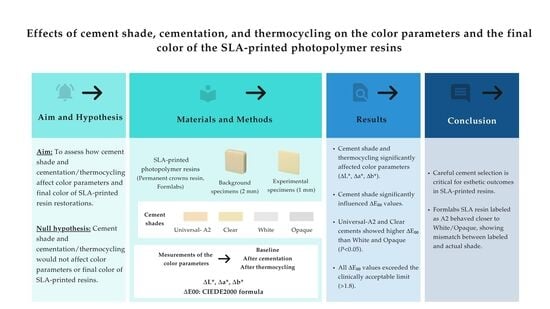
Effects of Cement Shade, Cementation, and Thermocycling on the Color Parameters and the Final Color of the SLA-Printed Photopolymer Resins †
Abstract
1. Introduction
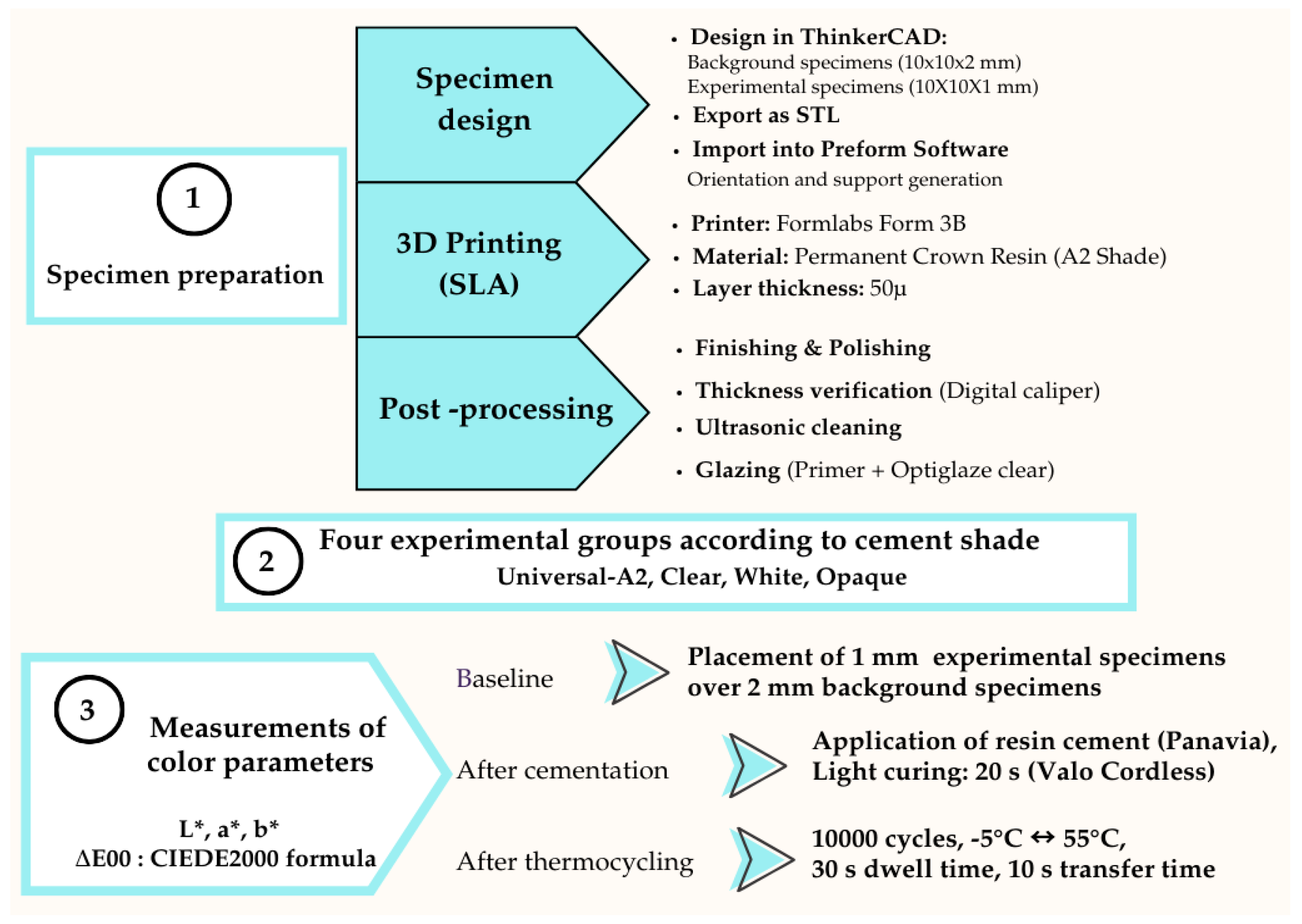
2. Materials and Methods
2.1. Sample Size Calculation and Study Design
2.2. Specimen Preparation
2.3. Thermocycling Procedure
2.4. Measurements of the Color Parameters
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3D | Three-Dimensional |
| AM | Additive Manufacturing |
| CAD-CAM | Computer-Aided Design—Computer-Aided Manufacturing |
| DLP | Digital Light Processing |
| LCD | Liquid Crystal Display |
| SLA | Stereolithography |
| STL | Standard Tessellation Language |
References
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef]
- Mandurino, M.; Cortili, S.; Coccoluto, L.; Greco, K.; Cantatore, G.; Gherlone, E.F.; Vichi, A.; Paolone, G. Mechanical Properties of 3D Printed vs. Subtractively Manufactured Composite Resins for Permanent Restorations: A Systematic Review. Materials 2025, 18, 985. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef]
- Di Fiore, A.; Stellini, E.; Alageel, O.; Alhotan, A. Comparison of Mechanical and Surface Properties of Two 3D Printed Composite Resins for Definitive Restoration. J. Prosthet. Dent. 2024, 132, 839.e1–839.e7. [Google Scholar] [CrossRef]
- Pot, G.J.; Van Overschelde, P.A.; Keulemans, F.; Kleverlaan, C.J.; Tribst, J.P.M. Mechanical Properties of Additive-Manufactured Composite-Based Resins for Permanent Indirect Restorations: A Scoping Review. Materials 2024, 17, 3951. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kwon, J.-S.; Park, J.-M.; Russo, L.L.; Shim, J.-S. Effects of Postpolymerization Conditions on the Physical Properties, Cytotoxicity, and Dimensional Accuracy of a 3D-Printed Dental Restorative Material. J. Prosthet. Dent. 2024, 132, 241–250. [Google Scholar] [CrossRef]
- Turker Kader, I.; Ozer, S.; Arican, B. An In Vitro Analysis of Marginal and Internal Fit of 3D-Printed Permanent Molar Endocrowns with Different Preparation Designs. Clin. Oral Investig. 2025, 29, 319. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.; Kang, Y.-J.; Kim, H.; Kim, J.-H. Effect of Cement Space Settings on the Marginal and Internal Fit of 3D Printed Definitive Resin Crowns. J. Prosthet. Dent. 2025, 133, 821–826. [Google Scholar] [CrossRef]
- Prakash, J.; Shenoy, M.; Alhasmi, A.; Al Saleh, A.A.; Shivakumar, S.; Alsaleh, A.A., Jr. Biocompatibility of 3D-Printed Dental Resins: A Systematic Review. Cureus 2024, 16, 51721. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Cameron, A.B.; Choi, J.J.E. The Effect of Cement Shade on the Optical Properties of Additively Manufactured Permanent Crown Materials. J. Esthet. Restor. Dent. 2025, 37, 1930–1939. [Google Scholar] [CrossRef] [PubMed]
