Differential Function of a Novel Population of the CD19+CD24hiCD38hi Bregs in Psoriasis and Multiple Myeloma
Abstract
1. Introduction
2. Materials and Methods
2.1. The Study Groups
2.2. Blood and Bone Marrow Sampling
2.3. Bregs Phenotypic Analysis and Detection of Intracellular IL-10 Production
2.4. Enzyme-Linked Immunosorbent Assay (ELISA)
2.5. Statistical Analyses
3. Results
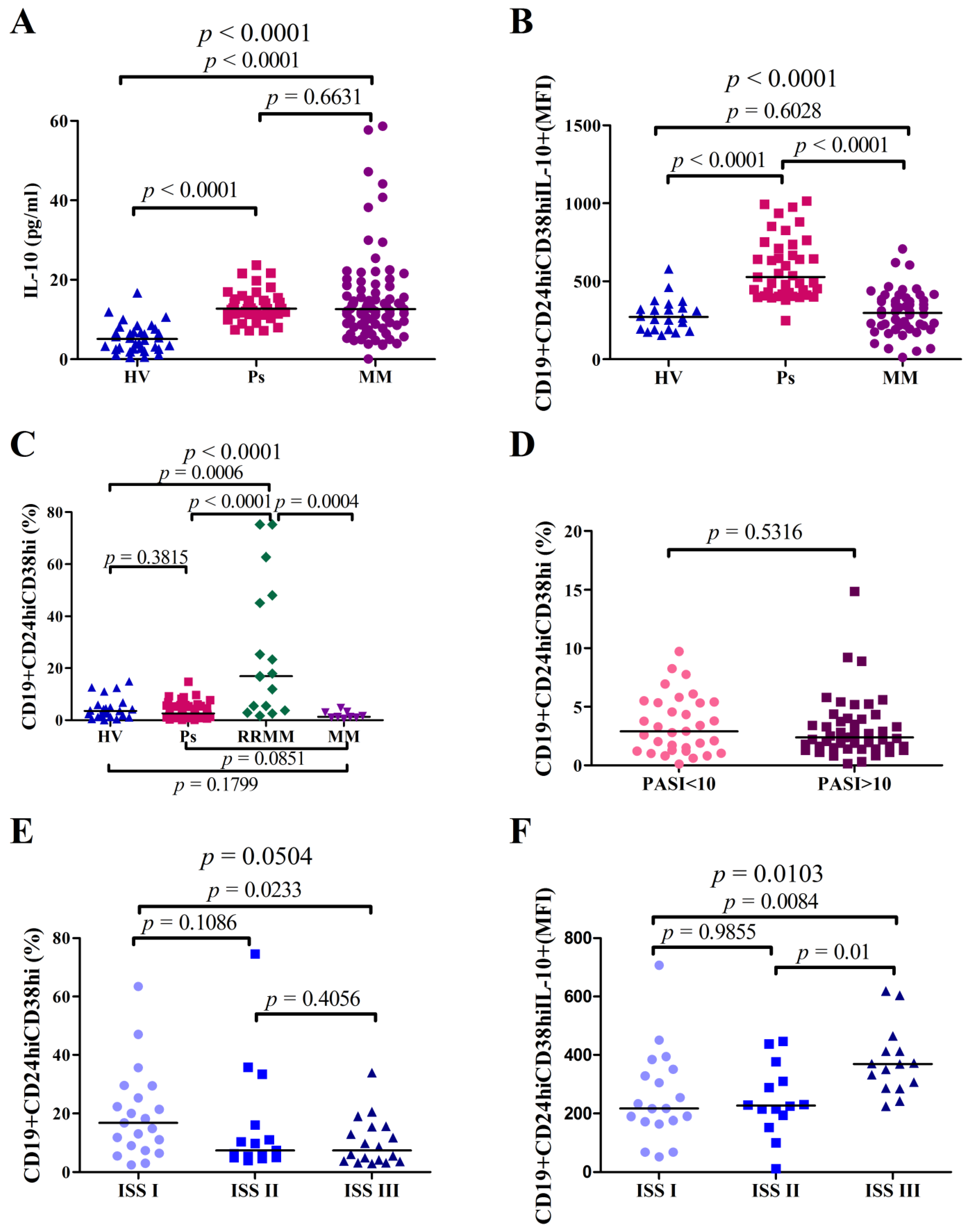
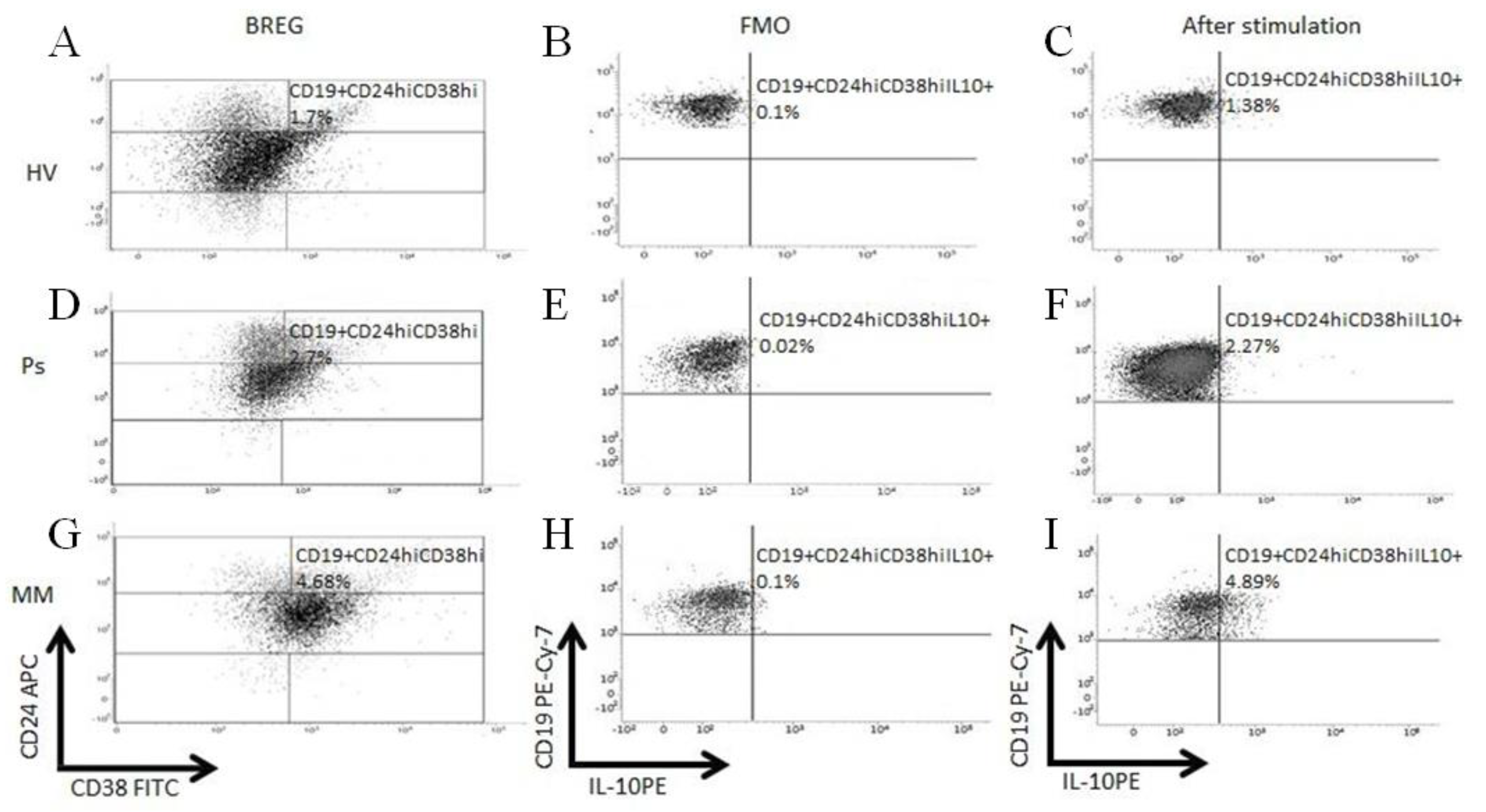
3.1. CD19+CD24hiCD38hi Bregs Are Increased in BMMCs of MM Patients, Whereas They Are Similar in PBMCs of Ps and MM Patients as Compared to HV
3.2. Higher Serum or Plasma IL-10 Concentrations in Ps Patients and MM Patients as Compared to HVs
3.3. IL-10 Production in Bregs Is Higher in Ps Patients Than in HVs and MM Patients
3.4. Correlations between the Percentage of CD19+CD24hiCD38hi Bregs and PASI in Ps Patients as well as ISS Stage in MM Patients
3.5. Decreased CD19+CD24hiCD38hi Bregs in RRMM Patients after Daratumumab Treatment
3.6. Comparison of IL-10 Plasma Concentration in RRMM Patients before and after Daratumumab Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cai, X.; Zhang, L.; Wei, W. Regulatory B cells in inflammatory diseases and tumor. Int. Immunopharmacol. 2019, 67, 281–286. [Google Scholar] [CrossRef]
- Sarvaria, A.; Madrigal, J.A.; Saudemont, A. B cell regulation in cancer and anti-tumor immunity. Cell. Mol. Immunol. 2017, 14, 662–674. [Google Scholar] [CrossRef]
- Blair, P.A.; Noreña, L.Y.; Flores-Borja, F.; Rawlings, D.J.; Isenberg, D.A.; Ehrenstein, M.R.; Mauri, C. CD19(+)CD24(hi)CD38(hi) B cells exhibit regulatory capacity in healthy individuals but are functionally impaired in systemic Lupus Erythematosus patients. Immunity 2010, 32, 129–140. [Google Scholar] [CrossRef]
- Li, T.; Yu, Z.; Qu, Z.; Zhang, N.; Crew, R.; Jiang, Y. Decreased number of CD19+CD24hiCD38hi regulatory B cells in Diabetic nephropathy. Mol. Immunol. 2019, 112, 233–239. [Google Scholar] [CrossRef]
- Berthelot, J.M.; Jamin, C.; Amrouche, K.; Le Goff, B.; Maugars, Y.; Youinou, P. Regulatory B cells play a key role in immune system balance. Jt. Bone Spine 2013, 80, 18–22. [Google Scholar] [CrossRef]
- Wu, H.; Su, Z.; Barnie, P.A. The role of B regulatory (B10) cells in inflammatory disorders and their potential as therapeutic targets. Int. Immunopharmacol. 2020, 78, 106111. [Google Scholar] [CrossRef]
