Fracture Resistance of Glass-Fiber-Reinforced Direct Restorations on Endodontically Treated Molar Teeth with Furcal Perforation
Abstract
1. Introduction
2. Materials and Methods
2.1. Tooth Selection
2.2. Endodontic Treatment
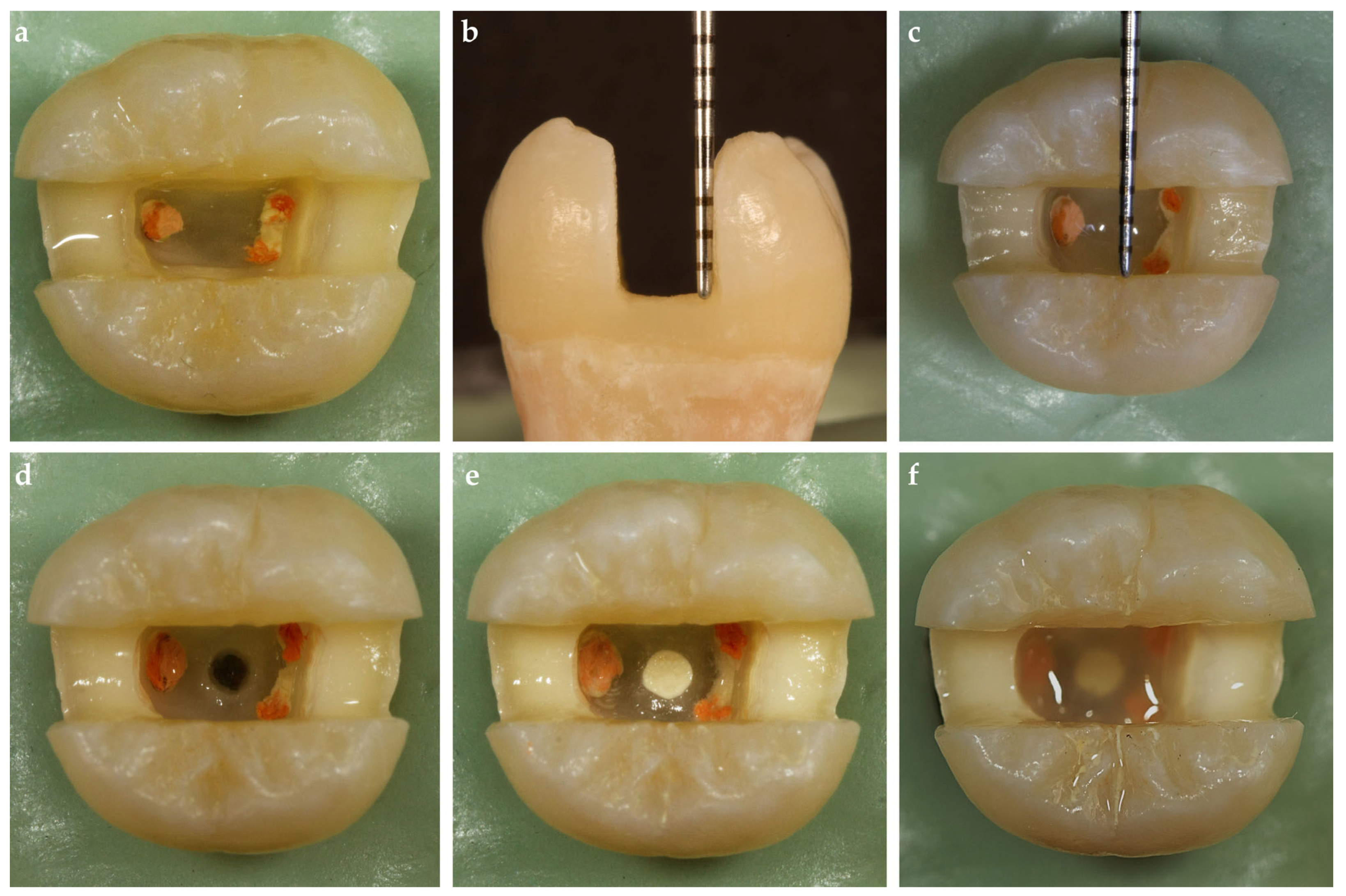
2.3. MOD Cavity Preparations
2.4. Furcal Perforation and Repair
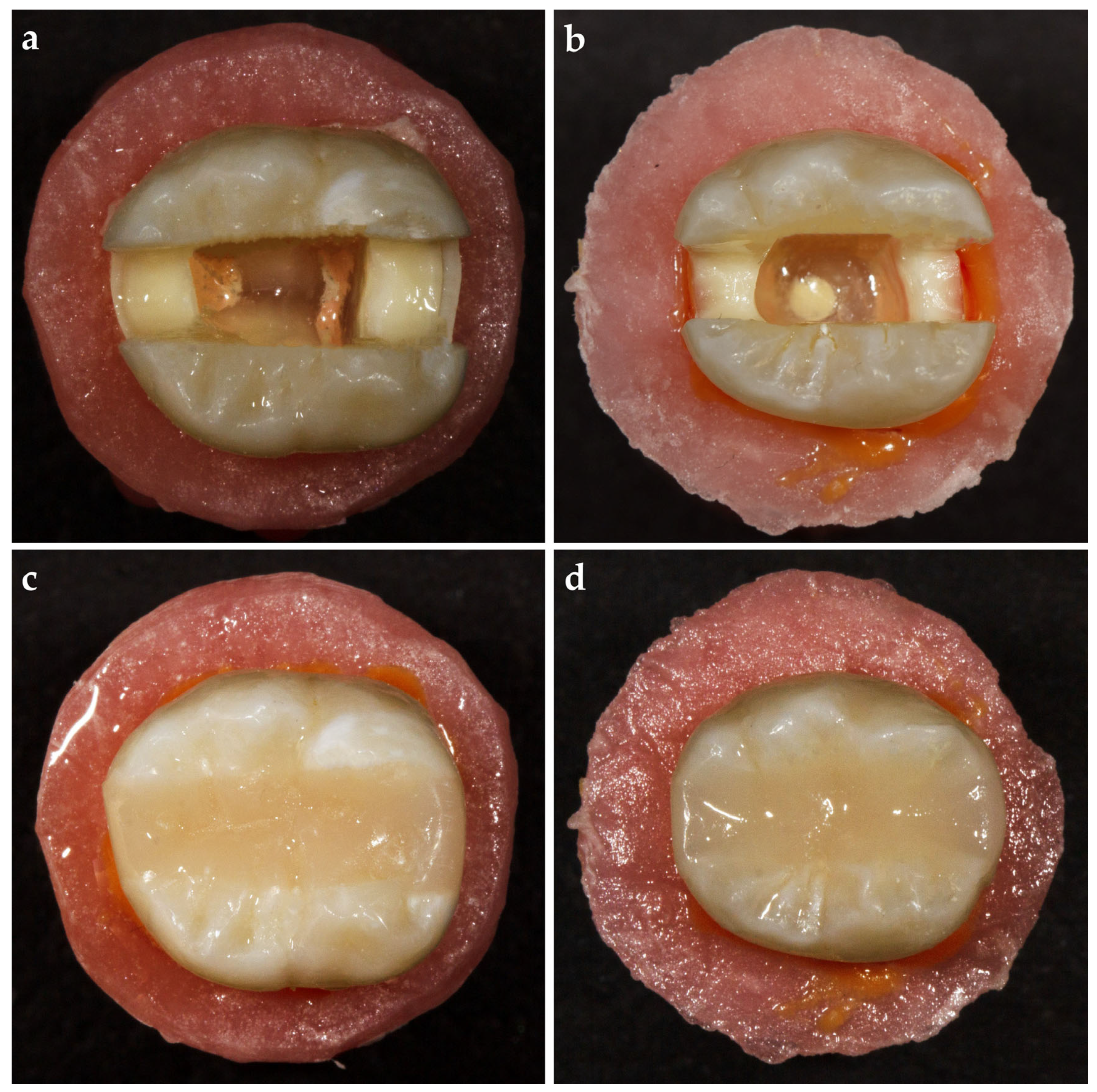
2.5. Periodontal Ligament Simulation
2.6. Adhesive Application
2.7. Control Group
2.8. Resin Composite (RC) Group