- Pérez, M.M.; Espinar, C.; Pecho, O.E.; Tejada-Casado, M.; Della Bona, A. Effect of Aging on Optical Behavior and Color of 3D Printing Resin-Based Dental Restorative Materials. J. Dent. 2025, 157, 105734. [Google Scholar] [CrossRef] [PubMed]
- Espinar, C.; Della Bona, A.; Tejada-Casado, M.; Pulgar, R.; Perez, M.M. Optical Behavior of 3D-Printed Dental Restorative Resins: Influence of Thickness and Printing Angle. Dent. Mater. 2023, 39, 894–902. [Google Scholar] [CrossRef]
- Lee, E.-H.; Ahn, J.-S.; Lim, Y.-J.; Kwon, H.-B.; Kim, M.-J. Effect of Layer Thickness and Printing Orientation on the Color Stability and Stainability of a 3D-Printed Resin Material. J. Prosthet. Dent. 2022, 127, 784.e1–784.e7. [Google Scholar] [CrossRef]
- Sasany, R.; Jamjoon, F.Z.; Kendirci, M.Y.; Yilmaz, B. Effect of Printing Layer Thickness on Optical Properties and Surface Roughness of 3D-Printed Resins: An In Vitro Study. Int. J. Prosthodont. 2024, 37, 165–173. [Google Scholar] [CrossRef]
- Yüceer, Ö.M.; Kaynak Öztürk, E.; Çiçek, E.S.; Aktaş, N.; Bankoğlu Güngör, M. Three-Dimensional-Printed Photopolymer Resin Materials: A Narrative Review on Their Production Techniques and Applications in Dentistry. Polymers 2025, 17, 316. [Google Scholar] [CrossRef]
- Stefaniak, A.B.; Brusak, E.D.; Robinson, S.; Bowers, L.N.; Roemer, M.; Matheson, J.; Virji, M.A. Influence of Resin Color and Printer Brand on Emissions from Stereolithography (SLA) 3-D printers. ACS Chem. Health Saf. 2025, 32, 504–512. [Google Scholar] [CrossRef]
- Gad, M.M.; Al Mahfoudh, H.A.; Al Mahfuth, F.A.; Hashim, K.A.; Khan, S.Q.; Al-Qarni, F.D.; Baba, N.Z.; Al-Harbi, F.A. A Comparative Study of Strength and Surface Properties of Permanent 3D-Printed Resins with CAD-CAM Milled Fixed Dental Prostheses. J. Prosthodont. 2024, in press. [Google Scholar] [CrossRef]
- Espinar, C.; Della Bona, A.; Pérez, M.M.; Pulgar, R. Color and Optical Properties of 3D Printing Restorative Polymer-Based Materials: A Scoping Review. J. Esthet. Restor. Dent. 2022, 34, 853–864. [Google Scholar] [CrossRef]
- Del Hougne, M.; Di Lorenzo, I.; Höhne, C.; Schmitter, M. A Retrospective Cohort Study on 3D Printed Temporary Crowns. Sci. Rep. 2024, 14, 17295. [Google Scholar] [CrossRef]
- Ozdogan, A.; Erdas, G.; Gulmez, O.; Karatas, F. Color Matching between Resin Cements and Try-in Pastes in Glass Ceramics at Different Thicknesses. J. Adv. Oral Res. 2024, 15, 30–38. [Google Scholar] [CrossRef]
