Clinical Characterization of Korean Patients with Pseudoxanthoma Elasticum and Angioid Streaks
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Settings
2.2. Patient Evaluation
2.3. Sample Collection and Sequencing
2.4. Diagnosis of Pseudoxanthoma Elasticum
3. Results
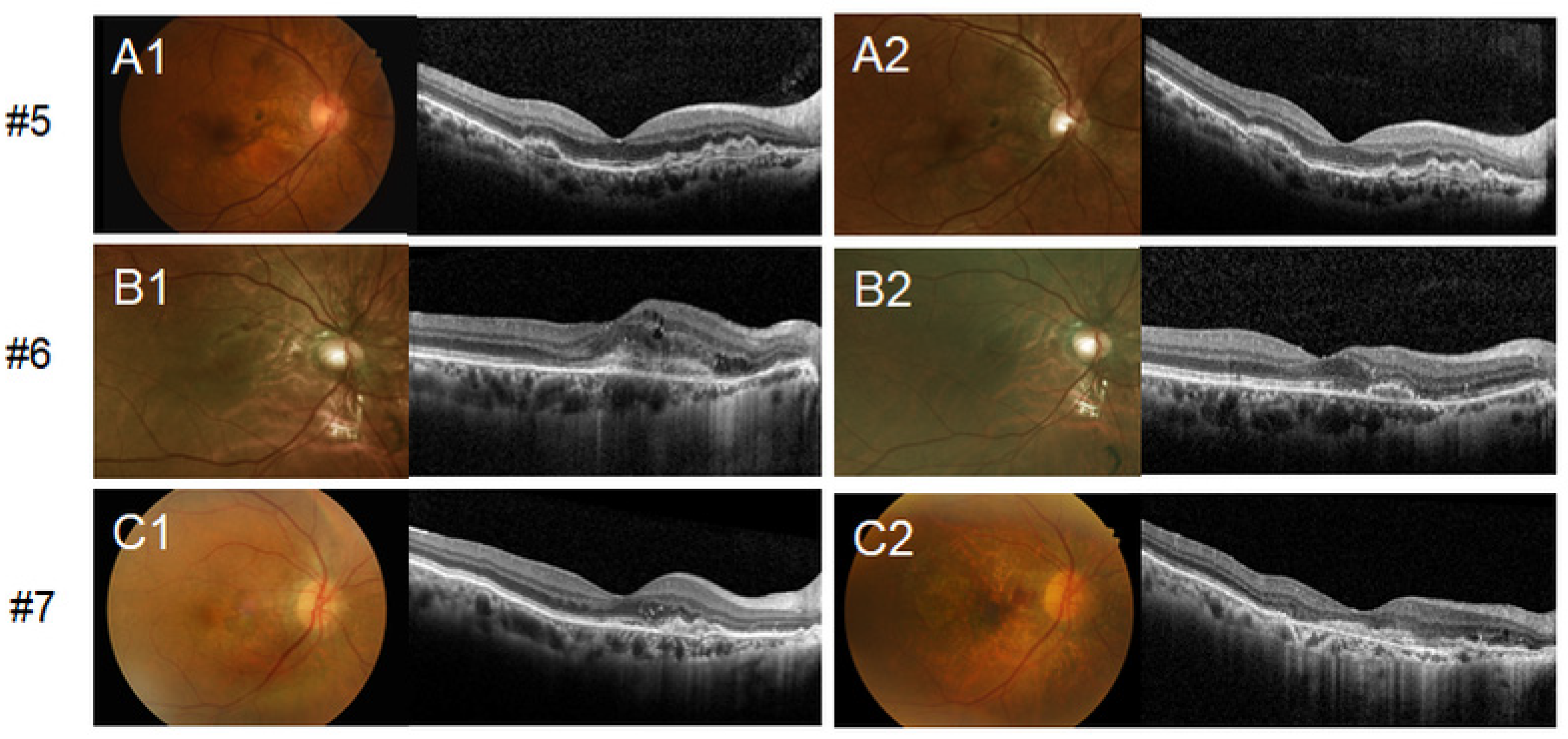
3.1. Retinal Phenotypic Features of Patients
3.2. Genotypes of Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gliem, M.; Zaeytijd, J.D.; Finger, R.P.; Holz, F.G.; Leroy, B.P.; Issa, P.C. An update on the ocular phenotype in patients with pseudoxanthoma elasticum. Front. Genet. 2013, 4, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plomp, A.S.; Toonstra, J.; Bergen, A.A.B.; van Dijk, M.R.; de Jong, P.T.V.M. Proposal for updating the pseudoxanthoma elasticum classification system and a review of the clinical findings. Am. J. Med. Genet. A 2010, 152A, 1049–1058. [Google Scholar] [CrossRef]
- Bartstra, J.W.; Risseeuw, S.; de Jong, P.A.; van Os, B.; Kalsbeek, L.; Mol, C.; Baas, A.F.; Verschuere, S.; Vanakker, O.; Florijn, R.J.; et al. Genotype-phenotype correlation in pseudoxanthoma elasticum. Atherosclerosis 2021, 324, 18–26. [Google Scholar] [CrossRef]
- Georgalas, I.; Papaconstantinou, D.; Koutsandrea, C.; Kalantzis, G.; Karagiannis, D.; Georgopoulos, G.; Ladas, I. Angioid streaks, clinical course, complications, and current therapeutic management. Ther. Clin. Risk Manag. 2009, 5, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Germain, D.P. Pseudoxanthoma elasticum. Orphanet J. Rare Dis. 2017, 12, 85. [Google Scholar] [CrossRef]
- Le Saux, O.; Urban, Z.; Tschuch, C.; Csiszar, K.; Bacchelli, B.; Quaglino, D.; Pasquali-Ronchetti, I.; Pope, F.M.; Richards, A.; Terry, S.; et al. Mutations in a gene encoding an ABC transporter cause pseudoxanthoma elasticum. Nat. Genet. 2000, 25, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Issa, P.C.; Tysoe, C.; Caswell, R. Late-onset pseudoxanthoma elasticum associated with a hypomorphic ABCC6 variant. Am. J. Ophthalmol. 2020, 218, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Finger, R.P.; Issa, P.C.; Ladewig, M.S.; Götting, C.; Szliska, C.; Scholl, H.P.; Holz, F.G. Pseudoxanthoma elasticum: Genetics, clinical manifestations and therapeutic approaches. Surv. Ophthalmol. 2009, 54, 272–285. [Google Scholar] [CrossRef] [PubMed]
- Hesse, R.J.; Groetsch, J.; Burshell, A. Pseudoxanthoma elasticum: A novel mutation in the ABCC6 gene that affects eye manifestations of the disease. Ochsner J. 2010, 10, 13–15. [Google Scholar]
- Sun, Q.; Wang, W.; Wu, L.; Cheng, L.; Tong, X.; Xu, X. Unexpected ABCC6 mRNA splicing in a Chinese family with pseudoxanthoma elasticum. Acta Ophthalmol. 2019, 97, e381–e389. [Google Scholar] [CrossRef]