2.9. everX Flow (EXF) and everX Posterior (EXP) Groups
2.10. Modified Transfixed (MT) Group
2.11. Horizontal Glass-Fiber (HGF) Group
2.12. Bioblock (BB) Group
2.13. Fracture Resistance Test
2.14. Statistical Analyses
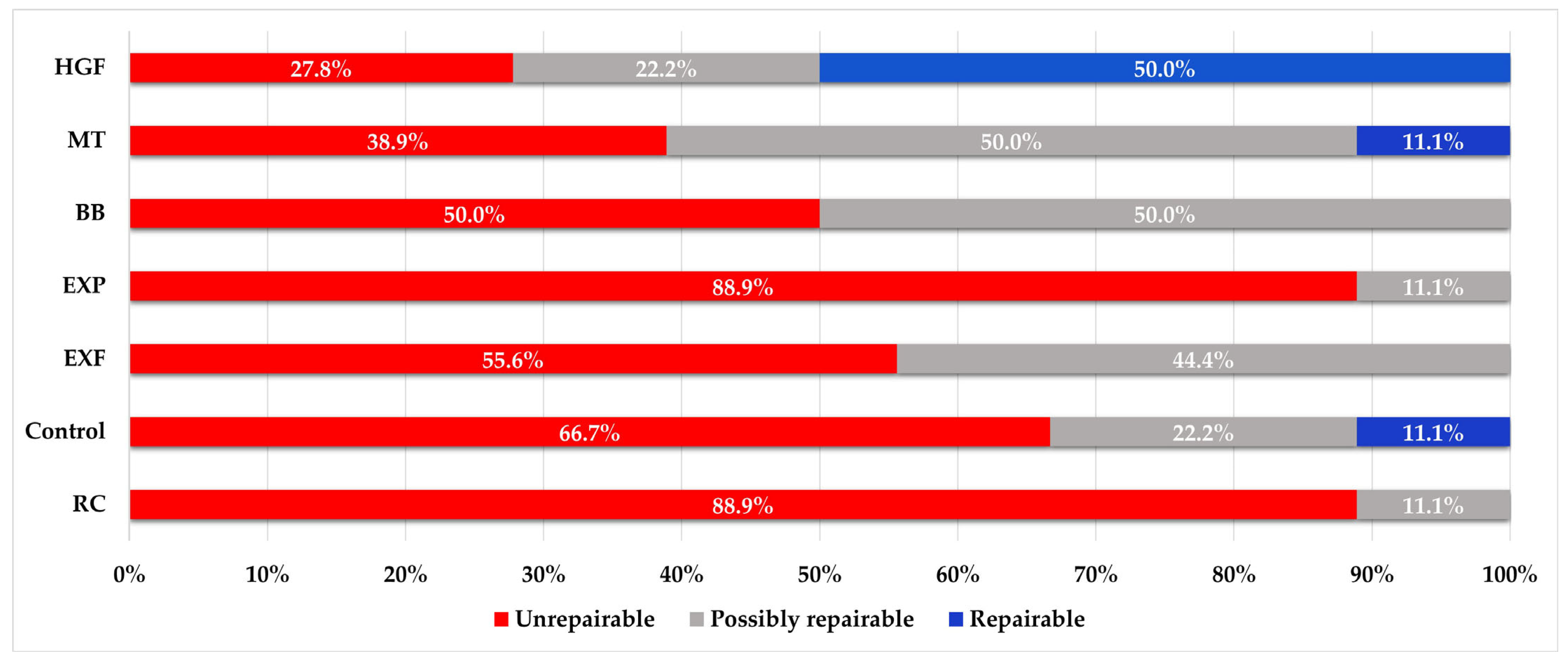
3. Results
4. Discussion
5. Conclusions
- Loss of tissue in the pericervical dentin region increases the risk of tooth fracturing.
- Direct restorations using techniques such as Bioblock, modified transfixed, horizontal glass-fiber, and dentin replacement materials including everX posterior and everX Flow can compensate for the reduction in fracture resistance caused by furcal perforation.
- The horizontal glass-fiber technique shows a superior fracture resistance, and in cases where this technique cannot be applied clinically, the modified transfixed technique using everStick C&B could offer a conservative treatment option to increase fracture resistance.
