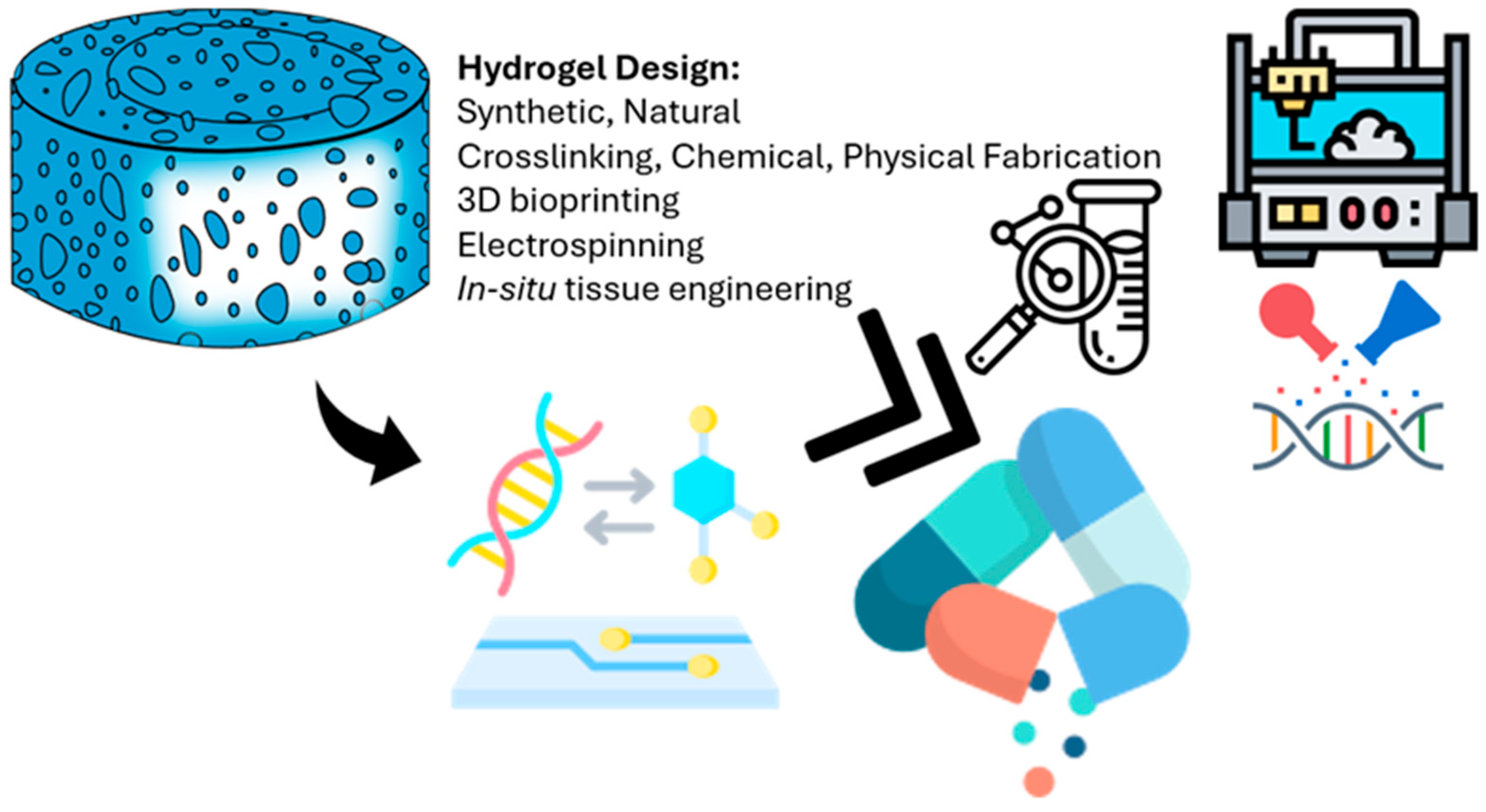
Next-Generation Hydrogel Design: Computational Advances in Synthesis, Characterization, and Biomedical Applications
Abstract
1. Introduction
2. Literature Parsing and Analysis
2.1. Focused Questions
2.2. Eligibility Criteria
3. Classification of Hydrogels
3.1. Natural Hydrogels
3.2. Synthetic Hydrogels
4. Hydrogel Physicochemical Properties and Their Impact on the Cell System
4.1. Stiffness
4.2. Stimulus-Responsive Hydrogels
5. Trends in Hydrogel Customization for Regenerative Medicine
6. Dynamic Mechanical Properties in Tissue Development
6.1. Incorporating Dynamic Properties into Hydrogels
6.2. Supramolecular Chemistry in Hydrogel Design
6.3. Future Applications of Regenerative Medicine in 3D Bioprinting
6.4. Cartilage Repair
7. Integration of Classical Molecular Modeling Methods in Hydrogel Research
8. Integration of Artificial Intelligence in Hydrogel Research
9. Conclusions and Future Outlook
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sofi, H.S.; Ashraf, R.; Khan, A.H.; Beigh, M.A.; Majeed, S.; Sheikh, F.A. Reconstructing nanofibers from natural polymers using surface functionalization approaches for applications in tissue engineering, drug delivery and biosensing devices. Mater. Sci. Eng. C 2019, 94, 1102–1124. [Google Scholar] [CrossRef] [PubMed]
- Ravichandran, R.; Sundarrajan, S.; Venugopal, J.R.; Mukherjee, S.; Ramakrishna, S. Advances in polymeric systems for tissue engineering and biomedical applications. Macromol. Biosci. 2012, 12, 286–311. [Google Scholar] [CrossRef] [PubMed]
- Abune, L.; Davis, B.; Wang, Y. Aptamer-functionalized hydrogels: An emerging class of biomaterials for protein delivery, cell capture, regenerative medicine, and molecular biosensing. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2021, 13, e1731. [Google Scholar] [CrossRef] [PubMed]
- Culver, H.R.; Clegg, J.R.; Peppas, N.A. Analyte-responsive hydrogels: Intelligent materials for biosensing and drug delivery. Acc. Chem. Res. 2017, 50, 170–178. [Google Scholar] [CrossRef]
- Negut, I.; Bita, B. Exploring the potential of artificial intelligence for hydrogel development—A short review. Gels 2023, 9, 845. [Google Scholar] [CrossRef]
- Akhtar, Z.B.; Gupta, A.D. Advancements within molecular engineering for regenerative medicine and biomedical applications: An investigation analysis towards a computing retrospective. J. Electron. Electromed. Eng. Med. Inform. 2024, 6, 54–72. [Google Scholar] [CrossRef]
- Patel, R.A.; Webb, M.A. Data-driven design of polymer-based biomaterials: High-throughput simulation, experimentation, and machine learning. ACS Appl. Bio Mater. 2023, 7, 510–527. [Google Scholar] [CrossRef]
- Döring, A.; Birnbaum, W.; Kuckling, D. Responsive hydrogels–structurally and dimensionally optimized smart frameworks for applications in catalysis, micro-system technology and material science. Chem. Soc. Rev. 2013, 42, 7391–7420. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.S.; Khademhosseini, A. Advances in engineering hydrogels. Science 2017, 356, eaaf3627. [Google Scholar] [CrossRef]
- Finster, R.; Sankaran, P.; Bihar, E. Computational and AI-driven design of hydrogels for bioelectronic applications. Adv. Electron. Mater. 2025, 2025, 2400763. [Google Scholar] [CrossRef]
- Cao, H.; Duan, L.; Zhang, Y.; Cao, J.; Zhang, K. Current hydrogel advances in physicochemical and biological response-driven biomedical application diversity. Signal Transduct. Target. Ther. 2021, 6, 426. [Google Scholar] [CrossRef]
- Ahadian, S.; Sadeghian, R.B.; Salehi, S.; Ostrovidov, S.; Bae, H.; Ramalingam, M.; Khademhosseini, A. Bioconjugated hydrogels for tissue engineering and regenerative medicine. Bioconjug. Chem. 2015, 26, 1984–2001. [Google Scholar] [CrossRef]
- Farazin, A.; Gheisizadeh, A. Revolutionizing bone repair and regeneration: The role of machine learning in designing advanced nanocomposite hydrogels. Polym. Adv. Technol. 2025, 36, e70161. [Google Scholar] [CrossRef]
- El-Tanani, M.; Satyam, S.M.; Rabbani, S.A.; El-Tanani, Y.; Aljabali, A.A.A.; Al Faouri, I.; Rehman, A. Revolutionizing drug delivery: The impact of advanced materials science and technology on precision medicine. Pharmaceutics 2025, 17, 375. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Li, Z.; Xu, S.; Liu, Z. Recent advances of hydrogel network models for studies on mechanical behaviors. Acta Mech. Sin. 2021, 37, 367–386. [Google Scholar] [CrossRef]
- Lei, L.; Bai, Y.; Qin, X.; Liu, J.; Huang, W.; Lv, Q. Current understanding of hydrogel for drug release and tissue engineering. Gels 2022, 8, 301. [Google Scholar] [CrossRef]
- Li, J.; Mooney, D.J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016, 1, 16071. [Google Scholar] [CrossRef]
