Abstract
The gut mucosal epithelium is one of the largest organs in the body and plays a critical role in regulating the crosstalk between the resident microbiome and the host. To this effect, the tight control of what is permitted through this barrier is of high importance. There should be restricted passage of harmful microorganisms and antigens while at the same time allowing the absorption of nutrients and water. An increased gut permeability, or “leaky gut”, has been associated with a variety of diseases ranging from infections, metabolic diseases, and inflammatory and autoimmune diseases to neurological conditions. Several factors can affect gut permeability, including cytokines, dietary components, and the gut microbiome. Here, we discuss how the gut microbiome impacts the permeability of the gut epithelial barrier and how this can be harnessed for therapeutic purposes.
1. Introduction
The intestinal barrier is a complex system that provides a physical separation between the inside of the body and the external world. This barrier is not impermeable, but delicately balances the inward and outward passage of molecules. Despite the simplistic view of the intestinal barrier as a single layer of cells, it is made up of a complex multilayer system (Figure 1). The outermost mucus layer serves as a filter for potential pathogens in the gut lumen, while simultaneously providing a nutrient-rich environment for the microbiota residing within and around it. Underneath the mucus layer sits the epithelium, a cellular barrier defining the boundaries between the interior and exterior of the body. These tightly packed cells are responsible for the absorption of nutrients, the regulation of water transport, metabolite exchange and the exclusion of antigens and microorganisms [1]. This filtering capacity is not only due to the secretion of mucus but also to the regulation of bridges between adjacent microvilli, creating a mesh that keeps microorganisms away from the main body of the organ [2,3]. It also mediates the crosstalk between the local microbiome and the host’s immune system. Residing within and under the epithelium are immune cells that work in close proximity with the epithelium, scouting for pathogenic invaders and sampling environmental components from both diet and the microbiome. The interaction between these three compartments—the microbiome, epithelium, and immune system—regulates gut permeability [4]. Allowing the passage of nutrients, water and other factors needed for the correct functioning of the body, whilst excluding the translocation of harmful substances or even microorganisms, is critical for the wellbeing of the organism, and increased permeability or leakiness is often linked to diseases.
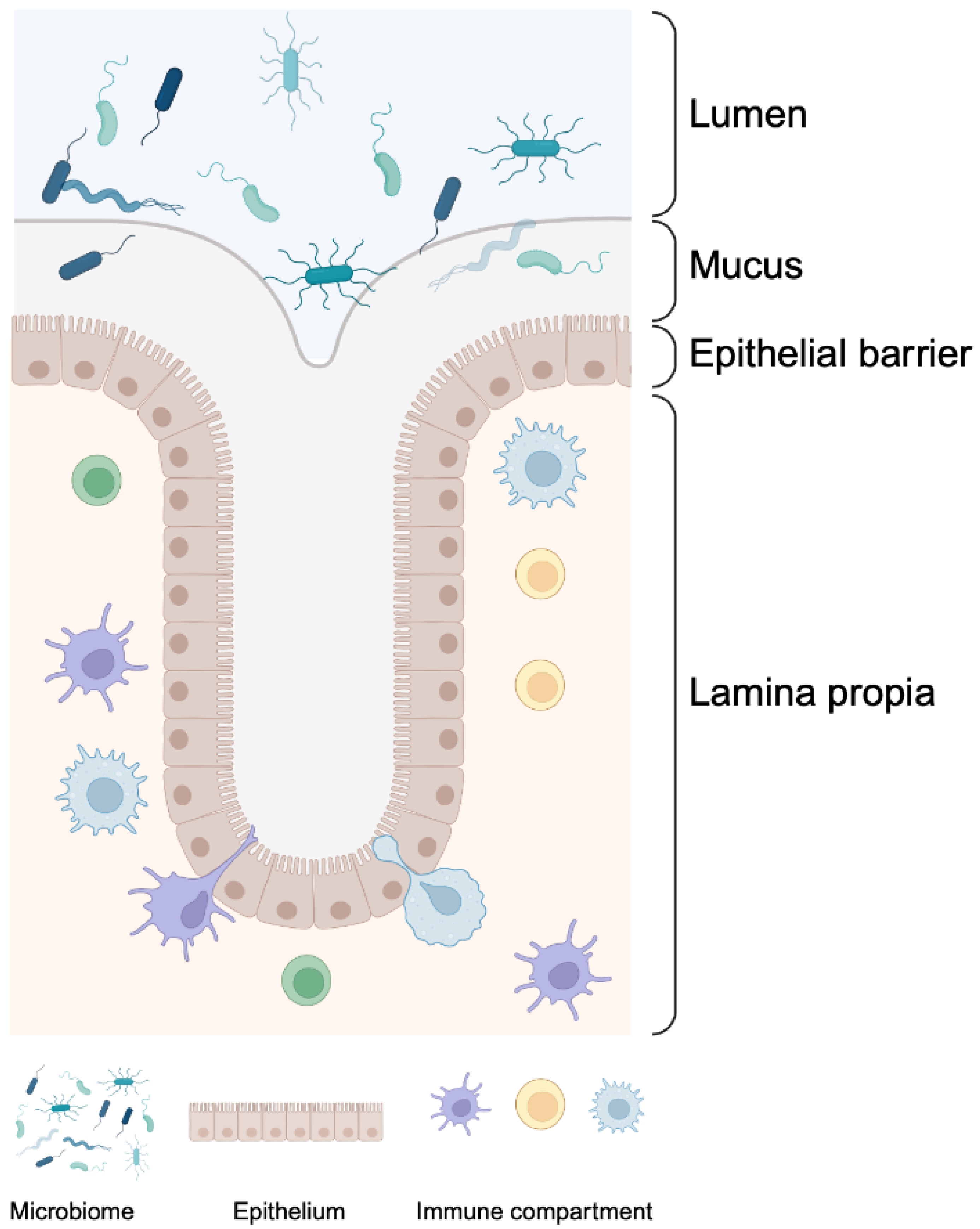
Figure 1.
The intestinal barrier is a complex, multilayered system. The mucus layer acts as a filter, impairing access to the epithelial layer underneath it while providing nutrients to the microbiota residing within and around it. The epithelial barrier is made up of tightly packed epithelial cells forming a physical boundary between the interior and exterior of the body and regulates the passage of nutrients, water, and other molecules. Immune cells reside within the epithelial layer and under it, in the lamina propria, patrolling in close proximity to the epithelium and constantly monitoring for pathogenic invaders and testing environmental molecules. The interactions between these three components, the microbiome, the epithelium, and the immune compartment, regulate permeability across the intestinal barrier. This figure was created with BioRender.com.
2. Key Elements in Barrier Permeability
The intestinal barrier is primarily maintained by the epithelial layer, and considering the diversity of its functions, it is not surprising that there is no single mechanism that controls permeability. Indeed, there are multiple molecules and mechanisms involved in the transport and exclusion of different molecules and microorganisms. Transportation through the epithelium takes place through two major routes: the transepithelial or transcellular pathway, which involves the translocation of molecules through epithelial cells; and the paracellular pathway (Figure 2A), which involves transport through the space between epithelial cells [5].
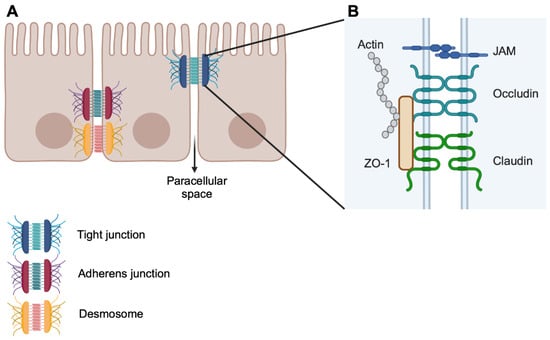
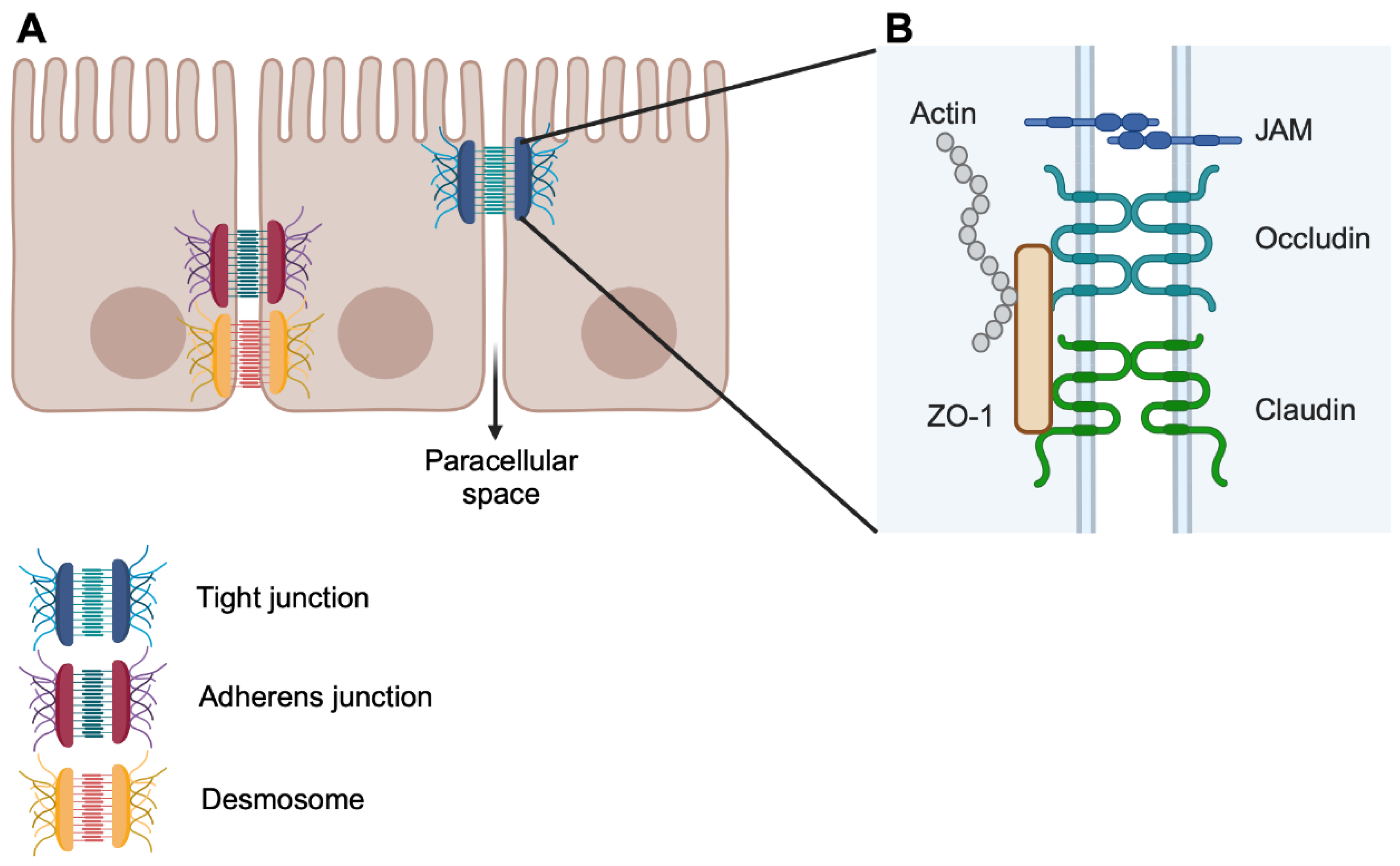
Figure 2.
Epithelial paracellular transport. (A) Epithelial cells are held together through a series of protein complexes that breach the gap between cells and seal the paracellular space. Desmosome and adherens junctions are primarily involved in cell–cell interactions and bring adjacent cells together and promote the formation of tight junctions. Tight junctions seal the paracellular space and regulate the passage of molecules. (B) Composition of tight junctions. Claudins form the backbone of the tight junctions, and the composition of the claudins forming the junction determines the flow rate through the junction. Occludin and JAM proteins stabilise the junction. The intracellular component, ZO-1, provides a scaffold for the transcellular components and a link to the actin cytoskeleton. JAM: junctional adhesion molecules; ZO-1: zonula occludens-1. This figure was created with BioRender.com.
Transport via the transcellular pathways is the physiological route for nutrient absorption and it involves specific transporters, such as for amino acids, sugars, short-chain fatty acids (SCFAs) [5], or it can occur in a non-specific manner through endocytosis (transcytosis) [6]. Although transcellular transport is important in the context of disease, in particular relating to diarrhoea, it has little impact on gut leakiness [7]. On the other hand, paracellular transport is regulated by intercellular complexes, which could belong to one of three types: desmosomes, adherens and tight junctions (Figure 2A) [5]. These complexes are located at the lateral membrane of the epithelial cells and keep the paracellular space closed.
Desmosomes are placed at the basolateral border and have intracellular and intercellular components. Intercellularly, desmosomal cadherins (Desmogleins and Desmocollins) provide the adhesive bond between cells. Intracellularly, the cadherins are anchored to desmosomal plaques, formed by the Armadillo proteins plakophilin and plakogoblin. This plaque is then linked to the cytoskeleton via desmoplakin [8]. Desmosomes provide resistance to mechanical stress [9], but they are also involved in managing intestinal permeability by creating strong cell–cell bonds and stabilising tight junctions [10,11].
Moving up apically along the lateral membrane are the adherens junctions. The primary role for adherens junctions is to mediate cell–cell adhesion, as well as taking part in cell signalling and transcriptional regulation [12]. Like desmosomes, adherens junctions include a cadherin family member as an intercell adhesion component anchored in the cytoplasm by Armadillo proteins. E-cadherin dimers bind homotypically to dimers on neighbouring cells. This is a weak cell–cell interaction that kick-starts the formation of the adherens junctions. Clusters of cadherins are then formed and spread, strengthening the bond between cells [13]. Intracellularly, E-cadherin binds to p120-catenin and b-catenin. These proteins provide a key link to the actin cytoskeleton and are therefore involved in cell motility and provide the plasticity needed in the regulation of cell–cell interactions [14]. Desmosomes and adherens junctions provide adhesive and mechanical features that stabilise cell–cell contact and lead to the assembly of the tight junctions [15]. Sitting close to the apical border, tight junctions seal the paracellular space and are the primary regulators of flux through the epithelium [13,16]
As with the other types of junctions, tight junctions have a transmembrane component and an associated cytoplasmic component (Figure 2B). The transmembrane component comprises two types of transmembrane proteins, namely claudins and occludin [14,17]. Claudins form the backbone of the tight junction by binding to each other in cis, forming rafts or strands. These strands then bind in trans to strands on the other side of the intercellular space, sealing the gap between cells [18], with occludin playing a stabilising role in bicellular junctions [14]. Junctional adhesion molecules (JAMs) also play a role in supporting the formation and maintenance of tight junctions and, together with occludin, stabilise the junction [19]. Sitting below the transmembrane proteins, zonula occludens proteins like ZO-1 and ZO-2 crosslink the tight junction, creating a scaffold connecting the transmembrane component to the underlying actin cytoskeleton [14].
Two tight junction-dependent pathways regulate transport across the gut epithelium: the pore and leak pathways. A third route, the unrestricted pathway, allows the passage of material due to breaching of the epithelium and involves epithelial cell damage or death [17]. Pore pathways allow the passage of molecules up to 0.6 nm, and this is dependent on claudins [17,20]. There are 27 members of the claudin family, and they can be divided into barrier and pore claudins, depending on their ability to increase or decrease transepithelial resistance, a method of assessing barrier function by measuring the flow of an electrical current through a cellular monolayer [21]. Pore-forming claudins increase permeability and include claudin 2, claudin 7, claudin 10 and claudin 15. Barrier-forming claudins, on the other hand, decrease permeability, and this group includes claudin 1, claudin 3 and claudin 5, among others [22,23]. In some cases, depending on the coupling between claudin, barrier forming claudins can act like pore claudins and increase permeability, with an example being claudin 4/claudin 8 coupling [22]. The localisation of claudins varies along the intestinal villi, with barrier claudins more abundantly found towards the tip of the villi and pore claudins found around the crypt area [24].
