Cellular-Based Therapies in Systemic Sclerosis: From Hematopoietic Stem Cell Transplant to Innovative Approaches
Abstract
1. Introduction
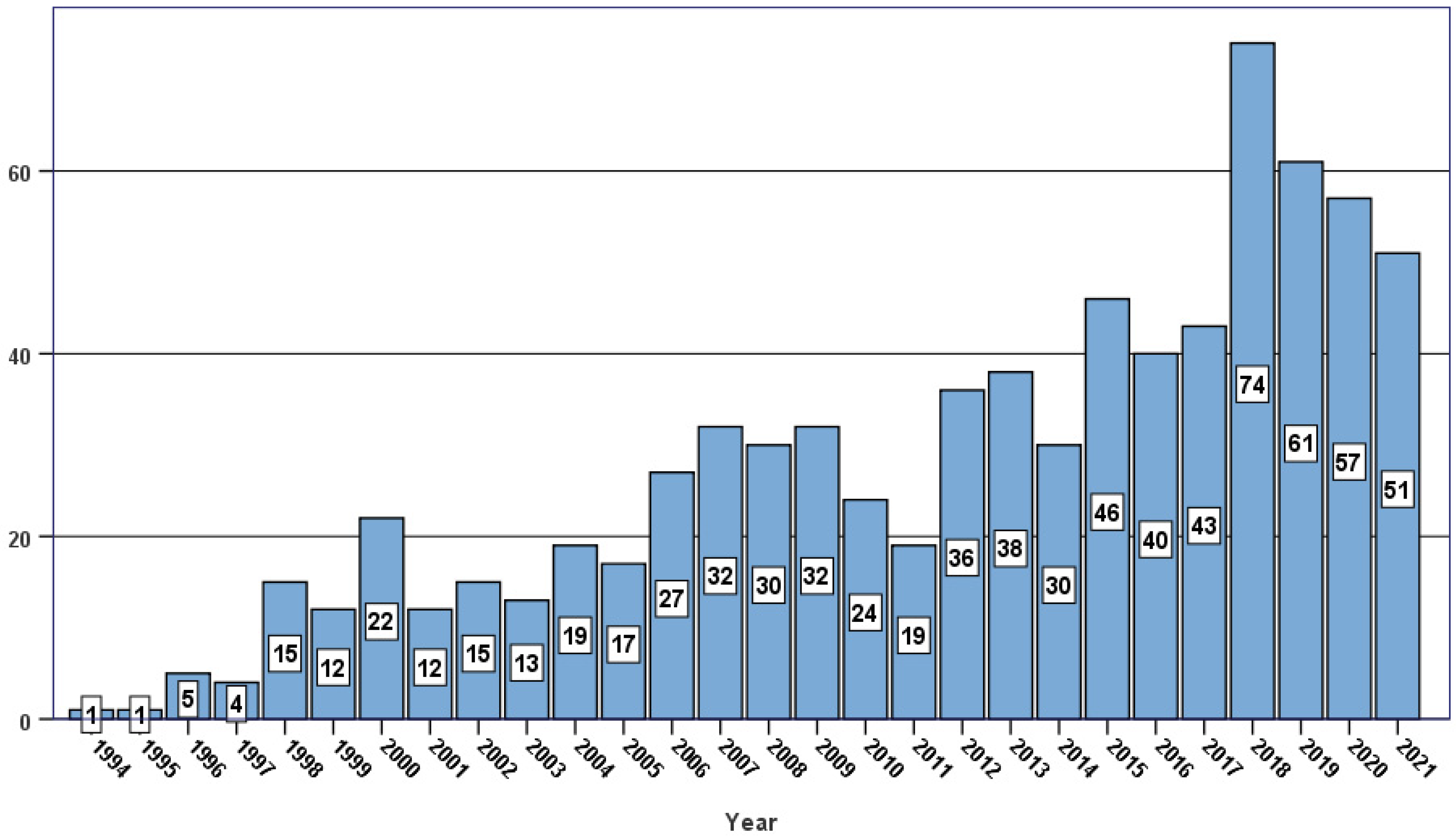
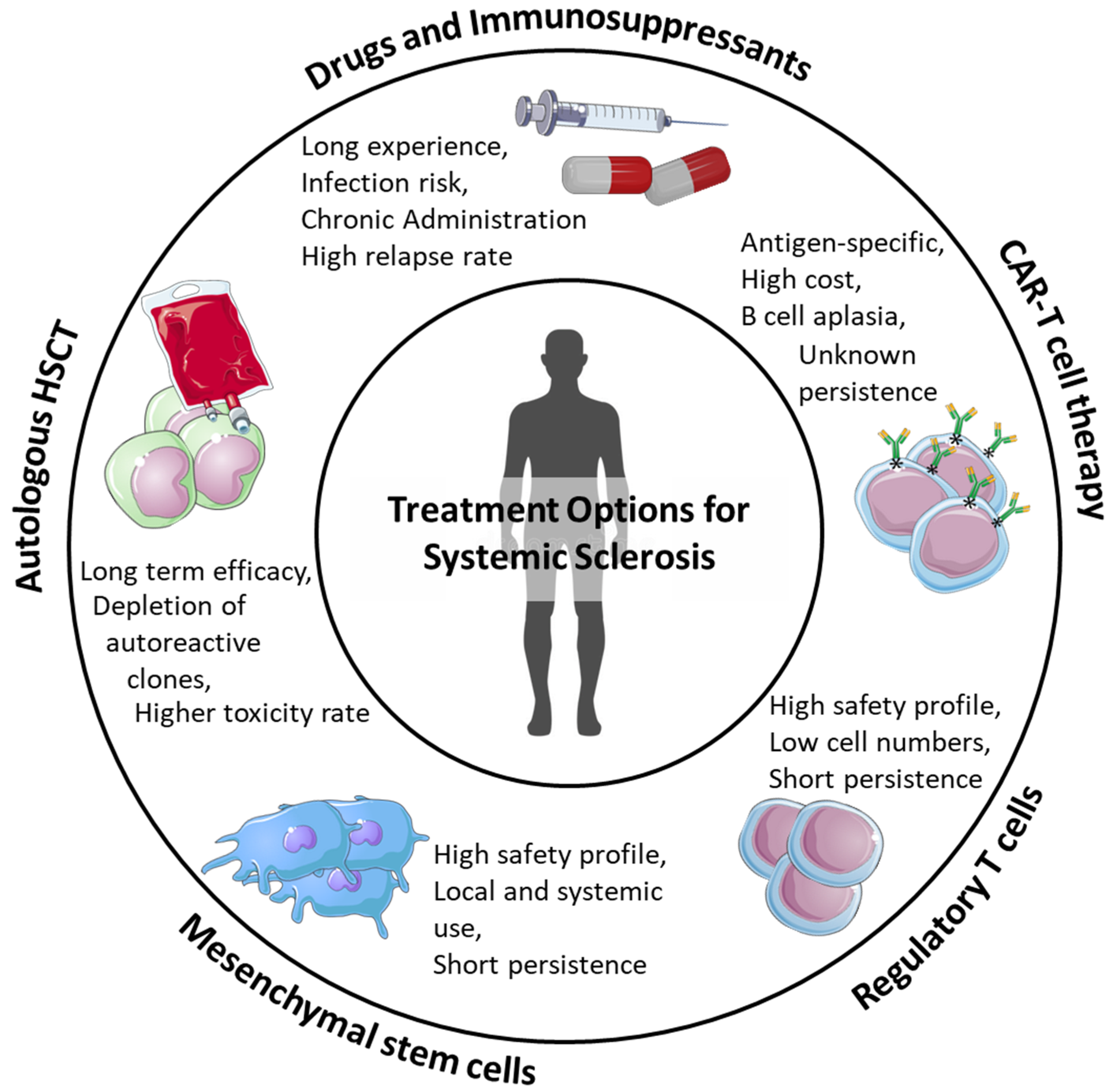
2. Hematopoietic Stem Cell Transplantation
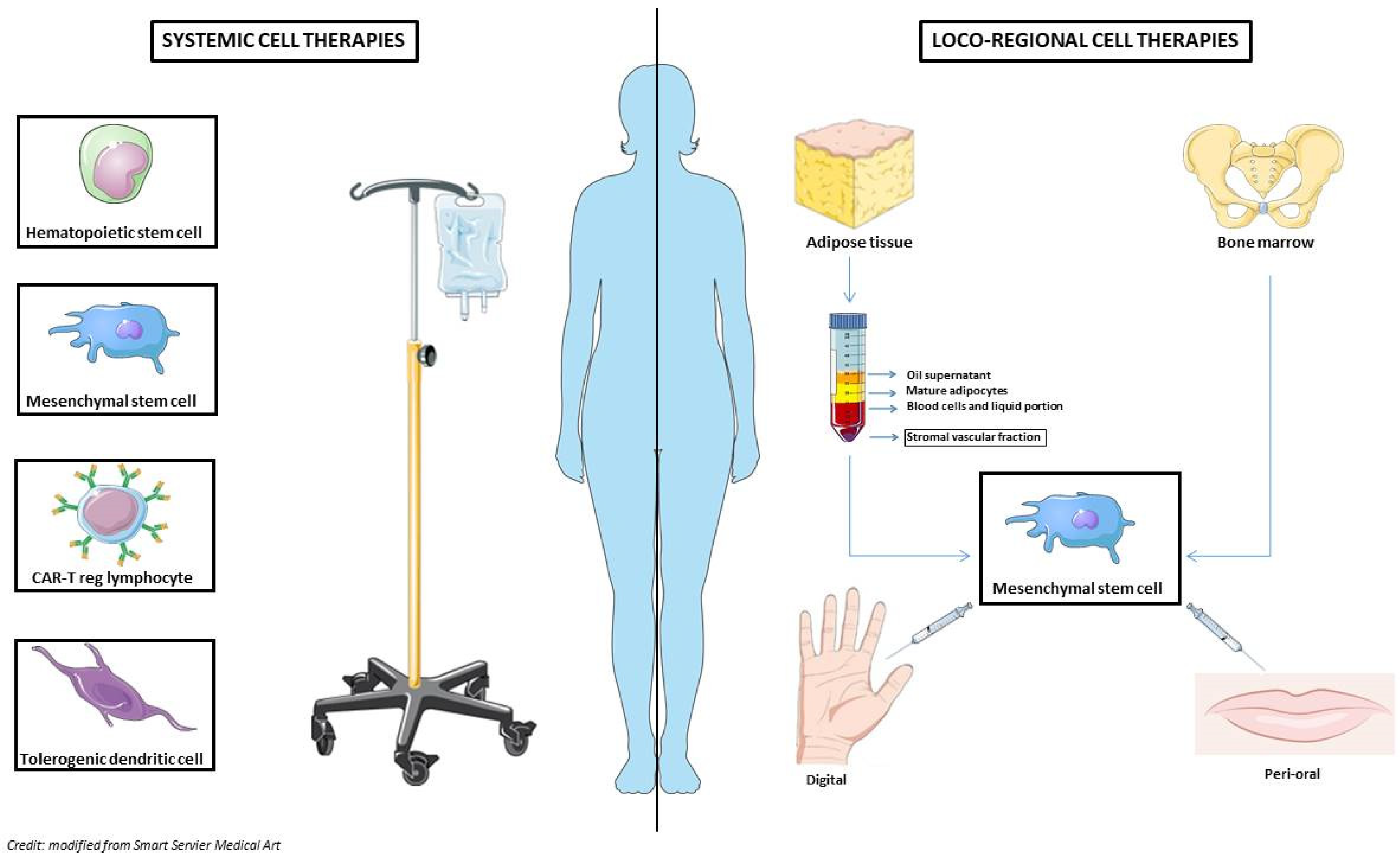
3. Adoptive Cellular Therapies
4. Mesenchymal Stem Cells (MSC)
4.1. Intravenous MSCs Use
4.2. Loco-Regional MSCs Use
5. Regulatory T Cells and Chimeric Antigen Receptor T Cells
6. Tolerogenic Dendritic Cells
7. Open Questions and Future Perspectives
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethics Statement
Additional Information
References
- Gabrielli, A.; Avvedimento, E.V.; Krieg, T. Scleroderma. N. Engl. J. Med. 2009, 360, 1989–2003. [Google Scholar] [CrossRef] [PubMed]
- Desbois, A.C.; Cacoub, P. Systemic sclerosis: An update in 2016. Autoimmun. Rev. 2016, 15, 417–426. [Google Scholar] [CrossRef]
- Elhai, M.; Meune, C.; Boubaya, M.; Avouac, J.; Hachulla, E.; Balbir-Gurman, A.; Riemekasten, G.; Airò, P.; Joven, B.; Vettori, S.; et al. Mapping and predicting mortality from systemic sclerosis. Ann. Rheum. Dis. 2017, 76, 1897–1905. [Google Scholar] [CrossRef] [PubMed]
- Poudel, D.R.; Jayakumar, D.; Danve, A.; Sehra, S.T.; Derk, C.T. Determinants of mortality in systemic sclerosis: A focused review. Rheumatol. Int. 2018, 38, 1847–1858. [Google Scholar] [CrossRef] [PubMed]
- Murdaca, G.; Contatore, M.; Gulli, R.; Mandich, P.; Puppo, F. Genetic factors and systemic sclerosis. Autoimmun. Rev. 2016, 15, 427–432. [Google Scholar] [CrossRef]
- De Martinis, M.; Ciccarelli, F.; Sirufo, M.M.; Ginaldi, L. An overview of environmental risk factors in systemic sclerosis. Expert Rev. Clin. Immunol. 2016, 12, 465–478. [Google Scholar] [CrossRef]
- Marie, I.; Gehanno, J.F. Environmental risk factors of systemic sclerosis. Semin. Immunopathol. 2015, 37, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Benfaremo, D.; Svegliati, S.; Paolini, C.; Agarbati, S.; Moroncini, G. Systemic Sclerosis: From Pathophysiology to Novel Therapeutic Approaches. Biomedicines 2022, 10, 163. [Google Scholar] [CrossRef] [PubMed]
- Denton, C.P.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef]
- Mosanya, C.H.; Isaacs, J.D. Tolerising cellular therapies: What is their promise for autoimmune disease? Ann. Rheum. Dis. 2019, 78, 297–310. [Google Scholar] [CrossRef]
- Snowden, J.A.; Sánchez-Ortega, I.; Corbacioglu, S.; Basak, G.W.; Chabannon, C.; de la Camara, R.; Dolstra, H.; Duarte, R.F.; Glass, B.; Greco, R.; et al. Indications for haematopoietic cell transplantation for haematological diseases, solid tumours and immune disorders: Current practice in Europe, 2022. Bone Marrow Transplant. 2022, 57, 1217–1239. [Google Scholar] [CrossRef]
- Alexander, T.; Greco, R. Hematopoietic stem cell transplantation and cellular therapies for autoimmune diseases: Overview and future considerations from the Autoimmune Diseases Working Party (ADWP) of the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant. 2022, 57, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, K.M.; Goldmuntz, E.A.; Furst, D.E. Autologous Stem-Cell Transplantation for Severe Scleroderma. N. Engl. J. Med. 2018, 378, 1066–1067. [Google Scholar] [CrossRef]
- Sullivan, K.M.; Goldmuntz, E.A.; Keyes-Elstein, L.; McSweeney, P.A.; Pinckney, A.; Welch, B.; Mayes, M.D.; Nash, R.A.; Crofford, L.J.; Eggleston, B.; et al. Myeloablative Autologous Stem-Cell Transplantation for Severe Scleroderma. N. Engl. J. Med. 2018, 378, 35–47. [Google Scholar] [CrossRef]
- Burt, R.K.; Shah, S.J.; Dill, K.; Grant, T.; Gheorghiade, M.; Schroeder, J.; Craig, R.; Hirano, I.; Marshall, K.; Ruderman, E.; et al. Autologous non-myeloablative haemopoietic stem-cell transplantation compared with pulse cyclophosphamide once per month for systemic sclerosis (ASSIST): An open-label, randomised phase 2 trial. Lancet 2011, 378, 498–506. [Google Scholar] [CrossRef]
- van Laar, J.M.; Farge, D.; Sont, J.K.; Naraghi, K.; Marjanovic, Z.; Larghero, J.; Schuerwegh, A.J.; Marijt, E.W.; Vonk, M.C.; Schattenberg, A.V.; et al. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: A randomized clinical trial. JAMA 2014, 311, 2490–2498. [Google Scholar] [CrossRef]
- Burt, R.K.; Han, X.; Quigley, K.; Arnautovic, I.; Shah, S.J.; Lee, D.C.; Freed, B.H.; Jovanovic, B.; Helenowski, I.B. Cardiac safe hematopoietic stem cell transplantation for systemic sclerosis with poor cardiac function: A pilot safety study that decreases neutropenic interval to 5 days. Bone Marrow Transplant. 2021, 56, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Alexander, T.; Greco, R.; Snowden, J.A. Hematopoietic Stem Cell Transplantation for Autoimmune Disease. Annu. Rev. Med. 2021, 72, 215–228. [Google Scholar] [CrossRef]
- Cencioni, M.T.; Genchi, A.; Brittain, G.; de Silva, T.I.; Sharrack, B.; Snowden, J.A.; Alexander, T.; Greco, R.; Muraro, P.A. Immune Reconstitution Following Autologous Hematopoietic Stem Cell Transplantation for Multiple Sclerosis: A Review on Behalf of the EBMT Autoimmune Diseases Working Party. Front. Immunol. 2021, 12, 813957. [Google Scholar] [CrossRef]
- Bohgaki, T.; Atsumi, T.; Bohgaki, M.; Furusaki, A.; Kondo, M.; Sato-Matsumura, K.C.; Abe, R.; Kataoka, H.; Horita, T.; Yasuda, S.; et al. Immunological reconstitution after autologous hematopoietic stem cell transplantation in patients with systemic sclerosis: Relationship between clinical benefits and intensity of immunosuppression. J. Rheumatol. 2009, 36, 1240–1248. [Google Scholar] [CrossRef]
- Arruda, L.C.M.; Malmegrim, K.C.R.; Lima-Júnior, J.R.; Clave, E.; Dias, J.B.E.; Moraes, D.A.; Douay, C.; Fournier, I.; Moins-Teisserenc, H.; Alberdi, A.J.; et al. Immune rebound associates with a favorable clinical response to autologous HSCT in systemic sclerosis patients. Blood Adv. 2018, 2, 126–141. [Google Scholar] [CrossRef]
- Roord, S.T.; de Jager, W.; Boon, L.; Wulffraat, N.; Martens, A.; Prakken, B.; van Wijk, F. Autologous bone marrow transplantation in autoimmune arthritis restores immune homeostasis through CD4+CD25+Foxp3+ regulatory T cells. Blood 2008, 111, 5233–5241. [Google Scholar] [CrossRef][Green Version]
- Hendrawan, K.; Visweswaran, M.; Ma, D.D.F.; Moore, J.J. Tolerance regeneration by T regulatory cells in autologous haematopoietic stem cell transplantation for autoimmune diseases. Bone Marrow Transplant. 2020, 55, 857–866. [Google Scholar] [CrossRef]