- Grän, F.; Kerstan, A.; Serfling, E.; Goebeler, M.; Muhammad, K. Current Developments in the Immunology of Psoriasis. Yale J. Biol. Med. 2020, 93, 97–110. [Google Scholar] [PubMed]
- Sibaud, V. Dermatologic Reactions to Immune Checkpoint Inhibitors: Skin Toxicities and Immunotherapy. Am. J. Clin. Dermatol. 2018, 19, 345–361. [Google Scholar] [CrossRef]
- De Bock, M.; Hulstaert, E.; Kruse, V.; Brochez, L. Psoriasis Vulgaris Exacerbation during Treatment with a PD-1 Checkpoint Inhibitor: Case Report and Literature Review. Case Rep. Dermatol. 2018, 10, 190–197. [Google Scholar] [CrossRef]
- Bartosińska, J.; Zakrzewska, E.; Purkot, J.; Michalak-Stoma, A.; Kowal, M.; Krasowska, D.; Chodorowska, G.; Giannopoulos, K. Decreased blood CD4+PD-1+ and CD8+PD-1+ T cells in psoriatic patients with and without arthritis. Adv. Dermatol. Alergol. 2018, 35, 344–350. [Google Scholar] [CrossRef]
- Ruiz-Bañobre, J.; García-González, J. Anti-PD-1/PD-L1-induced psoriasis from an oncological perspective. J. Eur. Acad. Dermatol. Venereol. 2017, 31, e407–e408. [Google Scholar] [CrossRef]
- Bommarito, D.; Hall, C.; Taams, L.S.; Corrigall, V.M. Inflammatory cytokines compromise programmed cell death-1 (PD-1)-mediated T cell suppression in inflammatory arthritis through up-regulation of soluble PD-1. Clin. Exp. Immunol. 2017, 188, 455–466. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, M.; Otano, I.; Minute, L.; Ochoa, M.C.; Perez-Ruiz, E.; Melero, I.; Berraondo, P. Impact of prophylactic TNF blockade in the dual PD-1 and CTLA-4 immunotherapy efficacy and toxicity. Cell. Stress 2019, 3, 236–239. [Google Scholar] [CrossRef]
- Shah, N.; Sandigursky, S.; Mor, A. The Potential Role of Inhibitory Receptors in the Treatment of Psoriasis. Bull. Hosp. Jt. Dis. 2017, 75, 155–163. [Google Scholar]
- Mantovani, A. Molecular pathways linking inflammation and cancer. Curr. Mol. Med. 2010, 10, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Giannopoulos, K.; Kaminska, W.; Hus, I.; Dmoszynska, A. The frequency of T regulatory cells modulates the survival of multiple myeloma patients: Detailed characterisation of immune status in multiple myeloma. Br. J. Cancer 2012, 106, 546–552. [Google Scholar] [CrossRef] [PubMed]