The regulation of permeability through the pore pathways is achieved through the regulation of claudins. Both pore and barrier claudins are regulated by the same factors, although usually in the opposite direction [25]. In fact, pore-forming claudins are upregulated, whereas barrier claudins are downregulated, in diseases where epithelial barrier integrity is compromised. In particular, claudin 2 upregulation has been associated with many pathologies linked to leakiness, as this pore-forming claudin also regulates water transport [17,26,27].
The leak pathway is not as well understood as the pore pathway. Although they do share molecular components, the mechanism behind them is different. Whereas the pore pathway transport mechanism is centred on the transmembrane component of the tight junction (claudins), permeability is regulated by the intracellular component in the leak pathway [17]. Flow through the leak pathway happens via the breaking and annealing of claudin strands, meaning the claudins on either side of the tight junction are pulled apart and there is a transient, localised break in the barrier [27]. Tension is regulated by the actin cytoskeleton through the branching of F-actin and the contraction of the perijunctional actomyosin ring [27]. ZO-1’s ability to bind both F-actin and claudin highlights its key role as a regulator of the leak pathway. Indeed, the absence of ZO proteins or modifications on the actin-binding site drastically alters barrier function [28]. However, the most well-studied effect of the actin cytoskeleton on permeability involves the regulation of the contraction of the perijunctional actomyosin ring by myosin light-chain kinase (MLKC) [27,29]. MLCK proteins phosphorylate the myosin light chain (MLC), causing a contraction of the ring, leading to a disruption in tight junction [17,29]. The transmembrane component does contribute to the leak pathway (claudin post-translational modifications and occludin expression can alter permeability by modifying strand strength and stability), but it is not the driving factor [27,30].
As mentioned previously, gut epithelial permeability is regulated via a three-way interaction between the epithelium, the microbiome, and the immune system. So far, we have introduced the molecular players involved in keeping the epithelial cellular barrier together and managing the passage of substances through it. We will now look into how the intestinal microbiome influences gut permeability.
3. Regulation of Barrier Permeability by the Gut Microbiome
The gut microbiome is an important component of the intestinal barrier, not only fending off pathogens by competing for resources and producing antimicrobial compounds but also by directly regulating hosts functions through the production of metabolites. Several microbiome-derived metabolites have been shown to impact barrier permeability (Figure 3) [31,32,33,34]. For instance, butyrate, a SCFA, can improve barrier function by facilitating the assembly of tight junction proteins and inducing the expression of claudin 1 in cell line models [31,35]. Other SCFAs, like propionate, can also induce the expression of tight junction proteins like ZO-1 and occludin and thus regulate paracellular transport [36,37,38]. However, at high concentrations, butyrate can cause a barrier breach, probably due apoptosis induction [31,39]. Moreover, conjugated fatty acids are produced by some intestinal bacteria (Bifidobacterium, Butyrivibrio, Enterobacter, Roseburia, among others) in the presence of a fat-rich diet. Conjugated fatty acids, like conjugated linoleic acid (CLA), can cause the redistribution of ZO-1, occludin and claudin 3, increasing paracellular permeability, as observed in a Caco-2 assay [40]. However, in in vivo models of colitis, CLA shows a protective effect and induces the expression of tight junction proteins, increasing barrier function [41,42].

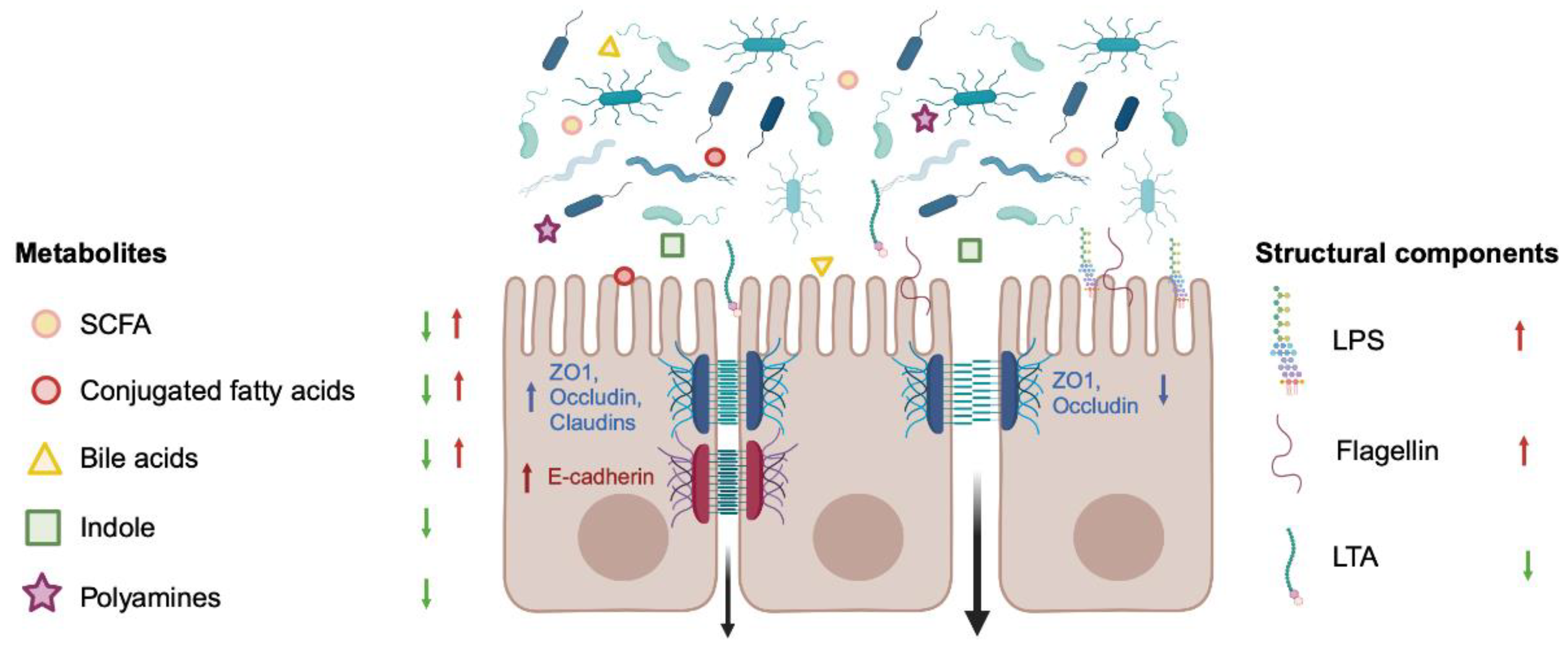
Figure 3.
Regulation of epithelial barrier permeability by the microbiome. Bacterial metabolites secreted by the microbiome as well as bacterial structural components can regulate epithelial permeability. Structural components like LPS or flagellin have a negative effect on barrier function, increasing permeability (red arrows), whereas secreted metabolites like indole or polyamines reduce permeability (green arrows). Some metabolites, like SCFAs, can improve or worsen barrier function depending on compound or dose. These metabolites regulate permeability by modifying the expression and/or localisation of tight junction or adherens junction proteins. LPS: lipopolysaccharide; LTA: lipoteichoic acid; SCFAs: short-chain fatty acids; ZO-1: zonula occludens-1. This figure was created with BioRender.com.
Germ-free (GF) mice have been shown to display increased gut permeability compared to conventionally raised mice. This observation has been attributed to the significantly lower concentration of indole and indole derivatives in GF mice. This was associated with lower expression of both adherens and tight junction proteins (claudin 1, occludin, ZO-1, E-cadherin) [31,43]. It has also been shown that indol-3-propionic acid regulates the expression of occludin, ZO1 and claudin 1 in an in vitro cell line model as well as an in vivo rat model, resulting in reduced permeability [44,45].
The role of bile acids in regulating permeability is not clear, as there are reports of some bile acid metabolites having both a positive and negative effect on barrier function, depending on the type of bile acid, concentrations tested, and cell type used for the study [31,46]. Bile acids like chenodeoxycholic acid (CDCA) and ursodeoxycholic acid (UDCA) can regulate permeability via occludin phosphorylation, ZO-1 expression, and tight junction rearrangement, but whereas CDCA has a negative effect on permeability [46,47], UDCA promotes the expression of occludin and claudin 4, increasing barrier function [48].
Polyamines are metabolised from the diet by the gut microbiota, but also produced by the host in the small intestine [49]. Polyamines increase barrier function, controlling permeability not only through the regulation of tight junction proteins like occludin and ZO-1 [50,51] but also by promoting the expression of E-cadherin [52,53]. It is not only the secreted bacterial products that can have an effect on epithelial barrier permeability; rather structural components like lipopolysaccharide (LPS), flagellin or lipoteichoic acid (LTA) can also regulate barrier function via Toll-like receptor (TLR) activation, although with different outcomes [31].
The activation of TLR2 with ligands like LTA has been shown to reduce gut permeability and induce the expression of tight junction proteins in vitro [54] and preserve tight junction assembly both in vitro and ex vivo in a mouse dextran sodium sulphate (DSS)-dependent colitis model [55]. On the other hand, activation of TLR4 and TLR5 by LPS and flagellin, respectively, results in increased permeability and altered expression of tight junction proteins, both in vivo and in vitro [56,57,58].
Breaches in barrier function and increased permeability can lead to translocation of bacteria or bacterial products, which can in turn activate the immune cells patrolling the lamina propria. Many diseases have been linked to altered permeability and we will now explore how permeability can be both a result and a trigger for the pathological state and how the microbiome can contribute to ameliorating it.
4. Infections and Gastrointestinal Permeability
Increased intestinal permeability is a hallmark of gastrointestinal (GI) infections. This is due to many enteric pathogens actively disrupting the intestinal epithelial barrier [4,59,60,61,62,63,64] by altering the structure and function of gut epithelial tight junctions [4,59,65] (Table 1). Various infectious bacteria, viruses, parasites, and fungi dysregulate tight junctions by means of different mechanisms, including the degradation of specific tight junction proteins, the activation of host cell signalling pathways and the alteration of cell cytoskeleton [60,66,67].

Table 1.
Examples of pathogen-induced modulation of gut permeability. CAR: coxsackievirus and adenovirus receptor; cGMP: cyclic guanosine monophosphate; CTA: cholera toxin subunit A; ERK1/2: extracellular signal-regulated kinase ½; Ha/P: hemagglutinin protease; HtrA: high temperature requirement protein A; JAM-A: junctional adhesion molecules-A; MLCK: myosin light-chain kinase; PKA: protein kinase A; Rho: RAS homolog; TJ: tight junction; ZOT: zonula occludens toxin.
4.1. Tight Junction Protein Degradation and Reorganisation
The direct targeting of tight junction proteins can lead to impaired junctional barrier structure and function caused by virulence factors either being secreted in the GI tract or situated on the external layer of the pathogen. These enterotoxins can degrade the tight junction by exerting a proteolytic effect, for example Campylobacter jejuni serine protease high-temperature-requirement protein A (HtrA), specifically cleaving occludin and E-cadherin proteins, thus breaking the cell-to-cell junction and leaving the basal epithelial layer vulnerable to bacterial invasion [68,69]. Other enterotoxins can interact directly with tight junction proteins as reported for Clostridium perfringens enterotoxin binding to claudin 4 or Entamoeba histolytica with claudins 1 and 2, leading to tight junction destruction [68,69,70,71,72,73,74,75].
Tight junction barrier structure and function can be altered quite dramatically by Vibrio cholerae, the well-known etiologic agent of cholera, a life-threatening infection characterised by acute diarrhoea. V. cholerae-derived cholera toxin subunit A (CTA) is responsible for adenylate cyclase activation and the subsequent increase in cyclic adenosine monophosphate (AMP) levels and opening of chloride ion channels, resulting in the substantial leakage of electrolytes and fluids (diarrhoea), characteristic of V. cholerae infections [76]. Strains lacking CTA are still able to induce diarrhoea, but with a less dramatic presentation. It is known that V. cholerae produces another tight junction-altering toxin that affects ZO-1 morphology, called zonula occludens toxin (ZOT), which targets barrier permeability specifically in the small intestine [77,78]. Another V. cholerae toxin targeting cell-to-cell junctions is hemagglutinin protease (Ha/P), a metalloproteinase with two functions, namely being substrate-lytic and a CT subunit A activator. This protease causes leakiness by degrading the transmembrane protein occludin, leading to the rearrangement of ZO-1 and F-actin morphology [59,78].
4.2. Activation of Host Cell Signalling Pathways
Microbial pathogens can also increase intestinal epithelial permeability through the modulation of signalling pathways associated with the tight junction complex. Changes in the gene expression of tight junction proteins and post-transcriptional events of key pathways like myosin light-chain kinase (MLCK), RAS homolog (Rho) and protein kinase A (PKA) can increase GI permeability. For example, the enteropathogenic Escherichia coli heat-stable enterotoxin A binds to extracellular domains like guanylate cyclase receptor (GC-C), triggering cyclic guanosine monophosphate (cGMP) formation and cAMP-dependent-protein kinase A (PKA), contributing to occludin’s rearrangement into the cytosol [79]. Shigella flexneri was also demonstrated to modulate the extracellular signal-regulated kinase 1/2 (ERK1/2) pathway, triggering alterations to the phosphorylation of claudins 2 and 4 as well as the occludin and ZO-1 proteins, resulting in altered barrier function and increased interleukin (IL)-6 and IL-8 [78,80]. Both Camplylobacter concinus zonula occludens toxin (ZOT) and E. coli heat-stable toxin B display similarities with V. cholerae ZOT and probably share regulatory pathways of the TJ complex [79,80,81].
Viruses, such as Adenovirus, Rotavirus and Coxsackievirus, target cellular receptors of the tight junction complex [82]. Both Coxsackievirus and Adenovirus target, as the name suggests, the coxsackievirus and adenovirus receptor (CAR), a transmembrane protein that, upon binding to the virus, triggers a molecular cascade leading to occludin internalisation within macropinosomes with subsequent tight junction disruption [81,82]. Although Coxsackievirus does not induce major tight junction disruption, additional viral interactions with the epithelial protein decay-accelerating factor (DAF) contribute to actin remodelling of the cell cytoskeleton and viral delivery to the tight junction with subsequent cell entry [87,88]. Rotaviruses also gain cellular entry through cellular receptors, specifically the junctional adhesion molecules-A (JAM-A), triggering an entry pathway associated with this superfamily similar to coxsackievirus [82].
4.3. Cell Cytoskeleton Alteration
Some microorganisms increase GI permeability through the modulation of the epithelial cell cytoskeleton either by destabilising toxins, or triggering myosin/actin contraction by MLCK, Rho GTPases pathway activation [89,90,91].
The pathology of salmonellosis is associated with virulence factors’ intra-epithelial translocation to the host cell cytoplasm via the type 3 secretion system (T3SS), primarily SopB, SopE, SopE2 and SipA, that also play a role in RhoGTPase pathway activation and the subsequent actin dynamics [59,60,83,84]. E. coli also uses T3SS to inject secreted proteins, EspB, EspF, EspH and Tir, and induce actin/myosin contraction by activating MLCK processes [66,85]. Furthermore, fungi in the Aspergillus and Penicillium genera have been cited to alter the epithelial cell cytoskeleton by disrupting F-actin filaments, leading to an impaired cellular function and TJ structure [86].
The gastro-intestinal barrier can be challenged by a multitude of infectious agents that have developed a variety of mechanisms to disrupt normal GI function and permeability, mainly through the exploitation of tight junction structures. As concisely but not exhaustively described, the infectious aetiology can present dynamic strategies for addressing gut leakiness.