- Vichi, A.; Ferrari, M.; Davidson, C.L. Influence of Ceramic and Cement Thickness on the Masking of Various Types of Opaque Posts. J. Prosthet. Dent. 2000, 83, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Azer, S.S.; Ayash, G.M.; Johnston, W.M.; Khalil, M.F.; Rosenstiel, S.F. Effect of Esthetic Core Shades on the Final Color of IPS Empress All-Ceramic Crowns. J. Prosthet. Dent. 2006, 96, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Karaagaclioglu, L.; Yilmaz, B. Influence of Cement Shade and Water Storage on the Final Color of Leucite-Reinforced Ceramics. Oper. Dent. 2008, 33, 386–391. [Google Scholar] [CrossRef]
- Chang, J.; Da Silva, J.D.; Sakai, M.; Kristiansen, J.; Ishikawa-Nagai, S. The Optical Effect of Composite Luting Cement on All Ceramic Crowns. J. Dent. 2009, 37, 937–943. [Google Scholar] [CrossRef]
- Chaiyabutr, Y.; Kois, J.C.; LeBeau, D.; Nunokawa, G. Effect of Abutment Tooth Color, Cement Color, and Ceramic Thickness on the Resulting Optical Color of a CAD/CAM Glass-Ceramic Lithium Disilicate-Reinforced Crown. J. Prosthet. Dent. 2011, 105, 83–90. [Google Scholar] [CrossRef]
- Turgut, S.; Bagis, B.; Ayaz, E.A. Achieving the Desired Colour in Discoloured Teeth, Using Leucite-Based CAD-CAM Laminate Systems. J. Dent. 2014, 42, 68–74. [Google Scholar] [CrossRef]
- Al-Ameri, A.; Alothman, O.Y.; Alsadon, O.; Bangalore, D. An In-Vitro Evaluation of Strength, Hardness, and Color Stability of Heat-Polymerized and 3D-Printed Denture Base Polymers After Aging. Polymers 2025, 17, 288. [Google Scholar] [CrossRef]
- Izzettinoglu, E.; Eroglu, E. Evaluation of Mechanical Properties and Color Stability of 3D-Printed Denture Base Materials Following Two Surface Treatments. BMC Oral Health 2025, 25, 671. [Google Scholar] [CrossRef]
- Temizci, T.; Kölüş, T. Effects of Printing Angle and Post-Curing Time on the Color and Translucency of 3D-Printed Temporary Restoration. Biomimetics 2024, 9, 420. [Google Scholar] [CrossRef]
- Gale, M.; Darvell, B. Thermal Cycling Procedures for Laboratory Testing of Dental Restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Durmus, D. CIELAB Color Space Boundaries under Theoretical Spectra and 99 Test Color Samples. Color Res. Appl. 2020, 45, 796–802. [Google Scholar] [CrossRef]
- Paravina, R.D.; Ghinea, R.; Herrera, L.J.; Bona, A.D.; Igiel, C.; Linninger, M.; Sakai, M.; Takahashi, H.; Tashkandi, E.; Perez, M.d.M. Color Difference Thresholds in Dentistry. J. Esthet. Restor. Dent. 2015, 27, S1–S9. [Google Scholar] [CrossRef]
- Albrecht, M.; Schmidt, F.; Menzel, F.; Yassine, J.; Beuer, F.; Unkovskiy, A. Comparative Analysis of Modern 3D-Printed Hybrid Resin-Ceramic Materials for Indirect Restorations: An In Vitro Study. Polymers 2024, 16, 3161. [Google Scholar] [CrossRef]
