Physical Assessment of CAD/CAM and 3D-Printed Resin-Based Ceramics Integrating Additive and Subtractive Methods
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Preparation
2.3. Sample Testing
2.3.1. Water Sorption and Solubility
2.3.2. Surface Roughness
2.4. Analytical or Inferential Statistics
3. Results
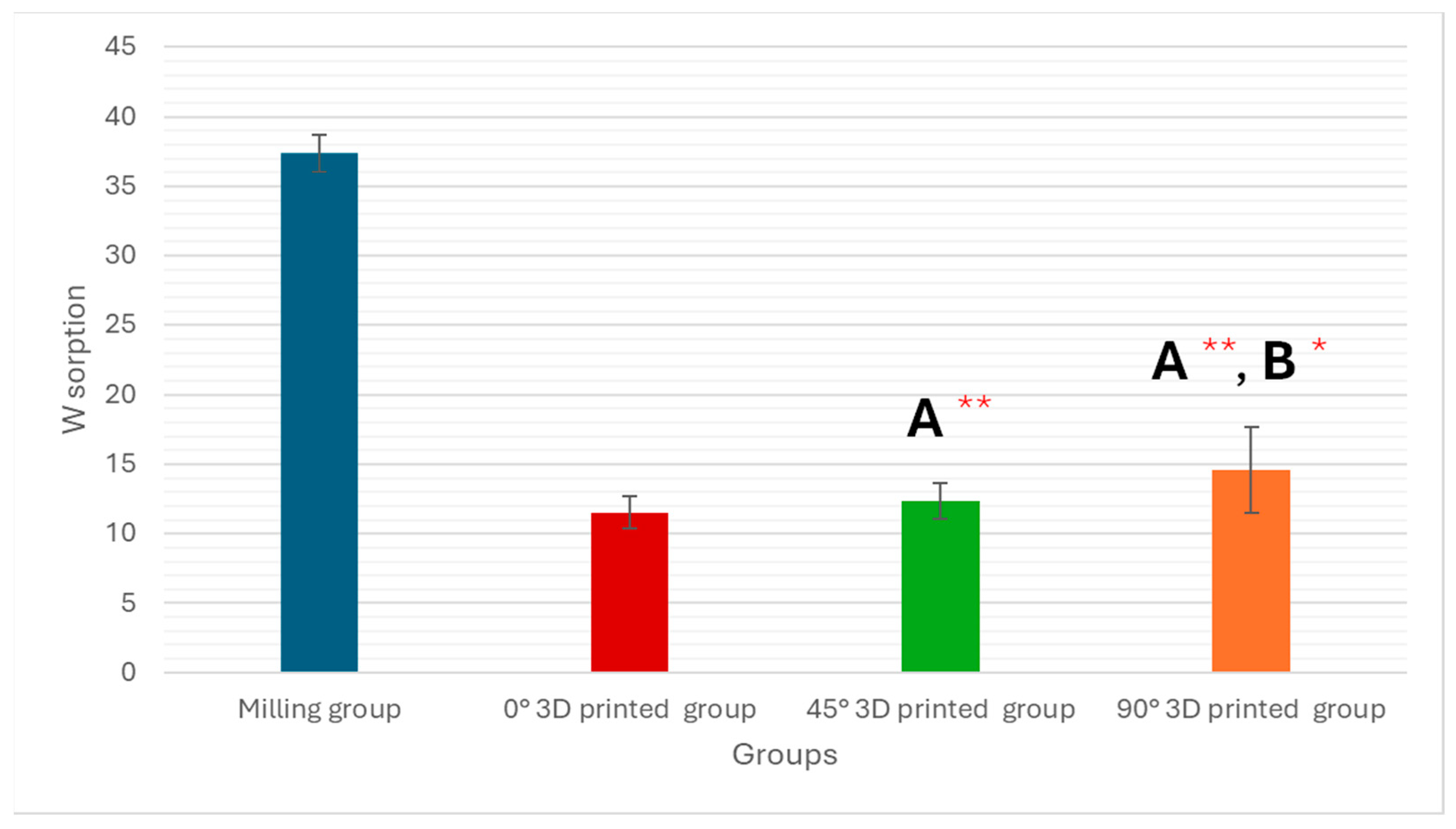
3.1. Water Sorption Test
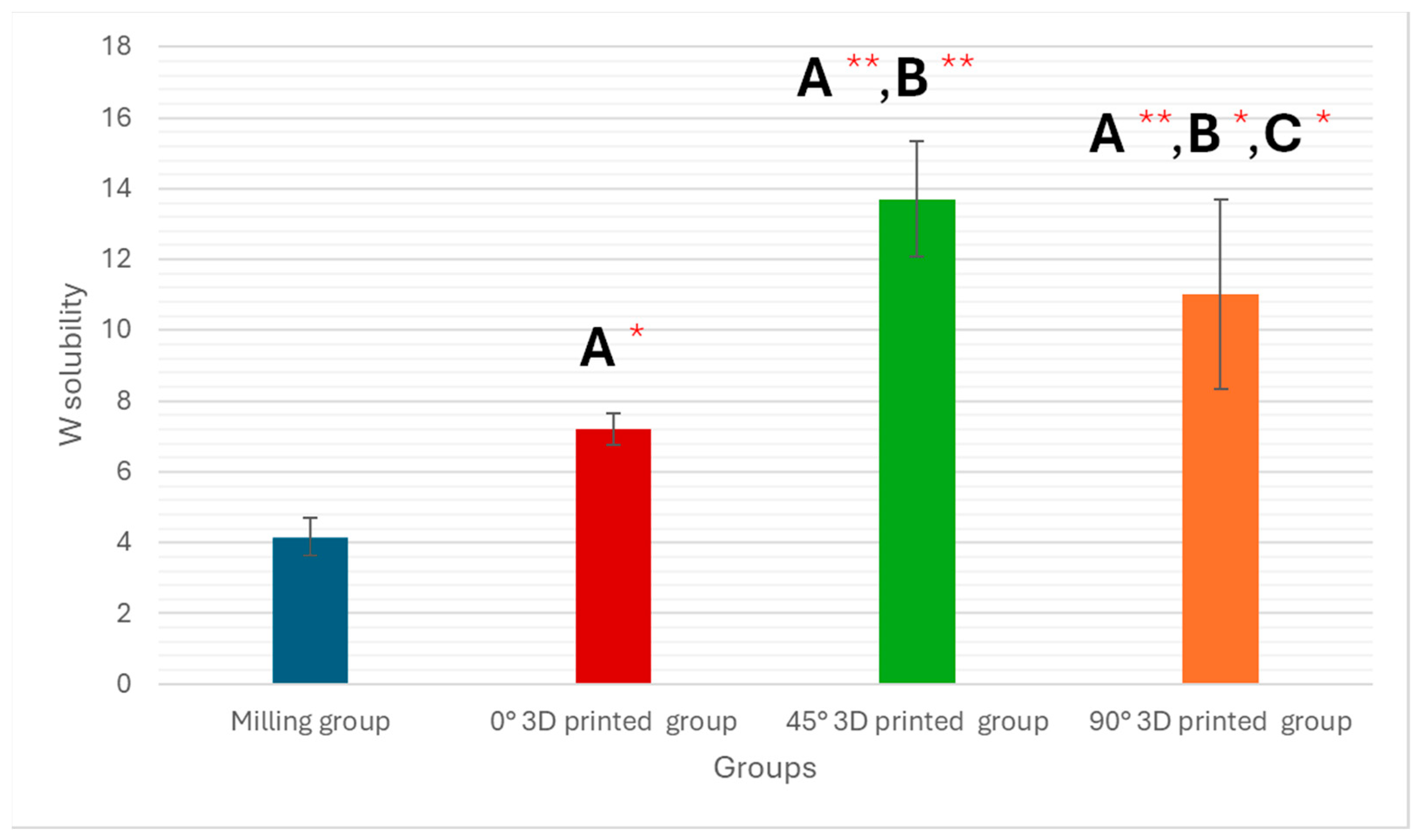
3.2. Water Solubility Test
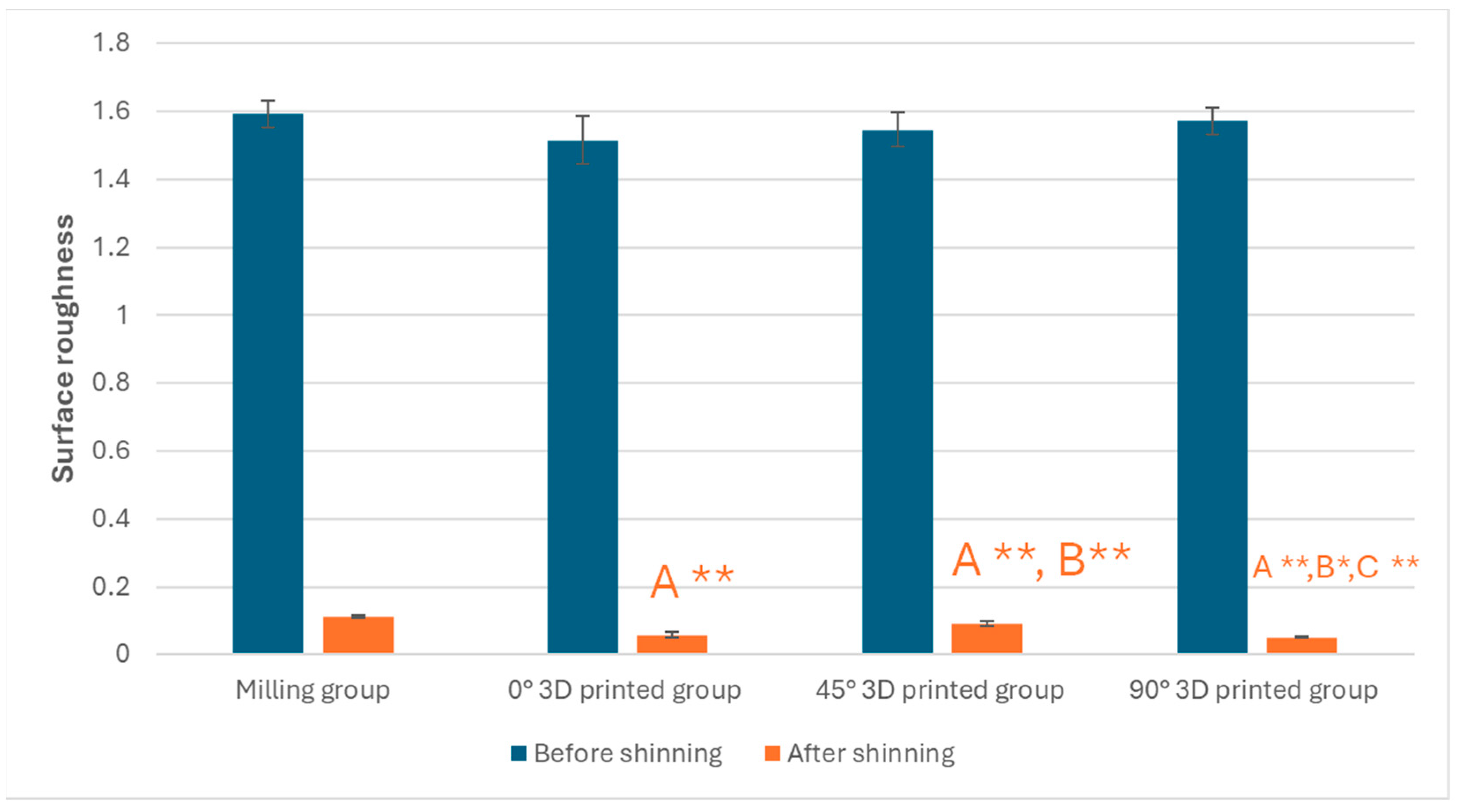
3.3. Surface Roughness Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef] [PubMed]
- Moon, W.; Kim, S.; Lim, B.-S.; Park, Y.-S.; Kim, R.J.-Y.; Chung, S.H. Dimensional accuracy evaluation of temporary dental restorations with different 3D printing systems. Materials 2021, 14, 1487. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Piromalis, D. 3D and 4D printing as integrated manufacturing methods of industry 4.0. Am. J. Eng. Appl. Sci. 2023, 16, 12–22. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and machinable dental restorative composites for CAD/CAM application—Comparison of mechanical properties, fractographic, texture and fractal dimension analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.; Ardu, S.; di