- Tamura, H.; Ishibashi, M.; Sunakawa-Kii, M.; Inokuchi, K. PD-L1-PD-1 Pathway in the Pathophysiology of Multiple Myeloma. Cancers 2020, 12, 924. [Google Scholar] [CrossRef] [PubMed]
- Durer, C.; Durer, S.; Lee, S.; Chakraborty, R.; Malik, M.N.; Rafae, A.; Zar, M.A.; Kamal, A.; Rosko, N.; Samaras, C.; et al. Treatment of relapsed multiple myeloma: Evidence-based recommendations. Blood Rev. 2020, 39, 100616. [Google Scholar] [CrossRef] [PubMed]
- Kitadate, A.; Kobayashi, H.; Abe, Y.; Narita, K.; Miura, D.; Takeuchi, M.; Matsue, K. Pre-treatment CD38-positive regulatory T cells affect the durable response to daratumumab in relapsed/refractory multiple myeloma patients. Haematologica 2020, 105, e37–e40. [Google Scholar] [CrossRef]
- Han, J.; Sun, L.; Fan, X.; Wang, Z.; Cheng, Y.; Zhu, J.; Jin, T. Role of regulatory b cells in neuroimmunologic disorders. J. Neurosci. Res. 2016, 94, 693–701. [Google Scholar] [CrossRef]
- Hayashi, T.; Hideshima, T.; Nguyen, A.N.; Munoz, O.; Podar, K.; Hamasaki, M.; Ishitsuka, K.; Yasui, H.; Richardson, P.; Chakravarty, S.; et al. Clin Cancer Res. Transforming growth factor beta receptor I kinase inhibitor down-regulates cytokine secretion and multiple myeloma cell growth in the bone marrow microenvironment. Clin. Cancer Res. 2004, 10, 7540–7546. [Google Scholar] [CrossRef] [PubMed]
- Salomon-Perzyński, A.; Walter-Croneck, A.; Usnarska-Zubkiewicz, L.; Dytfeld, D.; Zielińska, P.; Wojciechowska, M.; Hołojda, J.; Robak, P.; Pasternak, A.; Knopińska-Posłuszny, W.; et al. Efficacy of daratumumab monotherapy in real-world heavily pretreated patients with relapsed or refractory multiple myeloma. Adv. Med. Sci. 2019, 64, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Yanaba, K.; Umezawa, Y.; Yoshihara, Y.; Kikuchi, S.; Ishiuji, Y.; Saeki, H.; Nakagawa, H. IL-10-producing regulatory B cells are decreased in patients with psoriasis. J. Dermatol. Sci. 2016, 81, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Mavropoulos, A.; Varna, A.; Zafiriou, E.; Liaskos, C.; Alexiou, I.; Roussaki-Schulze, A.; Vlychou, M.; Katsiari, C.; Bogdanos, D.P.; Sakkas, L.I. IL-10 producing Bregs are impaired in psoriatic arthritis and psoriasis and inversely correlate with IL-17- and IFNγ-producing T cells. Clin. Immunol. 2017, 184, 33–41. [Google Scholar] [CrossRef]
