The Efficacy of HGF/VEGF Gene Therapy for Limb Ischemia in Mice with Impaired Glucose Tolerance: Shift from Angiogenesis to Axonal Growth and Oxidative Potential in Skeletal Muscle
Abstract
1. Introduction
2. Methods and Materials
2.1. Animal Strain, Housing, Diets and Ethical Approval
2.2. Glucose and Insulin Tolerance Tests
2.3. Plasmid Vector Design and Purification
2.4. Hindlimb Ischemia Modeling and Postsurgical Care
2.5. Laser Doppler Perfusion Measurement
2.6. Hematoxylin/Eosin Staining
2.7. Immunofluorescent Staining
2.8. Western Blotting
2.9. Statistical Analysis
3. Results
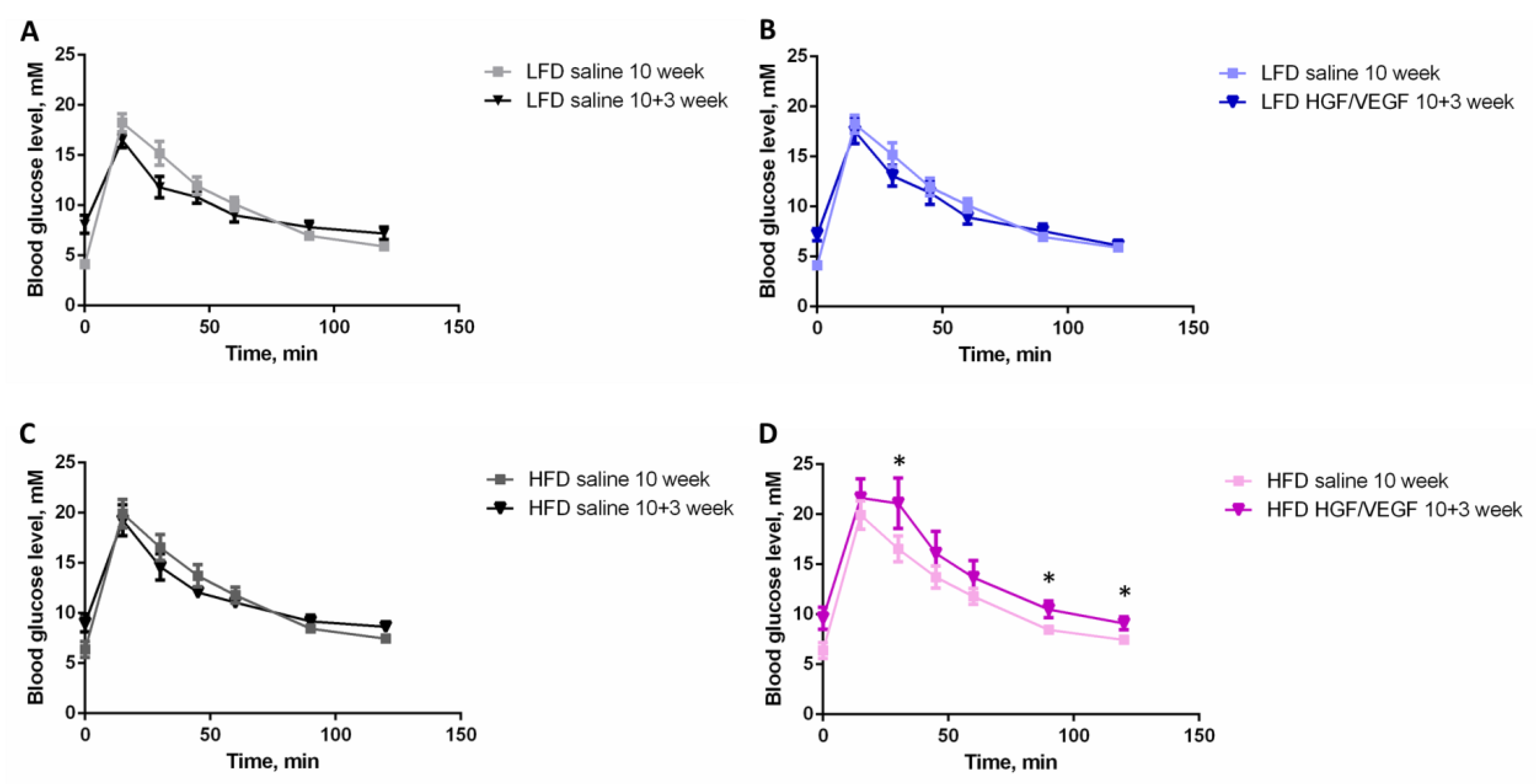
3.1. HGF/VEGF Plasmid Injection to Ischemic Muscle Aggravates Glucose Intolerance in HFD Conditions at 13 Week of Dietary Intervention
3.2. GTT Demonstrates a Shift to Glucose Intolerance after HGF/VEGF Plasmid Injection to Ischemic Muscle under HFD Conditions
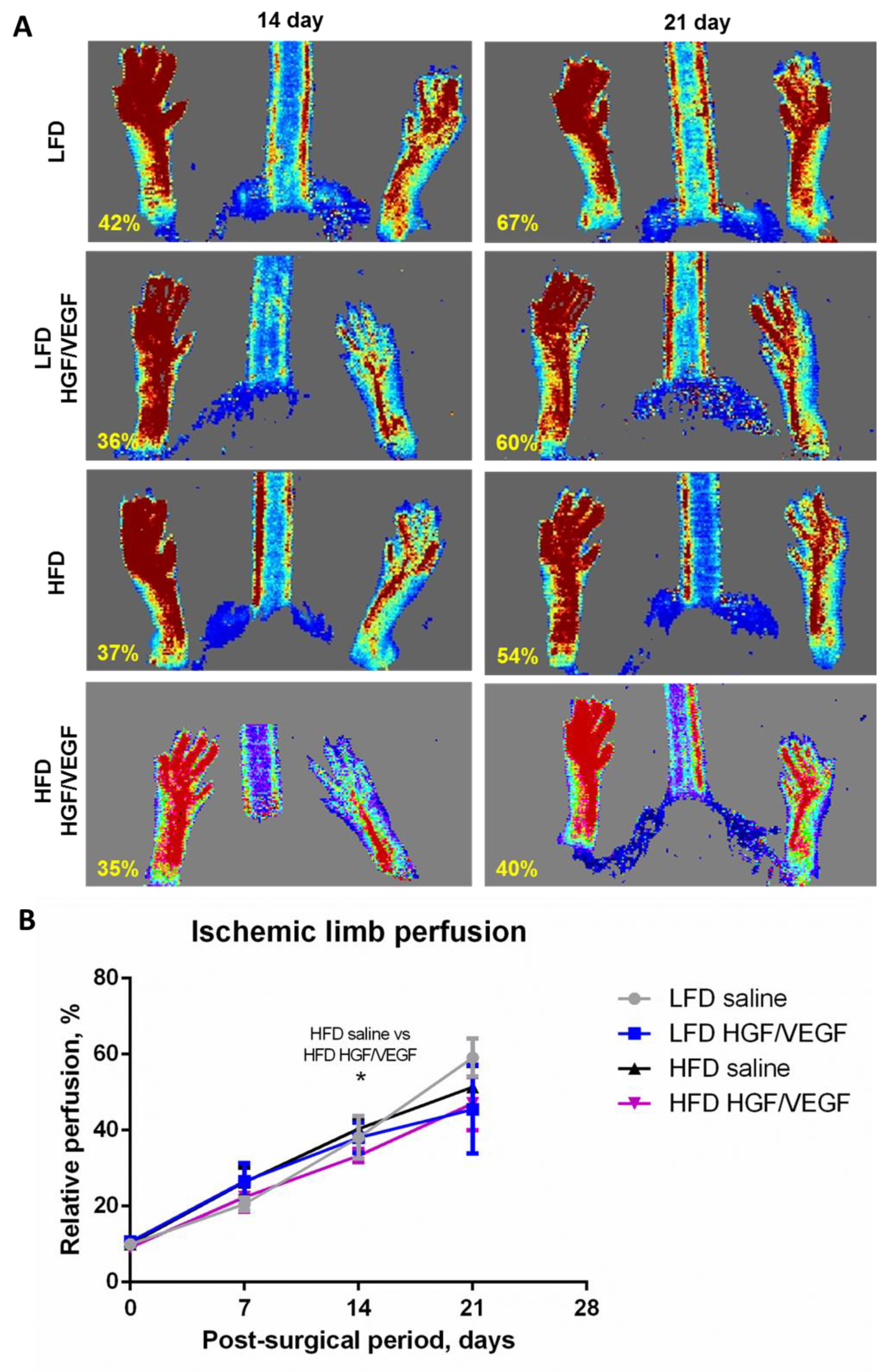
3.3. HGF/VEGF Plasmid Injection under HFD Conditions Results in Delayed Blood Flow Recovery with Similar Outcome at 3 Weeks in All Study Groups
3.4. HGF/VEGF Plasmid Injection had No Effects on Necrosis and Inflammation under HFD Conditions, but Increased These Parameters under LFD Conditions
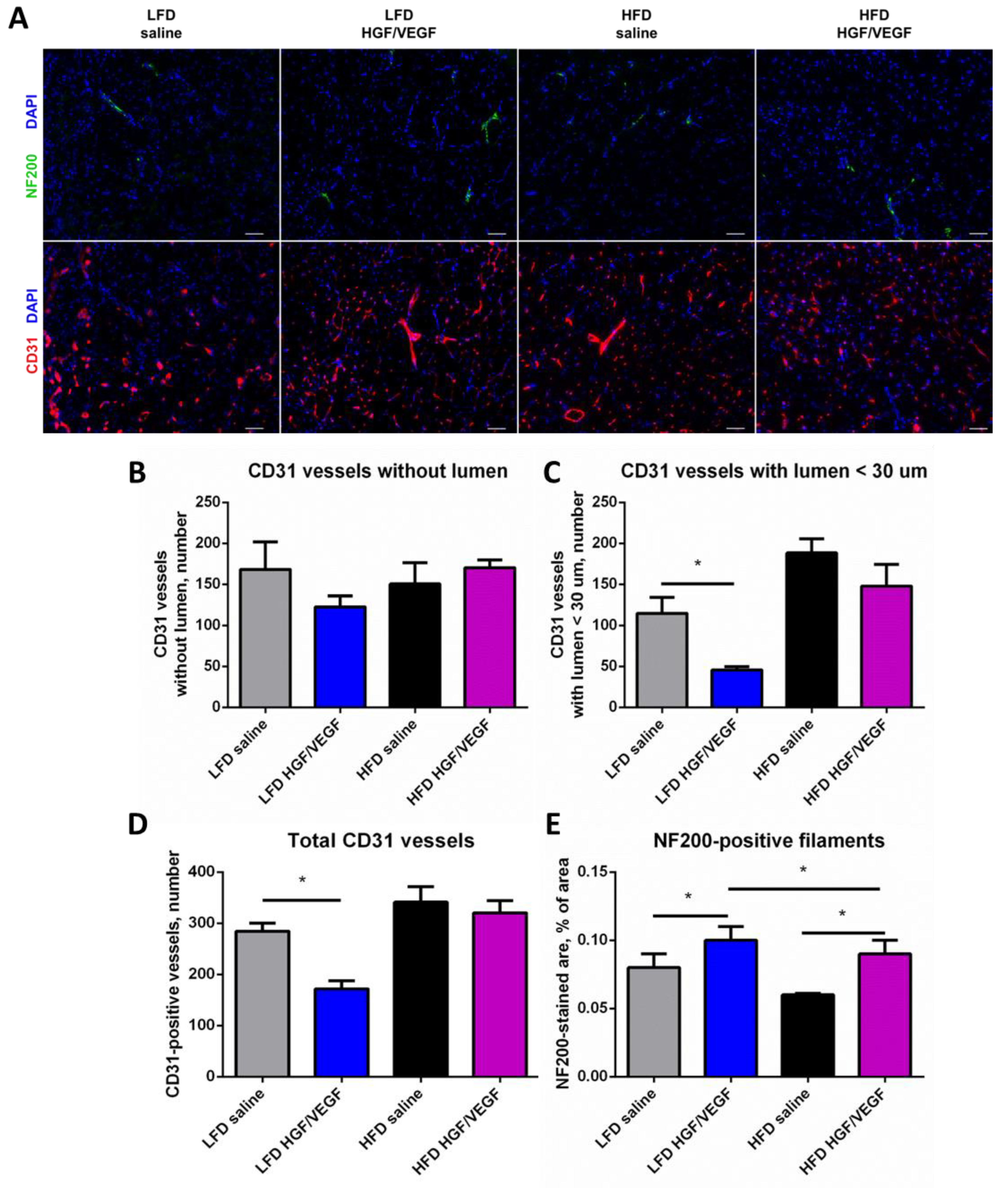
3.5. Delivery of HGF/VEGF Plasmid Fails to Improve Vascularization, but Activates Neuritogenesis under Both Dietary Settings
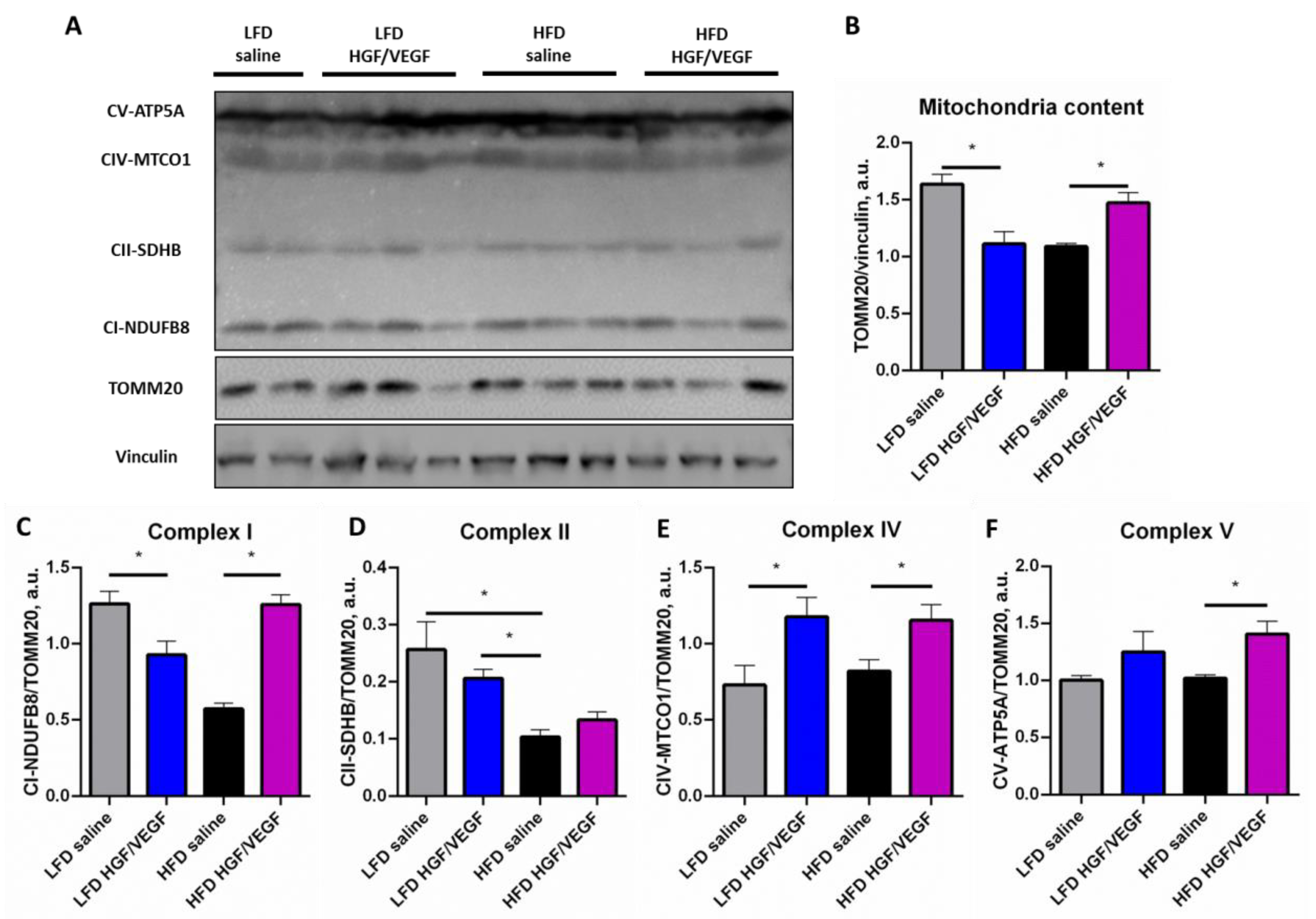
3.6. HGF/VEGF Plasmid Injection Stimulated Mitochondrial Biogenesis and ETC Components Expression in Ischemic Skeletal Muscle under HFD Conditions
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Hammer, A.; Steiner, S. Gene therapy for therapeutic angiogenesis in peripheral arterial disease—A systematic review and meta-analysis of randomized, controlled trials. Vasa 2013, 42, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Morishita, R.; Shimamura, M.; Takeya, Y.; Nakagami, H.; Chujo, M.; Ishihama, T.; Yamada, E.; Rakugi, H. Combined analysis of clinical data on HGF gene therapy