Proactive Immunotherapeutic Approaches against Inflammatory Breast Cancer May Improve Patient Outcomes
Abstract
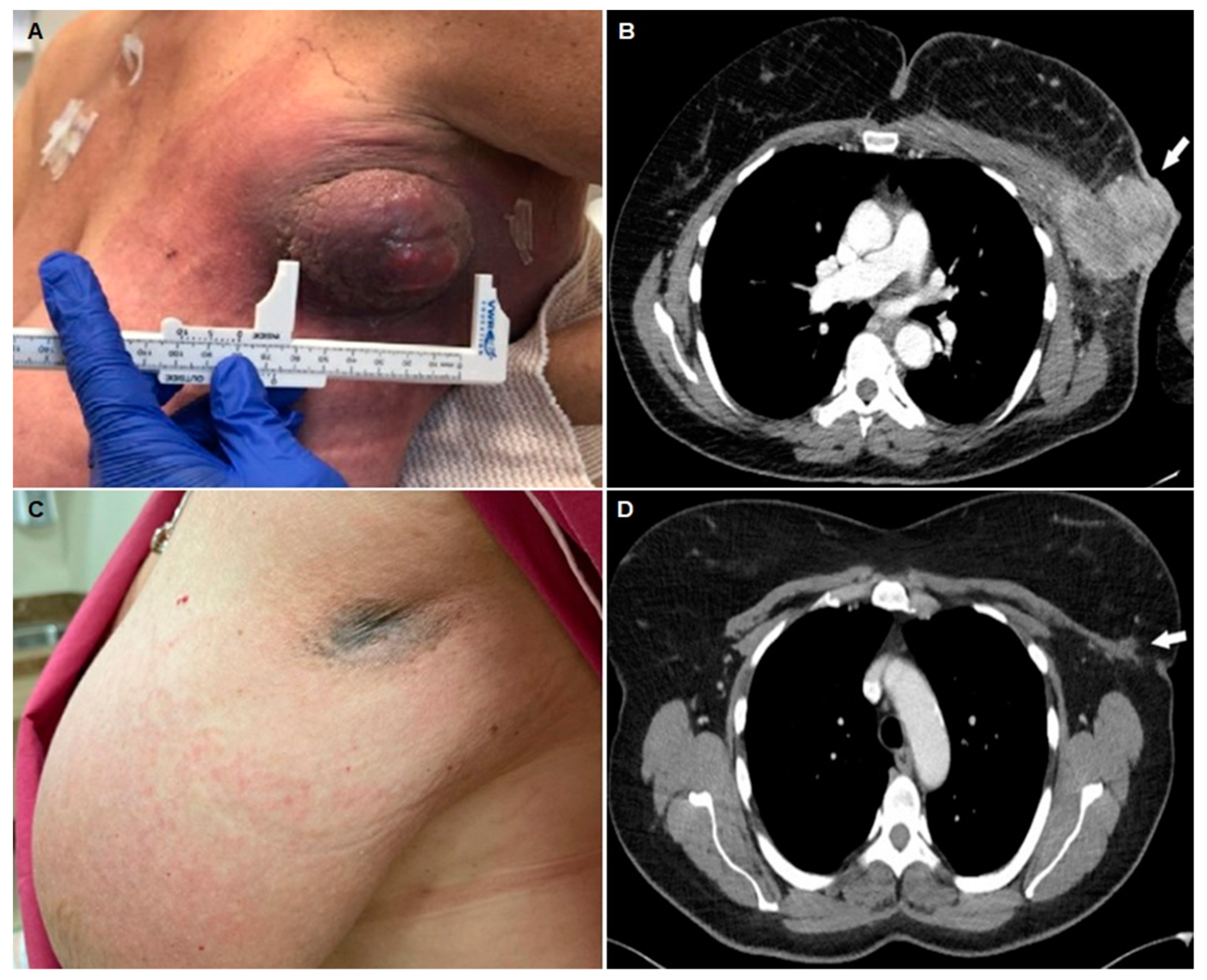
1. The Clinical Burden of IBC
2. The Urgency of Applying Novel Efficacious and Economically Available Therapies against IBC
3. Can We Achieve Good Clinical Responses and Improve Outcomes with Low Biologic and Economic Toxicity for IBC Patients?
4. What Other Immunotherapies Could Be Applied with ISV to IBC Patients?
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hance, K.W.; Anderson, W.F.; Devesa, S.S.; Young, H.A.; Levine, P.H. Trends in Inflammatory Breast Carcinoma Incidence and Survival: The Surveillance, Epidemiology, and End Results Program at the National Cancer Institute. J. Natl. Cancer Inst. 2005, 97, 966–975. [Google Scholar] [CrossRef] [PubMed]
- Goldner, B.; Behrendt, C.E.; Schoellhammer, H.F.; Lee, B.; Chen, S.L. Incidence of Inflammatory Breast Cancer in Women, 1992–2009, United States. Ann. Surg. Oncol. 2014, 21, 1267–1270. [Google Scholar] [CrossRef] [PubMed]
- Van Uden, D.J.P.; Bretveld, R.; Siesling, S.; de Wilt, J.H.W.; Blanken-Peeters, C.F.J.M. Inflammatory breast cancer in the Netherlands; improved survival over the last decades. Breast Cancer Res. Treat. 2017, 162, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Fayanju, O.M.; Ren, Y.; Greenup, R.A.; Plichta, J.K.; Rosenberger, L.H.; Force, J.; Suneja, G.; Devi, G.R.; King, T.A.; Nakhlis, F.; et al. Extent of axillary surgery in inflammatory breast cancer: A survival analysis of 3500 patients. Breast Cancer Res. Treat. 2020, 180, 207–217. [Google Scholar] [CrossRef]
- Low, J.A.; Berman, A.W.; Steinberg, S.M.; Danforth, D.N.; Lippman, M.E.; Swain, S.M. Long-term follow-up for locally advanced and inflammatory breast cancer patients treated with multimodality therapy. J. Clin. Oncol. 2004, 22, 4067–4074. [Google Scholar] [CrossRef]
