Sex-Dependent Differences in Colorectal Cancer: With a Focus on Obesity
Abstract
1. Introduction
2. Method
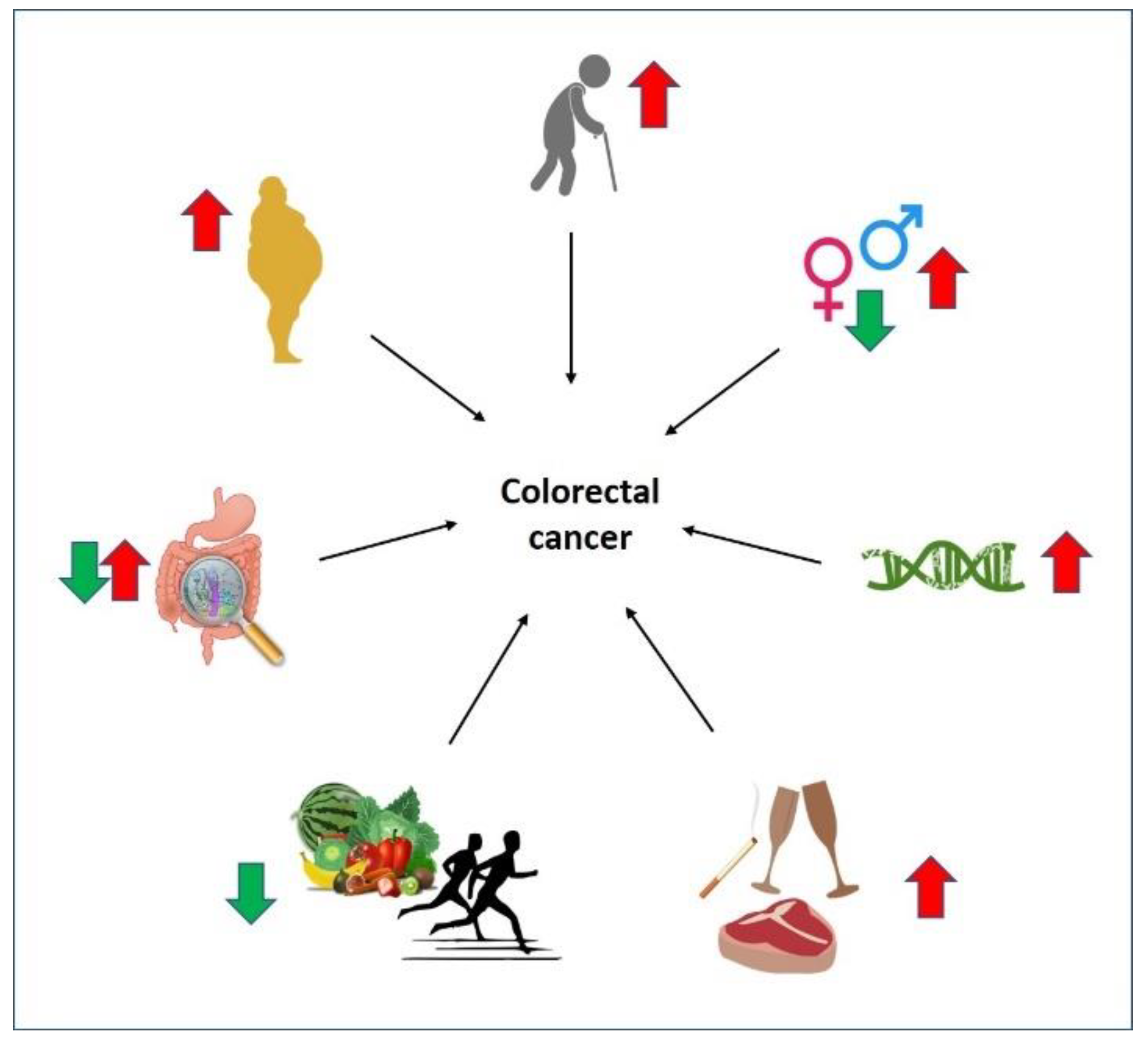
3. Factors Influencing CRC
3.1. Age
3.2. Sex
3.3. Location, Lifestyle, and Diet
3.4. Gut Microbiome
3.5. Other Diseases Leading to CRC
4. Sex-Dependent Differences in Obesity-Associated CRC
4.1. Obesity Increases CRC Incidence Differently in Males and Females
4.2. Sex-Based Effect of Adipokines in Obesity-Associated CRC
4.3. Obesity-Induced Chronic Inflammation Sex-Dependently Affects CRC
4.4. Obesity and Sex Hormones Affect CRC
4.4.1. Estrogens and Their Receptors
4.4.2. Androgens and Their Receptors
5. Lifestyle and Its Sex-Dependent Impact on CRC
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Agency for Research on Cancer Global Cancer Observatory: Cancer Today. Available online: https://gco.iarc.fr/ (accessed on 20 September 2022).