to treat critical limb ischemia in Japan. Curr. Gene Ther. 2020, 20, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Korpela, H.; Järveläinen, N.; Siimes, S.; Lampela, J.; Airaksinen, J.; Valli, K.; Turunen, M.; Pajula, J.; Nurro, J.; Ylä-Herttuala, S. Gene therapy for ischaemic heart disease and heart failure. J. Intern. Med. 2021, 290, 567–582. [Google Scholar] [CrossRef] [PubMed]
- Kastrup, J.; Jørgensen, E.; Rück, A.; Tägil, K.; Glogar, D.; Ruzyllo, W.; Bøtker, H.E.; Dudek, D.; Drvota, V.; Hesse, B.; et al. Direct intramyocardial plasmid vascular endothelial growth factor-A165 gene therapy in patients with stable severe angina pectoris A randomized double-blind placebo-controlled study: The Euroinject One trial. J. Am. Coll. Cardiol. 2005, 45, 982–988. [Google Scholar] [CrossRef] [PubMed]
- Penn, M.S.; Mendelsohn, F.O.; Schaer, G.L.; Sherman, W.; Farr, M. An open-label dose escalation study to evaluate the safety of administration of nonviral stromal cell-derived factor-1 plasmid to treat symptomatic ischemic heart failure. Circ. Res. 2013, 112, 816–825. [Google Scholar] [CrossRef] [PubMed]
- Shishehbor, M.H.; Rundback, J.; Bunte, M.; Hammad, T.A.; Miller, L.; Patel, P.D.; Sadanandan, S.; Fitzgerald, M.; Pastore, J.; Kashyap, V.; et al. SDF-1 plasmid treatment for patients with peripheral artery disease (STOP-PAD): Randomized, double-blind, placebo-controlled clinical trial. Vasc. Med. 2019, 24, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Makarevich, P.I.; Dergilev, K.V.; Tsokolaeva, Z.I.; Boldyreva, M.A.; Shevchenko, E.K.; Gluhanyuk, E.V.; Gallinger, J.O.; Menshikov, M.Y.; Parfyonova, Y.V. Angiogenic and pleiotropic effects of VEGF165 and HGF combined gene therapy in a rat model of myocardial infarction. PLoS ONE 2018, 13, e0197566. [Google Scholar] [CrossRef] [PubMed]
- Slobodkina, E.; Boldyreva, M.; Karagyaur, M.; Eremichev, R.; Alexandrushkina, N.; Balabanyan, V.; Akopyan, Z.; Parfyonova, Y.; Tkachuk, V.; Makarevich, P. Therapeutic angiogenesis by a “Dynamic Duo”: Simultaneous expression of HGF and VEGF165 by novel bicistronic plasmid restores blood flow in ischemic skeletal muscle. Pharmaceutics 2020, 12, 1231. [Google Scholar] [CrossRef] [PubMed]
