Influence of Different Adhesives and Surface Treatments on Shear and Tensile Bond Strength and Microleakage with Micro-CT of Repaired Bulk-Fill Composites
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation for Micro-Shear Bond Strength (µSBS)
2.2. Specimen Preparation for Microtensile Bond Strength (μTBS)
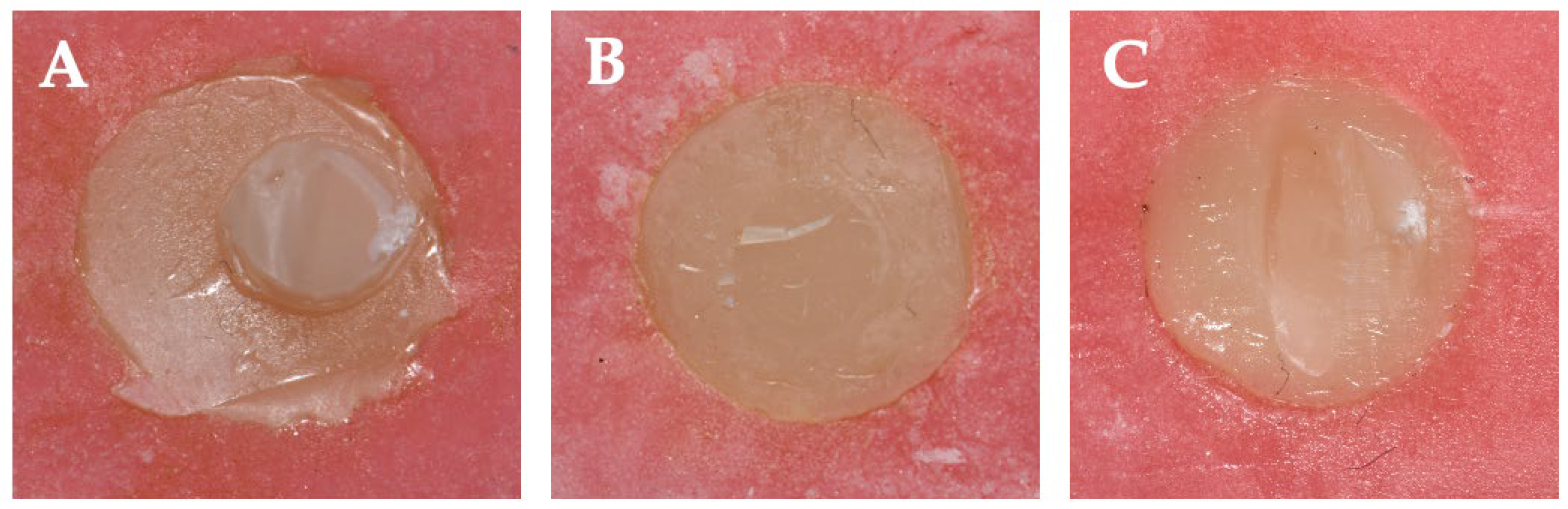
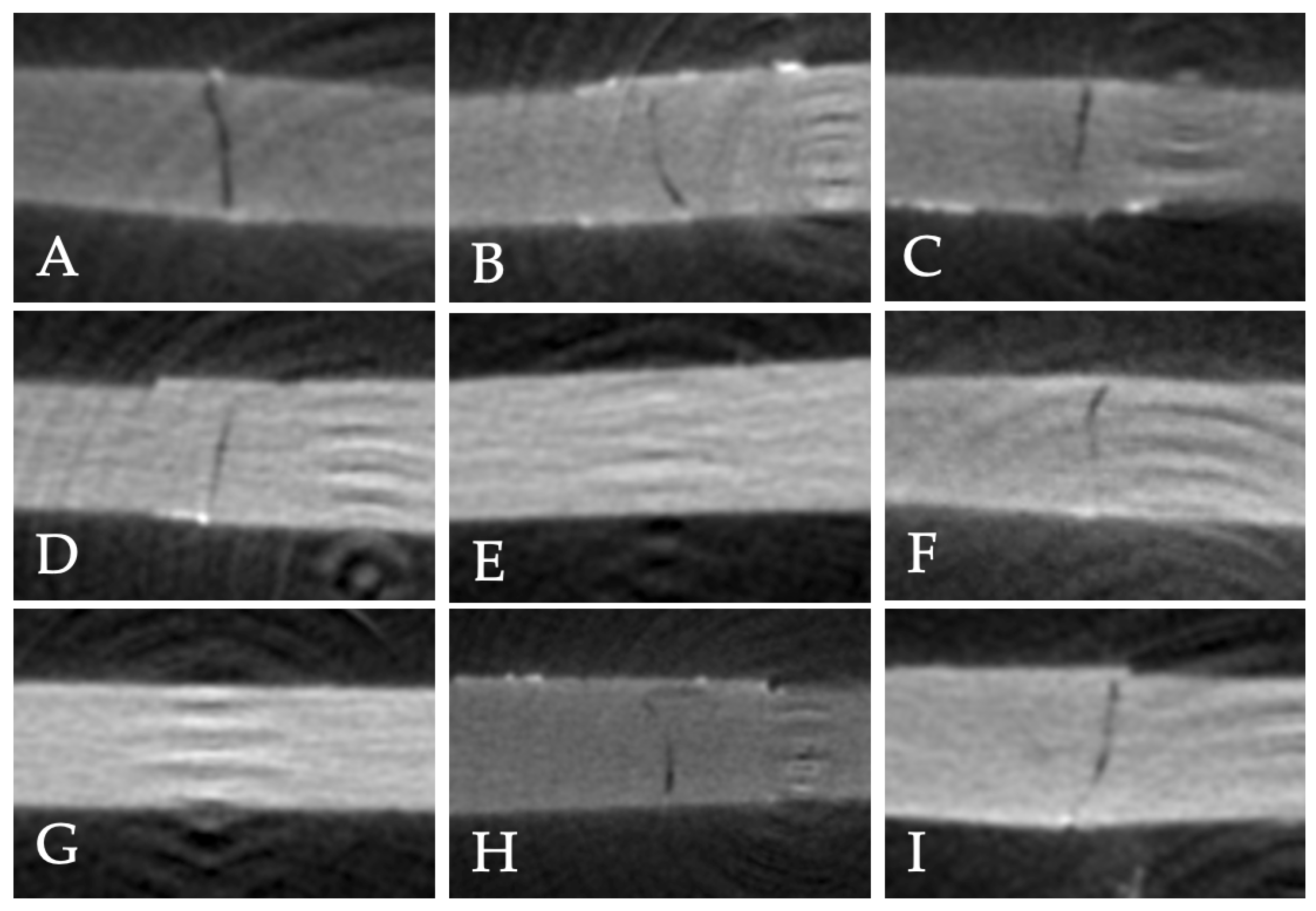
2.3. Microleakage Evaluation
- 0 = No dye penetration
- 1 = Dye penetration up to one-half of the repair interface
- 2 = Dye penetration beyond one-half of the interface, without complete involvement
- 3 = Complete involvement of the repair interface
2.4. Statistical Analysis
3. Results
3.1. Micro-Shear Bond Strength (µSBS)
3.2. Microtensile Bond Strength (µTBS)
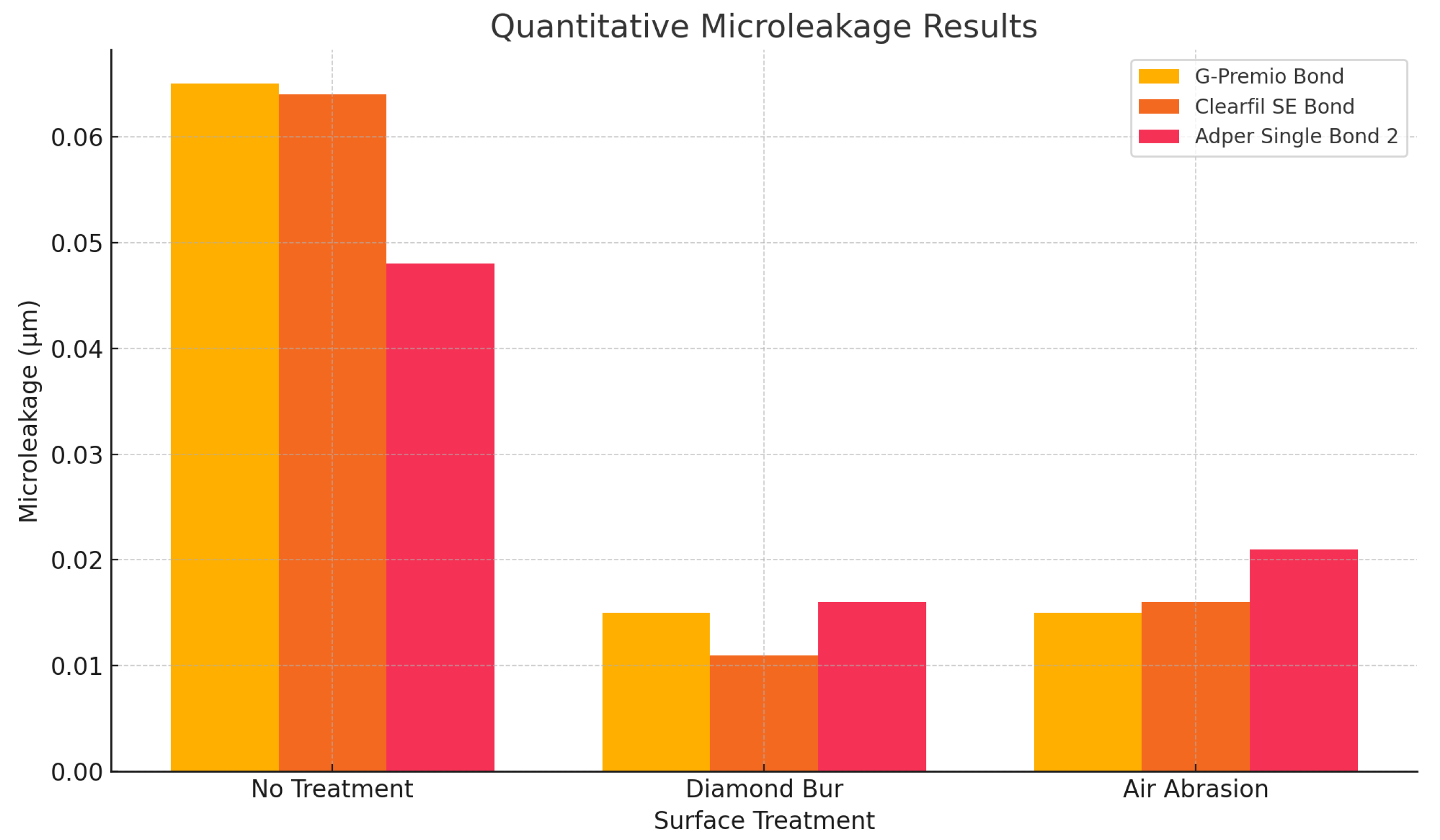
3.3. Qualitative and Quantitative Microleakage Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| µSBS | Micro-shear bond strength |
| µTBS | Microtensile bond strength |
| 10-MDP | 10-methacryloyloxydecyl dihydrogen phosphate |
References
- Hickel, R.; Brüshaver, K.; Ilie, N. Repair of restorations—criteria for decision making and clinical recommendations. Dent. Mater. 2013, 29, 28–50. [Google Scholar] [CrossRef] [PubMed]
- Gordan, V.V.; Mjör, I.A.; Blum, I.R.; Wilson, N. Teaching students the repair of resin-based composite restorations: A survey of North American dental schools. J. Am. Dent. Assoc. 2003, 134, 317–323. [Google Scholar] [PubMed]
- Blum, I.R.; Lynch, C.D.; Wilson, N.H. Factors influencing repair of dental restorations with resin composite. Clin. Cosmet. Investig. Dent. 2014, 6, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Al-Asmar, A.A.; Al-Hiyasat, A.S.; Pitts, N.B. Reframing perceptions in operative dentistry relating evidence-based dentistry and clinical decision making: A cross-sectional study among Jordanian dentists. BMC Oral Health 2022, 22, 637. [Google Scholar] [CrossRef]
- Blum, I.R.; Özcan, M. Reparative Dentistry: Possibilities and Limitations. Curr. Oral Health Rep. 2018, 5, 264–269. [Google Scholar] [CrossRef]