- Yoshida, S.; Honda, M.; Yoshida, A.; Nakao, S.; Goto, Y.; Nakamura, T.; Fujisawa, K.; Ishibashi, T. Novel mutation in ABCC6 gene in a Japanese pedigree with pseudoxanthoma elasticum and retinitis pigmentosa. Eye 2005, 19, 215–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birtel, J.; Yusuf, I.H.; Priglinger, C.; Rudolph, G.; Issa, P.C. Diagnosis of inherited retinal diseases. Klin. Monbl. Augenheilkd 2021, 238, 249–259. [Google Scholar]
- Gliem, M.; Birtel, J.; Müller, P.L.; Hendig, D.; Faust, I.; Herrmann, P.; Holz, F.G.; Adamus, G.; Issa, P.C. Acute retinopathy in pseudoxanthoma elasticum. JAMA Ophthalmol. 2019, 137, 1165–1173. [Google Scholar] [CrossRef]
- Cai, L.; Lumsden, A.; Guenther, U.P.; Neldner, S.A.; Zäch, S.; Knoblauch, H.; Ramesar, R.; Hohl, D.; Callen, D.F.; Neldner, K.H.; et al. A novel Q378X mutation exists in the transmembrane transporter protein ABCC6 and its pseudogene: Implications for mutation analysis in pseudoxanthoma elasticum. J. Mol. Med. 2001, 79, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Costrop, L.M.; Vanakker, O.O.; Van Laer, L.; Le Saux, O.; Martin, L.; Chassaing, N.; Guerra, D.; Pasquali-Ronchetti, I.; Coucke, P.J.; De Paepe, A. Novel deletions causing pseudoxanthoma elasticum underscore the genomic instability of the ABCC6 region. J. Hum. Genet. 2010, 55, 112–117. [Google Scholar] [CrossRef] [Green Version]
- Sato, N.; Nakayama, T.; Mizutani, Y.; Yuzawa, M. Novel mutations of ABCC6 gene in Japanese patients with Angioid streaks. Biochem. Biophys. Res. Commun. 2009, 380, 548–553. [Google Scholar] [CrossRef]
- Miksch, S.; Lumsden, A.; Guenther, U.P.; Foernzler, D.; Christen-Zäch, S.; Daugherty, C.; Ramesar, R.K.; Lebwohl, M.; Hohl, D.; Neldner, K.H.; et al. Molecular genetics of pseudoxanthoma elasticum: Type and frequency of mutations in ABCC6. Hum. Mutat. 2005, 26, 235–248. [Google Scholar] [CrossRef]
- Le Saux, O.; Beck, K.; Sachsinger, C.; Silvestri, C.; Treiber, C.; Göring, H.H.; Johnson, E.W.; De Paepe, A.; Pope, F.M.; Pasquali-Ronchetti, I.; et al. A spectrum of ABCC6 mutations is responsible for pseudoxanthoma elasticum. Am. J. Hum. Genet. 2001, 69, 749–764. [Google Scholar] [CrossRef] [Green Version]
- Martin, L.; Maître, F.; Bonicel, P.; Daudon, P.; Verny, C.; Bonneau, D.; Le Saux, O.; Chassaing, N. Heterozygosity for a single mutation in the ABCC6 gene may closely mimic PXE: Consequences of this phenotype overlap for the definition of PXE. Arch. Dermatol. 2008, 144, 301–306. [Google Scholar] [CrossRef] [Green Version]
- Bergen, A.A.; Plomp, A.S.; Schuurman, E.J.; Terry, S.; Breuning, M.; Dauwerse, H.; Swart, J.; Kool, M.; van Soest, S.; Baas, F.; et al. Mutations in ABCC6 cause pseudoxanthoma elasticum. Nat. Genet. 2000, 25, 228–231. [Google Scholar] [CrossRef]