- Mavropoulos, A.; Zafiriou, E.; Simopoulou, T.; Brotis, A.G.; Liaskos, C.; Roussaki-Schulze, A.; Katsiari, C.G.; Bogdanos, D.P.; Sakkas, L.I. Apremilast increases IL-10-producing regulatory B cells and decreases proinflammatory T cells and innate cells in psoriatic arthritis and psoriasis. Rheumatology (Oxford) 2019, 58, 2240–2250. [Google Scholar] [CrossRef] [PubMed]
- Dass, S.; Vital, E.M.; Emery, P. Development of psoriasis after B cell depletion with rituximab. Arthritis Rheumatol. 2007, 56, 2715–2718. [Google Scholar] [CrossRef] [PubMed]
- Yanaba, K.; Kamata, M.; Ishiura, N.; Shibata, S.; Asano, Y.; Tada, Y.; Sugaya, M.; Kadono, T.; Tedder, T.F.; Sato, S. Regulatory B cells suppress imiquimod-induced, psoriasis-like skin inflammation. J. Leukoc. Biol. 2013, 94, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Inoue, S.; Leitner, W.W.; Golding, B.; Scott, D. Inhibitory effects of B cells on antitumor immunity. Cancer Res. 2006, 66, 7741–7747. [Google Scholar] [CrossRef]
- Zhang, L.; Tai, Y.T.; Ho, M.; Xing, L.; Chauhan, D.; Gang, A.; Qiu, L.; Anderson, K.C. Regulatory B cell-myeloma cell interaction confers immunosuppression and promotes their survival in the bone marrow milieu. Blood Cancer J. 2017, 7, e547. [Google Scholar] [CrossRef]
- Benjamin, D.; Park, C.D.; Sharma, V. Human B cell interleukin 10. Leuk. Lymphoma 1994, 12, 205–210. [Google Scholar] [CrossRef]
- Gabryšová, L.; Howes, A.; Saraiva, M.; O’Garra, A. The regulation of IL-10 expression. Curr. Top. Microbiol. Immunol. 2014, 380, 157–190. [Google Scholar]
- Boonpiyathad, T.; Satitsuksanoa, P.; Akdis, M.; Akdis, C.A. Il-10 producing T and B cells in allergy. Semin. Immunol. 2019, 44, 101326. [Google Scholar] [CrossRef] [PubMed]
- McInnes, I.B.; Illei, G.G.; Danning, C.L.; Yarboro, C.H.; Crane, M.; Kuroiwa, T.; Schlimgen, R.; Lee, E.; Foster, B.; Flemming, D.; et al. IL-10 improves skin disease and modulates endothelial activation and leukocyte effector function in patients with psoriatic arthritis. J. Immunol. 2001, 167, 4075–4082. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Tsuji, H.; Hashimoto, Y.; Ishida-Yamamoto, A.; Iizuka, H. Serum cytokines and growth factor levels in Japanese patients with psoriasis. Clin. Exp. Dermatol. 2010, 35, 645–649. [Google Scholar] [CrossRef]
- Jacob, S.E.; Nassiri, M.; Kerdel, F.A.; Vincek, V. Simultaneous measurement of multiple Th1 and Th2 serum cytokines in psoriasis and correlation with disease severity. Mediat. Inflamm. 2003, 12, 309–313. [Google Scholar] [CrossRef]
