Unraveling Atopic Dermatitis: Insights into Pathophysiology, Therapeutic Advances, and Future Perspectives
Abstract
1. Introduction
- Infantile (with an onset below two years)—In this case, the patient presents acute lesions characterized by poorly defined redness (erythema) accompanied by swelling (edema), small blisters (vesicles), scratch marks (excoriations), and a clear fluid discharge (serous exudate) on the face, cheeks, and scalp.
- Childhood (seen from two years to adolescence)—In this case, the nature of eczema tends to evolve into a more localized and chronic condition. The acute, widespread erythema and vesicular lesions of infancy give way to paler redness, increased dryness (xerosis), and less-distinct lesions. These changes predominantly affect the body’s flexural areas, such as the inner elbows and knees, where the skin may also thicken (lichenify) due to chronic scratching.
- Adult (after puberty)—This form manifests as chronic hand eczema, exclusively affecting the hands, or it may also involve head–neck dermatitis, impacting the upper trunk, shoulders, and scalp [9].
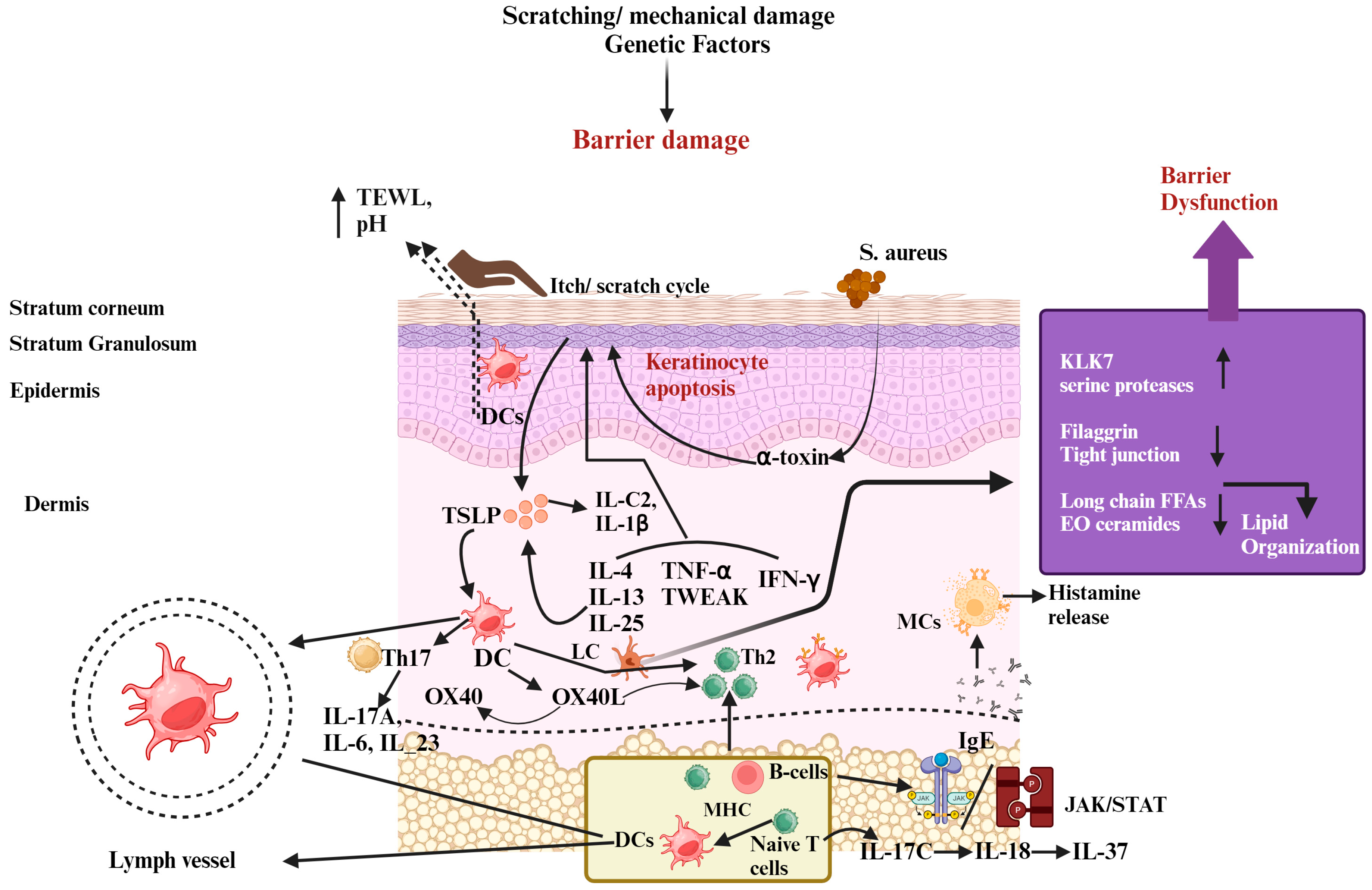
2. Pathogenesis of AD
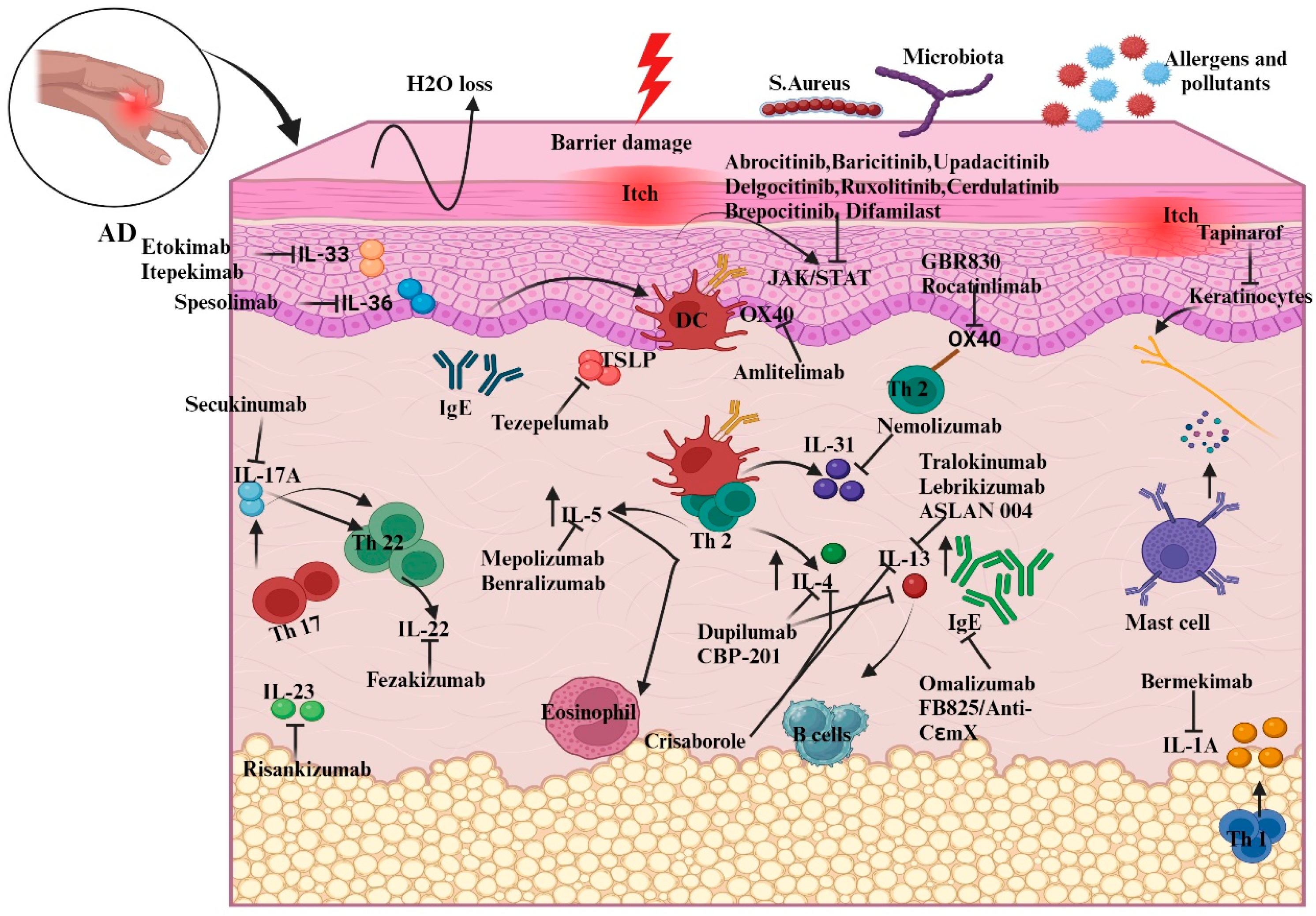
3. Emerging Therapies and Therapeutics
3.1. Microbiome Modulation
3.2. Targeting the Function of the Epidermal Barrier
3.3. Controlling Immunological Response
3.3.1. Innate Immune Response
- Aryl-hydrocarbon receptor (AhR)
- SPINK5
- IL-36R
- IL-1
- IL-33
3.3.2. Adaptive Immune Response
- IL-4 and IL-13
- IL-5
- IL-31
- JAK
- OX40
- IL-4R
- IL-17A
- IL-22
- IL-18 and IL-37
| Method | Mode of Application | Category | Therapeutic Agent | Name of Company | Target | Clinical Phase | ID of Clinical Trial |
|---|---|---|---|---|---|---|---|
| Microbiome modulation | Topical | Bacterial strain | B244 | AO Biome | Nitric acid donor | IIb | NCT04490109 |
| FB-401 | Forte Biosciences | TNFR activation and Bacterial substitution | IIB | NCT04504279 | |||
| ShA9 | NIAID | Microbiota selected for transplant | I/Iia | NCT03151148 | |||
| Topical | Small molecule | Atx201/niclosamide | Union Therapeutics | Activity of protonophore | II | NCT04339985 | |
| CLS-001/omiganan | Cutaneous Life Sciences | Improved cell membrane | II | NCT02456480 | |||
| Oral | Bacterial strain | EDP1815 | Evelo | Regulation of systemic inflammation | Ib | NCT03733353 | |
| STMC-103H | Siolta therapeutics | Using the microbiome to modulate immunity | Ib | NCT03819881 | |||
| Target-innate immune response | Topical | Biologic | Tapinarof | Dermavant | Ahr agonist | IIB | NA |
| Injection | Biologic | Tezepelumab | AstraZeneca | TSLP | IIA | NCT02525094 | |
| Biologic | Etokimab | AnaptysBio | Interleukin-33 | IIA | NCT03533751 | ||
| Biologic | REGN3500 | Regeneron | Interleukin-33 | IIA | NCT03738423 | ||
| Biologic | Astegolimab | Genentech | Interleukin-33 | IIA | NCT03747575 | ||
| Biologic | MEDI3506 | MedImmune | Interleukin-33 | IIA | NCT04212169 | ||
| Biologic | Bermekimab | Janssen | Interleukin-1a | IIA | NCT03496974 | ||
| Biologic | Spesolimab | Bohringer Ingelheim | Interleukin-36R | IIA | NCT03822832 | ||
| Target- Adaptive immune response | Injection | Biologic | CBP-201 | Connect Biopharma | Interleukin-4Ra | IIB | NCT04444752 |
| Biologic | Dupilumab | Sanofi | Interleukin-4Ra | Approved | NCT03346434 | ||
| Biologic | ASLAN004 | ASLAN | Interleukin-13Ra1 | Ib | NCT04090229 | ||
| Biologic | Tralokinumab | LEO Pharma | Interleukin-13 | Approved | NCT03526861 | ||
| Biologic | Lebrikizumab | Allmiral/Lilly | Interleukin-13 | III | NCT04250350 | ||
| Biologic | Benralizumab | AstraZeneca | Interleukin-5Ra | IIA | NCT04605094 | ||
| Biologic | Omalizumab | Novartis | Immunoglobulin E | IIA | NCT02300701 | ||
| Biologic | FB825/anti-CεmX | LEO Pharma | Immunoglobulin E | IIA | NCT04413942 | ||
| Biologic | Fezakimuab | IIT | Interleukin-22 | IIA | NCT01941537 | ||
| Biologic | Secukinumab | Novartis | Interleukin-17a | IIA | NCT03568136 | ||
| Biologic | Risankizumab | AbbVie | Interleukin-23 | IIA | NCT03706040 | ||
| Injection | Biologic | Nemolizumab | Mitchga Syringes | Interleukin-31 | Approved | NCT03921411 | |
| Biologic | Mepolizumab | Nucala | Interleukin-5 | II | NCT03055195 | ||
| Biologic | Amditelimab | Sanofi | OX-40 | II | NCT03754309 | ||
| Biologic | Rocatinlimab | Kyowa Kirin | OX-40 | II | NCT03703102 | ||
| Oral | Small molecule | Abrocitinib | Cibinqo | JAK1 | III | NCT04345367 | |
| Small molecule | Bacricitinib | Eli Lilly & Company | JAK1 | III | NCT03334396 | ||
| Small molecule | Upadacitinib | Rinvoq | JAK1 | III | NCT03569293 | ||
| Topical | Small molecule | Delgocitinib | Leo Pharma | JAK1 | IIB | NCT03683719 | |
| Small molecule | Ruxolitinib | Incyte Corp | JAK1 | I | NCT03920852 | ||
| Small molecule | Cerdulatinib | AstraZeneca | JAK1 | Ib | DMVT-502-1001 | ||
| Small molecule | Brepocitinib | Pfizer | JAK1 | IIB | NCT0390382213 |
3.4. Treatment Strategies for AD and a Recently Developed Novel Drug Delivery System Based on Nanotechnology
| Delivery Agent | Formulation/Dosage Form | Technique Used | Inferences | References |
|---|---|---|---|---|
| Tacrolimus/Nicotinamide | Nanoparticles | Ionic gelation method | It enhances penetration through and into the skin’s layers, lowers treatment dosages, and acts as an adjuvant in the fight against AD. | [117] |
| Tacrolimus and hyaluronic acid | Chitosan-based nanoparticles | High-pressure homogenization solvent evaporation method | Their delivery system plays a significant role, which does not affect a patient’s preferences | [119] |
| Betamethasone and Hyaluronic acid | Chitosan-nanoparticles | High-pressure homogenization solvent evaporation method | A better-sustained release pattern and greater drug retention capacity were observed. | [123] |
| Oat-ceramides | Lecithin-based microemulsions and starch-based nanoparticles | Emulsification solvent evaporation method | The gel increased permeation of oat ceramides was deep into the skin. | [124] |
| Pioglitazone | Nanoemulsion | Water titration method | ↑ stratum corneum hydration (SCH), ↑ suppression of inflammatory cytokines levels, redness reduction, ↓ dermis thickness, ↓ TEWL biocompatible with skin, and controlled release of the formulation were observed. | [125] |
| Clobetasol propionate | Nanoemulsion | NA | ↓ edema inhibition and skin irritation. | [126] |