- Ömeroğlu, M.K.; Çam, M.; Doğruer, I.; Kaynar, Z.B. The effect of different surface treatments and adhesive systems on shear bond strength in universal nanohybrid composite resin repair. BMC Oral Health 2025, 25, 459. [Google Scholar]
- Neto, H.N.M.; Leite, J.V.C.; de Medeiros, J.M.; Muniz, I.D.; De Andrade, A.K.; Duarte, R.M.; De Souza, G.M.; Lima, R.B. Scoping review: Effect of surface treatments on bond strength of resin composite repair. J. Dent. 2024, 140, 104737. [Google Scholar] [CrossRef]
- Altinci, P.; Mutluay, M.; Tezvergil-Mutluay, A. Repair bond strength of nanohybrid composite resins with a universal adhesive. Acta Biomater. Odontol. Scand. 2018, 4, 10–19. [Google Scholar] [CrossRef]
- Özcan, M.; Corazza, P.H.; Marocho, S.M.; Barbosa, S.H.; Bottino, M.A. Repair bond strength of microhybrid, nanohybrid and nanofilled resin composites: Effect of substrate resin type, surface conditioning and ageing. Clin. Oral Investig. 2013, 17, 1751–1758. [Google Scholar]
- de Jesus Tavarez, R.R.; Almeida Júnior, L.; Guará, T.C.G.; Ribeiro, I.S.; Maia Filho, E.M.; Firoozmand, L.M. Shear bond strength of different surface treatments in bulk fill, microhybrid, and nanoparticle repair resins. Clin. Cosmet. Investig. Dent. 2017, 9, 61–66. [Google Scholar] [CrossRef]
- Ahlholm, P.; Staxrud, F.; Sipilä, K.; Vallittu, P. Repair bond strength of bulk-fill composites: Influence of different primers and direction of debonding stress. Biomater. Investig. Dent. 2023, 10, 2258924. [Google Scholar] [CrossRef] [PubMed]
- Aquino, C.; Mathias, C.; Barreto, S.C.; Cavalcanti, A.N.; Marchi, G.M.; Mathias, P. Repair Bond Strength and Leakage of Non-Aged and Aged Bulk-fill Composite. Oral Health Prev. Dent. 2020, 18, 783–791. [Google Scholar] [PubMed]
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Celik, E.U.; Ergücü, Z.; Türkün, L.S.; Ercan, U.K. Tensile bond strength of an aged resin composite repaired with different protocols. J. Adhes. Dent. 2011, 13, 359–366. [Google Scholar]