- Horizontal bonding of the buccal and lingual walls with long, continuous glass fibers improves the fracture pattern more than short-fiber reinforcement techniques.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- El-Helali, R.; Dowling, A.H.; McGinley, E.L.; Duncan, H.F.; Fleming, G.J. Influence of resin-based composite restoration technique and endodontic access on cuspal deflection and cervical microleakage scores. J. Dent. 2013, 41, 216–222. [Google Scholar] [CrossRef]
- Bromberg, C.R.; Alves, C.B.; Stona, D.; Spohr, A.M.; Rodrigues-Junior, S.A.; Melara, R.; Burnett, L.H., Jr. Fracture resistance of endodontically treated molars restored with horizontal fiberglass posts or indirect techniques. J. Am. Dent. Assoc. 2016, 147, 952–958. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Gao, Y.; Gao, Y.; Tan, X.; Zhang, L.; Huang, D. Threedimensional analysis of coronal root canal morphology of 136 permanent mandibular first molars by micro-computed tomography. J. Dent. Sci. 2022, 17, 482–489. [Google Scholar] [CrossRef]
- Krishan, R.; Paqué, F.; Ossareh, A.; Kishen, A.; Dao, T.; Friedman, S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J. Endod. 2014, 40, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Gorni, F.G.; Andreano, A.; Ambrogi, F.; Brambilla, E.; Gagliani, M. Patient and clinical characteristics associated with primary healing of iatrogenic perforations after root canal treatment: Results of a long-term Italian study. J. Endod. 2016, 42, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Askerbeyli Örs, S.; Aksel, H.; Küçükkaya Eren, S.; Serper, A. Effect of perforation size and furcal lesion on stress distribution in mandibular molars: A finite element analysis. Int. Endod. J. 2019, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Airsang, A.; Adarsha, M.S.; Meena, N.; Vikram, R.; Gowda, V.; Harti, S.A. Effect of pulpal floor perforation repair on biomechanical response of mandibular molar: A finite element analysis. J. Conserv. Dent. 2021, 24, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, Q.; Meng, X.; Ye, Y.; Feng, D.; Xue, J.; Wang, H.; Huang, H.; Wang, M.; Wang, J. Rheological and Mechanical Properties of Resin-Based Materials Applied in Dental Restorations. Polymers 2021, 13, 2975. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, I.; Otsuki, M.; Sadr, A.; Nomura, T.; Kishikawa, R.; Tagami, J. Effect of filler content of flowable composites on resin-cavity interface. Dent. Mater. J. 2009, 28, 679–685. [Google Scholar] [CrossRef]
- Dos Santos, P.H.; Catelan, A.; Albuquerque Guedes, A.P.; Umeda Suzuki, T.Y.; de Lima Godas, A.G.; Fraga Briso, A.L.; Bedran- Russo, A.K. Effect of thermocycling on roughness of nanofill, microfill and microhybrid composites. Acta Odontol. Scand. 2015, 73, 176–181. [Google Scholar] [CrossRef]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of large MOD restorations: Composite resin inlays vs. short fiber-reinforced direct restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef]
- Huang, Q.; Qin, W.; Garoushi, S.; He, J.; Lin, Z.; Liu, F.; Vallittu, P.K.; Lassila, L.V.J. Physicochemical properties of discontinuous S2-glass fiber reinforced resin composite. Dent. Mater. J. 2018, 37, 95–103. [Google Scholar] [CrossRef]
- Vallittu, P.K. High-aspect ratio fillers: Fiber-reinforced composites and their anisotropic properties. Dent. Mater. 2015, 31, 1–7. [Google Scholar] [CrossRef]
- Magne, P.; Milani, T. Short-fiber Reinforced MOD Restorations of Molars with Severely Undermined Cusps. J. Adhes. Dent. 2023, 25, 99–106. [Google Scholar] [PubMed]
- Peroz, I.; Blankenstein, F.; Lange, K.P.; Naumann, M. Restoring endodontically treated teeth with posts and cores-A review. Quintessence Int. 2005, 36, 737–746. [Google Scholar]