- Burt, R.K.; Traynor, A.E.; Pope, R.; Schroeder, J.; Cohen, B.; Karlin, K.H.; Lobeck, L.; Goolsby, C.; Rowlings, P.; Davis, F.A.; et al. Treatment of autoimmune disease by intense immunosuppressive conditioning and autologous hematopoietic stem cell transplantation. Blood 1998, 92, 3505–3514. [Google Scholar] [CrossRef]
- Binks, M.; Passweg, J.R.; Furst, D.; McSweeney, P.; Sullivan, K.; Besenthal, C.; Finke, J.; Peter, H.H.; van Laar, J.; Breedveld, F.C.; et al. Phase I/II trial of autologous stem cell transplantation in systemic sclerosis: Procedure related mortality and impact on skin disease. Ann. Rheum. Dis. 2001, 60, 577–584. [Google Scholar] [CrossRef]
- Farge, D.; Marolleau, J.P.; Zohar, S.; Marjanovic, Z.; Cabane, J.; Mounier, N.; Hachulla, E.; Philippe, P.; Sibilia, J.; Rabian, C.; et al. Autologous bone marrow transplantation in the treatment of refractory systemic sclerosis: Early results from a French multicentre phase I-II study. Br. J. Haematol. 2002, 119, 726–739. [Google Scholar] [CrossRef]
- Assassi, S.; Wang, X.; Chen, G.; Goldmuntz, E.; Keyes-Elstein, L.; Ying, J.; Wallace, P.K.; Turner, J.; Zheng, W.J.; Pascual, V.; et al. Myeloablation followed by autologous stem cell transplantation normalises systemic sclerosis molecular signatures. Ann. Rheum. Dis. 2019, 78, 1371–1378. [Google Scholar] [CrossRef]
- Burt, R.K.; Oliveira, M.C.; Shah, S.J.; Moraes, D.A.; Simoes, B.; Gheorghiade, M.; Schroeder, J.; Ruderman, E.; Farge, D.; Chai, Z.J.; et al. Cardiac involvement and treatment-related mortality after non-myeloablative haemopoietic stem-cell transplantation with unselected autologous peripheral blood for patients with systemic sclerosis: A retrospective analysis. Lancet 2013, 381, 1116–1124. [Google Scholar] [CrossRef]
- Farge, D.; Burt, R.K.; Oliveira, M.C.; Mousseaux, E.; Rovira, M.; Marjanovic, Z.; de Vries-Bouwstra, J.; Del Papa, N.; Saccardi, R.; Shah, S.J.; et al. Cardiopulmonary assessment of patients with systemic sclerosis for hematopoietic stem cell transplantation: Recommendations from the European Society for Blood and Marrow Transplantation Autoimmune Diseases Working Party and collaborating partners. Bone Marrow Transplant. 2017, 52, 1495–1503. [Google Scholar] [CrossRef]
- Henes, J.; Oliveira, M.C.; Labopin, M.; Badoglio, M.; Scherer, H.U.; Del Papa, N.; Daikeler, T.; Schmalzing, M.; Schroers, R.; Martin, T.; et al. Autologous stem cell transplantation for progressive systemic sclerosis: A prospective non-interventional study from the European Society for Blood and Marrow Transplantation Autoimmune Disease Working Party. Haematologica 2021, 106, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Ayano, M.; Tsukamoto, H.; Mitoma, H.; Kimoto, Y.; Akahoshi, M.; Arinobu, Y.; Miyamoto, T.; Horiuchi, T.; Niiro, H.; Nagafuji, K.; et al. CD34-selected versus unmanipulated autologous haematopoietic stem cell transplantation in the treatment of severe systemic sclerosis: A post hoc analysis of a phase I/II clinical trial conducted in Japan. Arthritis Res. Ther. 2019, 21, 30. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.C.; Labopin, M.; Henes, J.; Moore, J.; Del Papa, N.; Cras, A.; Sakellari, I.; Schroers, R.; Scherer, H.U.; Cuneo, A.; et al. Does ex vivo CD34+ positive selection influence outcome after autologous hematopoietic stem cell transplantation in systemic sclerosis patients? Bone Marrow Transplant. 2016, 51, 501–505. [Google Scholar] [CrossRef]
- Greco, R.; Alexander, T.; Burman, J.; Del Papa, N.; de Vries-Bouwstra, J.; Farge, D.; Henes, J.; Kazmi, M.; Kirgizov, K.; Muraro, P.A.; et al. Hematopoietic stem cell transplantation for autoimmune diseases in the time of COVID-19: EBMT guidelines and recommendations. Bone Marrow Transplant. 2021, 56, 1493–1508. [Google Scholar] [CrossRef]
- Shiratsuchi, M.; Motomura, S.; Abe, Y.; Shiokawa, S.; Nishimura, J. Long-term follow-up after nonmyeloablative allogeneic hematopoietic stem cell transplantation for systemic sclerosis. Clin. Rheumatol. 2008, 27, 1207–1209. [Google Scholar] [CrossRef]
- Khorshid, O.; Hosing, C.; Bibawi, S.; Ueno, N.; Reveille, J.; Mayes, M.D.; Champlin, R.E. Nonmyeloablative stem cell transplant in a patient with advanced systemic sclerosis and systemic lupus erythematosus. J. Rheumatol. 2004, 31, 2513–2516. [Google Scholar]
- Nash, R.A.; McSweeney, P.A.; Nelson, J.L.; Wener, M.; Georges, G.E.; Langston, A.A.; Shulman, H.; Sullivan, K.M.; Lee, J.; Henstorf, G.; et al. Allogeneic marrow transplantation in patients with severe systemic sclerosis: Resolution of dermal fibrosis. Arthritis Rheum. 2006, 54, 1982–1986. [Google Scholar] [CrossRef]
- Loh, Y.; Oyama, Y.; Statkute, L.; Verda, L.; Quigley, K.; Yaung, K.; Barr, W.; Jovanovic, B.; Burt, R.K. Non-myeloablative allogeneic hematopoietic stem cell transplantation for severe systemic sclerosis: Graft-versus-autoimmunity without graft-versus-host disease? Bone Marrow Transplant. 2007, 39, 435–437. [Google Scholar] [CrossRef]
- Greco, R.; Labopin, M.; Badoglio, M.; Veys, P.; Furtado Silva, J.M.; Abinun, M.; Gualandi, F.; Bornhauser, M.; Ciceri, F.; Saccardi, R.; et al. Allogeneic HSCT for Autoimmune Diseases: A Retrospective Study from the EBMT ADWP, IEWP, and PDWP Working Parties. Front. Immunol. 2019, 10, 1570. [Google Scholar] [CrossRef]
- Farge, D.; Loisel, S.; Lansiaux, P.; Tarte, K. Mesenchymal stromal cells for systemic sclerosis treatment. Autoimmun. Rev. 2021, 20, 102755. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Wang, M.; Xu, X.; Lei, X.; Tan, J.; Xie, H. Mesenchymal stem cell-based therapy for burn wound healing. Burn. Trauma 2021, 9, tkab002. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Guo, F.; Pan, Q.; Chen, S.; Chen, J.; Liu, H.F. Mesenchymal Stem Cell Therapy: Hope for Patients with Systemic Lupus Erythematosus. Front. Immunol. 2021, 12, 728190. [Google Scholar] [CrossRef]
- Lan, T.; Luo, M.; Wei, X. Mesenchymal stem/stromal cells in cancer therapy. J. Hematol. Oncol. 2021, 14, 195. [Google Scholar] [CrossRef] [PubMed]
- Izadi, M.; Sadr Hashemi Nejad, A.; Moazenchi, M.; Masoumi, S.; Rabbani, A.; Kompani, F.; Hedayati Asl, A.A.; Abbasi Kakroodi, F.; Jaroughi, N.; Mohseni Meybodi, M.A.; et al. Mesenchymal stem cell transplantation in newly diagnosed type-1 diabetes patients: A phase I/II randomized placebo-controlled clinical trial. Stem Cell Res. Ther. 2022, 13, 264. [Google Scholar] [CrossRef]