- Hashemzade, Z.; Alihemmati, M.; Hakimaneh, S.M.R.; Shayegh, S.S.; Bafandeh, M.A.; Mohammadi, Z. Comparison of Color Stability and Surface Roughness of Interim Crowns Fabricated by Conventional, Milling and 3D Printing Methods. Clin. Exp. Dent. Res. 2025, 11, e70119. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Oosterveen-Rüegsegger, A.L.; Akay, C.; Schimmel, M.; Yilmaz, B.; Donmez, M.B. Influence of Polishing Technique and Coffee Thermal Cycling on the Surface Roughness and Color Stability of Additively and Subtractively Manufactured Resins Used for Definitive Restorations. J. Prosthodont. 2024, 33, 467–474. [Google Scholar] [CrossRef]
- Nam, N.-E.; Hwangbo, N.-K.; Kim, J.-E. Effects of Surface Glazing on the Mechanical and Biological Properties of 3D Printed Permanent Dental Resin Materials. J. Prosthodont. Res. 2024, 68, 273–282. [Google Scholar] [CrossRef]
- Rojas-Rueda, S.; Alsahafi, T.A.; Hammamy, M.; Surathu, N.; Surathu, N.; Lawson, N.C.; Sulaiman, T.A. Roughness and Gloss of 3D-Printed Crowns Following Polishing or Varnish Application. Materials 2025, 18, 3308. [Google Scholar] [CrossRef]
- Lask, M.; Mayinger, F.; Reymus, M.; Meinen, J.; Stawarczyk, B. Impact of Glazing, Coating, and Polishing on the Color Stability and Surface Properties of a 3D Printed Resin and Two Veneering Composite Resins. J. Esthet. Restor. Dent. 2025, 37, 1814–1826. [Google Scholar] [CrossRef]
- Almejrad, L.; Yang, C.C.; Morton, D.; Lin, W.S. The Effects of Beverages and Surface Treatments on the Color Stability of 3D-Printed Interim Restorations. J. Prosthodont. 2022, 31, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and Perceptibility Thresholds in Dentistry: A Comprehensive Review of Clinical and Research Applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Aydoğdu, H.M.; Yıldız, P.; Ünlü, D.G. A Comparative Study of Translucency and Color Perception in Monolithic Zirconia and Lithium Disilicate Veneers. Heliyon 2024, 10, e23789. [Google Scholar] [CrossRef]
- Porojan, L.; Toma, F.R.; Uțu, I.-D.; Vasiliu, R.D. Optical Behavior and Surface Analysis of Dental Resin Matrix Ceramics Related to Thermocycling and Finishing. Appl. Sci. 2022, 12, 4346. [Google Scholar] [CrossRef]
- Taşın, S.; Ismatullaev, A. Effect of Coffee Thermocycling on the Color and Translucency of Milled and 3D Printed Definitive Restoration Materials. J. Prosthet. Dent. 2024, 131, 969.e1–969.e7. [Google Scholar] [CrossRef]
- De Oliveira, D.C.R.S.; Ayres, A.P.A.; Rocha, M.G.; Giannini, M.; Puppin Rontani, R.M.; Ferracane, J.L.; Sinhoreti, M.A.C. Effect of Different In Vitro Aging Methods on Color Stability of a Dental Resin-Based Composite Using CIELAB and CIEDE2000 Color-Difference Formulas. J. Esthet. Restor. Dent. 2015, 27, 322–330. [Google Scholar] [CrossRef]
