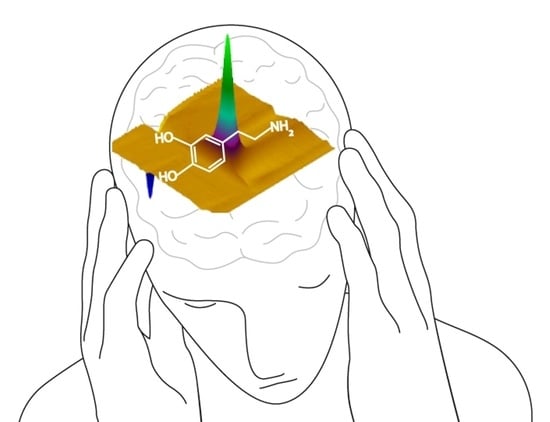
Applying a Fast-Scan Cyclic Voltammetry to Explore Dopamine Dynamics in Animal Models of Neuropsychiatric Disorders
Abstract
1. Introduction
2. Drug and Alcohol Addictions
3. Parkinson’s Disease
4. Schizophrenia
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Adams, R.N. Electrochemistry at Solid Electrodes; M. Dekker: New York, NY, USA, 1969. [Google Scholar]
- Armstrong-James, M.; Millar, J. Carbon fibre microelectrodes. J. Neurosci. Methods 1979, 1, 279–287. [Google Scholar] [CrossRef]
- Baur, J.E.; Kristensen, E.W.; May, L.J.; Wiedemann, D.J.; Wightman, R.M. Fast-scan voltammetry of biogenic amines. Anal. Chem. 1988, 60, 1268–1272. [Google Scholar] [CrossRef] [PubMed]
- Millar, J.; Stamford, J.A.; Kruk, Z.L.; Wightman, R.M. Electrochemical, pharmacological and electrophysiological evidence of rapid dopamine release and removal in the rat caudate nucleus following electrical stimulation of the median forebrain bundle. Eur. J. Pharmacol. 1985, 109, 341–348. [Google Scholar] [CrossRef]
- Budygin, E.; Jones, S. Electrochemical characterization of dopamine transporters. In Dopamine Transporters: Chemistry, Biology, and Pharmacology; Trudell, M.L., Izenwasser, S., Eds.; Wiley: Hoboken, NJ, USA, 2008; pp. 97–121. [Google Scholar]
- Robinson, D.L.; Hermans, A.; Seipel, A.T.; Wightman, R.M. Monitoring rapid chemical communication in the brain. Chem. Rev. 2008, 108, 2554–2584. [Google Scholar] [CrossRef]
- Sandberg, S.G.; Garris, P.A. Neurochemistry of Addiction: Monitoring Essential Neurotransmitters of Addiction. In Advances in the Neuroscience of Addiction, 2nd ed.; Kuhn, C.M., Koob, G.F., Eds.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2010; Chapter 3. [Google Scholar]
- Venton, B.J.; Cao, Q. Fundamentals of fast-scan cyclic voltammetry for dopamine detection. Analyst 2020, 145, 1158–1168. [Google Scholar] [CrossRef]
- Banerjee, S.; McCracken, S.; Hossain, M.F.; Slaughter, G. Electrochemical Detection of Neurotransmitters. Biosensors 2020, 10, 101. [Google Scholar] [CrossRef]
- Wickham, R.J.; Solecki, W.; Rathbun, L.R.; Neugebauer, N.M.; Wightman, R.M.; Addy, N.A. Advances in studying phasic dopamine signaling in brain reward mechanisms. Front. Biosci. (Elite Ed.) 2013, 5, 982–999. [Google Scholar] [CrossRef][Green Version]
- Phillips, P.E.; Stuber, G.D.; Heien, M.L.; Wightman, R.M.; Carelli, R.M. Subsecond dopamine release promotes cocaine seeking. Nature 2003, 422, 614–618. [Google Scholar] [CrossRef]
- Stuber, G.D.; Wightman, R.M.; Carelli, R.M. Extinction of cocaine self-administration reveals functionally and temporally distinct dopaminergic signals in the nucleus accumbens. Neuron 2005, 46, 661–669. [Google Scholar] [CrossRef]
- Ostlund, S.B.; LeBlanc, K.H.; Kosheleff, A.R.; Wassum, K.M.; Maidment, N.T. Phasic mesolimbic dopamine signaling encodes the facilitation of incentive motivation produced by repeated cocaine exposure. Neuropsychopharmacology 2014, 39, 2441–2449. [Google Scholar] [CrossRef] [PubMed]
- Wassum, K.M.; Ostlund, S.B.; Loewinger, G.C.; Maidment, N.T. Phasic mesolimbic dopamine release tracks reward seeking during expression of Pavlovian-to-instrumental transfer. Biol. Psychiatry 2013, 73, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Day, J.J.; Roitman, M.F.; Wightman, R.M.; Carelli, R.M. Associative learning mediates dynamic shifts in dopamine signaling in the nucleus accumbens. Nat. Neurosci. 2007, 10, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Zweifel, L.S.; Parker, J.G.; Lobb, C.J.; Rainwater, A.; Wall, V.Z.; Fadok, J.P.; Darvas, M.; Kim, M.J.; Mizumori, S.J.; Paladini, C.A. Disruption of NMDAR-dependent burst firing by dopamine neurons provides selective assessment of phasic dopamine-dependent behavior. Proc. Natl. Acad. Sci. USA 2009, 106, 7281–7288. [Google Scholar] [CrossRef] [PubMed]
- Hart, A.S.; Rutledge, R.B.; Glimcher, P.W.; Phillips, P.E. Phasic dopamine release in the rat nucleus accumbens symmetrically encodes a reward prediction error term. J. Neurosci. 2014, 34, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Heien, M.L.; Johnson, M.A.; Wightman, R.M. Resolving neurotransmitters detected by fast-scan cyclic voltammetry. Anal. Chem. 2004, 76, 5697–5704. [Google Scholar] [CrossRef]
- Willuhn, I.; Burgeno, L.M.; Everitt, B.J.; Phillips, P.E. Hierarchical recruitment of phasic dopamine signaling in the striatum during the progression of cocaine use. Proc. Natl. Acad. Sci. USA 2012, 109, 20703–20708. [Google Scholar] [CrossRef]
- Willuhn, I.; Burgeno, L.M.; Groblewski, P.A.; Phillips, P.E. Excessive cocaine use results from decreased phasic dopamine signaling in the striatum. Nat. Neurosci. 2014, 17, 704–709. [Google Scholar] [CrossRef]
- Anstrom, K.K.; Miczek, K.A.; Budygin, E. Increased phasic dopamine signaling in the mesolimbic pathway during social defeat in rats. Neuroscience 2009, 161, 3–12. [Google Scholar] [CrossRef]
- Kishida, K.T.; Saez, I.; Lohrenz, T.; Witcher, M.R.; Laxton, A.W.; Tatter, S.B.; White, J.P.; Ellis, T.L.; Phillips, P.E.; Montague, P.R. Subsecond dopamine fluctuations in human striatum encode superposed error signals about actual and counterfactual reward. Proc. Natl. Acad. Sci. USA 2016, 113, 200–205. [Google Scholar] [CrossRef]