- Borska, L.; Andrys, C.; Krejsek, J.; Hamakova, K.; Kremlacek, J.; Ettler, K.; Fiala, Z. Serum levels of the pro-inflammatory cytokine interleukin-12 and the anti-inflammatory cytokine interleukin-10 in patients with psoriasis treated by the Goeckerman regimen. Int. J. Dermatol. 2008, 47, 800–805. [Google Scholar] [CrossRef]
- Deeva, I.; Mariani, S.; De Luca, C.; Pacifico, V.; Leoni, L.; Raskovic, D.; Kharaeva, Z.; Korkina, L.; Pastore, S. Wide-spectrum profile of inflammatory mediators in the plasma and scales of patients with psoriatic disease. Cytokine 2010, 49, 163–170. [Google Scholar] [CrossRef]
- Dowlatshahi, E.A.; van der Voort, E.A.; Arends, L.R.; Nijsten, T. Markers of systemic inflammation in psoriasis: A systematic review and meta-analysis. Br. J. Dermatol. 2013, 169, 266–282. [Google Scholar] [CrossRef] [PubMed]
- Lauta, V.M. A review of the cytokine network in multiple myeloma: Diagnostic, prognostic, and therapeutic implications. Cancer 2003, 97, 2440–2452. [Google Scholar] [CrossRef]
- Otsuki, T.; Yata, K.; Sakaguchi, H.; Uno, M.; Fujii, T.; Wada, H.; Sugihara, T.; Ueki, A. IL-10 in myeloma cells. Leuk. Lymphoma 2002, 43, 969–974. [Google Scholar] [CrossRef]
- Alexandrakis, M.G.; Goulidaki, N.; Pappa, C.A.; Boula, A.; Psarakis, F.; Neonakis, I.; Tsirakis, G. Interleukin-10 Induces Both Plasma Cell Proliferation and Angiogenesis in Multiple Myeloma. Pathol. Oncol. Res. 2015, 21, 929–934. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, E. Interleukin-6 leads to interleukin-10 production in several human multiple myeloma cell lines. Does interleukin-10 enhance the proliferation of these cells? Leuk. Res. 2010, 34, 912–916. [Google Scholar] [CrossRef]
- Wang, H.; Wang, L.; Chi, P.D.; Wang, W.D.; Chen, X.Q.; Geng, Q.R.; Xia, Z.J.; Lu, Y. High level of interleukin-10 in serum predicts poor prognosis in multiple myeloma. Br. J. Cancer 2016, 114, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Pappa, C.; Miyakis, S.; Tsirakis, G.; Sfiridaki, A.; Alegakis, A.; Kafousi, M.; Stathopoulos, E.N.; Alexandrakis, M.G. Serum levels of interleukin-15 and interleukin-10 and their correlation with proliferating cell nuclear antigen in multiple myeloma. Cytokine 2007, 37, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Moreau, P.; van de Donk, N.W.; San Miguel, J.; Lokhorst, H.; Nahi, H.; Ben-Yehuda, D.; Cavo, M.; Cook, G.; Delforge, M.; Einsele, H.; et al. Practical Considerations for the Use of Daratumumab, a Novel CD38 Monoclonal Antibody, in Myeloma. Drugs 2016, 76, 853–867. