RAC1, a Potential Diagnostic and Prognostic Marker for Diffuse Large B Cell Lymphoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Multiple Cancer Dataset Source and Preprocessing
2.2. Diagnostic Analysis
2.3. Survival Analysis
2.4. Correlation Analysis
2.5. Immunohistochemical Staining (IHC)
2.6. Statistical Analysis
3. Results
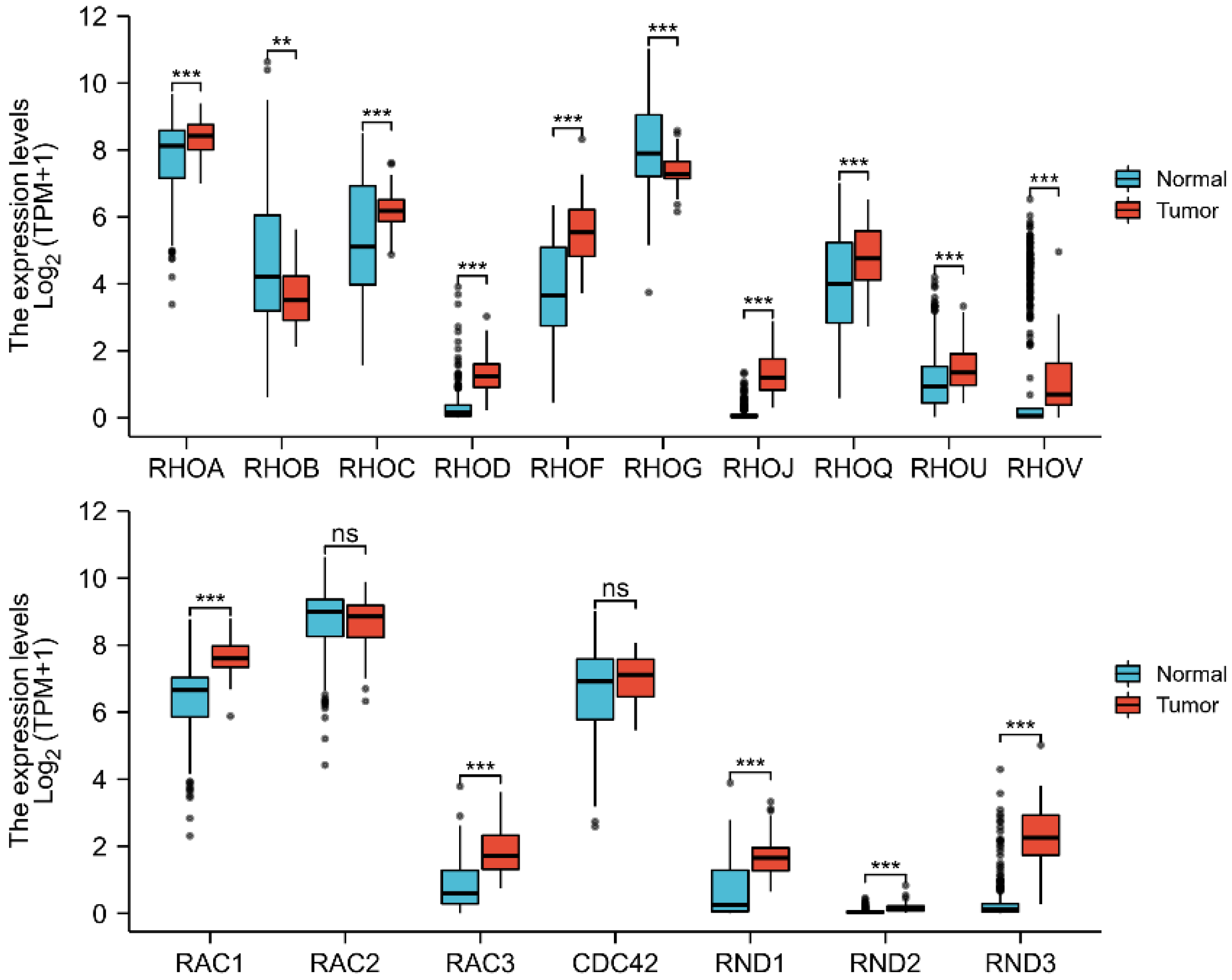
3.1. Expression of the Rho/Rac Family Members in DLBCL
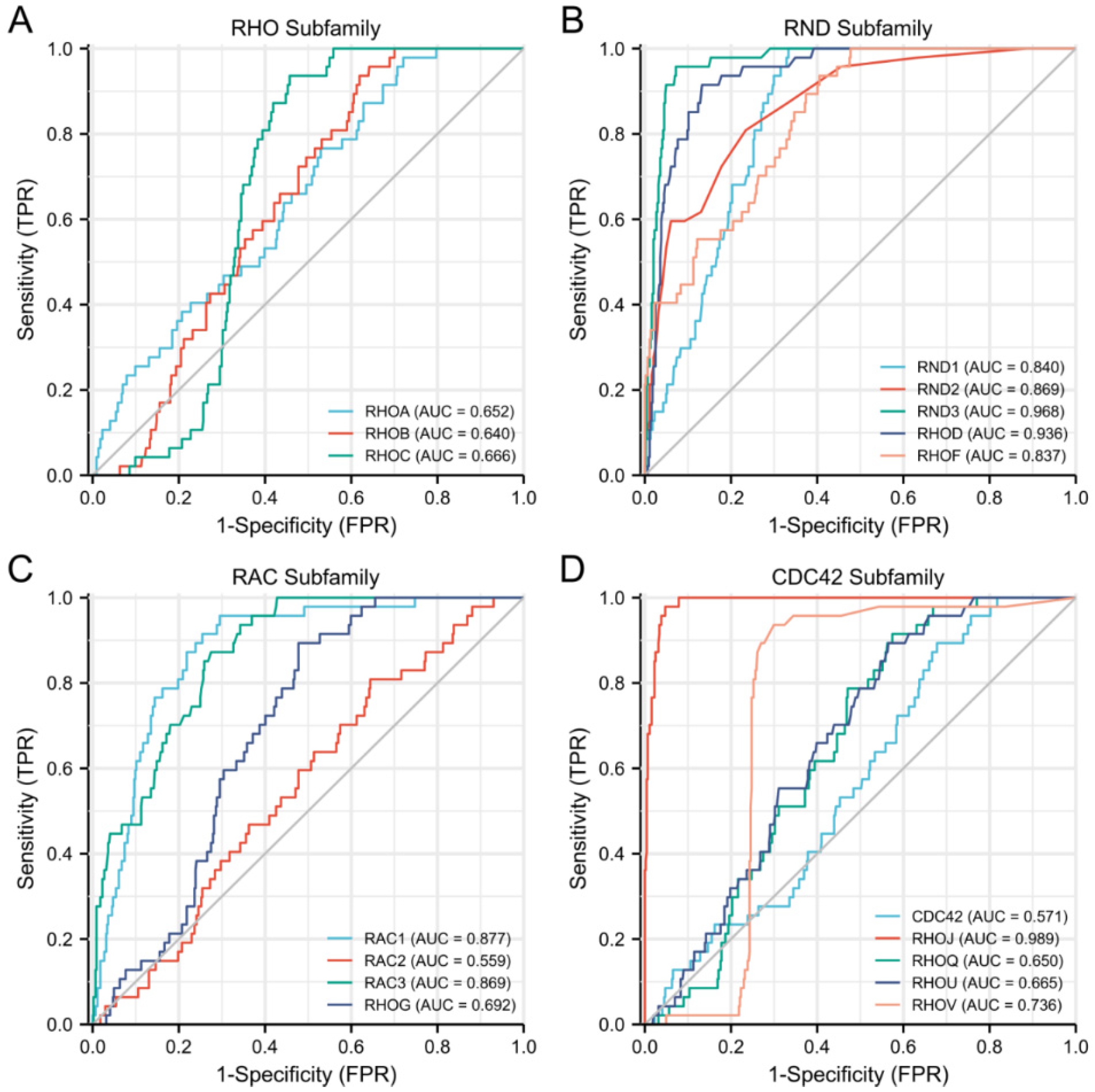
3.2. Diagnostic Value of the Rho/Rac Family Members in DLBCL
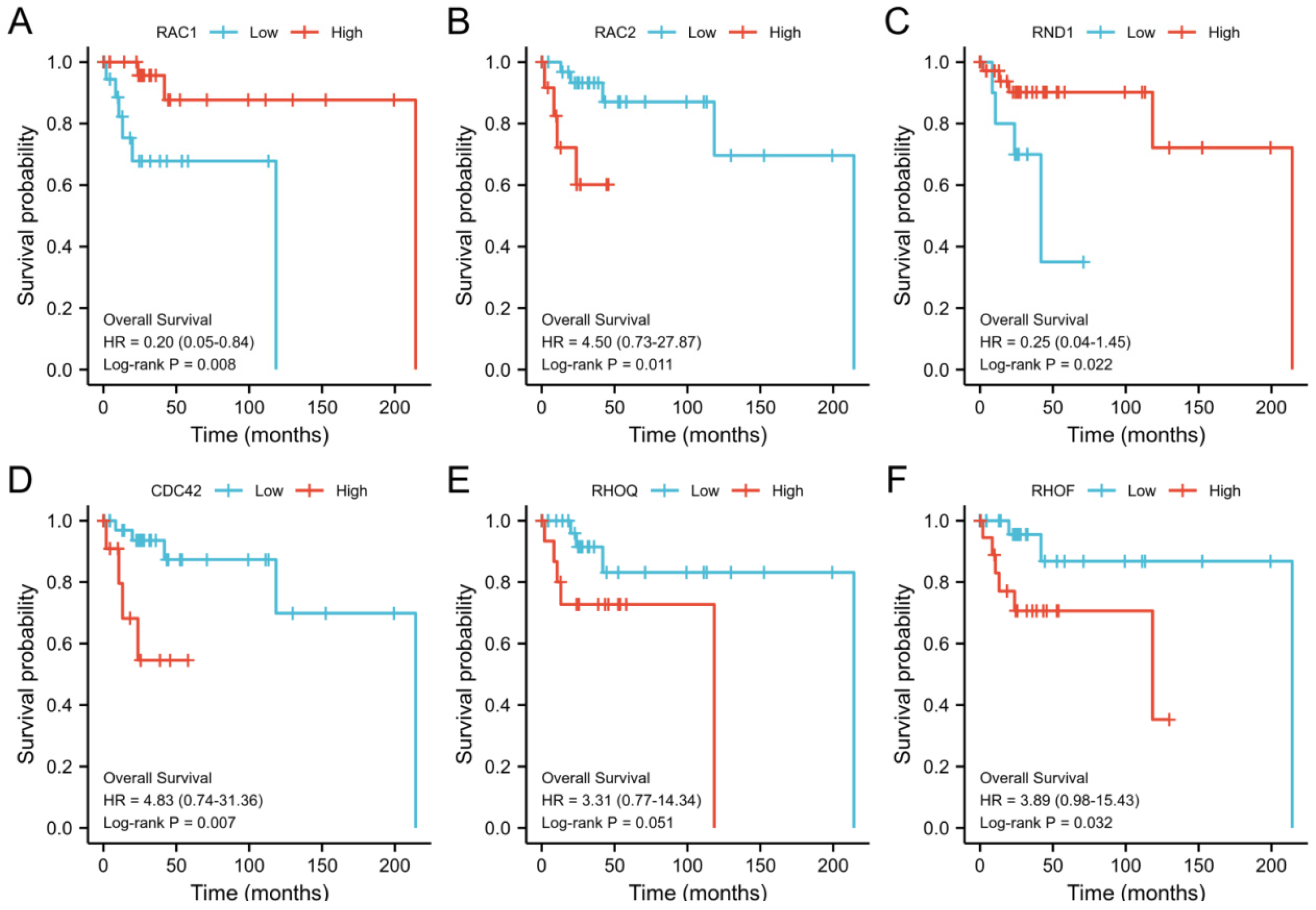
3.3. Prognostic Potential of the Rho/Rac Family Members for DLBCL
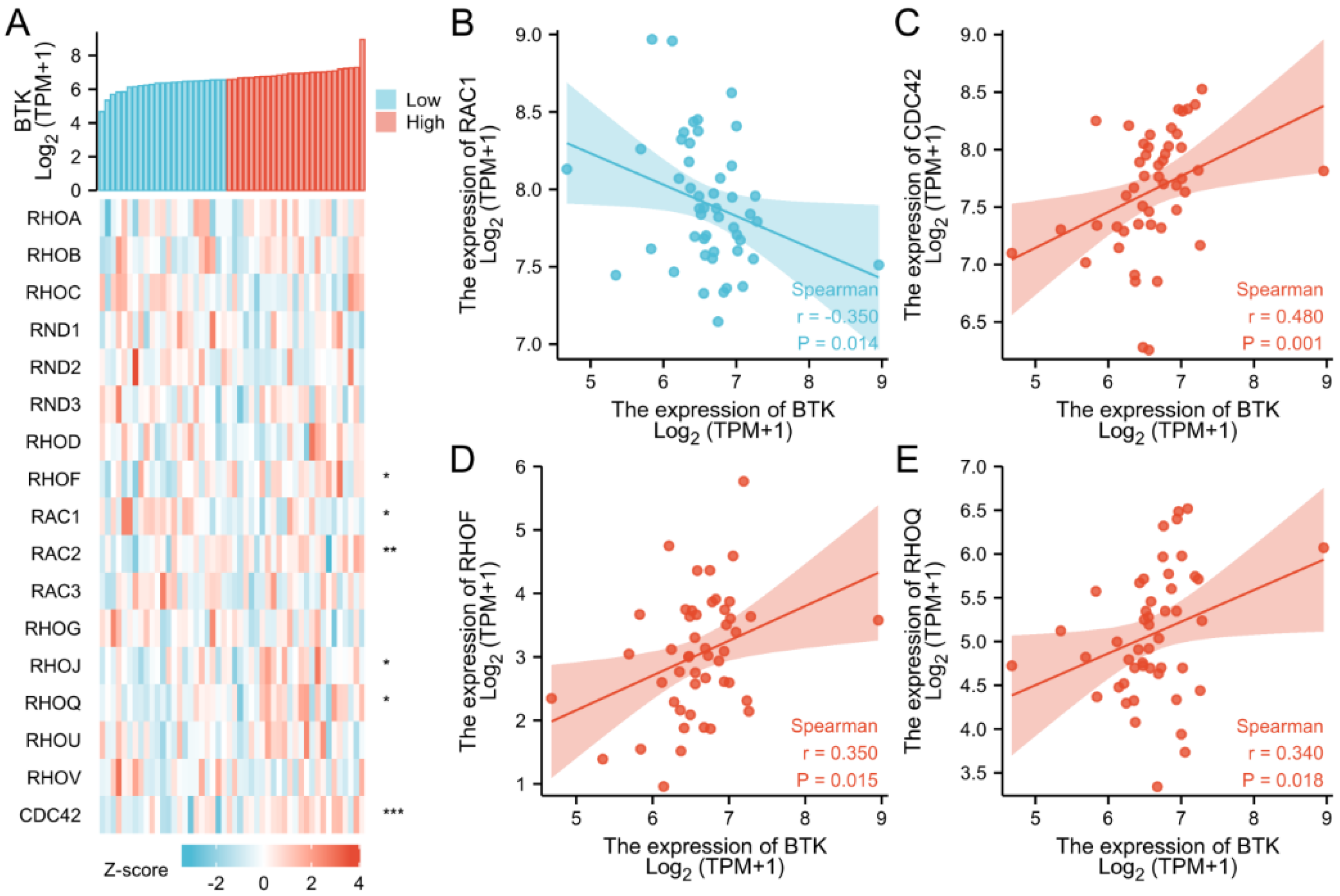
3.4. Correlation between the Expression of Rho/Rac Family Members and BTK
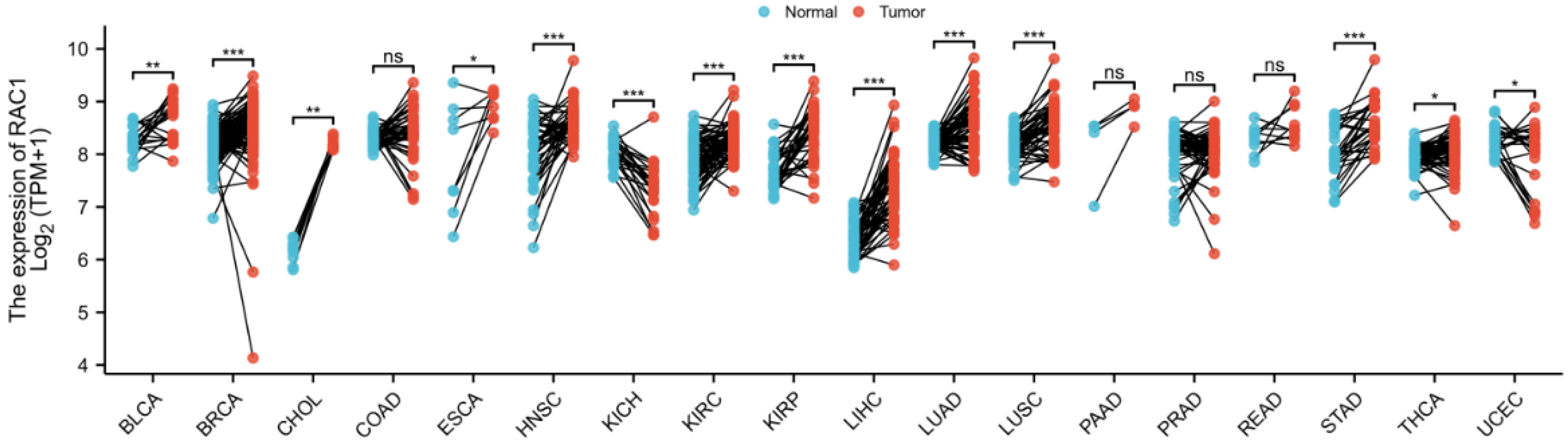
3.5. Expression Levels of RAC1 in Multiple Cancers
3.6. Correlation between RAC1 Expression and DLBCL Clinical Characteristics
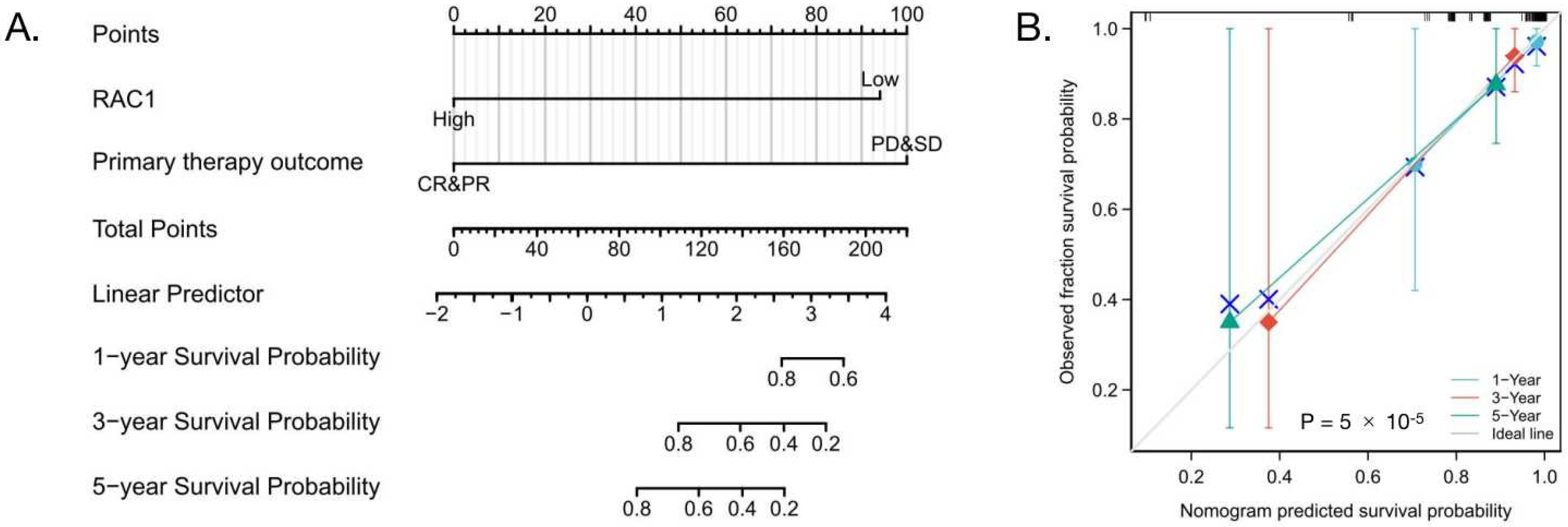
3.7. High-Level Expression of RAC1 Is an Independent Risk Factor for OS of DLBCL