- Niess, H.; von Einem, J.C.; Thomas, M.N.; Michl, M.; Angele, M.K.; Huss, R.; Günther, C.; Nelson, P.J.; Bruns, C.J.; Heinemann, V. Treatment of advanced gastrointestinal tumors with genetically modified autologous mesenchymal stromal cells (TREAT-ME1): Study protocol of a phase I/II clinical trial. BMC Cancer 2015, 15, 237. [Google Scholar] [CrossRef] [PubMed]
- Abouzaid, A.M.; El Mokadem, M.E.; Aboubakr, A.K.; Kassem, M.A.; Al Shora, A.K.; Solaiman, A. Effect of autologous fat transfer in acute burn wound management: A randomized controlled study. Burns 2022, 48, 1368–1385. [Google Scholar] [CrossRef]
- Ryan, J.M.; Barry, F.P.; Murphy, J.M.; Mahon, B.P. Mesenchymal stem cells avoid allogeneic rejection. J. Inflamm. 2005, 2, 8. [Google Scholar] [CrossRef]
- Caplan, H.; Olson, S.D.; Kumar, A.; George, M.; Prabhakara, K.S.; Wenzel, P.; Bedi, S.; Toledano-Furman, N.E.; Triolo, F.; Kamhieh-Milz, J.; et al. Mesenchymal Stromal Cell Therapeutic Delivery: Translational Challenges to Clinical Application. Front. Immunol. 2019, 10, 1645. [Google Scholar] [CrossRef]
- Khan, R.S.; Newsome, P.N. A Comparison of Phenotypic and Functional Properties of Mesenchymal Stromal Cells and Multipotent Adult Progenitor Cells. Front. Immunol. 2019, 10, 1952. [Google Scholar] [CrossRef]
- Eliopoulos, N.; Stagg, J.; Lejeune, L.; Pommey, S.; Galipeau, J. Allogeneic marrow stromal cells are immune rejected by MHC class I- and class II-mismatched recipient mice. Blood 2005, 106, 4057–4065. [Google Scholar] [CrossRef]
- Eggenhofer, E.; Benseler, V.; Kroemer, A.; Popp, F.C.; Geissler, E.K.; Schlitt, H.J.; Baan, C.C.; Dahlke, M.H.; Hoogduijn, M.J. Mesenchymal stem cells are short-lived and do not migrate beyond the lungs after intravenous infusion. Front. Immunol. 2012, 3, 297. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, E.M.; Gordon, P.L.; Koo, W.K.; Marx, J.C.; Neel, M.D.; McNall, R.Y.; Muul, L.; Hofmann, T. Isolated allogeneic bone marrow-derived mesenchymal cells engraft and stimulate growth in children with osteogenesis imperfecta: Implications for cell therapy of bone. Proc. Natl. Acad. Sci. USA 2002, 99, 8932–8937. [Google Scholar] [CrossRef]
- Maria, A.T.; Toupet, K.; Maumus, M.; Fonteneau, G.; Le Quellec, A.; Jorgensen, C.; Guilpain, P.; Noël, D. Human adipose mesenchymal stem cells as potent anti-fibrosis therapy for systemic sclerosis. J. Autoimmun. 2016, 70, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Gnecchi, M.; He, H.; Liang, O.D.; Melo, L.G.; Morello, F.; Mu, H.; Noiseux, N.; Zhang, L.; Pratt, R.E.; Ingwall, J.S.; et al. Paracrine action accounts for marked protection of ischemic heart by Akt-modified mesenchymal stem cells. Nat. Med. 2005, 11, 367–368. [Google Scholar] [CrossRef]
- Duan, X.; Lu, L.; Wang, Y.; Zhang, F.; Mao, J.; Cao, M.; Lin, B.; Zhang, X.; Shuai, X.; Shen, J. The long-term fate of mesenchymal stem cells labeled with magnetic resonance imaging-visible polymersomes in cerebral ischemia. Int. J. Nanomed. 2017, 12, 6705–6719. [Google Scholar] [CrossRef] [PubMed]
- Guiducci, S.; Manetti, M.; Romano, E.; Mazzanti, B.; Ceccarelli, C.; Dal Pozzo, S.; Milia, A.F.; Bellando-Randone, S.; Fiori, G.; Conforti, M.L.; et al. Bone marrow-derived mesenchymal stem cells from early diffuse systemic sclerosis exhibit a paracrine machinery and stimulate angiogenesis in vitro. Ann. Rheum. Dis. 2011, 70, 2011–2021. [Google Scholar] [CrossRef]
- Guiducci, S.; Porta, F.; Saccardi, R.; Guidi, S.; Ibba-Manneschi, L.; Manetti, M.; Mazzanti, B.; Dal Pozzo, S.; Milia, A.F.; Bellando-Randone, S.; et al. Autologous mesenchymal stem cells foster revascularization of ischemic limbs in systemic sclerosis: A case report. Ann. Intern. Med. 2010, 153, 650–654. [Google Scholar] [CrossRef]
- Del Papa, N.; Quirici, N.; Soligo, D.; Scavullo, C.; Cortiana, M.; Borsotti, C.; Maglione, W.; Comina, D.P.; Vitali, C.; Fraticelli, P.; et al. Bone marrow endothelial progenitors are defective in systemic sclerosis. Arthritis Rheum. 2006, 54, 2605–2615. [Google Scholar] [CrossRef]
- Maumus, M.; Jorgensen, C.; Noël, D. Mesenchymal stem cells in regenerative medicine applied to rheumatic diseases: Role of secretome and exosomes. Biochimie 2013, 95, 2229–2234. [Google Scholar] [CrossRef]
- Griffin, M.; Ryan, C.M.; Pathan, O.; Abraham, D.; Denton, C.P.; Butler, P.E. Characteristics of human adipose derived stem cells in scleroderma in comparison to sex and age matched normal controls: Implications for regenerative medicine. Stem Cell Res. Ther. 2017, 8, 23. [Google Scholar] [CrossRef]
- Kastrinaki, M.C.; Sidiropoulos, P.; Roche, S.; Ringe, J.; Lehmann, S.; Kritikos, H.; Vlahava, V.M.; Delorme, B.; Eliopoulos, G.D.; Jorgensen, C.; et al. Functional, molecular and proteomic characterisation of bone marrow mesenchymal stem cells in rheumatoid arthritis. Ann. Rheum. Dis. 2008, 67, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Larghero, J.; Farge, D.; Braccini, A.; Lecourt, S.; Scherberich, A.; Foïs, E.; Verrecchia, F.; Daikeler, T.; Gluckman, E.; Tyndall, A.; et al. Phenotypical and functional characteristics of in vitro expanded bone marrow mesenchymal stem cells from patients with systemic sclerosis. Ann. Rheum. Dis. 2008, 67, 443–449. [Google Scholar] [CrossRef]
- Capelli, C.; Zaccara, E.; Cipriani, P.; Di Benedetto, P.; Maglione, W.; Andracco, R.; Di Luca, G.; Pignataro, F.; Giacomelli, R.; Introna, M.; et al. Phenotypical and Functional Characteristics of In Vitro-Expanded Adipose-Derived Mesenchymal Stromal Cells from Patients with Systematic Sclerosis. Cell Transplant. 2017, 26, 841–854. [Google Scholar] [CrossRef]
- Vanneaux, V.; Farge-Bancel, D.; Lecourt, S.; Baraut, J.; Cras, A.; Jean-Louis, F.; Brun, C.; Verrecchia, F.; Larghero, J.; Michel, L. Expression of transforming growth factor β receptor II in mesenchymal stem cells from systemic sclerosis patients. BMJ Open 2013, 3, e001890. [Google Scholar] [CrossRef] [PubMed]
- Di Benedetto, P.; Panzera, N.; Cipriani, P.; Mastroiaco, V.; Tessitore, A.; Liakouli, V.; Ruscitti, P.; Berardicurti, O.; Carubbi, F.; Guggino, G.; et al. Mesenchymal stem cells of Systemic Sclerosis patients, derived from different sources, show a profibrotic microRNA profiling. Sci. Rep. 2019, 9, 7144. [Google Scholar] [CrossRef] [PubMed]