| Betamethasone valerate/Diflucortolone valerate | Liposomes/Nanoparticles | Thin-film hydration method/direct injection method | ↑ edema inhibition, ↓ TEWL and erythema, and ↑ stratum corneum and epidermis retention. | [127] |
| Nicotinamide | Ethosome | Cold method | Results show that there was a decrease in IgE levels and inflammation. In vitro permeation results show that there was an increase in skin retention in rat models. | [128] |
| Glycyrrhizic acid | Transfersomes | Thin-film hydration method | The controlled release was followed by transfersomes for up to 24 h, ↓ in scratching and erythema score, and hematological parameters were normal. | [129] |
| Cyclosporine A | Multilamelar vesicles (transfersomes and ethosomes) | Thin-film hydration method | Ethosomes released the drug up to 24 h at controlled rate. If we compare this finding with the types of transfersomes, increases in flux and diffusion of CsA-loaded ethosomes were more concentrated than in other formulations. | [130] |
| Tacrolimus | Thermosensitive SLNs | Modified emulsification and low-temperature solidification. | In contrast to the reference product, it distributes more medications into deeper layers of skin and penetrates deeper into the epidermal layer. | [131] |
| Betamethasone valerate | NLCs | NA | When comparing drug-loaded NLC gel with BMV gel, a significant 2.59-fold increase in permeation, controlled release with non-Fickian diffusion, and a noteworthy increase in anti-inflammatory action were observed. | [132] |
| Vitamin E | NLCs | Hot high-pressure homogenization and ultrasound technique | In vitro studies showed that nanoparticles were biocompatible and non-irritant. | [133] |
| Methotrexate | NLCs | Hot ultrasonication method | The sustained release profile was shown by nanoparticles, which were non-toxicity and biocompatible. | [134] |
| Betamethasone dipropionate | Nanocrystal | Wet bead milling method | Ex vivo results show increases in drug accumulation in the skin layers and a decrease in flux. | [135] |
| Betamethasone dipropionate | Polymeric micelles | Thin-film hydration method | Polymeric micelles show increased skin retention of the drug and a ↓ the amount of drug permeated. Almost-complete skin healing was achieved before the conventional treatment. | [135] |
| Tacrolimus | NPs | Ultrasonication method | Results show increased skin retention and permeation. | [136] |
| Encapsulated fluorophore | NPs | Solvent diffusion method | No toxicity was seen over 8 days. Ex vivo results show decreases in permeation vs. poly lactic acid NPs suspension, ↑ inhibition of cell proliferation, and IL-2 secretion. | [137] |
| Tacrolimus | NPs | NA | ↑ in skin layer penetration; when the optimized formulation was compared to commercial treatment, an increase in inhibition of IL-2 and TSLP was observed. | [138] |
| Cyclosporine A | NPs | NA | Results show an increase in the penetration of formulation into different deeper skin layers, preserved skin integrity, prevention of skin thickening, decreased swelling, and even in serum levels of IFN-γ, IgE, and IL-4. | [139] |
| Betamethasone valerate | NPs | Emulsion-diffusion-evaporation method | When a commercial cream was compared with the optimized NP loaded with BMV, it was found that there was a decrease in the skin thickness and blanching. Epidermis retention increased compared to that for the commercial treatment. | [140] |
| Hydrocortisone/Hydroxytyrosol | NPs | Ionic cross-linking method | There was an increase in skin retention and a decrease in flux, TEWL, intensity of erythema, skin thickness, and dermatitis index. | [141] |
| Methotrexate | NPs | Ultrasonication method | Results show great permeation of the drug into the skin. | [142] |
| ER143 | Nanocapsules | Emulsion solvent evaporation method | There was an increase in erythema inhibition compared to conventional treatment, an ↑ in skin retention, and skin permeation. | [143] |
| Desonide | Nanocapsules | Interfacial deposition method | Slightly irritant, non-phototoxic, and shows a biphasic release profile | [144] |
| Auraptene | SLNs | Hot homogenization and ultrasound method | Improvement in anti-inflammatory properties and sustained release of drugs. | [146] |
| Nicotinamide | W/O/W multiple-emulsion and microemulsion | High agitation and incorporation | Multiple emulsions elicited no changes in the permeability of the skin | [147] |
| Mizolastine | PLGA-mPEG microparticles | O/W emulsification solvent evaporation method | Significant reduction in ear thickness and the dermatitis index as well as a suppression of the infiltration of cells related to inflammation and immunoglobulin E | [148] |
| Levocetirizine | Noisome and chitosan nanoparticles | Thin-film hydration method and ionic gelation method | Niosomes gel optimized had superior skin retention | [149] |
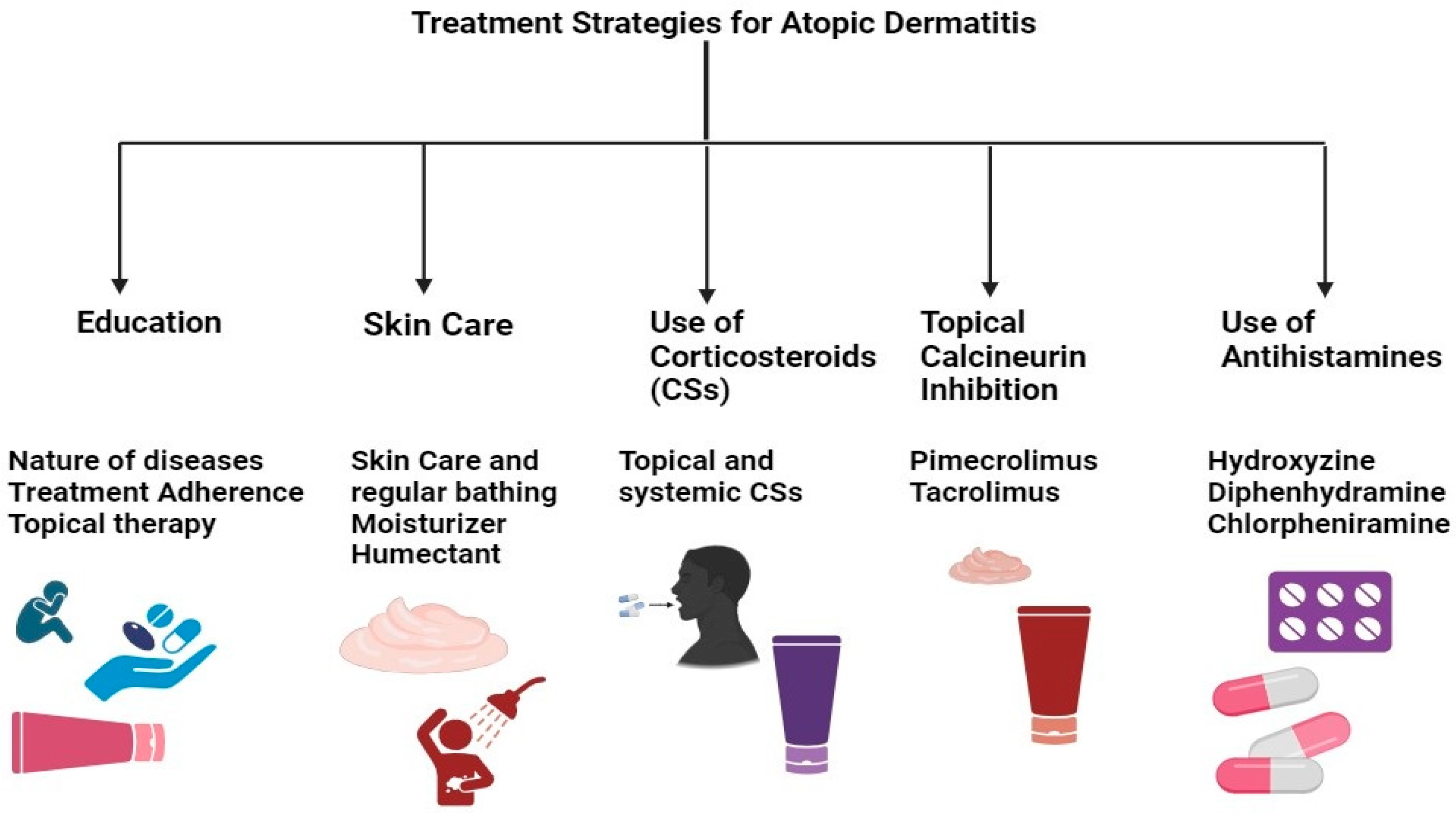
4. FDA-Approved Medical Therapies for AD Treatment
5. Future Prospective
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Moyle, M.; Cevikbas, F.; Harden, J.L.; Guttman-Yassky, E. Understanding the immune landscape in atopic dermatitis: The era of biologics and emerging therapeutic approaches. Exp. Dermatol. 2019, 28, 756–768. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Barbarot, S.; Gadkari, A.; Simpson, E.L.; Weidinger, S.; Mina-Osorio, P.; Rossi, A.B.; Brignoli, L.; Saba, G.; Guillemin, I.; et al. Atopic dermatitis in the pediatric population. Ann. Allergy Asthma Immunol. 2021, 126, 417–428. [Google Scholar] [CrossRef]
- Barbarot, S.; Auziere, S.; Gadkari, A.; Girolomoni, G.; Puig, L.; Simpson, E.L.; Margolis, D.J.; De Bruin-Weller, M.; Eckert, L. Epidemiology of atopic dermatitis in adults: Results from an international survey. Allergy 2018, 73, 1284–1293. [Google Scholar] [CrossRef]
- Eckert, L.; Gupta, S.; Gadkari, A.; Mahajan, P.; Gelfand, J.M. Burden of illness in adults with atopic dermatitis: Analysis of National Health and Wellness Survey data from France, Germany, Italy, Spain, and the United Kingdom. J. Am. Acad. Dermatol. 2019, 81, 187–195. [Google Scholar] [CrossRef]
- Bawany, F.; Beck, L.A.; Järvinen, K.M. Halting the March: Primary prevention of atopic dermatitis and food allergies. J. Allergy Clin. Immunol. Pract. 2020, 8, 860–875. [Google Scholar] [CrossRef]
- Dharmage, S.C.; Lowe, A.J.; Matheson, M.C.; Burgess, J.A.; Allen, K.J.; Abramson, M.J. AD and the atopic march revisited. Allergy 2013, 69, 17–27. [Google Scholar] [CrossRef]
