1. Introduction
Since Brannemark’s fortuitous discovery of osseointegration in 1952, and from the 1970s onwards, significant efforts have been invested in developing dental implants, which have become an indispensable part of today’s dentistry [
1]. Long-term global studies show that the survival rate of implants is 96.1% (95% CI: 87.3, 98.9%) at five years [
1,
2,
3,
4].
Dental implants comprise a system in which an alloplastic device surgically inserted in the alveolar ridge is connected through an abutment to a superstructure (implant-supported prosthesis) that replaces the missing tooth [
5]. Part of the successful survival of dental implants will depend on the transmucosal region, the transition zone separating the osseointegrated implant in the bone, and the prosthetic tooth exposed to the oral cavity. This transmucosal region contains gingival fluids, saliva, and bacteria and mainly comprises epithelium and connective tissue [
6].
The sealing of the peri-implant tissue is a determining factor in long-term implant survival [
5,
7]. The architecture of peri-implant soft tissues is similar to that established around natural teeth [
8], composed of a sulcus, junctional epithelium, and with connective tissue insertion. However, their histological features differ in several aspects. The peri-implant epithelium is not similar to the junctional epithelium around the teeth. However, it has some similarities, establishing a hemidesmosomes junction between the epithelial cells and the implant surface. The sulcus is slightly larger, from 1 mm around natural teeth to 3–4 mm in dental implants [
9]. The connective tissue shows differences in the arrangement of collagen fibers, which form a dense network oriented parallel to the abutment surface, as well as less cellular and vascular proliferation [
8].
In healthy conditions, a mucosal seal is formed around the teeth that do not allow access to aggressive microflora to the underlying bone during tooth eruption. In the case of peri-implant tissues, once they have completed their healing, an effective mucosal seal forms around the transmucosal portion of the implant [
10,
11]. The hemidesmosomes present at the epithelial junction, immune cells, and the mechanical buffering of the connective tissue ensure a protective mechanical and biological barrier to the underlying bone at this location [
8,
12]. However, the constant exposure of tissues to microorganisms in the oral cavity makes mucosal healing around transmucosal abutments a significant challenge [
10].
The characteristics of peri-implant connective tissue (lower cellularity and vascularity and the parallel arrangement of collagen fibers) could make supracrestal soft tissues more susceptible to peri-implant disease and its progression [
8]. In the dental implant region, the ideal healing and regenerative process involves rapid revascularization and effective neoangiogenesis to promote the formation of connective tissue and bone around the implant. The presence of blood vessels is crucial to supply nutrients, oxygen, and immune cells, as well as to facilitate the bone remodeling process. Differences in the arrangement of collagen fibers around implants, with an orientation parallel to the implant abutment and less cellular and vascular proliferation, can negatively affect osseointegration and long-term implant stability. Prevascularized spheroids could improve this environment by providing a scaffold for cell growth and orientation, as well as promoting enhanced neoangiogenesis [
13]. For example, if prevascularized spheroids are incorporated into the implant site, they could help establish a microvascular network in the tissue surrounding the implant abutment. This network could enhance the integration and proliferation of connective tissue cells, as well as facilitate the formation of a well-structured collagen network that improves implant support and stability. Furthermore, improved vascularization may lead to a better immune response and accelerate tissue healing and regeneration. Maintenance of the soft tissue peri-implant is essential to preserve long-term oral health and ensure the success of dental implants [
8,
12,
14].