- Ueno, N.T.; Buzdar, A.U.; Singletary, S.E.; Ames, F.C.; McNeese, M.D.; Holmes, F.A.; Theriault, R.L.; Strom, E.A.; Wasaff, B.J.; Asmar, L.; et al. Combined-modality treatment of inflammatory breast carcinoma: Twenty years of experience at M. D. Anderson Cancer Center. Cancer Chemother. Pharmacol. 1997, 40, 321–329. [Google Scholar] [CrossRef]
- Chainitikun, S.; Saleem, S.; Lim, B.; Valero, V.; Ueno, N.T. Update on systemic treatment for newly diagnosed inflammatory breast cancer. J. Adv. Res. 2020, 29, 1–12. [Google Scholar] [CrossRef]
- Woodward, W.A. Inflammatory breast cancer: Unique biological and therapeutic considerations. Lancet Oncol. 2015, 16, e568–e576. [Google Scholar] [CrossRef]
- Lim, B.; Woodward, W.A.; Wang, X.; Reuben, J.M.; Ueno, N.T. Inflammatory breast cancer biology: The tumour microenvironment is key. Nat. Rev. Cancer 2018, 18, 485–499. [Google Scholar] [CrossRef]
- Rosenbluth, J.M.; Overmoyer, B.A. Inflammatory Breast Cancer: A Separate Entity. Curr. Oncol. Rep. 2019, 21, 86. [Google Scholar] [CrossRef]
- Menta, A.; Fouad, T.M.; Lucci, A.; Le-Petross, H.; Stauder, M.C.; Woodward, W.A.; Ueno, N.T.; Lim, B. Inflammatory Breast Cancer: What to Know About This Unique, Aggressive Breast Cancer. Surg. Clin. North Am. 2018, 98, 787–800. [Google Scholar] [CrossRef] [PubMed]
- Dawood, S.; Cristofanilli, M. IBC as a Rapidly Spreading Systemic Disease: Clinical and Targeted Approaches Using the Neoadjuvant Model. J. Natl. Cancer Inst. Monogr. 2015, 2015, 56–59. [Google Scholar] [CrossRef]
- Gonzalez-Angulo, A.M.; Hennessy, B.T.; Broglio, K.; Meric-Bernstam, F.; Cristofanilli, M.; Giordano, S.H.; Buchholz, T.A.; Sahin, A.; Singletary, S.E.; Buzdar, A.U.; et al. Trends for Inflammatory Breast Cancer: Is Survival Improving? Oncologist 2007, 12, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Kharel, Z.; Nemer, O.P.; Xi, W.; Upadhayaya, B.; Falkson, C.I.; O’Regan, R.M.; Dhakal, A. Inflammatory