- Siegel, R.L.; Miller, K.D.; Goding Sauer, A.; Fedewa, S.A.; Butterly, L.F.; Anderson, J.C.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Xi, Y.; Xu, P. Global colorectal cancer burden in 2020 and projections to 2040. Transl. Oncol. 2021, 14, 101174. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Lu, B.; Luo, C.; Cai, J.; Lu, M.; Zhang, Y.; Chen, H.; Dai, M. Incidence, mortality, survival, risk factor and screening of colorectal cancer: A comparison among China, Europe, and northern America. Cancer Lett. 2021, 522, 255–268. [Google Scholar] [CrossRef]
- Chung, R.Y.; Tsoi, K.K.F.; Kyaw, M.H.; Lui, A.R.; Lai, F.T.T.; Sung, J.J. A population-based age-period-cohort study of colorectal cancer incidence comparing Asia against the West. Cancer Epidemiol. 2019, 59, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Al-Joufi, F.A.; Setia, A.; Salem-Bekhit, M.M.; Sahu, R.K.; Alqahtani, F.Y.; Widyowati, R.; Aleanizy, F.S. Molecular pathogenesis of colorectal cancer with an emphasis on recent advances in biomarkers, as well as nanotechnology-based diagnostic and therapeutic approaches. Nanomaterials 2022, 12, 169. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Yue, G.G.L.; Leung, P.C.; Wong, C.K.; Lau, C.B.S. A review on the molecular mechanisms, the therapeutic treatment including the potential of herbs and natural products, and target prediction of obesity-associated colorectal cancer. Pharmacol. Res. 2022, 175, 106031. [Google Scholar] [CrossRef] [PubMed]
- Grady, W.M.; Markowitz, S.D. The molecular pathogenesis of colorectal cancer and its potential application to colorectal cancer screening. Dig. Dis. Sci. 2015, 60, 762–772. [Google Scholar] [CrossRef]
- Bacher, J.W.; Flanagan, L.A.; Smalley, R.L.; Nassif, N.A.; Burgart, L.J.; Halberg, R.B.; Megid, W.M.; Thibodeau, S.N. Development of a fluorescent multiplex assay for detection of MSI-High tumors. Dis. Markers 2004, 20, 237–250. [Google Scholar] [CrossRef]
- Grady, W.M. Genomic instability and colon cancer. Cancer Metastasis Rev. 2004, 23, 11–27. [Google Scholar] [CrossRef]
- Imperiale, T.F.; Ransohoff, D.F.; Itzkowitz, S.H.; Levin, T.R.; Lavin, P.; Lidgard, G.P.; Ahlquist, D.A.; Berger, B.M. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 2014, 370, 1287–1297. [Google Scholar] [CrossRef]
- Chen, W.D.; Han, Z.J.; Skoletsky, J.; Olson, J.; Sah, J.; Myeroff, L.; Platzer, P.; Lu, S.; Dawson, D.; Willis, J.; et al. Detection in fecal DNA of colon cancer-specific methylation of the nonexpressed vimentin gene. J. Natl. Cancer Inst. 2005, 97, 1124–1132. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Prz. Gastroenterol. 2019, 14, 89–103. [Google Scholar] [CrossRef] [PubMed]
- White, A.; Ironmonger, L.; Steele, R.J.C.; Ormiston-Smith, N.; Crawford, C.; Seims, A. A review of sex-related differences in colorectal cancer incidence, screening uptake, routes to diagnosis, cancer stage and survival in the UK. BMC Cancer 2018, 18, 906. [Google Scholar] [CrossRef] [PubMed]
- Keum, N.; Giovannucci, E. Global burden of colorectal cancer: Emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 713–732. [Google Scholar] [CrossRef] [PubMed]