Once osseointegration is consolidated, the main concern is to avoid peri-implant disease: mucositis and peri-implantitis. Bleeding during soft probing (<0.25 N) is the primary indicator to diagnose the presence of mucositis [
15]. The histopathologic and clinical conditions that lead to conversion from mucositis to peri-implantitis are not entirely clear, but it is known that mucositis is the precursor to peri-implantitis [
15,
16]. Peri-implantitis is a pathologic condition of peri-implant tissues, characterized by the inflammation of connective tissue and progressive and irreversible bone loss [
16]. The bacterial biofilm adhering to the implant–abutment surfaces and the host response are responsible for triggering the inflammatory response [
4]. The disease progresses in a nonlinear and accelerating pattern, leading to the loss of peri-implant bone support [
16]. Several studies suggest achieving a better mucosal seal that prevents the passage of bacteria and less bacterial colonization by modifying the biomaterials’ surface to make transepithelial abutments (polished surfaces, drugs, etc.) [
6,
12,
17]. Zirconium (zirconium oxide or zirconia) has gained popularity in dental practice, especially for the fabrication of implant abutments and prostheses due to its good aesthetics and biocompatibility. Zirconia has been documented to have low plaque retention, which is an important contributing factor in preventing bacterial growth and, therefore, may have positive implications in decreasing the risk of infection and peri-implant disease [
18,
19]. Similarly, dental ceramics are well-known for their excellent aesthetic properties and resistance to wear and corrosion. In terms of antibacterial properties, some ceramics may have a surface that discourages bacterial adhesion, which helps to maintain good health in the tissue surrounding the implant. However, its antibacterial efficacy can vary and is highly dependent on the surface roughness and chemical composition of the material [
18]. On the contrary, PMMA does not have inherent antibacterial properties. However, it can be modified by the incorporation of antimicrobial agents, such as metal nanoparticles (e.g., silver or copper) or other antibacterial additives to improve its resistance to bacterial colonization [
19,
20]. Some have obtained promising results, such as modulating and orienting epithelial tissues to achieve more excellent soft tissue sealing by modifying the surface with technologies that are not yet on the market [
6]. However, it should be taken into account that the transmucosal region is not only in contact with the transepithelial abutment but also the cervical fraction of the prosthetic crown, which will be submerged and in contact with these tissues. Thus, the mucointegration of the peri-implant soft tissues will also be influenced by the biomaterial’s surface used for prosthetic restoration.
In recent decades, the number of restorative materials for implant-supported prostheses has increased significantly. Ceramics have gained great popularity due to their many advantages, such as high biocompatibility, more natural appearance, and metal-free structure. Thus, they are characterized by translucency, color stability, low plaque adhesion, wear resistance, and low thermal conductivity [
18]. In vitro studies have indicated that they are materials that induce favorable biological responses and exhibit excellent long-term stability [
18]. Among ceramic materials, zirconium dioxide has become one of the most widely used restorative materials due to its low cost and high strength [
17], and it is known for its high biocompatibility and chemical stability, which contributes to low inflammation and good integration with gingival tissues [
18,
21]. Zirconia is resistant to corrosion in the moist and acidic environment of the mouth, which helps to maintain its structural stability over time [
18]. Similarly, modern materials, such as IPS e.max lithium disilicate from Ivoclar Vivadent, which stands out for its translucent color and good durability, are also available on the market. Both materials can be milled in monobloc using CAD–CAM (computer-aided design–computer-aided manufacturing) technology, which reduces the number of appointments and increases the precision of the final restoration [
17].
On the other hand, the materials used for temporary restorations have significantly advanced in their aesthetic and functional characteristics. However, due to their short time in the mouth, their biological properties have been little studied. In a previous study, our team compared the tissue response to materials used as prosthetic temporaries, focusing on histological analysis of the reaction of keratinized tissue, connective tissue, and the inflammatory response to temporary restorations on dental implants [
22]. These materials have a long history of use in dentistry but can be susceptible to fracture and crack formation, potentially compromising their stability [
20]. They are known to be modified to improve their mechanical properties and resistance to bacterial biofilm growth. However, in their unmodified form, they may not be as stable as ceramic materials or zirconia, especially when subjected to repetitive chewing loads [
20]. The stability of these materials also depends on factors such as the design and fabrication of the prosthesis or implant component, patient compliance with care protocols, and precision in fabrication.
It is, therefore, necessary to know whether the biological response generated in the peri-implant soft tissues by provisional materials is similar to that found in the case of the use of definitive restorative materials during the phase of formation and establishment of the surrounding mucosa. On the other hand, the use of monolithic materials seems to present advantages over conventionally veneered ones [
23].
This study compares the tissue response generated by definitive prosthetic restorative materials and temporary polymeric materials from a histological point of view. For this purpose, new histological data on connective tissue composition, keratinized epithelium and non-keratinized epithelium, and the inflammatory response to lithium disilicate (IPS™ e.Max CAD LT®, IVOCLAR Vivadent, Madrid, Spain), zirconium oxide (Cercon xt ML Multilayer®, Dentsply Sirona, Barcelona, Spain), and PMMA (Telio CAD®, Ivoclar Vivadent, Madrid, Spain) are examined. This study aimed to determine the influence of these materials on the formation of adhesive structures for sealing the peri-implant mucosa as well as determine which definitive restorative material favors a better tissue response. The null hypothesis of the present study is that the biological response generated in the peri-implant tissues is similar to restorations made of temporary and definitive materials.
2. Materials and Methods
2.1. Type of Study
The current study is a prospective observational cohort study involving the for-mation of three distinct groups.