- Andersen, Y.M.F.; Egeberg, A.; Skov, L.; Thyssen, J.P. Comorbidities of Atopic Dermatitis: Beyond Rhinitis and Asthma. Curr. Dermatol. Rep. 2017, 6, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, J.I. Measurement properties of the hospital anxiety and depression scale used in atopic dermatitis in adults. J. Investig. Dermatol. 2019, 139, 1388–1391. [Google Scholar] [CrossRef] [PubMed]
- Langan, S.M.; Irvine, A.D.; Weidinger, S. Atopic dermatitis. Lancet 2020, 396, 345–360. [Google Scholar] [CrossRef]
- Kapur, S.; Watson, W.; Carr, S. Atopic dermatitis. Allergy Asthma Clin. Immunol. 2018, 14, 52. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Yokozeki, H.; Karasuyama, H.; Satoh, T. IL-31–generating network in atopic dermatitis comprising macrophages, basophils, thymic stromal lymphopoietin, and periostin. J. Allergy Clin. Immunol. 2023, 151, 737–746.e6. [Google Scholar] [CrossRef]
- Chovatiya, R.; Silverberg, J.I. Pathophysiology of atopic dermatitis and Psoriasis: Implications for management in children. Children 2019, 6, 108. [Google Scholar] [CrossRef]
- Celebi Sozener, Z.; Ozdel Ozturk, B.; Cerci, P.; Turk, M.; Gorgulu Akin, B.; Akdis, M.; Altiner, S.; Ozbey, U.; Ogulur, I.; Mitamura, Y.; et al. Epithelial barrier hypothesis: Effect of the external exposome on the microbiome and epithelial barriers in allergic disease. Allergy 2022, 77, 1418–1449. [Google Scholar] [CrossRef]
- Ezzedine, K.; Kechichian, E. Épidémiologie de la dermatite atopique [Epidemiology of atopic dermatitis]. Ann. Dermatol. Venereol. 2017, VS4–VS7, 29433636. [Google Scholar]
- Beck, L.A.; Cork, M.J.; Amagai, M.; De Benedetto, A.; Kabashima, K.; Hamilton, J.D.; Rossi, A.B. Type 2 inflammation contributes to skin barrier dysfunction in atopic dermatitis. JID Innov. 2022, 2, 100131. [Google Scholar] [CrossRef]
- Gong, J.Q.; Lin, L.; Lin, T.; Hao, F.; Zeng, F.Q.; Bi, Z.G.; Yi, D.; Zhao, B. Skin colonization by Staphylococcus aureus in patients with eczema and atopic dermatitis and relevant combined topical therapy: A double-blind multicentre randomized controlled trial. Br. J. Dermatol. 2006, 155, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Alexander, H.; Paller, A.S.; Traidl-Hoffmann, C.; Beck, L.A.; De Benedetto, A.; Dhar, S.; Girolomoni, G.; Irvine, A.D.; Spuls, P.; Su, J.; et al. The role of bacterial skin infections in atopic dermatitis: Expert statement and review from the International Eczema Council Skin Infection Group. Br. J. Dermatol. 2020, 182, 1331–1342. [Google Scholar] [CrossRef] [PubMed]
- Clausen, M.L.; Agner, T.; Lilje, B.; Edslev, S.M.; Johannesen, T.B.; Andersen, P.S. Association of Disease Severity with Skin Microbiome and Filaggrin Gene Mutations in Adult Atopic Dermatitis. JAMA Dermatol. 2018, 154, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.R.; Nakatsuji, T.; Sanford, J.A.; Vrbanac, A.F.; Gallo, R.L. Staphylococcus aureus Induces Increased Serine Protease Activity in Keratinocytes. J. Investig. Dermatol. 2017, 137, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Berube, B.J.; Bubeck Wardenburg, J. Staphylococcus aureus α-toxin: Nearly a century of intrigue. Toxins 2013, 5, 1140–1166. [Google Scholar] [CrossRef]
- Nakamura, Y.; Oscherwitz, J.; Cease, K.B.; Chan, S.M.; Muñoz-Planillo, R.; Hasegawa, M.; Villaruz, A.E.; Cheung, G.Y.; McGavin, M.J.; Travers, J.B.; et al. Staphylococcus δ-toxin induces allergic skin disease by activating mast cells. Nature 2013, 503, 397–401. [Google Scholar] [CrossRef]
- Cesare, A.D.; Meglio, P.D.; Nestle, F.O. A role for Th17 cells in the immunopathogenesis of atopic dermatitis. J. Investig. Dermatol. 2008, 128, 2569–2571. [Google Scholar] [CrossRef] [PubMed]
- Kee, J.Y.; Jeon, Y.D.; Kim, D.S.; Han, Y.H.; Park, J.; Youn, D.H.; Kim, S.J.; Ahn, K.S.; Um, J.Y.; Hong, S.H. Korean Red Ginseng improves atopic dermatitis-like skin lesions by suppressing expression of proinflammatory cytokines and chemokines in vivo and in vitro. J. Ginseng Res. 2017, 41, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Tsakok, T.; Woolf, R.; Smith, C.; Weidinger, S.; Flohr, C. Atopic dermatitis: The skin barrier and beyond. Br. J. Dermatol. 2018, 180, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Nakatsuji, T.; Chen, T.H.; Two, A.M.; Chun, K.; Narala, S.; Geha, R.S.; Hata, T.; Gallo, R.L. Staphylococcus aureus Exploits Epidermal Barrier Defects in atopic dermatitis to Trigger Cytokine Expression. J. Investig. Dermatol. 2016, 136, 2192–2200. [Google Scholar] [CrossRef] [PubMed]
- Zaniboni, M.C.; Samorano, L.P.; Orfali, R.L.; Aoki, V. Skin barrier in atopic dermatitis: Beyond filaggrin. An. Bras. De Dermatol. 2016, 91, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Vattepu, R.; Zhang, S. Chemokines and innate lymphoid cells in skin inflammation. Cells 2021, 10, 3074. [Google Scholar] [CrossRef]
- Peng, W.; Novak, N. Pathogenesis of atopic dermatitis. Clinical and experimental allergy. J. Br. Soc. Allergy Clin. Immunol. 2015, 45, 566–574. [Google Scholar] [CrossRef]
- Gilles, S.; Akdis, C.A.; Lauener, R.; Schmid-Grendelmeier, P.; Bieber, T.; Schäppi, G.; Traidl-Hoffmann, C. The role of environmental factors in allergy: A critical reappraisal. Exp. Dermatol. 2018, 27, 1193–1200. [Google Scholar] [CrossRef]
- Stefanovic, N.; Flohr, C.; Irvine, A.D. The exposome in atopic dermatitis. Allergy 2019, 75, 63–74. [Google Scholar] [CrossRef]
- Meisel, J.S.; Sfyroera, G.; Bartow-McKenney, C.; Gimblet, C.; Bugayev, J.; Horwinski, J.; Kim, B.; Brestoff, J.R.; Tyldsley, A.S.; Zheng, Q.; et al. Commensal microbiotas modulate gene expression in the skin. Microbiome 2018, 6, 20. [Google Scholar] [CrossRef]
- Weidinger, S.; Beck, L.A.; Bieber, T.; Kabashima, K.; Irvine, A.D. Atopic dermatitis. Nat. Rev. Dis. Primers 2018, 4, 1. [Google Scholar] [CrossRef]
- Mack, M.R.; Kim, B. The Itch–Scratch Cycle: A neuroimmune perspective. Trends Immunol. 2018, 39, 980–991. [Google Scholar] [CrossRef]
- Wollenberg, A.; Barbarot, S.; Bieber, T.; Christen-Zaech, S.; Deleuran, M.; Fink-Wagner, A.; Gieler, U.; Girolomoni, G.; Lau, S.K.C.; Muraro, A.; et al. Consensus-based European guidelines for treatment of atopic Eczema (atopic dermatitis) in adults and children: Part I. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 657–682. [Google Scholar] [CrossRef] [PubMed]