5. Leaky Gut and Diseases
Most diseases are multifactorial, with genetic predispositions and environmental triggers conspiring and initiating these diseases. Environmental variations, such as diet, pollution and hygiene, can lead to a dysbiotic gut. As discussed above, changes in microbiota composition can have detrimental effects on the gut epithelial barrier, increasing its permeability and allowing the translocation of bacteria and their products from the gut lumen, leading to systemic effects. This strong connection between an altered intestinal microbiome and a leaky gut is proposed to be the initiating event underlying a wide spectrum of disorders from inflammatory and autoimmune diseases to metabolic and neurological diseases (Table 2). In this section, we will address the involvement of the leaky gut in the pathogenesis of these diseases, as well as therapy-induced gut complications.

Table 2.
Summary of gut epithelial mechanisms, contributing to the pathology of inflammatory bowel diseases (IBDs), rheumatic diseases and metabolic diseases. ACF-7: actin crosslinking factor 7; AS: ankylosing spondylitis; BRG1: brahma-related gene 1; CD: Chron’s disease; DNMT3A: DNA methyltransferase 3 A; DSS: dextran sodium sulfate; GGTase1: geranylgeranyltransferase type 1; HFD: high-fat diet; IBD: inflammatory bowel disease; IL-10: interleukin 10; IPA: indole-3-propionic acid; JAM-1: junction adhesion molecule-1; MMP-7: matrix metalloproteinases-7; PsA: psoriatic arthritis; RA: rheumatoid arthritis; ROS: reactive oxygen species; SLE: systemic lupus erythematosus; UC: ulcerative colitis; ZO-1: zonula occludens-1.
5.1. Inflammatory Bowel Diseases (IBDs)
IBDs include ulcerative colitis (UC) and Crohn’s disease (CD), and both diseases have a similar complex and a not fully defined aetiology. However, there is strong evidence that epithelial barrier dysfunction contributes to the onset of these diseases. Disrupted expression, cellular localisation and the function of tight junction proteins are key contributors to disrupted barriers in IBDs. Whereas the expression of some tight junction proteins, such as occludin, is reduced in IBD patients [92], the expression of others is upregulated, like claudin 1 and claudin 2 [93]. This increased expression can be attributed to the effect of the inflammatory cytokine IL-6, which is found in abundance in IBD patients [124]. Conversely, the microRNA miR-195-5p, which is reduced in UC patients in comparison to healthy controls, can impede the expression of these two claudins [125]. Furthermore, miR-24 is another microRNA that has been revealed to be specifically elevated in the colon tissue and even the blood of UC patients. This upregulated expression of miR-24 was shown to compromise epithelial barrier function in vitro by reducing the expression of cingulin, a tight junction-associated protein that is also downregulated in UC patients [94]. In addition to forming a protective physical barrier, intestinal epithelial cells play a role by influencing immune function. Aryl hydrocarbon receptor (AhR) signalling in the gut epithelia was shown to be indispensable for the induction and colonic accumulation of regulatory T cells (Tregs), following treatment with Indigo naturalis, which ameliorates the disease in UC patients and in a DSS-induced colitis mouse model [126].
Irregularities in the microbiome have been linked to IBDs. Higher numbers of bacteria were identified in the intestinal mucosal layer of IBD patients when compared to healthy individuals [95]. These changes in the microbiome can also have an impact on tight junction proteins. Fusobacterium nucleatum, found in abundance in IBD patients, has a damaging effect on the intestinal epithelial barrier by regulating the expression and distribution of the tight junction proteins ZO-1 and occludin. This damaging effect was demonstrated by the promoted colitis in DSS-treated mice receiving F. nucleatum [96]. A multiomics study of two IBD patient cohorts revealed that a subset of UC patients displayed an abundance of proteases originating from the bacterial species Bacteroides vulgatus, which disrupted the epithelial barrier by altering the tight junction proteins ZO-1 and occludin in vitro. Protease inhibitors prevented disease development in IL-10-deficient mice colonised by B. vulgatus [97]. Moreover, host-derived matrix metalloproteinases (MMPs) have been shown to be expressed at higher levels in IBD patients in comparison to healthy controls [127]. It has been demonstrated that inflammatory factors drive the expression of MMP-7, which is present at high levels in UC patients and rodent models of colitis [98]. Through targeting the degradation of the tight junction protein claudin-7, MMP-7 increases gut epithelial permeability and consequently aggravates the ongoing inflammation, which was ameliorated in MMP-7-deficient mice or by using MMP-7-blocking antibodies [98].
Microbiome-derived metabolites are also known to affect epithelial barrier fitness. In a longitudinal study in both UC and CD patients showed a reduction in the tryptophan metabolite indole-3-propionic acid (IPA) in UC patients in comparison to non-IBD individuals [99]. IPA is well known for its role in maintaining a healthy barrier [44]. A bacterial consortium used for the treatment of UC (mouse model) had an immunological effect and showed increased concentrations of IPA and butyrate [128]. Other tryptophan metabolites, like xanthurenic (XANA) and kynurenic (KYNA) acids, are negatively correlated with inflammation severity both in human IBD patients and mouse DSS models [129]. Supplementing mice with these two metabolites enhanced the viability and proliferation of epithelial cells, as well as modulating T-cell responses, leading to ameliorated disease severity in the DSS model [129].
Host-generated bile acids are also documented to influence the gut epithelial barrier. Cholic acid, one of the major bile acids produced by the liver, has been found to be more abundant in IBD patients and colitic mice due to the induction of cytochrome P450 8B1 (CYP8B1), which synthesises this bile acid. By inhibiting peroxisome proliferator-activated receptor alpha (PPARα), cholic acid hindered fatty acid oxidation and blocked intestinal stem cell renewal. The importance of this pathway is demonstrated in Cyb8b1-deficient mice, which are resistant to induced colitis [100]. Furthermore, chenodeoxycholic acid (CDCA) is another primary bile acid with detrimental effects on the epithelial barrier.
A dysfunctional actin cytoskeleton can also be the underlying reason for a defective barrier. Indeed, epithelial-specific abrogation of non-muscle myosin II, a cytoskeletal protein that regulates actin distribution and dynamics, causes alterations in tight junction proteins’ localisation, leading to compromised barrier function and mucosal inflammation [130]. Actin crosslinking factor 7 (ACF7) is another key player in cytoskeletal stability. Loss of ACF7 in Caco-2 cells has been demonstrated to destabilise tight junction proteins. In mice, intestinal-specific ACF7 knockout renders these mice more susceptible to DSS-induced colitis. Interestingly, the expression of the ACF7 gene has been shown to be reduced in UC patients, when compared to healthy controls, implying its potential role in the disease pathology [101]. Furthermore, a deficiency of geranylgeranyltransferase type 1 (GGTase1), a phenyltransferase, in epithelial cells in mice causes cytoskeleton rearrangements and consequently arrested cell shedding, eventually leading to increased gut permeability and ensuing immune activation [102]. In another study, a subset of IBD patients exhibited high expression levels of tripartite motif-containing protein 40 (TRIM40), which is epigenetically silenced in healthy controls. Downstream signalling of TRIM40 is detrimental for cortical actin formation and stabilisation, leading to compromised barrier function and subsequently persistent inflammation. TRIM40 deficiency protects mice from DSS-induced colitis, further demonstrating the key role of this protein [131]. Another example of the importance of epigenetic regulation of epithelial functions is the association between IBDs, particularly CD, and genetic variants in the DNA methyltransferase 3 A (DNMT3A) [103], which plays an important role in de novo DNA methylation [132]. DNMT3A expression is reduced in gut epithelial cells of CD patients, in comparison to healthy controls, and in mouse intestinal organoids following exposure to tumour necrosis factor (TNF). Mice with DNMT3A-deficient epithelial cells display structural alterations in the gut epithelia, as well as increased colonic permeability, rendering these mice more prone to experimentally induced colitis [133]. Finally, microbiome-derived butyrate was demonstrated to epigenetically regulate the expression of synaptopodin, an actin-binding protein that localises to epithelial tight junctions, playing a critical role in barrier function and cell motility [134].
The maintenance of healthy intestinal epithelial barrier functions relies heavily on autophagy, which regulates different physiological aspects [135]. Several genes within the autophagy pathway, such as autophagy-related 16-like 1 (ATG16L1) [104,105,106], immunity-related GTPase M (IRGM) [107,108], unc51-like autophagy-activating kinase 1 (ULK1) [108,109], and leucine-rich repeat kinase 2 (LRRK2) [110] are associated with susceptibility to CD. Furthermore, an association between IBDs and the autophagy factor and transcriptional regulator brahma-related gene 1 (BRG1) has been demonstrated [111]. Indeed, BRG1 mRNA and protein colonic expression was shown to be downregulated in UC and CD patients in comparison to healthy controls. Through regulating the transcription of autophagy factors, BRG1 regulates the levels of reactive-oxygen species (ROS), which at high levels lead to epithelial cell apoptosis and defective barrier functions. Mice with intestinal epithelial-specific deletion of BRG1 develop spontaneous colitis and demonstrate disrupted barrier functions and increased permeability, further emphasising the role of BRG1 [111]. Intestinal epithelial autophagy can be influenced by microbiome-derived mediators. The colonic protective effects of butyrate against DSS-induced injury have been attributed to its ability to regulate epithelial cell autophagy via hypoxia-inducible factor-1α (HIF-1α) [136]. Furthermore, UC patients exhibit elevated levels of autotaxin, a secreted glycoprotein that amplifies barrier disruption by inhibiting mammalian target of rapamycin (mTOR)-dependent autophagy [137]. The inhibition of autotaxin and the administration of rapamycin ameliorated colonic inflammation and reversed epithelial barrier damage in DSS-treated mice [137].
In conclusion, all factors impacting epithelial barrier health, whether intrinsic, like autophagy, or extrinsic, like the microbiome, can contribute to IBD pathology.
5.2. Rheumatic Diseases
The concept of the gut–joint axis has recently emerged following the strong evidence of gut involvement in the aetiology of rheumatic diseases. Indeed, gut microbiome dysbiosis has been described in a wide variety of rheumatic diseases, such as rheumatoid arthritis (RA), ankylosing spondylitis (AS), psoriatic arthritis (PsA) and systemic lupus erythematosus (SLE) [138]. The importance of the gut microbiome in RA initiation has been demonstrated in different RA mouse models, where mice raised under germ-free conditions only develop mild autoimmune arthritis, in comparison to specific-pathogen free (SPF) mice [139,140]. Interestingly, colonising those germ-free mice with specific bacterial species, such as segmented filamentous bacteria [140], Lactobacillus bifidus [139] and Subdoligranulum didolesgii [141] was sufficient for disease induction.
In addition to modifying immune functions, gut dysbiosis is hypothesised to contribute to RA pathology by disrupting the gut barrier function, which would facilitate the translocation of bacteria or their components/products into the lamina propria, spreading systemically and eventually leading to inflammatory responses [142]. Impaired barrier function has been reported in individuals with pre-clinical RA, early onset RA and fully established RA [112,143]. This is demonstrated by the reduced expression of the tight junction proteins occludin and claudin-1 in the intestinal epithelium [112] and increased circulating concentrations of LPS and LPS-binding protein in RA patients [143] when compared to healthy controls. This was accompanied by increased gut intestinal permeability in these patients [112]. In connection to facilitated bacterial trafficking through the gut barrier, bacterial DNA and bacterial wall components were traced in the synovial fluid of RA patients [144,145,146]. 16S rRNA gene sequencing of RA patients’ synovial fluid samples revealed that this joint invasion occurs mainly in advanced stage 4 RA (RAS4) patients, with the highly RA-associated species Prevotella copri [146,147,148] being found in most of these samples. Scanning electron microscopy analysis of the synovial fluid samples of RAS4 patients revealed objects with a rod-like or spheric shapes, and some bacterial species were successfully cultured in a fraction of these samples, clearly indicating the active bacterial invasion of the joints [146].
The observed alterations in intestinal barrier functions, associated with RA, can be attributed to changes in gut bacteria. For instance, the bacterial genus Collinsella, found in abundance in RA patients, can compromise the gut barrier [113,149,150]. Collinsella aerofaciens that has been reported to reduce the expression of the tight junction proteins ZO-1 and occludin in the Caco-2 cell line and increase disease severity in collagen-induced arthritis-susceptible HLA-DQ8 mice [113]. Similarly, the increased abundance of Enterobacteriaceae in RA patients [114] could contribute to amplified inflammation by increasing gut permeability, as previously reported in diabetic patients and healthy individuals with reduced barrier function [123]. Conversely, a lower abundance of Bifidobacterium adolescentis, Bifidobacterium longum and Faecalibacterium prausnitzii, all known for their gut barrier protective properties [151,152,153,154,155], has been reported in RA [114]. Interestingly, restoring barrier function via the administration of Bifidobacterium adolescentis [156] or butyrate [112] was shown to mitigate arthritis in rodent models. RA patients responding to biological disease-modifying antirheumatic drugs (bDMARDs) also displayed improved gut barrier function, demonstrated by a reduction in circulating permeability markers [157]. Collectively, all of these data indicate the key role of intestinal barrier function in the initiating events and pathology of RA.
Patients with AS or PsA have been reported to exhibit dysbiotic intestinal microbiota, as well as subclinical gut inflammation [115,116,117], implying a role of the microbiome in disease pathogenesis. Furthermore, healthy individuals with the HLA-B27 risk allele, associated with AS, display altered microbial composition [158]. Raising HLA-B27 transgenic rats under germ-free conditions was reported to protect against the spontaneous development of gastrointestinal and joint inflammation, further supporting the potential role of the microbiome in AS [159,160]. Furthermore, AS patients were reported to have a reduced gut epithelial expression of the tight junction proteins claudin 1, claudin 4, occludin and ZO-1, accompanied by increased gut permeability and surging systemic concentrations of permeability markers (LPS and LBP) [118]. These findings suggest that gut dysbiosis leads to a deteriorating gut barrier function, initiating inflammatory events in AS. Interestingly, restored gut barrier integrity and tight junction protein expression were associated with reduced disease activity, following the application of the tryptophan metabolite indole-3-acetic acid in an AS mouse model [161].
In SLE, the enhanced concentrations of patients’ faecal calprotectin, a widely recognised marker of increased gut permeability [162], indicate the role of intestinal barrier impairment in SLE development [163,164]. This role is further corroborated in mice, where inducing gut leakiness in two murine models of lupus, FcgRIIb−/− and pristane-induced, intensified disease progression [119]. The increased gut permeability in these models was found to promote the translocation of gut microbial components, as demonstrated by higher endotoxin and β-glucan serum concentrations and a higher bacterial burden in mesenteric lymph nodes (MLNs), which induced host cell apoptosis and eventually triggered the production of anti-dsDNA autoantibodies and immune complex formation, leading to disease aggravation [119]. Another study demonstrated that microbiome dysbiosis in a MRL/Ipr lupus mouse model was associated with increased colonic oxidative stress and intestinal permeability, leading to inflammatory responses [165]. Interestingly, significant disease amelioration in mouse models, following treatment with antibiotics, probiotics or antioxidants, was associated with an improved intestinal barrier, providing further evidence of the role of barrier function in SLE [165,166,167].
Altogether, there is a strong link between different rheumatic diseases and the integrity of the gut epithelial barrier and the interaction of the latter with the gut microbiome. Further understanding of this three-way relationship may prompt novel therapies of these diseases.
5.3. Metabolic Diseases
High-fat diets (HFD) are major drivers of prevalent metabolic diseases, like type 2 diabetes and non-alcoholic fatty liver disease (NAFLD), which are characterised by underlying low-grade inflammation that can be linked to a leaky gut. Indeed, dietary fats have been demonstrated to have a direct impact on epithelial barrier integrity. For instance, exposing obese rat strains to a HFD for 16 weeks led to a reduction in the expression of intestinal tight junction proteins, such as claudin-1, claudin-3 and junction adhesion molecule (JAM)-1, which correlated with increased gut permeability [120]. Similarly, mice exposed to a prolonged HFD not only displayed classic metabolic manifestations, such as glucose intolerance and body weight gain, but also elevated intestinal permeability, which correlated with a reduced expression of the tight junction protein ZO-1. Notably, these effects were reversed by the administration of wide-spectrum antibiotics in combination with HFD, indicating the involvement of gut microbiota in mediating the impact of HFDs [168].