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, A.; Howell, D.; Patmore, R.; Jack, A.; Roman, E. Incidence of haematological malignancy by sub-type: A report from the Haematological Malignancy Research Network. Br. J. Cancer 2011, 105, 1684–1692. [Google Scholar] [CrossRef] [PubMed]
- International non-Hodgkin’s Lymphoma Prognostic Factors project. A predictive model for aggressive non-Hodgkin’s lymphoma. N. Engl. J. Med. 1993, 329, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Salles, G.; Jong, D.; Xie, W.L.; Rosenwald, A.; Chhanabhai, M.; Gaulard, P.; Klapper, W.; Calaminici, M.; Sander, B.; Thorns, C.; et al. Prognostic significance of immunohistochemical biomarkers in diffuse large B-cell lymphoma: A study from the Lunenburg Lymphoma Biomarker Consortium. Blood 2011, 117, 7070–7078. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.W.; King, R.L.; Staiger, A.M.; Ben-Neriah, S.; Jiang, A.X.; Horn, H.; Mottok, A.; Farinha, P.; Slack, G.W.; Ennishi, D.; et al. High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements with diffuse large B-cell lymphoma morphology. Blood 2018, 131, 2060–2064. [Google Scholar] [CrossRef] [PubMed]
- Madaule, P.; Axel, R. A novel ras-related gene family. Cell 1985, 41, 31–40. [Google Scholar] [CrossRef]
- Ridley, A.J. Rho GTPases and actin dynamics in membrane protrusions and vesicle trafficking. Trends Cell Biol. 2006, 16, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Hall, A. Rho family GTPases. Biochem. Soc. Trans. 2012, 40, 1378–1382. [Google Scholar] [CrossRef] [PubMed]
- Etienne-Manneville, S.; Hall, A. Rho GTPases in cell biology. Nature 2002, 420, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.P.; Papaioannou, A.; Malliri, A. Deregulation of Rho GTPases in cancer. Small GTPases 2016, 7, 123–138. [Google Scholar] [CrossRef] [PubMed]
- Masuda, M.; Maruyama, T.; Ohta, T.; Ito, A.; Hayashi, T.; Tsukasaki, K.; Kamihira, S.; Yamaoka, S.; Hoshino, H.; Yoshida, T.; et al. CADM1 interacts with Tiam1 and promotes invasive phenotype of human T-cell leukemia virus type I-transformed cells and adult T-cell leukemia cells. J. Biol. Chem. 2010, 285, 15511–15522. [Google Scholar] [CrossRef] [PubMed]