- Ye, P.; Xi, Y.; Huang, Z.; Xu, P. Linking obesity with colorectal cancer: Epidemiology and mechanistic insights. Cancers 2020, 12, 1408. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.R.; Chang, D.K. Colorectal cancer in inflammatory bowel disease: The risk, pathogenesis, prevention and diagnosis. World J. Gastroenterol. 2014, 20, 9872–9881. [Google Scholar] [CrossRef]
- Dekker, E.; Tanis, P.J.; Vleugels, J.L.A.; Kasi, P.M.; Wallace, M.B. Colorectal cancer. Lancet 2019, 394, 1467–1480. [Google Scholar] [CrossRef]
- Kim, S.E.; Paik, H.Y.; Yoon, H.; Lee, J.E.; Kim, N.; Sung, M.K. Sex- and gender-specific disparities in colorectal cancer risk. World J. Gastroenterol. 2015, 21, 5167–5175. [Google Scholar] [CrossRef]
- Carr, P.R.; Alwers, E.; Bienert, S.; Weberpals, J.; Kloor, M.; Brenner, H.; Hoffmeister, M. Lifestyle factors and risk of sporadic colorectal cancer by microsatellite instability status: A systematic review and meta-analyses. Ann. Oncol. 2018, 29, 825–834. [Google Scholar] [CrossRef]
- Tomkovich, S.; Yang, Y.; Winglee, K.; Gauthier, J.; Mühlbauer, M.; Sun, X.; Mohamadzadeh, M.; Liu, X.; Martin, P.; Wang, G.P.; et al. Locoregional effects of microbiota in a preclinical model of colon carcinogenesis. Cancer Res. 2017, 77, 2620–2632. [Google Scholar] [CrossRef]
- Rajamäki, K.; Taira, A.; Katainen, R.; Välimäki, N.; Kuosmanen, A.; Plaketti, R.M.; Seppälä, T.T.; Ahtiainen, M.; Wirta, E.V.; Vartiainen, E.; et al. Genetic and epigenetic characteristics of inflammatory bowel disease-associated colorectal cancer. Gastroenterology 2021, 161, 592–607. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Swartjes, H.; Brouwer, N.P.M.; de Nes, L.C.F.; van Erning, F.N.; Verhoeven, R.H.A.; Vissers, P.A.J.; de Wilt, J.H.W. Incidence, treatment and relative survival of early-onset colorectal cancer in the Netherlands since 1989. Eur. J. Cancer 2022, 166, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Araghi, M.; Soerjomataram, I.; Bardot, A.; Ferlay, J.; Cabasag, C.J.; Morrison, D.S.; De, P.; Tervonen, H.; Walsh, P.M.; Bucher, O.; et al. Changes in colorectal cancer incidence in seven high-income countries: A population-based study. Lancet Gastroenterol. Hepatol. 2019, 4, 511–518. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Huang, J.; Lok, V.; Wang, J.; Fung, F.; Ding, H.; Zheng, Z.J. Differences in incidence and mortality trends of colorectal cancer worldwide based on sex, age, and anatomic location. Clin. Gastroenterol. Hepatol. 2021, 19, 955–966.e61. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Torre, L.A.; Soerjomataram, I.; Hayes, R.B.; Bray, F.; Weber, T.K.; Jemal, A. Global patterns and trends in colorectal cancer incidence in young adults. Gut 2019, 68, 2179–2185. [Google Scholar] [CrossRef]
- Purim, O.; Gordon, N.; Brenner, B. Cancer of the colon and rectum: Potential effects of sex-age interactions on incidence and outcome. Med. Sci. Monit. 2013, 19, 203–209. [Google Scholar] [PubMed]
- Brenner, H.; Hoffmeister, M.; Arndt, V.; Haug, U. Gender differences in colorectal cancer: Implications for age at initiation of screening. Br. J. Cancer 2007, 96, 828–831. [Google Scholar] [CrossRef] [PubMed]
- Caiazza, F.; Ryan, E.J.; Doherty, G.; Winter, D.C.; Sheahan, K. Estrogen receptors and their implications in colorectal carcinogenesis. Front. Oncol. 2015, 5, 19. [Google Scholar] [CrossRef]
- Kim, H.I.; Lim, H.; Moon, A. Sex differences in cancer: Epidemiology, genetics and therapy. Biomol. Ther. 2018, 26, 335–342. [Google Scholar] [CrossRef]