Similar observations of compromised barrier function and increased bacterial translocation were confirmed in obese leptin receptor-deficient mice [121]. However, obesity per se was not identified as a cause of barrier dysfunction, which was attributed to hyperglycaemia; a common feature between obesity and HFD models [121]. This link was further corroborated in a streptozotocin (STZ)-induced type 1 diabetes model, which displayed deteriorating barrier function that could be mitigated by the application of insulin [121]. An in vitro analysis of the Caco-2 epithelial cell line revealed that exposure to increasing glucose concentrations altered epithelial cell functions and barrier integrity. This is facilitated by the bidirectional glucose transporter GLUT2, as the epithelial-specific deletion of GLUT2 protected against the STZ-induced reprogramming of epithelial cells and the loss of expression of tight junction proteins [121]. In line with these findings, high-glucose (HGD) and high-fructose (HFrD) diets were revealed to cause glucose intolerance and increase barrier permeability, attributed to a reduced expression of occludin and ZO-1, as well as an increased expression of inflammatory mediators [122]. In line with these findings, a recent study highlighted a correlation between a compromised gut barrier, determined by the reduced expression of mucins and antimicrobial peptides, and a reduced abundance of short chain fatty acids-producing bacteria, like Bifidobacterium dentium, Clostridium butyricum and Roseburia intestinalis [169]. Altogether, systemic elevation of glucose concentrations, achieved by means of different methods, is a major cause of gut epithelial barrier disruption in metabolic diseases.
The diet-induced impairment of barrier function can also be caused by changes in the microbiome’s makeup. In addition to barrier disruption, a HFD was found to introduce dramatic changes in the mouse caecal microbiome composition, in comparison to a normal diet, with a strong reduction in the abundance of Lactobacillus species, Bifidobacterium species and Bacteriodes-Prevotella species [168]. Furthermore, a HFD was revealed to favour a higher abundance of hydrogen sulphide-producing bacteria, compared to a normal diet, which was associated with poorer colonic transepithelial resistance [170]. Similarly, mice subjected to a HGD and HFrD displayed a lower abundance of Bacteriodetes and an increase in Proteobacteria in comparison to mice fed with a normal diet, which was associated with a disrupted barrier [122]. Finally, the Gram-negative order Enterobacteriales was reported to be enriched in type 2 diabetes patients and healthy controls with high colonic permeability, indicating its contribution to disease development by impairing barrier functions [123].
Dietary fat may indirectly modulate gut barrier function by promoting bile acid production. This was demonstrated in mice fed with HFD, which prompted hyperpermeability in jejunum and colon. This correlated with an increase in the faecal concentrations of almost all bile acids [171]. This is supported by previous studies investigating the effect of bile acids on epithelial cells in vitro. Cholic acid has been shown to reduce the electric transepithelial resistance (TEER) of Caco-2 cell monolayers, implying compromised barrier function. This effect was mediated by increasing the production of ROS in epithelial cells [172]. This was corroborated by another study that showed similar effects being exerted by cholic acid, deoxycholic acid (DCA) and CDCA, which led to increased permeability of Caco-2 cell monolayers, led by epidermal growth factor receptor (EGFR) autophosphorylation and occludin redistribution in tight junctions [173].
6. Therapy-Induced Epithelial Barrier Dysfunction
In this section, we will cover gut epithelial barrier disruption resulting from certain therapeutics and the mechanisms of action and consequences of those disruptions. We will not discuss immunotherapy-related colitis, which is the outcome of T-cell hyperactivity, leading to inflammatory colitis, rather than the direct disruption of the gut epithelium.
6.1. Radiation Enteritis
Radiation enteritis is a bowel injury resulting from radiotherapy of malignancies in the abdominal or pelvic regions. It affects almost 90% of patients undergoing radiotherapy, with up to 10% suffering from severe forms of enteritis [174]. The high turnover rates of the small intestinal and colonic epithelia, estimated to be the highest amongst solid tissues [175], render them prone to radiation injury. This sensitivity is manifested in the well-documented radiation-induced increase in gut epithelial permeability and abrogation of the expression of tight junction protein expression [176,177]. The interplay between the intestinal epithelial barrier and the microbiome is believed to be the major contributor to radiation enteritis. Indeed, germ-free mice are resistant to radiation enteritis [178]. Consistently, antibiotic treatment prior to radiation was found to improve gut injury through microbiome remodelling and consequently inflammation inhibition [179]. Moreover, gut microbiome dysbiosis has been associated with radiation enteritis in patients exposed to pelvic radiation. Patients suffering from radiation enteritis displayed an increased abundance of Proteobacteria and Gammaproteobacteria and a lower abundance of Bacteroides. Upon co-culture with colon epithelial cells, the dysbiotic microbiome from radiation enteritis patients led to disrupted barrier function and the induction of inflammatory cytokines [180]. Dysbiosis correction through faecal microbiota transplantation (FMT) has been revealed to protect against radiation-induced gut injury in a radiation mouse model. This was demonstrated by enhanced barrier function and an increase in mucin production [181]. Interestingly, the efficacy of FMT in relieving radiation-induced enteritis was demonstrated in a pilot study with cancer patients. Three out of the five treated patients responded by displaying improvement in symptoms following FMT application, which was completely safe [182]. The protective effect of the microbiome can be attributed to certain bacterial metabolites that enhance epithelial barrier function. Supplementing mice undergoing abdominal irradiation with IPA, a microbiome-derived tryptophan metabolite, was shown to mitigate radiation-induced gut injury and restore the gut barrier function [183]. In a different study, IPA was shown to improve barrier function by increasing the expression of tight junction proteins and mucins when applied to the epithelial cell lines Caco-2 and HT29 [44]. In conclusion, structuring the microbiome to be supportive of the gut epithelial barrier by means of the administration of antibiotics, FMT or any form of live biotherapeutic products (LBPs) is the way forward for the treatment of radiation enteritis.
6.2. Chemotherapy-Induced Gut Toxicity
One of the major adverse effects of cancer chemotherapy is gastrointestinal tract toxicity, causing nausea, vomiting and diarrhoea. These effects are attributed to chemotherapy-induced disruption of the structure and function of the epithelial barrier. Chemotherapeutic agents can stimulate enteroendocrine cells to produce mediators, such as prostaglandins and 5-hydroxy tryptamine, which trigger an emetic response by activating the vagal nerve [184]. Furthermore, chemotherapy-induced histological damage, including crypt ablation, epithelial atrophy and villi blunting, is highly regarded as the driver of the accompanying diarrhoea [185,186].
In addition to clinical manifestations, chemotherapy can lead to bacterial translocation from the gut into the blood stream due to the disrupted gut epithelial barrier. The ensuing infections are central to chemotherapy-associated morbidity and mortality, particularly in children’s haematological malignancies [187]. It has become clear that the gut microbiome plays a significant role in this serious complication. Indeed, the abundance of Enterococcaceae or Streptococcaceae at any stage of chemotherapy can predict infections in children treated for acute lymphoblastic leukaemia (ALL) [188]. This was further supported by another study, demonstrating clear differences in microbiome composition between ALL patients contracting pneumonia, following chemotherapy, and unaffected ALL patients [189]. Altogether, chemotherapy-induced barrier disruption not only resulted in gastrointestinal symptoms, but also, in combination with a certain microbiome makeup, can lead to life-threatening infections.
6.3. Graft-versus-Host Disease
Graft-versus-host disease (GVHD) is a common complication of allogenic hematopoietic stem cell transplantation, whereby donor T cells target the recipient’s antigens, leading to tissue damage. MHC-II antigen presentation by IEC is the initiating event of gastrointestinal GVHD. Indeed, gut epithelial damage, resulting from pretransplant conditioning such as radiation, has been shown to be important for the initiation of GVHD [190]. Furthermore, loss of gut barrier function is postulated to support the propagation phase of GVHD, as a poorer intestinal barrier was demonstrated to correlate with disease severity [191,192]. This was further corroborated by observing that long myosin light-chain kinase (MLCK210), a key regulator of tight junction permeability, is elevated in human GVHD biopsies [193]. Transplant-receiving mice that lack MLCK210 displayed less disease propagation [193]. This clearly demonstrates that increased gut permeability, dependent on MLCK210, is required for GVHD propagation. Another important element within the epithelial barrier is goblet cells, responsible for mucus layer formation. Loss of goblet cells is characteristic of severe GVHD and results in the disruption of the inner mucus layer and increased bacterial translocation [194]. This is supported by observing the beneficial effects of the administration of IL-25, a goblet cell growth factor, prior to transplantation in ameliorating GVHD [194].
The gut microbiome has been revealed to contribute to the development of GVHD, as germ-free mice are partially protected from disease development [195], and antibiotic treatment showed clinical benefits in humans [196]. This implies that microbiome–barrier interactions could play a role in GVHD. Indeed, MHC-II expression by intestinal epithelial cells, required for antigen presentation and the activation of donor CD4+ T cells, is dependent on gut microbiota, as IECs from germ-free mice lacked MHC-II [197]. Moreover, donor T cells not only target intestinal stem cells but also innate lymphoid cells (iLC), which mediate intestinal barrier recovery following pre-transplant conditioning through the production of IL-22 [198]. Collectively, the interplay between the gut epithelial barrier, the microbiome and the immune system is important for the initiation and progression of GVHD.
7. Concluding Remarks
The interaction of the intestinal microbiome with the gut epithelium has a significant impact on the integrity of the barrier, as outlined above. The disturbance of this axis can lead to a loss of barrier integrity during enteric infections, with V. cholerae and enteropathogenic E. coli being extreme examples. Non-pathogen-induced changes in the microbiome can also lead to gut leakiness and the unregulated escape of gut luminal contents from food antigens into bacterial products. This has been associated with local inflammation and pathology in intestinal diseases, such as IBDs and radiation enteritis, but also distal and/or systemic effects in other diseases including several autoimmune and metabolic diseases.
The human intestinal microbiome typically consists of trillions of bacteria belonging to hundreds of different species that vary among individuals, and each strain/species is likely to interact with the host via multiple mechanisms. Despite this complexity, the research discussed in this review demonstrates the considerable progress made in elucidating the mechanisms by which the microbiome affects the epithelial barrier. Undoubtedly, there are more mechanisms to be unravelled in health and disease. The most significant challenge to the field will be understanding how these mechanisms interact and working toward an integrated understanding of how the entire ecosystem leads to an overall positive or negative impact.
Given the contribution of the gut microbiome–epithelium axis to the pathology of several conditions, this axis should be a target for disease prevention and therapeutic intervention. Diet, probiotics and FMT can impact the microbiome to a greater or lesser degree and have been used in many of the above indications. Diet can have significant benefits in metabolic disease, such as reversing type 2 diabetes, but obviously the impact here is multifaceted. Beyond this, specific diets have had limited consistent therapeutic benefits in many of the other indications [199]. Personalising these diets based on an individual’s microbiome, as used to improve glucose control [200,201], may be the answer to achieve therapeutic benefit. Likewise, probiotics have modest effects at best in broad patient populations, despite preclinical data suggesting a positive benefit on barrier integrity [202]. FMT can impact the microbiome and has been shown to lead to a positive outcome in dysbiotic diseases, including IBDs [203]. Normalisation of a dysbiotic microbiome by FMT will have multiple effects on the patient, with restoring gut barrier integrity likely to be a key mechanism [204]. However, FMT can be challenging due to the availability of healthy donor stools, patient acceptability and the possibility of transferring adventitious agents including multidrug-resistant organisms, plus FMT is inconsistent, leading to the “super-donor” concept [205].
Beyond these non-specific approaches to modulating the microbiome, there is a paucity of medicines, including those in development, targeting the leaky gut. This review outlines the increasing appreciation of the full complexity of microbiome–epithelium interactions, which should allow for new medicines to be developed that target the axis more specifically. New microbiome modalities targeted at key bacterial species, such as consortia of beneficial commensal bacteria or bacteriophages to deplete negative species, are being developed for other mechanisms and could be developed for the leaky gut. In addition, a detailed understanding of the metabolites involved could enable new small molecule modulators of the axis.
The data discussed above clearly demonstrate that the interaction between the intestinal microbiome and the epithelium is incredibly important for the maintenance of gut barrier integrity and contributes to the leakiness that feeds into the pathology of several diseases. Current and future advances might inspire a new wave of therapeutics that could have benefits that cannot be realised by current medicines.
Author Contributions
Writing—original draft preparation, F.S., I.B., M.J.R. and G.B.; writing—review and editing, F.S., I.B., M.J.R. and G.B. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no external funding.
Conflicts of Interest
All Authors are employed by the company Microbiotica Ltd. The company had no role in the writing of the manuscript.