- Pfendner, E.G.; Vanakker, O.M.; Terry, S.F.; Vourthis, S.; McAndrew, P.E.; McClain, M.R.; Fratta, S.; Marais, A.S.; Hariri, S.; Coucke, P.J.; et al. Mutation detection in the ABCC6 gene and genotype-phenotype analysis in a large international case series affected by pseudoxanthoma elasticum. J. Med. Genet. 2007, 44, 621–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jansen, R.S.; Duijst, S.; Mahakena, S.; Sommer, D.; Szeri, F.; Váradi, A.; Plomp, A.; Bergen, A.A.; Oude Elferink, R.P.; Borst, P.; et al. ABCC6-mediated ATP secretion by the liver is the main source of the mineralization inhibitor inorganic pyrophosphate in the systemic circulation-brief report. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1985–1989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jansen, R.S.; Küçükosmanoglu, A.; de Haas, M.; Sapthu, S.; Otero, J.A.; Hegman, I.E.; Bergen, A.A.; Gorgels, T.G.; Borst, P.; van de Wetering, K. ABCC6 prevents ectopic mineralization seen in pseudoxanthoma elasticum by inducing cellular nucleotide release. Proc. Natl. Acad. Sci. USA 2013, 110, 20206–20211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plomp, A.S.; Bergen, A.A.; Florijn, R.J.; Terry, S.F.; Toonstra, J.; van Dijk, M.R.; de Jong, P.T. Pseudoxanthoma elasticum: Wide phenotypic variation in homozygotes and no signs in heterozygotes for the c.3775delT mutation in ABCC6. Genet. Med. 2009, 11, 852–858. [Google Scholar] [CrossRef] [Green Version]
- Navasiolava, N.; Gnanou, M.; Douillard, M.; Saulnier, P.; Aranyi, T.; Ebran, J.M.; Henni, S.; Humeau, H.; Lefthériotis, G.; Martin, L. The extent of pseudoxanthoma elasticum skin changes is related to cardiovascular complications and visual loss: A cross-sectional study. Br. J. Dermatol. 2019, 180, 207–208. [Google Scholar] [CrossRef] [Green Version]
- Utani, A.; Tanioka, M.; Yamamoto, Y.; Taki, R.; Araki, E.; Tamura, H.; Miyachi, Y. Relationship between the distribution of pseudoxanthoma elasticum skin and mucous membrane lesions and cardiovascular involvement. J. Dermatol. 2010, 37, 130–136. [Google Scholar] [CrossRef]
- Risseeuw, S.; Ossewaarde-van Norel, J.; Klaver, C.C.W.; Colijn, J.M.; Imhof, S.M.; van Leeuwen, R. Visual acuity in pseudoxanthoma elasticum. Retina 2019, 39, 1580–1587. [Google Scholar] [CrossRef]
- Gliem, M.; Müller, P.L.; Birtel, J.; Hendig, D.; Holz, F.G.; Issa, P.C. Frequency, phenotypic characteristics and progression of atrophy associated with a diseased Bruch’s membrane in pseudoxanthoma elasticum. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3323–3330. [Google Scholar] [CrossRef]