- Callewaert, C.; Knödlseder, N.; Karoglan, A.; Güell, M.; Paetzold, B. Skin microbiome transplantation and manipulation: Current state of the art. Comput. Struct. Biotechnol. J. 2021, 19, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Paller, A.S.; Kong, H.H.; Seed, P.C.; Naik, S.; Scharschmidt, T.C.; Gallo, R.L.; Luger, T.A.; Irvine, A.D. The microbiome in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2019, 143, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Myles, I.A.; Castillo, C.R.; Barbian, K.D.; Kanakabandi, K.; Virtaneva, K.; Fitzmeyer, E.; Paneru, M.; Otaizo-Carrasquero, F.; Myers, T.G.; Markowitz, T.E.; et al. Therapeutic responses to Roseomonas mucosa in atopic dermatitis may involve lipid-mediated TNF-related epithelial repair. Sci. Transl. Med. 2020, 12, eaaz8631. [Google Scholar] [CrossRef]
- Nakatsuji, T.; Chen, T.H.; Narala, S.; Chun, K.; Two, A.; Tong, Y.; Shafiq, F.; Kotol, P.; Bouslimani, A.; Melnik, A.V.; et al. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci. Transl. Med. 2017, 9, eaah4680. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, J.I.; Lio, P.A.; Simpson, E.L.; Li, C.; Brownell, D.R.; Gryllos, I.; Ng-Cashin, J.; Krueger, T.S.; Swaidan, V.R.; Bliss, R.; et al. Efficacy and safety of topically applied therapeutic ammonia oxidizing bacteria in adults with mild-to-moderate atopic dermatitis and moderate-to-severe pruritus: A randomized, double-blind, placebo-controlled, dose-ranging, phase 2b trial. EclinicalMedicine 2023, 60, 102002. [Google Scholar] [CrossRef] [PubMed]
- Zapotoczna, M.; Forde, É.; Hogan, S.; Humphreys, H.; O’Gara, J.P.; Fitzgerald-Hughes, D.; Devocelle, M.; O’Neill, E. Eradication of Staphylococcus aureus Biofilm Infections Using Synthetic Antimicrobial Peptides. J. Infect. Dis. 2017, 215, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.R.; Costa, S.K.; Zaramela, L.S.; Khalil, S.; Todd, D.A.; Winter, H.L.; Sanford, J.A.; O’Neill, A.M.; Liggins, M.C.; Nakatsuji, T.; et al. Quorum sensing between bacterial species on the skin protects against epidermal injury in atopic dermatitis. Sci. Transl. Med. 2019, 11, eaat8329. [Google Scholar] [CrossRef] [PubMed]
- Bieber, T. AD: An expanding therapeutic pipeline for a complex disease. Nat. Rev. Drug Discov. 2021, 21, 21–40. [Google Scholar] [CrossRef] [PubMed]
- Wollenberg, A.; Christen-Zäch, S.; Taïeb, A.; Paul, C.; Thyssen, J.P.; De Bruin-Weller, M.; Vestergaard, C.; Seneschal, J.; Werfel, T.; Cork, M.J.; et al. ETFAD/EADV Eczema Task Force 2020 position paper on diagnosing and treating atopic dermatitis in adults and children. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2717–2744. [Google Scholar] [CrossRef]
- Czarnowicki, T.; Malajian, D.; Khattri, S.; Da Rosa, J.C.; Dutt, R.; Finney, R.; Dhingra, N.; Peng, X.; Xu, H.; Estrada, Y.; et al. Petrolatum: Barrier repair and antimicrobial responses underlying this “inert” moisturizer. J. Allergy Clin. Immunol. 2016, 137, 1091–1102.e7. [Google Scholar] [CrossRef]
- Segre, J.A. Epidermal barrier formation and recovery in skin disorders. J. Clin. Investig. 2006, 116, 1150–1158. [Google Scholar] [CrossRef]
- Chieosilapatham, P.; Kiatsurayanon, C.; Umehara, Y.; Trujillo-Paez, J.V.; Peng, G.; Yue, H.; Nguyen, L.; Niyonsaba, F. Keratinocytes: Innate immune cells in atopic dermatitis. Clin. Exp. Immunol. 2021, 204, 296–309. [Google Scholar] [CrossRef]
- Trikha, P.; Lee, D.A. The role of AhR in transcriptional regulation of immune cell development and function. Biochim. Et Biophys. Acta-Rev. Cancer 2020, 1873, 188335. [Google Scholar] [CrossRef]
- Van Den Bogaard, E.H.; Bergboer, J.G.; Vonk-Bergers, M.; Van Vlijmen-Willems, I.M.; Hato, S.V.; Van Der Valk, P.; Schröder, J.; Joosten, I.; Zeeuwen, P.L.; Schalkwijk, J. Coal tar induces AHR-dependent skin barrier repair in atopic dermatitis. J. Clin. Investig. 2013, 123, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Paller, A.S.; Gold, L.F.S.; Soung, J.; Tallman, A.M.; Rubenstein, D.S.; Gooderham, M. Efficacy and patient-reported outcomes from a phase 2b, randomized clinical trial of tapinarof cream for the treatment of adolescents and adults with atopic dermatitis. J. Am. Acad. Dermatol. 2021, 84, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Hammad, H.; Lambrecht, B.N. Barrier Epithelial Cells and the Control of Type 2 Immunity. Immunity 2015, 43, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Leiferman, K.M. Eosinophils in atopic dermatitis. J. Allergy Clin. Immunol. 1994, 94, 1310–1317. [Google Scholar] [CrossRef]
- Menzies-Gow, A.; Ponnarambil, S.; Downie, J.A.; Bowen, K.; Hellqvist, Å.; Colice, G. A phase 3, multicentre, randomized, double-blind, placebo-controlled, parallel-group trial to evaluate the long-term safety and tolerability of tezepelumab in adults and adolescents with severe, uncontrolled asthma. Respir. Res. 2020, 21, 279. [Google Scholar] [CrossRef]
- Mullard, A. Tezepelumab prepares to enter the asthma antibody fray. Nat. Rev. Drug Discov. 2021, 20, 91. [Google Scholar] [CrossRef] [PubMed]
- Simpson, E.L.; Parnes, J.R.; She, D.; Crouch, S.; Rees, W.; Mo, M.; Van Der Merwe, R. Tezepelumab, an anti–thymic stromal lymphopoietin monoclonal antibody, in the treatment of moderate to severe atopic dermatitis: A randomized phase 2a clinical trial. J. Am. Acad. Dermatol. 2019, 80, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Archer, N.K.; Dillen, C.; Wang, Y.; Ashbaugh, A.G.; Ortines, R.V.; Kao, T.; Lee, S.K.; Cai, S.Y.; Miller, R.J.; et al. Staphylococcus aureus Epicutaneous Exposure Drives Skin Inflammation via IL-36-Mediated T Cell Responses. Cell Host Microbe 2017, 22, 653–666.e5. [Google Scholar] [CrossRef] [PubMed]
- Kupper, T.S.; Ballard, D.W.; Chua, A.O.; Mcguire, J.; Flood, P.M.; Horowitz, M.C.; Langdon, R.C.; Lightfoot, L.; Gubler, U. Human keratinocytes contain mRNA indistinguishable from monocyte interleukin 1 alpha and beta mRNA. Keratinocyte epidermal cell-derived thymocyte-activating factor is identical to interleukin 1. J. Exp. Med. 1986, 164, 2095–2100. [Google Scholar] [CrossRef] [PubMed]
- Abramovits, W.; Rivas Bejarano, J.J.; Valdecantos, W.C. Role of interleukin 1 in atopic dermatitis. Dermatol. Clin. 2013, 31, 437–444. [Google Scholar] [CrossRef] [PubMed]
- A Phase II Study of Bermekimab (MABP1) in Patients with Moderate to Severe Atopic Dermatitis. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT03496974 (accessed on 21 December 2023).