- Le Blanc, K.; Rasmusson, I.; Sundberg, B.; Götherström, C.; Hassan, M.; Uzunel, M.; Ringdén, O. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 2004, 363, 1439–1441. [Google Scholar] [CrossRef]
- Introna, M.; Lucchini, G.; Dander, E.; Galimberti, S.; Rovelli, A.; Balduzzi, A.; Longoni, D.; Pavan, F.; Masciocchi, F.; Algarotti, A.; et al. Treatment of graft versus host disease with mesenchymal stromal cells: A phase I study on 40 adult and pediatric patients. Biol. Blood Marrow Transplant. 2014, 20, 375–381. [Google Scholar] [CrossRef]
- Muroi, K.; Miyamura, K.; Ohashi, K.; Murata, M.; Eto, T.; Kobayashi, N.; Taniguchi, S.; Imamura, M.; Ando, K.; Kato, S.; et al. Unrelated allogeneic bone marrow-derived mesenchymal stem cells for steroid-refractory acute graft-versus-host disease: A phase I/II study. Int. J. Hematol. 2013, 98, 206–213. [Google Scholar] [CrossRef]
- von Bahr, L.; Sundberg, B.; Lönnies, L.; Sander, B.; Karbach, H.; Hägglund, H.; Ljungman, P.; Gustafsson, B.; Karlsson, H.; Le Blanc, K.; et al. Long-term complications, immunologic effects, and role of passage for outcome in mesenchymal stromal cell therapy. Biol. Blood Marrow Transplant. 2012, 18, 557–564. [Google Scholar] [CrossRef]
- Ning, H.; Yang, F.; Jiang, M.; Hu, L.; Feng, K.; Zhang, J.; Yu, Z.; Li, B.; Xu, C.; Li, Y.; et al. The correlation between cotransplantation of mesenchymal stem cells and higher recurrence rate in hematologic malignancy patients: Outcome of a pilot clinical study. Leukemia 2008, 22, 593–599. [Google Scholar] [CrossRef]
- Kebriaei, P.; Isola, L.; Bahceci, E.; Holland, K.; Rowley, S.; McGuirk, J.; Devetten, M.; Jansen, J.; Herzig, R.; Schuster, M.; et al. Adult human mesenchymal stem cells added to corticosteroid therapy for the treatment of acute graft-versus-host disease. Biol Blood Marrow Transplant. 2009, 15, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Kurtzberg, J.; Prockop, S.; Teira, P.; Bittencourt, H.; Lewis, V.; Chan, K.W.; Horn, B.; Yu, L.; Talano, J.A.; Nemecek, E.; et al. Allogeneic human mesenchymal stem cell therapy (remestemcel-L, Prochymal) as a rescue agent for severe refractory acute graft-versus-host disease in pediatric patients. Biol. Blood Marrow Transplant. 2014, 20, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhang, M.; He, P. Pre-infusion single-dose mesenchymal stem cells promote platelet engraftment and decrease severe acute graft versus host disease without relapse in haploidentical peripheral blood stem cell transplantation. J. Int. Med. Res. 2020, 48, 300060520920438. [Google Scholar] [CrossRef] [PubMed]
- Kuzmina, L.A.; Petinati, N.A.; Parovichnikova, E.N.; Lubimova, L.S.; Gribanova, E.O.; Gaponova, T.V.; Shipounova, I.N.; Zhironkina, O.A.; Bigildeev, A.E.; Svinareva, D.A.; et al. Multipotent Mesenchymal Stromal Cells for the Prophylaxis of Acute Graft-versus-Host Disease-A Phase II Study. Stem Cells Int. 2012, 2012, 968213. [Google Scholar] [CrossRef]
- Maziarz, R.T.; Devos, T.; Bachier, C.R.; Goldstein, S.C.; Leis, J.F.; Devine, S.M.; Meyers, G.; Gajewski, J.L.; Maertens, J.; Deans, R.J.; et al. Single and multiple dose MultiStem (multipotent adult progenitor cell) therapy prophylaxis of acute graft-versus-host disease in myeloablative allogeneic hematopoietic cell transplantation: A phase 1 trial. Biol. Blood Marrow Transplant. 2015, 21, 720–728. [Google Scholar] [CrossRef]
- Gao, L.; Zhang, Y.; Hu, B.; Liu, J.; Kong, P.; Lou, S.; Su, Y.; Yang, T.; Li, H.; Liu, Y.; et al. Phase II Multicenter, Randomized, Double-Blind Controlled Study of Efficacy and Safety of Umbilical Cord-Derived Mesenchymal Stromal Cells in the Prophylaxis of Chronic Graft-Versus-Host Disease After HLA-Haploidentical Stem-Cell Transplantation. J. Clin. Oncol. 2016, 34, 2843–2850. [Google Scholar] [CrossRef]
- Lazarus, H.M.; Koc, O.N.; Devine, S.M.; Curtin, P.; Maziarz, R.T.; Holland, H.K.; Shpall, E.J.; McCarthy, P.; Atkinson, K.; Cooper, B.W.; et al. Cotransplantation of HLA-identical sibling culture-expanded mesenchymal stem cells and hematopoietic stem cells in hematologic malignancy patients. Biol. Blood Marrow Transplant. 2005, 11, 389–398. [Google Scholar] [CrossRef]
- Baron, F.; Lechanteur, C.; Willems, E.; Bruck, F.; Baudoux, E.; Seidel, L.; Vanbellinghen, J.F.; Hafraoui, K.; Lejeune, M.; Gothot, A.; et al. Cotransplantation of mesenchymal stem cells might prevent death from graft-versus-host disease (GVHD) without abrogating graft-versus-tumor effects after HLA-mismatched allogeneic transplantation following nonmyeloablative conditioning. Biol. Blood Marrow Transplant. 2010, 16, 838–847. [Google Scholar] [CrossRef]
- Zhao, F.; Zhang, Y.F.; Liu, Y.G.; Zhou, J.J.; Li, Z.K.; Wu, C.G.; Qi, H.W. Therapeutic effects of bone marrow-derived mesenchymal stem cells engraftment on bleomycin-induced lung injury in rats. Transplant. Proc. 2008, 40, 1700–1705. [Google Scholar] [CrossRef]
- Moodley, Y.; Atienza, D.; Manuelpillai, U.; Samuel, C.S.; Tchongue, J.; Ilancheran, S.; Boyd, R.; Trounson, A. Human umbilical cord mesenchymal stem cells reduce fibrosis of bleomycin-induced lung injury. Am. J. Pathol. 2009, 175, 303–313. [Google Scholar] [CrossRef]
- Yang, Y.; Zhu, S.; Li, Y.; Lu, Q.; Zhang, Q.; Su, L.; Zhao, Y.; Luo, Y.; Liu, Y. Human umbilical cord mesenchymal stem cells ameliorate skin fibrosis development in a mouse model of bleomycin-induced systemic sclerosis. Exp. Ther. Med. 2020, 20, 257. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Hou, J.; Zheng, K.; Wei, D.; Zhang, A.; Wang, S.; Mei, H.; Li, C.; Cheng, L.; Sun, X. Umbilical Cord Mesenchymal Stem Cells for Inhibiting the Fibrosis and Autoimmune Development in HOCl-Induced Systemic Scleroderma Mouse Model. Int. J. Stem Cells 2021, 14, 262–274. [Google Scholar] [CrossRef] [PubMed]
- Elessawi, D.F.; Gabr, H.; Badawy, M.M.M.; Gheita, T.A. Therapeutic potential of mesenchymal stem cells for scleroderma induced in mouse model. Tissue Cell 2021, 73, 101671. [Google Scholar] [CrossRef] [PubMed]