This study was approved by the Andalusian Biomedical Research Ethics Coordi-nating Committee (Code US-DTL-2022.1) and complies with all the guidelines of the World Medical Association Declaration of Helsinki: Ethical Principles for Medical Re-search Involving Human Subjects [
24]. In compliance with this, all patients received the information sheet and gave informed consent for the intervention in question and par-ticipation in the project.
The patients’ only invasive procedure was the biopsy of the peri-implant tissues of those restorations whose crowns were made of the materials to be studied.
2.2. Samples
A group of patients requiring implant-supported prosthetic rehabilitation in the posterior sectors (from premolars to molars) of both arches (maxilla and mandible) were selected.
These were selected after applying the following inclusion and exclusion criteria:
Inclusion criteria.
- ○
Patients over 18 years of age;
- ○
Patients with posterior partial edentulism requiring implant-supported prosthetic restorations;
- ○
Patients who do not present any absolute contraindication for the placement of dental implants;
- ○
Patients without active periodontal disease.
Exclusion criteria.
- ○
Patients who are smokers (>10 cigarettes/day);
- ○
Patients with pathology or undergoing treatment that alters bone metabolism or soft tissue healing;
- ○
Patients with poor oral hygiene;
- ○
Patients with uncontrolled periodontal disease;
- ○
Patients with alcoholism or drug problems.
2.3. Surgical Protocol for the Placement of Dental Implants
All surgeries were performed by the same oral surgeon without complications. All patients were administered local anesthesia (articaine hydrochloride + epinephrine; Ar-tinibsa® 40 mg/mL + 0.01 mg/mL; Inibsa dental, Barcelona, Spain). Once the area was anesthetized, a mid-crestal incision was made, preserving 2 mm of keratinized tissue on both sides of the incision. A small full-thickness flap was elevated, and the implant bed was prepared with abundant saline irrigation.
The Astra EV system (Astra Tech Implant System® EV, Dentsply Sirona S.A., Barcelona, Spain) is a bone-level dental implant with a defined rough surface, obtained by a patented titanium bombardment technique, followed by a process including treatment in dilute hydrofluoric acid. The external part of the collar has micro threads (MicroThread). The type of connection is a conical connection between the implant and the abutment for a firm and stable connection between them (Conical Seal Design).
The diameter of the implants ranged from 3.6 mm to 4.8 mm, depending on the tooth to be replaced and bone availability.
To avoid a second access surgery and take into account the individual conditions of each patient, a healing abutment was screwed in, which had been previously chosen based on the patient’s gingival height.
2.4. Description of Restorative Materials
The materials chosen for the fabrication of the prosthetic restorations, according to their properties and purpose, were as follows:
Cercon xt ML Multilayer® (Dentsply Sirona, Barcelona, Spain): an extra translucent multilayer zirconia consisting mainly of zirconium oxide, yttrium oxide 9%, and hafnium oxide <3% (aluminum oxide, silicon oxide, and other oxides <2%). It presents a translucency of 49% (being one of the most translucent zirconia) and a range of colors composed of 16 shades of VITA®2 and BL2, achieving a realistic aesthetic. This monobloc presentation allows the use of the CAD–CAM system, facilitating production.
IPS™ e.Max CAD LT® (Ivoclar Vivadent, Madrid, Spain): a glass ceramic formed by a microstructure of lithium disilicate crystals embedded in a glass matrix, used for the fabrication of crowns or as a coating for a metal core. Its characteristics allow a minimally invasive preparation and the use of the CAD–CAM system, achieving adequate adjust-ments. It stands out for its excellent aesthetic properties (desired opalescence, translucency), mechanical properties (high fracture resistance and adaptation), and high technical tolerance. Thanks to the anterior and the assortment of IPS™ e.Max CAD blocks comprising a selection of shades and levels of translucency, great clinical results are achieved. In addition, its durability and enamel-like wear rate make it a very suitable material.
Telio CAD® (Ivoclar Vivadent, Madrid, Spain): blocks of cross-linked polymethyl methyl methacrylate (PMMA) designed for the fabrication of long-term temporary restorations (up to 12 months) using the CAD–CAM system. Its industrial polymerization process makes it highly homogeneous, avoiding polymerization shrinkage. Its physical properties include resistance to bending and fracture (130 ± 10 MPa), almost total transparency, low water absorption, and low density. Its aesthetic properties include its range of colors and lasting stability. At the same time, its advantages, such as ease of repair and good marginal adaptation, should be valued. Its finishing and fitting can be performed with conventional tungsten carbide cross-cutting burs.
2.5. Design and Fabrication of Restorations
Once the three months of osseointegration had elapsed, digital measurements were taken using the Primescan™ intraoral scanner (Software Connect 5.1, Dentsply Sirona S.A., Barcelona, Spain) for the design on Atlantis titanium nitride abutments (Dentsply Sirona S.A., Barcelona, Spain).