- Savinko, T.; Matikainen, S.; Saarialho-Kere, U.; Lehto, M.; Wang, G.; Lehtimäki, S.; Karisola, P.; Reunala, T.; Wolff, H.; Lauerma, A.; et al. IL-33 and ST2 in Atopic dermatitis: Expression profiles and modulation by triggering factors. J. Investig. Dermatol. 2012, 132, 1392–1400. [Google Scholar] [CrossRef]
- Chen, Y.; Gutowska-Owsiak, D.; Hardman, C.S.; Westmoreland, M.; MacKenzie, T.; Cifuentes, L.; Waithe, D.; Lloyd-Lavery, A.; Marquette, A.; Londei, M.; et al. Proof-of-concept clinical trial of etokimab shows a key role for IL-33 in atopic dermatitis pathogenesis. Sci. Transl. Med. 2019, 11, eaax2945. [Google Scholar] [CrossRef] [PubMed]
- Efficacy and Safety of REGN3500 Monotherapy and Combination of REGN3500 Plus Dupilumab in Adult Patients with Moderate-to-Severe Atopic Dermatitis. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT03736967 (accessed on 21 December 2023).
- Zhou, L.; Leonard, A.; Pavel, A.B.; Malik, K.; Raja, A.; Glickman, J.W.; Estrada, Y.; Peng, X.; Del Duca, E.; Sanz-Cabanillas, J.L.; et al. Age-specific changes in the molecular phenotype of patients with moderate-to-severe atopic dermatitis. J. Allergy Clin. Immunol. 2019, 144, 144–156. [Google Scholar] [CrossRef]
- Paller, A.S.; Kabashima, K.; Bieber, T. Therapeutic pipeline for atopic dermatitis: End of the drought? J. Allergy Clin. Immunol. 2017, 140, 633–643. [Google Scholar] [CrossRef]
- Gandhi, N.A.; Bennett, B.L.; Graham, N.M.; Pirozzi, G.; Stahl, N.; Yancopoulos, G.D. Targeting key proximal drivers of type 2 inflammation in disease. Nat. Rev. Drug Discov. 2016, 15, 35–50. [Google Scholar] [CrossRef]
- Roesner, L.M.; Zeitvogel, J.; Heratizadeh, A. Common and different roles of IL-4 and IL-13 in skin allergy and clinical implications. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Popovic, B.; Breed, J.; Rees, D.; Gardener, M.J.; Vinall, L.; Kemp, B.; Spooner, J.; Keen, J.; Minter, R.; Uddin, F.; et al. Structural characterization reveals mechanism of IL-13-Neutralising monoclonal antibody tralokinumab as inhibition of binding to IL-13RA1 and IL-13RA2. J. Mol. Biol. 2017, 429, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Guttman-Yassky, E.; Blauvelt, A.; Eichenfield, L.F.; Paller, A.S.; Armstrong, A.W.; Drew, M.J.R.; Gopalan, R.; Simpson, E.L. Efficacy and safety of lebrikizumab, a High-Affinity interleukin 13 inhibitor, in adults with moderate to severe atopic dermatitis. JAMA Dermatol. 2020, 156, 411. [Google Scholar] [CrossRef] [PubMed]
- Ultsch, M.; Bevers, J.; Nakamura, G.; Vandlen, R.; Kelley, R.F.; Wu, L.C.; Eigenbrot, C. Structural basis of signaling blockade by anti-IL-13 antibody Lebrikizumab. J. Mol. Biol. 2013, 425, 1330–1339. [Google Scholar] [CrossRef]
- Kägi, M.; Joller-Jemelka, H.; Wüthrich, B. Correlation of Eosinophils, Eosinophil Cationic Protein and Soluble lnterleukin-2 Receptor with the Clinical Activity of Atopic Dermatitis. Dermatology 1992, 185, 88–92. [Google Scholar] [CrossRef]
- Simon, D.; Braathen, L.R.; Simon, H. Eosinophils and atopic dermatitis. Allergy 2004, 59, 561–570. [Google Scholar] [CrossRef]
- Tidwell, W.J.; Fowler, J.F. T-cell inhibitors for atopic dermatitis. J. Am. Acad. Dermatol. 2018, 78, S67–S70. [Google Scholar] [CrossRef]
- Kang, E.; Narayana, P.K.; Pouliquen, I.; Lopez, M.C.; Ferreira-Cornwell, M.C.; Getsy, J. Efficacy and safety of mepolizumab administered subcutaneously for moderate to severe atopic dermatitis. Allergy 2019, 75, 950–953. [Google Scholar] [CrossRef]
- Facheris, P.; Jeffery, J.; Del Duca, E.; Guttman-Yassky, E. The translational revolution in atopic dermatitis: The paradigm shifts from pathogenesis to treatment. Cell. Mol. Immunol. 2023, 20, 448–474. [Google Scholar] [CrossRef]
- Saleem, M.; Oussedik, E.; D’Amber, V.; Feldman, S.R. Interleukin-31 pathway and its role in atopic dermatitis: A systematic review. J. Dermatol. Treat. 2017, 28, 591–599. [Google Scholar] [CrossRef]
- Kabashima, K.; Matsumura, T.; Komazaki, H.; Kawashima, M. Trial of Nemolizumab and Topical Agents for atopic dermatitis with Pruritus. N. Engl. J. Med. 2020, 383, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Keam, S.J. Nemolizumab: First approval. Drugs 2022, 82, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, L.; Hacini-Rachinel, F.; Fogel, P.; Rousseau, F.; Xing, X.; Patrick, M.; Billi, A.C.; Berthier, C.C.; Kahlenberg, J.M.; Lazzari, A.; et al. Transcriptomic characterization of prurigo nodularis and the therapeutic response to nemolizumab. J. Allergy Clin. Immunol. 2022, 149, 1329–1339. [Google Scholar] [CrossRef]
- Gündüz, Z. JAK/STAT pathway modulation: Does it work in dermatology? Dermatol. Ther. 2019, 32, e12903. [Google Scholar] [CrossRef]
- Hu, X.; Li, J.; Fu, M.; Zhao, X.; Wang, W. The JAK/STAT signaling pathway: From bench to clinic. Signal Transduct. Target. Ther. 2021, 6, 402. [Google Scholar] [CrossRef]
- Lin, C.M.A.; Cooles, F.A.H.; Isaacs, J.D. Basic mechanisms of JAK inhibition. Mediterr. J. Rheumatol. 2020, 31 (Suppl. S1), 100. [Google Scholar] [CrossRef]
- Silverberg, J.I.; De Bruin-Weller, M.; Bieber, T.; Soong, W.; Kabashima, K.; Costanzo, A.; Rosmarin, D.; Lynde, C.; Liu, J.; Gamelli, A.; et al. Upadacitinib plus topical corticosteroids in atopic dermatitis: Week 52 atopic dermatitis Up study results. J. Allergy Clin. Immunol. 2020, 149, 977–987.e14. [Google Scholar] [CrossRef]
- Simpson, E.L.; Sinclair, R.; Forman, S.; Wollenberg, A.; Aschoff, R.; Cork, M.J.; Bieber, T.; Thyssen, J.P.; Yosipovitch, G.; Flohr, C.; et al. Efficacy and safety of abrocitinib in adults and adolescents with moderate-to-severe atopic dermatitis (JADE MONO-1): A multicentre, double-blind, randomized, placebo-controlled, phase 3 trial. Lancet 2020, 396, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Reich, K.; DeLozier, A.M.; Nunes, F.P.; Thyssen, J.P.; Eichenfield, L.F.; Wollenberg, A.; Terres, J.A.R.; Watts, S.; Chen, Y.F.; Simpson, E.L.; et al. Baricitinib improves symptoms in patients with moderate-to-severe atopic dermatitis and inadequate response to topical corticosteroids: Patient-reported outcomes from two randomized monotherapy phase III trials. J. Dermatol. Treat. 2020, 33, 1521–1530. [Google Scholar] [CrossRef]
- Nakagawa, H.; Nemoto, O.; Igarashi, A.; Saeki, H.; Kabashima, K.; Oda, M.; Nagata, T. Delgocitinib ointment in pediatric patients with atopic dermatitis: A phase 3, randomized, double-blind, vehicle-controlled study and a subsequent open-label, long-term study. J. Am. Acad. Dermatol. 2021, 85, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Bissonnette, R.; Call, R.S.; Raoof, T.J.; Zhu, Z.W.; Yeleswaram, S.; Gong, X.; Lee, M. A Maximum-Use Trial of Ruxolitinib Cream in Adolescents and Adults with Atopic Dermatitis. Am. J. Clin. Dermatol. 2022, 23, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Piscitelli, S.C.; Pavel, A.B.; McHale, K.; Jett, J.E.; Collins, J.; Gillmor, D.; Tabolt, G.; Li, R.; Song, T.; Zhang, N.; et al. A Phase 1b, Randomized, Single-Center Trial of Topical Cerdulatinib (DMVT-502) in Patients with Mild-to-Moderate Atopic Dermatitis. J. Investig. Dermatol. 2021, 41, 1847–1851. [Google Scholar] [CrossRef] [PubMed]