- Maria, A.T.; Toupet, K.; Bony, C.; Pirot, N.; Vozenin, M.C.; Petit, B.; Roger, P.; Batteux, F.; Le Quellec, A.; Jorgensen, C.; et al. Antifibrotic, Antioxidant, and Immunomodulatory Effects of Mesenchymal Stem Cells in HOCl-Induced Systemic Sclerosis. Arthritis Rheumatol. 2016, 68, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Rozier, P.; Maumus, M.; Maria, A.T.J.; Toupet, K.; Jorgensen, C.; Guilpain, P.; Noël, D. Lung Fibrosis Is Improved by Extracellular Vesicles from IFNγ-Primed Mesenchymal Stromal Cells in Murine Systemic Sclerosis. Cells 2021, 10, 2727. [Google Scholar] [CrossRef] [PubMed]
- Huldani, H.; Abdalkareem Jasim, S.; Olegovich Bokov, D.; Abdelbasset, W.K.; Nader Shalaby, M.; Thangavelu, L.; Margiana, R.; Qasim, M.T. Application of extracellular vesicles derived from mesenchymal stem cells as potential therapeutic tools in autoimmune and rheumatic diseases. Int. Immunopharmacol. 2022, 106, 108634. [Google Scholar] [CrossRef]
- Christopeit, M.; Schendel, M.; Föll, J.; Müller, L.P.; Keysser, G.; Behre, G. Marked improvement of severe progressive systemic sclerosis after transplantation of mesenchymal stem cells from an allogeneic haploidentical-related donor mediated by ligation of CD137L. Leukemia 2008, 22, 1062–1064. [Google Scholar] [CrossRef]
- Keyszer, G.; Christopeit, M.; Fick, S.; Schendel, M.; Taute, B.M.; Behre, G.; Müller, L.P.; Schmoll, H.J. Treatment of severe progressive systemic sclerosis with transplantation of mesenchymal stromal cells from allogeneic related donors: Report of five cases. Arthritis Rheum. 2011, 63, 2540–2542. [Google Scholar] [CrossRef]
- Rozier, P.; Maria, A.; Goulabchand, R.; Jorgensen, C.; Guilpain, P.; Noël, D. Mesenchymal Stem Cells in Systemic Sclerosis: Allogenic or Autologous Approaches for Therapeutic Use? Front. Immunol. 2018, 9, 2938. [Google Scholar] [CrossRef]
- Liang, J.; Zhang, H.; Kong, W.; Deng, W.; Wang, D.; Feng, X.; Zhao, C.; Hua, B.; Wang, H.; Sun, L. Safety analysis in patients with autoimmune disease receiving allogeneic mesenchymal stem cells infusion: A long-term retrospective study. Stem Cell Res. Ther. 2018, 9, 312. [Google Scholar] [CrossRef]
- Zhang, H.; Liang, J.; Tang, X.; Wang, D.; Feng, X.; Wang, F.; Hua, B.; Wang, H.; Sun, L. Sustained benefit from combined plasmapheresis and allogeneic mesenchymal stem cells transplantation therapy in systemic sclerosis. Arthritis Res. Ther. 2017, 19, 165. [Google Scholar] [CrossRef] [PubMed]
- Farge, D.; Loisel, S.; Resche-Rigon, M.; Lansiaux, P.; Colmegna, I.; Langlais, D.; Tarte, K. Safety and preliminary efficacy of allogeneic bone marrow-derived multipotent mesenchymal stromal cells for systemic sclerosis: A single-centre, open-label, dose-escalation, proof-of-concept, phase 1/2 study. Lancet Rheumatol. 2022, 4, e91–e104. [Google Scholar] [CrossRef]
- van Rhijn-Brouwer, F.C.C.; Gremmels, H.; Fledderus, J.O.; Schuurman, A.H.; Bonte-Mineur, F.; Vonk, M.C.; Voskuyl, A.E.; de Vries-Bouwstra, J.K.; Coert, J.H.; Radstake, T.R.D.J.; et al. A randomised placebo-controlled double-blind trial to assess the safety of intramuscular administration of allogeneic mesenchymal stromal cells for digital ulcers in systemic sclerosis: The MANUS Trial protocol. BMJ Open 2018, 8, e020479. [Google Scholar] [CrossRef] [PubMed]
- Gimble, J.M.; Katz, A.J.; Bunnell, B.A. Adipose-derived stem cells for regenerative medicine. Circ. Res. 2007, 100, 1249–1260. [Google Scholar] [CrossRef] [PubMed]
- Bourin, P.; Bunnell, B.A.; Casteilla, L.; Dominici, M.; Katz, A.J.; March, K.L.; Redl, H.; Rubin, J.P.; Yoshimura, K.; Gimble, J.M. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: A joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy 2013, 15, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I.; Dennis, J.E. Mesenchymal stem cells as trophic mediators. J. Cell Biochem. 2006, 98, 1076–1084. [Google Scholar] [CrossRef] [PubMed]
- Kilroy, G.E.; Foster, S.J.; Wu, X.; Ruiz, J.; Sherwood, S.; Heifetz, A.; Ludlow, J.W.; Stricker, D.M.; Potiny, S.; Green, P.; et al. Cytokine profile of human adipose-derived stem cells: Expression of angiogenic, hematopoietic, and pro-inflammatory factors. J. Cell Physiol. 2007, 212, 702–709. [Google Scholar] [CrossRef]
- Hsiao, S.T.; Lokmic, Z.; Peshavariya, H.; Abberton, K.M.; Dusting, G.J.; Lim, S.Y.; Dilley, R.J. Hypoxic conditioning enhances the angiogenic paracrine activity of human adipose-derived stem cells. Stem Cells Dev. 2013, 22, 1614–1623. [Google Scholar] [CrossRef]
- Kondo, K.; Shintani, S.; Shibata, R.; Murakami, H.; Murakami, R.; Imaizumi, M.; Kitagawa, Y.; Murohara, T. Implantation of adipose-derived regenerative cells enhances ischemia-induced angiogenesis. Arter. Thromb. Vasc. Biol. 2009, 29, 61–66. [Google Scholar] [CrossRef]
- Perin, E.C.; Sanz-Ruiz, R.; Sánchez, P.L.; Lasso, J.; Pérez-Cano, R.; Alonso-Farto, J.C.; Pérez-David, E.; Fernández-Santos, M.E.; Serruys, P.W.; Duckers, H.J.; et al. Adipose-derived regenerative cells in patients with ischemic cardiomyopathy: The PRECISE Trial. Am. Hear. J. 2014, 168, 88–95.e82. [Google Scholar] [CrossRef]
- Abu-Ghname, A.; Perdanasari, A.T.; Reece, E.M. Principles and Applications of Fat Grafting in Plastic Surgery. Semin. Plast. Surg. 2019, 33, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.W.; Scutaru, T.T.; Ghetu, N.; Carasevici, E.; Lupascu, C.D.; Ferariu, D.; Pieptu, D.; Coman, C.G.; Danciu, M. The Effects of Adipose-Derived Stem Cell-Differentiated Adipocytes on Skin Burn Wound Healing in Rats. J. Burn Care Res. 2017, 38, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Scuderi, N.; Ceccarelli, S.; Onesti, M.G.; Fioramonti, P.; Guidi, C.; Romano, F.; Frati, L.; Angeloni, A.; Marchese, C. Human adipose-derived stromal cells for cell-based therapies in the treatment of systemic sclerosis. Cell Transplant. 2013, 22, 779–795. [Google Scholar] [CrossRef] [PubMed]
- Granel, B.; Daumas, A.; Jouve, E.; Harlé, J.R.; Nguyen, P.S.; Chabannon, C.; Colavolpe, N.; Reynier, J.C.; Truillet, R.; Mallet, S.; et al. Safety, tolerability and potential efficacy of injection of autologous adipose-derived stromal vascular fraction in the fingers of patients with systemic sclerosis: An open-label phase I trial. Ann. Rheum. Dis. 2015, 74, 2175–2182. [Google Scholar] [CrossRef]
- Guillaume-Jugnot, P.; Daumas, A.; Magalon, J.; Jouve, E.; Nguyen, P.S.; Truillet, R.; Mallet, S.; Casanova, D.; Giraudo, L.; Veran, J.; et al. Autologous adipose-derived stromal vascular fraction in patients with systemic sclerosis: 12-month follow-up. Rheumatology 2016, 55, 301–306. [Google Scholar] [CrossRef]