- Durand-Onayli, V.; Haslauer, T.; Harzschel, A.; Hartmann, T.N. Rac GTPases in Hematological Malignancies. Int. J. Mol. Sci. 2018, 19, 4041. [Google Scholar] [CrossRef] [PubMed]
- Sosa, M.S.; Lopez-Haber, C.; Yang, C.F.; Wang, H.B.; Lemmon, M.A.; Busillo, J.M.; Luo, J.S.; Benovic, J.L.; Klein-Szanto, A.; Yagi, H.; et al. Identification of the Rac-GEF P-Rex1 as an essential mediator of ErbB signaling in breast cancer. Mol. Cell 2010, 40, 877–892. [Google Scholar] [CrossRef] [PubMed]
- Citterio, C.; Menacho-Márquez, M.; García-Escudero, R.; Larive, R.M.; Barreiro, O.; Sánchez-Madrid, F.; Paramio, J.M.; Bustelo, X.R. The rho exchange factors vav2 and vav3 control a lung metastasis-specific transcriptional program in breast cancer cells. Sci. Signal. 2012, 5, ra71. [Google Scholar] [CrossRef] [PubMed]
- Ognibene, M.; Barbieri, O.; Vanni, C.; Mastracci, L.; Astigiano, S.; Emionite, L.; Salani, B.; Fedele, M.; Resaz, R.; Tenca, C.; et al. High frequency of development of B cell lymphoproliferation and diffuse large B cell lymphoma