- Lin, C.C.; Metters, A.T. Hydrogels in controlled release formulations: Network design and mathematical modeling. Adv. Drug Deliv. Rev. 2006, 58, 1379–1408. [Google Scholar] [CrossRef]
- Wang, C.; Varshney, R.R.; Wang, D.-A. Therapeutic cell delivery and fate control in hydrogels and hydrogel hybrids. Adv. Drug Deliv. Rev. 2010, 62, 699–710. [Google Scholar] [CrossRef]
- Caccavo, D.; Cascone, S.; Lamberti, G.; Barba, A.A. Hydrogels: Experimental characterization and mathematical modelling of their mechanical and diffusive behaviour. Chem. Soc. Rev. 2018, 47, 2357–2373. [Google Scholar] [CrossRef]
- Vernerey, F.J.; Sridhar, S.L.; Muralidharan, A.; Bryant, S.J. Mechanics of 3D cell–hydrogel interactions: Experiments, models, and mechanisms. Chem. Rev. 2021, 121, 11085–11148. [Google Scholar] [CrossRef] [PubMed]
- Catoira, M.C.; Fusaro, L.; Francesco, D.D.; Ramella, M.; Boccafoschi, F. Overview of natural hydrogels for regenerative medicine applications. J. Mater. Sci. Mater. Med. 2019, 30, 115. [Google Scholar] [CrossRef] [PubMed]
- Varghese, S.A.; Rangappa, S.M.; Siengchin, S.; Parameswaranpillai, J. Natural polymers and the hydrogels prepared from them. In Hydrogels Based on Natural Polymers; Elsevier: Amsterdam, The Netherlands, 2020; pp. 17–47. [Google Scholar]
- Ahmad, Z.; Salman, S.; Khan, S.A.; Amin, A.; Rahman, Z.U.; Al-Ghamdi, Y.O.; Akhtar, K.; Bakhsh, E.M.; Khan, S.B. Versatility of hydrogels: From synthetic strategies, classification, and properties to biomedical applications. Gels 2022, 8, 167. [Google Scholar] [CrossRef]
- Gong, J.P. Why are double network hydrogels so tough? Soft Matter 2010, 6, 2583–2590. [Google Scholar] [CrossRef]
- Dau, H.; Jones, G.R.; Tsogtgerel, E.; Nguyen, D.; Keyes, A.; Liu, Y.-S.; Rauf, H.; Ordonez, E.; Puchelle, V.; Alhan, H.B.; et al. Linear block copolymer synthesis. Chem. Rev. 2022, 122, 14471–14553. [Google Scholar] [CrossRef]
- Soman, A.; Mathew, F.; Chacko, A.J.; Alias, M.; Poosan, G.V. Interpenetrating polymer network (IPN)-hydrogels. Pharma Innov. 2014, 3 Pt A, 59. [Google Scholar]
- Rizwan, M.; Yahya, R.; Hassan, A.; Yar, M.; Azzahari, A.D.; Selvanathan, V.; Sonsudin, F.; Abouloula, C.N. pH sensitive hydrogels in drug delivery: Brief history, properties, swelling, and release mechanism, material selection and applications. Polymers 2017, 9, 137. [Google Scholar] [CrossRef] [PubMed]
- Borges, F.T.P.; Papavasiliou, G.; Teymour, F. Characterizing the molecular architecture of hydrogels and crosslinked polymer networks beyond Flory–Rehner theory. Biomacromolecules 2020, 21, 5104–5118. [Google Scholar] [CrossRef]
- Bashir, S.; Hina, M.; Iqbal, J.; Rajpar, A.H.; Mujtaba, M.A.; Alghamdi, N.A.; Wageh, S.; Ramesh, K.; Ramesh, S. Fundamental concepts of hydrogels: Synthesis, properties, and their applications. Polymers 2020, 12, 2702. [Google Scholar] [CrossRef]
- Mukherjee, C.; Varghese, D.; Krishna, J.S.; Boominathan, T.; Rakeshkumar, R.; Dineshkumar, S.; Brahmananda Rao, C.V.S.; Sivaramakrishna, A. Recent advances in biodegradable polymers–properties, applications and future prospects. Eur. Polym. J. 2023, 192, 112068. [Google Scholar] [CrossRef]
- Garcia-Garcia, A.; Muñana-González, S.; Lanceros-Mendez, S.; Ruiz-Rubio, L.; Alvarez, L.P.; Vilas-Vilela, J.L. Biodegradable natural hydrogels for tissue engineering, controlled release, and soil remediation. Polymers 2024, 16, 2599. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Atif, M.; Haseen, M.; Kamal, S.; Khan, M.S.; Shahid, S.; Nami, S.A.A. Synthesis, classification and properties of hydrogels: Their applications in drug delivery and agriculture. J. Mater. Chem. B 2022, 10, 170–203. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.; Hubbell, J.A. Enhanced proteolytic degradation of molecularly engineered PEG hydrogels in response to MMP-1 and MMP-2. Biomaterials 2010, 31, 7836–7845. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, C.; Wu, S.; Fan, Y.; Li, X. Influence of the mechanical properties of biomaterials on degradability, cell behaviors and signaling pathways: Current progress and challenges. Biomater. Sci. 2020, 8, 2714–2733. [Google Scholar] [CrossRef]
- Lee, S.C.; Gillispie, G.; Prim, P.; Lee, S.J. Physical and chemical factors influencing the printability of hydrogel-based extrusion bioinks. Chem. Rev. 2020, 120, 10834–10886. [Google Scholar] [CrossRef]
- Vasile, C.; Pamfil, D.; Stoleru, E.; Baican, M. New developments in medical applications of hybrid hydrogels containing natural polymers. Molecules 2020, 25, 1539. [Google Scholar] [CrossRef]
- Reguieg, F.; Ricci, L.; Bouyacoub, N.; Belbachir, M.; Bertoldo, M. Thermal characterization by DSC and TGA analyses of PVA hydrogels with organic and sodium MMT. Polym. Bull. 2020, 77, 929–948. [Google Scholar] [CrossRef]