- Özdemir, B.C.; Gerard, C.L.; da Silva, C.E. Sex and gender differences in anticancer treatment toxicity—A call for revisiting drug dosing in oncology. Endocrinology 2022, 163, bqac058. [Google Scholar] [CrossRef] [PubMed]
- Bishehsari, F.; Mahdavinia, M.; Vacca, M.; Malekzadeh, R.; Mariani-Costantini, R. Epidemiological transition of colorectal cancer in developing countries: Environmental factors, molecular pathways, and opportunities for prevention. World J. Gastroenterol. 2014, 20, 6055–6072. [Google Scholar] [CrossRef] [PubMed]
- Jochem, C.; Leitzmann, M. Obesity and colorectal cancer. Recent Results Cancer Res. 2016, 208, 17–41. [Google Scholar] [PubMed]
- Murphy, N.; Moreno, V.; Hughes, D.J.; Vodicka, L.; Vodicka, P.; Aglago, E.K.; Gunter, M.J.; Jenab, M. Lifestyle and dietary environmental factors in colorectal cancer susceptibility. Mol. Asp. Med. 2019, 69, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Marley, A.R.; Nan, H. Epidemiology of colorectal cancer. Int. J. Mol. Epidemiol. Genet. 2016, 7, 105–114. [Google Scholar]
- Conti, L.; Del Cornò, M.; Gessani, S. Revisiting the impact of lifestyle on colorectal cancer risk in a gender perspective. Crit. Rev. Oncol. Hematol. 2020, 145, 102834. [Google Scholar] [CrossRef]
- Yang, J.; McDowell, A.; Kim, E.K.; Seo, H.; Lee, W.H.; Moon, C.M.; Kym, S.M.; Lee, D.H.; Park, Y.S.; Jee, Y.K.; et al. Development of a colorectal cancer diagnostic model and dietary risk assessment through gut microbiome analysis. Exp. Mol. Med. 2019, 51, 1–15. [Google Scholar] [CrossRef]
- Liao, H.; Li, C.; Ai, Y.; Kou, Y. Gut microbiome is more stable in males than in females during the development of colorectal cancer. J. Appl. Microbiol. 2021, 131, 435–448. [Google Scholar] [CrossRef]
- Song, C.H.; Kim, N.; Nam, R.H.; Choi, S.I.; Lee, H.N.; Surh, Y.J. 17β-Estradiol supplementation changes gut microbiota diversity in intact and colorectal cancer-induced ICR male mice. Sci. Rep. 2020, 10, 12283. [Google Scholar] [CrossRef]
- Li, H.; Yang, G.; Xiang, Y.B.; Zhang, X.; Zheng, W.; Gao, Y.T.; Shu, X.O. Body weight, fat distribution and colorectal cancer risk: A report from cohort studies of 134255 Chinese men and women. Int. J. Obes. 2013, 37, 783–789. [Google Scholar] [CrossRef]
- Hases, L.; Archer, A.; Indukuri, R.; Birgersson, M.; Savva, C.; Korach-André, M.; Williams, C. High-fat diet and estrogen impacts the colon and its transcriptome in a sex-dependent manner. Sci. Rep. 2020, 10, 16160. [Google Scholar] [CrossRef] [PubMed]
- Weige, C.C.; Allred, K.F.; Allred, C.D. Estradiol alters cell growth in nonmalignant colonocytes and reduces the formation of preneoplastic lesions in the colon. Cancer Res. 2009, 69, 9118–9124. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, C.M.; Billimek, A.R.; Allred, K.F.; Sturino, J.M.; Weeks, B.R.; Allred, C.D. A novel shift in estrogen receptor expression occurs as estradiol suppresses inflammation-associated colon tumor formation. Endocr. Relat. Cancer 2013, 20, 515–525. [Google Scholar] [CrossRef]