- Landis, M.N.; Arya, M.; Smith, S.; Draelos, Z.D.; Usdan, L.; Tarabar, S.; Pradhan, V.; Aggarwal, S.; Banfield, C.; Peeva, E.; et al. Efficacy and safety of topical brepocitinib for the treatment of mild-to-moderate atopic dermatitis: A phase IIb, randomized, double-blind, vehicle-controlled, dose-ranging and parallel-group study. Br. J. Dermatol. 2022, 187, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Shih, P.Y.; Li, C.; Yong, S. Emerging trends in clinical research on Janus kinase inhibitors for atopic dermatitis treatment. Int. Immunopharmacol. 2023, 124, 111029. [Google Scholar] [CrossRef]
- Czarnowicki, T.; Gonzalez, J.; Shemer, A.; Malajian, D.; Xu, H.; Zheng, X.; Khattri, S.; Gilleaudeau, P.; Sullivan-Whalen, M.; Suárez-Fariñas, M.; et al. Severe atopic dermatitis is characterized by selective expansion of circulating TH2/TC2 and TH22/TC22, but not TH17/TC17, cells within the skin-homing T-cell population. J. Allergy Clin. Immunol. 2015, 136, 104–115.e7. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ito, T.; Wang, Y.; Homey, B.; Watanabe, N.; Martin, R.; Barnes, C.J.; McIntyre, B.W.; Gilliet, M.; Kumar, R.; et al. Maintenance and polarization of human TH2 central memory T cells by thymic stromal Lymphopoietin-Activated dendritic cells. Immunity 2006, 24, 827–838. [Google Scholar] [CrossRef] [PubMed]
- Guttman-Yassky, E.; Pavel, A.B.; Zhou, L.; Estrada, Y.; Zhang, N.; Xu, H.; Peng, X.; Wen, H.; Govas, P.; Gudi, G.; et al. GBR 830, an anti-OX40, improves skin gene signatures and clinical scores in patients with AD. J. Allergy Clin. Immunol. 2019, 144, 482–493.e7. [Google Scholar] [CrossRef]
- Weidinger, S.; Cork, M.; Reich, A.; Bieber, T.; Gilbert, S.; Brennan, N.; Wilson, R.; Lucchesi, D.; Rynkiewicz, N.; Stebegg, M.; et al. 345 Treatment with amlitelimab—A novel non-depleting, non-cytotoxic anti-OX40Ligand monoclonal antibody—Reduces IL-22 serum levels in a phase 2a randomized, placebo-controlled trial in patients with moderate-to-severe atopic dermatitis. Br. J. Dermatol. 2023, 188 (Suppl. S2). [Google Scholar] [CrossRef]
- Kyowa Kirin Announces Positive Phase 2 Results for KHK4083 in Patients with Moderate to Severe Atopic Dermatitis. Available online: https://www.kyowakirin.com/media_center/news_releases/2021/e20210218_01.html (accessed on 21 December 2023).
- Otsuka’s Moizerto® Ointment Granted Approval in Japan as a Treatment for Atopic Dermatitis. Available online: https://www.otsuka.co.jp/en/company/newsreleases/2021/20210927_1.html (accessed on 21 December 2023).
- De Bruin-Weller, M.; Thaçi, D.; Smith, C.; Reich, K.; Cork, M.J.; Radin, A.; Zhang, Q.; Akinlade, B.; Gadkari, A.; Eckert, L.; et al. Dupilumab with concomitant topical corticosteroid treatment in adults with atopic dermatitis with an inadequate response or intolerance to ciclosporin A or when this treatment is medically inadvisable: A placebo-controlled, randomized phase III clinical t. Br. J. Dermatol. 2018, 178, 1083–1101. [Google Scholar] [CrossRef]
- Ungar, B.; Pavel, A.B.; Li, R.; Kimmel, G.W.; Nia, J.K.; Hashim, P.W.; Kim, H.J.; Chima, M.; Vekaria, A.S.; Estrada, Y.; et al. Phase 2 randomized, double-blind study of IL-17 targeting with secukinumab in atopic dermatitis. J. Allergy Clin. Immunol. 2021, 147, 394–397. [Google Scholar] [CrossRef]
- Eyerich, K.; Dimartino, V.; Cavani, A. IL-17 and IL-22 in immunity: Driving protection and pathology. Eur. J. Immunol. 2017, 47, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Gutowska-Owsiak, D.; Schaupp, A.; Salimi, M.; Taylor, S.; Ogg, G.S. Interleukin-22 downregulates filaggrin expression and affects expression of profilaggrin processing enzymes. Br. J. Dermatol. 2011, 165, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Guttman-Yassky, E.; Brunner, P.M.; Neumann, A.U.; Khattri, S.; Pavel, A.B.; Malik, K.; Singer, G.; Baum, D.; Gilleaudeau, P.; Sullivan-Whalen, M.; et al. Efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in adults with moderate-to-severe atopic dermatitis inadequately controlled by conventional treatments: A randomized, double-blind, phase 2a trial. J. Am. Acad. Dermatol. 2018, 78, 872–881.e6. [Google Scholar] [CrossRef] [PubMed]
- Matarazzo, L.; Hernandez-Santana, Y.; Walsh, P.; Fallon, P.G. The IL-1 cytokine family as custodians of barrier immunity. Cytokine 2022, 154, 155890. [Google Scholar] [CrossRef] [PubMed]
- Ihim, S.A.; Abubakar, S.D.; Zian, Z.; Sasaki, T.; Saffarioun, M.; Maleknia, S.; Azizi, G. Interleukin-18 cytokine in immunity, inflammation, and autoimmunity: Biological role in induction, regulation, and treatment. Front. Immunol. 2022, 13, 919973. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, N.; Kimura, T.; Arita, K.; Ariyoshi, M.; Ohnishi, H.; Yamamoto, T.; Zuo, X.; Maenaka, K.; Park, E.Y.; Kondo, N.; et al. The structural basis for receptor recognition of human interleukin-18. Nat. Commun. 2014, 5, 5340. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, S.; Tavecchio, S.; Marzano, A.V.; Buffon, S. Emerging Systemic Treatments for atopic dermatitis. Dermatol. Ther. 2023, 13, 1071–1081. [Google Scholar] [CrossRef]
- Singh, S.; Behl, T.; Sharma, N.; Zahoor, I.; Chigurupati, S.; Yadav, S.; Rachamalla, M.; Sehgal, A.; Naved, T.; Pritima, A.S.; et al. Targeting therapeutic approaches and highlighting the potential role of nanotechnology in atopic dermatitis. Environ. Sci. Pollut. Res. 2022, 29, 32605–32630. [Google Scholar] [CrossRef]
- Sroka-Tomaszewska, J.; Trzeciak, M. Molecular mechanisms of atopic dermatitis pathogenesis. Int. J. Mol. Sci. 2021, 22, 4130. [Google Scholar] [CrossRef]
- Darlenski, R.; Kazandjieva, J.; Hristakieva, E.; Fluhr, J.W. Atopic dermatitis as a systemic disease. Clin. Dermatol. 2014, 32, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Nie, L.; Zou, P.; Suo, J. Drug-loaded PLGA-mPEG microparticles as treatment for atopic dermatitis-like skin lesions in BALB/c mice model. J. Microencapsul. 2014, 32, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Shershakova, N.N.; Baraboshkina, E.H.; Andreev, S.M.; Purgina, D.; Struchkova, I.; Kamyshnikov, O.; Nikonova, A.; Khaitov, M. Anti-inflammatory effect of fullerene C60 in a mice model of atopic dermatitis. J. Nanobiotechnol. 2016, 14, 8. [Google Scholar] [CrossRef] [PubMed]
- Lugović-Mihić, L.; Meštrović-Štefekov, J.; Potočnjak, I.; Cindrić, T.; Ilić, I.; Lovrić, I.; Skalicki, L.; Bešlić, I.; Pondeljak, N. Atopic Dermatitis: Disease Features, Therapeutic Options, and a Multidisciplinary Approach. Life 2023, 13, 1419. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.D.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Jing, M.; Yu, Q.; Ge, X.; Yuan, F.; Shi, L. Treatments in psoriasis: From standard pharmacotherapy to nanotechnology therapy. Postep. Dermatol. I Alergol. 2022, 39, 460–471. [Google Scholar] [CrossRef] [PubMed]
- Damiani, G.; Eggenhöffner, R.; Pigatto, P.D.; Bragazzi, N.L. Nanotechnology meets atopic dermatitis: Current solutions, challenges and future prospects. Insights and implications from a systematic review of the literature. Bioact. Mater. 2019, 4, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Parekh, K.; Mehta, T.; Dhas, N.; Kumar, P.A.; Popat, A. Emerging nanomedicines for the treatment of atopic dermatitis. AAPS Pharmscitech 2021, 22, 55. [Google Scholar] [CrossRef]
- Sun, L.; Liu, Z.; Cun, D.; Tong, H.H.; Zheng, Y. Application of Nano- and Micro-Particles on the topical therapy of Skin-Related Immune Disorders. Curr. Pharm. Des. 2015, 21, 2643–2667. [Google Scholar] [CrossRef]
- Korting, H.C.; Schäfer-Korting, M. Carriers in the topical treatment of skin disease. In Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2009; pp. 435–468. [Google Scholar]