in Dbl knock-in mice. J. Mol. Med. 2011, 89, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, X.Q.; Zhang, H.; Li, X.Y.; Li, X.X.; Cong, M.; Peng, F.L.; Yu, J.Y.; Zhang, X.; Yang, Q.F.; Hu, G.H. Differential effects on lung and bone metastasis of breast cancer by Wnt signalling inhibitor DKK1. Nat. Cell Biol. 2017, 19, 1274–1285. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.L.; Yu, Z.L.; Rong, Z.Y.; Luo, Z.; Zhang, J.; Qiu, Z.J.; Huang, C. The novel GINS4 axis promotes gastric cancer growth and progression by activating Rac1 and CDC42. Theranostics 2019, 9, 8294–8311. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.Z.; Qiu, Q.Z.; Qian, X.Y.; Yi, J.N.; Jiao, J.L.; Yu, M.Q.; Li, X.F.; Li, J.; Mi, C.Y.; Zhang, J.S.; et al. Long noncoding RNA LCAT1 functions as a ceRNA to regulate RAC1 function by sponging miR-4715-5p in lung cancer. Mol. Cancer 2019, 18, 171. [Google Scholar] [CrossRef] [PubMed]
- Payapilly, A.; Malliri, A. Compartmentalisation of RAC1 signalling. Curr. Opin. Cell Biol. 2018, 54, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Kato, R.M.; Garcia-Lloret, M.; Wahl, M.I.; Rawlings, D.J. Engagement of the human pre-B cell receptor generates a lipid raft-dependent calcium signaling complex. Immunity 2000, 13, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Inabe, K.; Ishiai, M.; Scharenberg, A.M.; Freshney, N.; Downward, J.; Kurosaki, T. Vav3 modulates B cell receptor responses by regulating phosphoinositide 3-kinase activation. J. Exp. Med. 2002, 195, 189–200. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Low-Level Expression of RAC1 | High-Level Expression of RAC1 | p |
|---|---|---|---|
| n | 24 | 24 | |
| Age, n (%) | 0.244 | ||
| ≤60 | 11 (22.9%) | 16 (33.3%) | |
| >60 | 13 (27.1%) | 8 (16.7%) | |
| Gender, n (%) | 0.772 | ||
| Female | 12 (25%) | 14 (29.2%) | |
| Male | 12 (25%) | 10 (20.8%) | |
| Clinical stage, n (%) | 0.056 | ||
| Stage I | 1 (2.4%) | 7 (16.7%) | |
| Stage II | 8 (19%) | 9 (21.4%) | |
| Stage III | 4 (9.5%) | 1 (2.4%) | |
| Stage IV | 8 (19%) | 4 (9.5%) | |
| Primary therapy outcome, n (%) | 0.26 | ||
| PD | 3 (6.5%) | 2 (4.3%) | |