- Offermans, N.S.M.; Ketcham, S.M.; van den Brandt, P.A.; Weijenberg, M.P.; Simons, C. Alcohol intake, ADH1B and ADH1C genotypes, and the risk of colorectal cancer by sex and subsite in the Netherlands Cohort Study. Carcinogenesis 2018, 39, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Dai, X.; Gakidou, E.; Lopez, A.D. Evolution of the global smoking epidemic over the past half century: Strengthening the evidence base for policy action. Tob. Control 2022, 31, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.W.; Kim, S.E.; Sung, M.K. Sex differences in the incidence of obesity-related gastrointestinal cancer. Int. J. Mol. Sci. 2021, 22, 1253. [Google Scholar] [CrossRef] [PubMed]
- Palmer, B.F.; Clegg, D.J. The sexual dimorphism of obesity. Mol. Cell. Endocrinol. 2015, 402, 113–119. [Google Scholar] [CrossRef]
- Chun, K.A.; Kocarnik, J.M.; Hardikar, S.S.; Robinson, J.R.; Berndt, S.I.; Chan, A.T.; Figueiredo, J.C.; Lindor, N.M.; Song, M.; Schoen, R.E.; et al. Leptin gene variants and colorectal cancer risk: Sex-specific associations. PLoS ONE 2018, 13, e0206519. [Google Scholar] [CrossRef]
- Izano, M.; Wei, E.K.; Tai, C.; Swede, H.; Gregorich, S.; Harris, T.B.; Klepin, H.; Satterfield, S.; Murphy, R.; Newman, A.B.; et al. Chronic inflammation and risk of colorectal and other obesity-related cancers: The health, aging and body composition study. Int. J. Cancer 2016, 138, 1118–1128. [Google Scholar] [CrossRef]
- Abancens, M.; Bustos, V.; Harvey, H.; McBryan, J.; Harvey, B.J. Sexual dimorphism in colon cancer. Front. Oncol. 2020, 10, 607909. [Google Scholar] [CrossRef]
- Harris, B.H.L.; Macaulay, V.M.; Harris, D.A.; Klenerman, P.; Karpe, F.; Lord, S.R.; Harris, A.L.; Buffa, F.M. Obesity: A perfect storm for carcinogenesis. Cancer Metastasis Rev. 2022, 41, 491–515. [Google Scholar] [CrossRef] [PubMed]
- Bergström, A.; Pisani, P.; Tenet, V.; Wolk, A.; Adami, H.O. Overweight as an avoidable cause of cancer in Europe. Int. J. Cancer 2001, 91, 421–430. [Google Scholar] [CrossRef]
- Nam, G.E.; Baek, S.J.; Choi, H.B.; Han, K.; Kwak, J.M.; Kim, J.; Kim, S.H. Association between abdominal obesity and incident colorectal cancer: A nationwide cohort study in Korea. Cancers 2020, 12, 1368. [Google Scholar] [CrossRef] [PubMed]
- Bailly, L.; Fabre, R.; Pradier, C.; Iannelli, A. Colorectal cancer risk following bariatric surgery in a nationwide study of French individuals with obesity. JAMA Surg. 2020, 155, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Ciccioriccio, M.C.; Iossa, A.; Boru, C.E.; De Angelis, F.; Termine, P.; Giuffrè, M.; Silecchia, G. Colorectal cancer after bariatric surgery (Cric-Abs 2020): Sicob (Italian society of obesity surgery) endorsed national survey. Int. J. Obes. 2021, 45, 2527–2531. [Google Scholar] [CrossRef] [PubMed]
- Aravani, A.; Downing, A.; Thomas, J.D.; Lagergren, J.; Morris, E.J.A.; Hull, M.A. Obesity surgery and risk of colorectal and other obesity-related cancers: An English population-based cohort study. Cancer Epidemiol. 2018, 53, 99–104. [Google Scholar] [CrossRef]
- Kwak, M.; Mehaffey, J.H.; Hawkins, R.B.; Hedrick, T.L.; Slingluff, C.L., Jr.; Schirmer, B.; Hallowell, P.T.; Friel, C.M. Bariatric surgery is independently associated with a decrease in the development of colorectal lesions. Surgery 2019, 166, 322–326. [Google Scholar] [CrossRef]
- Kedrin, D.; Gandhi, S.C.; Wolf, M.; Roper, J.; Yilmaz, O.; Corey, K.; Khalili, H.; Stanford, F.C.; Gala, M. Bariatric surgery prior to index screening colonoscopy is associated with a decreased rate of colorectal adenomas in obese individuals. Clin. Transl. Gastroenterol. 2017, 8, e73. [Google Scholar] [CrossRef]