breast cancer with excellent response to pembrolizumab-chemotherapy combination: A case report. Breast Disease 2022, 41, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Cortés, J.; Dent, R.; Pusztai, L.; McArthur, H.; Kuemmel, S.; Bergh, J.; Denkert, C.; Park, Y.; Hui, R.; et al. KEYNOTE-522: Phase 3 study of pembrolizumab (pembro) + chemotherapy (chemo) vs placebo (pbo) + chemo as neoadjuvant treatment, followed by pembro vs pbo as adjuvant treatment for early triple-negative breast cancer (TNBC). Ann. Oncol. 2019, 30, v851–v934. [Google Scholar] [CrossRef]
- Schmid, P.; Cortes, J.; Pusztai, L.; McArthur, H.; Kümmel, S.; Bergh, J.; Denkert, C.; Park, Y.H.; Hui, R.; Harbeck, N.; et al. Pembrolizumab for Early Triple-Negative Breast Cancer. N. Engl. J. Med. 2020, 382, 810–821. [Google Scholar] [CrossRef] [PubMed]
- Kepp, O.; Senovilla, L.; Vitale, I.; Vacchelli, E.; Adjemian, S.; Agostinis, P.; Apetoh, L.; Aranda, F.; Barnaba, V.; Bloy, N.; et al. Consensus guidelines for the detection of immunogenic cell death. OncoImmunology 2014, 3, e955691. [Google Scholar] [CrossRef]
- Pol, J.; Vacchelli, E.; Aranda, F.; Castoldi, F.; Eggermont, A.; Cremer, I.; Sautès-Fridman, C.; Fucikova, J.; Galon, J.; Spisek, R.; et al. Trial Watch: Immunogenic cell death inducers for anticancer chemotherapy. OncoImmunology 2015, 4, e1008866. [Google Scholar] [CrossRef]
- Galluzzi, L.; Vitale, I.; Warren, S.; Adjemian, S.; Agostinis, P.; Martinez, A.B.; Chan, T.A.; Coukos, G.; Demaria, S.; Deutsch, E.; et al. Consensus guidelines for the definition, detection and interpretation of immunogenic cell death. J. Immunother. Cancer 2020, 8, e000337. [Google Scholar] [CrossRef]
- Dhakal, A. (1425 Portland Avenue, Rochester General Hospital, Rochester 14621, NY, USA). Personal communication, Follow-up of patient treated with pembrolizumab and reported.d in this communication in reference 14, 5 May 2022.