| SD | 2 (4.3%) | 1 (2.2%) | |
| PR | 3 (6.5%) | 0 (0%) | |
| CR | 15 (32.6%) | 20 (43.5%) | |
| Age, mean ± SD | 56.67 ± 14.42 | 55.88 ± 13.76 | 0.847 |
| Characteristics | Total (N) | OR | p Value |
|---|---|---|---|
| Age (>60 vs. ≤60) | 48 | 0.423 (0.127–1.338) | 0.149 |
| Gender (Male vs. Female) | 48 | 0.714 (0.225–2.229) | 0.563 |
| Clinical stage (Stage III and Stage IV vs. Stage I and Stage II) | 42 | 0.234 (0.058–0.844) | 0.032 |
| Primary therapy outcome (PD and SD vs. CR and PR) | 46 | 0.540 (0.099–2.520) | 0.441 |
| Characteristics | Total (N) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | ||
| Age | 48 | ||||
| ≤60 | 27 | Reference | |||
| >60 | 21 | 1.666 (0.416–6.673) | 0.471 | ||
| Gender | 48 | ||||
| Female | 26 | Reference | |||
| Male | 22 | 1.039 (0.250–4.324) | 0.958 | ||
| Clinical stage | 42 | ||||
| Stage I and Stage II | 25 | Reference | |||
| Stage III and Stage IV | 17 | 1.917 (0.422–8.715) | 0.400 | ||
| Primary therapy outcome | 46 | ||||
| CR and PR | 38 | Reference | |||
| SD and PD | 8 | 10.480 (2.292–47.922) | 0.002 | 15.676 (2.603–94.406) | 0.003 |