- Karahalios, A.; English, D.R.; Simpson, J.A. Weight change and risk of colorectal cancer: A systematic review and meta-analysis. Am. J. Epidemiol. 2015, 181, 832–845. [Google Scholar] [CrossRef]
- Słomian, G.; Świętochowska, E.; Nowak, G.; Pawlas, K.; Żelazko, A.; Nowak, P. Chemotherapy and plasma adipokines level in patients with colorectal cancer. Postep. Hig. Med. Dosw. Online 2017, 71, 281–290. [Google Scholar] [CrossRef]
- Wang, D.; Chen, J.; Chen, H.; Duan, Z.; Xu, Q.; Wei, M.; Wang, L.; Zhong, M. Leptin regulates proliferation and apoptosis of colorectal carcinoma through PI3K/Akt/mTOR signalling pathway. J. Biosci. 2012, 37, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Socol, C.T.; Chira, A.; Martinez-Sanchez, M.A.; Nuñez-Sanchez, M.A.; Maerescu, C.M.; Mierlita, D.; Rusu, A.V.; Ruiz-Alcaraz, A.J.; Trif, M.; Ramos-Molina, B. Leptin signaling in obesity and colorectal cancer. Int. J. Mol. Sci. 2022, 23, 4713. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, T.; Farahani, H.; Nobakht, H.; Dabiri, R.; Zali, M.R. Genetic variations in leptin and leptin receptor and susceptibility to colorectal cancer and obesity. Iran. J. Cancer Prev. 2016, 9, e7013. [Google Scholar] [CrossRef] [PubMed]
- Stattin, P.; Palmqvist, R.; Söderberg, S.; Biessy, C.; Ardnor, B.; Hallmans, G.; Kaaks, R.; Olsson, T. Plasma leptin and colorectal cancer risk: A prospective study in Northern Sweden. Oncol. Rep. 2003, 10, 2015–2021. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, J.; Fu, X.; Li, J.; Liu, L.; Alkohlani, A.; Tan, S.C.; Low, T.Y.; Hou, Y. Association of circulating leptin and adiponectin levels with colorectal cancer risk: A systematic review and meta-analysis of case-control studies. Cancer Epidemiol. 2021, 73, 101958. [Google Scholar] [CrossRef]
- Gialamas, S.P.; Sergentanis, T.N.; Antonopoulos, C.N.; Dessypris, N.; Chrousos, G.P.; Petridou, E.T. Circulating leptin levels and risk of colorectal cancer and adenoma: A case–control study and meta-analysis. Cancer Causes Control 2013, 24, 2129–2141. [Google Scholar] [CrossRef]
- Bai, Y.; Sun, Q. Macrophage recruitment in obese adipose tissue. Obes. Rev. 2015, 16, 127–136. [Google Scholar] [CrossRef]
- Song, M.; Wu, K.; Ogino, S.; Fuchs, C.S.; Giovannucci, E.L.; Chan, A.T. A prospective study of plasma inflammatory markers and risk of colorectal cancer in men. Br. J. Cancer 2013, 108, 1891–1898. [Google Scholar] [CrossRef]
- Huang, Y.; Hua, X.; Labadie, J.D.; Harrison, T.A.; Dai, J.Y.; Lindstrom, S.; Lin, Y.; Berndt, S.I.; Buchanan, D.D.; Campbell, P.T.; et al. Genetic variants associated with circulating C-reactive protein levels and colorectal cancer survival: Sex-specific and lifestyle factors specific associations. Int. J. Cancer 2022, 150, 1447–1454. [Google Scholar] [CrossRef]
- Lin, J.H.; Zhang, S.M.; Rexrode, K.M.; Manson, J.E.; Chan, A.T.; Wu, K.; Tworoger, S.S.; Hankinson, S.E.; Fuchs, C.; Gaziano, J.M.; et al. Association between sex hormones and colorectal cancer risk in men and women. Clin. Gastroenterol. Hepatol. 2013, 11, 419–424.e1. [Google Scholar] [CrossRef]
