Impact of CAD/CAM Material Thickness and Translucency on the Polymerization of Dual-Cure Resin Cement in Endocrowns
Abstract
1. Introduction
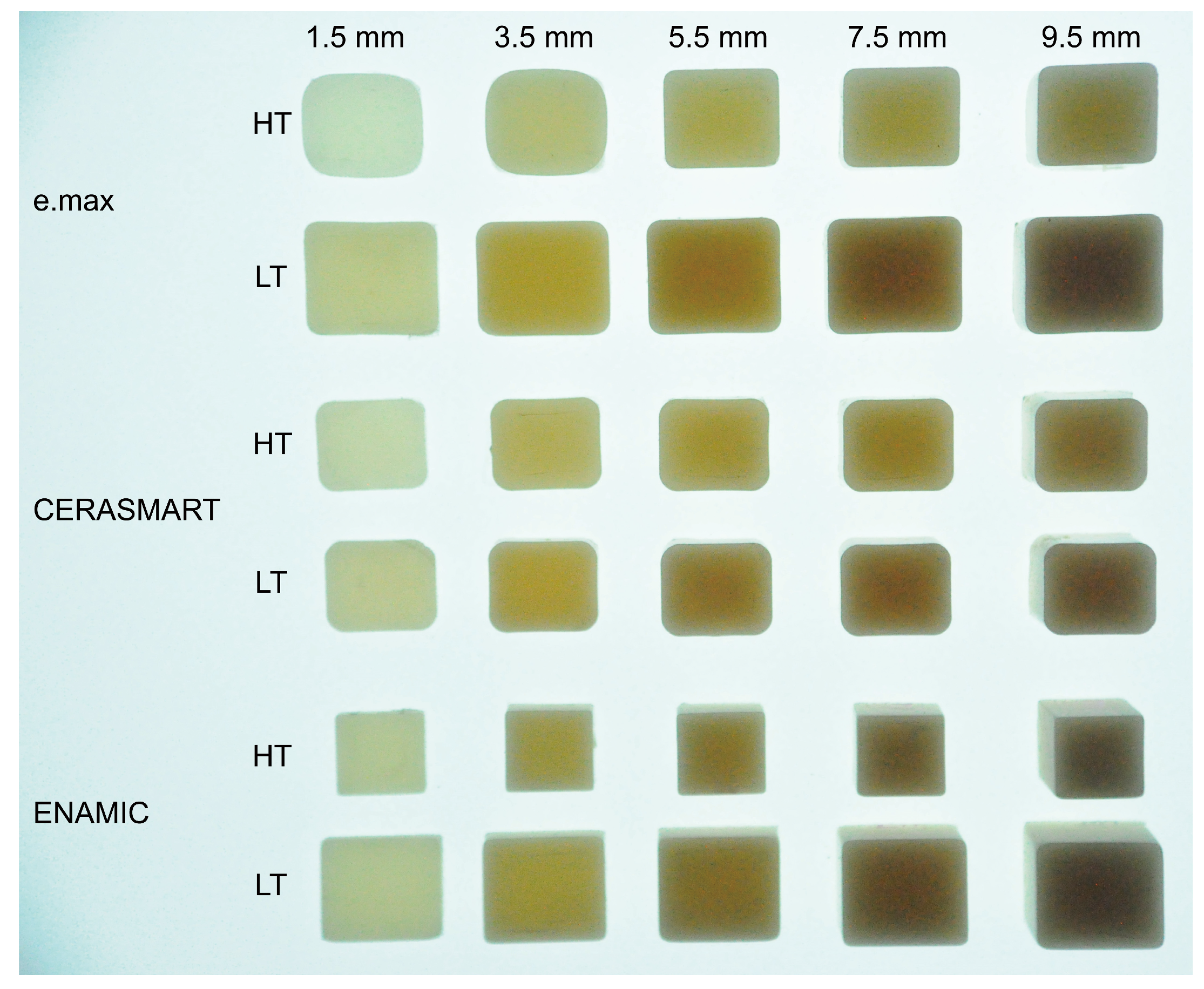
2. Materials and Methods
2.1. Materials
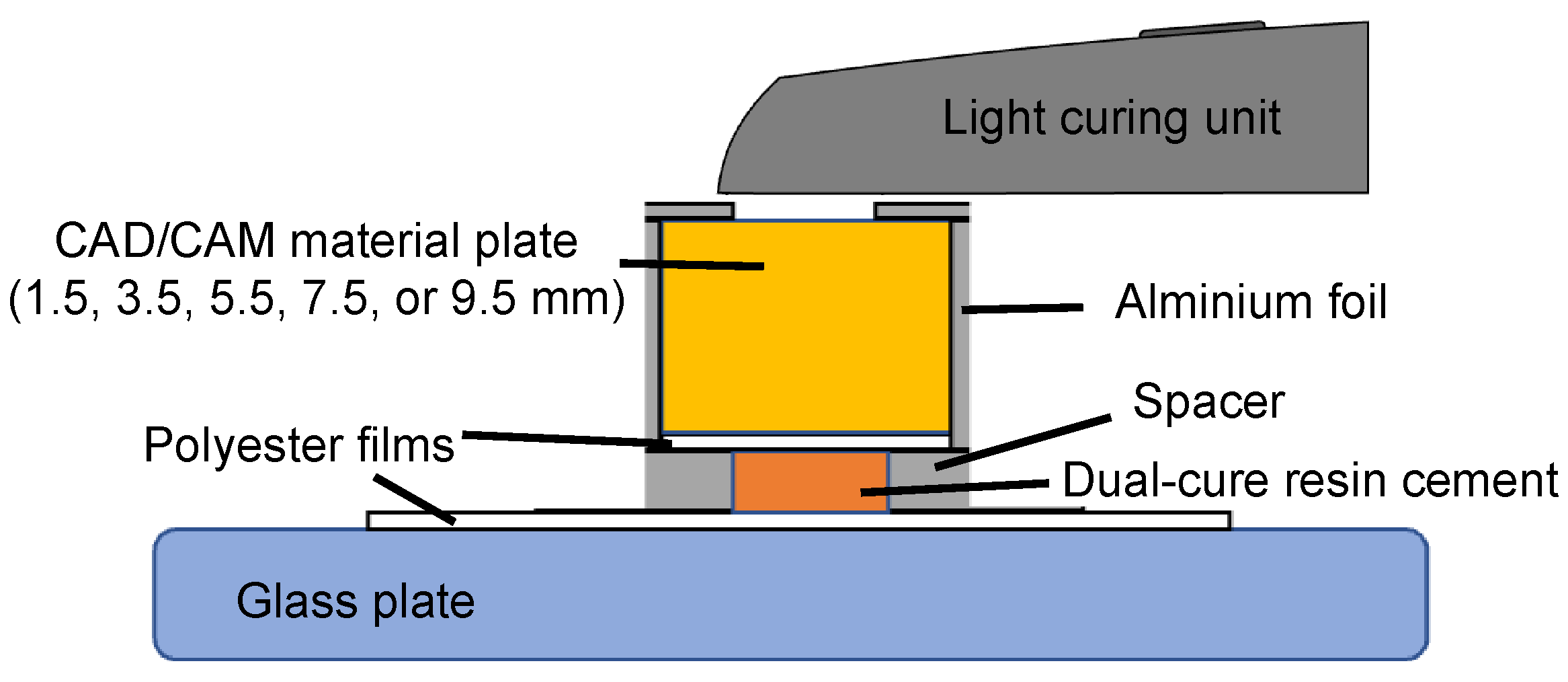
2.2. Photopolymerization of Dual-Cure Resin Cement and Post-Polymerization Treatment by Aging
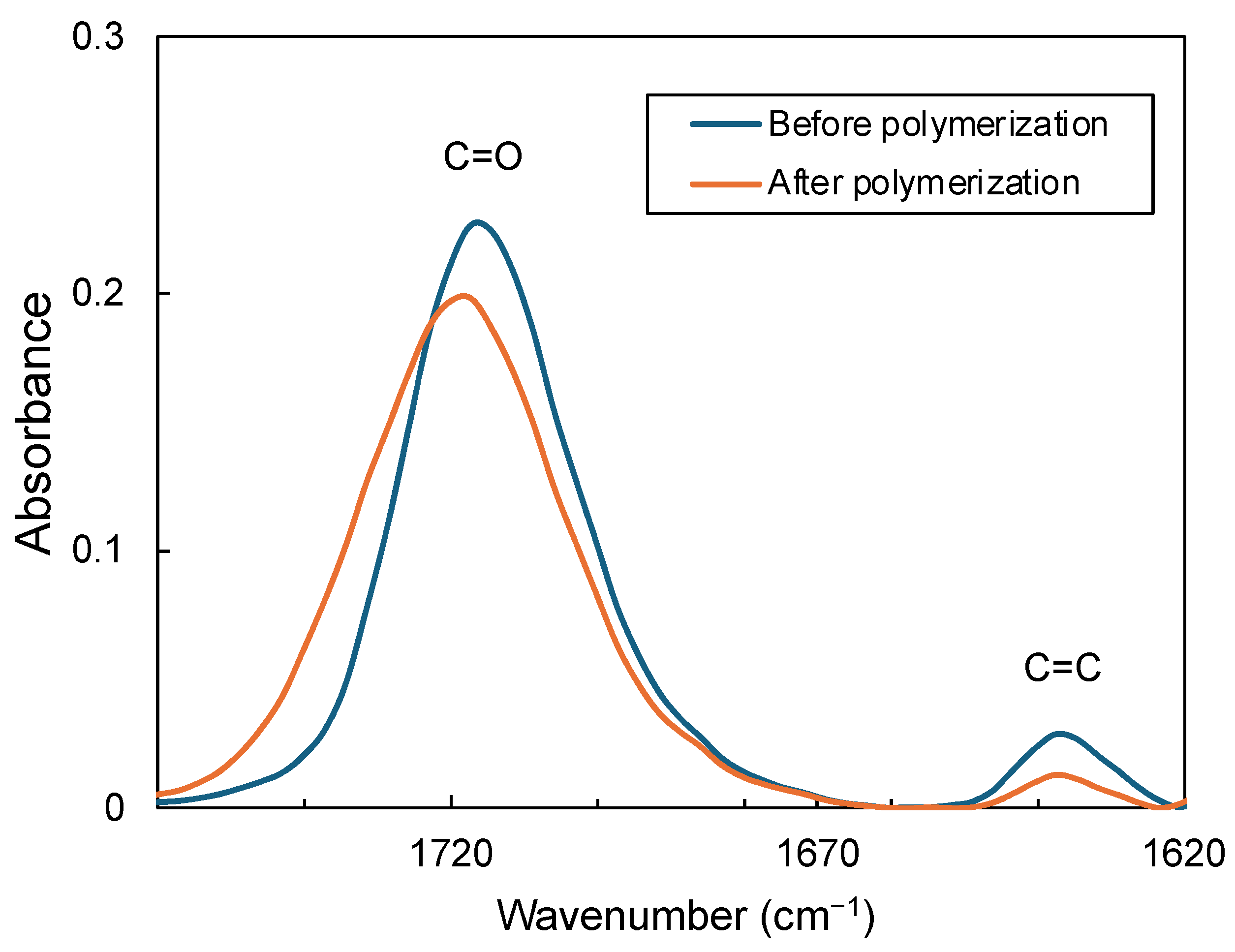
2.3. Fourier Transform Infrared (FTIR) Spectroscopy
2.4. Microhardness Test
2.5. Statistical Analysis
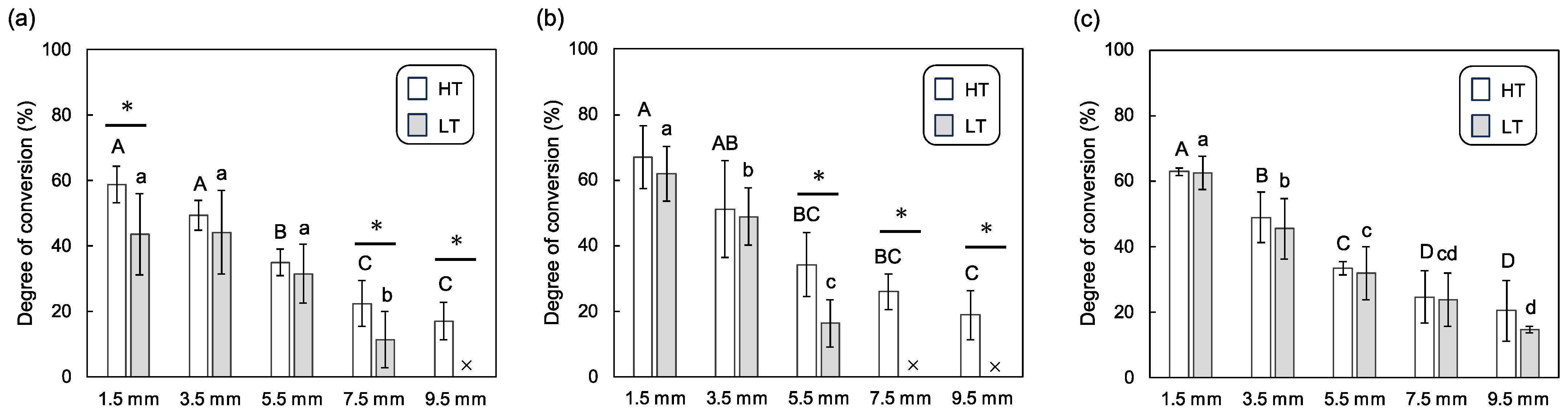
3. Results
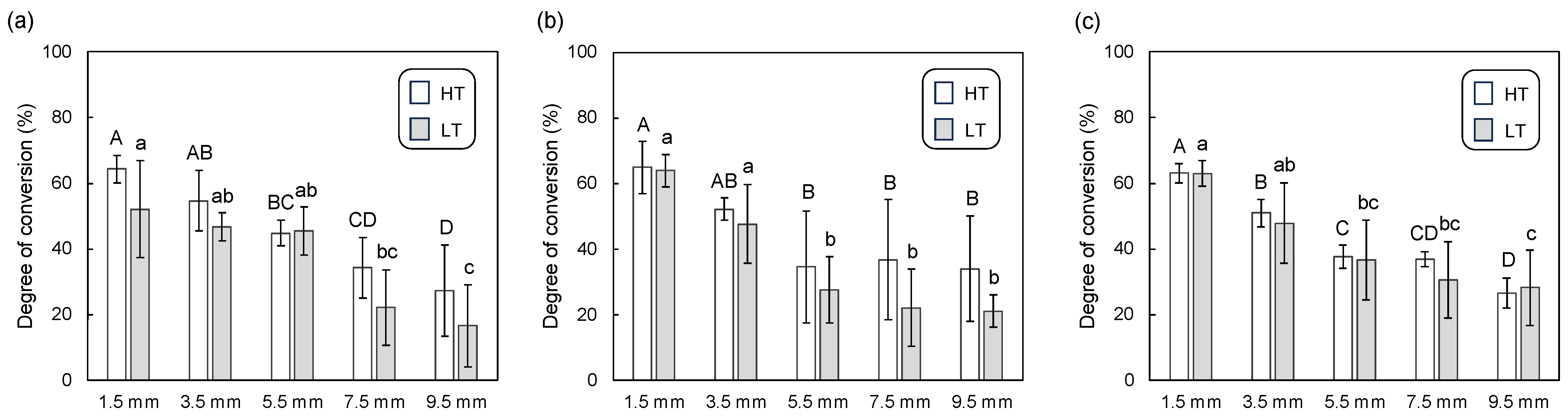
3.1. Degree of Conversion
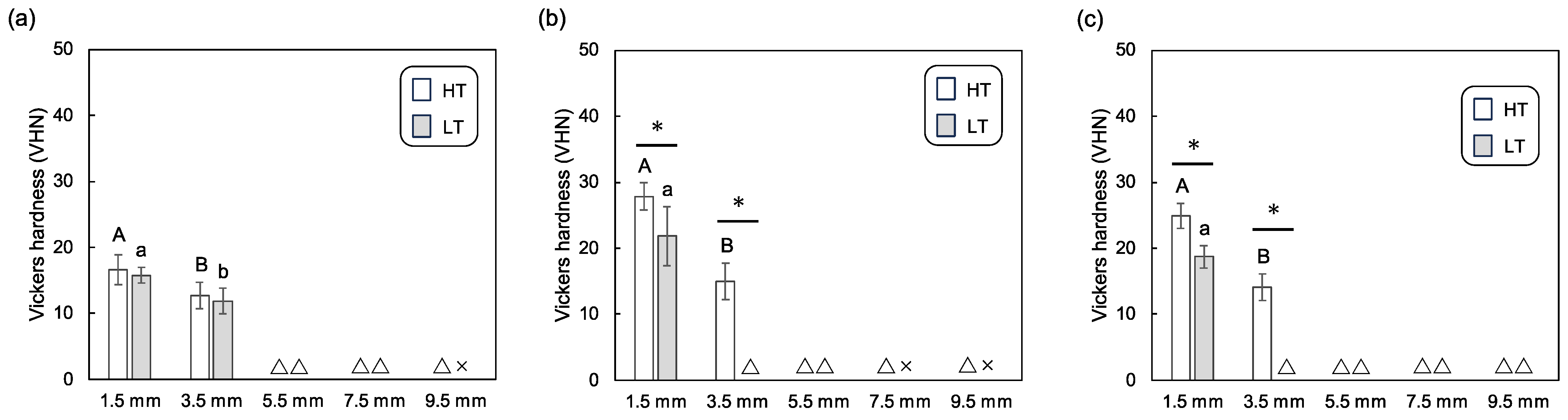
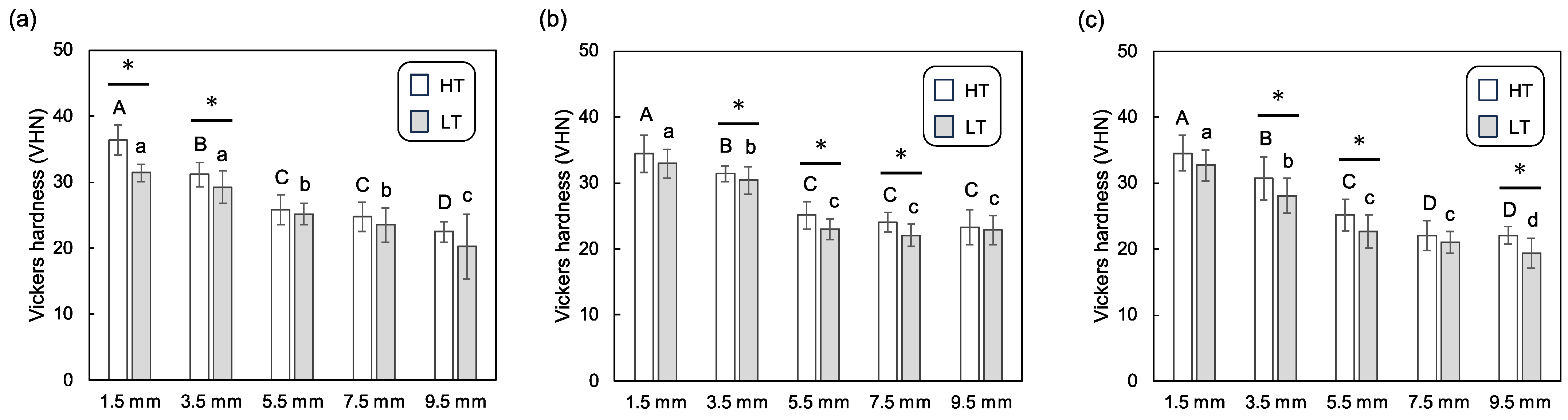
3.2. Vickers Hardness
4. Discussion
5. Conclusions
- Polymerization of the dual-cure resin cement decreased with increasing CAD/CAM material thickness, suggesting that thicker materials impeded the curing process.
- Significant differences in polymerization were observed between samples with a 1.5 mm thickness (conventional crowns) and those with a thickness of 5.5 mm or greater (endocrowns).
- The translucency grades influenced the polymerization of the dual-cure resin cement immediately after light irradiation. However, these differences were either eliminated or substantially reduced after post-polymerization treatment by aging.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Sedrez-Porto, J.A.; Rosa, W.L.; da Silva, A.F.; Munchow, E.A.; Pereira-Cenci, T. Endocrown restorations: A systematic review and meta-analysis. J. Dent. 2016, 52, 8–14. [Google Scholar] [CrossRef]
- Mannocci, F.; Bitter, K.; Sauro, S.; Ferrari, P.; Austin, R.; Bhuva, B. Present status and future directions: The restoration of root filled teeth. Int. Endod. J. 2022, 55 (Suppl. S4), 1059–1084. [Google Scholar] [CrossRef] [PubMed]