- Arias-Pulido, H.; Cimino-Mathews, A.; Chaher, N.; Qualls, C.; Joste, N.; Colpaert, C.; Marotti, J.D.; Foisey, M.; Prossnitz, E.R.; Emens, L.A.; et al. The combined presence of CD20 + B cells and PD-L1 + tumor-infiltrating lymphocytes in inflammatory breast cancer is prognostic of improved patient outcome. Breast Cancer Res. Treat. 2018, 171, 273–282. [Google Scholar] [CrossRef]
- Arias-Pulido, H.; Cimino-Mathews, A.M.; Chaher, N.; Qualls, C.R.; Joste, N.; Colpaert, C.; Marotti, J.D.; Chamberlin, M.D.; Foisey, M.G.; Prossnitz, E.R.; et al. Differential effects of CD20+ B cells and PD-L1+ immune cells on pathologic complete response and outcome: Comparison between inflammatory breast cancer and locally advanced breast cancer patients. Breast Cancer Res. Treat. 2021, 190, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Van Berckelaer, C.; Rypens, C.; van Dam, P.; Pouillon, L.; Parizel, M.; Schats, K.A.; Kockx, M.; Tjalma, W.A.A.; Vermeulen, P.; van Laere, S.; et al. Infiltrating stromal immune cells in inflammatory breast cancer are associated with an improved outcome and increased PD-L1 expression. Breast Cancer Res. 2019, 21, 28. [Google Scholar] [CrossRef] [PubMed]
- Van Berckelaer, C.; Vermeiren, I.; Vercauteren, L.; Rypens, C.; Oner, G.; Trinh, X.B.; Tjalma, W.A.A.; Broeckx, G.; Charafe-Jauffret, E.; Van Laere, S.; et al. The Evolution and Prognostic Role of Tumour-Infiltrating Lymphocytes and Peripheral Blood-Based Biomarkers in Inflammatory Breast Cancer Patients Treated with Neoadjuvant Chemotherapy. Cancers 2021, 13, 4656. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.-A.; Shaw Wright, G.; et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef]
- Cortes, J.; Cescon, D.W.; Rugo, H.S.; Nowecki, Z.; Im, S.A.; Yusof, M.M.; Gallardo, C.; Lipatov, O.; Barrios, C.H.; Holgado, E.; et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): A randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet 2020, 396, 1817–1828. [Google Scholar] [CrossRef]
- Shepherd, J.H.; Ballman, K.; Polley, M.C.; Campbell, J.D.; Fan, C.; Selitsky, S.; Fernandez-Martinez, A.; Parker, J.S.; Hoadley, K.A.; Hu, Z.; et al. CALGB 40603 (Alliance): Long-Term Outcomes and Genomic Correlates of Response and Survival After Neoadjuvant Chemotherapy with or without Carboplatin and Bevacizumab in Triple-Negative Breast Cancer. J. Clin. Oncol. 2022, 40, 1323–1334. [Google Scholar] [CrossRef]
- Ghate, S.R.; Li, Z.; Tang, J.; Nakasato, A.R. Economic Burden of Adverse Events Associated with Immunotherapy and Targeted Therapy for Metastatic Melanoma in the Elderly. Am. Health Drug Benefits 2018, 11, 334–343. [Google Scholar]
- Fotakis, G.; Trajanoski, Z.; Rieder, D. Computational cancer neoantigen prediction: Current status and recent advances. Immuno-Oncol. Technol. 2021, 12, 100052. [Google Scholar] [CrossRef]
- Aznar, M.A.; Tinari, N.; Rullán, A.J.; Sánchez-Paulete, A.R.; Rodriguez-Ruiz, M.E.; Melero, I. Intratumoral Delivery of Immunotherapy-Act Locally, Think Globally. J. Immunol. 2017, 198, 31–39. [Google Scholar] [CrossRef]
- Marabelle, A.; Tselikas, L.; de Baere, T.; Houot, R. Intratumoral immunotherapy: Using the tumor as the remedy. Ann. Oncol. 2017, 28, xii33–xii43. [Google Scholar] [CrossRef]