- Akhtar, N.; Verma, A.; Pathak, K. Exploring preclinical and clinical effectiveness of nanoformulations in the treatment of atopic dermatitis: Safety aspects and patent reviews. Bull. Fac. Pharm. Cairo Univ. 2017, 55, 1–10. [Google Scholar] [CrossRef]
- Yu, K.; Wang, Y.; Wan, T.; Zhai, Y.; Cao, S.; Ruan, W.; Wu, C.; Xu, Y. Tacrolimus nanoparticles based on chitosan combined with nicotinamide: Enhancing percutaneous delivery and treatment efficacy for atopic dermatitis and reducing dose. Int. J. Nanomed. 2018, 13, 129–142. [Google Scholar] [CrossRef]
- Bains, P.; Kaur, M.; Kaur, J.; Sharma, S. Nicotinamide: Mechanism of action and indications in dermatology. Indian J. Dermatol. Venereol. Leprol. 2018, 84, 234. [Google Scholar] [CrossRef] [PubMed]
- Fan, Z.; Abourehab, M.A.S.; Hussain, Z. Hyaluronic acid decorated tacrolimus-loaded nanoparticles: Efficient approach to maximize dermal targeting and anti-dermatitis efficacy. Carbohydr. Polym. 2018, 197, 478–489. [Google Scholar]
- Singh, N.; Parashar, P.; Tripathi, C.B.; Kanoujia, J.; Kaithwas, G.; Saraf, S.A. Oral delivery of allopurinol niosomes in treatment of gout in animal model. J. Liposome Res. 2017, 27, 130–138. [Google Scholar] [CrossRef]
- Dong, W.; Wang, X.; Liu, C.; Zhang, X.; Zhang, X.; Chen, X.; Kou, Y.; Mao, S. Chitosan based polymer-lipid hybrid nanoparticles for oral delivery of enoxaparin. Int. J. Pharm. 2018, 547, 499–505. [Google Scholar] [CrossRef]
- Kalam, M.A. Development of chitosan nanoparticles coated with hyaluronic acid for topical ocular delivery of dexamethasone. Int. J. Biol. Macromol. 2016, 89, 127–136. [Google Scholar] [CrossRef]
- Pandey, M.; Choudhury, H.; Gunasegaran, T.A.P.; Nathan, S.; Shadab, G.B.; Tripathy, M.; Hussain, Z. Hyaluronic acid-modified betamethasone encapsulated polymeric nanoparticles: Fabrication, characterization, in vitro release kinetics, and dermal targeting. Drug Deliv. Transl. Res. 2018, 9, 520–533. [Google Scholar] [CrossRef] [PubMed]
- Tessema, E.N.; Gebre-Mariam, T.; Paulos, G.; Wohlrab, J.; Neubert, R.H. Delivery of oat-derived phytoceramides into the stratum corneum of the skin using nanocarriers: Formulation, characterization and in vitro and ex-vivo penetration studies. Eur. J. Pharm. Biopharm. 2018, 127, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, L.C.; Silva-Abreu, M.; Calpena, A.C.; Rodriguez-Lagunas, M.J.; Fabrega, M.J.; Garduno-Ramirez, M.L.; Clares, B. Nanoemulsion strategy of pioglitazone for the treatment of skin inflammatory diseases. Nanomed. Nanotechnol. Biol. Med. 2019, 19, 115–125. [Google Scholar] [CrossRef]
- Alam, M.S.; Ali, M.S.; Alam, N.; Siddiqui, M.R.; Shamim, M.; Safhi, M.M. In vivo study of clobetasol propionate loaded nanoemulsion for topical application in psoriasis and atopic dermatitis. Drug Invent. Today 2013, 5, 8–12. [Google Scholar] [CrossRef]
- Eroglu, I.; Azizoglu, E.; Ozyazici, M.; Nenni, M.; Gurer Orhan, H.; Ozbal, S. Effective topical delivery systems for corticosteroids: Dermatological and histological evaluations. Drug Deliv. 2016, 23, 1502–1513. [Google Scholar] [PubMed]
- El-Menshawe, S.F.; Sayed, O.M.; Abou-Taleb, H.A.; El Tellawy, N. Skin permeation enhancement of nicotinamide through using fluidization and deformability of positively charged ethosomal vesicles: A new approach for treatment of atopic Eczema. J. Drug Deliv. Sci. Technol. 2019, 52, 687–701. [Google Scholar] [CrossRef]
- Chauhan, S.; Gulati, N.; Nagaich, U. Fabrication, and evaluation of ultra deformable vesicles for atopic dermatitis as topical delivery. Int. J. Polym. Mater. Polym. Biomater. 2018, 68, 266–277. [Google Scholar] [CrossRef]
- Carreras, J.J.; Tapia-Ramirez, W.E.; Sala, A.; Guillot, A.J.; Garrigues, T.M.; Melero, A. Ultraflexible lipid vesicles allow topical absorption of cyclosporin A. Drug Deliv. Transl. Res. 2020, 10, 486–497. [Google Scholar] [CrossRef]
- Kang, J.; Chon, J.; Kim, Y.I.; Lee, H.; Oh, D.; Lee, H.; Han, C.; Kim, D.; Park, C. Preparation and evaluation of tacrolimus-loaded thermosensitive solid lipid nanoparticles for improved dermal distribution. Int. J. Nanomed. 2019, 14, 5381–5396. [Google Scholar] [CrossRef]
- Nagaich, U.; Gulati, N. Preclinical Assessment of Steroidal Nanostructured Lipid Carriers Based Gels for Atopic Dermatitis: Optimization and Product Development. Curr. Drug Deliv. 2018, 15, 641–651. [Google Scholar] [CrossRef]
- Eiras, F.; Amaral, M.H.; Silva, R.; Martins, E.; Lobo, J.M.S.; Silva, A.C. Characterization and biocompatibility evaluation of cutaneous formulations containing lipid nanoparticles. Int. J. Pharm. 2017, 519, 373–380. [Google Scholar] [CrossRef]
- Ferreira, M.; Silva, E.; Barreiros, L.; Segundo, M.A.; Costa Lima, S.A.; Reis, S. Methotrexate loaded lipid nanoparticles for topical management of skin-related diseases: Design, characterization and skin permeation potential. Int. J. Pharm. 2016, 512, 14–21. [Google Scholar] [CrossRef]
- Assem, M.; Khowessah, O.M.; Ghorab, D. Nano-crystallization as a tool for the enhancement of beclomethasone dipropionate dermal deposition: Formulation, in vitro characterization and ex vivo study. J. Drug Delivery Sci. Technol. 2019, 54, 101318. [Google Scholar] [CrossRef]
- Pan, W.; Qin, M.; Zhang, G.; Long, Y.; Ruan, W.; Pan, J. Combination of hydrotropic nicotinamide with nanoparticles for enhancing tacrolimus percutaneous delivery. Int. J. Nanomed. 2016, 11, 4037–4050. [Google Scholar]
- Boisgard, A.S.; Lamrayah, M.; Dzikowski, M.; Salmon, D.; Kirilov, P.; Primard, C. Innovative drug vehicle for local treatment of inflammatory skin diseases: Ex vivo and in vivo screening of five topical formulations containing poly(lactic acid) (PLA) nanoparticles. Eur. J. Pharm. Biopharm. Off. J. Arbeitsgemeinschaft Fur Pharm. Verfahrenstechnik 2017, 116, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Zabihi, F.; Graff, P.; Schumacher, F.; Kleuser, B.; Hedtrich, S.; Haag, R. Synthesis of poly(lactide-co-glycerol) as a biodegradable and biocompatible polymer with high loading capacity for dermal drug delivery. Nanoscale 2018, 10, 16848–16856. [Google Scholar] [CrossRef] [PubMed]
- Badihi, A.; Frusic-Zlotkin, M.; Soroka, Y.; Benhamron, S.; Tzur, T.; Nassar, T. Topical nano-encapsulated cyclosporine formulation for atopic dermatitis treatment. Nanomed. Nanotechnol. Biol. Med. 2020, 24, 102140. [Google Scholar] [CrossRef]
- Ozcan, I.; Azizoglu, E.; Senyiit, T.; Ozyazici, M.; Ozer, O. Comparison of PLGA and lecithin/chitosan nanoparticles for dermal targeting of betamethasone valerate. J. Drug Target. 2013, 21, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Katas, H.; Mohd Amin, M.C.; Kumolosasi, E.; Buang, F.; Sahudin, S. Self-assembled polymeric nanoparticles for percutaneous co-delivery of hydrocortisone/hydroxytyrosol: An ex vivo and in vivo study using an NC/Nga mouse model. Int. J. Pharm. 2013, 444, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, A.I.; Costa Lima, S.A.; Reis, S. Development of methotrexate loaded fucoidan/chitosan nanoparticles with anti-inflammatory potential and enhanced skin permeation. Int. J. Biol. Macromol. 2019, 124, 1115–1122. [Google Scholar] [CrossRef] [PubMed]
- Marto, J.; Ruivo, E.; Lucas, S.D.; Goncalves, L.M.; Simoes, S.; Gouveia, L.F. Starch nanocapsules containing a novel neutrophil elastase inhibitor with improved pharmaceutical performance. Eur. J. Pharm. Biopharm. Off. J. Arbeitsgemeinschaft Fur Pharm. Verfahrenstechnik 2018, 127, 1–11. [Google Scholar] [CrossRef]