- Lindsey, D.T.; Wee, A.G. Perceptibility and Acceptability of CIELAB Color Differences in Computer-Simulated Teeth. J. Dent. 2007, 35, 593–599. [Google Scholar] [CrossRef]
- Günal-Abduljalil, B.; Ulusoy, M.M. The Effect of Resin Cement Shade and Restorative Material Type and Thickness on the Final Color of Resin-Matrix Ceramics. J. Prosthodont. Res. 2022, 66, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Atay, A.; Palazli, Z.; Gürdal, İ.; Üşümez, A. Color Change of Different Dual-Cure Resin Cements After Thermocycling. Odovtos-Int. J. Dent. Sci. 2019, 21, 53–62. [Google Scholar] [CrossRef]
- Mahn, E.; Tortora, S.C.; Olate, B.; Cacciuttolo, F.; Kernitsky, J.; Jorquera, G. Comparison of Visual Analog Shade Matching, a Digital Visual Method with a Cross-Polarized Light Filter, and a Spectrophotometer for Dental Color Matching. J. Prosthet. Dent. 2021, 125, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Philippi, A.; Sabatini, G.; Freitas, M.; Oshima, S.; Tango, R.; Gonçalves, T. Clinical Tooth Color Matching: In Vivo Comparisons of Digital Photocolorimetric and Spectrophotometric Analyses. Oper. Dent. 2023, 48, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, M.J.; Gómez-Polo, M.; Gómez-Polo, C.; Celemin-Viñuela, A. Study of Attached Gingiva Space Color According to Gender and Age in Caucasian Population. J. Esthet. Restor. Dent. 2023, 35, 834–841. [Google Scholar] [CrossRef]
- Yamalı, Y.; Güngör, M.B.; Nemli, S.K.; Bal, B.T. The Effects of Cement Thickness and Cement Shade on the Final Color of Lithium Disilicate Crowns. J. Adv. Prosthodont. 2023, 15, 93. [Google Scholar] [CrossRef] [PubMed]
- Bozoğulları, H.N.; Temizci, T. Evaluation of the Color Stability, Stainability, and Surface Roughness of Permanent Composite-Based Milled and 3D-Printed CAD/CAM Restorative Materials After Thermocycling. Appl. Sci. 2023, 13, 11895. [Google Scholar] [CrossRef]
- Karaoğlanoğlu, S.; Aydın, N.; Oktay, E.; Ersöz, B. Comparison of the Surface Properties of 3D-Printed Permanent Restorative Resins and Resin-Based CAD/CAM Blocks. Oper. Dent. 2023, 48, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Kaynak Öztürk, E.; Yılmaz Biçer, E.; Güney, B.; Saygılı, S.; Aktaş, N.; Bankoğlu Güngör, M. Effects of Cement Shade, Cementation, and Thermocycling on the Color Parameters and the Final Color of the SLA-Printed Photopolymer Resins. In Proceedings of the 29th International Congress of Esthetic Dentistry, İstanbul, Türkiye, 16–18 October 2025; OP-09. Available online: https://www.edad2025.org/files/Bildiri-Kitabi.pdf?t=001 (accessed on 18 October 2025).