- Oleson, E.B.; Talluri, S.; Childers, S.R.; Smith, J.E.; Roberts, D.; Bonin, K.D.; Budygin, E.A. Dopamine uptake changes associated with cocaine self-administration. Neuropsychopharmacology 2009, 34, 1174–1184. [Google Scholar] [CrossRef] [PubMed]
- Pattison, L.P.; McIntosh, S.; Budygin, E.A.; Hemby, S.E. Differential regulation of accumbal dopamine transmission in rats following cocaine, heroin and speedball self-administration. J. Neurochem. 2012, 122, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Mateo, Y.; Lack, C.M.; Morgan, D.; Roberts, D.; Jones, S.R. Reduced dopamine terminal function and insensitivity to cocaine following cocaine binge self-administration and deprivation. Neuropsychopharmacology 2005, 30, 1455–1463. [Google Scholar] [CrossRef] [PubMed]
- Ferris, M.J.; Mateo, Y.; Roberts, D.C.; Jones, S.R. Cocaine-insensitive dopamine transporters with intact substrate transport produced by self-administration. Biol. Psychiatry 2011, 69, 201–207. [Google Scholar] [CrossRef]
- Budygin, E.A.; John, C.E.; Mateo, Y.; Daunais, J.B.; Friedman, D.P.; Grant, K.A.; Jones, S.R. Chronic ethanol exposure alters presynaptic dopamine function in the striatum of monkeys: A preliminary study. Synapse 2003, 50, 266–268. [Google Scholar] [CrossRef]
- Budygin, E.A.; Oleson, E.B.; Mathews, T.A.; Läck, A.K.; Diaz, M.R.; McCool, B.A.; Jones, S.R. Effects of chronic alcohol exposure on dopamine uptake in rat nucleus accumbens and caudate putamen. Psychopharmacology 2007, 193, 495–501. [Google Scholar] [CrossRef]
- Deal, A.L.; Konstantopoulos, J.K.; Weiner, J.L.; Budygin, E.A. Exploring the consequences of social defeat stress and intermittent ethanol drinking on dopamine dynamics in the rat nucleus accumbens. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef]
- Karkhanis, A.N.; Alexander, N.J.; McCool, B.A.; Weiner, J.L.; Jones, S.R. Chronic social isolation during adolescence augments catecholamine response to acute ethanol in the basolateral amygdala. Synapse 2015, 69, 385–395. [Google Scholar] [CrossRef]
- Ferris, M.J.; Calipari, E.S.; Rose, J.H.; Siciliano, C.A.; Sun, H.; Chen, R.; Jones, S.R. A single amphetamine infusion reverses deficits in dopamine nerve-terminal function caused by a history of cocaine self-administration. Neuropsychopharmacology 2015, 40, 1826–1836. [Google Scholar] [CrossRef]
- Bergstrom, B.P.; Sanberg, S.G.; Andersson, M.; Mithyantha, J.; Carroll, F.I.; Garris, P.A. Functional reorganization of the presynaptic dopaminergic terminal in parkinsonism. Neuroscience 2011, 193, 310–322. [Google Scholar] [CrossRef]
- Jones, S.R.; Gainetdinov, R.R.; Jaber, M.; Giros, B.; Wightman, R.M.; Caron, M.G. Profound neuronal plasticity in response to inactivation of the dopamine transporter. Proc. Natl. Acad. Sci. USA 1998, 95, 4029–4034. [Google Scholar] [CrossRef] [PubMed]
- Budygin, E.A.; Kilpatrick, M.R.; Gainetdinov, R.R.; Wightman, R.M. Correlation between behavior and extracellular dopamine levels in rat striatum: Comparison of microdialysis and fast-scan cyclic voltammetry. Neurosci. Lett. 2000, 281, 9–12. [Google Scholar] [CrossRef]
- Leo, D.; Sukhanov, I.; Zoratto, F.; Illiano, P.; Caffino, L.; Sanna, F.; Messa, G.; Emanuele, M.; Esposito, A.; Dorofeikova, M. Pronounced hyperactivity, cognitive dysfunctions, and BDNF dysregulation in dopamine transporter knock-out rats. J. Neurosci. 2018, 38, 1959–1972. [Google Scholar] [CrossRef] [PubMed]
- Budygin, E.A.; Brodie, M.S.; Sotnikova, T.D.; Mateo, Y.; John, C.E.; Cyr, M.; Gainetdinov, R.R.; Jones, S.R. Dissociation of rewarding and dopamine transporter-mediated properties of amphetamine. Proc. Natl. Acad. Sci. USA 2004, 101, 7781–7786. [Google Scholar] [CrossRef]
- Mathews, T.A.; Brookshire, B.R.; Budygin, E.A.; Hamre, K.; Goldowitz, D.; Jones, S.R. Ethanol-induced hyperactivity is associated with hypodopaminergia in the 22-TNJ ENU-mutated mouse. Alcohol (Fayettev. N.Y.) 2009, 43, 421–431. [Google Scholar] [CrossRef]
- Sotnikova, T.D.; Budygin, E.A.; Jones, S.R.; Dykstra, L.A.; Caron, M.G.; Gainetdinov, R.R. Dopamine transporter-dependent and -independent actions of trace amine beta-phenylethylamine. J. Neurochem. 2004, 91, 362–373. [Google Scholar] [CrossRef]
- Budygin, E.A.; Gainetdinov, R.R.; Kilpatrick, M.R.; Rayevsky, K.S.; Männistö, P.T.; Wightman, R.M. Effect of tolcapone, a catechol-O-methyltransferase inhibitor, on striatal dopaminergic transmission during blockade of dopamine uptake. Eur. J. Pharmacol. 1999, 370, 125–131. [Google Scholar] [CrossRef]
- Leopold, A.V.; Shcherbakova, D.M.; Verkhusha, V.V. Fluorescent Biosensors for Neurotransmission and Neuromodulation: Engineering and Applications. Front. Cell. Neurosci. 2019, 13, 474. [Google Scholar] [CrossRef]
- Willuhn, I.; Wanat, M.J.; Clark, J.J.; Phillips, P.E. Dopamine signaling in the nucleus accumbens of animals self-administering drugs of abuse. In Behavioral Neuroscience of Drug Addiction; Springer: Berlin/Heidelberg, Germany, 2010; Volume 3, pp. 29–71. [Google Scholar]