- Li, Y.; Rodrigues, J.; Tomás, H. Injectable and biodegradable hydrogels: Gelation, biodegradation and biomedical applications. Chem. Soc. Rev. 2012, 41, 2193–2221. [Google Scholar] [CrossRef] [PubMed]
- Chartoff, R.P.; Menczel, J.D.; Dillman, S.H. Dynamic mechanical analysis (DMA). In Thermal Analysis of Polymers: Fundamentals and Applications; John and Wiley Sons: Hoboken, NJ, USA, 2009; pp. 387–495. [Google Scholar]
- Oyen, M.L. Mechanical characterisation of hydrogel materials. Int. Mater. Rev. 2014, 59, 44–59. [Google Scholar] [CrossRef]
- Kravanja, K.A.; Finšgar, M. Analytical techniques for the characterization of bioactive coatings for orthopaedic implants. Biomedicines 2021, 9, 1936. [Google Scholar] [CrossRef]
- Abbass, M.M.S.; El-Rashidy, A.A.; Sadek, K.M.; El-Moshy, S.; Radwan, I.A.; Rady, D.; Dörfer, C.E.; El-Sayed, K.M.F. Hydrogels and dentin–pulp complex regeneration: From the benchtop to clinical translation. Polymers 2020, 12, 2935. [Google Scholar] [CrossRef]
- Kumar, A.; Han, S.S. PVA-based hydrogels for tissue engineering: A review. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 159–182. [Google Scholar] [CrossRef]
- Curvello, R.; Raghuwanshi, V.S.; Garnier, G. Engineering nanocellulose hydrogels for biomedical applications. Adv. Colloid Interface Sci. 2019, 267, 47–61. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Florit, M.; Pardo, A.; Domingues, R.M.A.; Graça, A.L.; Babo, P.S.; Reis, R.L.; Gomes, M.E. Natural-based hydrogels for tissue engineering applications. Molecules 2020, 25, 5858. [Google Scholar] [CrossRef]
- Radulescu, D.-M.; Neacsu, I.A.; Grumezescu, A.-M.; Andronescu, E. New insights of scaffolds based on hydrogels in tissue engineering. Polymers 2022, 14, 799. [Google Scholar] [CrossRef] [PubMed]
- Samiraninezhad, N.; Asadi, K.; Rezazadeh, H.; Gholami, A. Using chitosan, hyaluronic acid, alginate, and gelatin-based smart biological hydrogels for drug delivery in oral mucosal lesions: A review. Int. J. Biol. Macromol. 2023, 252, 126573. [Google Scholar] [CrossRef]
- Rana, M.M.; De la Hoz Siegler, H. Evolution of hybrid hydrogels: Next-generation biomaterials for drug delivery and tissue engineering. Gels 2024, 10, 216. [Google Scholar] [CrossRef]
- Ho, T.-C.; Chang, C.-C.; Chan, H.-P.; Chung, T.-W.; Shu, C.-W.; Chuang, K.-P.; Duh, T.-H.; Yang, M.-H.; Tyan, Y.-C. Hydrogels: Properties and applications in biomedicine. Molecules 2022, 27, 2902. [Google Scholar] [CrossRef]
- Liu, J.; Yang, L.; Liu, K.; Gao, F. Hydrogel scaffolds in bone regeneration: Their promising roles in angiogenesis. Front. Pharmacol. 2023, 14, 1050954. [Google Scholar] [CrossRef]
- Brandl, F.; Kastner, F.; Gschwind, R.M.; Blunk, T.; Teßmar, J.; Göpferich, A. Hydrogel-based drug delivery systems: Comparison of drug diffusivity and release kinetics. J. Control. Release 2010, 142, 221–228. [Google Scholar] [CrossRef]
- Monfared, V. Application of artificial intelligence (machine learning) in additive manufacturing, bio-systems, bio-medicine, and composites. In Additive Manufacturing for Biocomposites and Synthetic Composites; CRC Press: New York, NY, USA, 2023; pp. 152–203. [Google Scholar]
- Wang, S.; Sun, Z. Hydrogel and machine learning for soft robots’ sensing and signal processing: A Review. J. Bionic Eng. 2023, 20, 845–857. [Google Scholar] [CrossRef]
- Zhao, J.; Santino, F.; Giacomini, D.; Gentilucci, L. Integrin-targeting peptides for the design of functional cell-responsive biomaterials. Biomedicines 2020, 8, 307. [Google Scholar] [CrossRef] [PubMed]
- El-Husseiny, H.M.; Mady, E.A.; Hamabe, L.; Abugomaa, A.; Shimada, K.; Yoshida, T.; Tanaka, T.; Yokoi, A.; Elbadawy, M.; Tanaka, R. Smart/stimuli-responsive hydrogels: Cutting-edge platforms for tissue engineering and other biomedical applications. Mater. Today Bio 2022, 13, 100186. [Google Scholar] [CrossRef]
- Ma, Y.; Han, T.; Yang, Q.; Wang, J.; Feng, B.; Jia, Y.; Wei, Z.; Xu, F. Viscoelastic cell microenvironment: Hydrogel-based strategy for recapitulating dynamic ECM mechanics. Adv. Funct. Mater. 2021, 31, 2100848. [Google Scholar] [CrossRef]
- Khansari, M.M.; Sorokina, L.V.; Mukherjee, P.; Mukhtar, F.; Shirdar, M.R.; Shahidi, M.; Shokuhfar, T. Classification of hydrogels based on their source: A review and application in stem cell regulation. JOM 2017, 69, 1340–1347. [Google Scholar] [CrossRef]
- Morales, X.; Cortes-Dominguez, I.; Solorzano, C.O. Modeling the mechanobiology of cancer cell migration using 3D biomimetic hydrogels. Gels 2021, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Niethammer, P. Components and mechanisms of nuclear mechanotransduction. Annu. Rev. Cell Dev. Biol. 2021, 37, 233–256. [Google Scholar] [CrossRef]