References
- Brandtzaeg, P. The gut as communicator between environment and host: Immunological consequences. Eur. J. Pharmacol. 2011, 668 (Suppl. 1), S16–S32. [Google Scholar] [CrossRef]
- Mödl, B.; Schmidt, K.; Moser, D.; Eferl, R. The intermicrovillar adhesion complex in gut barrier function and inflammation. Explor. Dig. Dis. 2022, 1, 72–79. [Google Scholar] [CrossRef]
- In, J.; Foulke-Abel, J.; Zachos, N.C.; Hansen, A.M.; Kaper, J.B.; Bernstein, H.D.; Halushka, M.; Blutt, S.; Estes, M.K.; Donowitz, M.; et al. Enterohemorrhagic Escherichia coli reduce mucus and intermicrovillar bridges in human stem cell-derived colonoids. Cell. Mol. Gastroenterol. Hepatol. 2016, 2, 48–62.e43. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M. Intestinal permeability--a new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef]
- Groschwitz, K.R.; Hogan, S.P. Intestinal barrier function: Molecular regulation and disease pathogenesis. J. Allergy Clin. Immunol. 2009, 124, 3–20; quiz 21–22. [Google Scholar] [CrossRef] [PubMed]
- Menard, S.; Cerf-Bensussan, N.; Heyman, M. Multiple facets of intestinal permeability and epithelial handling of dietary antigens. Mucosal Immunol. 2010, 3, 247–259. [Google Scholar] [CrossRef]
- Clemente-Suarez, V.J.; Martin-Rodriguez, A.; Redondo-Florez, L.; Villanueva-Tobaldo, C.V.; Yanez-Sepulveda, R.; Tornero-Aguilera, J.F. Epithelial Transport in Disease: An Overview of Pathophysiology and Treatment. Cells 2023, 12, 2455. [Google Scholar] [CrossRef] [PubMed]
- Garrod, D.; Chidgey, M. Desmosome structure, composition and function. Biochim. Biophys. Acta 2008, 1778, 572–587. [Google Scholar] [CrossRef]
- Kowalczyk, A.P.; Green, K.J. Structure, function, and regulation of desmosomes. Prog. Mol. Biol. Transl. Sci. 2013, 116, 95–118. [Google Scholar] [CrossRef]
- Schlegel, N.; Boerner, K.; Waschke, J. Targeting desmosomal adhesion and signalling for intestinal barrier stabilization in inflammatory bowel diseases—Lessons from experimental models and patients. Acta Physiol. 2021, 231, e13492. [Google Scholar] [CrossRef]
- Nagler, S.; Ghoreishi, Y.; Kollmann, C.; Kelm, M.; Gerull, B.; Waschke, J.; Burkard, N.; Schlegel, N. Plakophilin 2 regulates intestinal barrier function by modulating protein kinase C activity in vitro. Tissue Barriers 2022, 11, 2138061. [Google Scholar] [CrossRef] [PubMed]
- Lessey, L.R.; Robinson, S.C.; Chaudhary, R.; Daniel, J.M. Adherens junction proteins on the move—From the membrane to the nucleus in intestinal diseases. Front. Cell Dev. Biol. 2022, 10, 998373. [Google Scholar] [CrossRef]
- Hartsock, A.; Nelson, W.J. Adherens and tight junctions: Structure, function and connections to the actin cytoskeleton. Biochim. Biophys. Acta 2008, 1778, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Niessen, C.M. Tight junctions/adherens junctions: Basic structure and function. J. Investig. Dermatol. 2007, 127, 2525–2532. [Google Scholar] [CrossRef]
- Gierynska, M.; Szulc-Dabrowska, L.; Struzik, J.; Mielcarska, M.B.; Gregorczyk-Zboroch, K.P. Integrity of the Intestinal Barrier: The Involvement of Epithelial Cells and Microbiota—A Mutual Relationship. Animals 2022, 12, 145. [Google Scholar] [CrossRef] [PubMed]
- Vermette, D.; Hu, P.; Canarie, M.F.; Funaro, M.; Glover, J.; Pierce, R.W. Tight junction structure, function, and assessment in the critically ill: A systematic review. Intensive Care Med. Exp. 2018, 6, 37. [Google Scholar] [CrossRef]
- Horowitz, A.; Chanez-Paredes, S.D.; Haest, X.; Turner, J.R. Paracellular permeability and tight junction regulation in gut health and disease. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 417–432. [Google Scholar] [CrossRef]
- Suzuki, H.; Tani, K.; Fujiyoshi, Y. Crystal structures of claudins: Insights into their intermolecular interactions. Ann. N. Y. Acad. Sci. 2017, 1397, 25–34. [Google Scholar] [CrossRef]
- Hartmann, C.; Schwietzer, Y.A.; Otani, T.; Furuse, M.; Ebnet, K. Physiological functions of junctional adhesion molecules (JAMs) in tight junctions. Biochim. Biophys. Acta Biomembr. 2020, 1862, 183299. [Google Scholar] [CrossRef]
- Shen, L.; Weber, C.R.; Raleigh, D.R.; Yu, D.; Turner, J.R. Tight junction pore and leak pathways: A dynamic duo. Annu. Rev. Physiol. 2011, 73, 283–309. [Google Scholar] [CrossRef]
- Angelow, S.; Ahlstrom, R.; Yu, A.S. Biology of claudins. Am. J. Physiol. Renal Physiol. 2008, 295, F867–F876. [Google Scholar] [CrossRef]
- Gunzel, D.; Yu, A.S. Claudins and the modulation of tight junction permeability. Physiol. Rev. 2013, 93, 525–569. [Google Scholar] [CrossRef]
- Meoli, L.; Gunzel, D. Channel functions of claudins in the organization of biological systems. Biochim. Biophys. Acta Biomembr. 2020, 1862, 183344. [Google Scholar] [CrossRef]
- Capaldo, C.T. Claudin Barriers on the Brink: How Conflicting Tissue and Cellular Priorities Drive IBD Pathogenesis. Int. J. Mol. Sci. 2023, 24, 8562. [Google Scholar] [CrossRef]
- Schulzke, J.D.; Gunzel, D.; John, L.J.; Fromm, M. Perspectives on tight junction research. Ann. N. Y. Acad. Sci. 2012, 1257, 1–19. [Google Scholar] [CrossRef]
- Rosenthal, R.; Gunzel, D.; Krug, S.M.; Schulzke, J.D.; Fromm, M.; Yu, A.S. Claudin-2-mediated cation and water transport share a common pore. Acta Physiol. 2017, 219, 521–536. [Google Scholar] [CrossRef]
- Monaco, A.; Ovryn, B.; Axis, J.; Amsler, K. The Epithelial Cell Leak Pathway. Int. J. Mol. Sci. 2021, 22, 7677. [Google Scholar] [CrossRef] [PubMed]
- Belardi, B.; Hamkins-Indik, T.; Harris, A.R.; Kim, J.; Xu, K.; Fletcher, D.A. A Weak Link with Actin Organizes Tight Junctions to Control Epithelial Permeability. Dev. Cell 2020, 54, 792–804.e7. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Blikslager, A.T. The Regulation of Intestinal Mucosal Barrier by Myosin Light Chain Kinase/Rho Kinases. Int. J. Mol. Sci. 2020, 21, 3550. [Google Scholar] [CrossRef] [PubMed]
- Varadarajan, S.; Stephenson, R.E.; Miller, A.L. Multiscale dynamics of tight junction remodeling. J. Cell Sci. 2019, 132, jcs229286. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Whitley, C.S.; Haribabu, B.; Jala, V.R. Regulation of Intestinal Barrier Function by Microbial Metabolites. Cell Mol. Gastroenterol. Hepatol. 2021, 11, 1463–1482. [Google Scholar] [CrossRef]
- Di Vincenzo, F.; Del Gaudio, A.; Petito, V.; Lopetuso, L.R.; Scaldaferri, F. Gut microbiota, intestinal permeability, and systemic inflammation: A narrative review. Intern. Emerg. Med. 2023. [Google Scholar] [CrossRef]
- Alam, A.; Neish, A. Role of gut microbiota in intestinal wound healing and barrier function. Tissue Barriers 2018, 6, 1539595. [Google Scholar] [CrossRef] [PubMed]
- Barbara, G.; Barbaro, M.R.; Fuschi, D.; Palombo, M.; Falangone, F.; Cremon, C.; Marasco, G.; Stanghellini, V. Inflammatory and Microbiota-Related Regulation of the Intestinal Epithelial Barrier. Front. Nutr. 2021, 8, 718356. [Google Scholar] [CrossRef]
- Peng, L.; He, Z.; Chen, W.; Holzman, I.R.; Lin, J. Effects of butyrate on intestinal barrier function in a Caco-2 cell monolayer model of intestinal barrier. Pediatr. Res. 2007, 61, 37–41. [Google Scholar] [CrossRef]
- McArthur, S. Regulation of Physiological Barrier Function by the Commensal Microbiota. Life 2023, 13, 396. [Google Scholar] [CrossRef]
- Ma, J.; Piao, X.; Mahfuz, S.; Long, S.; Wang, J. The interaction among gut microbes, the intestinal barrier and short chain fatty acids. Anim. Nutr. 2022, 9, 159–174. [Google Scholar] [CrossRef]
- Saleri, R.; Borghetti, P.; Ravanetti, F.; Cavalli, V.; Ferrari, L.; De Angelis, E.; Andrani, M.; Martelli, P. Effects of different short-chain fatty acids (SCFA) on gene expression of proteins involved in barrier function in IPEC-J2. Porcine Health Manag. 2022, 8, 21. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, D.S.G.; Jensen, B.B.; Theil, P.K.; Nielsen, T.S.; Knudsen, K.E.B.; Purup, S. Effect of butyrate and fermentation products on epithelial integrity in a mucus-secreting human colon cell line. J. Funct. Foods 2018, 40, 9–17. [Google Scholar] [CrossRef]
- Roche, H.M.; Terres, A.M.; Black, I.B.; Gibney, M.J.; Kelleher, D. Fatty acids and epithelial permeability: Effect of conjugated linoleic acid in Caco-2 cells. Gut 2001, 48, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Ren, Q.; Yang, B.; Zhang, H.; Ross, R.P.; Stanton, C.; Chen, H.; Chen, W. c9, t11, c15-CLNA and t9, t11, c15-CLNA from Lactobacillus plantarum ZS2058 Ameliorate Dextran Sodium Sulfate-Induced Colitis in Mice. J. Agric. Food Chem. 2020, 68, 3758–3769. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, H.; Ding, J.; Stanton, C.; Ross, R.P.; Zhao, J.; Zhang, H.; Yang, B.; Chen, W. Bifidobacterium longum Ameliorates Dextran Sulfate Sodium-Induced Colitis by Producing Conjugated Linoleic Acid, Protecting Intestinal Mechanical Barrier, Restoring Unbalanced Gut Microbiota, and Regulating the Toll-Like Receptor-4/Nuclear Factor-kappaB Signaling Pathway. J. Agric. Food Chem. 2021, 69, 14593–14608. [Google Scholar] [CrossRef]
- Shimada, Y.; Kinoshita, M.; Harada, K.; Mizutani, M.; Masahata, K.; Kayama, H.; Takeda, K. Commensal bacteria-dependent indole production enhances epithelial barrier function in the colon. PLoS ONE 2013, 8, e80604. [Google Scholar] [CrossRef]
- Li, J.; Zhang, L.; Wu, T.; Li, Y.; Zhou, X.; Ruan, Z. Indole-3-propionic Acid Improved the Intestinal Barrier by Enhancing Epithelial Barrier and Mucus Barrier. J. Agric. Food Chem. 2021, 69, 1487–1495. [Google Scholar] [CrossRef]
- Zhao, Z.H.; Xin, F.Z.; Xue, Y.; Hu, Z.; Han, Y.; Ma, F.; Zhou, D.; Liu, X.L.; Cui, A.; Liu, Z.; et al. Indole-3-propionic acid inhibits gut dysbiosis and endotoxin leakage to attenuate steatohepatitis in rats. Exp. Mol. Med. 2019, 51, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sarathy, J.; Detloff, S.J.; Ao, M.; Khan, N.; French, S.; Sirajuddin, H.; Nair, T.; Rao, M.C. The Yin and Yang of bile acid action on tight junctions in a model colonic epithelium. Physiol. Rep. 2017, 5, e13294. [Google Scholar] [CrossRef] [PubMed]
- Munch, A.; Strom, M.; Soderholm, J.D. Dihydroxy bile acids increase mucosal permeability and bacterial uptake in human colon biopsies. Scand. J. Gastroenterol. 2007, 42, 1167–1174. [Google Scholar] [CrossRef]
- Keely, S.J.; Steer, C.J.; Lajczak-McGinley, N.K. Ursodeoxycholic acid: A promising therapeutic target for inflammatory bowel diseases? Am. J. Physiol. Gastrointest. Liver Physiol. 2019, 317, G872–G881. [Google Scholar] [CrossRef] [PubMed]
- Rao, J.N.; Xiao, L.; Wang, J.Y. Polyamines in Gut Epithelial Renewal and Barrier Function. Physiology 2020, 35, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Xiao, L.; Rao, J.N.; Zou, T.; Liu, L.; Bellavance, E.; Gorospe, M.; Wang, J.Y. JunD represses transcription and translation of the tight junction protein zona occludens-1 modulating intestinal epithelial barrier function. Mol. Biol. Cell 2008, 19, 3701–3712. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.X.; Wang, P.Y.; Rao, J.N.; Zou, T.; Liu, L.; Xiao, L.; Gorospe, M.; Wang, J.Y. Chk2-dependent HuR phosphorylation regulates occludin mRNA translation and epithelial barrier function. Nucleic Acids Res. 2011, 39, 8472–8487. [Google Scholar] [CrossRef]
- Guo, X.; Rao, J.N.; Liu, L.; Zou, T.T.; Turner, D.J.; Bass, B.L.; Wang, J.Y. Regulation of adherens junctions and epithelial paracellular permeability: A novel function for polyamines. Am. J. Physiol. Cell Physiol. 2003, 285, C1174–C1187. [Google Scholar] [CrossRef]
- Liu, L.; Guo, X.; Rao, J.N.; Zou, T.; Xiao, L.; Yu, T.; Timmons, J.A.; Turner, D.J.; Wang, J.Y. Polyamines regulate E-cadherin transcription through c-Myc modulating intestinal epithelial barrier function. Am. J. Physiol. Cell Physiol. 2009, 296, C801–C810. [Google Scholar] [CrossRef] [PubMed]
- Gu, M.J.; Song, S.K.; Lee, I.K.; Ko, S.; Han, S.E.; Bae, S.; Ji, S.Y.; Park, B.C.; Song, K.D.; Lee, H.K.; et al. Barrier protection via Toll-like receptor 2 signaling in porcine intestinal epithelial cells damaged by deoxynivalnol. Vet. Res. 2016, 47, 25. [Google Scholar] [CrossRef] [PubMed]
- Cario, E.; Gerken, G.; Podolsky, D.K. Toll-like receptor 2 controls mucosal inflammation by regulating epithelial barrier function. Gastroenterology 2007, 132, 1359–1374. [Google Scholar] [CrossRef] [PubMed]
- Zhan, L.; Zheng, J.; Meng, J.; Fu, D.; Pang, L.; Ji, C. Toll-like receptor 4 deficiency alleviates lipopolysaccharide-induced intestinal barrier dysfunction. Biomed. Pharmacother. 2022, 155, 113778. [Google Scholar] [CrossRef] [PubMed]
- Zou, P.; Yang, F.; Ding, Y.; Zhang, D.; Liu, Y.; Zhang, J.; Wu, D.; Wang, Y. Lipopolysaccharide downregulates the expression of ZO-1 protein through the Akt pathway. BMC Infect. Dis. 2022, 22, 774. [Google Scholar] [CrossRef]
- Lopetuso, L.R.; Jia, R.; Wang, X.M.; Jia, L.G.; Petito, V.; Goodman, W.A.; Meddings, J.B.; Cominelli, F.; Reuter, B.K.; Pizarro, T.T. Epithelial-specific Toll-like Receptor (TLR)5 Activation Mediates Barrier Dysfunction in Experimental Ileitis. Inflamm. Bowel Dis. 2017, 23, 392–403. [Google Scholar] [CrossRef]
- O’Hara, J.R.; Buret, A.G. Mechanisms of intestinal TJ disruption during infection. Front. Biosci. 2008, 13, 7008–7021. [Google Scholar] [CrossRef] [PubMed]
- Paradis, T.; Begue, H.; Basmaciyan, L.; Dalle, F.; Bon, F. Tight Junctions as a Key for Pathogens Invasion in Intestinal Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 2506. [Google Scholar] [CrossRef]