- European Society of Endodontology developed by; Mannocci, F.; Bhuva, B.; Roig, M.; Zarow, M.; Bitter, K. European Society of Endodontology position statement: The restoration of root filled teeth. Int. Endod. J. 2021, 54, 1974–1981. [Google Scholar] [CrossRef]
- El-Ma’aita, A.; AAl-Rabab’ah, M.; Abu-Awwad, M.; Hattar, S.; Devlin, H. Endocrowns Clinical Performance and Patient Satisfaction: A Randomized Clinical Trial of Three Monolithic Ceramic Restorations. J. Prosthodont. 2021, 31, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Vervack, V.; De Coster, P.; Vandeweghe, S. Clinical Evaluation of Resin Composite CAD/CAM Restorations Placed by Undergraduate Students. J. Clin. Med. 2021, 10, 3269. [Google Scholar] [CrossRef]
- Beji Vijayakumar, J.; Varadan, P.; Balaji, L.; Rajan, M.; Kalaiselvam, R.; Saeralaathan, S.; Ganesh, A. Fracture resistance of resin based and lithium disilicate endocrowns. Which is better?—A systematic review of in-vitro studies. Biomater. Investig. Dent. 2021, 8, 104–111. [Google Scholar] [CrossRef]
- Chistyakov, E.M.; Kolpinskaya, N.; Posokhova, V.; Chuev, V. Dental Composition Modified with Aryloxyphosphazene Containing Carboxyl Groups. Polymers 2020, 12, 1176. [Google Scholar] [CrossRef] [PubMed]
- Tyas, M.J.; Anusavice, K.J.; Frencken, J.E.; Mount, G.J. Minimal intervention dentistry—A review: FDI Commission Project 1–97. Int. Dent. J. 2000, 50, 1–12. [Google Scholar] [CrossRef]
- Mormann, W.H.; Bindl, A.; Luthy, H.; Rathke, A. Effects of preparation and luting system on all-ceramic computer-generated crowns. Int. J. Prosthodont. 1998, 11, 333–339. [Google Scholar]
- Pissis, P. Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract. Periodontics Aesthet. Dent. 1995, 7, 83–94. [Google Scholar]
- Bindl, A.; Mormann, W.H. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years-preliminary results. J. Adhes. Dent. 1999, 1, 255–265. [Google Scholar]