- Makarevich, P.; Tsokolaeva, Z.; Shevelev, A.; Rybalkin, I.; Shevchenko, E.; Beloglazova, I.; Vlasik, T.; Tkachuk, V.; Parfyonova, Y. Combined transfer of human VEGF165 and HGF genes renders potent angiogenic effect in ischemic skeletal muscle. PLoS ONE 2012, 7, e0038776. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.M.; Criqui, M.H.; Ferrucci, L.; Guralnik, J.M.; Tian, L.; Liu, K.; Greenland, P.; Tan, J.; Schneider, J.R.S.; Clark, E.; et al. Obesity, weight change, and functional decline in peripheral arterial disease. J. Vasc. Surg. 2006, 43, 1198–1204. [Google Scholar] [CrossRef]
- Barnes, J.A.; Eid, M.A.; Creager, M.A.; Goodney, P.P. Epidemiology and risk of amputation in patients with diabetes mellitus and peripheral artery disease. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1808–1817. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.K.; Bhatt, D.L.; Montvida, O. The association of amputations and peripheral artery disease in patients with type 2 diabetes mellitus receiving sodium-glucose cotransporter type-2 inhibitors: Real-world study. Eur. Heart J. 2021, 42, 1728–1738. [Google Scholar] [CrossRef]
- Lutz, T.A.; Woods, S.C. Overview of animal models of obesity. Curr. Protoc. Pharmacol. 2012, 58, 5.61.1–5.61.8. [Google Scholar] [CrossRef]
- Chua, S.C., Jr.; Chung, W.K.; Wu-Peng, X.S.; Zhang, Y.; Liu, S.M.; Tartaglia, L.; Leibel, R.L. Phenotypes of mouse diabetes and rat fatty due to mutations in the OB (leptin) receptor. Science 1996, 271, 994–996. [Google Scholar] [CrossRef]
- Asarian, L.; Geary, N. Cyclic estradiol treatment normalizes body weight and restores physiological patterns of spontaneous feeding and sexual receptivity in ovariectomized rats. Horm. Behav. 