- Bimpisidis, Z.; Wallén-Mackenzie, Å. Neurocircuitry of Reward and Addiction: Potential Impact of Dopamine-Glutamate Co-release as Future Target in Substance Use Disorder. J. Clin. Med. 2019, 8, 1887. [Google Scholar] [CrossRef]
- Schultz, W. Getting formal with dopamine and reward. Neuron 2002, 36, 241–263. [Google Scholar] [CrossRef]
- Bayer, H.M.; Glimcher, P.W. Midbrain dopamine neurons encode a quantitative reward prediction error signal. Neuron 2005, 47, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, E.E.; Keiflin, R.; Boivin, J.R.; Witten, I.B.; Deisseroth, K.; Janak, P.H. A causal link between prediction errors, dopamine neurons and learning. Nat. Neurosci. 2013, 16, 966–973. [Google Scholar] [CrossRef] [PubMed]
- Mikhailova, M.A.; Bass, C.E.; Grinevich, V.P.; Chappell, A.M.; Deal, A.L.; Bonin, K.D.; Weiner, J.L.; Gainetdinov, R.R.; Budygin, E.A. Optogenetically-induced tonic dopamine release from VTA-nucleus accumbens projections inhibits reward consummatory behaviors. Neuroscience 2016, 333, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Budygin, E.A.; Bass, C.E.; Grinevich, V.P.; Deal, A.L.; Bonin, K.D.; Weiner, J.L. Opposite consequences of tonic and phasic increases in accumbal dopamine on alcohol-seeking behavior. iScience 2020, 23, 100877. [Google Scholar] [CrossRef]
- Heien, M.L.; Khan, A.S.; Ariansen, J.L.; Cheer, J.F.; Phillips, P.E.; Wassum, K.M.; Wightman, R.M. Real-time measurement of dopamine fluctuations after cocaine in the brain of behaving rats. Proc. Natl. Acad. Sci. USA 2005, 102, 10023–10028. [Google Scholar] [CrossRef]
- Grinevich, V.P.; Krupitsky, E.M.; Gainetdinov, R.R.; Budygin, E.A. Linking Ethanol-Addictive Behaviors With Brain Catecholamines: Release Pattern Matters. Front. Behav. Neurosci. 2021, 15, 795030. [Google Scholar] [CrossRef]
- Bass, C.E.; Grinevich, V.P.; Gioia, D.; Day-Brown, J.; Bonin, K.D.; Stuber, G.D.; Weiner, J.L.; Budygin, E. Optogenetic stimulation of VTA dopamine neurons reveals that tonic but not phasic patterns of dopamine transmission reduce ethanol self-administration. Front. Behav. Neurosci. 2013, 7, 173. [Google Scholar] [CrossRef]
- Smith, J.E.; Co, C.; Coller, M.D.; Hemby, S.E.; Martin, T.J. Self-administered heroin and cocaine combinations in the rat: Additive reinforcing effects—Supra-additive effects on nucleus accumbens extracellular dopamine. Neuropsychopharmacology 2006, 31, 139–150. [Google Scholar] [CrossRef]
- Rothblat, D.S.; Rubin, E.; Schneider, J. Effects of chronic alcohol ingestion on the mesostriatal dopamine system in the rat. Neurosci. Lett. 2001, 300, 63–66. [Google Scholar] [CrossRef]
- Morgan, D.; Brebner, K.; Lynch, W.; Roberts, D. Increases in the reinforcing efficacy of cocaine after particular histories of reinforcement. Behav. Pharmacol. 2002, 13, 389–396. [Google Scholar] [CrossRef]
- Everitt, B.J.; Robbins, T.W. Neural systems of reinforcement for drug addiction: From actions to habits to compulsion. Nat. Neurosci. 2005, 8, 1481–1489. [Google Scholar] [CrossRef] [PubMed]
- Kalivas, P.W.; Volkow, N.D. The neural basis of addiction: A pathology of motivation and choice. Am. J. Psychiatry 2005, 162, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- Porrino, L.J.; Smith, H.R.; Nader, M.A.; Beveridge, T.J. The effects of cocaine: A shifting target over the course of addiction. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2007, 31, 1593–1600. [Google Scholar] [CrossRef] [PubMed]
- Lemos, J.C.; Wanat, M.J.; Smith, J.S.; Reyes, B.A.; Hollon, N.G.; Van Bockstaele, E.J.; Chavkin, C.; Phillips, P.E. Severe stress switches CRF action in the nucleus accumbens from appetitive to aversive. Nature 2012, 490, 402–406. [Google Scholar] [CrossRef]
- Lemos, J.C.; Shin, J.H.; Alvarez, V.A. Striatal cholinergic interneurons are a novel target of corticotropin releasing factor. J. Neurosci. 2019, 39, 5647–5661. [Google Scholar] [CrossRef]
- Steger, J.S.; Land, B.B.; Lemos, J.C.; Chavkin, C.; Phillips, P.E. Insidious transmission of a stress-related neuroadaptation. Front. Behav. Neurosci. 2020, 166. [Google Scholar] [CrossRef]
- Koller, W. When does Parkinson’s disease begin? Neurology 1992, 42, 27–31; discussion 41. [Google Scholar]
- Blesa, J.; Foffani, G.; Dehay, B.; Bezard, E.; Obeso, J.A. Motor and non-motor circuit disturbances in early Parkinson disease: Which happens first? Nat. Rev. Neurosci. 2022, 23, 115–128. [Google Scholar] [CrossRef]
- Shulman, J.M.; Yu, L.; Buchman, A.S.; Evans, D.A.; Schneider, J.A.; Bennett, D.A.; De Jager, P.L. Association of Parkinson disease risk loci with mild parkinsonian signs in older persons. JAMA Neurol. 2014, 71, 429–435. [Google Scholar] [CrossRef]
- Hornykiewicz, O. Basic research on dopamine in Parkinson’s disease and the discovery of the nigrostriatal dopamine pathway: The view of an eyewitness. Neuro-Degener. Dis. 2008, 5, 114–117. [Google Scholar] [CrossRef]
- Hornykiewicz, O. Brain dopamine in Parkinson’s disease and other neurological disturbances. Neurobiol. Dopamine 1979, 633–654. [Google Scholar]
- Elbaz, A.; Carcaillon, L.; Kab, S.; Moisan, F. Epidemiology of Parkinson’s disease. Rev. Neurol. 2016, 172, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Tysnes, O.B.; Storstein, A. Epidemiology of Parkinson’s disease. J. Neural Transm. (Vienna, Austria: 1996) 2017, 124, 901–905. [Google Scholar] [CrossRef] [PubMed]