- Claudino, M.; Zhang, X.; Alim, M.D.; Podgórski, M.; Bowman, C.N. Mechanistic kinetic modeling of thiol–Michael addition photopolymerizations via photocaged “superbase” generators: An analytical approach. Macromolecules 2016, 49, 8061–8074. [Google Scholar] [CrossRef]
- Aseervatham, J. Cytoskeletal remodeling in cancer. Biology 2020, 9, 385. [Google Scholar] [CrossRef]
- Mantha, S.; Pillai, S.; Khayambashi, P.; Upadhyay, A.; Zhang, Y.; Tao, O.; Pham, H.M.; Tran, S.D. Smart hydrogels in tissue engineering and regenerative medicine. Materials 2019, 12, 3323. [Google Scholar] [CrossRef]
- Wang, X.; Schmidt, C.K.; Sanchez, S.; Gracias, D.H.; Carazo-Salas, R.E.; Jackson, S.P.; Schmidt, O.G. Rolled-up functionalized nanomembranes as three-dimensional cavities for single cell studies. Nano Lett. 2014, 14, 4197–4204. [Google Scholar]
- Park, S. Development of the Engineered Biological Model Systems and Chemoselective Redox Responsive Ligation (CRRL). Ph.D. Thesis, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, 2010. [Google Scholar]
- Soleymani, S.; Naghib, S.M. 3D and 4D printing hydroxyapatite-based scaffolds for bone tissue engineering and regeneration. Heliyon 2023, 9, e19363. [Google Scholar] [CrossRef]
- Wellman, S.M.; Eles, J.R.; Ludwig, K.A.; Seymour, J.P.; Michelson, N.J.; McFadden, W.E.; Vazquez, A.L.; Kozai, T.D.Y. A materials roadmap to functional neural interface design. Adv. Funct. Mater. 2018, 28, 1701269. [Google Scholar] [CrossRef]
- Zhang, Y.; Huang, Y. Rational design of smart hydrogels for biomedical applications. Front. Chem. 2021, 8, 615665. [Google Scholar] [CrossRef]
- Han, X.; Chang, S.; Zhang, M.; Bian, X.; Li, C.; Li, D. Advances of hydrogel-based bioprinting for cartilage tissue engineering. Front. Bioeng. Biotechnol. 2021, 9, 746564. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, N.; Chouhan, D.; Mandal, B.B. Tissue engineered skin and wound healing: Current strategies and future directions. Curr. Pharm. Des. 2017, 23, 3455–3482. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, J.; Wang, Y.; Cui, W. Advanced electrospun hydrogel fibers for wound healing. Compos. Part B Eng. 2021, 223, 109101. [Google Scholar] [CrossRef]
- Rode, M.P.; Angulski, A.B.B.; Gomes, F.A.; da Silva, M.M.; Jeremias, T.S.; de Carvalho, R.G.; IV, D.G.; Oliveira, L.F.C.; des Maia, L.F.; Trentin, A.G.; et al. Carrageenan hydrogel as a scaffold for skin-derived multipotent stromal cells delivery. J. Biomater. Appl. 2018, 33, 422–434. [Google Scholar] [CrossRef] [PubMed]
- Omidian, H.; Chowdhury, S.D.; Wilson, R.L. Advancements and challenges in hydrogel engineering for regenerative medicine. Gels 2024, 10, 238. [Google Scholar] [CrossRef]
- Wang, H.; Shi, J.; Wang, Y.; Yin, Y.; Wang, L.; Liu, J.; Liu, Z.; Duan, C.; Zhu, P.; Wang, C. Promotion of cardiac differentiation of brown adipose derived stem cells by chitosan hydrogel for repair after myocardial infarction. Biomaterials 2014, 35, 3986–3998. [Google Scholar] [CrossRef]
- Hamsayegan, S.; Raissi, H.; Ghahari, A. Selective detection of food contaminants using engineered gallium-organic frameworks with MD and metadynamics simulations. Sci. Rep. 2024, 14, 18144. [Google Scholar] [CrossRef]
- Hinderer, S.; Layland, S.L.; Schenke-Layland, K. ECM and ECM-like materials—Biomaterials for applications in regenerative medicine and cancer therapy. Adv. Drug Deliv. Rev. 2016, 97, 260–269. [Google Scholar] [CrossRef]
- Sharma, S.; Bhende, M.; Goel, A. A review: Polysaccharide-based hydrogels and their biomedical applications. Polym. Bull. 2024, 81, 8573–8594. [Google Scholar] [CrossRef]
- Unagolla, J.M.; Jayasuriya, A.C. Hydrogel-based 3D bioprinting: A comprehensive review on cell-laden hydrogels, bioink formulations, and future perspectives. Appl. Mater. Today 2020, 18, 100479. [Google Scholar] [CrossRef]
- Rangel-Argote, M.; Claudio-Rizo, J.A.; Mata-Mata, J.L.; Mendoza-Novelo, B. Characteristics of collagen-rich extracellular matrix hydrogels and their functionalization with poly(ethylene glycol) derivatives for enhanced biomedical applications: A review. ACS Appl. Bio Mater. 2018, 1, 1215–1228. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Liu, J.; Qi, C.; Fang, Y.; Zhang, L.; Zhuo, R.; Jiang, X. Thermosensitive injectable in-situ forming carboxymethyl chitin hydrogel for three-dimensional cell culture. Acta Biomater. 2016, 35, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhang, H.; Ahlfeld, T.; Kilian, D.; Liu, Y.; Gelinsky, M.; Hu, Q. Evaluation of different crosslinking methods in altering the properties of extrusion-printed chitosan-based multi-material hydrogel composites. Bio-Des. Manuf. 2023, 6, 150–173. [Google Scholar] [CrossRef]
- Lin, F.-Y.; Chang, C.-Y.; Nguyen, H.; Li, H.; Fishel, M.L.; Lin, C.-C. Viscoelastic hydrogels for interrogating pancreatic cancer-stromal cell interactions. Mater. Today Bio 2023, 19, 100576. [Google Scholar] [CrossRef]