2002, 42, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Clegg, D.J.; Gotoh, K.; Kemp, C.; Wortman, M.D.; Benoit, S.C.; Brown, L.M.; D’Alessio, D.; Tso, P.; Seeley, R.J.; Woods, S.C. Consumption of a high-fat diet induces central insulin resistance independent of adiposity. Physiol. Behav. 2011, 103, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, L.N.; Capozzi, L.C.; Turchinsky, N.J.; Bell, R.C.; Wright, D.C. Time course of high-fat diet-induced reductions in adipose tissue mitochondrial proteins: Potential mechanisms and the relationship to glucose intolerance. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E1076–E1083. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Liao, J.K. A mouse model of diet-induced obesity and insulin resistance. Methods Mol. Biol. 2012, 821, 421–433. [Google Scholar] [CrossRef]
- Calligaris, S.D.; Lecanda, M.; Solis, F.; Ezquer, M.; Gutiérrez, J.; Brandan, E.; Leiva, A.; Sobrevia, L.; Conget, P. Mice long-term high-fat diet feeding recapitulates human cardiovascular alterations: An animal model to study the early phases of diabetic cardiomyopathy. PLoS ONE 2013, 8, e60931. [Google Scholar] [CrossRef]
- Albadawi, H.; Oklu, R.; Cormier, N.R.; O’Keefe, R.M.; Heaton, J.T.; Kobler, J.B.; Austen, W.G.; Watkins, M.T. Hind limb ischemia-reperfusion injury in diet-induced obese mice. J. Surg. Res. 2014, 190, 683–691. [Google Scholar] [CrossRef]
- Kim, K.; Ro, B.; Damen, F.W.; Gramling, D.P.; Lehr, T.D.; Song, Q.; Goergen, C.J.; Roseguini, B.T. Heat therapy improves body composition and muscle function but does not affect capillary or collateral growth in a model of obesity and hindlimb ischemia. J. Appl. Physiol. (1985) 2021, 130, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Stafeev, I.; Boldyreva, M.; Michurina, S.; Mamontova, E.; Ratner, E.; Menshikov, M.; Parfyonova, Y. Grain-based dietary background impairs restoration of blood flow and skeletal muscle during hindlimb ischemia in comparison with low-fat and high-fat diets. Front. Nutr. 2022, 8, 809732. [Google Scholar] [CrossRef]