- Picciotto, M.R.; Zoli, M. Nicotinic receptors in aging and dementia. J. Neurobiol. 2002, 53, 641–655. [Google Scholar] [CrossRef]
- Quik, M.; Huang, L.Z.; Parameswaran, N.; Bordia, T.; Campos, C.; Perez, X.A. Multiple roles for nicotine in Parkinson’s disease. Biochem. Pharmacol. 2009, 78, 677–685. [Google Scholar] [CrossRef]
- O’Neill, M.J.; Murray, T.K.; Lakics, V.; Visanji, N.P.; Duty, S. The role of neuronal nicotinic acetylcholine receptors in acute and chronic neurodegeneration. Curr. Drug Targets CNS Neurol. Disord. 2002, 1, 399–411. [Google Scholar] [CrossRef][Green Version]
- Bohnen, N.I.; Albin, R.L. The cholinergic system and Parkinson disease. Behav. Brain Res. 2011, 221, 564–573. [Google Scholar] [CrossRef]
- Iarkov, A.; Mendoza, C.; Echeverria, V. Cholinergic Receptor Modulation as a Target for Preventing Dementia in Parkinson’s Disease. Front. Neurosci. 2021, 15, 665820. [Google Scholar] [CrossRef]
- Myslivecek, J. Two Players in the Field: Hierarchical Model of Interaction between the Dopamine and Acetylcholine Signaling Systems in the Striatum. Biomedicines 2021, 9, 25. [Google Scholar] [CrossRef]
- Wonnacott, S.; Kaiser, S.; Mogg, A.; Soliakov, L.; Jones, I.W. Presynaptic nicotinic receptors modulating dopamine release in the rat striatum. Eur. J. Pharmacol. 2000, 393, 51–58. [Google Scholar] [CrossRef]
- Zoli, M.; Moretti, M.; Zanardi, A.; McIntosh, J.M.; Clementi, F.; Gotti, C. Identification of the nicotinic receptor subtypes expressed on dopaminergic terminals in the rat striatum. J. Neurosci. 2002, 22, 8785–8789. [Google Scholar] [CrossRef] [PubMed]
- Salminen, O.; Murphy, K.L.; McIntosh, J.M.; Drago, J.; Marks, M.J.; Collins, A.C.; Grady, S.R. Subunit composition and pharmacology of two classes of striatal presynaptic nicotinic acetylcholine receptors mediating dopamine release in mice. Mol. Pharmacol. 2004, 65, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Sulzer, D. Regulation of striatal dopamine release by presynaptic auto- and heteroreceptors. Basal Ganglia 2012, 2, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.M.; Liang, Y.; Dani, J.A. Endogenous nicotinic cholinergic activity regulates dopamine release in the striatum. Nat. Neurosci. 2001, 4, 1224–1229. [Google Scholar] [CrossRef]
- Rice, M.E.; Cragg, S.J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 2004, 7, 583–584. [Google Scholar] [CrossRef]
- Zhang, H.; Sulzer, D. Frequency-dependent modulation of dopamine release by nicotine. Nat. Neurosci. 2004, 7, 581–582. [Google Scholar] [CrossRef]
- Patel, J.C.; Rossignol, E.; Rice, M.E.; Machold, R.P. Opposing regulation of dopaminergic activity and exploratory motor behavior by forebrain and brainstem cholinergic circuits. Nat. Commun. 2012, 3, 1172. [Google Scholar] [CrossRef]
- Threlfell, S.; Lalic, T.; Platt, N.J.; Jennings, K.A.; Deisseroth, K.; Cragg, S.J. Striatal dopamine release is triggered by synchronized activity in cholinergic interneurons. Neuron 2012, 75, 58–64. [Google Scholar] [CrossRef]
- Cachope, R.; Mateo, Y.; Mathur, B.N.; Irving, J.; Wang, H.L.; Morales, M.; Lovinger, D.M.; Cheer, J.F. Selective activation of cholinergic interneurons enhances accumbal phasic dopamine release: Setting the tone for reward processing. Cell Rep. 2012, 2, 33–41. [Google Scholar] [CrossRef]
- Yavich, L.; Oksman, M.; Tanila, H.; Kerokoski, P.; Hiltunen, M.; van Groen, T.; Puoliväli, J.; Männistö, P.T.; García-Horsman, A.; MacDonald, E.; et al. Locomotor activity and evoked dopamine release are reduced in mice overexpressing A30P-mutated human alpha-synuclein. Neurobiol. Dis. 2005, 20, 303–313. [Google Scholar] [CrossRef]
- Janezic, S.; Threlfell, S.; Dodson, P.D.; Dowie, M.J.; Taylor, T.N.; Potgieter, D.; Parkkinen, L.; Senior, S.L.; Anwar, S.; Ryan, B.; et al. Deficits in dopaminergic transmission precede neuron loss and dysfunction in a new Parkinson model. Proc. Natl. Acad. Sci. USA 2013, 110, E4016–E4025. [Google Scholar] [CrossRef] [PubMed]
- Taylor, T.N.; Potgieter, D.; Anwar, S.; Senior, S.L.; Janezic, S.; Threlfell, S.; Ryan, B.; Parkkinen, L.; Deltheil, T.; Cioroch, M.; et al. Region-specific deficits in dopamine, but not norepinephrine, signaling in a novel A30P α-synuclein BAC transgenic mouse. Neurobiol. Dis. 2014, 62, 193–207. [Google Scholar] [CrossRef] [PubMed]
- Chadchankar, H.; Yavich, L. Sub-regional differences and mechanisms of the short-term plasticity of dopamine overflow in striatum in mice lacking alpha-synuclein. Brain Res. 2011, 1423, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Anwar, S.; Peters, O.; Millership, S.; Ninkina, N.; Doig, N.; Connor-Robson, N.; Threlfell, S.; Kooner, G.; Deacon, R.M.; Bannerman, D.M.; et al. Functional alterations to the nigrostriatal system in mice lacking all three members of the synuclein family. J. Neurosci. 2011, 31, 7264–7274. [Google Scholar] [CrossRef] [PubMed]
- Threlfell, S.; Mohammadi, A.S.; Ryan, B.J.; Connor-Robson, N.; Platt, N.J.; Anand, R.; Serres, F.; Sharp, T.; Bengoa-Vergniory, N.; Wade-Martins, R.; et al. Striatal Dopamine Transporter Function Is Facilitated by Converging Biology of α-Synuclein and Cholesterol. Front. Cell. Neurosci. 2021, 15, 658244. [Google Scholar] [CrossRef]