- Bertsch, P.; Diba, M.; Mooney, D.J.; Leeuwenburgh, S.C.G. Self-healing injectable hydrogels for tissue regeneration. Chem. Rev. 2022, 123, 834–873. [Google Scholar] [CrossRef]
- Simińska-Stanny, J.; Hachemi, F.; Dodi, G.; Cojocaru, F.D.; Gardikiotis, I.; Podstawczyk, D.; Delporte, C.; Jiang, G.; Nie, L.; Shavandi, A. Optimizing phenol-modified hyaluronic acid for designing shape-maintaining biofabricated hydrogel scaffolds in soft tissue engineering. Int. J. Biol. Macromol. 2023, 244, 125201. [Google Scholar] [CrossRef]
- Chang, B.; Ahuja, N.; Ma, C.; Liu, X. Injectable scaffolds: Preparation and application in dental and craniofacial regeneration. Mater. Sci. Eng. R. Rep. 2017, 111, 1–26. [Google Scholar] [CrossRef]
- Gorecka, J.; Kostiuk, V.; Fereydooni, A.; Gonzalez, L.; Luo, J.; Dash, B.; Isaji, T.; Ono, S.; Liu, S.; Lee, S.R.; et al. The potential and limitations of induced pluripotent stem cells to achieve wound healing. Stem Cell Res. Ther. 2019, 10, 87. [Google Scholar] [CrossRef]
- Thanaskody, K.; Jusop, A.S.; Tye, G.J.; Zaman, W.S.W.K.; Dass, S.A.; Nordin, F. MSCs vs. iPSCs: Potential in therapeutic applications. Front. Cell Dev. Biol. 2022, 10, 1005926. [Google Scholar] [CrossRef]
- Chen, X.; Zhu, L.; Wang, X.; Xiao, J. Insight into heart-tailored architectures of hydrogel to restore cardiac functions after myocardial infarction. Mol. Pharm. 2022, 20, 57–81. [Google Scholar] [CrossRef] [PubMed]
- Bonde, S.; Chandarana, C.; Prajapati, P.; Vashi, V. A comprehensive review on recent progress in chitosan composite gels for biomedical uses. Int. J. Biol. Macromol. 2024, 272, 132723. [Google Scholar] [CrossRef]
- Abdelaziz, A.G.; Nageh, H.; Abdo, S.M.; Abdalla, M.S.; Amer, A.A.; Abdal-Hay, A.; Barhoum, A. A review of 3D polymeric scaffolds for bone tissue engineering: Principles, fabrication techniques, immunomodulatory roles, and challenges. Bioengineering 2023, 10, 204. [Google Scholar] [CrossRef] [PubMed]
- Rezakhani, L.; Gharibshahian, M.; Salehi, M.; Zamani, S.; Abpeikar, Z.; Ghaderzadeh, O.; Alizadeh, M.; Masoudi, A.; Rezaei, N.; Cheraghali, D. Recent advances in hydrogels applications for tissue engineering and clinical trials. Regen. Ther. 2024, 26, 635–645. [Google Scholar] [CrossRef]
- Li, C.-S.; Xu, Y.; Li, J.; Qin, S.-H.; Huang, S.-W.; Chen, X.-M.; Luo, Y.; Gao, C.-T.; Xiao, J.-H. Ultramodern natural and synthetic polymer hydrogel scaffolds for articular cartilage repair and regeneration. Biomed. Eng. Online 2025, 24, 13. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Hu, D.A.; Wu, D.; He, F.; Wang, H.; Huang, L.; Shi, D.; Liu, Q.; Ni, N.; Pakvasa, M.; et al. Applications of biocompatible scaffold materials in stem cell-based cartilage tissue engineering. Front. Bioeng. Biotechnol. 2021, 9, 603444. [Google Scholar] [CrossRef]
- Sofat, N.; Kuttapitiya, A. Future directions for the management of pain in osteoarthritis. Int. J. Clin. Rheumatol. 2014, 9, 197. [Google Scholar] [CrossRef]
- Hashemi-Afzal, F.; Fallahi, H.; Bagheri, F.; Collins, M.N.; Eslaminejad, M.B.; Seitz, H. Advancements in hydrogel design for articular cartilage regeneration: A comprehensive review. Bioact. Mater. 2025, 43, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.T.; Ren, X.; Afizah, M.H.; Tarigan-Panjaitan, S.; Yang, Z.; Wu, Y.; Chian, K.S.; Mikos, A.G.; Hui, J.H.P. Repair of osteochondral defects with rehydrated freeze-dried oligo[poly(ethylene glycol) fumarate] hydrogels seeded with bone marrow mesenchymal stem cells in a porcine model. Tissue Eng. Part A 2013, 19, 1852–1861. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, H.B.; Dogru, S.; Lashkarinia, S.S.; Pekkan, K. Soft-tissue material properties and mechanogenetics during cardiovascular development. J. Cardiovasc. Dev. Dis. 2022, 9, 64. [Google Scholar] [CrossRef]
- Kim, B.S.; Das, S.; Jang, J.; Cho, D.-W. Decellularized extracellular matrix-based bioinks for engineering tissue- and organ-specific microenvironments. Chem. Rev. 2020, 120, 10608–10661. [Google Scholar] [CrossRef] [PubMed]
- Sreekumaran, S.; Radhakrishnan, A.; Rauf, A.A.; Kurup, M. Nanohydroxyapatite incorporated photocrosslinked gelatin methacryloyl/poly(ethylene glycol) diacrylate hydrogel for bone tissue engineering. Prog. Biomater. 2021, 10, 43–51. [Google Scholar] [CrossRef]
- Xiao, S.; Zhao, T.; Wang, J.; Wang, C.; Du, J.; Ying, L.; Lin, J.; Zhang, C.; Hu, W.; Wang, L.; et al. Gelatin methacrylate (GelMA)-based hydrogels for cell transplantation: An effective strategy for tissue engineering. Stem Cell Rev. Rep. 2019, 15, 664–679. [Google Scholar] [CrossRef]