- Jin, K.; Zhu, Y.; Sun, Y.; Mao, X.O.; Xie, L.; Greenberg, D.A. Vascular endothelial growth factor (VEGF) stimulates neurogenesis in vitro and in vivo. Proc. Natl. Acad. Sci. USA 2002, 99, 11946–11950. [Google Scholar] [CrossRef] [PubMed]
- Molokotina, Y.D.; Boldyreva, M.A.; Stafeev, I.S.; Semina, E.V.; Shevchenko, E.K.; Zubkova, E.S.; Beloglazova, I.B.; Parfenova, E.V. Combined action of GDNF and HGF up-regulates axonal growth by increasing ERK1/2 phosphorylation. Bull. Exp. Biol. Med. 2019, 167, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Elias, I.; Franckhauser, S.; Ferré, T.; Vilà, L.; Tafuro, S.; Muñoz, S.; Roca, C.; Ramos, D.; Pujol, A.; Riu, E.; et al. Adipose tissue overexpression of vascular endothelial growth factor protects against diet-induced obesity and insulin resistance. Diabetes 2012, 61, 1801–1813. [Google Scholar] [CrossRef] [PubMed]
- Bonner, J.S.; Lantier, L.; Hasenour, C.M.; James, F.D.; Bracy, D.P.; Wasserman, D.H. Muscle-specific vascular endothelial growth factor deletion induces muscle capillary rarefaction creating muscle insulin resistance. Diabetes 2013, 62, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Muratsu, J.; Iwabayashi, M.; Sanada, F.; Taniyama, Y.; Otsu, R.; Rakugi, H.; Morishita, R. Hepatocyte growth factor prevented high-fat diet-induced obesity and improved insulin resistance in mice. Sci. Rep. 2017, 7, 130. [Google Scholar] [CrossRef] [PubMed]
- Szlapinski, S.K.; Hill, D.J. Metabolic adaptations to pregnancy in healthy and gestational diabetic pregnancies: The pancreas-placenta axis. Curr. Vasc. Pharmacol. 2021, 19, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Thorell, A.; Nygren, J.; Ljungqvist, O. Insulin resistance: A marker of surgical stress. Curr. Opin. Clin. Nutr. Metab. Care 1999, 2, 69–78. [Google Scholar] [CrossRef]
- Wang, C.H.; Chen, K.T.; Mei, H.F.; Lee, J.F.; Cherng, W.J.; Lin, S.J. Assessment of mouse hind limb endothelial function by measuring femoral artery blood flow responses. J. Vas. Surg. 2011, 53, 1350–1358. [Google Scholar] [CrossRef]
