Cytological Study of Topical Effect of Azelastine Hydrochloride on the Nasal Mucous Membrane Cells in Various Nasal Rhinitis Types
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Methodology of Performing Swabs and Their Evaluation
2.3. Statistical Analysis
3. Results
3.1. Analysis of Nasal Mucosal Cells of Patients with Rhinitis Symptoms Based on Swabs Taken before Treatment: Evaluation in Relation to the Control Group
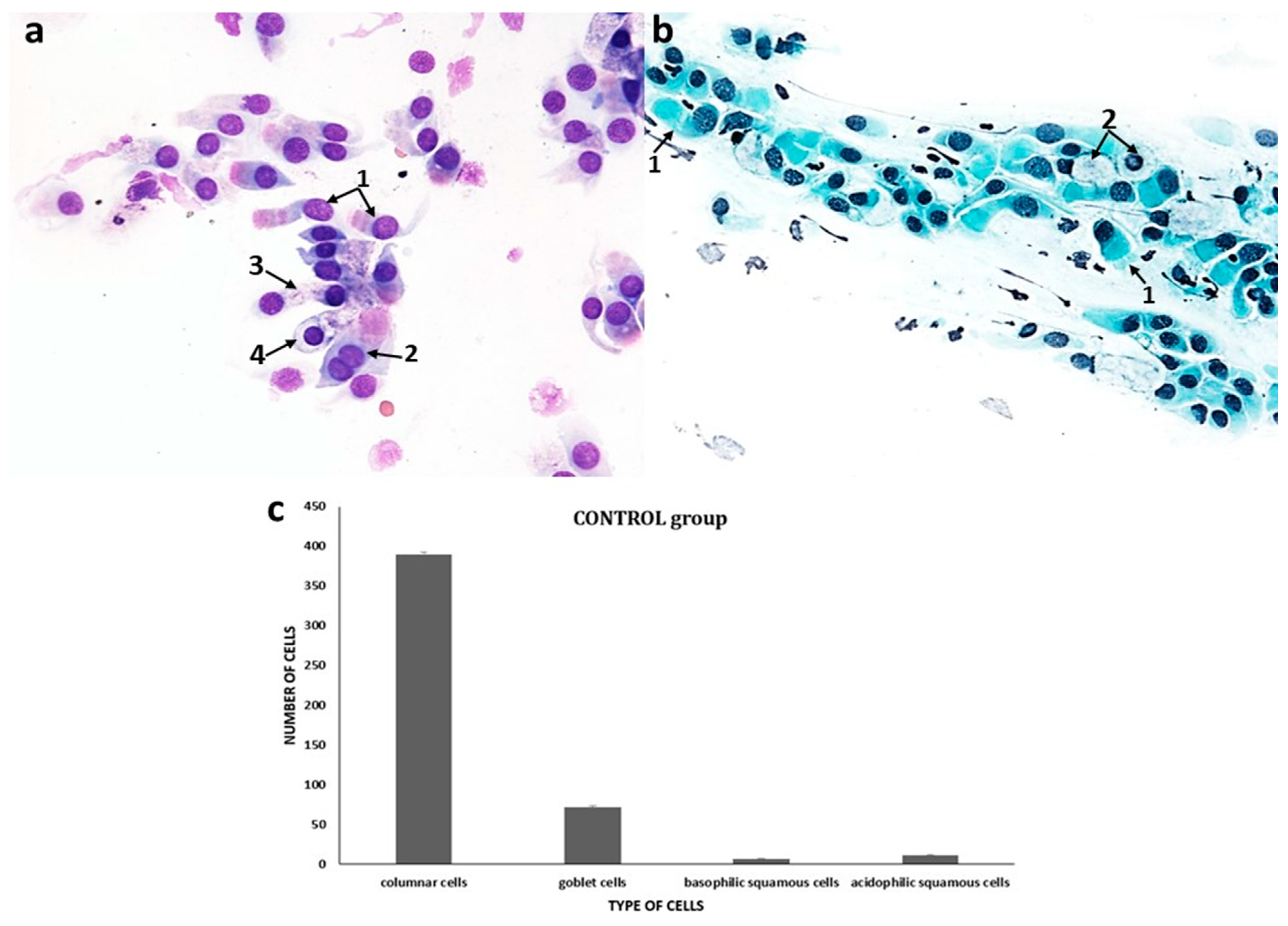
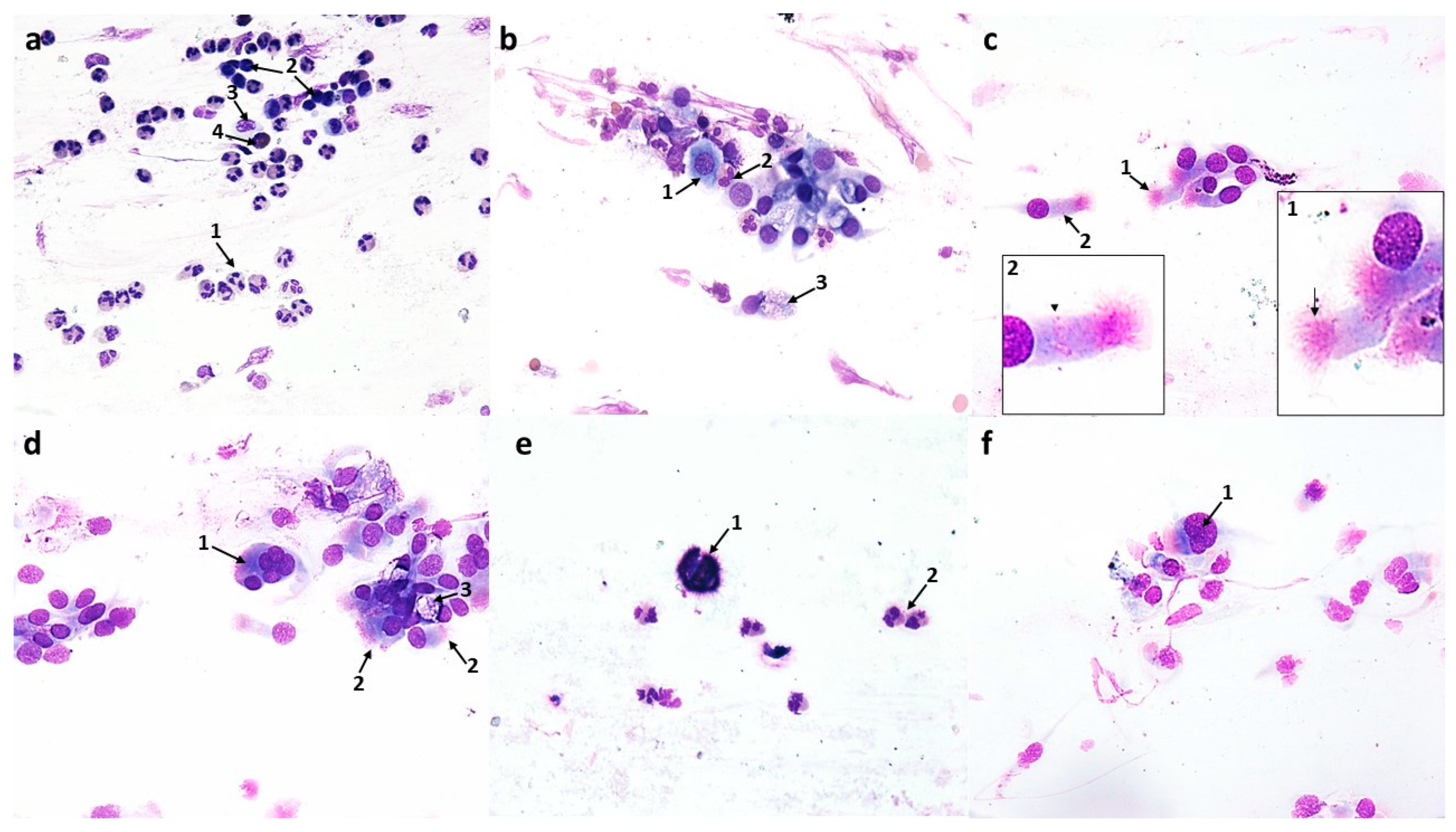
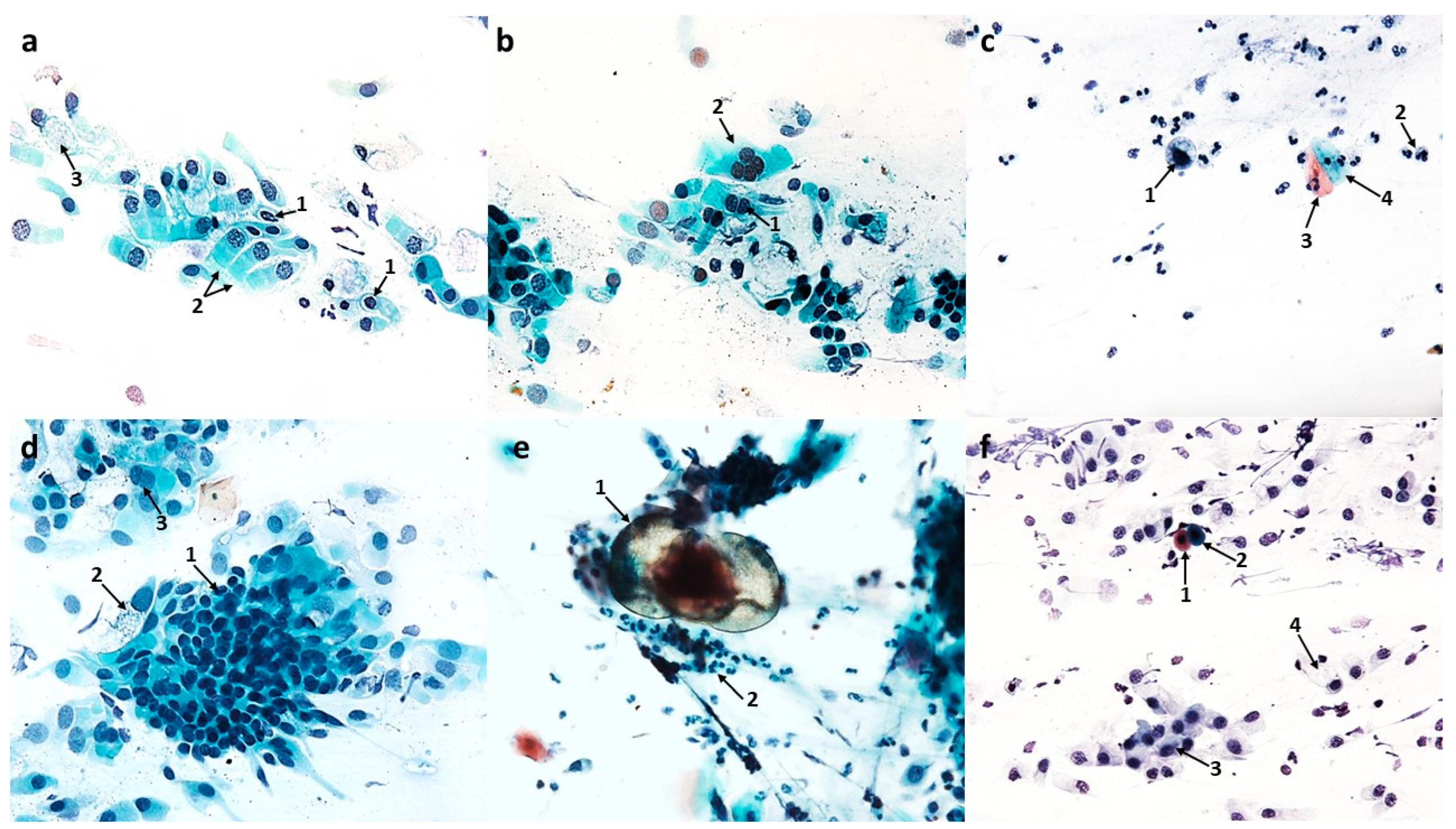
3.1.1. Normal Cytogram of the Nasal Mucosa
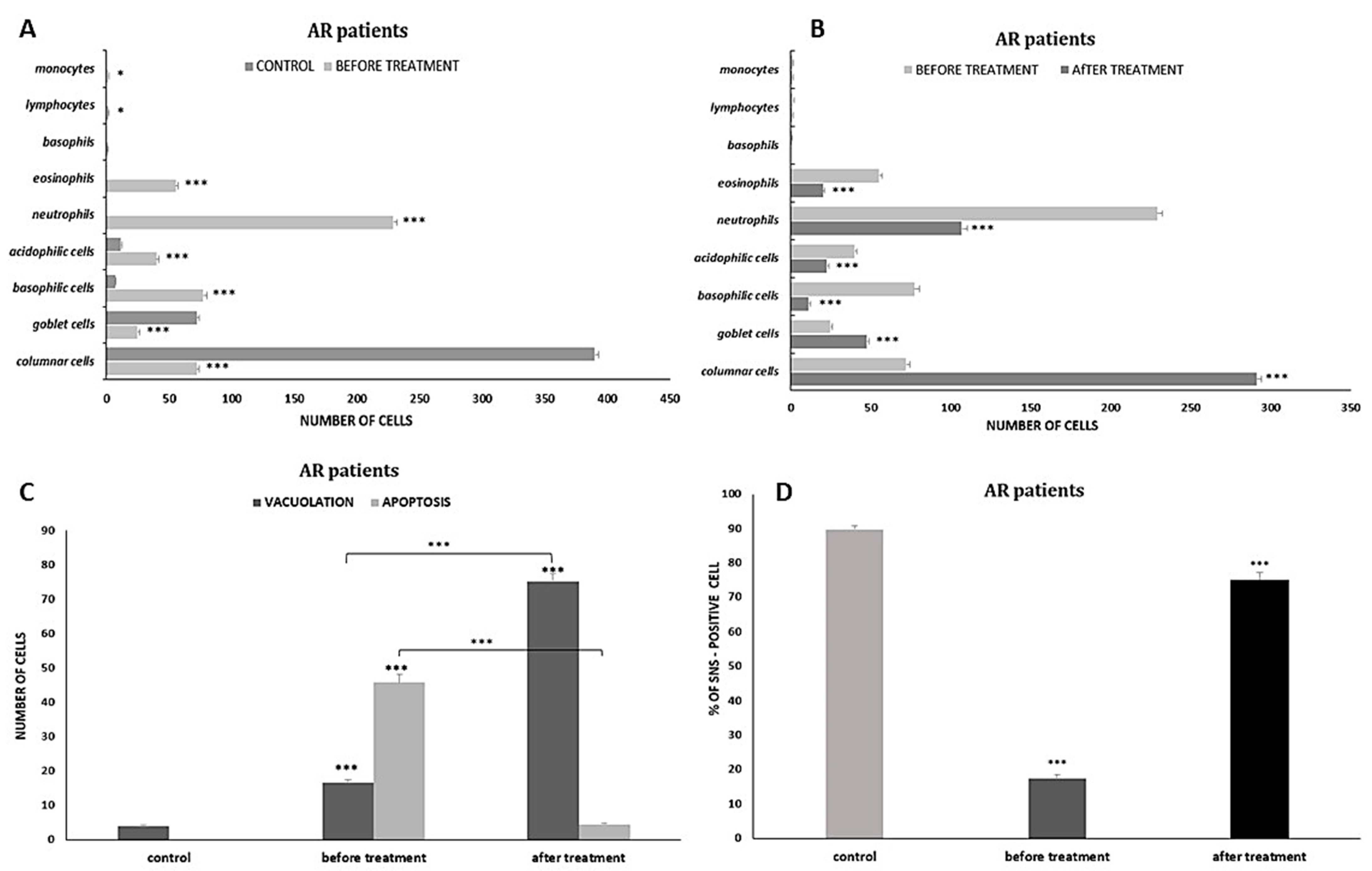
3.1.2. Cytological Profile of Allergic Rhinitis (AR)

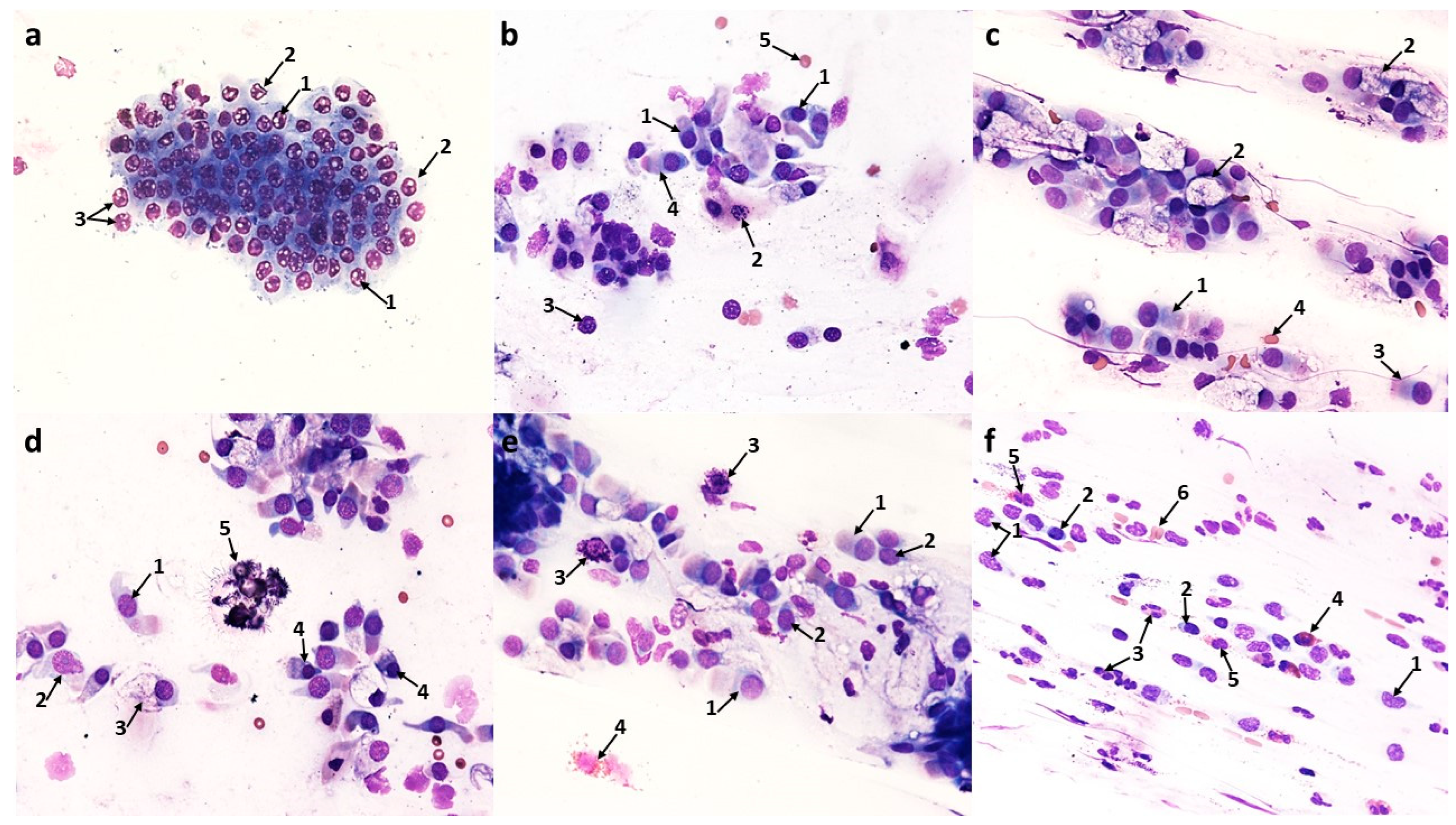
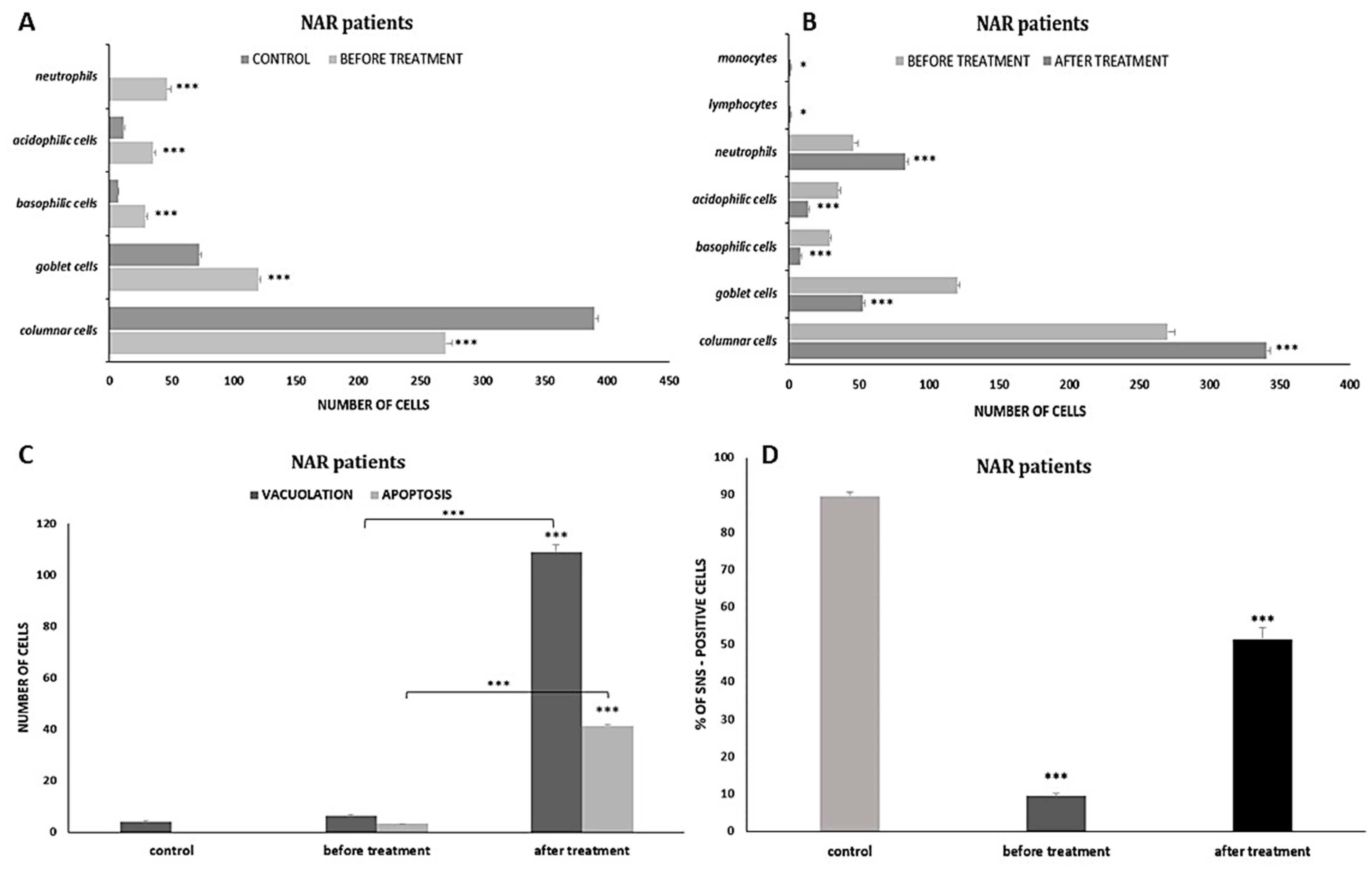
3.1.3. Cytological Profile of Nonallergic/Vasomotor Rhinitis (NAR/VMR)

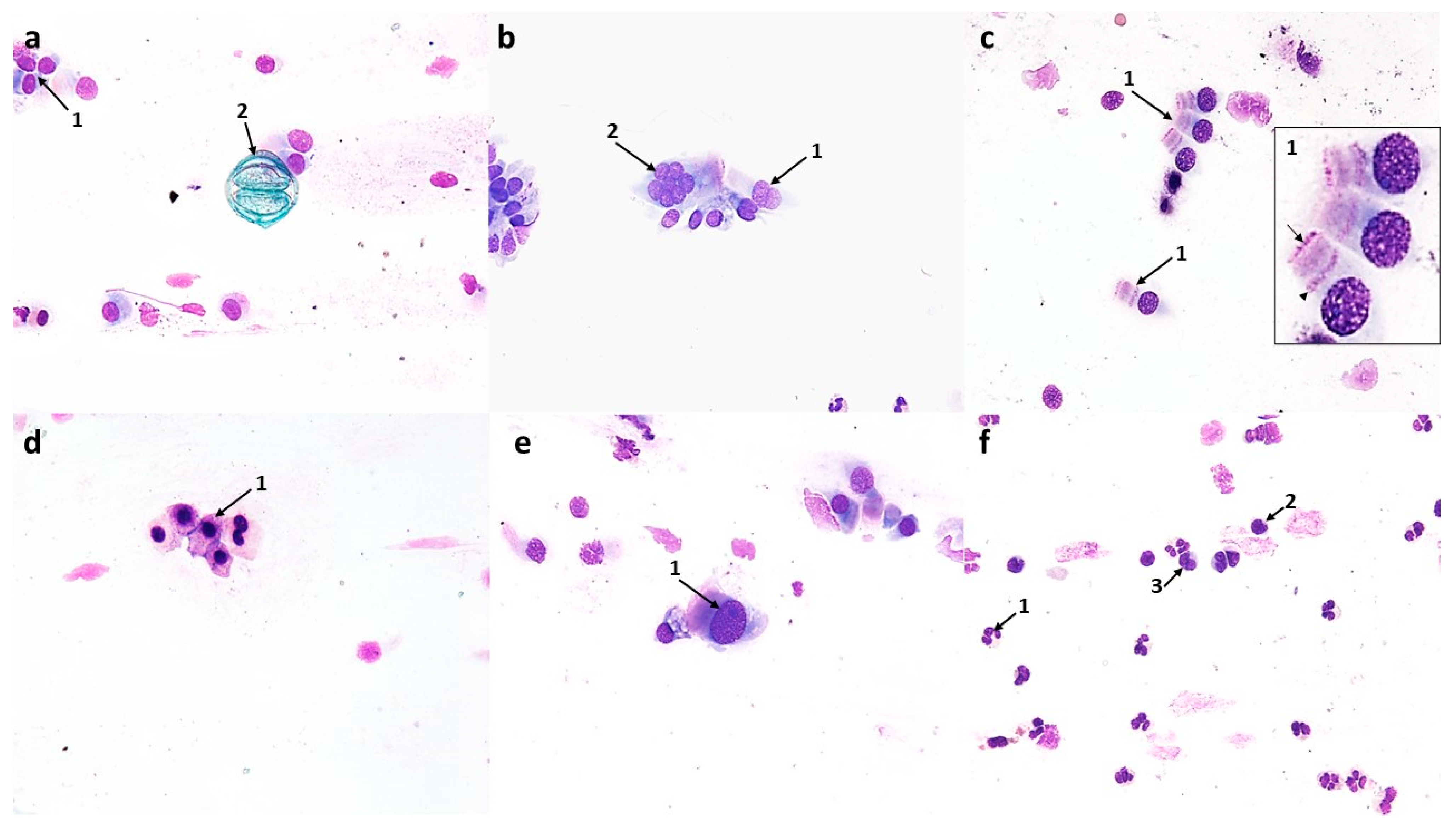
3.2. Analysis of Nasal Mucosal Cells of Patients with Rhinitis Symptoms Based on Swabs Taken after Treatment with Azelastine Hydrochloride: Evaluation in Relation to the State before Treatment
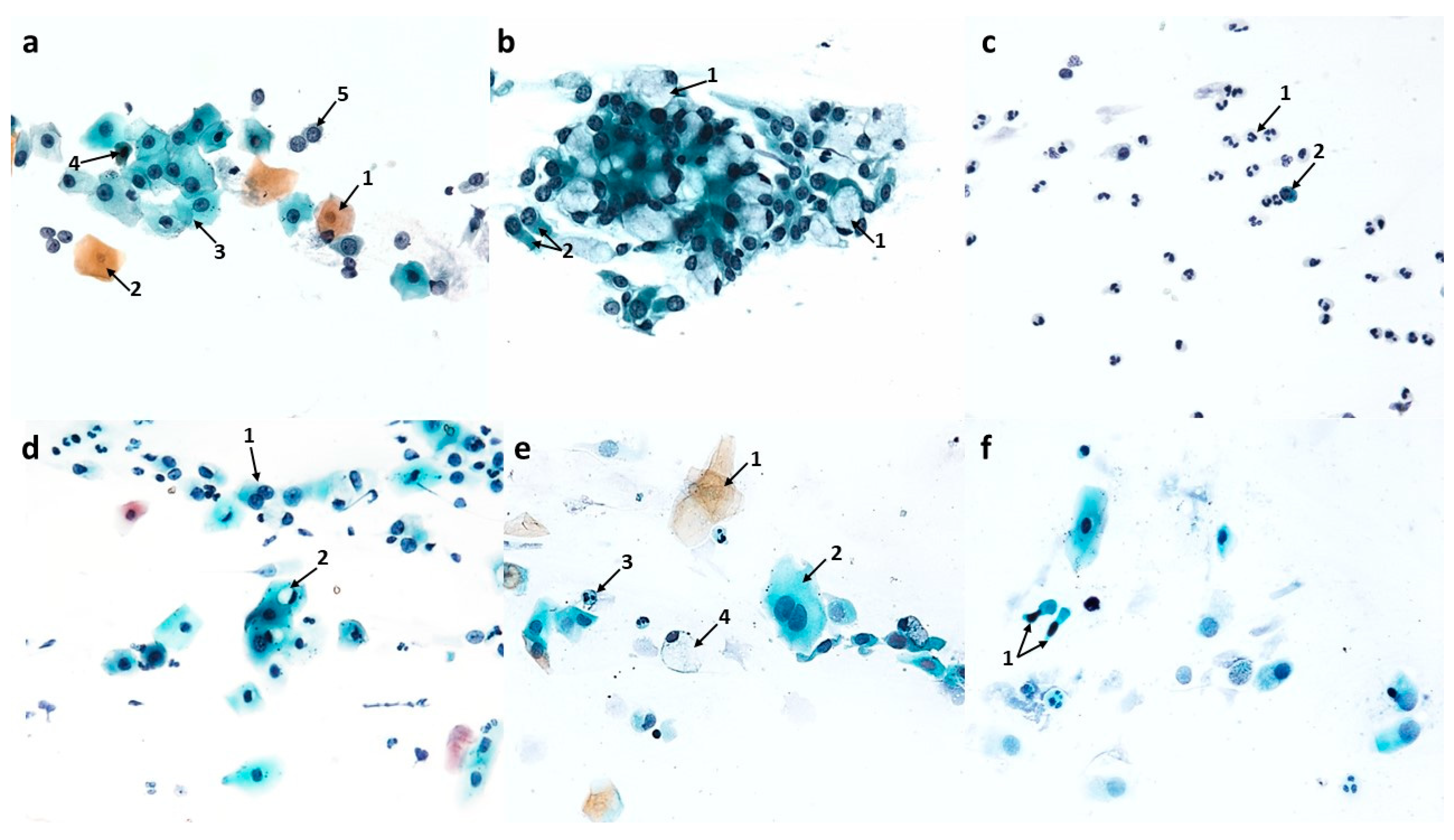
3.2.1. Changes Induced in Nasal Mucosal Cells of Patients with Allergic Rhinitis (AR)
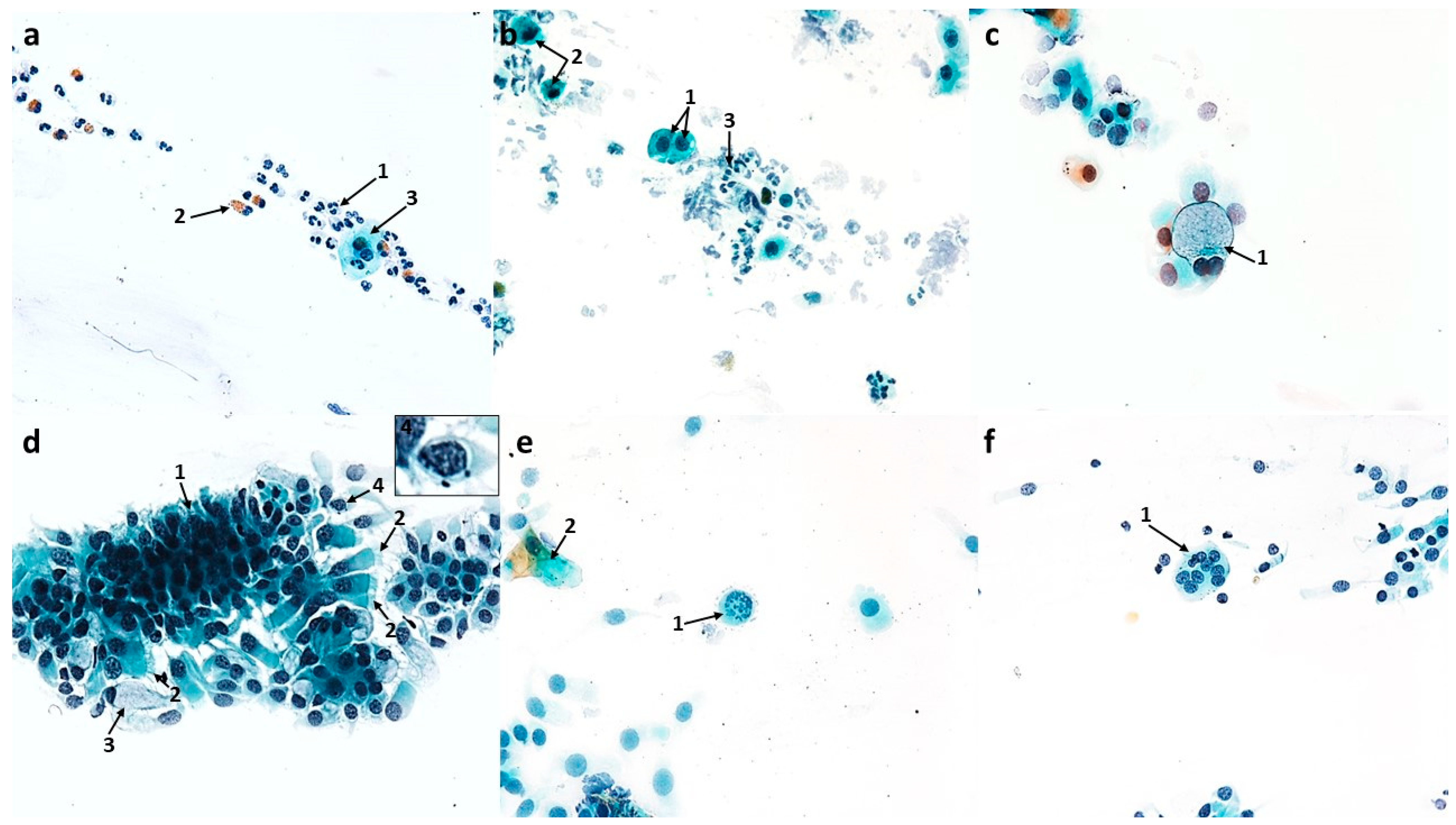
3.2.2. Changes Induced in Nasal Mucosal Cells of Patients with Nonallergic/Vasomotor Rhinitis (NAR/VMR)


4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Procopiou, P.A.; Ford, A.J.; Gore, P.M.; Looker, B.E.; Hodgson, S.T.; Holmes, D.S.; Vile, S.; Clark, K.L.; Saunders, K.A.; Slack, R.J.; et al. Design of Phthalazinone Amide Histamine H(1) Receptor Antagonists for Use in Rhinitis. ACS Med. Chem. Lett. 2017, 8, 577–581. [Google Scholar] [CrossRef]
- Lee, C.; Corren, J. Review of azelastine nasal spray in the treatment of allergic and non-allergic rhinitis. Expert Opin. Pharmacother. 2007, 8, 701–709. [Google Scholar] [CrossRef]
- Ellis, A.K.; Zhu, Y.; Steacy, L.M.; Walker, T.; Day, J.H. A four-way, double-blind, randomized, placebo controlled study to determine the efficacy and speed of azelastine nasal spray, versus loratadine, and cetirizine in adult subjects with allergen-induced seasonal allergic rhinitis. Allergy Asthma Clin. Immunol. 2013, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Horbal, J.M.; Bernstein, J.A. Azelastine HCl: A Review of the Old and New Formulations. Clin. Med. Insights Ther. 2010, 2, 427–437. [Google Scholar] [CrossRef]