- Bernhart, J.; Brauning, A.; Altenburger, M.J.; Wrbas, K.T. Cerec3D endocrowns-two-year clinical examination of CAD/CAM crowns for restoring endodontically treated molars. Int. J. Comput. Dent. 2010, 13, 141–154. [Google Scholar]
- Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral Res. 2018, 32, e74. [Google Scholar] [CrossRef]
- Al-Dabbagh, R.A. Survival and success of endocrowns: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 415.e1–415.e9. [Google Scholar] [CrossRef]
- Thomas, R.M.; Kelly, A.; Tagiyeva, N.; Kanagasingam, S. Comparing endocrown restorations on permanent molars and premolars: A systematic review and meta-analysis. Br. Dent. J. 2020. [Google Scholar] [CrossRef]
- Sahebi, M.; Ghodsi, S.; Berahman, P.; Amini, A.; Zeighami, S. Comparison of retention and fracture load of endocrowns made from zirconia and zirconium lithium silicate after aging: An in vitro study. BMC Oral Health 2022, 22, 41. [Google Scholar] [CrossRef] [PubMed]
- Buyukerkmen, E.B.; Bozkurt, D.A.; Terlemez, A. Effect of surface treatment, ferrule height, and luting agent type on pull-out bond strength of monolithic zirconia endocrowns. J. Oral Sci. 2022, 64, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Papalexopoulos, D.; Samartzi, T.-K.; Sarafianou, A. A Thorough Analysis of the Endocrown Restoration: A Literature Review. J. Contemp. Dent. Pract. 2021, 22, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Gregor, L.; Bouillaguet, S.; Onisor, I.; Ardu, S.; Krejci, I.; Rocca, G.T. Microhardness of light- and dual-polymerizable luting resins polymerized through 7.5-mm-thick endocrowns. J. Prosthet. Dent. 2014, 112, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.; Ardu, S.; Kleverlaan, C.J.; DiBella, E.; Feilzer, A.J.; Krejci, I. Effect of light-curing time on microhardness of a restorative bulk-fill resin composite to lute CAD-CAM resin composite endocrowns. Am. J. Dent. 2020, 33, 331–336. [Google Scholar]