- McKay, D.M.; Shute, A.; Lopes, F. Helminths and intestinal barrier function. Tissue Barriers 2017, 5, e1283385. [Google Scholar] [CrossRef]
- Basmaciyan, L.; Bon, F.; Paradis, T.; Lapaquette, P.; Dalle, F. Candida Albicans Interactions with the Host: Crossing the Intestinal Epithelial Barrier. Tissue Barriers 2019, 7, 1612661. [Google Scholar] [CrossRef]
- Allert, S. Candida albincans induced epithelial damage mediates translocation through intestinal barrier. Am. Soc. Microbiol. 2018, 9. [Google Scholar] [CrossRef]
- Labarta-Bajo, L.; Nilsen, S.P.; Humphrey, G.; Schwartz, T.; Sanders, K.; Swafford, A.; Knight, R.; Turner, J.R.; Zuniga, E.I. Type I IFNs and CD8 T cells increase intestinal barrier permeability after chronic viral infection. J. Exp. Med. 2020, 217, e20192276. [Google Scholar] [CrossRef] [PubMed]
- English, J.; Connolly, L.; Stewart, L.D. Increased Intestinal Permeability: An Avenue for the Development of Autoimmune Disease? Expo. Health 2023. [Google Scholar] [CrossRef]
- Berkes, J.; Viswanathan, V.K.; Savkovic, S.D.; Hecht, G. Intestinal epithelial responses to enteric pathogens. Gut 2003, 52, 439–451. [Google Scholar] [CrossRef]
- Allain, T.; Amat, C.B.; Motta, J.P.; Manko, A.; Buret, A.G. Interactions of Giardia sp. with the intestinal barrier: Epithelium, mucus, and microbiota. Tissue Barriers 2017, 5, e1274354. [Google Scholar] [CrossRef] [PubMed]
- Harrer, A.; Bucker, R.; Boehm, M.; Zarzecka, U.; Tegtmeyer, N.; Sticht, H.; Schulzke, J.D.; Backert, S. Campylobacter jejuni enters gut epithelial cells and impairs intestinal barrier function through cleavage of occludin by serine protease HtrA. Gut Pathog. 2019, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Boehm, M.; Simson, D.; Escher, U.; Schmidt, A.M.; Bereswill, S.; Tegtmeyer, N.; Backert, S.; Heimesaat, M.M. Function of Serine Protease HtrA in the Lifecycle of the Foodborne Pathogen Campylobacter jejuni. Eur. J. Microbiol. Immunol. 2018, 8, 70–77. [Google Scholar] [CrossRef]
- Roxas, J.L.; Viswanathan, V.K. Modulation of Intestinal Paracellular Transport by Bacterial Pathogens. Compr. Physiol. 2018, 8, 823–842. [Google Scholar] [CrossRef] [PubMed]
- Elmi, A.; Nasher, F.; Jagatia, H.; Gundogdu, O.; Bajaj-Elliott, M.; Wren, B.; Dorrell, N. Campylobacter jejuni outer membrane vesicle-associated proteolytic activity promotes bacterial invasion by mediating cleavage of intestinal epithelial cell E-cadherin and occludin. Cell Microbiol. 2016, 18, 561–572. [Google Scholar] [CrossRef]
- Wu, Z.; Nybom, P.; Magnusson, K.-E. Distinct effects of Vibrio cholerae haemagglutinin-protease on the structure and localization of the tight junction-associated proteins occludin and ZO1. Cell. Microbiol. 2000, 2, 11–17. [Google Scholar] [CrossRef]
- Popoff, M.R. Multifaceted interactions of bacterial toxins with the gastrointestinal mucosa. Future Microbiol. 2011, 6, 763–797. [Google Scholar] [CrossRef]
- Eichner, M.; Augustin, C.; Fromm, A.; Piontek, A.; Walther, W.; Bucker, R.; Fromm, M.; Krause, G.; Schulzke, J.D.; Gunzel, D.; et al. In Colon Epithelia, Clostridium perfringens Enterotoxin Causes Focal Leaks by Targeting Claudins Which are Apically Accessible Due to Tight Junction Derangement. J. Infect. Dis. 2017, 217, 147–157. [Google Scholar] [CrossRef]
- Cuellar, P.; Hernandez-Nava, E.; Garcia-Rivera, G.; Chavez-Munguia, B.; Schnoor, M.; Betanzos, A.; Orozco, E. Entamoeba histolytica EhCP112 Dislocates and Degrades Claudin-1 and Claudin-2 at Tight Junctions of the Intestinal Epithelium. Front. Cell Infect. Microbiol. 2017, 7, 372. [Google Scholar] [CrossRef] [PubMed]
- Sears, C.L.; Kaper, J.B. Enteric Bacterial Toxins- Mechanisms of Action and Linkage to Intestinal Secretion. Am. Soc. Microbiol. 1996, 60, 167–215. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A.; Baudry, B.; Pumplin, D.W.; Wasserman, S.S.; Tall, B.D.; Ketley, J.M.; Kaper, J.B. Vibrio cholerae produces a second enterotoxin, which affects intestinal tight junctions. Proc. Natl. Acad. Sci. USA 1991, 88, 5242–5246. [Google Scholar] [CrossRef] [PubMed]
- Perez-Reytor, D.; Jana, V.; Pavez, L.; Navarrete, P.; Garcia, K. Accessory Toxins of Vibrio Pathogens and Their Role in Epithelial Disruption during Infection. Front. Microbiol. 2018, 9, 2248. [Google Scholar] [CrossRef] [PubMed]
- Forte, L.R.; Thorne, P.K.; Eber, S.L.; Krause, W.J.; Freeman, R.H.; Francis, S.H.; Corbin, J.D. Stimulation of intestinal Cl− transport by heat-stable enterotoxin: Activation of cAMP-dependent protein kinase by cGMP. Am. J. Physiol. Cell Physiol. 1992, 263, C607–C615. [Google Scholar] [CrossRef]
- Sarkar, P.; Saha, T.; Sheikh, I.A.; Chakraborty, S.; Aoun, J.; Chakrabarti, M.K.; Rajendran, V.M.; Ameedn, N.A.; Dutta, S.; Hoque, K.M. Zinc ameliorates Intestinal Barrieri Dysfunction in Shigellosis by Reinstating Claudin-2 and -4 on the membranes. Am. J. Physiol. Gastrointest. Liver Physiol. 2019, 316, G229–G246. [Google Scholar] [CrossRef]
- Deshpande, N.P.; Wilkins, M.R.; Castano-Rodriguez, N.; Bainbridge, E.; Sodhi, N.; Riordan, S.M.; Mitchell, H.M.; Kaakoush, N.O. Campylobacter concisus pathotypes induce distinct global responses in intestinal epithelial cells. Sci. Rep. 2016, 6, 34288. [Google Scholar] [CrossRef]
- Ngendahayo Mukiza, C.; Dubreuil, J.D. Escherichia coli heat-stable toxin b impairs intestinal epithelial barrier function by altering tight junction proteins. Infect. Immun. 2013, 81, 2819–2827. [Google Scholar] [CrossRef]
- Moser, L.A.; Carter, M.; Schultz-Cherry, S. Astrovirus increases epithelial barrier permeability independently of viral replication. J. Virol. 2007, 81, 11937–11945. [Google Scholar] [CrossRef]
- Barbieri, J.T.; Riese, M.J.; Aktories, K. Bacterial toxins that modify the actin cytoskeleton. Annu. Rev. Cell Dev. Biol. 2002, 18, 315–344. [Google Scholar] [CrossRef]
- Bishop, A.L.; Hall, A. Rho GTPases and their effector proteins. Biochem. J. 2000, 384, 241–255. [Google Scholar] [CrossRef]
- LaRock, D.L.; Chaudhary, A.; Miller, S.I. Salmonellae interactions with host processes. Nat. Rev. Microbiol. 2015, 13, 191–205. [Google Scholar] [CrossRef] [PubMed]
- Kaakoush, N.O.; Man, S.M.; Lamb, S.; Raftery, M.J.; Wilkins, M.R.; Kovach, Z.; Mitchell, H. The secretome of Campylobacter concisus. FEBS J. 2010, 277, 1606–1617. [Google Scholar] [CrossRef] [PubMed]
- Torres-Flores, J.M.; Arias, C.F. Tight Junctions Go Viral! Viruses 2015, 7, 5145–5154. [Google Scholar] [CrossRef]
- Coyne, C.B.; Bergelson, J.M. Virus-induced Abl and Fyn kinase signals permit coxsackievirus entry through epithelial tight junctions. Cell 2006, 124, 119–131. [Google Scholar] [CrossRef]
- Cohen, C.J.; Shieh, J.T.C.; Pickles, R.J.; Okegawa, T.; HSLEH, J.-T.; Bergelson, H.M. The coxsackievirus and adenovirus receptor is a transmembrane component of the tight junction. Proc. Natl. Acad. Sci. USA 2001, 98, 15191–15196. [Google Scholar] [CrossRef]
- Dickman, K.G.; Hempson, S.J.; Anderson, J.; Lippe, S.; Zhao, L.; Burakoff, R.; Shaw, R.D. Rotavirus alters paracellular permeability and energy metabolism in Caco-2 cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 279, G757–G766. [Google Scholar] [CrossRef]
- Poritz, L.S.; Harris, L.R., 3rd; Kelly, A.A.; Koltun, W.A. Increase in the tight junction protein claudin-1 in intestinal inflammation. Dig. Dis. Sci. 2011, 56, 2802–2809. [Google Scholar] [CrossRef]
- Weber, C.R.; Nalle, S.C.; Tretiakova, M.; Rubin, D.T.; Turner, J.R. Claudin-1 and claudin-2 expression is elevated in inflammatory bowel disease and may contribute to early neoplastic transformation. Lab. Investig. 2008, 88, 1110–1120. [Google Scholar] [CrossRef]
- Soroosh, A.; Rankin, C.R.; Polytarchou, C.; Lokhandwala, Z.A.; Patel, A.; Chang, L.; Pothoulakis, C.; Iliopoulos, D.; Padua, D.M. miR-24 Is Elevated in Ulcerative Colitis Patients and Regulates Intestinal Epithelial Barrier Function. Am. J. Pathol. 2019, 189, 1763–1774. [Google Scholar] [CrossRef]
- Schultsz, C.; Van Den Berg, F.M.; Ten Kate, F.W.; Tytgat, G.N.; Dankert, J. The intestinal mucus layer from patients with inflammatory bowel disease harbors high numbers of bacteria compared with controls. Gastroenterology 1999, 117, 1089–1097. [Google Scholar] [CrossRef]
- Liu, H.; Hong, X.L.; Sun, T.T.; Huang, X.W.; Wang, J.L.; Xiong, H. Fusobacterium nucleatum exacerbates colitis by damaging epithelial barriers and inducing aberrant inflammation. J. Dig. Dis. 2020, 21, 385–398. [Google Scholar] [CrossRef]
- Mills, R.H.; Dulai, P.S.; Vazquez-Baeza, Y.; Sauceda, C.; Daniel, N.; Gerner, R.R.; Batachari, L.E.; Malfavon, M.; Zhu, Q.; Weldon, K.; et al. Multi-omics analyses of the ulcerative colitis gut microbiome link Bacteroides vulgatus proteases with disease severity. Nat. Microbiol. 2022, 7, 262–276. [Google Scholar] [CrossRef]
- Xiao, Y.; Lian, H.; Zhong, X.S.; Krishnachaitanya, S.S.; Cong, Y.; Dashwood, R.H.; Savidge, T.C.; Powell, D.W.; Liu, X.; Li, Q. Matrix metalloproteinase 7 contributes to intestinal barrier dysfunction by degrading tight junction protein Claudin-7. Front. Immunol. 2022, 13, 1020902. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Price, J.; Arze, C.; Ananthakrishnan, A.N.; Schirmer, M.; Avila-Pacheco, J.; Poon, T.W.; Andrews, E.; Ajami, N.J.; Bonham, K.S.; Brislawn, C.J.; et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature 2019, 569, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Jiao, T.; Liu, W.; Luo, Y.; Wang, J.; Guo, X.; Tong, X.; Lin, Z.; Sun, C.; Wang, K.; et al. Hepatic cytochrome P450 8B1 and cholic acid potentiate intestinal epithelial injury in colitis by suppressing intestinal stem cell renewal. Cell Stem Cell 2022, 29, 1366–1381.e9. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Yue, J.; Zhang, Y.; Shi, C.; Odenwald, M.; Liang, W.G.; Wei, Q.; Goel, A.; Gou, X.; Zhang, J.; et al. ACF7 regulates inflammatory colitis and intestinal wound response by orchestrating tight junction dynamics. Nat. Commun. 2017, 8, 15375. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Martinez-Sanchez, L.D.C.; Ngo, P.A.; Pradhan, R.; Becker, L.S.; Boehringer, D.; Soteriou, D.; Kubankova, M.; Schweitzer, C.; Koch, T.; Thonn, V.; et al. Epithelial RAC1-dependent cytoskeleton dynamics controls cell mechanics, cell shedding and barrier integrity in intestinal inflammation. Gut 2023, 72, 275–294. [Google Scholar] [CrossRef] [PubMed]
- Franke, A.; McGovern, D.P.; Barrett, J.C.; Wang, K.; Radford-Smith, G.L.; Ahmad, T.; Lees, C.W.; Balschun, T.; Lee, J.; Roberts, R.; et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat. Genet. 2010, 42, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Hampe, J.; Franke, A.; Rosenstiel, P.; Till, A.; Teuber, M.; Huse, K.; Albrecht, M.; Mayr, G.; De La Vega, F.M.; Briggs, J.; et al. A genome-wide association scan of nonsynonymous SNPs identifies a susceptibility variant for Crohn disease in ATG16L1. Nat. Genet. 2007, 39, 207–211. [Google Scholar] [CrossRef]
- Rioux, J.D.; Xavier, R.J.; Taylor, K.D.; Silverberg, M.S.; Goyette, P.; Huett, A.; Green, T.; Kuballa, P.; Barmada, M.M.; Datta, L.W.; et al. Genome-wide association study identifies new susceptibility loci for Crohn disease and implicates autophagy in disease pathogenesis. Nat. Genet. 2007, 39, 596–604. [Google Scholar] [CrossRef]
- Prescott, N.J.; Fisher, S.A.; Franke, A.; Hampe, J.; Onnie, C.M.; Soars, D.; Bagnall, R.; Mirza, M.M.; Sanderson, J.; Forbes, A.; et al. A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn’s disease and is independent of CARD15 and IBD5. Gastroenterology 2007, 132, 1665–1671. [Google Scholar] [CrossRef]
- Parkes, M.; Barrett, J.C.; Prescott, N.J.; Tremelling, M.; Anderson, C.A.; Fisher, S.A.; Roberts, R.G.; Nimmo, E.R.; Cummings, F.R.; Soars, D.; et al. Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn’s disease susceptibility. Nat. Genet. 2007, 39, 830–832. [Google Scholar] [CrossRef]
- Rufini, S.; Ciccacci, C.; Di Fusco, D.; Ruffa, A.; Pallone, F.; Novelli, G.; Biancone, L.; Borgiani, P. Autophagy and inflammatory bowel disease: Association between variants of the autophagy-related IRGM gene and susceptibility to Crohn’s disease. Dig. Liver Dis. 2015, 47, 744–750. [Google Scholar] [CrossRef]
- Henckaerts, L.; Cleynen, I.; Brinar, M.; John, J.M.; Van Steen, K.; Rutgeerts, P.; Vermeire, S. Genetic variation in the autophagy gene ULK1 and risk of Crohn’s disease. Inflamm. Bowel Dis. 2011, 17, 1392–1397. [Google Scholar] [CrossRef]
- Hui, K.Y.; Fernandez-Hernandez, H.; Hu, J.; Schaffner, A.; Pankratz, N.; Hsu, N.Y.; Chuang, L.S.; Carmi, S.; Villaverde, N.; Li, X.; et al. Functional variants in the LRRK2 gene confer shared effects on risk for Crohn’s disease and Parkinson’s disease. Sci. Transl. Med. 2018, 10, eaai7795. [Google Scholar] [CrossRef]
- Liu, M.; Sun, T.; Li, N.; Peng, J.; Fu, D.; Li, W.; Li, L.; Gao, W.Q. BRG1 attenuates colonic inflammation and tumorigenesis through autophagy-dependent oxidative stress sequestration. Nat. Commun. 2019, 10, 4614. [Google Scholar] [CrossRef] [PubMed]
- Tajik, N.; Frech, M.; Schulz, O.; Schalter, F.; Lucas, S.; Azizov, V.; Durholz, K.; Steffen, F.; Omata, Y.; Rings, A.; et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat. Commun. 2020, 11, 1995. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wright, K.; Davis, J.M.; Jeraldo, P.; Marietta, E.V.; Murray, J.; Nelson, H.; Matteson, E.L.; Taneja, V. An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Med. 2016, 8, 43. [Google Scholar] [CrossRef] [PubMed]