Bella, E.; Krejci, I.; Duc, O. Efficiency of 3D-printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J. Prosthet. Dent. 2024, 131, 943–950. [Google Scholar] [CrossRef]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical properties of 3D-printed and milled composite resins for definitive restorations: An in vitro comparison of initial strength and fatigue behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Elkaffas, A.A.; Eltoukhy, R.I.; Elnegoly, S.A.; Mahmoud, S.H. 36-Month Randomized Clinical Trial Evaluation of Preheated and Room Temperature Resin Composite. Oper. Dent. 2022, 47, 11–19. [Google Scholar] [CrossRef]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. In-vitro strength degradation of dental ceramics and novel PICN material by sharp indentation. J. Mech. Behav. Biomed. Mater. 2013, 26, 34–42. [Google Scholar] [CrossRef]
- Wendler, M.; Belli, R.; Valladares, D.; Petschelt, A.; Lohbauer, U. Chairside CAD/CAM materials. Part 3: Cyclic fatigue parameters and lifetime predictions. Dent. Mater. 2018, 34, 910–921. [Google Scholar] [CrossRef]
- Bondarenko, A.V.; Islamov, S.R.; Ignatyev, K.V.; Mardashov, D.V. Laboratory investigation of polymer compositions for ell killing in fractured reservoirs. Perm J. Pet. Min. Eng. 2020, 20, 37–48. [Google Scholar]