- de Kuijper, M.; Ong, Y.; Gerritsen, T.; Cune, M.S.; Gresnigt, M.M.M. Influence of the ceramic translucency on the relative degree of conversion of a direct composite and dual-curing resin cement through lithium disilicate onlays and endocrowns. J. Mech. Behav. Biomed. Mater. 2021, 122, 104662. [Google Scholar] [CrossRef] [PubMed]
- Viljanen, E.K.; Skrifvars, M.; Vallittu, P.K. Degree of conversion of a copolymer of an experimental monomer and methyl methacrylate for dental applications. J. Appl. Polym. Sci. 2004, 93, 1908–1912. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Garoushi, S.; Vallittu, P.; Lassila, L. Evaluation of flexible three-dimensionally printed occlusal splint materials: An in vitro study. Dent. Mater. 2023, 39, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Faria, E.S.A.L.; Pfeifer, C.S. Delayed photo-activation and addition of thio-urethane: Impact on polymerization kinetics and stress of dual-cured resin cements. J. Dent. 2017, 65, 101–109. [Google Scholar] [CrossRef]
- Kowalska, A.; Sokolowski, J.; Bociong, K. The photoinitiators used in resin based dental composite—A review and future perspectives. Polymers 2021, 13, 470. [Google Scholar] [CrossRef]
- Barcelos, L.M.; Braga, S.; Pereira, R.; Price, R.B.; Soares, C.J. Effect of Using Manufacturer-recommended Exposure Times to Photo-activate Bulk-fill and Conventional Resin-based Composites. Oper. Dent. 2023, 48, 304–316. [Google Scholar] [CrossRef]
- Aldhafyan, M.; Silikas, N.; Watts, D.C. Influence of curing modes on conversion and shrinkage of dual-cure resin-cements. Dent. Mater. 2022, 38, 194–203. [Google Scholar] [CrossRef]
- Pick, B.; Gonzaga, C.C.; Junior, W.S.; Kawano, Y.; Braga, R.R.; Cardoso, P.E. Influence of curing light attenuation caused by aesthetic indirect restorative materials on resin cement polymerization. Eur. J. Dent. 2010, 4, 314–323. [Google Scholar] [CrossRef]