- Daumas, A.; Magalon, J.; Jouve, E.; Truillet, R.; Casanova, D.; Giraudo, L.; Veran, J.; Benyamine, A.; Dignat-George, F.; Magalon, G.; et al. Long-term follow-up after autologous adipose-derived stromal vascular fraction injection into fingers in systemic sclerosis patients. Curr. Res. Transl. Med. 2017, 65, 40–43. [Google Scholar] [CrossRef]
- Park, Y.; Lee, Y.J.; Koh, J.H.; Lee, J.; Min, H.K.; Kim, M.Y.; Kim, K.J.; Lee, S.J.; Rhie, J.W.; Kim, W.U.; et al. Clinical Efficacy and Safety of Injection of Stromal Vascular Fraction Derived from Autologous Adipose Tissues in Systemic Sclerosis Patients with Hand Disability: A Proof-Of-Concept Trial. J. Clin. Med. 2020, 9, 3023. [Google Scholar] [CrossRef]
- Del Papa, N.; Caviggioli, F.; Sambataro, D.; Zaccara, E.; Vinci, V.; Di Luca, G.; Parafioriti, A.; Armiraglio, E.; Maglione, W.; Polosa, R.; et al. Autologous fat grafting in the treatment of fibrotic perioral changes in patients with systemic sclerosis. Cell Transplant. 2015, 24, 63–72. [Google Scholar] [CrossRef]
- Onesti, M.G.; Fioramonti, P.; Carella, S.; Fino, P.; Marchese, C.; Scuderi, N. Improvement of Mouth Functional Disability in Systemic Sclerosis Patients over One Year in a Trial of Fat Transplantation versus Adipose-Derived Stromal Cells. Stem Cells Int. 2016, 2016, 2416192. [Google Scholar] [CrossRef]
- Sautereau, N.; Daumas, A.; Truillet, R.; Jouve, E.; Magalon, J.; Veran, J.; Casanova, D.; Frances, Y.; Magalon, G.; Granel, B. Efficacy of Autologous Microfat Graft on Facial Handicap in Systemic Sclerosis Patients. Plast. Reconstr. Surg. Glob. Open 2016, 4, e660. [Google Scholar] [CrossRef]
- Almadori, A.; Griffin, M.; Ryan, C.M.; Hunt, D.F.; Hansen, E.; Kumar, R.; Abraham, D.J.; Denton, C.P.; Butler, P.E.M. Stem cell enriched lipotransfer reverses the effects of fibrosis in systemic sclerosis. PLoS ONE 2019, 14, e0218068. [Google Scholar] [CrossRef] [PubMed]
- Blezien, O.; D’Andrea, F.; Nicoletti, G.F.; Ferraro, G.A. Effects of Fat Grafting Containing Stem Cells in Microstomia and Microcheilia Derived from Systemic Sclerosis. Aesthetic Plast. Surg. 2017, 41, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Daumas, A.; Magalon, J.; Jouve, E.; Casanova, D.; Philandrianos, C.; Abellan Lopez, M.; Mallet, S.; Veran, J.; Auquit-Auckbur, I.; Farge, D.; et al. Adipose tissue-derived stromal vascular fraction for treating hands of patients with systemic sclerosis: A multicentre randomized trial Autologous AD-SVF versus placebo in systemic sclerosis. Rheumatology 2022, 61, 1936–1947. [Google Scholar] [CrossRef] [PubMed]
- Khanna, D.; Caldron, P.; Martin, R.W.; Kafaja, S.; Spiera, R.; Shahouri, S.; Shah, A.; Hsu, V.; Ervin, J.; Simms, R.; et al. Adipose-Derived Regenerative Cell Transplantation for the Treatment of Hand Dysfunction in Systemic Sclerosis: A Randomized Clinical Trial. Arthritis Rheumatol. 2022, 74, 1399–1408. [Google Scholar] [CrossRef]
- Del Papa, N.; Vitali, C.; Minniti, A.; Caporali, R. Is adipose-tissue (or its fraction) grafting really effective in the treatment of scleroderma hand? Rheumatology 2022, 61, 1756–1757. [Google Scholar] [CrossRef]
- Kamata, Y.; Takahashi, Y.; Iwamoto, M.; Matsui, K.; Murakami, Y.; Muroi, K.; Ikeda, U.; Shimada, K.; Yoshio, T.; Okazaki, H.; et al. Local implantation of autologous mononuclear cells from bone marrow and peripheral blood for treatment of ischaemic digits in patients with connective tissue diseases. Rheumatology 2007, 46, 882–884. [Google Scholar] [CrossRef][Green Version]
- Takahashi, M.; Izawa, A.; Ishigatsubo, Y.; Fujimoto, K.; Miyamoto, M.; Horie, T.; Aizawa, Y.; Amano, J.; Minota, S.; Murohara, T.; et al. Therapeutic neovascularization by the implantation of autologous mononuclear cells in patients with connective tissue diseases. Curr. Pharm. Des. 2009, 15, 2778–2783. [Google Scholar] [CrossRef]
- Nevskaya, T.; Ananieva, L.; Bykovskaia, S.; Eremin, I.; Karandashov, E.; Khrennikov, J.; Mach, E.; Zaprjagaeva, M.; Guseva, N.; Nassonov, E. Autologous progenitor cell implantation as a novel therapeutic intervention for ischaemic digits in systemic sclerosis. Rheumatology 2009, 48, 61–64. [Google Scholar] [CrossRef]
- Ishigatsubo, Y.; Ihata, A.; Kobayashi, H.; Hama, M.; Kirino, Y.; Ueda, A.; Takeno, M.; Shirai, A.; Ohno, S. Therapeutic angiogenesis in patients with systemic sclerosis by autologous transplantation of bone-marrow-derived cells. Mod. Rheumatol. 2010, 20, 263–272. [Google Scholar] [CrossRef]
- Takagi, G.; Miyamoto, M.; Tara, S.; Kirinoki-Ichikawa, S.; Kubota, Y.; Hada, T.; Takagi, I.; Mizuno, K. Therapeutic vascular angiogenesis for intractable macroangiopathy-related digital ulcer in patients with systemic sclerosis: A pilot study. Rheumatology 2014, 53, 854–859. [Google Scholar] [CrossRef]
- Bank, J.; Fuller, S.M.; Henry, G.I.; Zachary, L.S. Fat grafting to the hand in patients with Raynaud phenomenon: A novel therapeutic modality. Plast. Reconstr. Surg. 2014, 133, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Del Bene, M.; Pozzi, M.R.; Rovati, L.; Mazzola, I.; Erba, G.; Bonomi, S. Autologous fat grafting for scleroderma induced digital ulcers. An effective technique in patients with systemic sclerosis. Handchir. Mikrochir. Plast. Chir. 2014, 46, 242–247. [Google Scholar]
- Del Papa, N.; Di Luca, G.; Sambataro, D.; Zaccara, E.; Maglione, W.; Gabrielli, A.; Fraticelli, P.; Moroncini, G.; Beretta, L.; Santaniello, A.; et al. Regional implantation of autologous adipose tissue-derived cells induces a prompt healing of long-lasting indolent digital ulcers in patients with systemic sclerosis. Cell Transplant. 2015, 24, 2297–2305. [Google Scholar] [CrossRef] [PubMed]
- Del Papa, N.; Di Luca, G.; Andracco, R.; Zaccara, E.; Maglione, W.; Pignataro, F.; Minniti, A.; Vitali, C. Regional grafting of autologous adipose tissue is effective in inducing prompt healing of indolent digital ulcers in patients with systemic sclerosis: Results of a monocentric randomized controlled study. Arthritis Res. Ther. 2019, 21, 7. [Google Scholar] [CrossRef] [PubMed]
- Ugor, E.; Simon, D.; Almanzar, G.; Pap, R.; Najbauer, J.; Németh, P.; Balogh, P.; Prelog, M.; Czirják, L.; Berki, T. Increased proportions of functionally impaired regulatory T cell subsets in systemic sclerosis. Clin. Immunol. 2017, 184, 54–62. [Google Scholar] [CrossRef]