- Özcan, M.; Barbosa, S.H.; Melo, R.M.; Galhano, G.A.; Bottino, M.A. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent. Mater. 2007, 23, 1276–1282. [Google Scholar] [CrossRef]
- Hadilou, M.; Dolatabadi, A.; Ghojazadeh, M.; Hosseinifard, H.; Alizadeh Oskuee, P.; Pournaghi Azar, F. Effect of Different Surface Treatments on the Long-Term Repair Bond Strength of Aged Methacrylate-Based Resin Composite Restorations: A Systematic Review and Network Meta-analysis. Biomed. Res. Int. 2022, 2022, 7708643. [Google Scholar] [CrossRef]
- Ghavami-Lahiji, M.; Firouzmanesh, M.; Bagheri, H.; Jafarzadeh Kashi, T.S.; Razazpour, F.; Behroozibakhsh, M. The effect of thermocycling on the degree of conversion and mechanical properties of a microhybrid dental resin composite. Restor. Dent. Endod. 2018, 43, e26. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Andrade de Freitas, S.L.; Brandt, W.C.; Miranda, M.E.; Vitti, R.P. Effect of Thermocycling, Teeth, and Polymerization Methods on Bond Strength Teeth-Denture Base. Int. J. Dent. 2018, 2018, 2374327. [Google Scholar] [CrossRef]
- Akgül, S.; Kedici Alp, C.; Bala, O. Repair potential of a bulk-fill resin composite: Effect of different surface-treatment protocols. Eur. J. Oral Sci. 2021, 129, e12814. [Google Scholar] [CrossRef]
- Cuevas-Suárez, C.E.; Nakanishi, L.; Isolan, C.P.; Ribeiro, J.S.; Moreira, A.G.; Piva, E. Repair bond strength of bulk-fill resin composite: Effect of different adhesive protocols. Dent. Mater. J. 2020, 39, 236–241. [Google Scholar] [CrossRef]
- Loomans, B.; Özcan, M. Intraoral Repair of Direct and Indirect Restorations: Procedures and Guidelines. Oper. Dent. 2016, 41, S68–S78. [Google Scholar] [CrossRef]
- Cavalcanti, A.N.; De Lima, A.F.; Peris, A.R.; Mitsui, F.H.; Marchi, G.M. Effect of surface treatments and bonding agents on the bond strength of repaired composites. J. Esthet. Restor. Dent. 2007, 19, 90–98. [Google Scholar] [CrossRef]
- Costa, T.R.; Ferreira, S.Q.; Klein-Júnior, C.A.; Loguercio, A.D.; Reis, A. Durability of surface treatments and intermediate agents used for repair of a polished composite. Oper. Dent. 2010, 35, 231–237. [Google Scholar] [CrossRef]