| RAC1 | 48 | ||||
| Low | 24 | Reference | |||
| High | 24 | 0.106 (0.013–0.867) | 0.036 | 0.075 (0.008–0.726) | 0.025 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, X.; Li, Y.; Zhang, W.; Zhang, J.; Chen, B.; Ge, Z. RAC1, a Potential Diagnostic and Prognostic Marker for Diffuse Large B Cell Lymphoma. Cells 2022, 11, 4039. https://doi.org/10.3390/cells11244039
Wu X, Li Y, Zhang W, Zhang J, Chen B, Ge Z. RAC1, a Potential Diagnostic and Prognostic Marker for Diffuse Large B Cell Lymphoma. Cells. 2022; 11(24):4039. https://doi.org/10.3390/cells11244039
Chicago/Turabian StyleWu, Xue, Yuan Li, Wandong Zhang, Jing Zhang, Baoan Chen, and Zheng Ge. 2022. "RAC1, a Potential Diagnostic and Prognostic Marker for Diffuse Large B Cell Lymphoma" Cells 11, no. 24: 4039. https://doi.org/10.3390/cells11244039
APA StyleWu, X., Li, Y., Zhang, W., Zhang, J., Chen, B., & Ge, Z. (2022). RAC1, a Potential Diagnostic and Prognostic Marker for Diffuse Large B Cell Lymphoma. Cells, 11(24), 4039. https://doi.org/10.3390/cells11244039