- Bernstein, J.A. Azelastine hydrochloride: A review of pharmacology, pharmacokinetics, clinical efficacy and tolerability. Curr. Med. Res. Opin. 2007, 23, 2441–2452. [Google Scholar] [CrossRef] [PubMed]
- Marshall, G.D., Jr. Therapeutic options in allergic disease: Antihistamines as systemic antiallergic agents. J. Allergy Clin. Immunol. 2000, 106 (Suppl. S5), S303–S309. [Google Scholar] [CrossRef] [PubMed]
- Watts, A.M.; Cripps, A.W.; West, N.P.; Cox, A.J. Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers with Topical Pharmaceutical Agents. Front. Pharmacol. 2019, 10, 294. [Google Scholar] [CrossRef]
- Criado, P.R.; Criado, R.F.; Maruta, C.W.; Machado Filho, C. Histamine, histamine receptors and antihistamines: New concepts. An. Bras. Dermatol. 2010, 85, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Hill, S.J.; Ganellin, C.R.; Timmerman, H.; Schwartz, J.C.; Shankley, N.P.; Young, J.M.; Schunack, W.; Levi, R.; Haas, H.L. International Union of Pharmacology. XIII. Classification of histamine receptors. Pharmacol. Rev. 1997, 49, 253–278. [Google Scholar] [PubMed]
- Konrat, R.; Papp, H.; Kimpel, J.; Rossler, A.; Szijarto, V.; Nagy, G.; Madai, M.; Zeghbib, S.; Kuczmog, A.; Lanszki, Z.; et al. The Anti-Histamine Azelastine, Identified by Computational Drug Repurposing, Inhibits Infection by Major Variants of SARS-CoV-2 in Cell Cultures and Reconstituted Human Nasal Tissue. Front. Pharmacol. 2022, 13, 861295. [Google Scholar] [CrossRef]
- Papadopoulos, N.G.; Aggelides, X.; Stamataki, S.; Prokopakis, E.; Katotomichelakis, M.; Xepapadaki, P. New concepts in pediatric rhinitis. Pediatr. Allergy Immunol. 2021, 32, 635–646. [Google Scholar] [CrossRef]
- Berger, W.; Sher, E.; Gawchik, S.; Fineman, S. Safety of a novel intranasal formulation of azelastine hydrochloride and fluticasone propionate in children: A randomized clinical trial. Allergy Asthma Proc. 2018, 39, 110–116. [Google Scholar] [CrossRef]
- Church, M.K. Allergy, Histamine and Antihistamines. Handb. Exp. Pharmacol. 2017, 241, 321–331. [Google Scholar]
- Horak, F. Effectiveness of twice daily azelastine nasal spray in patients with seasonal allergic rhinitis. Ther. Clin. Risk Manag. 2008, 4, 1009–1022. [Google Scholar] [CrossRef]
- Patel, D.; Garadi, R.; Brubaker, M.; Conroy, J.P.; Kaji, Y.; Crenshaw, K.; Whitling, A.; Wall, G.M. Onset and duration of action of nasal sprays in seasonal allergic rhinitis patients: Olopatadine hydrochloride versus mometasone furoate monohydrate. Allergy Asthma Proc. 2007, 28, 592–599. [Google Scholar] [CrossRef]