- Belousov, A.; Lushpeev, V.; Sokolov, A.; Sultanbekov, R.; Tyan, Y.; Ovchinnikov, E.; Shvets, A.; Bushuev, V.; Islamov, S. Experimental Research of the Possibility of Applying the Hartmann–Sprenger Effect to Regulate the Pressure of Natural Gas in Non-Stationary Conditions. Processes 2025, 13, 1189. [Google Scholar] [CrossRef]
- Eldafrawy, M.; Nguyen, J.-F.; Mainjot, A.; Sadoun, M. A functionally graded PICN material for biomimetic CAD-CAM blocks. J. Dent. Res. 2018, 97, 1324–1330. [Google Scholar] [CrossRef]
- Shin, J.-W.; Kim, J.-E.; Choi, Y.-J.; Shin, S.-H.; Nam, N.-E.; Shim, J.-S.; Lee, K.-W. Evaluation of the color stability of 3D-printed crown and bridge materials against various sources of discoloration: An in vitro study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef]
- Yao, Q.; Morton, D.; Eckert, G.J.; Lin, W.-S. The effect of surface treatments on the color stability of CAD-CAM interim fixed dental prostheses. J. Prosthet. Dent. 2021, 126, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Atria, P.J.; Lagos, I.; Sampaio, C.S. In vitro evaluation of surface roughness, color stability, and color masking of provisional restoration materials for veneers and crowns. Int. J. Comput. Dent. 2020, 23, 343–350. [Google Scholar] [PubMed]
- Taşın, S.; Ismatullaev, A.; Usumez, A. Comparison of surface roughness and color stainability of 3-dimensionally printed interim prosthodontic material with conventionally fabricated and CAD-CAM milled materials. J. Prosthet. Dent. 2022, 128, 1094–1101. [Google Scholar] [CrossRef] [PubMed]
- Song, S.-Y.; Shin, Y.-H.; Lee, J.-Y.; Shin, S.-W. Color stability of provisional restorative materials with different fabrication methods. J. Adv. Prosthodont. 2020, 12, 259–264. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture tooth movement between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2018, 119, 108–115. [Google Scholar] [CrossRef]
- Özcan, C.; Lestriez, P.; Berry-Kromer, V.; Thiébaud, F.; Sockalingum, G.; Untereiner, V.; Angiboust, J.-F.; Josset, Y. Misinterpretation of ISO 4049 standard recommendations: Impact on Young’s modulus and conversion degree of dental composites. J. Mech. Behav. Biomed. Mater. 2020, 110, 103947. [Google Scholar] [CrossRef] [PubMed]
- ISO/FDIS:4049; Dentistry: Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2009.