- Abdulrab, S.; Geerts, G.; Al-Maweri, S.A.; Alhajj, M.N.; Alhadainy, H.; Ba-Hattab, R. The influence of horizontal glass fiber posts on fracture strength and fracture pattern of endodontically treated teeth: A systematic review and meta-analysis of in vitro studies. J. Prosthodont. 2023, 32, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.G.; Kim, S.S.; Levine, J.L.; Piracha, Y.S.; Solomon, C.S. A Novel Approach to Fracture Resistance Using Horizontal Posts after Endodontic Therapy: A Case Report and Review of Literature. J. Endod. 2020, 46, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Hazar, E.; Hazar, A. Effect of Long Glass Fiber Orientations or a Short-Fiber-Reinforced Composite on the Fracture Resistance of Endodontically Treated Premolars. Polymers 2024, 16, 1289. [Google Scholar] [CrossRef] [PubMed]
- Szabó, V.T.; Szabó, B.; Barcsayné-Tátrai, N.; Mészáros, C.; Braunitzer, G.; Szabó, B.P.; Lassila, L.; Garoushi, S.; Fráter, M. Fatigue Resistance of Dissected Lower First Molars Restored with Direct Fiber-Reinforced Bridges—An In Vitro Pilot Study. Polymers 2023, 15, 1343. [Google Scholar] [CrossRef] [PubMed]
- D’Arcangelo, C.; Cinelli, M.; De Angelis, F.; D’Amario, M. Theeffect of resin cement film thickness on the pullout strengthof a fiber-reinforced post system. J. Prosthet. Dent. 2007, 98, 193–198. [Google Scholar] [CrossRef]
- Fráter, M.; Lassila, L.; Braunitzer, G.; Vallittu, P.K.; Garoushi, S. Fracture resistance and marginal gap formation of post-corerestorations: Influence of different fiber-reinforcedcomposites. Clin. Oral Investig. 2020, 24, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Hazar, A.; Hazar, E. Effect of composite resins with and without fiber-reinforcement on the fracture resistance of teeth with non-carious cervical lesions. J. Appl. Biomater. Funct. Mater. 2024, 22, 22808000241303327. [Google Scholar] [CrossRef] [PubMed]
- Hofsteenge, J.W.; Scholtanus, J.D.; Özcan, M.; Nolte, I.M.; Cune, M.S.; Gresnigt, M.M.M. Clinical longevity of extensive direct resin composite restorations after amalgam replacement with a mean follow-up of 15 years. J. Dent. 2023, 130, 104409. [Google Scholar] [CrossRef]
- Alshehri, M.M.; Alhawsawi, B.F.; Alghamdi, A.; Aldobaikhi, S.O.; Alanazi, M.H.; Alahmad, F.A. The Management of Root Perforation: A Review of the Literature. Cureus 2024, 16, e72296. [Google Scholar] [CrossRef]
- Majeed, R.; Elnawawy, H.M.; Kutty, M.G.; Yahya, N.A.; Azami, N.H.; Abu Kasim, N.H.; Nabhan, M.S.; Cooper, P.R.; Camilleri, J.; Ahmed, H.M.A. Physicochemical, mechanical and biological properties of nano-calcium silicate-based cements: A systematic review. Odontology 2023, 111, 759–776. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, L.S.; Kopper, P.M.P.; Quintana, R.M.; Scarparo, R.K.; Grecca, F.S. Does MTA provide a more favourable histological response than other materials in the repair of furcal perforations? A systematic review. Int. Endod. J. 2021, 54, 2195–2218. [Google Scholar] [CrossRef]
- Mangoush, E.; Garoushi, S.; Lassila, L.; Vallittu, P.K.; Säilynoja, E. Effect of Fiber Reinforcement Type on the Performance of Large Posterior Restorations: A Review of In Vitro Studies. Polymers 2021, 13, 3682. [Google Scholar] [CrossRef]
- Selvaraj, H.; Krithikadatta, J.; Shrivastava, D.; Onazi, M.A.A.; Algarni, H.A.; Munaga, S.; Hamza, M.O.; Saad Al-Fridy, T.; Teja, K.V.; Janani, K.; et al. Systematic review fracture resistance of endodontically treated posterior teeth restored with fiber reinforced composites- a systematic review. BMC Oral Health 2023, 23, 566. [Google Scholar] [CrossRef] [PubMed]