- Slobodin, G.; Ahmad, M.S.; Rosner, I.; Peri, R.; Rozenbaum, M.; Kessel, A.; Toubi, E.; Odeh, M. Regulatory T cells (CD4(+)CD25(bright)FoxP3(+)) expansion in systemic sclerosis correlates with disease activity and severity. Cell. Immunol. 2010, 261, 77–80. [Google Scholar] [CrossRef]
- Kamio, K.; Azuma, A.; Matsuda, K.; Usuki, J.; Inomata, M.; Morinaga, A.; Kashiwada, T.; Nishijima, N.; Itakura, S.; Kokuho, N.; et al. Resolution of bleomycin-induced murine pulmonary fibrosis via a splenic lymphocyte subpopulation. Respir. Res. 2018, 19, 71. [Google Scholar] [CrossRef]
- Trzonkowski, P.; Bieniaszewska, M.; Juścińska, J.; Dobyszuk, A.; Krzystyniak, A.; Marek, N.; Myśliwska, J.; Hellmann, A. First-in-man clinical results of the treatment of patients with graft versus host disease with human ex vivo expanded CD4+CD25+CD127- T regulatory cells. Clin. Immunol. 2009, 133, 22–26. [Google Scholar] [CrossRef]
- Brunstein, C.G.; Miller, J.S.; Cao, Q.; McKenna, D.H.; Hippen, K.L.; Curtsinger, J.; Defor, T.; Levine, B.L.; June, C.H.; Rubinstein, P.; et al. Infusion of ex vivo expanded T regulatory cells in adults transplanted with umbilical cord blood: Safety profile and detection kinetics. Blood 2011, 117, 1061–1070. [Google Scholar] [CrossRef]
- Di Ianni, M.; Falzetti, F.; Carotti, A.; Terenzi, A.; Castellino, F.; Bonifacio, E.; Del Papa, B.; Zei, T.; Ostini, R.I.; Cecchini, D.; et al. Tregs prevent GVHD and promote immune reconstitution in HLA-haploidentical transplantation. Blood 2011, 117, 3921–3928. [Google Scholar] [CrossRef]
- Matsuoka, K.; Koreth, J.; Kim, H.T.; Bascug, G.; McDonough, S.; Kawano, Y.; Murase, K.; Cutler, C.; Ho, V.T.; Alyea, E.P.; et al. Low-dose interleukin-2 therapy restores regulatory T cell homeostasis in patients with chronic graft-versus-host disease. Sci. Transl. Med. 2013, 5, 179ra143. [Google Scholar] [CrossRef] [PubMed]
- Bluestone, J.A.; Buckner, J.H.; Fitch, M.; Gitelman, S.E.; Gupta, S.; Hellerstein, M.K.; Herold, K.C.; Lares, A.; Lee, M.R.; Li, K.; et al. Type 1 diabetes immunotherapy using polyclonal regulatory T cells. Sci. Transl. Med. 2015, 7, 315ra189. [Google Scholar] [CrossRef] [PubMed]
- Chwojnicki, K.; Iwaszkiewicz-Grześ, D.; Jankowska, A.; Zieliński, M.; Łowiec, P.; Gliwiński, M.; Grzywińska, M.; Kowalczyk, K.; Konarzewska, A.; Glasner, P.; et al. Administration of CD4. BioDrugs 2021, 35, 47–60. [Google Scholar] [CrossRef]
- Ellebrecht, C.T.; Bhoj, V.G.; Nace, A.; Choi, E.J.; Mao, X.; Cho, M.J.; Di Zenzo, G.; Lanzavecchia, A.; Seykora, J.T.; Cotsarelis, G.; et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science 2016, 353, 179–184. [Google Scholar] [CrossRef]
- Aghajanian, H.; Kimura, T.; Rurik, J.G.; Hancock, A.S.; Leibowitz, M.S.; Li, L.; Scholler, J.; Monslow, J.; Lo, A.; Han, W.; et al. Targeting cardiac fibrosis with engineered T cells. Nature 2019, 573, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Rurik, J.G.; Tombácz, I.; Yadegari, A.; Méndez Fernández, P.O.; Shewale, S.V.; Li, L.; Kimura, T.; Soliman, O.Y.; Papp, T.E.; Tam, Y.K.; et al. CAR T cells produced in vivo to treat cardiac injury. Science 2022, 375, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Mackensen, A.; Müller, F.; Mougiakakos, D.; Böltz, S.; Wilhelm, A.; Aigner, M.; Völkl, S.; Simon, D.; Kleyer, A.; Munoz, L.; et al. Anti-CD19 CAR T cell therapy for refractory systemic lupus erythematosus. Nat. Med. 2022, 28, 2124–2132. [Google Scholar] [CrossRef]
- Sadeqi Nezhad, M.; Seifalian, A.; Bagheri, N.; Yaghoubi, S.; Karimi, M.H.; Adbollahpour-Alitappeh, M. Chimeric Antigen Receptor Based Therapy as a Potential Approach in Autoimmune Diseases: How Close Are We to the Treatment? Front. Immunol. 2020, 11, 603237. [Google Scholar] [CrossRef]
- Elinav, E.; Waks, T.; Eshhar, Z. Redirection of regulatory T cells with predetermined specificity for the treatment of experimental colitis in mice. Gastroenterology 2008, 134, 2014–2024. [Google Scholar] [CrossRef]
- Blat, D.; Zigmond, E.; Alteber, Z.; Waks, T.; Eshhar, Z. Suppression of murine colitis and its associated cancer by carcinoembryonic antigen-specific regulatory T cells. Mol. Ther. 2014, 22, 1018–1028. [Google Scholar] [CrossRef]
- Tenspolde, M.; Zimmermann, K.; Weber, L.C.; Hapke, M.; Lieber, M.; Dywicki, J.; Frenzel, A.; Hust, M.; Galla, M.; Buitrago-Molina, L.E.; et al. Regulatory T cells engineered with a novel insulin-specific chimeric antigen receptor as a candidate immunotherapy for type 1 diabetes. J. Autoimmun. 2019, 103, 102289. [Google Scholar] [CrossRef] [PubMed]
- Comi, M.; Avancini, D.; Santoni de Sio, F.; Villa, M.; Uyeda, M.J.; Floris, M.; Tomasoni, D.; Bulfone, A.; Roncarolo, M.G.; Gregori, S. Coexpression of CD163 and CD141 identifies human circulating IL-10-producing dendritic cells (DC-10). Cell. Mol. Immunol. 2020, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Mansilla, M.J.; Sellès-Moreno, C.; Fàbregas-Puig, S.; Amoedo, J.; Navarro-Barriuso, J.; Teniente-Serra, A.; Grau-López, L.; Ramo-Tello, C.; Martínez-Cáceres, E.M. Beneficial effect of tolerogenic dendritic cells pulsed with MOG autoantigen in experimental autoimmune encephalomyelitis. CNS Neurosci. Ther. 2015, 21, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Tal, O.; Lim, H.Y.; Gurevich, I.; Milo, I.; Shipony, Z.; Ng, L.G.; Angeli, V.; Shakhar, G. DC mobilization from the skin requires docking to immobilized CCL21 on lymphatic endothelium and intralymphatic crawling. J. Exp. Med. 2011, 208, 2141–2153. [Google Scholar] [CrossRef]
- Ridolfi, R.; Riccobon, A.; Galassi, R.; Giorgetti, G.; Petrini, M.; Fiammenghi, L.; Stefanelli, M.; Ridolfi, L.; Moretti, A.; Migliori, G.; et al. Evaluation of in vivo labelled dendritic cell migration in cancer patients. J. Transl. Med. 2004, 2, 27. [Google Scholar] [CrossRef]
- Morante-Palacios, O.; Fondelli, F.; Ballestar, E.; Martínez-Cáceres, E.M. Tolerogenic Dendritic Cells in Autoimmunity and Inflammatory Diseases. Trends Immunol. 2021, 42, 59–75. [Google Scholar] [CrossRef]
- Kowal-Bielecka, O.; Fransen, J.; Avouac, J.; Becker, M.; Kulak, A.; Allanore, Y.; Distler, O.; Clements, P.; Cutolo, M.; Czirjak, L.; et al. Update of EULAR recommendations for the treatment of systemic sclerosis. Ann. Rheum. Dis. 2017, 76, 1327–1339. [Google Scholar] [CrossRef]
- Doglio, M.; Alexander, T.; Del Papa, N.; Snowden, J.A.; Greco, R. New insights in systemic lupus erythematosus: From regulatory T cells to CAR-T-cell strategies. J. Allergy Clin. Immunol. 2022, S0091-6749(22)01056-9. [Google Scholar] [CrossRef]