- Chiang, H.I.; Li, J.R.; Liu, C.C.; Liu, P.Y.; Chen, H.H.; Chen, Y.M.; Lan, J.L.; Chen, D.Y. An Association of Gut Microbiota with Different Phenotypes in Chinese Patients with Rheumatoid Arthritis. J. Clin. Med. 2019, 8, 1770. [Google Scholar] [CrossRef] [PubMed]
- Scher, J.U.; Ubeda, C.; Artacho, A.; Attur, M.; Isaac, S.; Reddy, S.M.; Marmon, S.; Neimann, A.; Brusca, S.; Patel, T.; et al. Decreased bacterial diversity characterizes the altered gut microbiota in patients with psoriatic arthritis, resembling dysbiosis in inflammatory bowel disease. Arthritis Rheumatol. 2015, 67, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Costello, M.E.; Ciccia, F.; Willner, D.; Warrington, N.; Robinson, P.C.; Gardiner, B.; Marshall, M.; Kenna, T.J.; Triolo, G.; Brown, M.A. Brief Report: Intestinal Dysbiosis in Ankylosing Spondylitis. Arthritis Rheumatol. 2015, 67, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.; Zheng, Z.; Shao, T.; Liu, L.; Xie, Z.; Le Chatelier, E.; He, Z.; Zhong, W.; Fan, Y.; Zhang, L.; et al. Quantitative metagenomics reveals unique gut microbiome biomarkers in ankylosing spondylitis. Genome Biol. 2017, 18, 142. [Google Scholar] [CrossRef]
- Ciccia, F.; Guggino, G.; Rizzo, A.; Alessandro, R.; Luchetti, M.M.; Milling, S.; Saieva, L.; Cypers, H.; Stampone, T.; Di Benedetto, P.; et al. Dysbiosis and zonulin upregulation alter gut epithelial and vascular barriers in patients with ankylosing spondylitis. Ann. Rheum. Dis. 2017, 76, 1123–1132. [Google Scholar] [CrossRef]
- Thim-Uam, A.; Surawut, S.; Issara-Amphorn, J.; Jaroonwitchawan, T.; Hiengrach, P.; Chatthanathon, P.; Wilantho, A.; Somboonna, N.; Palaga, T.; Pisitkun, P.; et al. Leaky-gut enhanced lupus progression in the Fc gamma receptor-IIb deficient and pristane-induced mouse models of lupus. Sci. Rep. 2020, 10, 777. [Google Scholar] [CrossRef]
- Suzuki, T.; Hara, H. Dietary fat and bile juice, but not obesity, are responsible for the increase in small intestinal permeability induced through the suppression of tight junction protein expression in LETO and OLETF rats. Nutr. Metab. 2010, 7, 19. [Google Scholar] [CrossRef]
- Thaiss, C.A.; Levy, M.; Grosheva, I.; Zheng, D.; Soffer, E.; Blacher, E.; Braverman, S.; Tengeler, A.C.; Barak, O.; Elazar, M.; et al. Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. Science 2018, 359, 1376–1383. [Google Scholar] [CrossRef]
- Do, M.H.; Lee, E.; Oh, M.J.; Kim, Y.; Park, H.Y. High-Glucose or -Fructose Diet Cause Changes of the Gut Microbiota and Metabolic Disorders in Mice without Body Weight Change. Nutrients 2018, 10, 761. [Google Scholar] [CrossRef]
- Pedersen, C.; Ijaz, U.Z.; Gallagher, E.; Horton, F.; Ellis, R.J.; Jaiyeola, E.; Duparc, T.; Russell-Jones, D.; Hinton, P.; Cani, P.D.; et al. Fecal Enterobacteriales enrichment is associated with increased in vivo intestinal permeability in humans. Physiol. Rep. 2018, 6, e13649. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Yoshinaga, N.; Tanabe, S. Interleukin-6 (IL-6) regulates claudin-2 expression and tight junction permeability in intestinal epithelium. J. Biol. Chem. 2011, 286, 31263–31271. [Google Scholar] [CrossRef]
- Scalavino, V.; Piccinno, E.; Lacalamita, A.; Tafaro, A.; Armentano, R.; Giannelli, G.; Serino, G. miR-195-5p Regulates Tight Junctions Expression via Claudin-2 Downregulation in Ulcerative Colitis. Biomedicines 2022, 10, 919. [Google Scholar] [CrossRef]
- Yoshimatsu, Y.; Sujino, T.; Miyamoto, K.; Harada, Y.; Tanemoto, S.; Ono, K.; Umeda, S.; Yoshida, K.; Teratani, T.; Suzuki, T.; et al. Aryl hydrocarbon receptor signals in epithelial cells govern the recruitment and location of Helios(+) Tregs in the gut. Cell Rep. 2022, 39, 110773. [Google Scholar] [CrossRef]
- Maronek, M.; Marafini, I.; Gardlik, R.; Link, R.; Troncone, E.; Monteleone, G. Metalloproteinases in Inflammatory Bowel Diseases. J. Inflamm. Res. 2021, 14, 1029–1041. [Google Scholar] [CrossRef]
- van der Lelie, D.; Oka, A.; Taghavi, S.; Umeno, J.; Fan, T.J.; Merrell, K.E.; Watson, S.D.; Ouellette, L.; Liu, B.; Awoniyi, M.; et al. Rationally designed bacterial consortia to treat chronic immune-mediated colitis and restore intestinal homeostasis. Nat. Commun. 2021, 12, 3105. [Google Scholar] [CrossRef] [PubMed]
- Michaudel, C.; Danne, C.; Agus, A.; Magniez, A.; Aucouturier, A.; Spatz, M.; Lefevre, A.; Kirchgesner, J.; Rolhion, N.; Wang, Y.; et al. Rewiring the altered tryptophan metabolism as a novel therapeutic strategy in inflammatory bowel diseases. Gut 2023, 72, 1296–1307. [Google Scholar] [CrossRef] [PubMed]
- Naydenov, N.G.; Feygin, A.; Wang, D.; Kuemmerle, J.F.; Harris, G.; Conti, M.A.; Adelstein, R.S.; Ivanov, A.I. Nonmuscle Myosin IIA Regulates Intestinal Epithelial Barrier in vivo and Plays a Protective Role during Experimental Colitis. Sci. Rep. 2016, 6, 24161. [Google Scholar] [CrossRef]
- Kang, S.; Kim, J.; Park, A.; Koh, M.; Shin, W.; Park, G.; Lee, T.A.; Kim, H.J.; Han, H.; Kim, Y.; et al. TRIM40 is a pathogenic driver of inflammatory bowel disease subverting intestinal barrier integrity. Nat. Commun. 2023, 14, 700. [Google Scholar] [CrossRef]
- Lyko, F. The DNA methyltransferase family: A versatile toolkit for epigenetic regulation. Nat. Rev. Genet. 2018, 19, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Fazio, A.; Bordoni, D.; Kuiper, J.W.P.; Weber-Stiehl, S.; Stengel, S.T.; Arnold, P.; Ellinghaus, D.; Ito, G.; Tran, F.; Messner, B.; et al. DNA methyltransferase 3A controls intestinal epithelial barrier function and regeneration in the colon. Nat. Commun. 2022, 13, 6266. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.X.; Lee, J.S.; Campbell, E.L.; Colgan, S.P. Microbiota-derived butyrate dynamically regulates intestinal homeostasis through regulation of actin-associated protein synaptopodin. Proc. Natl. Acad. Sci. USA 2020, 117, 11648–11657. [Google Scholar] [CrossRef] [PubMed]
- Foerster, E.G.; Mukherjee, T.; Cabral-Fernandes, L.; Rocha, J.D.B.; Girardin, S.E.; Philpott, D.J. How autophagy controls the intestinal epithelial barrier. Autophagy 2022, 18, 86–103. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Li, L.; Li, T.; Sun, L.; Yin, J.; Guan, H.; Wang, L.; Zhu, H.; Xu, P.; Fan, X.; et al. SCFAs induce autophagy in intestinal epithelial cells and relieve colitis by stabilizing HIF-1alpha. J. Mol. Med. 2020, 98, 1189–1202. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Peng, K.; Yu, H.; Wang, Z.; Xia, S.; Xiao, S.; Tian, D.; Vallance, B.A.; Yu, Q. Autotaxin (ATX) inhibits autophagy leading to exaggerated disruption of intestinal epithelial barrier in colitis. Biochim. Biophys. Acta Mol. Basis Dis. 2023, 1869, 166647. [Google Scholar] [CrossRef]
- Wang, Y.; Wei, J.; Zhang, W.; Doherty, M.; Zhang, Y.; Xie, H.; Li, W.; Wang, N.; Lei, G.; Zeng, C. Gut dysbiosis in rheumatic diseases: A systematic review and meta-analysis of 92 observational studies. EBioMedicine 2022, 80, 104055. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi-Roodsaz, S.; Joosten, L.A.; Koenders, M.I.; Devesa, I.; Roelofs, M.F.; Radstake, T.R.; Heuvelmans-Jacobs, M.; Akira, S.; Nicklin, M.J.; Ribeiro-Dias, F.; et al. Stimulation of TLR2 and TLR4 differentially skews the balance of T cells in a mouse model of arthritis. J. Clin. Investig. 2008, 118, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.J.; Ivanov, I.I.; Darce, J.; Hattori, K.; Shima, T.; Umesaki, Y.; Littman, D.R.; Benoist, C.; Mathis, D. Gut-residing segmented filamentous bacteria drive autoimmune arthritis via T helper 17 cells. Immunity 2010, 32, 815–827. [Google Scholar] [CrossRef]
- Chriswell, M.E.; Lefferts, A.R.; Clay, M.R.; Hsu, A.R.; Seifert, J.; Feser, M.L.; Rims, C.; Bloom, M.S.; Bemis, E.A.; Liu, S.; et al. Clonal IgA and IgG autoantibodies from individuals at risk for rheumatoid arthritis identify an arthritogenic strain of Subdoligranulum. Sci. Transl. Med. 2022, 14, eabn5166. [Google Scholar] [CrossRef]
- Romero-Figueroa, M.D.S.; Ramirez-Duran, N.; Montiel-Jarquin, A.J.; Horta-Baas, G. Gut-joint axis: Gut dysbiosis can contribute to the onset of rheumatoid arthritis via multiple pathways. Front. Cell Infect. Microbiol. 2023, 13, 1092118. [Google Scholar] [CrossRef] [PubMed]
- Matei, D.E.; Menon, M.; Alber, D.G.; Smith, A.M.; Nedjat-Shokouhi, B.; Fasano, A.; Magill, L.; Duhlin, A.; Bitoun, S.; Gleizes, A.; et al. Intestinal barrier dysfunction plays an integral role in arthritis pathology and can be targeted to ameliorate disease. Med 2021, 2, 864–883.e9. [Google Scholar] [CrossRef] [PubMed]
- van der Heijden, I.M.; Wilbrink, B.; Tchetverikov, I.; Schrijver, I.A.; Schouls, L.M.; Hazenberg, M.P.; Breedveld, F.C.; Tak, P.P. Presence of bacterial DNA and bacterial peptidoglycans in joints of patients with rheumatoid arthritis and other arthritides. Arthritis Rheum. 2000, 43, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, B.; Li, S.; Yang, L.; Zhu, D.; Wang, Y.; Wang, H.; Wang, T.; Shi, B.; Gai, Z.; et al. Detection and characterization of bacterial nucleic acids in culture-negative synovial tissue and fluid samples from rheumatoid arthritis or osteoarthritis patients. Sci. Rep. 2018, 8, 14305. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.; Zhao, Y.; Cui, Y.; Zhong, C.; Zha, Y.; Li, S.; Cao, G.; Li, M.; Zhang, L.; Ning, K.; et al. Stage-specific roles of microbial dysbiosis and metabolic disorders in rheumatoid arthritis. Ann. Rheum. Dis. 2022, 81, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Scher, J.U.; Sczesnak, A.; Longman, R.S.; Segata, N.; Ubeda, C.; Bielski, C.; Rostron, T.; Cerundolo, V.; Pamer, E.G.; Abramson, S.B.; et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife 2013, 2, e01202. [Google Scholar] [CrossRef]
- Pianta, A.; Arvikar, S.; Strle, K.; Drouin, E.E.; Wang, Q.; Costello, C.E.; Steere, A.C. Evidence of the Immune Relevance of Prevotella copri, a Gut Microbe, in Patients with Rheumatoid Arthritis. Arthritis Rheumatol. 2017, 69, 964–975. [Google Scholar] [CrossRef]
- Ruiz-Limon, P.; Mena-Vazquez, N.; Moreno-Indias, I.; Manrique-Arija, S.; Lisbona-Montanez, J.M.; Cano-Garcia, L.; Tinahones, F.J.; Fernandez-Nebro, A. Collinsella is associated with cumulative inflammatory burden in an established rheumatoid arthritis cohort. Biomed. Pharmacother. 2022, 153, 113518. [Google Scholar] [CrossRef]
- El Menofy, N.G.; Ramadan, M.; Abdelbary, E.R.; Ibrahim, H.G.; Azzam, A.I.; Ghit, M.M.; Ezz, A.S.; Gazar, Y.A.; Salah, M. Bacterial Compositional Shifts of Gut Microbiomes in Patients with Rheumatoid Arthritis in Association with Disease Activity. Microorganisms 2022, 10, 1820. [Google Scholar] [CrossRef]
- Srutkova, D.; Schwarzer, M.; Hudcovic, T.; Zakostelska, Z.; Drab, V.; Spanova, A.; Rittich, B.; Kozakova, H.; Schabussova, I. Bifidobacterium longum CCM 7952 Promotes Epithelial Barrier Function and Prevents Acute DSS-Induced Colitis in Strictly Strain-Specific Manner. PLoS ONE 2015, 10, e0134050. [Google Scholar] [CrossRef]
- Zhao, L.; Xie, Q.; Evivie, S.E.; Yue, Y.; Yang, H.; Lv, X.; Liu, F.; Li, B.; Huo, G. Bifidobacterium longum subsp. longum K5 alleviates inflammatory response and prevents intestinal barrier injury induced by LPS in vitro based on comparative genomics. J. Funct. Foods 2022, 92, 105030. [Google Scholar] [CrossRef]
- Li, Y.; Lv, L.; Ye, J.; Fang, D.; Shi, D.; Wu, W.; Wang, Q.; Wu, J.; Yang, L.; Bian, X.; et al. Bifidobacterium adolescentis CGMCC 15058 alleviates liver injury, enhances the intestinal barrier and modifies the gut microbiota in D-galactosamine-treated rats. Appl. Microbiol. Biotechnol. 2019, 103, 375–393. [Google Scholar] [CrossRef]
- Fan, L.; Qi, Y.; Qu, S.; Chen, X.; Li, A.; Hendi, M.; Xu, C.; Wang, L.; Hou, T.; Si, J.; et al. B. adolescentis ameliorates chronic colitis by regulating Treg/Th2 response and gut microbiota remodeling. Gut Microbes 2021, 13, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Laval, L.; Martin, R.; Natividad, J.N.; Chain, F.; Miquel, S.; Desclee de Maredsous, C.; Capronnier, S.; Sokol, H.; Verdu, E.F.; van Hylckama Vlieg, J.E.; et al. Lactobacillus rhamnosus CNCM I-3690 and the commensal bacterium Faecalibacterium prausnitzii A2-165 exhibit similar protective effects to induced barrier hyper-permeability in mice. Gut Microbes 2015, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fan, Z.; Yang, B.; Ross, R.P.; Stanton, C.; Shi, G.; Zhao, J.; Zhang, H.; Chen, W. Protective effects of Bifidobacterium adolescentis on collagen-induced arthritis in rats depend on timing of administration. Food Funct. 2020, 11, 4499–4511. [Google Scholar] [CrossRef] [PubMed]
- Audo, R.; Sanchez, P.; Rivière, B.; Mielle, J.; Tan, J.; Lukas, C.; Macia, L.; Morel, J.; Immediato Daien, C. Rheumatoid arthritis is associated with increased gut permeability and bacterial translocation that are reversed by inflammation control. Rheumatology 2023, 62, 1264–1271. [Google Scholar] [CrossRef] [PubMed]
- Asquith, M.; Sternes, P.R.; Costello, M.E.; Karstens, L.; Diamond, S.; Martin, T.M.; Li, Z.; Marshall, M.S.; Spector, T.D.; le Cao, K.A.; et al. HLA Alleles Associated with Risk of Ankylosing Spondylitis and Rheumatoid Arthritis Influence the Gut Microbiome. Arthritis Rheumatol. 2019, 71, 1642–1650. [Google Scholar] [CrossRef]