Once the abutment design was completed, the prosthetic crowns were fabricated. The restorations were fabricated from zirconia (Cercon xt ML®), lithium disilicate (IPS™ e.Max CAD LT®), or PMMA (Telio CAD®). They were aesthetically and functionally adapted to the abutment design, the antagonist arch, and the adjacent teeth.
The design of the restorations was extended more than 2 mm subgingivally to ensure the contact of the restorative material and the peri-implant mucosa. To obtain as smooth a surface as possible and thus avoid bacterial adhesion, all restorations were polished with a silicone disc (Edenta Exa Cerapol UM, EDENTA AG, Hauptstrasse 7, CH-9434 AU/SG, Switzerland), a mounted goat hair disc brush, and finally, a felt disc.
The crowns were cemented onto the Atlantis abutments out of the mouth with Relyx dual-type resin cement (Relyx™ Unicem 2 Automix Self-Adhesive Resin Cement, 3M Oral Care, 2510 Conway Avenue, St. Paul, MN 55144-1000 USA) for the definitive restorative materials and with zinc oxide–eugenol for the temporary material.
Subsequently, all the restorations were screwed at a torque force of 25 Ncm2, according to the manufacturer’s recommendation.
2.6. Biopsy
All biopsies were taken between 21 January 2021 and 28 July 2021, with an average of 180 days from the placement of the restoration of the material to be studied. The protocol was performed under local anesthesia (lidocaine 2% and epinephrine 1:100,000, Xilonibsa, Inibsa, Barcelona, Spain). Once the area was anesthetized, the sample was taken through an