- Zancope, K.; Borges, G.; Ribeiro, M.; Miranda, R.R.; Peres, T.S.; Soares, C.J. Influence of Mono- and Multiwave Light-curing Units on the Microhardness and Degree of Conversion of Light-cured Resin Cements. Oper. Dent. 2023. [Google Scholar] [CrossRef] [PubMed]
- Germscheid, W.; de Gorre, L.G.; Sullivan, B.; O’Neill, C.; Price, R.B.; Labrie, D. Post-curing in dental resin-based composites. Dent. Mater. 2018, 34, 1367–1377. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, F.; Vadini, M.; Capogreco, M.; D’Arcangelo, C.; D’Amario, M. Effect of Light-Sources and Thicknesses of Composite Onlays on Micro-Hardness of Luting Composites. Materials 2021, 14, 6849. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Papadogiannis, D.; Zinelis, S.; Eliades, G. Setting characteristics and mechanical properties of self-adhesive resin luting agents. Dent. Mater. 2017, 33, 344–357. [Google Scholar] [CrossRef]
- Dimitriadi, M.; Petropoulou, A.; Anagnostou, M.; Zafiropoulou, M.; Zinelis, S.; Eliades, G. Effect of curing mode on the conversion and IIT-derived mechanical properties of core build-up resin composites. J. Mech. Behav. Biomed. Mater. 2021, 123, 104757. [Google Scholar] [CrossRef]
- AlDabeeb, D.S.; Alakeel, N.S.; Al Jfshar, R.M.; Alkhalid, T.K. Endocrowns: Indications, Preparation Techniques, and Material Selection. Cureus 2023, 15, e49947. [Google Scholar] [CrossRef] [PubMed]
- Hiraba, H.; Nishio, K.; Takeuchi, Y.; Ito, T.; Yamamori, T.; Kamimoto, A. Application of one-piece endodontic crowns fabricated with CAD-CAM system to molars. Jpn. Dent. Sci. Rev. 2024, 60, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Zhan, D.; Xiang, J.; Li, L. Clinical research on restorations using CAD/CAM-fabricated monolithic zirconia endocrowns and post and core crowns after up to 5 years. Int. J. Comput. Dent. 2022, 25, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Bijelic-Donova, J.; Myyrylainen, T.; Karsila, V.; Vallittu, P.K.; Tanner, J. Direct Short-Fiber Reinforced Composite Resin Restorations and Glass-Ceramic Endocrowns in Endodontically Treated Molars: A 4-Year Clinical Study. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 284–295. [Google Scholar]