- Krishna, K.S.; Li, Y.; Li, S.; Kumar, C.S.S.R. Lab-on-a-chip synthesis of inorganic nanomaterials and quantum dots for biomedical applications. Adv. Drug Deliv. Rev. 2013, 65, 1470–1495. [Google Scholar] [CrossRef]
- Aguirre, M.; Ballard, N.; Gonzalez, E.; Hamzehlou, S.; Sardon, H.; Calderon, M.; Paulis, M.; Tomovska, R.; Dupin, D.; Bean, R.H.; et al. Polymer colloids: Current challenges, emerging applications, and new developments. Macromolecules 2023, 56, 2579–2607. [Google Scholar] [CrossRef]
- Thiele, J.; Ma, Y.; Bruekers, S.M.C.; Ma, S.; Huck, W.T.S. 25th anniversary article: Designer hydrogels for cell cultures: A materials selection guide. Adv. Mater. 2014, 26, 125–148. [Google Scholar] [CrossRef]
- Boateng, D.; Li, X.; Zhu, Y.; Zhang, H.; Wu, M.; Liu, J.; Kang, Y.; Zeng, H.; Han, L. Recent advances in flexible hydrogel sensors: Enhancing data processing and machine learning for intelligent perception. Biosens. Bioelectron. 2024, 261, 116499. [Google Scholar] [CrossRef]
- Spreiter, Q.; Walter, M. Classical molecular dynamics simulation with the velocity Verlet algorithm at strong external magnetic fields. J. Comput. Phys. 1999, 152, 102–119. [Google Scholar] [CrossRef]
- Marchetto, A.; Chaib, Z.S.; Rossi, C.A.; Ribeiro, R.P.; Pantano, S.; Rossetti, G.; Giorgetti, A. CGMD platform: Integrated web servers for the preparation, running, and analysis of coarse-grained molecular dynamics simulations. Molecules 2020, 25, 5934. [Google Scholar] [CrossRef]
- Lamas, C.P.; Sanz, E.; Vega, C.; Noya, E.G. Estimation of bubble cavitation rates in a symmetrical Lennard-Jones mixture by NVT seeding simulations. J. Chem. Phys. 2023, 158, 124109. [Google Scholar] [CrossRef]
- Chakraborty, P.; Mitra, S.; Kim, A.R.; Zhao, B.; Mitra, S.K. Density Functional Theory approach to interpret elastowetting of hydrogels. Langmuir 2024, 40, 7168–7177. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Sun, Y.; Dong, X.; Yin, Q.; Zhu, H.; Li, S.; Zhou, J.; Wang, C. Cell-derived extracellular matrix-coated silk fibroin scaffold for cardiogenesis of brown adipose stem cells through modulation of TGF-β pathway. Regen. Biomater. 2020, 7, 403–412. [Google Scholar] [CrossRef]
- Musharaf, H.M.; Roshan, U.; Mudugamuwa, A.; Trinh, Q.T.; Zhang, J.; Nguyen, N.-T. Computational fluid–structure interaction in microfluidics. Micromachines 2024, 15, 897. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, M.; Yan, Z.; Ji, S.; Xiao, S.; Gao, J. Metal nanoparticle hybrid hydrogels: The state-of-the-art of combining hard and soft materials to promote wound healing. Theranostics 2024, 14, 1534. [Google Scholar] [CrossRef]
- Filipecka-Szymczyk, K.; Makowska-Janusik, M.; Marczak, W. Molecular dynamics simulations of HEMA-based hydrogels for ophthalmological applications. Molecules 2024, 29, 5784. [Google Scholar] [CrossRef]
- Jiang, S.; Li, Y.; Yong, Z. Compatibility analysis between natural rubber/polybutadiene rubber and protective waxes based on experiments and Materials Studio simulations. J. Appl. Polym. Sci. 2024, 141, e55468. [Google Scholar] [CrossRef]
- Salave, S.; Rana, D.; Sharma, A.; Bharathi, K.; Gupta, R.; Khode, S.; Benival, D.; Kommineni, N. Polysaccharide-based implantable drug delivery: Development strategies, regulatory requirements, and future perspectives. Polysaccharides 2022, 3, 625–654. [Google Scholar] [CrossRef]
- Arif, Z.U. The role of polysaccharide-based biodegradable soft polymers in the healthcare sector. Adv. Ind. Eng. Polym. Res. 2024, 8, 132–156. [Google Scholar] [CrossRef]
- D’Andrea, L.D.; Iaccarino, G.; Fattorusso, R.; Sorriento, D.; Carannante, C.; Capasso, D.; Trimarco, B.; Pedone, C. Targeting angiogenesis: Structural characterization and biological properties of a de novo engineered VEGF mimicking peptide. Proc. Natl. Acad. Sci. USA 2005, 102, 14215–14220. [Google Scholar] [CrossRef]
- de Sousa, M.C.A.; Rodrigues, C.A.V.; Ferreira, I.A.F.; Diogo, M.M.; Linhardt, R.J.; Cabral, J.M.S.; Ferreira, F.C. Functionalization of electrospun nanofibers and fiber alignment enhance neural stem cell proliferation and neuronal differentiation. Front. Bioeng. Biotechnol. 2020, 8, 580135. [Google Scholar] [CrossRef] [PubMed]
- Foyt, D.A.; Norman, M.D.A.; Yu, T.T.L.; Gentleman, E. Exploiting advanced hydrogel technologies to address key challenges in regenerative medicine. Adv. Healthc. Mater. 2018, 7, 1700939. [Google Scholar] [CrossRef]
- Deore, A.B.; Dhumane, J.R.; Wagh, R.; Sonawane, R. The stages of drug discovery and development process. Asian J. Pharm. Res. Dev. 2019, 7, 62–67. [Google Scholar] [CrossRef]
- Ogata, S.; Lidorikis, E.; Shimojo, F.; Nakano, A.; Vashishta, P.; Kalia, R.K. Hybrid finite-element/molecular-dynamics/electronic-density-functional approach to materials simulations on parallel computers. Comput. Phys. Commun. 2001, 138, 143–154. [Google Scholar] [CrossRef]