| Material | Printing Technology | Manufacturer | Printing Parameters | Composition | Applications |
|---|---|---|---|---|---|
| Permanent Crown Resin | Stereolithography (SLA) | Formlabs, Somerville, MA, USA | Layer thickness: 50 μm Printing orientation: 90° | Organic Matrix: 50–<75% wt. Bis-EMA Esterification products of 4.4′-isopropylidiphenol, ethoxylated, and 2-methylprop-2enoic acid. Silanized dental glass, methyl benzoylformate, diphenyl [2,4,6-trimethylbenzoyl] phosphine oxide. Inorganic Filler: Silanized dental glass (particle size 0.7 μm) (30–50% wt.) | Permanent single crowns inlays onlays veneers |
| Cement Shade | Application | |
|---|---|---|
| Cementation (ΔL*-1) Mean (±SD) n = 10 | Thermocycling (ΔL*-2) Mean (±SD) n = 10 | |
| universal-A2 | −3.61 (±1.67) C, b | −1.92 (±1.61) B, a |
| clear | −3.97 (±0.55) C, b | −1.21 (±0.76) B, a |
| white | −2.50 (±0.79) B, b | 1.00 (±0.39) A, a |
| opaque | 1.43 (±0.83) A, a | 1.30 (±0.81) A, a |
| Cement Shade | Application | |
|---|---|---|
| Cementation (Δa*-1) Mean (±SD) n = 10 | Thermocycling (Δa*-2) Mean (±SD) n = 10 | |
| universal-A2 | 1.20 (±0.86) A, a | −1.36 (±0.66) B, b |
| clear | 0.83 (±0.48) A, a | −1.39 (±0.44) B, b |
| white | −1.03 (±0.21) B, b | −0.32 (±0.13) A, a |
| opaque | −1.23 (±0.25) B, b | −0.25 (±0.2) A, a |
| Cement Shade | Application | |
|---|---|---|
| Cementation (Δb*-1) Mean (±SD) n = 10 | Thermocycling (Δb*-2) Mean (±SD) n = 10 | |
| universal-A2 | −0.29 (±0.65) B, a | −4.77 (±1.02) C, b |
| clear | −0.52 (±0.74) B, a | −5.03 (±0.37) C, b |
| white | −0.67 (±0.70) B, a | −3.53 (±0.61) B, b |
| opaque | 3.09 (±1.06) A, a | −2.83 (±0.39) A, b |
| Cement Shade | Application | Total ΔE00 | |
|---|---|---|---|
| Cementation (ΔE00-1) Mean (±SD) n = 10 | Thermocycling (ΔE00-2) Mean (±SD) n = 10 | ||
| universal-A2 | 3.02 (±1.41) | 3.24 (±0.81) | 3.13 (±1.13) A |
| clear | 3.19 (±0.49) | 2.98 (±0.32) | 3.08 (±0.42) A |
| white | 2.19 (±0.46) | 2.02 (±0.37) | 2.10 (±0.41) B |
| opaque | 2.42 (±0.40) | 1.75 (±0.15) | 2.09 (±0.46) B |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaynak Öztürk, E.; Yılmaz Biçer, E.; Güney, B.; Saygılı, S.; Aktaş, N.; Bankoğlu Güngör, M. Effects of Cement Shade, Cementation, and Thermocycling on the Color Parameters and the Final Color of the SLA-Printed Photopolymer Resins. Polymers 2025, 17, 3127. https://doi.org/10.3390/polym17233127
Kaynak Öztürk E, Yılmaz Biçer E, Güney B, Saygılı S, Aktaş N, Bankoğlu Güngör M. Effects of Cement Shade, Cementation, and Thermocycling on the Color Parameters and the Final Color of the SLA-Printed Photopolymer Resins. Polymers. 2025; 17(23):3127. https://doi.org/10.3390/polym17233127
Chicago/Turabian StyleKaynak Öztürk, Esra, Elif Yılmaz Biçer, Beyza Güney, Sina Saygılı, Nagehan Aktaş, and Merve Bankoğlu Güngör. 2025. "Effects of Cement Shade, Cementation, and Thermocycling on the Color Parameters and the Final Color of the SLA-Printed Photopolymer Resins" Polymers 17, no. 23: 3127. https://doi.org/10.3390/polym17233127
APA StyleKaynak Öztürk, E., Yılmaz Biçer, E., Güney, B., Saygılı, S., Aktaş, N., & Bankoğlu Güngör, M. (2025). Effects of Cement Shade, Cementation, and Thermocycling on the Color Parameters and the Final Color of the SLA-Printed Photopolymer Resins. Polymers, 17(23), 3127. https://doi.org/10.3390/polym17233127