| MSC Isolation | Administration Route | Source | Treated Patients | Clinical Target | Outcome | Major Adverse Events | References |
|---|---|---|---|---|---|---|---|
| BM-derived MSCs | Intravenous | Allo | 1 | Severe diffuse SSc | Ulcer healing and improved skin elasticity/vascularization | None | Christopeit et al., 2008 |
| BM-derived MSCs | Intravenous | Allo | 5 | Severe diffuse SSc | All patients had temporary clinical improvement | Minor respiratory infection | Keyzer et al., 2011 |
| BM-derived MSCs | Intravenous | Allo | 20 | Severe diffuse SSc | 15 patients showed sustained improvement in skin thickness | None | Farge et al., 2022 |
| BM-derived MSCs and peripheral blood MSCs | Intramuscular injection | Auto | 6 (4 SSc, 2 mixed connective tissue disease) | Severe ischaemia and necrosis in fingers and/or toes | Pain relief in 5/6 patients | None | Kamata et al., 2007 |
| BM-derived MSCs and peripheral blood MSCs | Intramuscular injection | Auto | 2 | Severe digital and malleolar ulcers | All had improvements with ulcers healing, pain relief, reduction of RP | None | Nevskaya et al., 2009 |
| BM-derived MSCs and peripheral blood MSCs | Intramuscular injection | Auto | 46 (24 SSc, 22 other connective tissue diseases) | Severe digital ulcers | 20/23 SSc patients had improvement in pain and ulcers | None | Takahashi et al., 2009 |
| BM-derived MSCs | Intramuscular injection | Auto | 8 | Severe digital ulcers | All had ulcers size and pain improvement | None | Ishigatsubo et al., 2010 |
| BM-derived MSCs | Intramuscular injection | Auto | 40 (11 SSc, 29 with arteriosclerosis obliterans) | Severe digital ulcers | All had pain and trans-cutaneous oxygen tension improvement | Major limb amputation due to pre-existing osteomyelitis | Takagi et al., 2014 |
| Adipose derived cell fractions | Subcutaneous injection | Auto | 13 | Raynaud’s phenomenon | 10 patients had clinical benefit, 3 reported no changes. | None | Bank et al., 2014 |
| Adipose derived cell fractions | Subcutaneous injection | Auto | 20 | Peri-oral fibrosis | All patients had improved skin elasticity and vascularization | Small areas of ecchymosis | Del Papa et al., 2015 |
| Adipose derived cell fractions | Subcutaneous injection | Auto | 15 | Severe digital ulcers | All patients displayed clinical benefit with fast healing of digital ulcers | None | Del Papa et al., 2015 |
| Adipose derived cell fractions plus platelet-rich plasma | Subcutaneous injection | Auto | 6 | Peri-oral fibrosis | All patients had improved skin elasticity and vascularization | None | Virzì et al., 2017 |
| Adipose derived cell fractions | Subcutaneaous/perioral injection | Auto | 6 | Skin scleroderma | Improvement in 4 patients, stabilization in all | None | Scuderi et al., 2013 |
| Adipose derived cell fractions | Subcutaneous injection | Auto | 5 | Peri-oral fibrosis | All patients had improvement to perioral fibrosis | None | Onesti et al., 2016 |
| Adipose derived cell fractions plus platelet-rich plasma | Subcutaneous injection | Auto | 7 | Peri-oral fibrosis | All patients had improvement to perioral fibrosis | None | Blezien et al., 2017 |
| Adipose derived cell fractions | Subcutaneous injection | Auto | 62 | Peri-oral fibrosis | Improvement in mouth opening | Superficial wound infection | Almadori et al., 2019 |
| SVF | Subcutaneous injection | Auto | 12 | Severe hand dysfunction | Improvement of pain, grasping capacity, finger oedema, Raynaud’s phenomenom, quality of life | None | Guillaume-Jugnot et al., 2016, Daumas et al., 2017, Granel et al., 2015 |
| SVF | Subcutaneous injection | Auto | 18 | Severe hand dysfunction | Improvement of skin fibrosis, hand oedema, and quality of life | None | Park et al., 2020 |
| Adipose derived cell fractions | Subcutaneous injection | Auto | 9 | Severe digital ulcers | All patients had pain improvement, digital ulcers improvement or healing | None | Del Bene et al., 2014 |
| Adipose derived cell fractions vs placebo | Subcutaneous injection | Auto | 25 vs. 13 | Severe digital ulcers | 23/25 and 1/13 patients had digital ulcers improvement and healing, pain reduction and improvement on nail fold capillaroscopy | None | Del Papa et al., 2019 |
| SVF vs placebo | Subcutaneous injection | Auto | 20 vs. 20 | Severe hand dysfunction | Improvement of hand function in both groups, with no superiority of the SVF | Hypoxaemia during the surgical process | Daumas et al., 2022 |
| Adipose derived cell fractions vs placebo | Subcutaneous injection | Auto | 48 vs. 40 | Severe hand dysfunction | No improvement of hand function | Aspiration pneumonia, hypotension, angina | Khanna et al., 2022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xue, E.; Minniti, A.; Alexander, T.; Del Papa, N.; Greco, R.; on behalf of The Autoimmune Diseases Working Party (ADWP) of the European Society for Blood and Marrow Transplantation (EBMT). Cellular-Based Therapies in Systemic Sclerosis: From Hematopoietic Stem Cell Transplant to Innovative Approaches. Cells 2022, 11, 3346. https://doi.org/10.3390/cells11213346
Xue E, Minniti A, Alexander T, Del Papa N, Greco R, on behalf of The Autoimmune Diseases Working Party (ADWP) of the European Society for Blood and Marrow Transplantation (EBMT). Cellular-Based Therapies in Systemic Sclerosis: From Hematopoietic Stem Cell Transplant to Innovative Approaches. Cells. 2022; 11(21):3346. https://doi.org/10.3390/cells11213346
Chicago/Turabian StyleXue, Elisabetta, Antonina Minniti, Tobias Alexander, Nicoletta Del Papa, Raffaella Greco, and on behalf of The Autoimmune Diseases Working Party (ADWP) of the European Society for Blood and Marrow Transplantation (EBMT). 2022. "Cellular-Based Therapies in Systemic Sclerosis: From Hematopoietic Stem Cell Transplant to Innovative Approaches" Cells 11, no. 21: 3346. https://doi.org/10.3390/cells11213346
APA StyleXue, E., Minniti, A., Alexander, T., Del Papa, N., Greco, R., & on behalf of The Autoimmune Diseases Working Party (ADWP) of the European Society for Blood and Marrow Transplantation (EBMT). (2022). Cellular-Based Therapies in Systemic Sclerosis: From Hematopoietic Stem Cell Transplant to Innovative Approaches. Cells, 11(21), 3346. https://doi.org/10.3390/cells11213346







