; Li, S. The Role of COL5A2 in Patients With Muscle-Invasive Bladder Cancer: A Bioinformatics Analysis of Public Datasets Involving 787 Subjects and 29 Cell Lines. Front. Oncol. 2018, 8, 659. [Google Scholar] [CrossRef]
- Wang, L.; Bi, R.; Yin, H.; Liu, H.; Li, L. ENO1 Silencing Impaires Hypoxia-Induced Gemcitabine Chemoresistance Associated with Redox Modulation in Pancreatic Cancer Cells. Am. J. Transl. Res. 2019, 11, 4470–4480. [Google Scholar]
- Qian, X.; Xu, W.; Xu, J.; Shi, Q.; Li, J.; Weng, Y.; Jiang, Z.; Feng, L.; Wang, X.; Zhou, J.; et al. Enolase 1 Stimulates Glycolysis to Promote Chemoresistance in Gastric Cancer. Oncotarget 2017, 8, 47691–47708. [Google Scholar] [CrossRef]
- Zhou, X.; Zhang, Y.; Han, N.; Guo, S.; Xiao, T.; Cheng, S.; Gao, Y.; Zhang, K. [α-Enolase (ENO1) Inhibits Epithelial-Mesenchymal Transition in the A549 Cell line by Suppressing ERK1/2 Phosphorylation]. Zhongguo Fei Ai Za Zhi 2013, 16, 221–226. [Google Scholar] [CrossRef]
- Pardo-Pastor, C.; Rubio-Moscardo, F.; Vogel-González, M.; Serra, S.A.; Afthinos, A.; Mrkonjic, S.; Destaing, O.; Abenza, J.F.; Fernández-Fernández, J.M.; Trepat, X.; et al. Piezo2 Channel Regulates RhoA and Actin Cytoskeleton to Promote Cell Mechanobiological Responses. Proc. Natl. Acad. Sci. USA 2018, 115, 1925–1930. [Google Scholar] [CrossRef]
- Li, Y.; Xu, C.; Sun, B.; Zhong, F.; Cao, M.; Yang, L. Piezo1 Promoted Hepatocellular Carcinoma Progression and EMT through Activating TGF-β Signaling by Recruiting Rab5c. Cancer Cell Int. 2022, 22, 162. [Google Scholar] [CrossRef]
- Myers, A.L.; Lin, L.; Nancarrow, D.J.; Wang, Z.; Ferrer-Torres, D.; Thomas, D.G.; Orringer, M.B.; Lin, J.; Reddy, R.M.; Beer, D.G.; et al. IGFBP2 Modulates the Chemoresistant Phenotype in Esophageal Adenocarcinoma. Oncotarget 2015, 6, 25897–25916. [Google Scholar] [CrossRef]
- Kühnl, A.; Kaiser, M.; Neumann, M.; Fransecky, L.; Heesch, S.; Radmacher, M.; Marcucci, G.; Bloomfield, C.D.; Hofmann, W.-K.; Thiel, E.; et al. High Expression of IGFBP2 Is Associated with Chemoresistance in Adult Acute Myeloid Leukemia. Leuk Res. 2011, 35, 1585–1590. [Google Scholar] [CrossRef]
- Zhu, H.; Zhang, Y.; Geng, Y.; Lu, W.; Yin, J.; Li, Z.; Huang, L.; Liu, H.; Xu, N. IGFBP2 Promotes the EMT of Colorectal Cancer Cells by Regulating E-Cadherin Expression. Int. J. Clin. Exp. Pathol. 2019, 12, 2559–2565. [Google Scholar]
- Zhao, L.; Zhang, J.; Qu, X.; Yang, Y.; Gong, Z.; Yang, Y.; Wu, Z.; Guo, W. Microsatellite Instability-Related ACVR2A Mutations Partially Account for Decreased Lymph Node Metastasis in MSI-H Gastric Cancers. Onco Targets Ther. 2020, 13, 3809–3821. [Google Scholar] [CrossRef]
- Januchowski, R.; Świerczewska, M.; Sterzyńska, K.; Wojtowicz, K.; Nowicki, M.; Zabel, M. Increased Expression of Several Collagen Genes Is Associated with Drug Resistance in Ovarian Cancer Cell Lines. J. Cancer 2016, 7, 1295–1310. [Google Scholar] [CrossRef] [PubMed]