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | MM (N = 59) | RRMM (N = 17) | Ps (N = 80) | HVs (N = 23) |
|---|---|---|---|---|
| Age (years), median (range) | 68 (41–84) | 59 (47–82) | 47 (18–77) | 28 (18–58) |
| Sex | ||||
| Female, n | 26 | 12 | 14 | 10 |
| Male, n | 33 | 5 | 66 | 13 |
| ISS disease stage, n (%) | n/a | n/a | n/a | |
| I | 21 (38.9) | |||
| II | 15 (27.8) | |||
| III | 18 (33.3) | |||
| 5 n/a | ||||
| PASI, median (range) | n/a | n/a | 12.05 (2.7–49.4) | n/a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartosińska, J.; Purkot, J.; Karczmarczyk, A.; Chojnacki, M.; Zaleska, J.; Własiuk, P.; Grząśko, N.; Morawska, M.; Walter-Croneck, A.; Usnarska-Zubkiewicz, L.; et al. Differential Function of a Novel Population of the CD19+CD24hiCD38hi Bregs in Psoriasis and Multiple Myeloma. Cells 2021, 10, 411. https://doi.org/10.3390/cells10020411
Bartosińska J, Purkot J, Karczmarczyk A, Chojnacki M, Zaleska J, Własiuk P, Grząśko N, Morawska M, Walter-Croneck A, Usnarska-Zubkiewicz L, et al. Differential Function of a Novel Population of the CD19+CD24hiCD38hi Bregs in Psoriasis and Multiple Myeloma. Cells. 2021; 10(2):411. https://doi.org/10.3390/cells10020411
Chicago/Turabian StyleBartosińska, Joanna, Joanna Purkot, Agnieszka Karczmarczyk, Michał Chojnacki, Joanna Zaleska, Paulina Własiuk, Norbert Grząśko, Marta Morawska, Adam Walter-Croneck, Lidia Usnarska-Zubkiewicz, and et al. 2021. "Differential Function of a Novel Population of the CD19+CD24hiCD38hi Bregs in Psoriasis and Multiple Myeloma" Cells 10, no. 2: 411. https://doi.org/10.3390/cells10020411
APA StyleBartosińska, J., Purkot, J., Karczmarczyk, A., Chojnacki, M., Zaleska, J., Własiuk, P., Grząśko, N., Morawska, M., Walter-Croneck, A., Usnarska-Zubkiewicz, L., Zielińska, P., Jamroziak, K., Kowal, M., Krasowska, D., Chodorowska, G., & Giannopoulos, K. (2021). Differential Function of a Novel Population of the CD19+CD24hiCD38hi Bregs in Psoriasis and Multiple Myeloma. Cells, 10(2), 411. https://doi.org/10.3390/cells10020411