- Wendler, M.; Belli, R.; Panzer, R.; Skibbe, D.; Petschelt, A.; Lohbauer, U. Repair Bond Strength of Aged Resin Composite after Different Surface and Bonding Treatments. Materials 2016, 9, 547. [Google Scholar] [CrossRef]
- Martin, J.; Fernandez, E.; Estay, J.; Gordan, V.V.; Mjör, I.A.; Moncada, G. Minimal invasive treatment for defective restorations: Five-year results using sealants. Oper. Dent. 2013, 38, 125–133. [Google Scholar] [CrossRef]
- Baur, V.; Ilie, N. Repair of dental resin-based composites. Clin. Oral Investig. 2013, 17, 601–608. [Google Scholar] [CrossRef]
- Çakir, N.N.; Demirbuga, S.; Balkaya, H.; Karadaş, M. Bonding performance of universal adhesives on composite repairs, with or without silane application. J. Conserv. Dent. 2018, 21, 263–268. [Google Scholar] [CrossRef]
- Nagaoka, N.; Yoshihara, K.; Feitosa, V.P.; Tamada, Y.; Irie, M.; Yoshida, Y.; Van Meerbeek, B.; Hayakawa, S. Chemical interaction mechanism of 10-MDP with zirconia. Sci. Rep. 2017, 7, 45563. [Google Scholar] [CrossRef]
- Carrilho, E.; Cardoso, M.; Marques Ferreira, M.; Marto, C.M.; Paula, A.; Coelho, A.S. 10-MDP Based Dental Adhesives: Adhesive Interface Characterization and Adhesive Stability—A Systematic Review. Materials 2019, 12, 790. [Google Scholar] [CrossRef]
- Yin, H.; Kwon, S.; Chung, S.H.; Kim, R.J.Y. Performance of Universal Adhesives in Composite Resin Repair. Biomed. Res. Int. 2022, 2022, 7663490. [Google Scholar] [CrossRef]
- Cavalcanti, A.N.; Lavigne, C.; Fontes, C.M.; Mathias, P. Microleakage at the composite-repair interface: Effect of different adhesive systems. J. Appl. Oral Sci. 2004, 12, 219–222. [Google Scholar] [CrossRef]
- de Medeiros, T.C.; de Lima, M.R.; Bessa, S.C.; de Araújo, D.F.; Galvão, M.R. Repair bond strength of bulk fill composites after different adhesion protocols. J. Clin. Exp. Dent. 2019, 11, e1000–e1005. [Google Scholar] [CrossRef]





| Material | Manifacturer | Composition |
|---|---|---|