external bevel incision up to the vestibular epithelium in contact with the material, measuring 1–2 × 4–5 mm. Finally, the sample was preserved in a sterile jar with 40% formalin and sample coding for single-blind analysis.
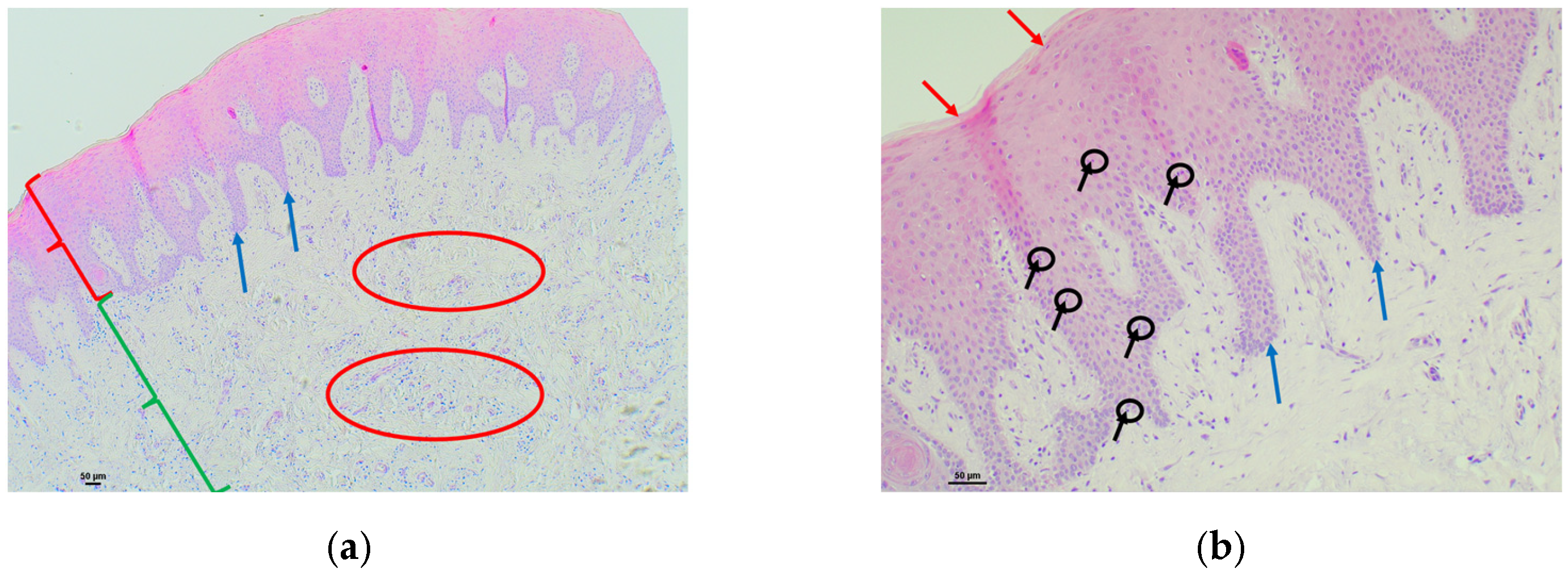
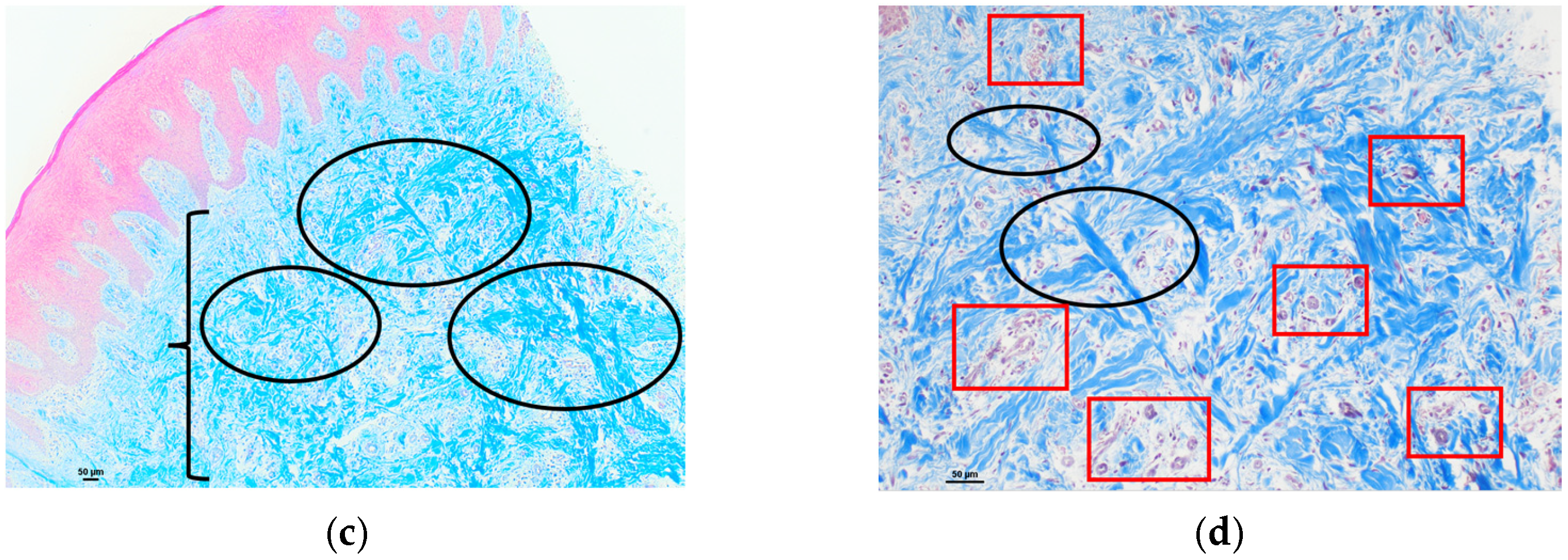
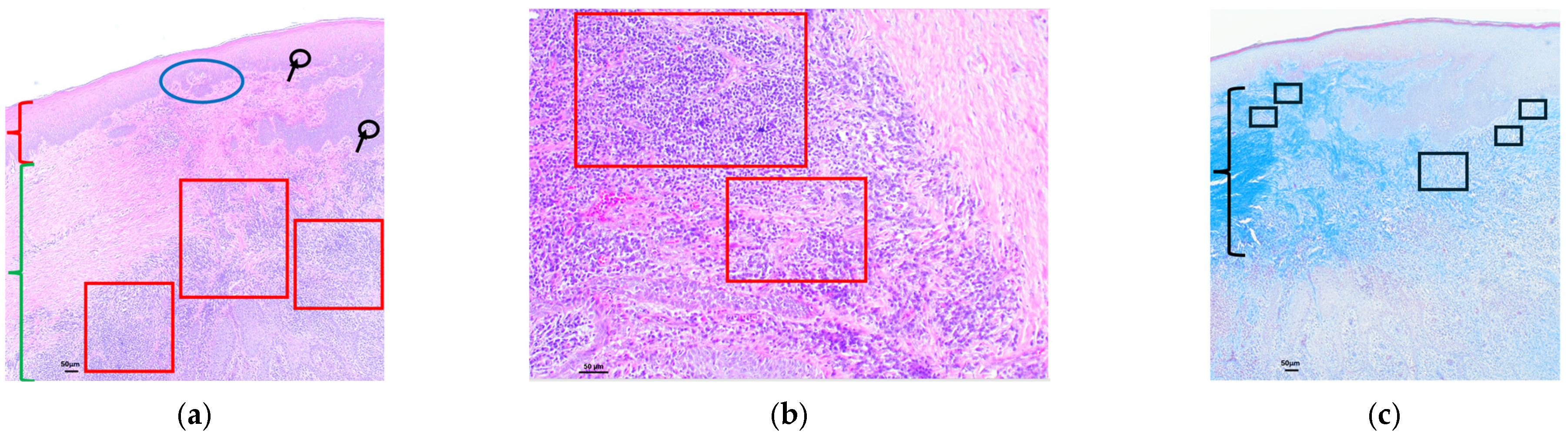
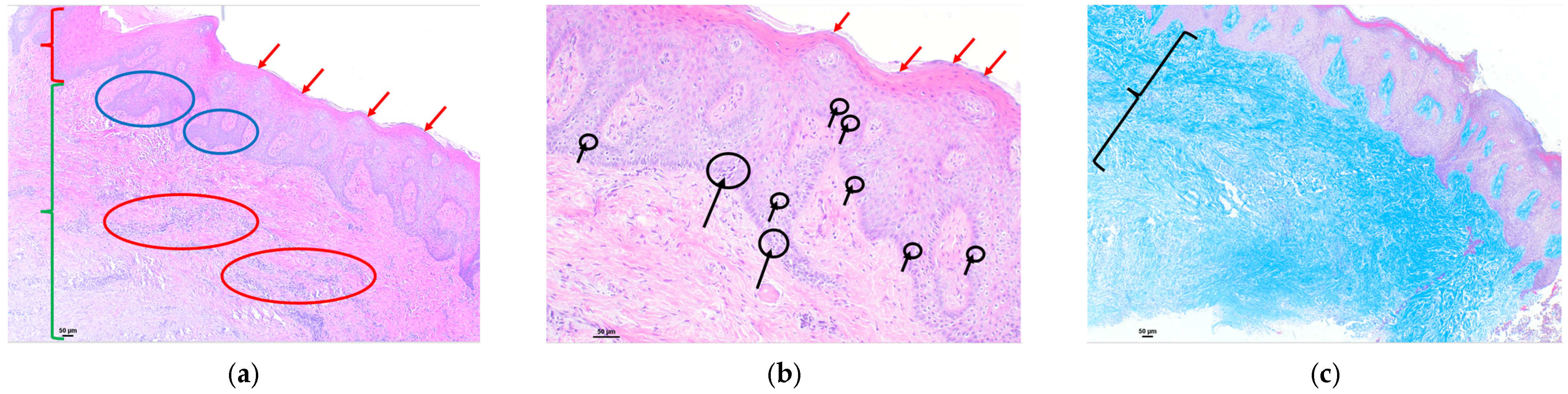
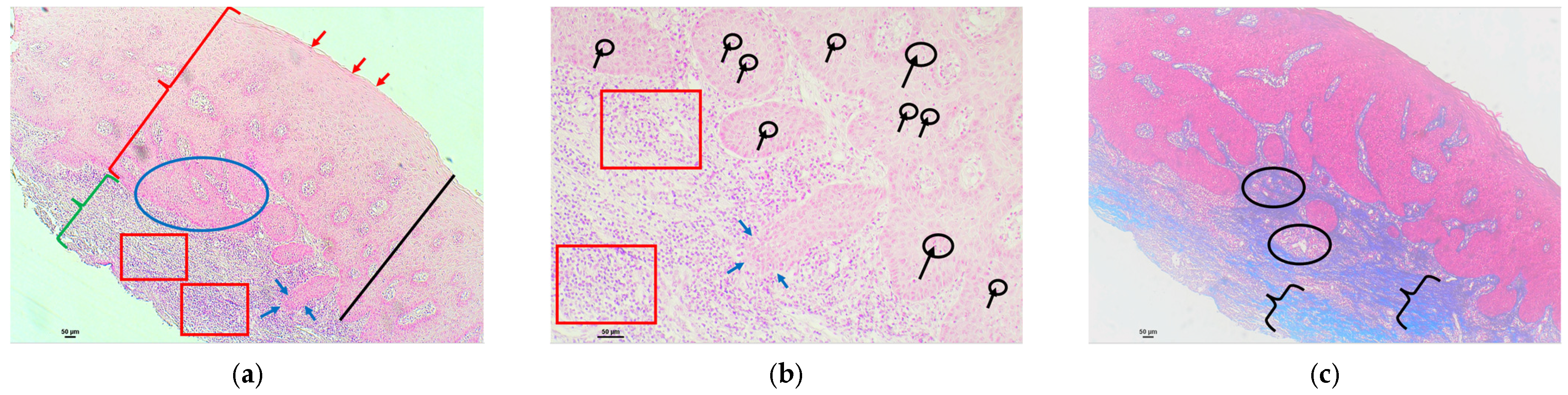
Each sample was processed in 4 mm sections fixed in formalin for embedding in kerosene. Subsequently, staining was performed with hematoxylin–eosin and Masson’s trichrome. The former allowed the identification of changes in the vascular and cellular components of the epithelium and connective tissue, while the latter showed the collagen fibers.