- Krosi, Z.; Casassus, P.; Valeyre, D.; Paolaggi, J.A.; Amouroux, J.; Battesti, J.P. [Chronic myeloid leukemia during the development of sarcoidosis]. Rev. Pneumol. Clin. 1988, 44, 33–35. [Google Scholar]
- Lohr, K.M.; Bernstein, A.I.; Stout, K.A.; Dunn, A.R.; Lazo, C.R.; Alter, S.P.; Wang, M.; Li, Y.; Fan, X.; Hess, E.J.; et al. Increased vesicular monoamine transporter enhances dopamine release and opposes Parkinson disease-related neurodegeneration in vivo. Proc. Natl. Acad. Sci. USA 2014, 111, 9977–9982. [Google Scholar] [CrossRef]
- Kordower, J.H.; Olanow, C.W.; Dodiya, H.B.; Chu, Y.; Beach, T.G.; Adler, C.H.; Halliday, G.M.; Bartus, R.T. Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain 2013, 136, 2419–2431. [Google Scholar] [CrossRef]
- Berg, D.; Adler, C.H.; Bloem, B.R.; Chan, P.; Gasser, T.; Goetz, C.G.; Halliday, G.; Lang, A.E.; Lewis, S.; Li, Y.; et al. Movement disorder society criteria for clinically established early Parkinson’s disease. Mov. Disord. 2018, 33, 1643–1646. [Google Scholar] [CrossRef]
- Fearnley, J.M.; Lees, A.J. Ageing and Parkinson’s disease: Substantia nigra regional selectivity. Brain 1991, 114, 2283–2301. [Google Scholar] [CrossRef]
- Galvan, A.; Wichmann, T. Pathophysiology of parkinsonism. Clin. Neurophysiol. 2008, 119, 1459–1474. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Kaeser, P.S. Mechanisms and regulation of dopamine release. Curr. Opin. Neurobiol. 2019, 57, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Fleckenstein, A.E.; Pögün, S.; Carroll, F.I.; Kuhar, M.J. Recovery of dopamine transporter binding and function after intrastriatal administration of the irreversible inhibitor RTI-76 [3 beta-(3p-chlorophenyl) tropan-2 beta-carboxylic acid p-isothiocyanatophenylethyl ester hydrochloride]. J. Pharmacol. Exp. Ther. 1996, 279, 200–206. [Google Scholar] [PubMed]
- Yavich, L.; MacDonald, E. Dopamine release from pharmacologically distinct storage pools in rat striatum following stimulation at frequency of neuronal bursting. Brain Res. 2000, 870, 73–79. [Google Scholar] [CrossRef]
- Herdon, H.; Strupish, J.; Nahorski, S.R. Differences between the release of radiolabelled and endogenous dopamine from superfused rat brain slices: Effects of depolarizing stimuli, amphetamine and synthesis inhibition. Brain Res. 1985, 348, 309–320. [Google Scholar] [CrossRef]
- Montague, P.R.; McClure, S.M.; Baldwin, P.; Phillips, P.E.; Budygin, E.A.; Stuber, G.D.; Kilpatrick, M.R.; Wightman, R.M. Dynamic gain control of dopamine delivery in freely moving animals. J. Neurosci. 2004, 24, 1754–1759. [Google Scholar] [CrossRef][Green Version]
- Kita, J.M.; Parker, L.E.; Phillips, P.E.; Garris, P.A.; Wightman, R.M. Paradoxical modulation of short-term facilitation of dopamine release by dopamine autoreceptors. J. Neurochem. 2007, 102, 1115–1124. [Google Scholar] [CrossRef]
- Garris, P.A.; Walker, Q.D.; Wightman, R.M. Dopamine release and uptake rates both decrease in the partially denervated striatum in proportion to the loss of dopamine terminals. Brain Res. 1997, 753, 225–234. [Google Scholar] [CrossRef]
- Bergstrom, B.P.; Garris, P.A. “Passive stabilization” of striatal extracellular dopamine across the lesion spectrum encompassing the presymptomatic phase of Parkinson’s disease: A voltammetric study in the 6-OHDA-lesioned rat. J. Neurochem. 2003, 87, 1224–1236. [Google Scholar] [CrossRef]
- Atcherley, C.W.; Wood, K.M.; Parent, K.L.; Hashemi, P.; Heien, M.L. The coaction of tonic and phasic dopamine dynamics. Chem. Commun. (Camb. Engl. ) 2015, 51, 2235–2238. [Google Scholar] [CrossRef]
- Oh, Y.; Park, C.; Kim, D.H.; Shin, H.; Kang, Y.M.; DeWaele, M.; Lee, J.; Min, H.K.; Blaha, C.D.; Bennet, K.E.; et al. Monitoring In Vivo Changes in Tonic Extracellular Dopamine Level by Charge-Balancing Multiple Waveform Fast-Scan Cyclic Voltammetry. Anal. Chem. 2016, 88, 10962–10970. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.A.; Rodeberg, N.T.; Wightman, R.M. Measurement of Basal Neurotransmitter Levels Using Convolution-Based Nonfaradaic Current Removal. Anal. Chem. 2018, 90, 7181–7189. [Google Scholar] [CrossRef] [PubMed]
- Puthongkham, P.; Venton, B.J. Nanodiamond Coating Improves the Sensitivity and Antifouling Properties of Carbon Fiber Microelectrodes. ACS Sens. 2019, 4, 2403–2411. [Google Scholar] [CrossRef]
- Oh, Y.; Heien, M.L.; Park, C.; Kang, Y.M.; Kim, J.; Boschen, S.L.; Shin, H.; Cho, H.U.; Blaha, C.D.; Bennet, K.E.; et al. Tracking tonic dopamine levels in vivo using multiple cyclic square wave voltammetry. Biosens. Bioelectron. 2018, 121, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Taylor, I.M.; Patel, N.A.; Freedman, N.C.; Castagnola, E.; Cui, X.T. Direct in Vivo Electrochemical Detection of Resting Dopamine Using Poly(3,4-ethylenedioxythiophene)/Carbon Nanotube Functionalized Microelectrodes. Anal. Chem. 2019, 91, 12917–12927. [Google Scholar] [CrossRef] [PubMed]