- Chen, J.; Iverson, D. Estrogen in obesity-associated colon cancer: Friend or foe? Protecting postmenopausal women but promoting late-stage colon cancer. Cancer Causes Control 2012, 23, 1767–1773. [Google Scholar] [CrossRef] [PubMed]
- Maingi, J.W.; Tang, S.; Liu, S.; Ngenya, W.; Bao, E. Targeting estrogen receptors in colorectal cancer. Mol. Biol. Rep. 2020, 47, 4087–4091. [Google Scholar] [CrossRef] [PubMed]
- Barzi, A.; Lenz, A.M.; Labonte, M.J.; Lenz, H.J. Molecular pathways: Estrogen pathway in colorectal cancer. Clin. Cancer Res. 2013, 19, 5842–5848. [Google Scholar] [CrossRef]
- Ji, J.; Sundquist, J.; Sundquist, K. Use of hormone replacement therapy improves the prognosis in patients with colorectal cancer: A population-based study in Sweden. Int. J. Cancer 2018, 142, 2003–2010. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Chlebowski, R.T.; Stefanick, M.L.; Aragaki, A.K.; Rossouw, J.E.; Prentice, R.L.; Anderson, G.; Howard, B.V.; Thomson, C.A.; LaCroix, A.Z.; et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA 2013, 310, 1353–1368. [Google Scholar] [CrossRef]
- Weyant, M.J.; Carothers, A.M.; Mahmoud, N.N.; Bradlow, H.L.; Remotti, H.; Bilinski, R.T.; Bertagnolli, M.M. Reciprocal expression of ERalpha and ERbeta is associated with estrogen-mediated modulation of intestinal tumorigenesis. Cancer Res. 2001, 61, 2547–2551. [Google Scholar]
- Roshan, M.H.K.; Tambo, A.; Pace, N.P. The role of testosterone in colorectal carcinoma: Pathomechanisms and open questions. EPMA J. 2016, 7, 22. [Google Scholar] [CrossRef]
- Amos-Landgraf, J.M.; Heijmans, J.; Wielenga, M.C.B.; Dunkin, E.; Krentz, K.J.; Clipson, L.; Ederveen, A.G.; Groothuis, P.G.; Mosselman, S.; Muncan, V.; et al. Sex disparity in colonic adenomagenesis involves promotion by male hormones, not protection by female hormones. Proc. Natl. Acad. Sci. USA 2014, 111, 16514–16519. [Google Scholar] [CrossRef]
- Kim, H.; Giovannucci, E.L. Sex differences in the association of obesity and colorectal cancer risk. Cancer Causes Control 2017, 28, 1–4. [Google Scholar] [CrossRef]
- Yang, W.; Giovannucci, E.L.; Hankinson, S.E.; Chan, A.T.; Ma, Y.; Wu, K.; Fuchs, C.S.; Lee, I.M.; Sesso, H.D.; Lin, J.H.; et al. Endogenous sex hormones and colorectal cancer survival among men and women. Int. J. Cancer 2020, 147, 920–930. [Google Scholar] [CrossRef]
- Erol, A.; Karpyak, V.M. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug Alcohol Depend. 2015, 156, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrova, K.; Nimptsch, K.; Pischon, T. Obesity and colorectal cancer. Front. Biosci. Elite Ed. 2013, 5, 61–77. [Google Scholar] [CrossRef] [PubMed]
- Ma, R.C.; Chan, J.C. Type 2 diabetes in East Asians: Similarities and differences with populations in Europe and the United States. Ann. N. Y. Acad. Sci. 2013, 1281, 64–91. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrova, K.; Nimptsch, K.; Pischon, T. Influence of obesity and related metabolic alterations on colorectal cancer risk. Curr. Nutr. Rep. 2013, 2, 1–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chiu, C.C.; Ho, C.H.; Hung, C.M.; Chao, C.M.; Lai, C.C.; Chen, C.M.; Liao, K.M.; Wang, J.J.; Wu, Y.C.; Shi, H.Y.; et al. Correlation of body mass index with oncologic outcomes in colorectal cancer patients: A large population-based study. Cancers 2021, 13, 3592. [Google Scholar] [CrossRef] [PubMed]