- Alhassan, M.; Maawadh, A.; Labban, N.; Alnafaiy, S.M.; Alotaibi, H.N.; BinMahfooz, A.M. Effect of different surface treatments on the surface roughness and gloss of resin-modified CAD/CAM ceramics. Appli Sci. 2022, 12, 11972. [Google Scholar] [CrossRef]
- Ling, L.; Ma, Y.; Malyala, R. A novel CAD/CAM resin composite block with high mechanical properties. Dent. Mater. 2021, 37, 1150–1155. [Google Scholar] [CrossRef]
- Alamoush, R.A.; Salim, N.A.; Silikas, N.; Satterthwaite, J.D. Long-term hydrolytic stability of CAD/CAM composite blocks. Eur. J. Oral Sci 2022, 130, e12834. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Long-term sorption and solubility of bulk-fill and conventional resin-composites in water and artificial saliva. J. Dent. 2015, 43, 1511–1518. [Google Scholar] [CrossRef]
- Figuerôa, R.M.S.; Conterno, B.; Arrais, C.A.G.; Sugio, C.Y.C.; Urban, V.M.; Neppelenbroek, K.H. Porosity, water sorption and solubility of denture base acrylic resins polymerized conventionally or in microwave. J. Appl. Oral Sci 2018, 26, e20170383. [Google Scholar] [CrossRef]
- Berli, C.; Thieringer, F.M.; Sharma, N.; Müller, J.A.; Dedem, P.; Fischer, J.; Rohr, N. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J. Prosthet. Dent. 2020, 124, 780–786. [Google Scholar] [CrossRef]
- Gad, M.M.; Alshehri, S.Z.; Alhamid, S.A.; Albarrak, A.; Khan, S.Q.; Alshahrani, F.A.; Alqarawi, F.K. Water sorption, solubility, and translucency of 3D-printed denture base resins. Dent. J. 2022, 10, 42. [Google Scholar] [CrossRef]
- Machado, C.; Rizzatti-Barbosa, C.M.; Gabriotti, M.N.; Joia, F.A.; Ribeiro, M.C.; Sousa, R.L. Influence of mechanical and chemical polishing in the solubility of acrylic resins polymerized by microwave irradiation and conventional water bath. Dent. Mater. 2004, 20, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3D-printed vs. heat-polymerizing and autopolymerizing denture base acrylic resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef]
- Misilli, T.; Gönülol, N. Water sorption and solubility of bulk-fill composites polymerized with a third generation LED LCU. Braz. Oral Res. 2017, 31, e80. [Google Scholar] [CrossRef]
- Cucci, A.L.M.; Vergani, C.E.; Giampaolo, E.T.; Afonso, M.C.d.S.F. Water sorption, solubility, and bond strength of two autopolymerizing acrylic resins and one heat-polymerizing acrylic resin. J. Prosthet. Dent. 1998, 80, 434–438. [Google Scholar] [CrossRef]
- Lassila, L.; Vallittu, P. Denture base polymer Alldent Sinomer®: Mechanical properties, water sorption and release of residual compounds. J. Oral Rehabil. 2001, 28, 607–613. [Google Scholar] [CrossRef]
- Alanazi, K.K.; Alzaid, A.A.; Elkaffas, A.A.; Bukhari, S.A.; Althubaitiy, R.O.; Alfaifi, K.A.; Alfahdi, I.M.; Alqahtani, H.A. Mechanical Assessment of CAD/CAM Fabricated Hybrid Ceramics: An In Vitro Study. Appl. Sci. 2024, 14, 7939. [Google Scholar] [CrossRef]
- Gajewski, V.E.; Pfeifer, C.S.; Fróes-Salgado, N.R.; Boaro, L.C.; Braga, R.R. Monomers used in resin composites: Degree of conversion, mechanical properties and water sorption/solubility. Braz. Dent. J. 2012, 23, 508–514. [Google Scholar] [CrossRef]
- Shim, J.S.; Kim, J.-E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Den. 2020, 124, 468–475. [Google Scholar] [CrossRef]
- Aati, S.; Akram, Z.; Shrestha, B.; Patel, J.; Shih, B.; Shearston, K.; Ngo, H.; Fawzy, A. Effect of post-curing light exposure time on the physico–mechanical properties and cytotoxicity of 3D-printed denture base material. Dent. Mater. 2022, 38, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of postcuring temperature on the mechanical properties and biocompatibility of three-dimensional printed dental resin material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Ang, S.F.; Scholz, T.; Klocke, A.; Schneider, G.A. Determination of the elastic/plastic transition of human enamel by nanoindentation. Dent. Mater. 2009, 25, 1403–1410. [Google Scholar] [CrossRef] [PubMed]