- Champiat, S.; Tselikas, L.; Farhane, S.; Raoult, T.; Texier, M.; Lanoy, E.; Massard, C.; Robert, C.; Ammari, S.; De Baère, T.; et al. Intratumoral Immunotherapy: From Trial Design to Clinical Practice. Clin. Cancer Res. 2021, 27, 665–679. [Google Scholar] [CrossRef] [PubMed]
- Melero, I.; Castanon, E.; Alvarez, M.; Champiat, S.; Marabelle, A. Intratumoural administration and tumour tissue targeting of cancer immunotherapies. Nat. Rev. Clin. Oncol. 2021, 18, 558–576. [Google Scholar] [CrossRef] [PubMed]
- Hamid, O.; Ismail, R.; Puzanov, I. Intratumoral Immunotherapy-Update 2019. Oncologist 2020, 25, e423–e438. [Google Scholar] [CrossRef] [PubMed]
- Sheen, M.R.; Fiering, S. In Situ Vaccination: Harvesting Low Hanging Fruit on the Cancer Immunotherapy Tree. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 11, e1524. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Miguel, D.; Valdivia, G.; Guerrera, D.; Perez-Alenza, M.D.; Pantelyushin, S.; Alonso-Diez, A.; Beiss, V.; Fiering, S.; Steinmetz, N.F.; Suarez-Redondo, M.; et al. Neoadjuvant in situ vaccination with cowpea mosaic virus as a novel therapy against canine inflammatory mammary cancer. J. Immunother. Cancer 2022, 10, e004044. [Google Scholar] [CrossRef]
- Lizotte, P.; Wen, A.M.; Sheen, M.R.; Fields, J.; Rojanasopondist, P.; Steinmetz, N.F.; Fiering, S. In situ vaccination with cowpea mosaic virus nanoparticles suppresses metastatic cancer. Nat Nanotechnol. 2016, 11, 295–303. [Google Scholar] [CrossRef]
- Kerstetter-Fogle, A.; Shukla, S.; Wang, C.; Beiss, V.; Harris, P.L.R.; Sloan, A.E.; Steinmetz, N.F. Plant Virus-Like Particle In Situ Vaccine for Intracranial Glioma Immunotherapy. Cancers 2019, 11, 515. [Google Scholar] [CrossRef]
- Cai, H.; Wang, C.; Shukla, S.; Steinmetz, N.F. Cowpea Mosaic Virus Immunotherapy Combined with Cyclophosphamide Reduces Breast Cancer Tumor Burden and Inhibits Lung Metastasis. Adv. Sci. (Weinh) 2019, 6, 1802281. [Google Scholar] [CrossRef]
- Wang, C.; Beiss, V.; Steinmetz, N.F. Cowpea Mosaic Virus Nanoparticles and Empty Virus-Like Particles Show Distinct but Overlapping Immunostimulatory Properties. J. Virol. 2019, 93, e00129-19. [Google Scholar] [CrossRef]
- Hoopes, P.J.; Wagner, R.J.; Duval, K.; Kang, K.; Gladstone, D.J.; Moodie, K.L.; Crary-Burney, M.; Ariaspulido, H.; Veliz, F.A.; Steinmetz, N.F.; et al. Treatment of Canine Oral Melanoma with Nanotechnology-Based Immunotherapy and Radiation. Mol. Pharm. 2018, 15, 3717–3722. [Google Scholar] [CrossRef]
- Raposo, T.P.; Arias-Pulido, H.; Chaher, N.; Fiering, S.N.; Argyle, D.J.; Prada, J.; Pires, I.; Queiroga, F.L. Comparative aspects of canine and human inflammatory breast cancer. Semin. Oncol. 2017, 44, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Marconato, L.; Romanelli, G.; Stefanello, D.; Giacoboni, C.; Bonfanti, U.; Bettini, G.; Finotello, R.; Verganti, S.; Valenti, P.; Ciaramella, L.; et al. Prognostic factors for dogs with mammary inflammatory carcinoma: 43 cases (2003–2008). J. Am. Vet. Med. Assoc. 2009, 235, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.; De Andrés, P.J.; Peña, L.; Pérez-Alenza, M.D. Survival time of dogs with inflammatory mammary cancer treated with palliative therapy alone or palliative therapy plus chemotherapy. Vet. Rec. 2009, 165, 78–81. [Google Scholar] [CrossRef]