- Kalpaklioglu, A.F.; Kavut, A.B. Comparison of azelastine versus triamcinolone nasal spray in allergic and nonallergic rhinitis. Am. J. Rhinol. Allergy 2010, 24, 29–33. [Google Scholar] [CrossRef]
- Scadding, G.K.; Kariyawasam, H.H.; Scadding, G.; Mirakian, R.; Buckley, R.J.; Dixon, T.; Durham, S.R.; Farooque, S.; Jones, N.; Leech, S.; et al. BSACI guideline for the diagnosis and management of allergic and non-allergic rhinitis (Revised Edition 2017; First edition 2007). Clin. Exp. Allergy 2017, 47, 856–889. [Google Scholar] [CrossRef]
- Ciprandi, G. Treatment of nonallergic perennial rhinitis. Allergy 2004, 59, 16–22; discussion 22–23. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Q.; Xie, Y.; Wang, Z.; Li, D.; Ma, L.; Pang, X.; Yu, W.; Zhong, N. The normative value of inflammatory cells in the nasal perfusate of Chinese adults: A pilot study. J. Thorac. Dis. 2014, 6, 905–912. [Google Scholar]
- Heffler, E.; Landi, M.; Caruso, C.; Fichera, S.; Gani, F.; Guida, G.; Liuzzo, M.T.; Pistorio, M.P.; Pizzimenti, S.; Riccio, A.M.; et al. Nasal cytology: Methodology with application to clinical practice and research. Clin. Exp. Allergy 2018, 48, 1092–1106. [Google Scholar] [CrossRef]
- Gelardi, M.; Iannuzzi, L.; Quaranta, N.; Landi, M.; Passalacqua, G. NASAL cytology: Practical aspects and clinical relevance. Clin. Exp. Allergy 2016, 46, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Gelardi, M.; Fiorella, M.L.; Leo, G.; Incorvaia, C. Cytology in the diagnosis of rhinosinusitis. Pediatr. Allergy Immunol. 2007, 18, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Anniko, M.; Bernal-Sprekelsen, M.; Bonkowsky, V.; Bradley, P.; Iurato, S. Otorhinolaryngology, Head and Neck Surgery; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Rutland, J.; Dewar, A.; Cox, T.; Cole, P. Nasal brushing for the study of ciliary ultrastructure. J. Clin. Pathol. 1982, 35, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Yum, H.Y.; Ha, E.K.; Shin, Y.H.; Han, M.Y. Prevalence, comorbidities, diagnosis, and treatment of nonallergic rhinitis: Real-world comparison with allergic rhinitis. Clin. Exp. Pediatr. 2021, 64, 373–383. [Google Scholar] [CrossRef]
- Gelardi, M.; Luigi Marseglia, G.; Licari, A.; Landi, M.; Dell’Albani, I.; Incorvaia, C.; Frati, F.; Quaranta, N. Nasal cytology in children: Recent advances. Ital. J. Pediatr. 2012, 38, 51. [Google Scholar] [CrossRef][Green Version]