- Rosa, P.; Friedrich, M.L.; Dos Santos, J.; Librelotto, D.R.N.; Maurer, L.H.; Emanuelli, T. Desonide nanoencapsulation with acai oil as oil core: Physicochemical characterization, photostability study and in vitro phototoxicity evaluation. J. Photochem. Photobiol. 2019, 199, 111606. [Google Scholar] [CrossRef]
- Paiva-Santos, A.C.; Gama, M.; Peixoto, D.; Sousa-Oliveira, I.; Ferreira-Faria, I.; Zeinali, M.; Abbaspour-Ravasjani, S.; Mascarenhas-Melo, F.; Hamishehkar, H.; Veiga, F. Nanocarrier-based dermopharmaceutical formulations for the topical management of atopic dermatitis. Int. J. Pharm. 2022, 618, 121656. [Google Scholar] [CrossRef]
- Daneshmand, S.; Jaafari, M.R.; Movaffagh, J.; Malaekeh-Nikouei, B.; Iranshahi, M.; Moghaddam, A.S.; Najaran, Z.T.; Golmohammadzadeh, S. Preparation, characterization, and optimization of auraptene-loaded solid lipid nanoparticles as a natural anti-inflammatory agent: In vivo and in vitro evaluations. Colloids Surf. B Biointerfaces 2018, 164, 332–339. [Google Scholar] [CrossRef]
- Kitaoka, M.; Nguyen, T.C.; Goto, M. Water-in-oil microemulsions composed of monoolein enhanced the transdermal delivery of nicotinamide. Int. J. Cosmet. Sci. 2021, 43, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Q.; Xie, Y.; Wang, J. Effect of mizolastine on atopic dermatitis and its possible mechanisms. Med. J. Wuhan Univ. 2017, 38, 313–316. [Google Scholar]
- Pal, R.R.; Maurya, A.K.; Parashar, P.; Saraf, S.A. A Comparative Study of Levocetirizine Loaded Vesicular and Matrix Type System for Topical Application: Appraisal of Therapeutic Potential against atopic dermatitis. J. Pharm. Innov. 2020, 16, 469–480. [Google Scholar] [CrossRef]
- Krakowski, A.C.; Eichenfield, L.F.; Dohil, M. Management of atopic dermatitis in the pediatric population. Pediatrics 2008, 122, 812–824. [Google Scholar] [CrossRef] [PubMed]
- Protopic 0.03% Ointment–Summary of Product Characteristics (SmPC). Available online: https://www.medicines.org.uk/emc/product/1612/smpc#gref (accessed on 21 December 2023).
- Luk, D.C.K.; Hon, K.L.; Dizon, M.V.; Leong, K.; Tay, Y.; Koh, M.J.; Chandran, N.S.; Wananukul, S.; Chatproedprai, S.; Luger, T.A. Practical recommendations for the topical treatment of atopic dermatitis in South and East Asia. Dermatol. Ther. 2020, 11, 275–291. [Google Scholar] [CrossRef] [PubMed]
- National Eczema Society. Methotrexate. Available online: https://eczema.org/information-and-advice/treatments-for-eczema/methotrexate/#:~:text=Methotrexate%20works%20as%20an%20immunosuppressant,the%20skin%20that%20drive%20eczema (accessed on 21 December 2023).
- Wollenberg, A.; Barbarot, S.; Bieber, T.; Christen-Zaech, S.; Deleuran, M.; Fink-Wagner, A.; Gieler, U.; Girolomoni, G.; Lau, S.K.C.; Muraro, A.; et al. Consensus-based European guidelines for treatment of atopic Eczema (atopic dermatitis) in adults and children: Part II. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 850–878. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, J.I.; Yosipovitch, G.; Simpson, E.L.; Kim, B.; Wu, J.J.; Eckert, L.; Guillemin, I.; Chen, Z.; Ardeleanu, M.; Bansal, A.; et al. Dupilumab treatment results in early and sustained improvements in itch in adolescents and adults with moderate to severe atopic dermatitis: Analysis of the randomized phase 3 studies SOLO 1 and SOLO 2, AD ADOL, and CHRONOS. J. Am. Acad. Dermatol. 2020, 82, 1328–1336. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.E.; Clark, A.K.; Tran, K.; Shi, V.Y. New and emerging targeted systemic therapies: A new era for atopic dermatitis. J. Dermatol. Treat. 2017, 29, 364–374. [Google Scholar] [CrossRef]
- Cork, M.J.; Eckert, L.; Simpson, E.L.; Armstrong, A.W.; Barbarot, S.; Puig, L.; Girolomoni, G.; De Bruin-Weller, M.; Wollenberg, A.; Kataoka, Y.; et al. Dupilumab improves patient-reported symptoms of atopic dermatitis, symptoms of anxiety and depression, and health-related quality of life in moderate-to-severe atopic dermatitis: Analysis of pooled data from the randomized trials SOLO 1 and SOLO 2. J. Dermatol. Treat. 2019, 31, 606–614. [Google Scholar] [CrossRef]
- Barbarot, S.; Wollenberg, A.; Silverberg, J.I.; Deleuran, M.; Pellacani, G.; Hita, J.C.A.; Chen, Z.; Shumel, B.; Eckert, L.; Gadkari, A.; et al. Dupilumab provides rapid and sustained improvement in SCORAD outcomes in adults with moderate-to-severe atopic dermatitis: Combined results of four randomized phase 3 trials. J. Dermatol. Treat. 2020, 33, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Perche, P.O.; Cook, M.K.; Feldman, S.R. Abrocitinib: A new FDA-Approved drug for Moderate-to-Severe AD. Ann. Pharmacother. 2022, 57, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Fierce Pharma. Can Sanofi and Regeneron’s Dupixent Steal Half of a $21B Eczema Market? Not So Fast: Analyst. Available online: https://www.fiercepharma.com/pharma/can-sanofi-and-regeneron-s-dupixent-steal-half-a-21b-eczema-market-not-so-fast-analyst (accessed on 21 December 2023).
- Fuxench, Z.C.C.; Block, J.; Boguniewicz, M.; Boyle, J.; Fonacier, L.; Gelfand, J.M.; Grayson, M.H.; Margolis, D.J.; Mitchell, L.; Silverberg, J.I.; et al. Atopic dermatitis in America Study: A Cross-Sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J. Investig. Dermatol. 2019, 139, 583–590. [Google Scholar] [CrossRef]
- Hon, K.L.; Leung, A.K.C.; Leung, T.N.; Lee, V. Investigational drugs for atopic dermatitis. Expert Opin. Investig. Drugs 2018, 27, 637–647. [Google Scholar] [CrossRef]
- Kleinman, E.; Laborada, J.; Metterle, L.; Eichenfield, L.F. What’s new in topicals for atopic dermatitis? Am. J. Clin. Dermatol. 2022, 23, 595–603. [Google Scholar] [CrossRef]
- Bissonnette, R.; Papp, K.; Poulin, Y.; Gooderham, M.; Raman, M.; Mallbris, L.; Wang, C.; Purohit, V.S.; Mamolo, C.; Papacharalambous, J.; et al. Topical tofacitinib for atopic dermatitis: A phase II a randomized trial. Br. J. Dermatol. 2016, 175, 902–911. [Google Scholar] [CrossRef] [PubMed]
- Owji, S.; Caldas, S.A.; Ungar, B. Management of Atopic Dermatitis: Clinical Utility of Ruxolitinib. J. Asthma Allergy 2022, 15, 1527–1537. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pareek, A.; Kumari, L.; Pareek, A.; Chaudhary, S.; Ratan, Y.; Janmeda, P.; Chuturgoon, S.; Chuturgoon, A. Unraveling Atopic Dermatitis: Insights into Pathophysiology, Therapeutic Advances, and Future Perspectives. Cells 2024, 13, 425. https://doi.org/10.3390/cells13050425
Pareek A, Kumari L, Pareek A, Chaudhary S, Ratan Y, Janmeda P, Chuturgoon S, Chuturgoon A. Unraveling Atopic Dermatitis: Insights into Pathophysiology, Therapeutic Advances, and Future Perspectives. Cells. 2024; 13(5):425. https://doi.org/10.3390/cells13050425
Chicago/Turabian StylePareek, Ashutosh, Lipika Kumari, Aaushi Pareek, Simran Chaudhary, Yashumati Ratan, Pracheta Janmeda, Sanam Chuturgoon, and Anil Chuturgoon. 2024. "Unraveling Atopic Dermatitis: Insights into Pathophysiology, Therapeutic Advances, and Future Perspectives" Cells 13, no. 5: 425. https://doi.org/10.3390/cells13050425
APA StylePareek, A., Kumari, L., Pareek, A., Chaudhary, S., Ratan, Y., Janmeda, P., Chuturgoon, S., & Chuturgoon, A. (2024). Unraveling Atopic Dermatitis: Insights into Pathophysiology, Therapeutic Advances, and Future Perspectives. Cells, 13(5), 425. https://doi.org/10.3390/cells13050425