- Mao, C.; Beiss, V.; Fields, J.; Steinmetz, N.F.; Fiering, S. Cowpea mosaic virus stimulates antitumor immunity through recognition by multiple MYD88-dependent toll-like receptors. Biomaterials 2021, 275, 120914. [Google Scholar] [CrossRef] [PubMed]
- Valdivia, G.; Alonso-Miguel, D.; Zimmermann, B.; Perez-Alenza, M.D.; Alonso-Diez, A.; Beiss, V.; Suárez-Redondo, M.; Fiering, S.; Steinmetz, N.F.; vom Berg, J.; et al. Neoadjuvant in situ vaccination with cowpea mosaic virus induces local and systemic antitumor efficacy in canine mammary cancer. 2022; manuscript in preparation. [Google Scholar]
- Wang, C.; Steinmetz, N.F. A Combination of Cowpea Mosaic Virus and Immune Checkpoint Therapy Synergistically Improves Therapeutic Efficacy in Three Tumor Models. Adv. Funct Mater. 2020, 30, 2002299. [Google Scholar] [CrossRef]
- Goldstein, D.A. Adjuvant Ipilimumab for Melanoma—The $1.8 Million per Patient Regimen. JAMA Oncol. 2017, 3, 1628–1629. [Google Scholar] [CrossRef]
- Ray, A.; Williams, M.A.; Meek, S.M.; Bowen, R.C.; Grossmann, K.F.; Andtbacka, R.H.; Bowles, T.L.; Hyngstrom, J.R.; Leachman, S.A.; Grossman, D.; et al. A phase I study of intratumoral ipilimumab and interleukin-2 in patients with advanced melanoma. Oncotarget 2016, 7, 64390–64399. [Google Scholar] [CrossRef]
- Huppert, L.A.; Mariotti, V.; Chien, A.J.; Soliman, H.H. Emerging immunotherapeutic strategies for the treatment of breast cancer. Breast Cancer Res. Treat. 2022, 191, 243–255. [Google Scholar] [CrossRef]
- Huang, A.; Pressnall, M.M.; Lu, R.; Huayamares, S.G.; Griffin, J.D.; Groer, C.; DeKosky, B.J.; Forrest, M.L.; Berkland, C.J. Human intratumoral therapy: Linking drug properties and tumor transport of drugs in clinical trials. J. Control. Release 2020, 326, 203–221. [Google Scholar] [CrossRef]
- Sheth, R.A.; Murthy, R.; Hong, D.S.; Patel, S.; Overman, M.J.; Diab, A.; Hwu, P.; Tam, A. Assessment of Image-Guided Intratumoral Delivery of Immunotherapeutics in Patients With Cancer. JAMA Netw. Open 2020, 3, e207911. [Google Scholar] [CrossRef]
- O’Day, S.; Perez, C.; Wise-Draper, T.; Hanna, G.; Bhatia, S.; Kelly, C.; Medina, T.; Laux, D.; Daud, A.; Chandra, S.; et al. 423 Safety and preliminary efficacy of intratumoral cavrotolimod (AST-008), a spherical nucleic acid TLR9 agonist, in combination with pembrolizumab in patients with advanced solid tumors. J. Immunother. Cancer 2020, 8, A257–A258. [Google Scholar]
- Carroll, C.S.E.; Andrew, E.R.; Malik, L.; Elliott, K.F.; Brennan, M.; Meyer, J.; Hintze, A.; Almonte, A.A.; Lappin, C.; MacPherson, P.; et al. Simple and effective bacterial-based intratumoral cancer immunotherapy. J. Immunother. Cancer 2021, 9, e002688. [Google Scholar] [CrossRef] [PubMed]
- Stinson, J.; Sheen, A.; Momin, N.; Hampel, J.; Bernstein, R.; Kamerer, R.; Samuelson, J.; Selting, K.; Fan, T.M.; Wittrup, K.D. Abstract nr 4171: Treatment of canine soft tissue sarcomas and melanomas with intratumoral colla-gen-anchored IL-2 and IL-12 is safe and effective [Abstract]. In Proceedings of the 97th Annual Meeting of the American Association for Cancer Research, New Orleans, LA, USA, 8–13 April 2022; AACR: Philadelphia, PA, USA, 2022. [Google Scholar]