- Li, Z.; Song, P.; Li, G.; Han, Y.; Ren, X.; Bai, L.; Su, J. AI energized hydrogel design, optimization and application in biomedicine. Mater. Today Bio 2024, 25, 101014. [Google Scholar] [CrossRef]
- Mahesh, B. Machine learning algorithms—A review. Int. J. Sci. Res. (IJSR) 2020, 9, 381–386. [Google Scholar] [CrossRef]
- Singh, A.; Thakur, N.; Sharma, A. A review of supervised machine learning algorithms. In Proceedings of the2016 3rd International Conference on Computing for Sustainable Global Development (INDIACom), New Delhi, India, 16–18 March 2016; pp. 1310–1315. [Google Scholar]
- Batra, R.; Song, L.; Ramprasad, R. Emerging materials intelligence ecosystems propelled by machine learning. Nat. Rev. Mater. 2021, 6, 655–678. [Google Scholar] [CrossRef]
- Wang, C.; He, T.; Zhou, H.; Zhang, Z.; Lee, C. Artificial intelligence enhanced sensors-enabling technologies to next-generation healthcare and biomedical platform. Bioelectron. Med. 2023, 9, 17. [Google Scholar] [CrossRef]
- Nosrati, H.; Nosrati, M. Artificial intelligence in regenerative medicine: Applications and implications. Biomimetics 2023, 8, 442. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z. Soft-Body Simulation with CUDA based on Mass-Spring Model and Verlet Integration Scheme; American Society of Mechanical Engineers: New York, NY, USA, 2020; Volume 7A, ISBN 978-0-7918-8454-6. [Google Scholar]
- Orio, M.; Pantazis, D.A.; Neese, F. Density functional theory. Photosynth. Res. 2009, 102, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Bagayoko, D. Understanding density functional theory (DFT) and completing it in practice. AIP Adv. 2014, 4, 127104. [Google Scholar] [CrossRef]
- Panagiotopoulou, O. Finite element analysis (FEA): Applying an engineering method to functional morphology in anthropology and human biology. Ann. Hum. Biol. 2009, 36, 609–623. [Google Scholar] [CrossRef]
- Chen, G.; Xian, W.; Wang, Q.; Li, Y. Molecular simulation guided and physics-informed mechanistic modeling of multifunctional polymers. Acta Mech. Sin. 2021, 37, 725–745. [Google Scholar] [CrossRef]
- Pissis, P.; Kyritsis, A. Electrical conductivity studies in hydrogels. Solid State Ion. 1997, 97, 105–113. [Google Scholar] [CrossRef]
- Díaz-Marín, C.D.; Zhang, L.; Lu, Z.; Alshrah, M.; Grossman, J.C.; Wang, E.N. Kinetics of sorption in hygroscopic hydrogels. Nano Lett. 2022, 22, 1100–1107. [Google Scholar] [CrossRef]
- Agatonovic-Kustrin, S.; Beresford, R. Basic concepts of artificial neural network (ANN) modeling and its application in pharmaceutical research. J. Pharm. Biomed. Anal. 2000, 22, 717–727. [Google Scholar] [CrossRef]
- Bemani, A.; Madani, M.; Kazemi, A. Machine learning-based estimation of nano-lubricants viscosity in different operating conditions. Fuel 2023, 352, 129102. [Google Scholar] [CrossRef]
- Xu, J.; Tsai, Y.-L.; Hsu, S.-h. Design strategies of conductive hydrogel for biomedical applications. Molecules 2020, 25, 5296. [Google Scholar] [CrossRef]
- Xu, S.; Chen, X.; Wang, S.; Chen, Z.; Pan, P.; Huang, Q. Integrating machine learning for the optimization of polyacrylamide/alginate hydrogel. Regen. Biomater. 2024, 11, rbae109. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Brooks, B.R. A double exponential potential for van der Waals interaction. AIP Adv. 2019, 9, 065304. [Google Scholar] [CrossRef] [PubMed]
- Younes, K.; Kharboutly, Y.; Antar, M.; Chaouk, H.; Obeid, E.; Mouhtady, O.; Abu-Samha, M.; Halwani, J.; Murshid, N. Application of unsupervised machine learning for the evaluation of aerogels’ efficiency towards ion removal—A principal component analysis (PCA) approach. Gels 2023, 9, 304. [Google Scholar] [CrossRef]
- Sumiea, E.H.; Abdulkadir, S.J.; Alhussian, H.S.; Al-Selwi, S.M.; Alqushaibi, A.; Ragab, M.G.; Fati, S.M. Deep deterministic policy gradient algorithm: A systematic review. Heliyon 2024, 10, e30697. [Google Scholar] [CrossRef]
- Krishani, M.; Shin, W.Y.; Suhaimi, H.; Sambudi, N.S. Development of scaffolds from bio-based natural materials for tissue regeneration applications: A review. Gels 2023, 9, 100. [Google Scholar] [CrossRef] [PubMed]
- Champa-Bujaico, E.; García-Díaz, P.; Díez-Pascual, A.M. Machine learning for property prediction and optimization of polymeric nanocomposites: A state-of-the-art. Int. J. Mol. Sci. 2022, 23, 10712. [Google Scholar] [CrossRef]
- Tiong, T.; Saad, I.; Teo, K.T.K.; Lago, H. Deep reinforcement learning with robust deep deterministic policy gradient. In Proceedings of the 2020 2nd International Conference on Electrical, Control and Instrumentation Engineering (ICECIE), Kuala Lumpur, Malaysia, 28 November 2020; pp. 1–5. [Google Scholar]