- Ciofalo, A.; Pasquariello, B.; Iannella, G.; Manno, A.; Angeletti, D.; Gulotta, G.; Pace, A.; Magliulo, G. The role of nasal cytology in the diagnosis of allergic and non-allergic rhinitis in adult and children. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 5065–5073. [Google Scholar]
- Pipolo, C.; Bianchini, S.; Barberi, S.; Landi, M.; D’Auria, E.; Fuccillo, E.; Gaffuri, M.; Marchisio, P.; Rosazza, C.; Saibene, A.M.; et al. Nasal cytology in children: Scraping or swabbing? Rhinology 2017, 55, 242–250. [Google Scholar] [CrossRef]
- Ciofalo, A.; Cavaliere, C.; Incorvaia, C.; Plath, M.; Ridolo, E.; Pucciarini, F.; Altissimi, G.; Greco, A.; de Vincentiis, M.; Masieri, S. Diagnostic performance of nasal cytology. Eur. Arch. Otorhinolaryngol. 2022, 279, 2451–2455. [Google Scholar] [CrossRef]
- Poddighe, D.; Gelardi, M.; Licari, A.; Del Giudice, M.M.; Marseglia, G.L. Non-allergic rhinitis in children: Epidemiological aspects, pathological features, diagnostic methodology and clinical management. World J. Methodol. 2016, 6, 200–213. [Google Scholar] [CrossRef]
- Canakcioglu, S.; Tahamiler, R.; Saritzali, G.; Alimoglu, Y.; Isildak, H.; Guvenc, M.G.; Acar, G.O.; Inci, E. Evaluation of nasal cytology in subjects with chronic rhinitis: A 7-year study. Am. J. Otolaryngol. 2009, 30, 312–317. [Google Scholar] [CrossRef]
- Ingels, K.; Durdurez, J.P.; Cuvelier, C.; van Cauwenberge, P. Nasal biopsy is superior to nasal smear for finding eosinophils in nonallergic rhinitis. Allergy 1997, 52, 338–341. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, J.; Zhou, Y.; Zhang, L.; Wang, Y.; Pepper, A.N.; Cho, S.H.; Kong, W. Individualized Treatment of Allergic Rhinitis According to Nasal Cytology. Allergy Asthma Immunol. Res. 2017, 9, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Diwakar, C.; Kumar, S.; Seema, K.; Aslami, N.A.; Alwa, B. A comparative study of nasal smear and nasal biopsy in the confirmation of the diagnosis of allergic rhinitis in a tertiary hospital of Rohtas district, Bihar. Int. J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 815–818. [Google Scholar] [CrossRef]
- Qamar, S.; Awan, N.; Cheema, K.M.; Raza, N.; Ashraf, S.; Rehman, A. Comparative Analysis of Nasal Smear Eosinophilia and Serum IgE Levels for the Diagnosis of Allergic Rhinitis. J. Coll. Physicians Surg. Pak. 2020, 30, 1297–1300. [Google Scholar] [PubMed]