- Otto, T.; Mormann, W.H. Clinical performance of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns up to 12 years. Int. J. Comput. Dent. 2015, 18, 147–161. [Google Scholar]
- Vervack, V.; Keulemans, F.; Hommez, G.; De Bruyn, H.; Vandeweghe, S. A completely digital workflow for nanoceramic endocrowns: A 5-year prospective study. Int. J. Prosthodont. 2022, 35, 259–268. [Google Scholar] [CrossRef]
- Facenda, J.C.; Borba, M.; Corazza, P.H. A literature review on the new polymer-infiltrated ceramic-network material (PICN). J. Esthet. Restor. Dent. 2018, 30, 281–286. [Google Scholar] [CrossRef]
- Elashmawy, Y.; Elshahawy, W. Effect of Thermomechanical Fatigue Loading on the Internal and Marginal Adaptation of Endocrowns Utilizing Different CAD/CAM Restorative Materials. Int. J. Prosthodont. 2023, 36, 738–747. [Google Scholar] [CrossRef]
- Chen, T.A.; Lu, P.Y.; Lin, P.Y.; Chi, C.W.; Cheng, H.Y.; Lai, Y.J.; Wang, F.; Chiang, Y.C. Effects of ceramic thickness, ceramic translucency, and light transmission on light-cured bulk-fill resin composites as luting cement of lithium disilicate based-ceramics. J. Prosthodont. Res. 2023. [Google Scholar] [CrossRef]
- Martins, F.V.; Vasques, W.F.; Fonseca, E.M. How the Variations of the Thickness in Ceramic Restorations of Lithium Disilicate and the Use of Different Photopolymerizers Influence the Degree of Conversion of the Resin Cements: A Systematic Review and Meta-Analysis. J. Prosthodont. 2019, 28, e395–e403. [Google Scholar] [CrossRef]
- de Paula, V.G.; Bonfante, G.; Lorenzoni, F.C.; Coelho, P.G.; Bonjardim, L.R.; Fardin, V.P.; Bonfante, E.A. Lifetime prediction of veneered versus monolithic lithium disilicate crowns loaded on marginal ridges. Dent. Mater. 2019, 35, 511–522. [Google Scholar] [CrossRef]