- Zhu, J.-A.; Jia, Y.; Lei, J.; Liu, Z. Deep learning approach to mechanical property prediction of single-network hydrogel. Mathematics 2021, 9, 2804. [Google Scholar] [CrossRef]
- Wang, Y.; Wallmersperger, T.; Ehrenhofer, A. Application of back propagation neural networks and random forest algorithms in material research of hydrogels. PAMM 2023, 23, e202200278. [Google Scholar] [CrossRef]
- Seifermann, M.; Reiser, P.; Friederich, P.; Levkin, P.A. High-throughput synthesis and machine learning assisted design of photodegradable hydrogels. Small Methods 2023, 7, 2300553. [Google Scholar] [CrossRef]
- Liu, D.; Ma, S.; Yuan, H.; Markert, B. Modelling and simulation of coupled fluid transport and time-dependent fracture in fibre-reinforced hydrogel composites. Comput. Methods Appl. Mech. Eng. 2022, 390, 114470. [Google Scholar] [CrossRef]



| Category | Subcategories |
|---|---|
| Source | Natural polymers and synthetic polymers |
| Polymer composition | Interpenetrating network, homopolymeric, copolymeric |
| Crosslinking | Physical, chemical |
| Degradability | Biodegradable, nonbiodegradable |
| Structure | Amorphous, semicrystalline |
| Physical Aspects | Film, gel, matrix, micro/nanoparticles |
| Stimulus responsiveness | Physical (such as temperature), chemical (such as pH), biochemical (e.g., antigen) |
| Charge | Cationic, anionic, and neutral |
| Category | Subcategories |
|---|---|
| Polymer composition | Homopolymeric (e.g., poly(N-isopropylacrylamide)), copolymeric (e.g., poly(PEGMA-monomethyl), heteropolymeric (e.g., poly(vinyl alcohol)-gelatin), hybrid (different polymers or phases) |
| Network structure | Physical cross-linking, chemical cross-linking |
| Stimulus responsiveness | Physical stimuli (temperature), chemical stimuli (pH, ionic strength), and biochemical stimuli (anti-gen, enzyme) |
| Physical aspects | Micro/nanoparticles: microbeads, nanogels, film: electrospun mats, matrix, scaffolds, and gel: injectable drug-loaded hydrogels |
| Configuration of chains | Noncrystalline (random structure in amorphous regions), semicrystalline (combination of amorphous and ordered/crystalline regions) |
| Hydrogel Type | Material | Properties | Applications |
|---|---|---|---|
| Natural | Collagen | Biocompatible, biodegrad- able, low mechanical strength | Tissue engineering and wound healing |
| Natural | Gelatin | Biodegradable, poor me-chanical strength, cross-linked forms available | Tissue scaffolds for re generative medicine |
| Natural | Hyaluronic Acid | Hydrophilic, cell-binding sites, varying molecular weights influence function | Drug delivery and tissue repair |
| Natural | Alginate | Bioinert, tunable me-chanical properties, cross-linkable with divalent cations | Cell encapsulation and tissue scaffolds |
| Synthetic | PEG derivatives | Easy to synthesize, bioin-ert, modifiable, tunable mechanical properties | Drug delivery and tissue engineering |
| Synthetic | PVA | Biocompatible, low me-chanical strength, enhanced by cross-linking | Contact lenses and artificial joints |
| Synthetic | PNIPAAm | Temperature-sensitive, poor biodegradability, cytotoxicity issues | Drug delivery and cell carriers |
| Category | Subcategories |
|---|---|
| Source of monomer/polymer | Natural, synthetic, and hybrid (nanocomposite) |
| Configuration | Amorphous (noncrystalline), semicrystalline, and crystalline |
| Polymeric composition | Homopolymeric, copolymeric, and multipolymer |
| Type of cross-linking | Chemical (covalent bonding) and physical (noncovalent bonding) |
| Pore size between polymer systems | Nonporous, microporous, and superporous |
| Stimuli responsiveness | Thermosensitive (chitosan), photosensitive (alginate), glucose-responsive (agarose), pH-responsive (hyaluronic acid), enzyme-responsive (PVA), ROS-responsive (PEG), biosensitive (DNA-based), multifunctional-responsive (peptide-based) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fareed, M.M.; Shityakov, S. Next-Generation Hydrogel Design: Computational Advances in Synthesis, Characterization, and Biomedical Applications. Polymers 2025, 17, 1373. https://doi.org/10.3390/polym17101373
Fareed MM, Shityakov S. Next-Generation Hydrogel Design: Computational Advances in Synthesis, Characterization, and Biomedical Applications. Polymers. 2025; 17(10):1373. https://doi.org/10.3390/polym17101373
Chicago/Turabian StyleFareed, Muhammad Mazhar, and Sergey Shityakov. 2025. "Next-Generation Hydrogel Design: Computational Advances in Synthesis, Characterization, and Biomedical Applications" Polymers 17, no. 10: 1373. https://doi.org/10.3390/polym17101373
APA StyleFareed, M. M., & Shityakov, S. (2025). Next-Generation Hydrogel Design: Computational Advances in Synthesis, Characterization, and Biomedical Applications. Polymers, 17(10), 1373. https://doi.org/10.3390/polym17101373