- Kumari, C.M.; Bhat, K.M.; Bansal, R. Evaluation of surface roughness of different restorative composites after polishing using atomic force microscopy. J. Conserv. Dent. 2016, 19, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Robaian, A.; Alshehri, A.M.; Alqhtani, N.R.; Almudahi, A.; Alanazi, K.K.; Abuelqomsan, M.A.; Raffat, E.M.; Elkaffas, A.; Hashem, Q.; Soliman, T.A. Effect of Surface Treatments and Thermal Aging on Bond Strength Between Veneering Resin and CAD/CAM Provisional Materials. Polymers 2025, 17, 563. [Google Scholar] [CrossRef] [PubMed]
- Elkaffas, A.A.; Alshehri, A.M.; Alqahtani, A.R.; Albaijan, R.S.; Soliman, T.A. Impact of Various Cavity-Preparation Designs on Fracture Resistance and Failure Mode of CAD/CAM Fabricated Ceramic Inlays and Onlays. Appl. Sci. 2024, 14, 3816. [Google Scholar] [CrossRef]


| Variables | Study Groups | Significance Test | |||
|---|---|---|---|---|---|
| Milling (n = 5) | 0° 3D-printed (n = 5) | 45° 3D-printed (n = 5) | 90° 3D-printed (n = 5) | ||
| Water Sorption | 37.37 ± 1.35 | 11.52 ± 1.12 | 12.32 ± 1.27 | 14.56 ± 3.11 | F = 212.688 p < 0.001 ** |
| P1 | <0.001 ** | <0.001 ** | <0.001 ** | ||
| P2 | 0.512 | 0.022 * | |||
| P3 | 0.080 | ||||
| Variables | Study Groups | Significance Test | |||
|---|---|---|---|---|---|
| Milling (n = 5) | 0° 3D-printed (n = 5) | 45° 3D-printed (n = 5) | 90° 3D-printed (n = 5) | ||
| Water Solubility | 4.16 ± 0.52 | 7.21 ± 0.45 | 13.70 ± 1.63 | 11.01 ± 2.69 | F = 33.856 p < 0.001 ** |
| P1 | 0.009 * | <0.001 ** | <0.001 ** | ||
| P2 | <0.001 ** | 0.002 * | |||
| P3 | 0.018 * | ||||
| Variables | Study Groups | Significance Test | |||
|---|---|---|---|---|---|
| Milling (n = 10) | 0° 3D-printed (n = 10) | 45° 3D-printed (n = 10) | 90° 3D-printed (n = 10) | ||
| Before Polishing (Shinning) | |||||
| Surface Roughness | 1.592 ± 0.039 | 1.515 ± 0.071 | 1.546 ± 0.050 | 1.571 ± 0.041 | F = 3.652 p = 0.023 * |
| P1 | 0.004 * | 0.072 | 0.393 | ||
| P2 | 0.210 | 0.030 * | |||
| P3 | 0.326 | ||||
| After Polishing (Shinning) | |||||
| Surface Roughness | 0.112 ± 0.002 | 0.058 ± 0.010 | 0.090 ± 0.007 | 0.050 ± 0.002 | F = 195.196 p < 0.001 ** |
| P1 | <0.001 ** | <0.001 ** | <0.001 ** | ||
| P2 | <0.001 ** | 0.013 * | |||
| P3 | <0.001 ** | ||||
| Comparison (before and after polishing) (Shinning) | t = 110.483 p < 0.001 ** | t = 61.583 p < 0.001 ** | t = 89.606 p < 0.001 ** | t = 108.441 p < 0.001 ** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, K.K.; Elkaffas, A.A. Physical Assessment of CAD/CAM and 3D-Printed Resin-Based Ceramics Integrating Additive and Subtractive Methods. Polymers 2025, 17, 2168. https://doi.org/10.3390/polym17162168
Alanazi KK, Elkaffas AA. Physical Assessment of CAD/CAM and 3D-Printed Resin-Based Ceramics Integrating Additive and Subtractive Methods. Polymers. 2025; 17(16):2168. https://doi.org/10.3390/polym17162168
Chicago/Turabian StyleAlanazi, Khalid K., and Ali A. Elkaffas. 2025. "Physical Assessment of CAD/CAM and 3D-Printed Resin-Based Ceramics Integrating Additive and Subtractive Methods" Polymers 17, no. 16: 2168. https://doi.org/10.3390/polym17162168
APA StyleAlanazi, K. K., & Elkaffas, A. A. (2025). Physical Assessment of CAD/CAM and 3D-Printed Resin-Based Ceramics Integrating Additive and Subtractive Methods. Polymers, 17(16), 2168. https://doi.org/10.3390/polym17162168