- Risseeuw, S.; Ossewaarde-van Norel, J.; van Buchem, C.; Spiering, W.; Imhof, S.M.; van Leeuwen, R. The extent of angioid streaks correlates with macular degeneration in pseudoxanthoma elasticum. Am. J. Ophthalmol. 2020, 220, 82–90. [Google Scholar] [CrossRef]
- Myung, J.S.; Bhatnagar, P.; Spaide, R.F.; Klancnik, J.M., Jr.; Cooney, M.J.; Yannuzzi, L.A.; Freund, K.B. Long-term outcomes of intravitreal antivascular endothelial growth factor therapy for the management of choroidal neovascularization in pseudoxanthoma elasticum. Retina 2010, 30, 748–755. [Google Scholar] [CrossRef]
- Birtel, J.; Lindner, M.; Mishra, D.K.; Müller, P.L.; Hendig, D.; Herrmann, P.; Holz, F.G.; Fleckenstein, M.; Gliem, M.; Issa, P.C. Retinal imaging including optical coherence tomography angiography for detecting active choroidal neovascularization in pseudoxanthoma elasticum. Clin. Exp. Ophthalmol. 2019, 47, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Issa, P.C.; Finger, R.P.; Götting, C.; Hendig, D.; Holz, F.G.; Scholl, H.P. Centrifugal fundus abnormalities in pseudoxanthoma elasticum. Ophthalmology 2010, 117, 1406–1414. [Google Scholar] [CrossRef] [PubMed]
- Gliem, M.; Hendig, D.; Finger, R.P.; Holz, F.G.; Issa, P.C. Reticular pseudodrusen associated with a diseased Bruch membrane in pseudoxanthoma elasticum. JAMA Ophthalmol. 2015, 133, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Gliem, M.; Wieg, I.; Birtel, J.; Müller, P.L.; Faust, I.; Hendig, D.; Holz, F.G.; Finger, R.P.; Issa, P.C. Retinal findings in carriers of monoallelic ABCC6 mutations. Br. J. Ophthalmol. 2020, 104, 1089–1092. [Google Scholar] [CrossRef] [PubMed]
- Kasemsarn, P.; Boonchai, W. Pseudoxanthoma elasticum-like lesions in beta-thalassemia/hemoglobin E patient: A case report. J. Dermatol. 2013, 40, 409–410. [Google Scholar] [CrossRef] [PubMed]
- Szeri, F.; Miko, A.; Navasiolava, N.; Kaposi, A.; Verschuere, S.; Li, Q.; Terry, S.F.; Boraldi, F.; Uitto, J.; van de Wetering, K.; et al. The pathogenic p.(R391G) ABCC6 displays incomplete penetrance implying the necessity of an interacting partner for the development of pseudoxanthoma elasticum. medRxiv 2020. [Google Scholar] [CrossRef]

| Patient ID | Sex | Age at Diagnosis (years) | Symptom | Follow-Up Duration (years) | BCVA at Baseline | BCVA at Last Follow-Up | Intravitreal Injections |
|---|---|---|---|---|---|---|---|
| #1 | F | 32 | None | 14.9 | (OD) 20/20 (OS) 20/20 | (OD) 20/20 (OS) 20/20 | None |
| #2 | F | 37 | None | 3.2 | (OD) 20/25 (OS) 20/25 | (OD) 20/20 (OS) 20/20 | None |
| #3 | M | 32 | None | 2.0 | (OD) 20/20 (OS) 20/25 | (OD) 20/20 (OS) 20/20 | None |
| #4 | F | 51 | None | 0.3 | (OD) 20/32 (OS) 20/25 | (OD) 20/32 (OS) 20/25 | None |