- Rozpedek, W.; Pytel, D.; Mucha, B.; Leszczynska, H.; Diehl, J.A.; Majsterek, I. The Role of the PERK/EIF2α/ATF4/CHOP Signaling Pathway in Tumor Progression During Endoplasmic Reticulum Stress. Curr. Mol. Med. 2016, 16, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Tao, T.; Li, H.; Zhu, X. MTOR Signaling Pathway and MTOR Inhibitors in Cancer: Progress and Challenges. Cell Biosci. 2020, 10, 31. [Google Scholar] [CrossRef] [PubMed]
- Yousafzai, N.A.; Jin, H.; Ullah, M.; Wang, X. Recent Advances of SIRT1 and Implications in Chemotherapeutics Resistance in Cancer. Am. J. Cancer Res. 2021, 11, 5233–5248. [Google Scholar]
- Sisto, M.; Ribatti, D.; Ingravallo, G.; Lisi, S. The Expression of Follistatin-like 1 Protein Is Associated with the Activation of the EMT Program in Sjögren’s Syndrome. J. Clin. Med. 2022, 11, 5368. [Google Scholar] [CrossRef]
- Loh, C.-Y.; Chai, J.Y.; Tang, T.F.; Wong, W.F.; Sethi, G.; Shanmugam, M.K.; Chong, P.P.; Looi, C.Y. The E-Cadherin and N-Cadherin Switch in Epithelial-to-Mesenchymal Transition: Signaling, Therapeutic Implications, and Challenges. Cells 2019, 8, 1118. [Google Scholar] [CrossRef]
- Yoo, H.C.; Yu, Y.C.; Sung, Y.; Han, J.M. Glutamine Reliance in Cell Metabolism. Exp. Mol. Med. 2020, 52, 1496–1516. [Google Scholar] [CrossRef]
- Liu, C.; Wang, H.; Wang, W.; Wang, L.; Liu, W.; Wang, J.; Geng, Q.; Lu, Y. ENO2 Promotes Cell Proliferation, Glycolysis, and Glucocorticoid-Resistance in Acute Lymphoblastic Leukemia. Cell. Physiol. Biochem. 2018, 46, 1525–1535. [Google Scholar] [CrossRef]
- Tang, W.; Zhou, M.; Dorsey, T.H.; Prieto, D.A.; Wang, X.W.; Ruppin, E.; Veenstra, T.D.; Ambs, S. Integrated Proteotranscriptomics of Breast Cancer Reveals Globally Increased Protein-MRNA Concordance Associated with Subtypes and Survival. Genome Med. 2018, 10, 94. [Google Scholar] [CrossRef]
- Cristobal, A.; van den Toorn, H.W.P.; van de Wetering, M.; Clevers, H.; Heck, A.J.R.; Mohammed, S. Personalized Proteome Profiles of Healthy and Tumor Human Colon Organoids Reveal Both Individual Diversity and Basic Features of Colorectal Cancer. Cell Rep. 2017, 18, 263–274. [Google Scholar] [CrossRef]
- Menyhárt, O.; Győrffy, B. Multi-Omics Approaches in Cancer Research with Applications in Tumor Subtyping, Prognosis, and Diagnosis. Comput. Struct. Biotechnol. J. 2021, 19, 949–960. [Google Scholar] [CrossRef]
- Zhao, E.; Hou, J.; Ke, X.; Abbas, M.N.; Kausar, S.; Zhang, L.; Cui, H. The Roles of Sirtuin Family Proteins in Cancer Progression. Cancers 2019, 11, 1949. [Google Scholar] [CrossRef]
- Byles, V.; Zhu, L.; Lovaas, J.D.; Chmilewski, L.K.; Wang, J.; Faller, D.V.; Dai, Y. SIRT1 Induces EMT by Cooperating with EMT Transcription Factors and Enhances Prostate Cancer Cell Migration and Metastasis. Oncogene 2012, 31, 4619–4629. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).