- Choi, Y.; Jeon, H.; Yang, E.A.; Yoon, J.S.; Kim, H.H. Nasal eosinophilia and eosinophil peroxidase in children and adolescents with rhinitis. Korean J. Pediatr. 2019, 62, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Zyla, M.; Lesniak, M.; Myszkowska, D.; Dabal, E.; Lorenc, J.; Wojtaszek-Czapla, M.; Obtulowicz, K.; Czarnobilska, E. Eosinophilic reaction in nasal cytology in patients sensitive to perennial and seasonal allergens. Przegląd Lek. 2013, 70, 1038–1042. [Google Scholar]
- Mierzejewska, A.; Jung, A.; Kalicki, B. Nasal Cytology as a Marker of Atopy in Children. Dis. Markers 2017, 2017, 4159251. [Google Scholar] [CrossRef]
- Bartoli, M.L.; Cristofani-Mencacci, L.; Scarano, M.; Nacci, A.; Latorre, M.; Bacci, E.; Paggiaro, P.; Seccia, V. Nasal Cytology: A Comparative Study of Two Different Techniques of Processing-Smeared versus Cytocentrifuged Slides. Mediat. Inflamm. 2018, 2018, 1640180. [Google Scholar] [CrossRef]
- Yamasaki, A.; Okazaki, R.; Harada, T. Neutrophils and Asthma. Diagnostics 2022, 12, 1175. [Google Scholar] [CrossRef]
- Arebro, J.; Ekstedt, S.; Hjalmarsson, E.; Winqvist, O.; Kumlien Georen, S.; Cardell, L.O. A possible role for neutrophils in allergic rhinitis revealed after cellular subclassification. Sci. Rep. 2017, 7, 43568. [Google Scholar] [CrossRef]
- Ciprandi, G.; Buscaglia, S.; Pesce, G.; Pronzato, C.; Ricca, V.; Parmiani, S.; Bagnasco, M.; Canonica, G.W. Minimal persistent inflammation is present at mucosal level in patients with asymptomatic rhinitis and mite allergy. J. Allergy Clin. Immunol. 1995, 96, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Gelardi, M.; Incorvaia, C.; Fiorella, M.L.; Petrone, P.; Quaranta, N.; Russo, C.; Puccinelli, P.; Dell’Albani, I.; Riario-Sforza, G.G.; Cattaneo, E.; et al. The clinical stage of allergic rhinitis is correlated to inflammation as detected by nasal cytology. Inflamm. Allergy Drug Targets 2011, 10, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Chanda, R.; Aggarwal, A.; Kohli, G.; Jaswal, T.; Gupta, K. Comparative study of nasal smear and biopsy in patients of Allergic Rhinitis. Indian J. Allergy Asthma Immunol. 2002, 16, 27–31. [Google Scholar]
- Szalay, L. Cytopathology of the Uterine Cervix, 1st ed.; Medical: Wien, Austria, 1990; pp. 1–304. [Google Scholar]
- Gelardi, M.; Cassano, P.; Cassano, M.; Fiorella, M.L. Nasal cytology: Description of a hyperchromatic supranuclear stria as a possible marker for the anatomical and functional integrity of the ciliated cell. Am. J. Rhinol. 2003, 17, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Gelardi, M.; Guerra, L.; Giangregorio, N.; Cassano, M.; Favia, M.; Ciprandi, G. The hyperchromatic supranuclear stria corresponds to the Golgi apparatus in nasal ciliated cells. Acta Biomed. 2020, 91, 373–375. [Google Scholar] [PubMed]