- Jurado, C.A.; Pinedo, F.; Trevino, D.A.C.; Williams, Q.; Marquez-Conde, A.; Irie, M.; Tsujimoto, A. CAD/CAM lithium disilicate ceramic crowns: Effect of occlusal thickness on fracture resistance and fractographic analysis. Dent. Mater. J. 2022, 41, 705–709. [Google Scholar] [CrossRef]
- Hayes, A.; Duvall, N.; Wajdowicz, M.; Roberts, H. Effect of Endocrown Pulp Chamber Extension Depth on Molar Fracture Resistance. Oper. Dent. 2017, 42, 327–334. [Google Scholar] [CrossRef]
- Munoz-Sanchez, M.L.; Linas, N.; Decerle, N.; Nicolas, E.; Hennequin, M.; Cousson, P.Y. A Combination of Full Pulpotomy and Chairside CAD/CAM Endocrown to Treat Teeth with Deep Carious Lesions and Pulpitis in a Single Session: A Preliminary Study. Int. J. Environ. Res. Public Health 2020, 17, 6340. [Google Scholar] [CrossRef]
- Zhang, Y.; Lai, H.; Meng, Q.; Gong, Q.; Tong, Z. The synergetic effect of pulp chamber extension depth and occlusal thickness on stress distribution of molar endocrowns: A 3-dimensional finite element analysis. J. Mater. Sci. Mater. Med. 2022, 33, 56. [Google Scholar] [CrossRef]
- Huang, Y.; Fokkinga, W.A.; Zhang, Q.; Creugers, N.H.J.; Jiang, Q. Biomechanical properties of different endocrown designs on endodontically treated teeth. J. Mech. Behav. Biomed. Mater. 2023, 140, 105691. [Google Scholar] [CrossRef]
- Bindl, A.; Richter, B.; Mormann, W.H. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int. J. Prosthodont. 2005, 18, 219–224. [Google Scholar] [CrossRef]
- Malysa, A.; Wezgowiec, J.; Grzebieluch, W.; Danel, D.P.; Wieckiewicz, M. Effect of Thermocycling on the Bond Strength of Self-Adhesive Resin Cements Used for Luting CAD/CAM Ceramics to Human Dentin. Int. J. Mol. Sci. 2022, 23, 745. [Google Scholar] [CrossRef] [PubMed]