All histological sections were digitally archived by taking photographs (Color Camera Nikon DS-Fi3, v. 100.06.3307.E9) under the optical microscope at different magnifications OLYMPUS VANOX AHBT3 (Olympus Corp., Tokyo, Japan)with 4×, 10×, 20×, and 40× objective lenses.
Subsequent image processing was performed with NIS Elements Imaging Software (v.5.21.00).
After the biopsies had been taken, those patients who had been fitted with a tem-porary PMMA restoration (Telio CAD®) had a definitive restoration made of zirconium oxide (IPS e.max ZirCAD™ Multi, IVOCLAR Vivadent, Madrid, Spain) cemented onto the previously screw-retained Atlantis abutment.
Finally, to ensure proper surgical site healing, all patients were revisited one month after the biopsy.
2.7. Statistical Analysis
Four dichotomous crosses were performed: zirconium/disilicate (together) vs. PMMA, zirconium vs. PMMA, disilicate vs. PMMA, and zirconium vs. disilicate.
2.7.1. Descriptive Analysis
A complete descriptive analysis of the following variables was performed:
Qualitative:
- ○
Primary location of inflammatory activity in the epithelium;
- ○
Lateral cellular composition of the inflammatory activity;
- ○
Cellular composition of the inflammatory activity;
- ○
Number of connective tissue collagen fibers;
- ○
Arrangement of the collagen fibers of the connective tissue;
- ○
Vascular proliferation of connective tissue.
Quantitative:
- ○
Increased thickness of keratinized epithelium;
- ○
Size of the ridges in the keratinized epithelium (mm);
- ○
Exocytosis. Number of lymphocytes per mm2 in the keratinized epithelium;
- ○
Exocytosis. Number of nuclear polymorphs per mm2 in the keratinized epithelium;
- ○
Exocytosis. Total number of cells per mm2 in the keratinized epithelium;
- ○
Parakeratosis. Exocytosis. Number of nuclei per mm2 in the keratinized epithelium;
- ○
Increased thickness of the non-keratinized epithelium (mm);
- ○
Size of the ridges in the non-keratinized epithelium;
- ○
Intensity of inflammatory activity. Percentage of inflammatory cells;
- ○
Number of connective tissue papillae.
2.7.2. Normality of Numerical Variables
The Kolmogorov–Smirnov test was applied to determine normality.
2.7.3. Cross-Tabulation of the Material and Qualitative Variables
The Chi2 test was carried out.
To determine the groups that make the difference, we used Haberman’s corrected typified residuals, which allowed us to obtain the significance of the cells independently; this significance implies that the percentage of the cell is statistically different from that corresponding to the total sample.
2.7.4. Cross-Tabulation of the Material and Numerical Variables
A one-way ANOVA was applied for normally distributed variables and the Kruskal–Wallis test for the rest.
4. Discussion
After implant insertion surgery, cells at the edges of the incision increase and adhere to the implant surface. These can produce basal lamina and hemidesmosomes, creating an epithelial junction similar to the junctional epithelium of natural teeth [
8]. Abrahamsson, in 2002 [
25], in a study on dogs, showed that, regardless of the type of abutment, a similar epithelial junction was formed, consisting mainly of a thin epithelium and connective tissue rich in fibroblasts in its most apical region. Similarly, other authors have shown in minipigs how zirconium oxide and titanium abutments allow soft tissue integration [
26]. However, these studies do not consider the prosthetic restorative material. The most apical region of implant-supported crowns and bridges is subgingival, being in intimate contact with the peri-implant soft tissues. For this reason, the present study aims to compare the biological response generated in the peri-implant soft tissue by materials used for temporary restorations versus materials used in implant-supported definitive restorations and their influence on the improvement of the formation of adhesive structures for sealing the peri-implant mucosa.