- Barath, A.S.; Rusheen, A.E.; Rojas Cabrera, J.M.; Price, J.B.; Owen, R.L.; Shin, H.; Jang, D.P.; Blaha, C.D.; Lee, K.H.; Oh, Y. Hypoxia-Associated Changes in Striatal Tonic Dopamine Release: Real-Time in vivo Measurements With a Novel Voltammetry Technique. Front. Neurosci. 2020, 14, 869. [Google Scholar] [CrossRef] [PubMed]
- Bucher, E.S.; Wightman, R.M. Electrochemical Analysis of Neurotransmitters. Annu. Rev. Anal. Chem. (Palo Alto Calif.) 2015, 8, 239–261. [Google Scholar] [CrossRef]
- Kahn, R.; Sommer, I.; Murray, R.; Meyer-Lindenberg, A.; Weinberger, D.; Cannon, T.; O’Donovan, M.; Correll, C.; Kane, J.; van Os, J.; et al. Schizophrenia. Nat. Rev. Dis Primers 2015, 1, 15067. [Google Scholar] [CrossRef]
- Leucht, S.; Arbter, D.; Engel, R.R.; Kissling, W.; Davis, J.M. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. Mol. Psychiatry 2009, 14, 429–447. [Google Scholar] [CrossRef]
- Huhn, M.; Nikolakopoulou, A.; Schneider-Thoma, J.; Krause, M.; Samara, M.; Peter, N.; Arndt, T.; Bäckers, L.; Rothe, P.; Cipriani, A.; et al. Comparative Efficacy and Tolerability of 32 Oral Antipsychotics for the Acute Treatment of Adults With Multi-Episode Schizophrenia: A Systematic Review and Network Meta-Analysis. Focus (Am. Psychiatr. Publ. ) 2020, 18, 443–455. [Google Scholar] [CrossRef]
- Lieberman, J.A.; Stroup, T.S.; McEvoy, J.P.; Swartz, M.S.; Rosenheck, R.A.; Perkins, D.O.; Keefe, R.S.; Davis, S.M.; Davis, C.E.; Lebowitz, B.D.; et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N. Engl. J. Med. 2005, 353, 1209–1223. [Google Scholar] [CrossRef] [PubMed]
- Acharya, S.; Kim, K.-M. Roles of the functional interaction between brain cholinergic and dopaminergic systems in the pathogenesis and treatment of schizophrenia and Parkinson’s disease. Int. J. Mol. Sci. 2021, 22, 4299. [Google Scholar] [CrossRef] [PubMed]
- Scarr, E.; Dean, B. Role of the cholinergic system in the pathology and treatment of schizophrenia. Expert Rev. Neurother. 2009, 9, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.F.; Freedman, R. Schizophrenia and the α7 nicotinic acetylcholine receptor. Int. Rev. Neurobiol. 2007, 78, 225–246. [Google Scholar] [PubMed]
- Carlsson, A.; Waters, N.; Holm-Waters, S.; Tedroff, J.; Nilsson, M.; Carlsson, M.L. Interactions between monoamines, glutamate, and GABA in schizophrenia: New evidence. Annu. Rev. Pharmacol. Toxicol. 2001, 41, 237–260. [Google Scholar] [CrossRef] [PubMed]
- McCutcheon, R.A.; Abi-Dargham, A.; Howes, O.D. Schizophrenia, dopamine and the striatum: From biology to symptoms. Trends Neurosci. 2019, 42, 205–220. [Google Scholar] [CrossRef] [PubMed]
- Piccart, E.; Courtney, N.A.; Branch, S.Y.; Ford, C.P.; Beckstead, M.J. Neurotensin induces presynaptic depression of D2 dopamine autoreceptor-mediated neurotransmission in midbrain dopaminergic neurons. J. Neurosci. 2015, 35, 11144–11152. [Google Scholar] [CrossRef]
- Castañé, A.; Cano, M.; Ruiz-Avila, L.; Miquel-Rio, L.; Celada, P.; Artigas, F.; Riga, M.S. Dual 5-HT3 and 5-HT6 Receptor Antagonist FPPQ Normalizes Phencyclidine-Induced Disruption of Brain Oscillatory Activity in Rats. Int. J. Neuropsychopharmacol. 2022. [Google Scholar] [CrossRef]
- Lipska, B.K.; Weinberger, D.R. To model a psychiatric disorder in animals: Schizophrenia as a reality test. Neuropsychopharmacology 2000, 23, 223–239. [Google Scholar] [CrossRef]
- Tarantino, L.; Bucan, M. Dissection of behavior and psychiatric disorders using the mouse as a model. Hum. Mol. Genet. 2000, 9, 953–965. [Google Scholar] [CrossRef][Green Version]
- Potvin, S.; Stip, E.; Roy, J.-Y. Toxic psychoses as pharmacological models of schizophrenia. Curr. Psychiatry Rev. 2005, 1, 23–32. [Google Scholar] [CrossRef]
- Corbett, R.; Camacho, F.; Woods, A.; Kerman, L.; Fishkin, R.; Brooks, K.; Dunn, R. Antipsychotic agents antagonize non-competitiveN-methyl-d-aspartate antagonist-induced behaviors. Psychopharmacology 1995, 120, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Duncan, G.; Zorn, S.; Lieberman, J. Mechanisms of typical and atypical antipsychotic drug action in relation to dopamine and NMDA receptor hypofunction hypotheses of schizophrenia. Mol. Psychiatry 1999, 4, 418–428. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gainetdinov, R.R.; Mohn, A.R.; Caron, M.G. Genetic animal models: Focus on schizophrenia. Trends Neurosci. 2001, 24, 527–533. [Google Scholar] [CrossRef]
- Kumar, U.; Medel-Matus, J.S.; Redwine, H.M.; Shin, D.; Hensler, J.G.; Sankar, R.; Mazarati, A. Effects of selective serotonin and norepinephrine reuptake inhibitors on depressive-and impulsive-like behaviors and on monoamine transmission in experimental temporal lobe epilepsy. Epilepsia 2016, 57, 506–515. [Google Scholar] [CrossRef]
- Wood, K.M.; Hashemi, P. Fast-scan cyclic voltammetry analysis of dynamic serotonin reponses to acute escitalopram. ACS Chem. Neurosci. 2013, 4, 715–720. [Google Scholar] [CrossRef]
- Asri, R.; O’Neill, B.; Patel, J.; Siletti, K.; Rice, M. Detection of evoked acetylcholine release in mouse brain slices. Analyst 2016, 141, 6416–6421. [Google Scholar] [CrossRef]
- Nicolai, E.N.; Trevathan, J.K.; Ross, E.K.; Lujan, J.L.; Blaha, C.D.; Bennet, K.E.; Lee, K.H.; Ludwig, K.A. Detection of norepinephrine in whole blood via fast scan cyclic voltammetry. In Proceedings of the 2017 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Rochester, MN, USA, 7–10 May 2017; pp. 111–116. [Google Scholar]