- Kelch, M.; Stawarczyk, B.; Mayinger, F. Time-dependent degree of conversion, Martens parameters, and flexural strength of different dual-polymerizing resin composite luting materials. Clin. Oral Investig. 2022, 26, 1067–1076. [Google Scholar] [CrossRef] [PubMed]
| Material Type | Product Name | Product Company | Composition |
|---|---|---|---|
| Lithium disilicate glass | IPS e.max CAD | Ivoclar Vivadent, Schaan, Liechtenstein | SiO2, Li2O, K2O, P2O5, ZrO2, ZnO, Al2O3, MgO, Coloring oxide |
| Resin composite | CERASMART300 | GC Corp., Tokyo, Japan | SiO2, Barium glass, urethane dimethacrylate, 2,2-bis(4-methacryloxypolyethoxyphenyl)propane |
| Polymer-infiltrated ceramic network | VITA ENAMIC | VITA Zahnfabrik, Nabertherm, Germany | SiO2, Al2O3, Polymer, Na2O, K2O, B2O3, ZrO2, CaO |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ikemoto, S.; Komagata, Y.; Yoshii, S.; Masaki, C.; Hosokawa, R.; Ikeda, H. Impact of CAD/CAM Material Thickness and Translucency on the Polymerization of Dual-Cure Resin Cement in Endocrowns. Polymers 2024, 16, 661. https://doi.org/10.3390/polym16050661
Ikemoto S, Komagata Y, Yoshii S, Masaki C, Hosokawa R, Ikeda H. Impact of CAD/CAM Material Thickness and Translucency on the Polymerization of Dual-Cure Resin Cement in Endocrowns. Polymers. 2024; 16(5):661. https://doi.org/10.3390/polym16050661
Chicago/Turabian StyleIkemoto, Soshi, Yuya Komagata, Shinji Yoshii, Chihiro Masaki, Ryuji Hosokawa, and Hiroshi Ikeda. 2024. "Impact of CAD/CAM Material Thickness and Translucency on the Polymerization of Dual-Cure Resin Cement in Endocrowns" Polymers 16, no. 5: 661. https://doi.org/10.3390/polym16050661
APA StyleIkemoto, S., Komagata, Y., Yoshii, S., Masaki, C., Hosokawa, R., & Ikeda, H. (2024). Impact of CAD/CAM Material Thickness and Translucency on the Polymerization of Dual-Cure Resin Cement in Endocrowns. Polymers, 16(5), 661. https://doi.org/10.3390/polym16050661