Several authors have observed increased collagen fibers in the peri-implant tissue (Ivanovski and Lee, Flores, Deraz). The different causes of this increase may be due to the chemical modification of the abutment surface [
8,
27] or the compressive loads generated around a loaded implant [
24]. However, Flores et al. (2021) [
28] demonstrated a significant increase in type V collagen fibers in peri-implant tissues affected by peri-implantitis. Similarly, Deraz et al. (2021) [
29] found excessive collagenization of connective tissue in all peri-implantitis cases. Some studies argue that the peri-implant connective tissue, rather than a defense structure, is a chronic inflammatory involvement because it has many collagenase-resistant type V collagen fibers [
9]. The present study shows that zirconia presents a normal distribution of collagen fibers in 90–95% of the cases.
The hallmarks of chronic inflammation are continued tissue damage, chronic inflammatory infiltration, and excess fibrous connective tissue (fibrosis). An infiltrate of lymphocytes, macrophages, and plasma cells characterizes the chronic inflammatory reaction. When it is a chronic non-immune provocative inflammatory reaction to a foreign body, it also has a defining feature of activated epithelioid macrophages and multinucleated giant cells. The fibroblasts present usually produce cellular matrix components such as collagen, causing fibrosis (increase in collagen fibers of the connective tissue) and thus resolving the process. When the noxious stimulus is removed, these fibroblasts progressively disappear from the tissue [
30].
Different inflammatory cell populations in the junctional epithelium of the peri-implant mucosa result from the microbial challenge posed in the sulcus areas [
10]. The lateral cellular composition of the inflammatory activity presents a statistically significant difference in the number of nuclear polymorphs found, increasing in the provisional material concerning the definitive materials. An increase of polymorphonuclear leukocytes (PMN) in peri-implant tissue is considered a significant indicator of inflammation, which could lead to mucositis and peri-implantitis (Berglundh et al., 2018; Schwarz et al., 2018). A single-cell sequencing study supports the involvement of PMNs in inflammation, as it has shown elevated levels of CXCL8, a PMN-attracting cytokine, in peri-implant tissue [
31]. Therefore, the presence of PMNs and their association with inflammation could indicate an association with the pathogenesis of peri-implant diseases [
32,
33].
Similarly, when comparing the response generated by disilicate versus PMMA, a statistically significant difference is found in the increase in exocytosis in the peri-implant tissue around provisional restorations. This increase in exocytosis is another important indicator of inflammation, which, as we have previously mentioned with PMNs, could be related to the possible development of peri-implant diseases [
34,
35]. The oral mucosa mainly comprises a superficial epithelium attached to the connective tissue by a basal lamina. This oral epithelium is a keratinized or non-keratinized stratified squamous epithelium, whose primary function is defense against mechanical, microbial, and chemical damage [
35]. The non-keratinized epithelium has a higher permeability than the keratinized oral mucosa or skin. The healthy gingival epithelium has a mean thickness of 285.04 ± 32.98 µm, its maximum non-pathological value being 333.04 ± 32.98 µm [
36]. It is noted that, among the materials examined in this study, no material caused pathological epithelial thickening. It was recorded that zirconium generated a more significant thickening of the non-keratinized epithelium within the physiological mean. We could indicate that an increase in the thickness of the epithelium implies an increase in all cell populations (epithelial cells, Langerhans cells, lymphocytes, etc.) and in the desmosomal junctions and collagen fibers that are established between them, providing a more significant barrier function and defense against microorganisms and pathological substances.
Characteristics such as surface roughness, surface energy, and the relationship of the material with the gingiva influence the state of the peri-implant mucosa and bacterial proliferation [
37]. Many current studies present different systems for modifying the zirconium oxide surface to improve its biological properties [
38,
39,
40,
41]. A smooth surface promotes good soft tissue sealing and less bacterial colonization [
42]. Zirconium oxide is a bioinert ceramic material that allows rapid fibroblastic proliferation on its surface, creating an excellent mucosal barrier. It also inhibits bacterial adhesion due to its hydrophobicity, surface wettability, and reduced surface energy [
42]. Monolithic zirconia restorations of nanometer particles have been shown to exhibit improved physical and translucency properties, and their excellent biocompatibility may indicate a high potential for clinical application [
38].
Based on the results obtained, we can assume that zirconia is the material presenting the most adequate biological response of peri-implant tissues. It shows a lower intensity of inflammatory cellular content with a predominance of lymphocytes. Likewise, it presents a total normality in the number of collagen fibers. The arrangement of the fibers is normal in 90% of the cases, and vascular proliferation of the connective tissue occurs in 83% of the cases. These parameters make it a material with a predictable response.