- Myszkowska, D.; Kubicka, J.; Gawlik, J.; Obtulowicz, K.; Czarnobilska, E. Squamous epithelium in the nasal cytology. Przegląd Lek. 2015, 72, 731–735. [Google Scholar]
- Chosia, M.; Domagała, W. Cytodiagnostyka Szyjki Macicy Podręcznik Dla Cytomorfologów Medycznych, 2nd ed.; Fundacja Pro Pharmacia Futura: Warsaw, Poland, 2017. [Google Scholar]
- Gelardi, M. Atlas of Nasal Cytology for the Differential Diagnosis of Nasal Diseases, 2nd ed.; Edi Ermes Exclusive: Rochester, MN, USA, 2012; pp. 1–194. [Google Scholar]
- Harkema, J.R.; Carey, S.A.; Wagner, J.G. The nose revisited: A brief review of the comparative structure, function, and toxicologic pathology of the nasal epithelium. Toxicol. Pathol. 2006, 34, 252–269. [Google Scholar] [CrossRef]
- Beule, A.G. Physiology and pathophysiology of respiratory mucosa of the nose and the paranasal sinuses. GMS Curr. Top Otorhinolaryngol. Head Neck Surg. 2010, 9, Doc07. [Google Scholar]
- Bruno, E.; Somma, G.; Russo, C.; Porozaj, D.; Pietroiusti, A.; Alessandrini, M.; Magrini, A. Nasal cytology as a screening tool in formaldehyde-exposed workers. Occup. Med. 2018, 68, 307–313. [Google Scholar] [CrossRef]
- Gelardi, M.; Fiorella, M.L.; Russo, C.; Fiorella, R.; Ciprandi, G. Role of nasal cytology. Int. J. Immunopathol. Pharmacol. 2010, 23 (Suppl. S1), 45–49. [Google Scholar] [CrossRef]
- Scarupa, M.D.; Kaliner, M.A. Nonallergic rhinitis, with a focus on vasomotor rhinitis: Clinical importance, differential diagnosis, and effective treatment recommendations. World Allergy Organ. J. 2009, 2, 20–25. [Google Scholar] [CrossRef]
- Wheeler, P.W.; Wheeler, S.F. Vasomotor rhinitis. Am. Fam. Physician 2005, 72, 1057–1062. [Google Scholar] [PubMed]
- Banov, C.H.; Lieberman, P.; Vasomotor Rhinitis Study, G. Efficacy of azelastine nasal spray in the treatment of vasomotor (perennial nonallergic) rhinitis. Ann. Allergy Asthma Immunol. 2001, 86, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Belaldavar, B.P.; Havaldar, R.R. Nasal Eosinophilia in Allergic Rhinitis: A Clinico-Correlative Observational Study. Otolaryngol. Open Access J. 2020, 5, 1–5. [Google Scholar]
- Ciprandi, G.; Ricca, V.; Passalacqua, G.; Truffelli, T.; Bertolini, C.; Fiorino, N.; Riccio, A.M.; Bagnasco, M.; Canonica, G.W. Seasonal rhinitis and azelastine: Long- or short-term treatment? J. Allergy Clin. Immunol. 1997, 99, 301–307. [Google Scholar] [CrossRef]