- Sams-Dodd, F. A test of the predictive validity of animal models of schizophrenia based on phencyclidine and D-amphetamine. Neuropsychopharmacology 1998, 18, 293–304. [Google Scholar] [CrossRef]
- Grinevich, V.P.; Papke, R.L.; Lippiello, P.M.; Bencherif, M. Atypical antipsychotics as noncompetitive inhibitors of α4β2 and α7 neuronal nicotinic receptors. Neuropharmacology 2009, 57, 183–191. [Google Scholar] [CrossRef]
- Giros, B.; Jaber, M.; Jones, S.R.; Wightman, R.M.; Caron, M.G. Hyperlocomotion and indifference to cocaine and amphetamine in mice lacking the dopamine transporter. Nature 1996, 379, 606–612. [Google Scholar] [CrossRef]
- Zhuang, X.; Oosting, R.S.; Jones, S.R.; Gainetdinov, R.R.; Miller, G.W.; Caron, M.G.; Hen, R. Hyperactivity and impaired response habituation in hyperdopaminergic mice. Proc. Natl. Acad. Sci. USA 2001, 98, 1982–1987. [Google Scholar] [CrossRef] [PubMed]
- Salahpour, A.; Ramsey, A.J.; Medvedev, I.O.; Kile, B.; Sotnikova, T.D.; Holmstrand, E.; Ghisi, V.; Nicholls, P.J.; Wong, L.; Murphy, K. Increased amphetamine-induced hyperactivity and reward in mice overexpressing the dopamine transporter. Proc. Natl. Acad. Sci. USA 2008, 105, 4405–4410. [Google Scholar] [CrossRef] [PubMed]
- Gainetdinov, R.R.; Hoener, M.C.; Berry, M.D. Trace amines and their receptors. Pharmacol. Rev. 2018, 70, 549–620. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.D.; Gainetdinov, R.R.; Hoener, M.C.; Shahid, M. Pharmacology of human trace amine-associated receptors: Therapeutic opportunities and challenges. Pharmacol. Ther. 2017, 180, 161–180. [Google Scholar] [CrossRef]
- Rutigliano, G.; Accorroni, A.; Zucchi, R. The case for TAAR1 as a modulator of central nervous system function. Front. Pharmacol. 2018, 8, 987. [Google Scholar] [CrossRef]
- Heffernan, M.L.; Herman, L.W.; Brown, S.; Jones, P.G.; Shao, L.; Hewitt, M.C.; Campbell, J.E.; Dedic, N.; Hopkins, S.C.; Koblan, K.S. Ulotaront: A TAAR1 Agonist for the Treatment of Schizophrenia. ACS Med. Chem. Lett. 2021, 13, 92–98. [Google Scholar] [CrossRef]
- Leo, D.; Mus, L.; Espinoza, S.; Hoener, M.; Sotnikova, T.; Gainetdinov, R. Taar1-mediated modulation of presynaptic dopaminergic neurotransmission: Role of D2 dopamine autoreceptors. Neuropharmacology 2014, 81, 283–291. [Google Scholar] [CrossRef]
- Javitt, D.C. Glutamate and schizophrenia: Phencyclidine, N-methyl-d-aspartate receptors, and dopamine–glutamate interactions. Int. Rev. Neurobiol. 2007, 78, 69–108. [Google Scholar]
- Jentsch, J.D.; Roth, R.H. The neuropsychopharmacology of phencyclidine: From NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 1999, 20, 201–225. [Google Scholar] [CrossRef]
- Mohn, A.R.; Gainetdinov, R.R.; Caron, M.G.; Koller, B.H. Mice with reduced NMDA receptor expression display behaviors related to schizophrenia. Cell 1999, 98, 427–436. [Google Scholar] [CrossRef]
- Ferris, M.J.; Milenkovic, M.; Liu, S.; Mielnik, C.A.; Beerepoot, P.; John, C.E.; España, R.A.; Sotnikova, T.D.; Gainetdinov, R.R.; Borgland, S.L. Sustained N-methyl-d-aspartate receptor hypofunction remodels the dopamine system and impairs phasic signaling. Eur. J. Neurosci. 2014, 40, 2255–2263. [Google Scholar] [CrossRef] [PubMed]
- Matosin, N.; Newell, K.A. Metabotropic glutamate receptor 5 in the pathology and treatment of schizophrenia. Neurosci. Biobehav. Rev. 2013, 37, 256–268. [Google Scholar] [CrossRef] [PubMed]
- Gupta, I.; Young, A.M. Metabotropic glutamate receptor modulation of dopamine release in the nucleus accumbens shell is unaffected by phencyclidine pretreatment: In vitro assessment using fast-scan cyclic voltammetry rat brain slices. Brain Res. 2018, 1687, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Lodge, D.J.; Grace, A.A. Hippocampal dysregulation of dopamine system function and the pathophysiology of schizophrenia. Trends Pharmacol. Sci. 2011, 32, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Modinos, G.; Allen, P.; Grace, A.A.; McGuire, P. Translating the MAM model of psychosis to humans. Trends Neurosci. 2015, 38, 129–138. [Google Scholar] [CrossRef]
- Howe, W.M.; Tierney, P.L.; Young, D.A.; Oomen, C.; Kozak, R. MAM (E17) rodent developmental model of neuropsychiatric disease: Disruptions in learning and dysregulation of nucleus accumbens dopamine release, but spared executive function. Psychopharmacology 2015, 232, 4113–4127. [Google Scholar] [CrossRef]
- Boules, M.; Li, Z.; Smith, K.; Fredrickson, P.; Richelson, E. Diverse roles of neurotensin agonists in the central nervous system. Front. Endocrinol. 2013, 4, 36. [Google Scholar] [CrossRef]
- Collins, A.L.; Aitken, T.J.; Huang, I.-W.; Shieh, C.; Greenfield, V.Y.; Monbouquette, H.G.; Ostlund, S.B.; Wassum, K.M. Nucleus accumbens cholinergic interneurons oppose cue-motivated behavior. Biol. Psychiatry 2019, 86, 388–396. [Google Scholar] [CrossRef]
- Shin, J.H.; Adrover, M.F.; Alvarez, V.A. Distinctive modulation of dopamine release in the nucleus accumbens shell mediated by dopamine and acetylcholine receptors. J. Neurosci. 2017, 37, 11166–11180. [Google Scholar] [CrossRef]