- Thiruvoipati, T.; Kielhorn, C.E.; Armstrong, E.J. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J. Diabetes 2015, 6, 961–969. [Google Scholar] [CrossRef] [PubMed]
- McMahon, J.M.; Wells, K.E.; Bamfo, J.E.; Cartwright, M.A.; Wells, D.J. Inflammatory responses following direct injection of plasmid DNA into skeletal muscle. Gene Ther. 1998, 5, 1283–1290. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yew, N.S.; Zhao, H.; Wu, I.H.; Song, A.; Tousignant, J.D.; Przybylska, M.; Cheng, S.H. Reduced inflammatory response to plasmid DNA vectors by elimination and inhibition of immunostimulatory CpG motifs. Mol. Ther. 2000, 1, 255–262. [Google Scholar] [CrossRef]
- Proto, J.D.; Tang, Y.; Lu, A.; Chen, W.C.W.; Stahl EPoddar, M.; Beckman, S.A.; Robbins, P.D.; Nidernhofer, L.J.; Imbrogno, K.; Hannigan, T.; et al. NF-κB inhibition reveals a novel role for HGF during skeletal muscle repair. Cell Death Dis. 2015, 6, e1730. [Google Scholar] [CrossRef][Green Version]
- Charles, M.; Ejskjaer, N.; Witte, D.R.; Borch-Johnsen, K.; Lauritzen, T.; Sandbaek, A. Prevalence of neuropathy and peripheral arterial disease and the impact of treatment in people with screen-detected type 2 diabetes: The ADDITION-Denmark study. Diabetes Care 2011, 34, 2244–2249. [Google Scholar] [CrossRef] [PubMed]
- Kessler, J.A.; Shaibani, A.; Sang, C.N.; Christiansen, M.; Kudrow, D.; Vinik, A.; Shin, N.; VM202 study group. Gene therapy for diabetic peripheral neuropathy: A randomized, placebo-controlled phase III study of VM202, a plasmid DNA encoding human hepatocyte growth factor. Clin. Transl. Sci. 2021, 14, 1176–1184. [Google Scholar] [CrossRef] [PubMed]
- Sondell, M.; Lundborg, G.; Kanje, M. Vascular endothelial growth factor has neurotrophic activity and stimulates axonal outgrowth, enhancing cell survival and Schwann cell proliferation in the peripheral nervous system. J. Neurosci. 1999, 19, 5731–5740. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.R.; Lee, J.; Lee, D.; Nho, B.; Kim, S. Hepatocyte growth factor (HGF) promotes peripheral nerve regeneration by activating repair Schwann cells. Sci. Rep. 2018, 8, 8316. [Google Scholar] [CrossRef] [PubMed]