- Demarco, F.F.; Corrêa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Keulemans, F.; Säilynoja, E.; Vallittu, P.K.; Garoushi, S. Mechanical properties and fracture behavior of flowable fiber reinforced composite restorations. Dent. Mater. 2018, 34, 598–606. [Google Scholar] [CrossRef]
- Lassila, L.; Keulemans, F.; Vallittu, P.K.; Garoushi, S. Characterization of restorative short-fiber reinforced dental composites. Dent. Mater. J. 2020, 39, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Ranka, S.; Rao, A.S.; Shah, U.; Solanki, D.; Pawar, A.M.; Reda, R.; Zanza, A.; Testarelli, L. Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars-A Randomized Clinical Study. Materials 2022, 15, 7858. [Google Scholar] [CrossRef] [PubMed]
- Borges, K.T.; Servín, M.P.M.; França, F.M.G.; Turssi, C.P.; Basting, R.T.; Hirata, R.; Vieira-Junior, W.F. Influence of viscosity and fiber reinforcement of resin composite on fracture strength and failure mode of restored molars. J. Esthet. Restor. Dent. 2024, 36, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Sáry, T.; Jókai, B.; Braunitzer, G.; Säilynoja, E.; Vallittu, P.K.; Lassila, L.; Garoushi, S. Fatigue behavior of endodontically treated premolars restored with different fiber-reinforced designs. Dent. Mater. 2021, 37, 391–402. [Google Scholar] [CrossRef]
- Kamourieh, N.; Faigenblum, M.; Blizard, R.; Leung, A.; Fine, P. Fracture Toughness of Short Fibre-Reinforced Composites-In Vitro Study. Materials 2024, 17, 5368. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Carvalho, M.A.; Milani, T. Shrinkage-induced cuspal deformation and strength of three different short fiber-reinforced composite resins. J. Esthet. Restor. Dent. 2023, 35, 56–63. [Google Scholar] [CrossRef]
- Le Bell-Rönnlöf, A.M.; Lassila, L.V.; Kangasniemi, I.; Vallittu, P.K. Load-bearing capacity of human incisor restored with various fiber-reinforced composite posts. Dent. Mater. 2011, 27, e107–e115. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Sáry, T.; Néma, V.; Braunitzer, G.; Vallittu, P.; Lassila, L.; Garoushi, S. Fatigue failure load of immature anterior teeth: Influence of different fiber post-core systems. Odontology 2021, 109, 222–230. [Google Scholar] [CrossRef]
- Bijelic, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Short fiber reinforced composite in restoring severely damaged incisors. Acta Odontol. Scand. 2013, 71, 1221–1231. [Google Scholar] [CrossRef]
- Jain, A.; Shah, N.C.; Kumar, M.; Ishwar, S.; Purkayastha, D.D.; Mishra, D.; Shanbhag, A. Stress distribution pattern in two different no-post systems in endodontically treated maxillary central incisors: A three-dimensional finite element analysis. J. Conserv. Dent. Endod. 2024, 27, 572–576. [Google Scholar] [CrossRef]
- Abou-Elnaga, M.Y.; Alkhawas, M.A.M.; Kim, H.C.; Refai, A.S. Effect of Truss Access and Artificial Truss Restoration on the Fracture Resistance of Endodontically Treated Mandibular First Molars. J. Endod. 2019, 45, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Burke, F.J. Tooth fracture in vivo and in vitro. J. Dent. 1992, 20, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Su, J.N.; Pan, Y.H.; Dorj, O.; Lin, J.C.; Salamanca, E.; Chen, I.W.; Wu, Y.F.; Chang, W.J. Association between oral health status and occlusal bite force in young adults. J. Dent. Sci. 2024, 19, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Tahoury, B.; Takeshita, L.; Moreira, Y.M.; Pavan, J.S.R.; Leles, C.R. Correlates and Comparability of Two Devices for Measuring Bite Force in Dentate Health Volunteers. J. Oral Rehabil. 2024; Epub ahead of print. [Google Scholar]