- Taurog, J.D.; Richardson, J.A.; Croft, J.T.; Simmons, W.A.; Zhou, M.; Fernandez-Sueiro, J.L.; Balish, E.; Hammer, R.E. The germfree state prevents development of gut and joint inflammatory disease in HLA-B27 transgenic rats. J. Exp. Med. 1994, 180, 2359–2364. [Google Scholar] [CrossRef]
- Rath, H.C.; Herfarth, H.H.; Ikeda, J.S.; Grenther, W.B.; Hamm, T.E., Jr.; Balish, E.; Taurog, J.D.; Hammer, R.E.; Wilson, K.H.; Sartor, R.B. Normal luminal bacteria, especially Bacteroides species, mediate chronic colitis, gastritis, and arthritis in HLA-B27/human beta2 microglobulin transgenic rats. J. Clin. Investig. 1996, 98, 945–953. [Google Scholar] [CrossRef]
- Shen, J.; Yang, L.; You, K.; Chen, T.; Su, Z.; Cui, Z.; Wang, M.; Zhang, W.; Liu, B.; Zhou, K.; et al. Indole-3-Acetic Acid Alters Intestinal Microbiota and Alleviates Ankylosing Spondylitis in Mice. Front. Immunol. 2022, 13, 762580. [Google Scholar] [CrossRef]
- Gisbert, J.P.; Bermejo, F.; Perez-Calle, J.L.; Taxonera, C.; Vera, I.; McNicholl, A.G.; Algaba, A.; Lopez, P.; Lopez-Palacios, N.; Calvo, M.; et al. Fecal calprotectin and lactoferrin for the prediction of inflammatory bowel disease relapse. Inflamm. Bowel Dis. 2009, 15, 1190–1198. [Google Scholar] [CrossRef]
- Manfredo Vieira, S.; Hiltensperger, M.; Kumar, V.; Zegarra-Ruiz, D.; Dehner, C.; Khan, N.; Costa, F.R.C.; Tiniakou, E.; Greiling, T.; Ruff, W.; et al. Translocation of a gut pathobiont drives autoimmunity in mice and humans. Science 2018, 359, 1156–1161. [Google Scholar] [CrossRef] [PubMed]
- Azzouz, D.; Omarbekova, A.; Heguy, A.; Schwudke, D.; Gisch, N.; Rovin, B.H.; Caricchio, R.; Buyon, J.P.; Alekseyenko, A.V.; Silverman, G.J. Lupus nephritis is linked to disease-activity associated expansions and immunity to a gut commensal. Ann. Rheum. Dis. 2019, 78, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, G.; Banerjee, N.; Liang, Y.; Du, X.; Boor, P.J.; Hoffman, K.L.; Khan, M.F. Aberrant Gut Microbiome Contributes to Intestinal Oxidative Stress, Barrier Dysfunction, Inflammation and Systemic Autoimmune Responses in MRL/lpr Mice. Front. Immunol. 2021, 12, 651191. [Google Scholar] [CrossRef] [PubMed]
- Mu, Q.; Tavella, V.J.; Kirby, J.L.; Cecere, T.E.; Chung, M.; Lee, J.; Li, S.; Ahmed, S.A.; Eden, K.; Allen, I.C.; et al. Antibiotics ameliorate lupus-like symptoms in mice. Sci. Rep. 2017, 7, 13675. [Google Scholar] [CrossRef] [PubMed]
- Toral, M.; Robles-Vera, I.; Romero, M.; de la Visitacion, N.; Sanchez, M.; O’Valle, F.; Rodriguez-Nogales, A.; Galvez, J.; Duarte, J.; Jimenez, R. Lactobacillus fermentum CECT5716: A novel alternative for the prevention of vascular disorders in a mouse model of systemic lupus erythematosus. FASEB J. 2019, 33, 10005–10018. [Google Scholar] [CrossRef]
- Cani, P.D.; Bibiloni, R.; Knauf, C.; Waget, A.; Neyrinck, A.M.; Delzenne, N.M.; Burcelin, R. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 2008, 57, 1470–1481. [Google Scholar] [CrossRef] [PubMed]
- Lo Conte, M.; Cosorich, I.; Ferrarese, R.; Antonini Cencicchio, M.; Nobili, A.; Palmieri, V.; Massimino, L.; Lamparelli, L.A.; Liang, W.; Riba, M.; et al. Alterations of the intestinal mucus layer correlate with dysbiosis and immune dysregulation in human Type 1 Diabetes. EBioMedicine 2023, 91, 104567. [Google Scholar] [CrossRef] [PubMed]
- Lam, Y.Y.; Ha, C.W.; Hoffmann, J.M.; Oscarsson, J.; Dinudom, A.; Mather, T.J.; Cook, D.I.; Hunt, N.H.; Caterson, I.D.; Holmes, A.J.; et al. Effects of dietary fat profile on gut permeability and microbiota and their relationships with metabolic changes in mice. Obesity 2015, 23, 1429–1439. [Google Scholar] [CrossRef]
- Stenman, L.K.; Holma, R.; Korpela, R. High-fat-induced intestinal permeability dysfunction associated with altered fecal bile acids. World J. Gastroenterol. 2012, 18, 923–929. [Google Scholar] [CrossRef]
- Araki, Y.; Katoh, T.; Ogawa, A.; Bamba, S.; Andoh, A.; Koyama, S.; Fujiyama, Y.; Bamba, T. Bile acid modulates transepithelial permeability via the generation of reactive oxygen species in the Caco-2 cell line. Free Radic. Biol. Med. 2005, 39, 769–780. [Google Scholar] [CrossRef]
- Raimondi, F.; Santoro, P.; Barone, M.V.; Pappacoda, S.; Barretta, M.L.; Nanayakkara, M.; Apicella, C.; Capasso, L.; Paludetto, R. Bile acids modulate tight junction structure and barrier function of Caco-2 monolayers via EGFR activation. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 294, G906–G913. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, T.; Rahman, F.; Smith, A.M. The Microbiome and Radiation Induced-Bowel Injury: Evidence for Potential Mechanistic Role in Disease Pathogenesis. Nutrients 2018, 10, 1405. [Google Scholar] [CrossRef] [PubMed]
- Darwich, A.S.; Aslam, U.; Ashcroft, D.M.; Rostami-Hodjegan, A. Meta-analysis of the turnover of intestinal epithelia in preclinical animal species and humans. Drug Metab. Dispos. 2014, 42, 2016–2022. [Google Scholar] [CrossRef] [PubMed]
- Nejdfors, P.; Ekelund, M.; Westrom, B.R.; Willen, R.; Jeppsson, B. Intestinal permeability in humans is increased after radiation therapy. Dis. Colon. Rectum 2000, 43, 1582–1587; discussion 1587–1588. [Google Scholar] [CrossRef]
- Shukla, P.K.; Gangwar, R.; Manda, B.; Meena, A.S.; Yadav, N.; Szabo, E.; Balogh, A.; Lee, S.C.; Tigyi, G.; Rao, R. Rapid disruption of intestinal epithelial tight junction and barrier dysfunction by ionizing radiation in mouse colon in vivo: Protection by N-acetyl-l-cysteine. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G705–G715. [Google Scholar] [CrossRef] [PubMed]
- Crawford, P.A.; Gordon, J.I. Microbial regulation of intestinal radiosensitivity. Proc. Natl. Acad. Sci. USA 2005, 102, 13254–13259. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Cheng, W.; Qu, W.; Shao, G.; Liu, S. Antibiotic Alleviates Radiation-Induced Intestinal Injury by Remodeling Microbiota, Reducing Inflammation, and Inhibiting Fibrosis. ACS Omega 2020, 5, 2967–2977. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, Q.; Wang, X.; Zhu, L.; Chen, J.; Zhang, B.; Chen, Y.; Yuan, Z. Gut microbial dysbiosis is associated with development and progression of radiation enteritis during pelvic radiotherapy. J. Cell Mol. Med. 2019, 23, 3747–3756. [Google Scholar] [CrossRef]
- Cui, M.; Xiao, H.; Li, Y.; Zhou, L.; Zhao, S.; Luo, D.; Zheng, Q.; Dong, J.; Zhao, Y.; Zhang, X.; et al. Faecal microbiota transplantation protects against radiation-induced toxicity. EMBO Mol. Med. 2017, 9, 448–461. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Li, Q.; Li, P.; Chen, X.; Xiang, L.; Bi, L.; Zhu, J.; Huang, X.; Cui, B.; Zhang, F. Fecal microbiota transplantation: A promising treatment for radiation enteritis? Radiother. Oncol. 2020, 143, 12–18. [Google Scholar] [CrossRef]
- Xiao, H.W.; Cui, M.; Li, Y.; Dong, J.L.; Zhang, S.Q.; Zhu, C.C.; Jiang, M.; Zhu, T.; Wang, B.; Wang, H.C.; et al. Gut microbiota-derived indole 3-propionic acid protects against radiation toxicity via retaining acyl-CoA-binding protein. Microbiome 2020, 8, 69. [Google Scholar] [CrossRef] [PubMed]
- Hesketh, P.J. Chemotherapy-induced nausea and vomiting. N. Engl. J. Med. 2008, 358, 2482–2494. [Google Scholar] [CrossRef] [PubMed]
- Logan, R.M.; Gibson, R.J.; Bowen, J.M.; Stringer, A.M.; Sonis, S.T.; Keefe, D.M. Characterisation of mucosal changes in the alimentary tract following administration of irinotecan: Implications for the pathobiology of mucositis. Cancer Chemother. Pharmacol. 2008, 62, 33–41. [Google Scholar] [CrossRef]
- McQuade, R.M.; Stojanovska, V.; Abalo, R.; Bornstein, J.C.; Nurgali, K. Chemotherapy-Induced Constipation and Diarrhea: Pathophysiology, Current and Emerging Treatments. Front. Pharmacol. 2016, 7, 414. [Google Scholar] [CrossRef]
- Masetti, R.; Muratore, E.; Leardini, D.; Zama, D.; Turroni, S.; Brigidi, P.; Esposito, S.; Pession, A. Gut microbiome in pediatric acute leukemia: From predisposition to cure. Blood Adv. 2021, 5, 4619–4629. [Google Scholar] [CrossRef]
- Hakim, H.; Dallas, R.; Wolf, J.; Tang, L.; Schultz-Cherry, S.; Darling, V.; Johnson, C.; Karlsson, E.A.; Chang, T.C.; Jeha, S.; et al. Gut Microbiome Composition Predicts Infection Risk during Chemotherapy in Children with Acute Lymphoblastic Leukemia. Clin. Infect. Dis. 2018, 67, 541–548. [Google Scholar] [CrossRef]
- Liu, X.; Zou, Y.; Zhang, Y.; Liu, L.; Duan, Y.; Zhang, A.; Zhang, X.; Zhang, R.; Zhao, B.; Li, X.; et al. Characteristics in gut microbiome is associated with chemotherapy-induced pneumonia in pediatric acute lymphoblastic leukemia. BMC Cancer 2021, 21, 1190. [Google Scholar] [CrossRef]
- Nalle, S.C.; Kwak, H.A.; Edelblum, K.L.; Joseph, N.E.; Singh, G.; Khramtsova, G.F.; Mortenson, E.D.; Savage, P.A.; Turner, J.R. Recipient NK cell inactivation and intestinal barrier loss are required for MHC-matched graft-versus-host disease. Sci. Transl. Med. 2014, 6, 243ra287. [Google Scholar] [CrossRef]
- Johansson, J.E.; Ekman, T. Gut toxicity during hemopoietic stem cell transplantation may predict acute graft-versus-host disease severity in patients. Dig. Dis. Sci. 2007, 52, 2340–2345. [Google Scholar] [CrossRef]
- Noth, R.; Lange-Grumfeld, J.; Stuber, E.; Kruse, M.L.; Ellrichmann, M.; Hasler, R.; Hampe, J.; Bewig, B.; Rosenstiel, P.; Schreiber, S.; et al. Increased intestinal permeability and tight junction disruption by altered expression and localization of occludin in a murine graft versus host disease model. BMC Gastroenterol. 2011, 11, 109. [Google Scholar] [CrossRef]
- Nalle, S.C.; Zuo, L.; Ong, M.; Singh, G.; Worthylake, A.M.; Choi, W.; Manresa, M.C.; Southworth, A.P.; Edelblum, K.L.; Baker, G.J.; et al. Graft-versus-host disease propagation depends on increased intestinal epithelial tight junction permeability. J. Clin. Investig. 2019, 129, 902–914. [Google Scholar] [CrossRef]
- Ara, T.; Hashimoto, D.; Hayase, E.; Noizat, C.; Kikuchi, R.; Hasegawa, Y.; Matsuda, K.; Ono, S.; Matsuno, Y.; Ebata, K.; et al. Intestinal goblet cells protect against GVHD after allogeneic stem cell transplantation via Lypd8. Sci. Transl. Med. 2020, 12, eaaw0720. [Google Scholar] [CrossRef]
- Heidt, P.J.; Vossen, J.M. Experimental and clinical gnotobiotics: Influence of the microflora on graft-versus-host disease after allogeneic bone marrow transplantation. J. Med. 1992, 23, 161–173. [Google Scholar]
- Beelen, D.W.; Elmaagacli, A.; Muller, K.D.; Hirche, H.; Schaefer, U.W. Influence of intestinal bacterial decontamination using metronidazole and ciprofloxacin or ciprofloxacin alone on the development of acute graft-versus-host disease after marrow transplantation in patients with hematologic malignancies: Final results and long-term follow-up of an open-label prospective randomized trial. Blood 1999, 93, 3267–3275. [Google Scholar] [CrossRef]
- Koyama, M.; Mukhopadhyay, P.; Schuster, I.S.; Henden, A.S.; Hulsdunker, J.; Varelias, A.; Vetizou, M.; Kuns, R.D.; Robb, R.J.; Zhang, P.; et al. MHC Class II Antigen Presentation by the Intestinal Epithelium Initiates Graft-versus-Host Disease and Is Influenced by the Microbiota. Immunity 2019, 51, 885–898.e7. [Google Scholar] [CrossRef]
- Hanash, A.M.; Dudakov, J.A.; Hua, G.; O’Connor, M.H.; Young, L.F.; Singer, N.V.; West, M.L.; Jenq, R.R.; Holland, A.M.; Kappel, L.W.; et al. Interleukin-22 protects intestinal stem cells from immune-mediated tissue damage and regulates sensitivity to graft versus host disease. Immunity 2012, 37, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Aleman, R.S.; Moncada, M.; Aryana, K.J. Leaky Gut and the Ingredients That Help Treat It: A Review. Molecules 2023, 28, 619. [Google Scholar] [CrossRef] [PubMed]
- Rein, M.; Ben-Yacov, O.; Godneva, A.; Shilo, S.; Zmora, N.; Kolobkov, D.; Cohen-Dolev, N.; Wolf, B.C.; Kosower, N.; Lotan-Pompan, M.; et al. Effects of personalized diets by prediction of glycemic responses on glycemic control and metabolic health in newly diagnosed T2DM: A randomized dietary intervention pilot trial. BMC Med. 2022, 20, 56. [Google Scholar] [CrossRef] [PubMed]
- Berry, S.E.; Valdes, A.M.; Drew, D.A.; Asnicar, F.; Mazidi, M.; Wolf, J.; Capdevila, J.; Hadjigeorgiou, G.; Davies, R.; Al Khatib, H.; et al. Human postprandial responses to food and potential for precision nutrition. Nat. Med. 2020, 26, 964–973. [Google Scholar] [CrossRef]
- Tsai, Y.L.; Lin, T.L.; Chang, C.J.; Wu, T.R.; Lai, W.F.; Lu, C.C.; Lai, H.C. Probiotics, prebiotics and amelioration of diseases. J. Biomed. Sci. 2019, 26, 3. [Google Scholar] [CrossRef]
- Allegretti, J.R.; Mullish, B.H.; Kelly, C.; Fischer, M. The evolution of the use of faecal microbiota transplantation and emerging therapeutic indications. Lancet 2019, 394, 420–431. [Google Scholar] [CrossRef]
- Craven, L.; Rahman, A.; Nair Parvathy, S.; Beaton, M.; Silverman, J.; Qumosani, K.; Hramiak, I.; Hegele, R.; Joy, T.; Meddings, J.; et al. Allogenic Fecal Microbiota Transplantation in Patients with Nonalcoholic Fatty Liver Disease Improves Abnormal Small Intestinal Permeability: A Randomized Control Trial. Am. J. Gastroenterol. 2020, 115, 1055–1065. [Google Scholar] [CrossRef]
- Wilson, B.C.; Vatanen, T.; Cutfield, W.S.; O’Sullivan, J.M. The Super-Donor Phenomenon in Fecal Microbiota Transplantation. Front. Cell Infect. Microbiol. 2019, 9, 2. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).