- Ciprandi, G.; Pronzato, C.; Passalacqua, G.; Ricca, V.; Grogen, J.; Mela, G.S.; Varese, P.; Bertolini, C.; Bagnasco, M.; Canonica, G.W. Topical azelastine reduces eosinophil activation and intercellular adhesion molecule-1 expression on nasal epithelial cells: An antiallergic activity. J. Allergy Clin. Immunol. 1996, 98, 1088–1096. [Google Scholar] [CrossRef]
- Chapelin, C.; Coste, A.; Gilain, L.; Poron, F.; Verra, F.; Escudier, E. Modified epithelial cell distribution in chronic airways inflammation. Eur. Respir. J. 1996, 9, 2474–2478. [Google Scholar] [CrossRef]
- Caruso, C.; Giancaspro, R.; Guida, G.; Macchi, A.; Landi, M.; Heffler, E.; Gelardi, M. Nasal Cytology: A Easy Diagnostic Tool in Precision Medicine for Inflammation in Epithelial Barrier Damage in the Nose. A Perspective Mini Review. Front. Allergy 2022, 3, 768408. [Google Scholar] [CrossRef]
- Aslani, F.S.; Khademi, B.; Yeganeh, F.; Kumar, P.V.; Bedayat, G.R. Nasal cytobrush cytology: Evaluation of the hyperchromatic supranuclear stria. Acta Cytol. 2006, 50, 430–434. [Google Scholar] [CrossRef]
- Myszkowska, D.; Bazgier, M.; Bronska, S.; Nowak, K.; Ozga, J.; Wozniak, A.; Stanisz, A.; Szaleniec, J. Scraping nasal cytology in the diagnostics of rhinitis and the comorbidities. Sci. Rep. 2022, 12, 14492. [Google Scholar] [CrossRef]
- Gastaminza, G.; Lombardero, M.; Bernaola, G.; Antepara, I.; Munoz, D.; Gamboa, P.M.; Audicana, M.T.; Marcos, C.; Ansotegui, I.J. Allergenicity and cross-reactivity of pine pollen. Clin. Exp. Allergy 2009, 39, 1438–1446. [Google Scholar] [CrossRef] [PubMed]
- Marcos, C.; Rodriguez, F.J.; Luna, I.; Jato, V.; Gonzalez, R. Pinus pollen aerobiology and clinical sensitization in northwest Spain. Ann. Allergy Asthma Immunol. 2001, 87, 39–42. [Google Scholar] [CrossRef]
- Lieberman, P. The role of antihistamines in the treatment of vasomotor rhinitis. World Allergy Organ. J. 2009, 2, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, P.L.; Smith, P. Nonallergic Rhinitis: Treatment. Immunol. Allergy Clin North Am. 2016, 36, 305–319. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, P.; Kaliner, M.A.; Wheeler, W.J. Open-label evaluation of azelastine nasal spray in patients with seasonal allergic rhinitis and nonallergic vasomotor rhinitis. Curr. Med. Res. Opin. 2005, 21, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Qian, M.; Fang, X.; Wang, X. Autophagy and inflammation. Clin. Transl. Med. 2017, 6, 24. [Google Scholar] [CrossRef]