- Zor, F.; Deveci, M.; Kilic, A.; Ozdag, M.F.; Kurt, B.; Sengezer, M.; Sönmez, T.T. Effect of VEGF gene therapy and hyaluronic acid film sheath on peripheral nerve regeneration. Microsurgery 2014, 34, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Boldyreva, M.A.; Bondar, I.V.; Stafeev, I.S.; Makarevich, P.I.; Beloglazova, I.B.; Zubkova, E.S.; Shevchenko, E.K.; Molokotina, Y.D.; Karagyaur, M.D.; Ratner, E.I.; et al. Plasmid-based gene therapy with hepatocyte growth factor stimulates peripheral nerve regeneration after traumatic injury. Biomed. Pharmacother. 2018, 101, 682–690. [Google Scholar] [CrossRef] [PubMed]
- Kelley, D.E.; He, J.; Menshikova, E.V.; Ritov, V.B. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002, 51, 2944–2950. [Google Scholar] [CrossRef]
- Brunetta, H.S.; de Paula, G.C.; de Oliveira, J.; Martins, E.L.; Dos Santos, G.J.; Galina, A.; Rafacho, A.; de Bem, A.F.; Nunes, E.A. Decrement in resting and insulin-stimulated soleus muscle mitochondrial respiration is an early event in diet-induced obesity in mice. Exp. Physiol. 2019, 104, 306–321. [Google Scholar] [CrossRef]
- Cannon, D.T.; Rodewohl, L.; Adams, V.; Breen, E.C.; Bowen, T.S. Skeletal myofiber VEGF deficiency leads to mitochondrial, structural, and contractile alterations in mouse diaphragm. J. Appl. Physiol. (1985) 2019, 127, 1360–1369. [Google Scholar] [CrossRef] [PubMed]
- Perdomo, G.; Martinez-Brocca, M.A.; Bhatt, B.A.; Brown, N.F.; O’Doherty, R.M.; Garcia-Ocaña, A. Hepatocyte growth factor is a novel stimulator of glucose uptake and metabolism in skeletal muscle cells. J. Biol. Chem. 2008, 283, 13700–13706. [Google Scholar] [CrossRef]