| Adper Single Bond 2 | 3M/ESPE, St. Paul, MN, USA | Bis-GMA, HEMA, dimethacrylates, ethanol, water, a novel photoinitiator system, and a methacrylate functional copolymer of polyacrylic and polyitaconic acids, silica nanofiller (5 nm diameter silica particles, 10 wt%). |
| Clearfill SE Bond | Kuraray, Osaka, Japan | Primer: MDP, HEMA, hydrophilicdimethacrylate, dl-camphorquinone, N,N-diethanol-p-toluidine, water. Bond: MDP, Bis-GMA, HEMA, hydrophobicdimethacrylate, dl-camphorquinone, N,N-diethanol-p-toluidine, silanated colloidalsilica |
| G-Premio Bond | GC Corporation, Tokyo, Japan | 10-MDP, 4-META, 10- methacryoyloxydecyl dihydrogen thiophosphate, methacrylate acid ester, distilled water, acetone, photo-initiators, silica fine powder |
| Filtek One Bulk Fill Restorative | 3M/ESPE, St. Paul, MN, USA | Filler: non-agglomerated/non-aggregated 20 nm silica filler, non-agglomerated/non-aggregated 4 to 11 nm zirconiafiller, aggregated zirconia/silica clusterfiller (comprising 20 nm silica and 4 to 11 nm zirconia particles) and aytterbium trifluoride filler agglomerate 100 nm particles. Matrix: AFM (dynamic stress-relieving monomer), AUDMA, UDMA and 1,12-dodecane-DMA |
| Repair Protocol | Bonding Materials | p | ||
|---|---|---|---|---|
| G-Premio Bond | Clearfil SE Bond | Adper Single Bond 2 | ||
| No treatment | 83.4 (15.1) A | 68.9 (35.6) A | 33.1 (22.9) a,B | 0.002 †,* |
| Diamond bur | 95.4 (34.9) A | 110.4 (17.3) A | 164.1 (31.8) b,B | 0.001 ‡,* |
| Air abrasion | 103.7 (40.2) | 108.4 (48.5) | 70.5 (17.8) c | 0.117 ‡ |
| p | 0.456 ‡ | 0.093 † | 0.001 ‡,* | |
| Repair Protocol | Bonding Materials | p | ||
|---|---|---|---|---|
| G-Premio Bond | Clearfil SE Bond | Adper Single Bond 2 | ||
| No treatment | 10.1 (1.7) a,A | 11.7 (2.9) a,A | 23.4 ± 6.4 a,B | <0.001 * |
| Diamond bur | 15.5 (3.9) b,A | 22.9 (14.7) b,A | 35.7 ± 6.7 b,B | <0.001 * |
| Air abrasion | 16.6 (3.2) b,A | 30.9 (7.3) c,B | 33.2 ± 5.1 b,B | <0.001 * |
| p | 0.001 * | <0.001 * | 0.001 * | |
| Repair Protocol | Bonding Materials | p | ||
|---|---|---|---|---|
| G-Premio Bond | Clearfil SE Bond | Adper Single Bond 2 | ||