- Cemma, M.; Brumell, J.H. Interactions of pathogenic bacteria with autophagy systems. Curr. Biol. 2012, 22, R540–R545. [Google Scholar] [CrossRef]
- Paludan, C.; Schmid, D.; Landthaler, M.; Vockerodt, M.; Kube, D.; Tuschl, T.; Munz, C. Endogenous MHC class II processing of a viral nuclear antigen after autophagy. Science 2005, 307, 593–596. [Google Scholar] [CrossRef]
- Deretic, V. Autophagy in inflammation, infection, and immunometabolism. Immunity 2021, 54, 437–453. [Google Scholar] [CrossRef]
- Pyo, J.O.; Jang, M.H.; Kwon, Y.K.; Lee, H.J.; Jun, J.I.; Woo, H.N.; Cho, D.H.; Choi, B.; Lee, H.; Kim, J.H.; et al. Essential roles of Atg5 and FADD in autophagic cell death: Dissection of autophagic cell death into vacuole formation and cell death. J. Biol. Chem. 2005, 280, 20722–20729. [Google Scholar] [CrossRef]
| n | Group AR | Group NAR |
|---|---|---|
| Number of patients | 10 | 10 |
| Male/Female | 7/3 | 7/3 |
| Age median | 8–14 10.9 | 7–14 11.1 |
| Symptoms of nose | ||
| rhinorrhea | 10 | 10 |
| congestion | 10 | 10 |
| itching | 6 | - |
| sneezing | 6 | 10 |
| Other symptoms | ||
| coughing | 5 | 5 |
| mucus in the throat | - | 10 |
| Concomitant diseases | ||
| conjuctivitis | 5 | - |
| asthma | 3 | 9 |
| atopic dermatitis | 2 * | 1 |
| Sensitized allergens | ||
| perennial (mites) pollen grains | 10 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trybus, E.; Trybus, W.; Król, T. Cytological Study of Topical Effect of Azelastine Hydrochloride on the Nasal Mucous Membrane Cells in Various Nasal Rhinitis Types. Cells 2023, 12, 2697. https://doi.org/10.3390/cells12232697
Trybus E, Trybus W, Król T. Cytological Study of Topical Effect of Azelastine Hydrochloride on the Nasal Mucous Membrane Cells in Various Nasal Rhinitis Types. Cells. 2023; 12(23):2697. https://doi.org/10.3390/cells12232697
Chicago/Turabian StyleTrybus, Ewa, Wojciech Trybus, and Teodora Król. 2023. "Cytological Study of Topical Effect of Azelastine Hydrochloride on the Nasal Mucous Membrane Cells in Various Nasal Rhinitis Types" Cells 12, no. 23: 2697. https://doi.org/10.3390/cells12232697
APA StyleTrybus, E., Trybus, W., & Król, T. (2023). Cytological Study of Topical Effect of Azelastine Hydrochloride on the Nasal Mucous Membrane Cells in Various Nasal Rhinitis Types. Cells, 12(23), 2697. https://doi.org/10.3390/cells12232697