- Cao, Z.; Xie, Y.; Yu, L.; Li, Y.; Wang, Y. Hepatocyte growth factor (HGF) and stem cell factor (SCF) maintained the stemness of human bone marrow mesenchymal stem cells (hBMSCs) during long-term expansion by preserving mitochondrial function via the PI3K/AKT, ERK1/2, and STAT3 signaling pathways. Stem Cell Res. Ther. 2020, 11, 329. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Roves, P.; Huss, J.M.; Han, D.H.; Hancock, C.R.; Iglesias-Gutierrez, E.; Chen, M.; Holloszy, J.O. Raising plasma fatty acid concentration induces increased biogenesis of mitochondria in skeletal muscle. Proc. Natl. Acad. Sci. USA 2007, 104, 10709–10713. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stafeev I, I.S.; Boldyreva, M.A.; Michurina, S.S.; Agareva, M.Y.; Radnaeva, A.V.; Menshikov, M.Y.; Hu, Y.-C.; Makarevich, P.I.; Parfyonova, Y.V. The Efficacy of HGF/VEGF Gene Therapy for Limb Ischemia in Mice with Impaired Glucose Tolerance: Shift from Angiogenesis to Axonal Growth and Oxidative Potential in Skeletal Muscle. Cells 2022, 11, 3824. https://doi.org/10.3390/cells11233824
Stafeev I IS, Boldyreva MA, Michurina SS, Agareva MY, Radnaeva AV, Menshikov MY, Hu Y-C, Makarevich PI, Parfyonova YV. The Efficacy of HGF/VEGF Gene Therapy for Limb Ischemia in Mice with Impaired Glucose Tolerance: Shift from Angiogenesis to Axonal Growth and Oxidative Potential in Skeletal Muscle. Cells. 2022; 11(23):3824. https://doi.org/10.3390/cells11233824
Chicago/Turabian StyleStafeev I, Iurii S., Maria A. Boldyreva, Svetlana S. Michurina, Margarita Yu. Agareva, Arina V. Radnaeva, Mikhail Yu. Menshikov, Yu-Chen Hu, Pavel I. Makarevich, and Yelena V. Parfyonova. 2022. "The Efficacy of HGF/VEGF Gene Therapy for Limb Ischemia in Mice with Impaired Glucose Tolerance: Shift from Angiogenesis to Axonal Growth and Oxidative Potential in Skeletal Muscle" Cells 11, no. 23: 3824. https://doi.org/10.3390/cells11233824
APA StyleStafeev I, I. S., Boldyreva, M. A., Michurina, S. S., Agareva, M. Y., Radnaeva, A. V., Menshikov, M. Y., Hu, Y.-C., Makarevich, P. I., & Parfyonova, Y. V. (2022). The Efficacy of HGF/VEGF Gene Therapy for Limb Ischemia in Mice with Impaired Glucose Tolerance: Shift from Angiogenesis to Axonal Growth and Oxidative Potential in Skeletal Muscle. Cells, 11(23), 3824. https://doi.org/10.3390/cells11233824