| No treatment | 0.065 (0.07) | 0.064 (0.01) a | 0.048 (0.05) | 0.404 |
| Diamond bur | 0.015 (0.01) | 0.011 (0.02) b | 0.016 (0.02) | 0.626 |
| Air abrasion | 0.015 (0.02) | 0.016 (0.02) b | 0.021 (0.01) | 0.808 |
| p | 0.269 | <0.001 * | 0.389 | |
| Repair Protocol | Bonding Materials | Scores | |||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| No treatment | G-Premio Bond | 3 (37.5%) | - | 3 (37.5%) | 2 (25%) |
| Clearfil SE Bond | - | 6 (75%) | 2 (25%) | - | |
| Adper Single Bond 2 | 5 (62.5%) | 1 (12.5%) | 2 (25%) | - | |
| Diamond bur | G-Premio Bond | 3 (37.5%) | 5 (62.5%) | - | - |
| Clearfil SE Bond | 5 (62.5%) | 3 (37.5%) | - | - | |
| Adper Single Bond 2 | 5 (62.5%) | 3 (37.5%) | - | ||
| Air abrasion | G-Premio Bond | 5 (62.5%) | 3 (37.5%) | - | - |
| Clearfil SE Bond | 6 (75%) | 2 (25%) | - | - | |
| Adper Single Bond 2 | 3 (37.5%) | 5 (62.5%) | - | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yıldırım-Işık, H.; Büyükgöze-Dindar, M. Influence of Different Adhesives and Surface Treatments on Shear and Tensile Bond Strength and Microleakage with Micro-CT of Repaired Bulk-Fill Composites. Polymers 2025, 17, 1680. https://doi.org/10.3390/polym17121680
Yıldırım-Işık H, Büyükgöze-Dindar M. Influence of Different Adhesives and Surface Treatments on Shear and Tensile Bond Strength and Microleakage with Micro-CT of Repaired Bulk-Fill Composites. Polymers. 2025; 17(12):1680. https://doi.org/10.3390/polym17121680
Chicago/Turabian StyleYıldırım-Işık, Handan, and Mediha Büyükgöze-Dindar. 2025. "Influence of Different Adhesives and Surface Treatments on Shear and Tensile Bond Strength and Microleakage with Micro-CT of Repaired Bulk-Fill Composites" Polymers 17, no. 12: 1680. https://doi.org/10.3390/polym17121680
APA StyleYıldırım-Işık, H., & Büyükgöze-Dindar, M. (2025). Influence of Different Adhesives and Surface Treatments on Shear and Tensile Bond Strength and Microleakage with Micro-CT of Repaired Bulk-Fill Composites. Polymers, 17(12), 1680. https://doi.org/10.3390/polym17121680