| #5 | M | 51 | Sudden vision loss | 3.9 | (OD) 20/63 (OS) 20/20 | (OD) 20/50 (OS) 20/100 | (OD) Bevacizumab 5 times (OS) Bevaicuzumab 3 times |
| #6 | F | 64 | Vision loss of unknown onset | 0.6 | (OD) 20/40 (OS) 20/25 | (OD) 20/25 (OS) 20/32 | (OD) Bevacizumab 4 times (OS) Bevaicuzumab 3 times |
| #7 | F | 69 | Vision loss of unknown onset | 12.1 | (OD) 20/50 (OS) 20/25 | (OD) 20/1000 (OS) 20/40 | (OD) Bevacizumab 33 times, Ranibizumab 13 times, Aflibercept 3 times (OS) Bevacizumab 25 times |
| Exon | Nucleotide Change | Protein Variant | Patient ID | CADD PHRED Score (GRCh37-v1.4) | Polyphen-2 (Score) | SIFT (Score) | MutationTaster | Allele Frequency (%) in gnomAD | Clinical Significance (ClinVar) | Pathogenicity (ACMG Classification) | Reference No. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 9 | c.1132C>T | p.Gln378Ter | #2 | 36 | N/A | N/A | Disease causing | 0.006 | Pathogenic | Pathogenic | [14] |
| 9 | Del_Exon9 | p.? | #2 | N/A | N/A | N/A | N/A | N/A | N/A | Pathogenic | [15] |
| 10 | c.1256G>A | p.Arg419Gln | #6 | 23.9 | Probably damaging (0.994) | Deleterious (0) | Disease causing | 0.008 | Pathogenic | Likely pathogenic | [16] |
| 16 | c.2035G>T | p.Glu679Ter | #5 | 48 | N/A | N/A | Disease causing | None | Novel | Pathogenic | N/A (novel variant) |
| 19 | c.2419C>T | p.Arg807Trp | #6 | 29.3 | Probably damaging (1.000) | Deleterious (0) | Disease causing | 0.002 | Pathogenic | Likely pathogenic | [17] |
| 19 | c.2542delA | p.Met848CysfsTer83 | #3, #7 | N/A | N/A | N/A | N/A | 0.020 | N/A | Pathogenic | [16] |
| 28 | c.3940C>T | p.Arg1314Trp | #4 | 32 | Probably damaging (1.000) | Deleterious (0) | Disease causing | 0.029 | Pathogenic | Pathogenic | [6] |
| 29 | c.4192C>T | p.Arg1398Ter | #1 | 38 | N/A | N/A | Disease causing | 0.002 | Pathogenic | Pathogenic | [18] |
| Del_ABCC6 | #7 | N/A | N/A | N/A | N/A | N/A | N/A | Pathogenic | [19] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, K.W.; Joo, K.; Woo, S.J. Clinical Characterization of Korean Patients with Pseudoxanthoma Elasticum and Angioid Streaks. Genes 2021, 12, 1207. https://doi.org/10.3390/genes12081207
Jin KW, Joo K, Woo SJ. Clinical Characterization of Korean Patients with Pseudoxanthoma Elasticum and Angioid Streaks. Genes. 2021; 12(8):1207. https://doi.org/10.3390/genes12081207
Chicago/Turabian StyleJin, Ki Won, Kwangsic Joo, and Se Joon Woo. 2021. "Clinical Characterization of Korean Patients with Pseudoxanthoma Elasticum and Angioid Streaks" Genes 12, no. 8: 1207. https://doi.org/10.3390/genes12081207
APA StyleJin, K. W., Joo, K., & Woo, S. J. (2021). Clinical Characterization of Korean Patients with Pseudoxanthoma Elasticum and Angioid Streaks. Genes, 12(8), 1207. https://doi.org/10.3390/genes12081207