- Patil, D.B.; Reddy, E.R.; Rani, S.T.; Kadge, S.S.; Patil, S.D.; Madki, P. Evaluation of stress in three different fiber posts with two-dimensional finite element analysis. J. Indian Soc. Pedod. Prev. Dent. 2021, 39, 178–182. [Google Scholar] [CrossRef] [PubMed]




| Material | Manufacturer | Fillers | Matrix |
|---|---|---|---|
| G-aenial Universal Injectable, flowable composite | GC Corporation, Tokyo, Japan (Lot number: 2205201) | Silicon dioxide (SiO2), barium glass, 69 wt%, 50 vol% | UDMA, Bis-MEPP, TEGDMA |
| everX Flow™, flowable short fiber reinforced composite | GC Corporation, Tokyo, Japan (Lot number: 2106221) | Micrometer scale glass fiber filler, barium glass, 70 wt%, 46 vol% | Bis-EMA, TEGDMA, UDMA |
| everX Posterior™, short fiber reinforced composite | GC Corporation, Tokyo, Japan (Lot number: 2308071) | Shot E-glass fiber filler, Barium glass 74.2 wt%, 53.6 vol% | Bis-GMA, PMMA, TEGDMA |
| everStick®C&B fibers | GC Corporation, Tokyo, Japan (Lot number: 2212192) | Silanated, unidirectional glass fibers | PMMA, Bis-GMA |
| Scotchbond Universal Plus Adhesive | 3M Deutschland GmbH, Neuss, Germany (Lot number: 10665120) | Bis-GMA, 10-MDP, 2-HEMA, Vitrebond copolymer, ethanol, water, initiators, fillers | |
| Biodentine™ | Septodont®, St. Maur-des-Fossés, France (Lot number: B31840) | Cement composition: tricalcium silicate (Ca3SiO5), dicalcium silicate (Ca2SiO4), zirconium oxide (ZrO2), calcium carbonate (CaCO3) Liquid composition: hydrosoluble polymer (polycarboxylate), calcium chloride (CaCl2), water | |
| Study Group | Representative Group Name | Furcal Perforation | Applied Material | Restoration Technique |
|---|---|---|---|---|
| Control | Control | No | G-aenial Universal Injectable | Injectable composite resin without fiber reinforcement—incremental technique |
| Resin composite | RC | Yes | G-aenial Universal Injectable | Injectable composite resin without fiber reinforcement—incremental technique |
| everX Flow | EXF | Yes | everX Flow™+ G-aenial Universal Injectable | Dentin replacement with flowable SFRC—bulk technique |
| everX Posterior | EXP | Yes | everX Posterior™+ G-aenial Universal Injectable | Dentin replacement with packable SFRC—bulk technique |
| Bioblock | BB | Yes | Everx flow+ G-aenial Universal Injectable | Radicular retention and dentin replacement with flowable SFRC—bulk technique |
| Modified transfixed | MT | Yes | everStick®C&B fibers + G-aenial Universal Injectable | Coronal, horizontal long glass-fiber application/ injectable composite resin without fiber reinforcement—incremental technique |
| Horizontal glass-fiber | HGF | Yes | X-Post + G-aenial Universal Injectable | Coronal, horizontal long glass-fiber application/ injectable composite resin without fiber reinforcement—incremental technique |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hazar, E.; Hazar, A. Fracture Resistance of Glass-Fiber-Reinforced Direct Restorations on Endodontically Treated Molar Teeth with Furcal Perforation. Polymers 2025, 17, 370. https://doi.org/10.3390/polym17030370
Hazar E, Hazar A. Fracture Resistance of Glass-Fiber-Reinforced Direct Restorations on Endodontically Treated Molar Teeth with Furcal Perforation. Polymers. 2025; 17(3):370. https://doi.org/10.3390/polym17030370
Chicago/Turabian StyleHazar, Ecehan, and Ahmet Hazar. 2025. "Fracture Resistance of Glass-Fiber-Reinforced Direct Restorations on Endodontically Treated Molar Teeth with Furcal Perforation" Polymers 17, no. 3: 370. https://doi.org/10.3390/polym17030370
APA StyleHazar, E., & Hazar, A. (2025). Fracture Resistance of Glass-Fiber-Reinforced Direct Restorations on Endodontically Treated Molar Teeth with Furcal Perforation. Polymers, 17(3), 370. https://doi.org/10.3390/polym17030370