- Soliman, A.; Banerjee, M.; Lo, A.; Ismail, K.; Hablas, A.; Seifeldin, I.; Ramadan, M.; Omar, H.; Fokuda, A.; Harford, J.; et al. High proportion of inflammatory breast cancer in the Population-based Cancer Registry of Gharbiah, Egypt. Breast J. 2009, 15, 432–434. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Slaoui, M.; Zoure, A.A.; Mouh, F.Z.; Bensouda, Y.; El Mzibri, M.; Bakri, Y.; Amrani, M. Outcome of inflammatory breast cancer in Moroccan patients: Clinical, molecular and pathological characteristics of 219 cases from the National Oncology Institute (INO). BMC Cancer 2018, 18, 713. [Google Scholar] [CrossRef]
- Manai, M.; Finetti, P.; Mejri, N.; Athimni, S.; Birnbaum, D.; Bertucci, F.; Rahal, K.; Gamoudi, A.; Chaffanet, M.; Manai, M.; et al. Inflammatory breast cancer in 210 patients: A retrospective study on epidemiological, anatomo-clinical features and therapeutic results. Mol. Clin. Oncol. 2019, 10, 223–230. [Google Scholar] [CrossRef]
- Propper, D.J.; Balkwill, F.R. Harnessing cytokines and chemokines for cancer therapy. Nat. Rev. Clin. Oncol. 2022, 19, 237–253. [Google Scholar] [CrossRef]
- Momin, N.; Mehta, N.K.; Bennett, N.R.; Ma, L.; Palmeri, J.R.; Chinn, M.M.; Lutz, E.A.; Kang, B.; Irvine, D.J.; Spranger, S.; et al. Anchoring of intratumorally administered cytokines to collagen safely potentiates systemic cancer immunotherapy. Sci. Transl. Med. 2019, 11, eaaw2614. [Google Scholar] [CrossRef]
- Momin, N.; Palmeri, J.R.; Lutz, E.A.; Jailkhani, N.; Mak, H.; Tabet, A.; Chinn, M.M.; Kang, B.H.; Spanoudaki, V.; Hynes, R.O.; et al. Maximizing response to intratumoral immunotherapy in mice by tuning local retention. Nat. Commun. 2022, 13, 109. [Google Scholar] [CrossRef]
- Torres, E.T.R.; Emens, L.A. Emerging combination immunotherapy strategies for breast cancer: Dual immune checkpoint modulation, antibody–drug conjugates and bispecific antibodies. Breast Cancer Res. Treat. 2022, 191, 291–302. [Google Scholar] [CrossRef]
- Howard, F.M.; Pearson, A.T.; Nanda, R. Clinical trials of immunotherapy in triple-negative breast cancer. Breast Cancer Res. Treat. 2022, 195, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.E.; Schmid, P. Emerging strategies for TNBC with early clinical data: New chemoimmunotherapy strategies. Breast Cancer Res. Treat. 2022, 193, 21–35. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso-Miguel, D.; Fiering, S.; Arias-Pulido, H. Proactive Immunotherapeutic Approaches against Inflammatory Breast Cancer May Improve Patient Outcomes. Cells 2022, 11, 2850. https://doi.org/10.3390/cells11182850
Alonso-Miguel D, Fiering S, Arias-Pulido H. Proactive Immunotherapeutic Approaches against Inflammatory Breast Cancer May Improve Patient Outcomes. Cells. 2022; 11(18):2850. https://doi.org/10.3390/cells11182850
Chicago/Turabian StyleAlonso-Miguel, Daniel, Steven Fiering, and Hugo Arias-Pulido. 2022. "Proactive Immunotherapeutic Approaches against Inflammatory Breast Cancer May Improve Patient Outcomes" Cells 11, no. 18: 2850. https://doi.org/10.3390/cells11182850
APA StyleAlonso-Miguel, D., Fiering, S., & Arias-Pulido, H. (2022). Proactive Immunotherapeutic Approaches against Inflammatory Breast Cancer May Improve Patient Outcomes. Cells, 11(18), 2850. https://doi.org/10.3390/cells11182850