- Hoebel, B.G.; Avena, N.M.; Rada, P. Accumbens dopamine-acetylcholine balance in approach and avoidance. Curr. Opin. Pharmacol. 2007, 7, 617–627. [Google Scholar] [CrossRef]
- Meltzer, H.Y.; Rajagopal, L.; Matrisciano, F.; Hao, J.; Svensson, K.A.; Huang, M. The allosteric dopamine D1 receptor potentiator, DETQ, ameliorates subchronic phencyclidine-induced object recognition memory deficits and enhances cortical acetylcholine efflux in male humanized D1 receptor knock-in mice. Behav. Brain Res. 2019, 361, 139–150. [Google Scholar] [CrossRef] [PubMed]
- McKinley, J.W.; Shi, Z.; Kawikova, I.; Hur, M.; Bamford, I.J.; Devi, S.P.S.; Vahedipour, A.; Darvas, M.; Bamford, N.S. Dopamine deficiency reduces striatal cholinergic interneuron function in models of Parkinson’s disease. Neuron 2019, 103, 1056–1072.e6. [Google Scholar] [CrossRef] [PubMed]
- Yavas, E.; Young, A.M. Repeated phencyclidine disrupts nicotinic acetylcholine regulation of dopamine release in nucleus accumbens: Implications for models of schizophrenia. Neurochem. Int. 2020, 140, 104836. [Google Scholar] [CrossRef]
- Ripke, S.; O’dushlaine, C.; Chambert, K.; Moran, J.L.; Kähler, A.K.; Akterin, S.; Bergen, S.E.; Collins, A.L.; Crowley, J.J.; Fromer, M. Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat. Genet. 2013, 45, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.M.; Famous, K.R.; Sadri-Vakili, G.; Kumaresan, V.; Schmidt, H.D.; Bass, C.E.; Terwilliger, E.F.; Cha, J.-H.J.; Pierce, R.C. CaMKII: A biochemical bridge linking accumbens dopamine and glutamate systems in cocaine seeking. Nat. Neurosci. 2008, 11, 344–353. [Google Scholar] [CrossRef]
- Terrillion, C.E.; Dao, D.T.; Cachope, R.; Lobo, M.K.; Puche, A.C.; Cheer, J.F.; Gould, T.D. Reduced levels of C acna1c attenuate mesolimbic dopamine system function. Genes Brain Behav. 2017, 16, 495–505. [Google Scholar] [CrossRef]
- Consoli, D.C.; Brady, L.J.; Bowman, A.B.; Calipari, E.S.; Harrison, F.E. Ascorbate deficiency decreases dopamine release in gulo(-/-) and APP/PSEN1 mice. J. Neurochem. 2021, 157, 656–665. [Google Scholar] [CrossRef]
- Mukhin, V.N.; Borovets, I.R.; Sizov, V.V.; Pavlov, K.I.; Klimenko, V.M. Differential Influence of Amyloid-β on the Kinetics of Dopamine Release in the Dorsal and Ventral Striatum of Rats. Neurotox. Res. 2021, 39, 1285–1292. [Google Scholar] [CrossRef]
- Vester, A.I.; Chen, M.; Marsit, C.J.; Caudle, W.M. A Neurodevelopmental Model of Combined Pyrethroid and Chronic Stress Exposure. Toxics 2019, 7, 24. [Google Scholar] [CrossRef]
- Regan, S.L.; Cryan, M.T.; Williams, M.T.; Vorhees, C.V.; Ross, A.E. Enhanced Transient Striatal Dopamine Release and Reuptake in Lphn3 Knockout Rats. ACS Chem. Neurosci. 2020, 11, 1171–1177. [Google Scholar] [CrossRef]
- Kishida, K.T.; Sandberg, S.G.; Lohrenz, T.; Comair, Y.G.; Sáez, I.; Phillips, P.E.; Montague, P.R. Sub-second dopamine detection in human striatum. PLoS ONE 2011, 6, e23291. [Google Scholar] [CrossRef] [PubMed]
- Bennet, K.E.; Tomshine, J.R.; Min, H.K.; Manciu, F.S.; Marsh, M.P.; Paek, S.B.; Settell, M.L.; Nicolai, E.N.; Blaha, C.D.; Kouzani, A.Z.; et al. A Diamond-Based Electrode for Detection of Neurochemicals in the Human Brain. Front. Hum. Neurosci. 2016, 10, 102. [Google Scholar] [CrossRef] [PubMed]
- Lohrenz, T.; Kishida, K.T.; Montague, P.R. BOLD and its connection to dopamine release in human striatum: A cross-cohort comparison. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2016, 371. [Google Scholar] [CrossRef] [PubMed]
- Montague, P.R.; Kishida, K.T. Computational Underpinnings of Neuromodulation in Humans. Cold Spring Harb. Symp. Quant. Biol. 2018, 83, 71–82. [Google Scholar] [CrossRef]
- Lucio Boschen, S.; Trevathan, J.; Hara, S.A.; Asp, A.; Lujan, J.L. Defining a Path Toward the Use of Fast-Scan Cyclic Voltammetry in Human Studies. Front. Neurosci. 2021, 15, 728092. [Google Scholar] [CrossRef]
- Puthongkham, P.; Venton, B.J. Recent advances in fast-scan cyclic voltammetry. Analyst 2020, 145, 1087–1102. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grinevich, V.P.; Zakirov, A.N.; Berseneva, U.V.; Gerasimova, E.V.; Gainetdinov, R.R.; Budygin, E.A. Applying a Fast-Scan Cyclic Voltammetry to Explore Dopamine Dynamics in Animal Models of Neuropsychiatric Disorders. Cells 2022, 11, 1533. https://doi.org/10.3390/cells11091533
Grinevich VP, Zakirov AN, Berseneva UV, Gerasimova EV, Gainetdinov RR, Budygin EA. Applying a Fast-Scan Cyclic Voltammetry to Explore Dopamine Dynamics in Animal Models of Neuropsychiatric Disorders. Cells. 2022; 11(9):1533. https://doi.org/10.3390/cells11091533
Chicago/Turabian StyleGrinevich, Vladimir P., Amir N. Zakirov, Uliana V. Berseneva, Elena V. Gerasimova, Raul R. Gainetdinov, and Evgeny A. Budygin. 2022. "Applying a Fast-Scan Cyclic Voltammetry to Explore Dopamine Dynamics in Animal Models of Neuropsychiatric Disorders" Cells 11, no. 9: 1533. https://doi.org/10.3390/cells11091533
APA StyleGrinevich, V. P., Zakirov, A. N., Berseneva, U. V., Gerasimova, E. V., Gainetdinov, R. R., & Budygin, E. A. (2022). Applying a Fast-Scan Cyclic Voltammetry to Explore Dopamine Dynamics in Animal Models of Neuropsychiatric Disorders. Cells, 11(9), 1533. https://doi.org/10.3390/cells11091533