- Bouras, E.; Papandreou, C.; Tzoulaki, I.; Tsilidis, K.K. Endogenous sex steroid hormones and colorectal cancer risk: A systematic review and meta-analysis. Discov. Oncol. 2021, 12, 8. [Google Scholar] [CrossRef]
- Song, C.H.; Kim, N.; Lee, S.M.; Nam, R.H.; Choi, S.I.; Kang, S.R.; Shin, E.; Lee, D.H.; Lee, H.N.; Surh, Y.J. Effects of 17β-estradiol on colorectal cancer development after azoxymethane/dextran sulfate sodium treatment of ovariectomized mice. Biochem. Pharmacol. 2019, 164, 139–151. [Google Scholar] [CrossRef]
| Factors of Differences in CRC | Male | Female |
|---|---|---|
| Incidence rate | High throughout life [28] | High at ≥65 years [19] |
| Mortality | More [18] | Less [18] |
| Willingness for screening tests | Less [14] | More [14] |
| CRC diagnosis stage | Stage I [14] | Stage II [14] |
| Survival advantage | High risk throughout life [28] | Low risk until 64 years for colon cancer and 74 years for rectal cancer [28] |
| Site of CRC | Distal colon [30] | Proximal colon [30] |
| Metastatic CRC | More likely to develop metastatic colon cancer [28] | More likely to develop metastatic rectal cancer [28] |
| Toxicity of commonly used anti-cancer drugs | Lower [31] | Higher [31] |
| Fiber intake | Lower [37] | Higher [37] |
| Sedentary lifestyle | Lower [37] | Higher [37] |
| Meat intake | Higher [14] | Lower [14] |
| Alcohol intake | Higher [14] | Lower [14] |
| Amount of alcohol consumption increases CRC risk | 0.1–29 g/day [45] | >30 g/day [45] |
| Prevalence of smoking | Higher [46] | Lower [46] |
| Prevalence of obesity | Lower [47] | Higher [47] |
| Obesity-induced CRC risk | Higher [42] | Lower [42] |
| Fat distribution | Abdominal region [48] | Thighs, hips, and buttocks [48] |
| Fat deposition | Visceral adipose tissue [47] | Subcutaneous adipose tissue [47] |
| Leptin SNPs LEP rs2167270 and LEP rs4731426 | No effect [49] | Increases risk, independent of obesity, only in females [49] |
| Adiponectin SNP ADIPOQ rs17366743 | Increases risk of obesity in males and thus CRC risk [49] | No effect [49] |
| Risk of CRC when CRP-1 levels are elevated | Higher [50] | Lower [50] |
| Gene variants of alcohol dehydrogenase (ADH) enzyme increase cancer risk | ADH1B rs4147536 SNP increases the risk of distal colon cancer [45] | ADH1C rs283415 SNP increases the risk of proximal colon cancer [45] |
| Microbial community in the gut | More stable [39] | Less stable [39] |
| Mutations/epigenetics | Mutations in APC and TP53 [51] | Hypermethylation, MSI, and CIMP, and mutations in BRAF and KRAS [14] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wele, P.; Wu, X.; Shi, H. Sex-Dependent Differences in Colorectal Cancer: With a Focus on Obesity. Cells 2022, 11, 3688. https://doi.org/10.3390/cells11223688
Wele P, Wu X, Shi H. Sex-Dependent Differences in Colorectal Cancer: With a Focus on Obesity. Cells. 2022; 11(22):3688. https://doi.org/10.3390/cells11223688
Chicago/Turabian StyleWele, Prachi, Xian Wu, and Haifei Shi. 2022. "Sex-Dependent Differences in Colorectal Cancer: With a Focus on Obesity" Cells 11, no. 22: 3688. https://doi.org/10.3390/cells11223688
APA StyleWele, P., Wu, X., & Shi, H. (2022). Sex-Dependent Differences in Colorectal Cancer: With a Focus on Obesity. Cells, 11(22), 3688. https://doi.org/10.3390/cells11223688








